Abstract
Introduction
Mycoplasma pneumoniae necrotizing pneumonia (MPNP) is an uncommon but increasingly recognized severe complication of pneumonia, and the delayed diagnosis and treatment are prone to pulmonary sequelae. The aim of this study is to explore independent risk factors for MPNP in children with lung consolidation.
Methods
A retrospective observational study was conducted on 118 children with MPNP (MPNP group) and 184 children with lung consolidation of Mycoplasma pneumoniae pneumonia (MPP) (control group) admitted to Children’s Hospital Affiliated to Zhengzhou University from June 2018 to August 2023. Clinical manifestations and laboratory data were analyzed and the independent risk factors for MPNP in children were analyzed by multivariate logistic regression.
Results
The age of onset, hospitalization days, fever days, proportion of dyspnea, chest pain, complications, and need for fiberoptic bronchoscopic alveolar lavage (FBAL) were higher than those in the control group, and the difference was statistically significant (P < 0.05). The levels of white blood cells (WBC), platelets, neutrophil percentage (N%), neutrophil-to-lymphocyte ratio (NLR), C-reactive protein (CRP), fibrinogen (Fbg), D-dimer (D-D), erythrocyte sedimentation rate (ESR), alanine transaminase (ALT), γ-glutamyl transpeptidase (γ-GGT), globulin, lactate dehydrogenase (LDH), α-hydroxybutyrate dehydrogenase (α-HBDH), urea, immunoglobulin G (IgG), immunoglobulin M (IgM), immunoglobulin A (IgA), complement component 3, antistreptolysin O (ASO), serum ferritin, and interleukin-6 (IL-6) in the MPNP group were higher than those in the control group. Red blood cell (RBC), lymphocyte percentage (L%), activated partial thromboplastin time (APTT), alkaline phosphatase (ALP), total protein, albumin, albumin-to-globulin ratio (AGR), creatine kinase (CK), uric acid, natrium, chlorine, calcium, and complement C4 in the MPNP group were lower than those in the control group, and the difference was statistically significant (P < 0.05). The results of multivariate logistic regression analysis showed that age ≥ 83.50 months, fever days ≥ 10.50, ALT ≥ 15.25 U/l, IgM ≥ 1.46 g/l, complement C3 ≥ 1.47 g/l, Fbg ≥ 3.93 g/l, dyspnea and needing FBAL were independent risk factors for MPNP in children.
Conclusions
Age, fever days, ALT, IgM, complement C3, Fbg, dyspnea, and needing FBAL were independent risk factors for MPNP in children. For children suspected of MPNP, pediatricians should pay close attention to the above indicators, strive for early diagnosis and treatment, and improve prognosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Mycoplasma pneumoniae necrotizing pneumonia (MPNP) is an uncommon but increasingly recognized severe complication of pneumonia, and the delayed diagnosis and treatment are prone to pulmonary sequelae. The aim of this study was to explore independent risk factors for MPNP in children with lung consolidation. |
What was learned from the study? |
Age, fever days, ALT, IgM, complement C3, Fbg, dyspnea, and needing FBAL were independent risk factors for MPNP in children. Furthermore, combining the above eight indexes could further improve the test efficiency [AUC (95% CI) = 0.883 (0.841–0.924)]. |
Introduction
Mycoplasma pneumoniae (MP) is one of the major causes of community-acquired pneumonia in children aged 5 years and older [1]. Mycoplasma pneumoniae pneumonia (MPP) is generally considered to be a mild and self-limiting disease but tends to occur in younger patients, with high mortality and complication rates [2]. Approximately 12% of children with MPP progress to severe Mycoplasma pneumoniae pneumonia (SMPP) or refractory Mycoplasma pneumoniae pneumonia (RMPP) [3], which can lead to severe intrapulmonary lesions such as pleural effusion, lung consolidation, pulmonary embolism, and even necrotizing pneumonia (NP). It can also cause serious extrapulmonary complications of the circulatory, digestive, blood, urinary, neurological, musculoskeletal, cutaneous mucosal, and other systems [1, 4].
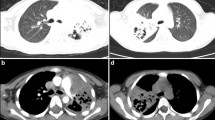
NP is usually caused by Streptococcus pneumoniae and Staphylococcus aureus [5]. In recent years, the incidence of Mycoplasma pneumoniae necrotizing pneumonia (MPNP) has been found to be on the rise, and MP is expected to become the main pathogen of NP [6]. Chest imaging of MPNP shows lung consolidation in the early stage of the disease, and secondary liquefaction and necrosis at the later stage in the lung consolidation area. NP is an uncommon but increasingly recognized severe complication of pneumonia where the delayed diagnosis and treatment are prone to pulmonary sequelae [5]. The clinical diagnosis of NP is based on the features shown in chest imaging, but its early diagnostic value is not high, and the diagnostic accuracy is affected by lung consolidation and pleural effusion. The delayed diagnosis of NP will lead to the extension of fever days and hospitalization days, which can affect the treatment and prognosis of children. However, there are few studies on the risk factors for MPNP in children. Therefore, it is of great clinical significance to explore independent risk factors for MPNP in children with lung consolidation. The aim of this study was to retrospectively analyze the clinical characteristics of lung consolidation and NP in children with MPP and to explore the independent risk factors for MPNP.
Methods
Study Population
A retrospective observational study was conducted on 118 children with MPNP (MPNP group) and 184 children with lung consolidation of MPP (control group) admitted to Children’s Hospital Affiliated to Zhengzhou University from June 2018 to August 2023. This study was approved by the Ethics Committee of Children's Hospital of Henan Province (2023-K-128). The need for informed consent was waived given the retrospective nature of the study, this study was conducted in accordance with the declaration of Helsinki.
The diagnosis of MPP was in accordance with the Guidelines for Diagnosis and Treatment of Mycoplasma pneumoniae Pneumonia in Children (2023 Edition) [7] to meet the following three points: (1) with fever, cough, wheezing, dyspnea, pulmonary rales and other respiratory manifestations; (2) chest imaging examinations were consistent with pneumonia; (3) compliance with ≥ 1 item: ① single serum MP antibody titer ≥ 1:160 (PA method); in the course of disease, the titer of double serum MP antibody increased by four times or more; ② positive MP-DNA or MP-RNA.
The inclusion criteria of the MPNP group were: (1) Age < 18 years; (2) The patient met the diagnostic criteria for MPP; (3) The patient met the diagnostic criteria for NP: patients with multiple air sacs or thin-walled cavities with empty air in the area of lung consolidation indicated chest imaging examination.
The inclusion criteria of the control group were: (1) Age < 18 years; (2) The patient met the diagnostic criteria for MPP; (3) The patient met the diagnostic criteria for lung consolidation: diagnosis of lobar/pulmonary segmental consolidation confirmed by chest imaging examination, with large hyperdense shadow or infiltrative changes in the lung parenchyma.
Exclusion criteria were: (1) Admission to the hospital during the MPP recovery period (patients with a disease course of more than 4 weeks, stable temperature for more than 1 week, and imaging absorption improvement); (2) Incomplete medical records.
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Children's Hospital of Henan Province (2023-K-128). The need for informed consent was waived given the retrospective nature of the study.
Data Extraction
Clinical data were collected retrospectively from patients' medical records. Outcome indicators were: (1) general data; (2) clinical manifestations; (3) co-pathogen infection; and (4) laboratory data.
Statistical Analysis
SPSS 27.0 statistical software was used for data analysis. Quantitative data of normal distribution are expressed as the mean ± standard deviation (\(\bar{\chi }\)± S), while non-normally distributed data are expressed as the median (interquartile distance) [M (Q1, Q3)]. Two-sample t tests or Mann–Whitney U tests were used for comparisons between groups. The categorical variable was expressed as the number of cases (percentage) [n (%)], and the component comparison was determined by the Chi-square test. Multivariate logistic regression analysis was used to explore the risk factors for MPNP. ROC curves were used to evaluate the efficacy of the study indicators in predicting MPNP. P < 0.05 was considered statistically significant.
Results
General Data
The age of onset was 84.00 (61.00–96.00) months in the MPNP group and 66.00 (41.25–84.00) months in the control group, and the difference was statistically significant (P < 0.05, Table 1). There were no significant differences in sex or primary disease between the two groups (P > 0.05, Table 1). The male-to-female ratio of MPP lung consolidation in children was 1.19:1. Among 302 MPP children with lung consolidation, 10.93% (n = 33) had primary diseases. There were ten cases of rhinitis or sinusitis, four cases of epilepsy, three cases of atrial septal defect, and two cases of Down syndrome. In addition, they may have primary diseases, including hydronephritis with ureterolithiasis, gallstones, rickets, anaphylactoid purpura, nutcracker syndrome, immune vasculitis, fused kidney, hydronephritis with kidney stones, growth retardation, ventricular septal defect, pulmonary artery fistula, inferior vena cava malformation, asthma, hereditary spherocytosis, and cold agglutination.
Clinical Manifestations
All patients developed a fever. Among them, 291 (96.40%) patients had a cough, and 46 (15.23%) had abdominal discomfort. There were no significant differences in the proportions of cough and abdominal discomfort between the two groups (P > 0.05, Table 1, Fig. 1).
The hospitalization days, fever days, dyspnea, proportions of chest pain and complications, and need for FBAL in the MPNP group were significantly higher than those in the control group (P < 0.05, Table 1, Fig. 1). A total of 99.34% of MPP patients with lung consolidation underwent fiberoptic bronchoscopy, and 76.16% had FBAL performed.
In addition, there were statistically significant differences in complications between the two groups. The proportions of complications in the respiratory, digestive, blood, and cutaneous mucosal systems in the MPNP group were higher than those in the control group (P < 0.05, Table 1). However, there was no significant difference in the proportion of circulatory or neurological complications between the two groups (P > 0.05, Table 1). Circulatory complications included pericardial effusion in 32 cases, myocardial damage in 15 cases, coronary dilation in two cases and infective endocarditis in one case. Neurological complications can manifest as nerve damage, encephalitis, toxic encephalopathy, ventricular dilatation, and others. Each system complication may have one or more manifestations. Details of complications in MPP children with lung consolidation are shown in Fig. 2.
Co-pathogen Infection
All patients were tested for etiology, and there was no significant difference in co-pathogen infection between the two groups (P > 0.05, Table 1). Among the study subjects, 120 patients (39.74%) were infected with other pathogens, among which viral co-infection was the highest, followed by bacterial co-infection, and fungal co-infection was the lowest. Co-infection with multiple pathogens was not uncommon. Details of co-pathogen infection in MPP children with lung consolidation are shown in Fig. 3.
Laboratory Data
There were no significant differences in prothrombin time (PT), glutamic oxaloacetic transaminase (AST), creatine kinase isoenzyme (CK-MB), creatinine, kalium, and procalcitonin (PCT) between the two groups (P > 0.05, Table 2).
WBC, platelet, N%, NLR, CRP, Fbg, D-D, ESR, ALT, γ-GGT, globulin, LDH, α-HBDH, carbonyldiamide, IgG, IgM, IgA, complement C3, ASO, ferroprotein and IL-6 in the MPNP group were higher than those in the control group. RBC, L%, APTT, ALP, total protein, albumin, AGR, CK, uric acid, natrium, chlorinum, calcium, and complement C4 were lower than those in the control group (P < 0.05, Table 2).
Logistic Regression Analysis
First, univariate logistic regression analysis was performed for the above indicators with statistically significant differences between the two groups, and a total of 35 potential risk factors for MPNP were screened. Second, multicollinearity analysis was carried out. Finally, multivariate logistic regression analysis showed that age, febrile days, ALT, IgM, complement C3, Fbg, dyspnea, and needing FBAL were independent risk factors for MPNP in children (P < 0.05, Table 3).
ROC Curve
ROC curve analysis showed that age, fever days, ALT, IgM, complement C3, Fbg, dyspnea, and needing FBAL were all valuable in predicting MPNP in children. MPP children with age ≥ 83.50 months, fever days ≥ 10.50, ALT ≥ 15.25 U/l, IgM ≥ 1.46 g/l, complement C3 ≥ 1.47 g/l, Fbg ≥ 3.93 g/l, dyspnea, and need for FBAL were associated with an increased risk of MPNP. Moreover, the combination of the above eight indexes could further improve the test efficiency [AUC (95% CI) = 0.883 (0.841–0.924)] (P < 0.05, Table 4, Fig. 4).
Discussion
In recent years, MP has gradually become one of the main pathogens of community-acquired pneumonia in children, and the incidence of MPNP has also increased. MP is expected to surpass Streptococcus pneumoniae and Staphylococcus aureus to become the main pathogen of NP [8, 9]. MPNP is a serious complication of MPP and is often accompanied by pulmonary embolism, empyema, and bronchopleural fistula. NP is mostly self-limited and reversible in children and has a good prognosis [5]. However, the delayed diagnosis and treatment of NP is prone to pulmonary sequelae. Therefore, actively exploring the risk factors for MPNP, improving diagnostic efficiency to help pediatricians diagnose and treat MPNP early, and avoiding serious sequelae have gradually become the focus of MPP. The purpose of this study was to retrospectively analyze the clinical characteristics of MPP lung consolidation in children, explore independent risk factors for MPNP, and establish joint predictors. We hope to provide a reference for the early diagnosis and treatment of MPNP.
The pathogenesis of NP may be related to various host susceptibility and bacterial virulence factors, and virus–bacteria interactions may also play an important role [10]. Under the action of inflammatory factors, abnormalities in the fibrinolysis coagulation system can cause pulmonary capillaries to be blocked by thrombosis and then cause pulmonary parenchymal ischemia and necrosis [11, 12].
Studies have shown that the combination of clinical features and laboratory indicators can effectively predict the occurrence of MPNP [13, 14]. Therefore, this study comprehensively considered the above indicators and explored the risk factors for MPNP. The results showed that age ≥ 83.50 months, IgM ≥ 1.46 g/l, complement C3 ≥ 1.47 g/l, Fbg ≥ 3.93 g/l, ALT ≥ 15.25 U/l, fever days ≥ 10.50, dyspnea, and needing FBAL were independent risk factors for MPNP in children.
MPP can be seen in all stages of children, but it is more common in preschool and school-age children. The immune response of the body is closely related to the severity of MPP, and older children have stronger immune responses and are more prone to MPNP [12]. Kutty [3] and Xia Wang [6] noted that the median age of MPP children was 7.0 (4.0–11.0) years and 5.1 (4.0–7.9) years, respectively. Ding Lin [21] further found that SMPP was mainly found in preschool children, and the incidence of SMPP in infants was significantly lower than that in other age groups. The population median age of our study was 72 (50–96) months, which is roughly consistent with the above studies. The occurrence of MPP lung consolidation and MPNP and other severe cases is rare in children under 3 years old, which may be related to the imperfection of infant immune function and the relatively low immune response stimulated by MP infection. In addition, we also found that the age of onset in the MPNP group was higher than that in the control group, suggesting that the severity of the disease was related to immune function. The immune system of older children is relatively mature, and the resistance is stronger. When MP infects older children, the immune system is activated, a large number of inflammatory cells and inflammatory factors are produced to promote the progression of MPP, and NP is more likely to occur.
Children with MPP often have cellular and humoral immune dysfunction, and dynamic monitoring of serum complement, immunoglobulin, and inflammatory cytokines is of great value in assessing the stage and severity of the disease. Relevant studies have shown that the levels of IgM and complement C3 in MPP children are both elevated, which are related to the severity of the disease [15]. Our results are consistent with this finding. After MP infection, B cells are activated to secrete immunoglobulin, and IgM is the main immune response in the acute phase [16]. The production of MPNP is related to the persistence of pathogens, immune function, and overactivation of the complement system. Therefore, IgM and complement C3 in the MPNP group were significantly higher than those in the control group.
Severe pneumonia is often accompanied by fibrinolytic coagulation system abnormalities and the release of a large number of inflammatory cytokines. Coagulation disorders are closely related to the severity of the disease. MPNP may be caused by an overreaction of immune inflammation, with abnormal changes in coagulation indexes (such as D-D and Fbg). Studies have shown that D-D and Fbg are significantly increased in severe pneumonia, and the combination is beneficial to disease diagnosis and prognosis assessment and can be used as a predictor of severe pneumonia [17, 18]. Wei Na [19] found that Fbg and D-D in MPP children were higher than those in healthy children. Moreover, Beilei Yang [12] found that Fbg in the MPNP group increased more significantly. The results of this study are consistent with the above, and the abnormal increase in Fbg and D-D is considered to be related to the enhancement of coagulation function. In a normal physiological state, the fibrinolysis and coagulation systems in the body are in dynamic balance. However, the immune inflammatory response in MPP children is activated, which abnormally enhances coagulation function and thrombosis formation, aggravating the progression of the disease. In addition, Fbg is also an acute phase protein synthesized by the liver, which is mostly associated with nonspecific inflammatory responses. Chinese clinical studies have shown that the increase in the Fbg level is related to the degree of infection, the number of infectious pathogens, the severity of the disease, and the prognosis [18].
Children with MPP with elevated ALT, persistent high fever, and dyspnea are at significantly increased risk of developing severe and critical illness [7]. It is necessary to identify early and avoid lung consolidation and NP. Our findings are consistent with the above. In addition, we found that ALT, fever days, and dyspnea were independent risk factors for MPNP. We also found that the combination of ALT, fever days, dyspnea, age, Fbg, IgM, complement C3, and needing FBAL could further improve the efficacy of the test and predict MPNP better in children.
ALT is recognized as a potential risk factor for severe MPP cases, and there are few studies related to MPNP in children. Recent studies have shown that ALT is significantly increased in MPNP and RMPP and is correlated with the severity of the disease [20, 21]. Hepatic function damage is not uncommon in severe MPP cases and is accompanied by changes in ALT and AST. Its pathogenesis may be caused by the indirect immune response of liver tissue to pathogens, rather than the direct invasion of liver tissue by MP [22]. Among 302 children, 44 (14.57%) had liver function impairment and significantly elevated ALT, and ALT was more significantly elevated in the MPNP group. In addition, Chen Yu [23] found that ALT was significantly elevated in children with macrolide-resistant MPP. Moreover, ALT combined with prolonged heating time, decreased blood oxygen saturation and increased LDH had a certain suggestive effect on RMPP.
In this study, the hospitalization days and fever days in the MPNP group were significantly higher than those in the control group and were closely related (P < 0.01). This is consistent with the results of many domestic and foreign studies [6, 11, 20]. The increase in hospitalization days and fever days was considered to be related to prolonged disease caused by an excessive inflammatory response and severe lung injury.
We found that the rate of dyspnea in the MPNP group was significantly higher than that in the control group (22.00%: 4.90%). Beilei Yang [12] found that the incidence of dyspnea in 11 children with MPNP was 45.45%, which was significantly lower than that of NP infected by other pathogens. Our different results are considered to be caused by the difference in data sample size. Our sample size is larger, with higher reliability and accuracy.
FBAL has both diagnostic and therapeutic functions. It has incomparable advantages over conventional diagnostic techniques and traditional treatments in the diagnosis and treatment of children with MPP, and its treatment efficiency is as high as 90% [24]. FBAL can effectively reduce symptoms, prevent disease progression, and avoid surgical intervention, making it an essential diagnostic and treatment method for children with MPP, SMPP, and RMPP. We found that needing FBAL can be used as a good predictor of MPNP in children, and its sensitivity is as high as 96.60%.
In addition, peripheral blood examination is an important method for detecting MPP and can be used to predict the risk of MPP and SMPP. The WBC, N%, L%, CRP, ESR, and D-D in peripheral blood can all be used as biomarkers of the immunoinflammatory response and are correlated with the severity of MPP [7]. Our research is consistent with that. The results showed statistically significant differences between the two groups, which were potential risk factors for MPNP, suggesting a high probability of MPNP occurrence.
We also found that the MPNP group had lower AGR and higher NLR compared to the control group. Both AGR and NLR are potential risk factors for MPNP and have important clinical value. AGR and NLR are considered to be related to the inflammatory state of the body and have greater clinical predictive value. In recent years, AGR and NLR have been used in the diagnosis, treatment, and severity assessment of MPP and have become new biomarkers for the diagnosis and prediction of MPP [25, 26]. In addition, Zheng [26] noted that the NLR is of great significance in the differential diagnosis of MPP and bacterial pneumonia. At present, there are few relevant studies on AGR and NLR in MPP lung consolidation and MPNP, and further studies are needed.
Relevant literature has suggested that primary disease and co-infection may be potential risk factors for SMPP [7, 27]. However, in this study, there was no significant difference in primary disease and co-infection between the MPNP and control groups. Considering that the sample size was relatively small and our study subjects were all SMPP, there might be selection bias. In recent years, the number of severe cases caused by MP combined with bacterial or viral infection in children has been on the rise [27, 28]. In this study, the co-infection rate was as high as 39.74% in all subjects. The clinical characteristics of pediatric pneumonia caused by mixed infection with multiple pathogens may not be typical, which makes it easy to delay diagnosis. Therefore, the occurrence of NP should be highly vigilant for MPP children with co-infection.
There are some limitations to this study. First, our sample size was relatively small. Second, this was a single-center retrospective study, with possible selection bias.
Conclusions
In conclusion, age ≥ 83.50 months, fever days ≥ 10.50, ALT ≥ 15.25 U/l, IgM ≥ 1.46 g/l, complement C3 ≥ 1.47 g/l, Fbg ≥ 3.93 g/l, dyspnea, and needing FBAL were independent risk factors for MPNP in children. Pediatricians should combine the above indicators to judge the condition of MPP children to make an early diagnosis, effective treatment, and improve prognosis.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Waites KB, et al. Mycoplasma pneumoniae from the respiratory tract and beyond. Clin Microbiol Rev. 2017;30(3):747–809.
Li ZJ, et al. Etiological and epidemiological features of acute respiratory infections in China. Nat Commun. 2021;12(1):5026.
Kutty PK, et al. Mycoplasma pneumoniae among children hospitalized with community-acquired pneumonia. Clin Infect Dis. 2019;68(1):5–12.
Moynihan KM, et al. Severe Mycoplasma pneumoniae infection in children admitted to pediatric intensive care. Pediatr Infect Dis J. 2018;37(12):e336–8.
Masters IB, Isles AF, Grimwood K. Necrotizing pneumonia: an emerging problem in children? Pneumonia (Nathan Qld). 2017;9:11.
Wang X, et al. Necrotizing pneumonia caused by refractory Mycoplasma pneumoniae pneumonia in children. World J Pediatr. 2018;14(4):344–9.
China NHCOTPSRU. Guidelines for diagnosis and treatment of Mycoplasma pneumoniae pneumonia in children (2023 Edition). China Licens Pharm. 2023;20(3):16–24.
Sawicki GS, et al. Necrotising pneumonia is an increasingly detected complication of pneumonia in children. Eur Respir J. 2008;31(6):1285–91.
Jing Q, et al. Analysis of clinical features and risk factors of necrotizing pneumonia in children. J Peking Univ (Health Sci). 2022;54(03):541–7.
Hsieh Y-C, et al. Clinical manifestations and molecular epidemiology of necrotizing pneumonia and empyema caused by Streptococcus pneumoniae in children in Taiwan. Clin Infect Dis. 2004;38(6):830–5.
Zheng B, Zhao J, Cao L. The clinical characteristics and risk factors for necrotizing pneumonia caused by Mycoplasma pneumoniae in children. BMC Infect Dis. 2020;20(1):391.
Yang B, et al. Differences of clinical features and prognosis between Mycoplasma pneumoniae necrotizing pneumonia and non-Mycoplasma pneumoniae necrotizing pneumonia in children. BMC Infect Dis. 2021;21(1):797.
Sauteur PMM, et al. Improved diagnostics help to identify clinical features and biomarkers that predict Mycoplasma pneumoniae community-acquired pneumonia in children. Clin Infect Dis. 2020;71(7):1645–54.
Chen J, et al. Mycoplasma pneumoniae infection prediction model for hospitalized community-acquired pneumonia children. Pediatr Pulmonol. 2021;56(12):4020–8.
Feibo G, et al. Value of changes of serum complement, immunoglobulin and inflammatory cytokines in children with Mycoplasma pneumonia. Chin J Immunol. 2017;33(6):910–3.
Lan-fang L, Xiao-bing L, Lan-qing Z. Analysis of changes of serum immunoglobulin, erythrocyte immunity and peripheral blood T lymphocyte subsets after Mycoplasma pneumoniae infection in children. Mater Child Health Care China. 2015;30(3):385–7.
Xin T. Changes and clinical significance of sTREM-1, fibrinogen and D-dimer levels in severe pneumonia patients. J Clin Pulm Med. 2018;23(9):1699–702.
Li H, Jun Z, Tie-shuan Z. Changes of D-dimer, fibrinogen and IL-6 levels in patients with severe pneumonia and their clinical significance. Chin J Respir Crit Care Med. 2017;16(1):71–3.
Na W. Changes and clinical significance of related index levels of blood coagulation function and immune function in children with Mycoplasma pneumoniae pneumonia. China Med Herald. 2016;13(32):94–7.
Zhi-long W, Zhi-ying H, Wei W. Analysis on the risk factors of Mycoplasma pneumoniae necrotizing pneumonia in children. Chin J New Clin Med. 2023;16(5):500–5.
Huang X, et al. Clinical significance of D-dimer levels in refractory Mycoplasma pneumoniae pneumonia. BMC Infect Dis. 2021;21(1):14.
Izumikawa K. Clinical features of severe or fatal Mycoplasma pneumoniae pneumonia. Front Microbiol. 2016;7:800.
Yu C, et al. Clinical features and treatment of macrolide-resistant Mycoplasma pneumoniae pneumonia in children. Chin J Contemp Pediatr. 2018;20(8):629–34.
Yan H. The advantages of bronchoalveolar lavage in the diagnosis and treatment of Mycoplasma pneumoniae pneumonia. Med Philos. 2018;39(01):16–8.
Kim YJ, Park KS, Cho SY. Mean platelet volume in pediatric patients infected with Mycoplasma pneumoniae. Clin Lab. 2021. https://doi.org/10.7754/Clin.Lab.2020.200944.
Zheng HH, et al. Clinical value of blood related indexes in the diagnosis of bacterial infectious pneumonia in children. Transl Pediatr. 2022;11(1):114–9.
Li F, et al. Mycoplasma pneumoniae and adenovirus coinfection cause pediatric severe community-acquired pneumonia. Microbiol Spectr. 2022;10(2): e0002622.
Choo S, Lee YY, Lee E. Clinical significance of respiratory virus coinfection in children with Mycoplasma pneumoniae pneumonia. BMC Pulm Med. 2022;22(1):212.
Acknowledgements
The authors sincerely thank the participants of the study.
Funding
No funding was secured for this study. The journal’s fee was funded by the authors.
Author information
Authors and Affiliations
Contributions
Xue Zhang participated in research design, data collection, data analysis, and writing. Ruiyang Sun, Wanyu Jia, and Peng Li participated in research design and data analysis. Chunlan Song participated in the study design and critically revised the important knowledge content.
Corresponding author
Ethics declarations
Conflict of Interest
Xue Zhang, Ruiyang Sun, Wanyu Jia, Peng Li and Chunlan Song declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethical Approval
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Children's Hospital of Henan Province (2023-K-128). The need for informed consent was waived given the retrospective nature of the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Zhang, X., Sun, R., Jia, W. et al. Clinical Characteristics of Lung Consolidation with Mycoplasma pneumoniae Pneumonia and Risk Factors for Mycoplasma pneumoniae Necrotizing Pneumonia in Children. Infect Dis Ther 13, 329–343 (2024). https://doi.org/10.1007/s40121-023-00914-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-023-00914-x