Abstract
Introduction
Invasive Escherichia coli disease (IED) can lead to sepsis and death and is associated with a substantial burden. Yet, there is scarce information on the burden of IED in Asian patients.
Methods
This retrospective study used US hospital data from the PINC AI™ Healthcare database (October 2015–March 2020) to identify IED cases among patients aged ≥ 60 years. IED was defined as a positive E. coli culture in blood or other normally sterile body site (group 1 IED) or positive culture of E. coli in urine with signs of sepsis (group 2 IED). Eligible patients with IED were classified into Asian and non-Asian cohorts based on their reported race. Entropy balancing was used to create cohorts with similar characteristics. Outcomes following IED were descriptively reported in the balanced cohorts.
Results
A total of 646 Asian and 19,127 non-Asian patients with IED were included (median age 79 years; 68% female after balancing). For both cohorts, most IED encounters had community-onset (> 95%) and required hospitalization (Asian 96%, mean duration 6.9 days; non-Asian 95%, mean duration 6.8 days), with frequent admission to intensive care (Asian 35%, mean duration 3.3 days; non-Asian 34%, mean duration 3.5 days), all standardized differences [SD] < 0.20. Compared to non-Asian patients, Asian patients were more likely to be discharged home (54% vs. 43%; SD = 0.22), and less likely to be discharged to a skilled nursing facility (24% vs. 31%; SD = 0.16). In-hospital fatality rates during the IED encounter were similar across cohorts (Asian 9%, non-Asian 10%; SD = 0.01). Most E. coli isolates showed resistance to ≥ 1 antibiotic (Asian 61%; non-Asian 64%) and 36% to ≥ 3 antibiotic classes (all SD < 0.20).
Conclusion
IED is associated with a substantial burden, including need for intensive care and considerable mortality, in Asian patients in the USA that is consistent with that observed for non-Asian patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out the study? |
Invasive Escherichia coli disease (IED) is a growing problem globally, but there is a paucity of data available on how the burden of disease affects Asian populations. |
We assessed clinical outcomes, medical resource utilization, and antibiotic resistance in Asian and non-Asian patients with IED in a US hospital-based database. |
What was learned from the study? |
The findings from this study indicate that IED is associated with a substantial burden, including need for intensive care and considerable mortality, in Asian patients that is consistent with that observed for non-Asian patients. |
This highlights the need for preventative measures that have the potential to reduce the clinical and economic burden associated with IED for both Asian and non-Asian patients. |
Introduction
Invasive Escherichia coli disease (IED) is a spectrum of disease states that resemble acute E. coli infection, encompassing urosepsis, bacteremia, meningitis, and peritonitis (among others), with potentially severe outcomes including sepsis and death [1,2,3,4,5]. IED may be classified into two subtypes based on the site of infection [2, 6]. Group 1 IED is identified by a positive E. coli culture in a specimen from blood or other normally sterile body site in a patient with signs of systemic inflammatory response syndrome (SIRS) and/or sepsis, and group 2 IED is identified by a positive E. coli culture from a urine sample in a patient with sepsis and no culture positive for E. coli from a normally sterile body site [2, 6]. Despite a relatively low incidence [7], IED is associated with substantial clinical and economic burden, especially among older patients. In a large study conducted in the USA, 97% of IED cases required hospitalization, with more than one-third of patients admitted to intensive care and 7% who died during the IED encounter [8]. Further, more than one-third of E. coli isolates showed multidrug resistance [8]. Antimicrobial resistance in E. coli is on the rise globally, including in Asian countries such as China and Japan, and is a major concern as it can increase the clinical and economic burden of IED [9,10,11].
Given the substantial disease and healthcare burden associated with IED, there is interest in understanding the factors that influence disease risk and outcomes. Age older than 60 years is a well-known risk factor for E. coli bacteremia [7]. Meanwhile, race/ethnicity may play a role in the incidence and severity of outcomes related to sepsis [8]: some US studies have reported differences in outcomes between Blacks or African-Americans compared with non-Hispanic Whites, although these analyses were confounded by socioeconomic status, type of insurance, or hospital-related factors [12,13,14]. By comparison, information on Asian patients in the USA is fairly limited, with conflicting results. For example, in-hospital sepsis mortality rates were found to be higher among Asian/Pacific Islander patients than among White, Black, and Hispanic patients in one study [12], whereas another study found that Asian-American patients had the lowest rates of sepsis-related mortality [15]. More generally, there are differences in the risks of certain comorbidities and health outcomes between Asian-Americans and non-Hispanic Whites or other minorities which could impact the prognosis following IED [16,17,18].
Although equality is a goal of US public health policy, there has been relatively little research focused on the health and healthcare of Asian-Americans compared with that for African-Americans and Hispanic/Latinos [19]. The aim of this retrospective study was to address this knowledge gap by characterizing the clinical burden of IED in Asian patients as well as non-Asian patients treated at US hospitals.
Methods
Data Source
Data from the PINC AI™ Healthcare database [20] from October 2015 to March 2020 were used to include recent data, but limit the potential impact of the COVID-19 pandemic on outcomes following IED. This hospital database from a representative set of more than 1000 US hospitals across all US regions includes information on patient demographics (e.g., age, race, primary payer), diagnoses, procedures, inpatient services, and hospital characteristics (e.g., number of beds, urban vs. rural, region). A subset of hospitals (approx. 25%) contribute microbiology laboratory data (e.g., specimen source, tests performed) enabling the microbiological confirmation of IED cases.
Study Design and Sample Selection
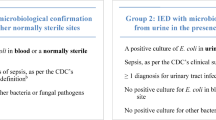
This was a descriptive retrospective study, for which the index date was defined as the date of the first observed IED encounter (index IED encounter; Fig. 1). Outcomes were assessed during the initial IED encounter and for up to 12 months following this encounter (i.e., observation period). IED was defined and classified on the basis of two types of infection and clinical signs (Fig. 2). Group 1 IED included patients with a positive E. coli culture in blood or other normally sterile body site, and at least one sign of SIRS, or signs of sepsis (as per the Centers for Disease Control and Prevention [CDC] clinical surveillance definition [21]) without a positive culture for other bacterial or fungal pathogens. Group 2 IED included patients with a positive culture of E. coli in urine in the presence of signs of sepsis (according to the CDC clinical surveillance definition [21]), diagnosis for a urinary tract infection, and without a positive culture of E. coli in blood or normally sterile body sites, nor a positive culture for other bacteria or fungal pathogens.
IED definition. Abbreviations: CDC, Centers for Disease Control and Prevention; IED, invasive Escherichia coli disease [1]. Normally sterile body sites include cerebrospinal fluid, pleural fluid (chest fluid, thoracentesis fluid), peritoneal fluid (abdominal fluid, ascites), pericardial fluid, bone (including bone marrow), joint fluid (synovial fluid, fluid, needle aspirate, or culture of any specific joint such as knee, ankle, elbow, hip, wrist), and internal body sites (lymph node, brain, heart, liver, spleen, vitreous fluid, kidney, pancreas, ovary, vascular tissue, deep wound). [2] The sepsis clinical surveillance definition utilizes an algorithm defined by Rhee et al. [21] and details and diagnosis codes were updated using the CDC’s Hospital Toolkit for Adult Sepsis Surveillance (March 2018). The algorithm was validated using medical records from 510 randomly selected hospitalizations, stratified into those that did and did not meet sepsis surveillance criteria
Eligible patients had at least one IED encounter in a US hospital that provided microbiology data for at least 6 months before and at least 12 months after their first observed IED encounter and were aged 60 years or older at that time. Patients who were reported to be Asian in their hospital record based on the UB-04 Form were classified in the Asian cohort. The UB-04 Form defines a person of Asian race as having origins in any of the original peoples of the Far East, Southeast Asia, or the Indian subcontinent, including, for example, Cambodia, China, India, Japan, Korea, Malaysia, Pakistan, the Philippine Islands, Thailand, and Vietnam. All other patients were classified in the non-Asian cohort, including White, Black or African American, other races (i.e., American Indian or Alaskan Native, Native Hawaiian, or other Pacific Islander), and those that declined to answer.
Measures, Outcomes, and Statistical Analyses
Measures assessed included patient demographics at the index date (e.g., age, gender, insurance plan type), patient comorbidities, and Charlson-Quan comorbidity index [CCI] [22, 23] measured in the 6 months prior to the index date, and hospital size, region, teaching status, urban/rural setting at the index date. Outcomes included clinical course of the index IED (i.e., discharge status, in-hospital fatality, antibiotic use, and antibiotic resistance), IED recurrence during the 12 months follow-up, and medical resource utilization (all-cause and infection-related) for services received in inpatient and outpatient hospital settings both during the index IED and during the 12 months observation period. Infection-related medical resource utilization was identified on the basis of services for which a diagnosis for any infection was recorded.
Entropy balancing was used to reweight non-Asian patients such that they have similar characteristics as Asian patients [24], in an attempt to control for possible confounding variables that could create bias in the analyses. This reweighting method consists of identifying weights that satisfy a pre-defined set of balance constraints (i.e., equalizing moments of selected variables across cohorts), while remaining as close as possible to the original weights to minimize the loss of information. Compared to commonly used matching methods, it has the advantage to retain all subjects and limit the iteration over different matching methods to create balanced groups. Entropy balancing has also been shown to reduce bias and outperform other matching methods, such as inverse probability weighting [25,26,27]. In this study, entropy balancing was specified to equalize the mean and standard deviation of the following variables across cohorts: age, gender, payer type, calendar year, CCI, hospital size (i.e., number of beds), region, teaching hospital status, urban/rural setting. Measures and outcomes were descriptively reported for each study cohort separately using means, standard deviations, and medians for continuous variables, and frequencies and proportions for categorical variables. Standardized differences (SD) were used to assess effect sizes across cohorts, with values greater than 0.20 typically considered as a noticeable difference [28]. For completeness, results were reported for both the unweighted and weighted cohorts. Analyses were carried out using SAS Enterprise Guide statistical software and Stata Statistical Software, Release 16.
Results
Patient and Hospital Characteristics
After all inclusion criteria were applied, 19,773 patients were included in the sample, 646 (3%) Asian and 19,127 (97%) non-Asian patients (Fig. 3). Prior to balancing, Asian and non-Asian patients had relatively similar characteristics in terms of age (median 79 vs. 77 years, respectively), gender (68% vs. 67% female, respectively), mean CCI (2.2 vs. 2.5, respectively), and calendar year (all SD ≤ 0.20; Table 1). However, Asian patients were less likely to have Medicare coverage than non-Asian patients (80% vs. 88%, respectively), and less likely to have chronic pulmonary disease (14% vs. 26%, respectively, all SD > 0.20). There were also differences in terms of hospital characteristics, with Asian patients more likely to be treated in smaller hospitals and more likely to be treated in the West and in urban settings (all SD > 0.20). After weighting, all characteristics were well-balanced (all SD < 0.20; Table 1).
Clinical Course of Index Invasive Escherichia coli Disease, Recurrence, and Medical Resource Utilization
Clinical characteristics of the index IED encounters were generally similar among balanced cohorts (Table 2). For both cohorts, most encounters involved community-onset IED (> 95%) and required an inpatient stay (Asian 96%, mean duration 6.9 days; non-Asian 95%, mean duration 6.8 days; all SD < 0.20). In addition, more than one-third of patients were admitted to intensive care units during their index IED encounter (Asian 35%, mean duration 3.3 days; non-Asian 34% mean duration 3.5 days) and more than 1 in 10 received mechanical ventilation (Asian 12%; non-Asian 11%, all SD < 0.20). However, there were some differences observed in terms of the type of IED, with 67% of Asian and 55% of non-Asian patients having group 1 IED (44% and 33% had group 1 IED with sepsis, respectively, all SD > 0.20). Given that group 2 patients have sepsis by definition, the overall proportion of patients with sepsis was similar for both cohorts (Asian 76.8%; non-Asian 78.6%; SD = 0.04). While most patients originated from non-healthcare facilities (> 85% for both cohorts), Asian patients were more likely to be discharged home than non-Asian patients (54% vs. 43%; SD = 0.22), and less likely to be discharged to a skilled nursing facility (24% vs. 31%, SD = 0.16). In-hospital fatality rates were similar in both cohorts, with 9% of Asian patients and 10% of non-Asian patients having died during the IED encounter (SD = 0.01); these rates increased to 11.9% and 13.3%, respectively, at 12 months post-index (SD = 0.04; data not shown). During the index IED encounter, patients received several antibiotics, with an average of approximately three antibiotics per patient for both Asian and non-Asian patients and more than 30% receiving four or more different antibiotics (all SD < 0.20). Among patients with at least one antibiotic susceptibility test performed (i.e., > 95% of the sample), 61% of Asian and 64% of non-Asian patients showed resistance to any antibiotic and 36% of patients in both cohorts showed resistance to three or more antibiotic classes (all SD < 0.20).
In the 12-month observation period, IED recurrence rates were similar for Asian and non-Asian patients (3% vs. 2%, respectively; SD = 0.07). Among patients with IED recurrences, Asian patients had slightly fewer recurrences than non-Asian patients (1.1 vs. 1.3, respectively; SD = 0.69), but had these recurrences sooner (Asian 4.7 months post-index; non-Asian 5.3 months post-index; SD = 0.22). (Table 2). Medical resource utilization in the 12 months observation period (excluding the index IED encounter) was similar across the two cohorts for both all-cause and infection-related hospital visits (all SD < 0.20; Fig. 4). In particular, nearly 1 in 3 patients had an inpatient stay in the 12 months post-index (Asian 31%; non-Asian 34%), with more than 75% of these patients having infection-related inpatient stays.
Medical resource utilization in the 12-month observation period (excluding the index IED encounter) among weighted cohorts. Abbreviation: IED, invasive Escherichia coli disease. [1] All standardized differences < 0.20
Discussion
This retrospective study assessed the clinical burden of IED in Asian and non-Asian patients treated at hospitals in the USA. Prior to entropy balancing, Asian patients were less likely to be Medicare-insured and more likely to be treated at smaller hospitals located in the West and in an urban setting. This disparity in insurance coverage may be partly explained by ineligibility based on minimum work or residency requirements for foreign-born Americans [29, 30] and could impact the type of hospitals at which Asian patients seek care. After balancing the cohorts, outcomes following IED were largely similar including duration of hospitalizations, admission to intensive care units, antibiotic use, and antimicrobial resistance, suggesting a comparable and substantial burden for both Asian and non-Asian patients in the USA. However, Asian patients were more likely to be discharged back home and less likely to have IED recurrences than non-Asian patients. In addition, the findings from this study suggest that IED may be associated with increased risk of subsequent illnesses beyond the initial IED encounter, with nearly one-third of patients being re-hospitalized for any cause over the following year for both the Asian and non-Asian cohorts.
While published data on the clinical and economic burden of IED are limited, our findings for IED burden are consistent with that of two recent studies using the same database, although there are some differences in certain specific results reported due to different characteristics (e.g., lower proportion of Medicare-insured patients) after reweighting cohorts to be more similar to the Asian population in this US database [8, 31]. In line with the findings from these studies, a substantial proportion of patients were discharged to a healthcare facility (e.g., skilled nursing facility) despite not originating from such a facility. This was one of the most notable differences in outcomes between cohorts, with 54% of Asian patients discharged back home compared with just 43% of non-Asian patients. A recent retrospective study of Canadian inpatients receiving palliative care stratified by race/birth country also reported that Asian patients were the most likely among all racial/ethnic groups to be discharged home [32]. Although the reasons for this difference may be complex, cultural attitudes about family caregiving among Asian Americans have been previously highlighted [33]. A study of California Medicaid home- and community-based services found that Asians had a greater preference for receiving home care from family members compared with non-Hispanic Whites [34].
The current study also highlights the potentially fatal consequences of IED, with nearly 1 in 10 patients dying during the initial IED encounter. This is consistent with the results of other studies in which mortality rates among patients with IED ranged from 8% to 20% [2, 35], but diverge from reports of differences in mortality rates between Asian and non-Asian patients. For example, Jones et al. noted significantly higher in-hospital sepsis mortality rates in Asian/Pacific Islander compared with White patients [12]. In another study, Asian patients were reported to have lower mortality rates for abdominal and genitourinary sepsis compared with White patients, and the lowest mortality rates for pulmonary sepsis [15]. The association between race/ethnicity and disease risk/outcomes is influenced by multiple factors, and some differences between the present results and those of other studies may be attributable to community-, patient-, pathogen-, and hospital-related factors that could not be adjusted for [13]. Although our study focused on in-hospital fatality, it is possible that a larger proportion of Asian patients died at home after discharge, which would not have been captured in our dataset. Additionally, the non-Asian cohort included races/ethnicities (e.g., Black, Hispanic) that may be distinct categories in other studies. One patient-related factor that may be overlooked in studies with different racial/ethnic populations is English language proficiency. Indeed, a study of patients with sepsis admitted to a hospital between 2012 and 2016 found that 62% of patients with limited English proficiency (LEP) were Asian and that LEP was an independent predictor of mortality across all races except among Black and Hispanic patients [36].
This study found that the use of medical resources following the initial IED encounter was considerable, suggesting potential long-term consequences of IED and the need for additional monitoring. Other studies have also reported substantial healthcare resource utilization and clinical burden during both the index IED encounter and subsequent year [8, 31], highlighting the need for post-IED follow-up for patients with a higher risk of recurrence or adverse outcomes and the importance of allocating resources and establishing measures for preventing IED. To this end, there is great interest in developing a vaccine to prevent IED in vulnerable populations [3, 37]; a 9-valent vaccine candidate for active immunization of adults 60 years of age and older is currently being investigated in a phase 3 trial [38, 39].
Strengths and Limitations
One of the strengths of this study is the use of the PINC AI™ Healthcare database, providing a large representative sample of patients admitted to over 1000 hospitals from all US regions. Microbiology laboratory data, often not available in other administrative claims databases, included information on specimen source as well as the tests performed and the results, allowing identification of IED encounters based on confirmed microbiological data.
Nonetheless, this study has limitations which must be considered. First, while IED encounters were identified using actual results from microbiological laboratory tests, their classification also relied in part on diagnosis codes, and procedure codes; accordingly, some patients may have been misclassified as having, or not having, IED. Second, medical resource utilization for a given patient was only available for encounters at a given hospital, such that medical services or medication received outside of this hospital were not captured. Also, these assessments of resource use were based on administrative claims. Furthermore, outcomes were assessed during the 12-month period following the index IED encounter for all patients, regardless of mortality; given that some patients died before the end of the observation period, this may have resulted in lower average medical resource utilization. Third, Asian patients included in this study may not be representative of Asian populations outside the USA. Additionally, the non-Asian cohort included patients with “Unknown” race, which could conceivably include some Asian patients who did not report or were not assigned a race in their hospital record, leading to potential misclassification of Asians. Further, non-Asian patients included White non-Hispanic, African-American, and Hispanic/Latino patients; therefore, it may be a topic for future research to compare the burden of IED for Asian cohort against that for each of these race/ethnicity groups.
Finally, while Asian and non-Asian patients were balanced on observable characteristics, there may be residual confounding due to unobserved confounders (e.g., body mass index).
Conclusions
The findings from this study indicate that IED is associated with a substantial burden, including need for intensive care and considerable mortality, in Asian patients that is comparable to that observed in non-Asian patients. The burden experienced during the first IED encounter extended in each of the cohorts beyond the initial IED encounter and remained substantial over the following year. This highlights the need for additional monitoring for patients with a higher risk of recurrence or adverse outcomes and the importance of allocating resources and establishing measures for preventing IED.
Data Availability
The datasets generated during and/or analyzed during the current study are not publicly available as they were used under license with PREMIER.
References
Biran D, Ron EZ. Extraintestinal pathogenic Escherichia coli. Curr Top Microbiol Immunol. 2018;416:149–61.
Doua J, Geurtsen J, Rodriguez-Bano J, et al. Epidemiology, clinical features, and antimicrobial resistance of invasive Escherichia coli disease in patients admitted in tertiary care hospitals. Open Forum Infect Dis. 2023;10(2):ofad026.
Poolman JT, Wacker M. Extraintestinal pathogenic Escherichia coli, a common human pathogen: challenges for vaccine development and progress in the field. J Infect Dis. 2016;213(1):6–13.
GBD 2019 Antimicrobial Resistance Collaborators. Global mortality associated with 33 bacterial pathogens in 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2022;400(10369):2221–48.
Kaper JB, Nataro JP, Mobley HL. Pathogenic Escherichia coli. Nat Rev Microbiol. 2004;2(2):123–40.
Geurtsen J, de Been M, Weerdenburg E, Zomer A, McNally A, Poolman J. Genomics and pathotypes of the many faces of Escherichia coli. FEMS Microbiol Rev. 2022. https://doi.org/10.1093/femsre/fuac031.
Bonten M, Johnson JR, van den Biggelaar AHJ, et al. Epidemiology of Escherichia coli bacteremia: a systematic literature review. Clin Infect Dis. 2021;72(7):1211–9.
Hernandez-Pastor L, Geurtsen J, Baugh B, et al. Clinical burden of invasive Escherichia coli disease among older adult patients treated in hospitals in the United States. BMC Infect Dis. 2023;23(1):550.
Hu FP, Guo Y, Zhu DM, et al. Resistance trends among clinical isolates in China reported from CHINET surveillance of bacterial resistance, 2005–2014. Clin Microbiol Infect. 2016;22(Suppl 1):S9-14.
Ohmagari N, Choi WS, Tang HJ, et al. Targeted literature review of the burden of extraintestinal pathogenic Escherichia coli among elderly patients in Asia Pacific regions. J Med Econ. 2023;26(1):168–78.
Tsuzuki S, Matsunaga N, Yahara K, et al. National trend of blood-stream infection attributable deaths caused by Staphylococcus aureus and Escherichia coli in Japan. J Infect Chemother. 2020;26(4):367–71.
Jones JM, Fingar KR, Miller MA, et al. Racial disparities in sepsis-related in-hospital mortality: using a broad case capture method and multivariate controls for clinical and hospital variables, 2004–2013. Crit Care Med. 2017;45(12):e1209–17.
Ko RE, Suh GY. Factors underlying racial and gender disparities in sepsis management. In: The sepsis codex. St. Louis: Elsevier; 2023. p. 247–55.
Minejima E, Wong-Beringer A. Impact of socioeconomic status and race on sepsis epidemiology and outcomes. J Appl Lab Med. 2021;6(1):194–209.
Prest J, Nguyen T, Rajah T, Prest AB, Sathananthan M, Jeganathan N. Sepsis-related mortality rates and trends based on site of infection. Crit Care Explor. 2022;4(10): e0775.
U.S. Department of Health and Human Services Office of Minority Health Profile: Asian Americans 2023. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=3&lvlid=63. Accessed 27 Sept 2023.
Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and trends in diabetes among adults in the United States, 1988–2012. JAMA. 2015;314(10):1021–9.
Torre LA, Sauer AM, Chen MS Jr, Kagawa-Singer M, Jemal A, Siegel RL. Cancer statistics for Asian Americans, Native Hawaiians, and Pacific Islanders, 2016: converging incidence in males and females. CA Cancer J Clin. 2016;66(3):182–202.
Liu Y, Elliott A, Strelnick H, Aguilar-Gaxiola S, Cottler LB. Asian Americans are less willing than other racial groups to participate in health research. J Clin Transl Sci. 2019;3(2–3):90–6.
PINC AI™ Healthcare Data White Paper: Data that informs and performs, 14 Sep 2021. PINC AI™ Applied Sciences, Premier Inc. https://offers.premierinc.com/rs/381-NBB-525/images/Premier-Healthcare-Database-Whitepaper-Final.pdf.
Rhee C, Dantes R, Epstein L, et al. Incidence and trends of sepsis in US hospitals using clinical vs claims data, 2009–2014. JAMA. 2017;318(13):1241–9.
Quan H, Li B, Couris CM, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173(6):676–82.
Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–9.
Hainmueller J. Entropy balancing for causal effects: a multivariate reweighting method to produce balanced samples in observational studies. Polit Anal. 2012;20(1):25–46.
Harvey RA, Hayden JD, Kamble PS, Bouchard JR, Huang JC. A comparison of entropy balance and probability weighting methods to generalize observational cohorts to a population: a simulation and empirical example. Pharmacoepidemiol Drug Saf. 2017;26(4):368–77.
Matschinger H, Heider D, Konig HH. A comparison of matching and weighting methods for causal inference based on routine health insurance data, or: what to do if an RCT is impossible. Gesundheitswesen. 2020;82(S02):S139–50.
Parish WJ, Keyes V, Beadles C, Kandilov A. Using entropy balancing to strengthen an observational cohort study design: lessons learned from an evaluation of a complex multi-state federal demonstration. Health Serv Outcomes Res Methodol. 2018;18(1):17–46.
Stuart EA, Lee BK, Leacy FP. Prognostic score-based balance measures can be a useful diagnostic for propensity score methods in comparative effectiveness research. J Clin Epidemiol. 2013;66(8 Suppl):S84-S901e1.
Kaiser Family Foundation. Can immigrants enroll in Medicare? https://www.kff.org/faqs/medicare-open-enrollment-faqs/can-immigrants-enroll-in-medicare/. Accessed 27 Sept 2023.
Ma KPK, Bacong AM, Kwon SC, Yi SS, Ethoan LN. The impact of structural inequities on older Asian Americans during COVID-19. Front Public Health. 2021;9: 690014.
Hernandez-Pastor L, Geurtsen J, Baugh B, et al. Economic burden of invasive Escherichia coli disease among older adult patients treated in hospitals in the United States. J Manag Care Spec Pharm. 2023;29(8):873–83.
Isenberg SR, Bonares M, Kurahashi AM, Algu K, Mahtani R. Race and birth country are associated with discharge location from hospital: a retrospective cohort study of demographic differences for patients receiving inpatient palliative care. EClinicalMedicine. 2022;45: 101303.
Sharma RK, Khosla N, Tulsky JA, Carrese JA. Traditional expectations versus US realities: first- and second-generation Asian Indian perspectives on end-of-life care. J Gen Intern Med. 2012;27(3):311–7.
Ko M, Newcomer RJ, Bindman AB, Kang T, Hulett D, Spetz J. Changing home care aides: differences between family and non-family care in California Medicaid home and community-based services. Home Health Care Serv Q. 2020;39(1):1–16.
Begier E, Rosenthal NA, Gurtman A, Kartashov A, Donald RGK, Lockhart SP. Epidemiology of invasive Escherichia coli infection and antibiotic resistance status among patients treated in US hospitals: 2009–2016. Clin Infect Dis. 2021;73(4):565–74.
Jacobs ZG, Prasad PA, Fang MC, Abe-Jones Y, Kangelaris KN. The association between limited English proficiency and sepsis mortality. J Hosp Med. 2020;15(3):140–6.
Pokharel P, Dhakal S, Dozois CM. The diversity of Escherichia coli pathotypes and vaccination strategies against this versatile bacterial pathogen. Microorganisms. 2023. https://doi.org/10.3390/microorganisms11020344.
US National Library of Medicine. Clinical Trials.gov. A study of vaccination with 9-valent extraintestinal pathogenic Escherichia coli Vaccine (ExPEC9V) in the prevention of invasive extraintestinal pathogenic Escherichia coli disease in adults aged 60 years and older with a history of urinary tract infection in the past 2 years. https://classic.clinicaltrials.gov/ct2/show/NCT04899336. Accessed 27 Sept 2023.
UC Davis Health launches new Invasive E. coli disease vaccine trial 2023. https://health.ucdavis.edu/news/headlines/uc-davis-health-launches-new-invasive-e-coli-disease-vaccine-trial/2023/05. Accessed 27 Sept 2023.
Acknowledgements
The authors would like to thank Shanshan Dong and Lu Wang of Johnson & Johnson (China) Investment Ltd for their contributions to the study.
Medical Writing/Editorial Assistance.
Medical writing assistance was provided by a professional medical writer, Christopher Crotty, PhD, who was an employee of Analysis Group, Inc., a consulting company that provided paid consulting services to Janssen Global LLC, the sponsor which funded the development and conduct of this study and manuscript.
Funding
This study was funded by Janssen Global LLC. The study sponsor was involved in several aspects of the research, including the study design, interpretation of data, writing of the manuscript, decision to submit the manuscript for publication, and the journal’s Rapid Service Fee.
Author information
Authors and Affiliations
Contributions
Chao Zhuo and Bo Zheng equally contributed as primary co-authors on this manuscript. Chao Zhuo, Bo Zheng, Kitima Wattanakamolkul, Yoshikazu Nakayama, Martin Cloutier, Marjolaine Gauthier-Loiselle, Jun Feng, David Wu, Maureen P. Neary, Jeroen Geursten, Antoine C. El Khoury, and Yoshiaki Gu have made substantial contributions to the conception or design of the study, or the acquisition, analysis, or interpretation of data, drafting the manuscript and revising it critically for important intellectual content, and have provided final approval of this version to be published and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of Interest
Bo Zheng, Yoshiaki Gu, and Chao Zhuo have no conflicts of interest. Yoshikazu Nakayama and Kittima Wattanakamolkul are employees of Janssen Pharmaceutical K.K. Jun Feng and David Wu are employees of Johnson & Johnson International (Singapore) PTE. Ltd. Jeroen Geurtsen is an employee of Janssen Vaccines & Prevention BV and owns stock. Maureen P. Neary and Antoine C. El Khoury are employees of Janssen Global Services, LLC and own stock. Martin Cloutier and Marjolaine Gauthier-Loiselle are employees of Analysis Group, Inc., a consulting company that has provided paid consulting services to Janssen Global LLC, which funded the development and conduct of this study and manuscript.
Ethical Approval
This study complies with the ethical standards of the Helsinki Declaration. Data were de-identified and comply with the patient requirements of the Health Insurance Portability and Accountability Act (HIPAA) of 1996; therefore, no review by an institutional review board was required per Title 45 of CFR, Part 46.101(b)(4) (https://www.hhs.gov/ohrp/regulations-and-policy/regulations/45-cfr-46/#46.101).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Zhuo, C., Zheng, B., Wattanakamolkul, K. et al. Impact of Invasive Escherichia Coli Disease on Clinical Outcomes and Medical Resource Utilization Among Asian Patients in the United States. Infect Dis Ther 13, 313–328 (2024). https://doi.org/10.1007/s40121-023-00911-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-023-00911-0