Abstract
Introduction
A favorable benefit-risk balance is required to support licensure of biologics, in keeping with regulatory agencies’ evolving recommendations, including the United States Food and Drugs Administration. We present a structured semi-quantitative benefit-risk analysis of MenACYW-TT, a quadrivalent meningococcal conjugate vaccine against Neisseria meningitidis serogroups, A, C, W and Y versus licensed comparators in individuals aged ≥ 12 months.
Methods
We used data from six MenACYW-TT clinical trials, stratified by age group, versus licensed vaccines: toddlers (12–23 months; Nimenrix® [MCV4-TT]), children (2–9 years; Menveo® [MCV4-CRM]), adolescents (10–17 years; MCV4-CRM or Menactra® [MCV4-DT]), adults (18–55 years; MCV4-DT) and older adults (≥ 56 years; Menomune®–A/C/Y/W-135 [MPSV4]). Eight benefit (seroresponse and seroprotection for A, C, W and Y) and five risk outcomes (any and grade 3 solicited injection site and systemic reactions, and serious adverse events) were measured at Day 30 after initial vaccination. Analyses were conducted by baseline vaccination status (meningococcal vaccine-naïve or vaccine-primed).
Results
MenACYW-TT showed favorable seroresponse and seroprotection among vaccine-naïve participants aged ≥ 2 years, against all serogroups, compared with MCV4-CRM, MCV4-DT and MPSV4. In vaccine-naïve toddlers, there was a favorable effect for serogroup C, but no difference between MenACYW-TT and MCV4-TT for serogroups A, Y and W. A favorable effect for MenACYW-TT against serogroup C was observed in all vaccine-naïve and combined vaccine-naïve and MenC conjugate vaccine-primed groups. For all risk criteria, there were no differences between MenACYW-TT and MCV4s in toddlers, children, adolescents and adults. Results for solicited injection site and systemic reactions favored MPSV4 in older adults.
Conclusions
The benefit-risk profile for MenACYW-TT showed favorable seroresponse and seroprotection in individuals aged ≥ 2 years and no difference in risk criteria between MenACYW-TT and MCV4s. MenACYW-TT may provide an alternative to the standard-of-care for meningococcal disease prevention in those aged ≥ 12 months.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
There is a need to understand the balance between the benefits and risks of meningococcal vaccination to support informed and adequate public health decision making. |
We conducted a structured benefit-risk analysis for the meningococcal vaccine MenACYW-TT, using results from six pre-licensure clinical trials of MenACYW-TT versus licensed meningococcal vaccines in individuals aged 12 months and older. |
Structured benefit risk assessment constitutes a useful tool to support regulatory decisions during the evaluation for licensure of new vaccines, in agreement with the evolving recommendations of some regulatory agencies. |
What was learned from the study? |
The benefit-risk profile of MenACYW-TT vaccine showed a favorable immune response compared with licensed comparator vaccines used in children (MCV4-CRM), adolescents (MCV4-CRM and MCV4-DT), adults (MCV4-DT) and older adults (≥ 65 years; MPSV4) across all serogroups, with a comparable risk of adverse events compared with MCV4s. |
Based on the favorable benefit-risk profile across each age group, MenACYW-TT may provide an alternative to standard-of-care vaccines in individuals 12 months and older, contributing to the prevention and control of invasive meningococcal disease. |
This structured benefit-risk analysis is in line with the US FDA recommendations on benefit-risk assessment for new drug and biological products. |
Introduction
Invasive meningococcal disease (IMD) is an acute life-threatening infection caused by the gram-negative bacterium Neisseria meningitidis [1]. Meningitis is the most common presentation of IMD, with meningococcal septicemia occurring in 5–20% of IMD cases [2]. IMD often progresses rapidly, with a case fatality rate of 10–15% even with suitable antibiotic therapy, and can be higher in those who develop septicemia [2]. Up to 20% of patients have permanent sequelae such as hearing loss, neurological damage, or loss of a limb [2]. Globally, there are approximately half a million cases of IMD annually [1], with an incidence rate that varies across geographical regions, ranging from 0.1 cases per 100,000 in the USA to 0.6 per 100,000 cases in Europe [3]. Incidence rates are highest in children < 1 year old, followed by a second peak among adolescents and young adults [3].
Worldwide, the serogroups responsible for the most cases of IMD are A, B, C, W, X and Y [1]. In Europe, the most prevalent serogroups are B and C; however, in recent years, an increase of IMD infections caused by serogroup W has been reported [4]. Similarly, serogroup Y is becoming increasingly prevalent in the USA and, more recently, the UK [1, 5]. However, meningococcal vaccines have helped reduce the incidence of IMD in countries with vaccination programs. Dynamic changes in the disease-causing serogroups highlight the need for meningococcal vaccines that provide protection against a range of serogroups and across the entire population.
Four meningococcal conjugate quadrivalent vaccines (MCV4s) are licensed and cover serogroups A, C, W and Y. Menveo® (MCV4-CRM; GlaxoSmithKline, Italy) is recommended for individuals ≥ 2 months to 55 years of age in the USA and ≥ 2 years in the European Union (EU) [6]. Menactra® (MCV4-DT; Sanofi Pasteur, USA) is recommended for individuals ≥ 9 months in the USA but is not licensed in the EU [7]. Nimenrix® (MCV4-TT; Pfizer, Belgium) is recommended for individuals ≥ 6 weeks of age in the EU but is not licensed in the USA [8]. MenQuadfi® (MenACYW-TT; Sanofi, USA) is a new MCV4 with a tetanus toxoid carrier and is currently approved with an age indication ≥ 12 months in the EU and > 40 other countries so far and ≥ 2 years in the USA. The meningococcal quadrivalent polysaccharide vaccine, MSPV4 (Menomune®–A/C/Y/W-135, Sanofi, USA), was used in the USA [9], and globally, for immunization against IMD caused by serogroups A, C, W and Y in individuals aged ≥ 2 years [9], including older adults aged ≥ 56 years, until its discontinuation worldwide in 2017 [9, 10]. Following its discontinuation, and until the licensure of MenACYW-TT, there was no meningococcal vaccine licensed for use in those aged ≥ 56 years in the USA. Individuals ≥ 56 years were advised to receive a MCV4 instead, despite the lack of an approved product for this age group [9]. The safety and immunogenicity of MenACYW-TT have been evaluated in a series of randomized active-controlled clinical trials in participants aged 12 months to ≥ 56 years [11,12,13,14,15,16,17,18,19,20].
The EMA and FDA developed and recommended several tools, processes and frameworks for the structured evaluation of benefit-risk for drugs and biological products [21, 22]. The Center for Biologics Evaluation and Research (CBER), within the US Food and Drug Administration (FDA), requires an evaluation of scientific and clinical data submitted by manufacturers for new biologics or new indications for approved products to determine whether the product meets CBER’s standards for approval based on a favorable benefit-risk balance for the population [23]. Understanding the balance between the benefits and risks of vaccination is essential to support informed and adequate public health decision making [24]. This needs to be done in a structured way to provide an objective assessment of the benefit-risk profile of a vaccine, ensuring greater transparency for decision-making purposes. Several structured benefit-risk framework and visual representations have been proposed and recommended [25, 26].
In this study, we aimed to present a structured, semi-quantitative benefit-risk assessment for MenACYW-TT using data from six pivotal pre-licensure studies (Table 1) of MenACYW-TT versus licensed active comparator vaccines in individuals aged 12 months or older.
Methods
Frameworks have been developed to evaluate the benefit-risk balance of medicinal products in a structured way for decision making purposes and regulatory approval [21, 22, 25, 26]. In this assessment, both a structured qualitative and a semi-quantitative framework were used following stepwise instructions for the benefit-risk evaluation based on BRAT (Benefit-Risk Action Team), which standardizes and supports the decision and communication of a benefit-risk assessment [22].
This approach facilitates the identification of critical issues regarding benefit-risk and improves transparency of the assumptions used by the marketing authorization holder to evaluate the benefit-risk profile. The following steps of the benefit-risk framework were applied:
-
Definition of decision context;
-
Identification and selection of key favorable and key unfavorable outcomes (creation of the value tree) and documentation of the rationale for including/excluding important outcomes;
-
Identification of data sources and analysis: determine and document all data sources, extract relevant data for the assessment and analyze the data;
-
Presentation and interpretation of results based on the combination of a value tree, a benefit-risk framework table [21] and forest plots.
Decision Context
The decision context includes the definition of several items including: the objective of the benefit-risk assessment, the drug, dose, formulation, indication, patient population, comparator(s), time horizon for outcomes and perspective for decision makers (regulator, sponsor, patient or physician) (Table 2).
Patient Population
This semi-quantitative framework analysis was performed using data from six pivotal clinical trials of MenACYW-TT conducted in meningococcal vaccine-naïve (participants without prior history of meningococcal vaccination) or vaccine-primed (individuals who had a background of prior vaccination with any meningococcal vaccine) individuals aged ≥ 12 months (Table 1) [11,12,13,14,15, 20]. The populations evaluated included toddlers aged 12–23 months, children aged 2–9 years, adolescents aged 10–17 years, adults aged 18–55 years and older adults ≥ 56 years.
Comparators
The analysis was conducted to demonstrate immunogenicity by assessing the non-inferiority of immune responses induced by MenACYW-TT compared to those induced by licensed meningococcal quadrivalent standard-of-care vaccines. Comparator vaccines in this analysis were the meningococcal quadrivalent conjugated vaccines MCV4-TT (in toddlers 12–23 months), MCV4-CRM (in children 2–9 years and adolescents 10–17 years) and MCV4-DT (in adolescents 10–17 years and adults 18–55 years) as well as the meningococcal quadrivalent polysaccharide vaccine MPSV4 (in older adults ≥ 56 years).
Selection of Key Favorable and Unfavorable Outcomes
Favorable effects are defined as any beneficial effects associated with the product (often referred to as ‘benefits’ or ‘clinical benefits’) for the target population. Unfavorable effects are defined as any detrimental effects (often referred to as risks, harms and hazards both known and unknown) that can be attributed to the product or that are otherwise of concern for their undesirable effect on patients’ health, public health or the environment [22].
Favorable Effects
Eight immunogenicity benefit outcome measures, based on human serum bactericidal antibodies assay (hSBA) titer, were integrated: rates of vaccine seroresponse (a post-vaccination hSBA titer ≥ 1:16 in those with pre-vaccination titers < 1:8 or a ≥ fourfold increase in titers in those with pre-vaccination titers ≥ 1:8) and rates of vaccine seroprotection (hSBA titers ≥ 1:8) at Day 30 after vaccination for each serogroup A, C, W and Y. Antibodies against each of the four serogroups were measured with serum bactericidal antibody assay using human complement at baseline and Day 30 post-vaccination in each study. While hSBA titers ≥ 1:4 are defined as a surrogate of short-term protection, hSBA titers ≥ 1:8 represent a more conservative serological correlate of individual protection against meningococcal disease, widely used and accepted by regulatory agencies [27,28,29,30,31]. Thus, hSBA titers ≥ 1:8 were used as threshold for seroprotection in the six studies.
Unfavorable Effects
Five safety risk outcome measures were integrated: the rates of any solicited injection site reaction, any solicited systemic reaction, any Grade 3 solicited injection site reaction and any Grade 3 solicited systemic reactions for 7 days post-vaccination, and the rate of any serious adverse events (SAEs) for 6 months post-vaccination. Safety data were collected up to 6 months post-vaccination, except the study in toddlers (MET51), where safety data were collected for 30 days post-vaccination. Safety data were collected based on the Medical Dictionary for Regulatory Activities (MedDRA) coding and predefined queries. It is important to note that the MedDRA coding version was updated during the MenACYW-TT clinical development program; the same version of MedDRA was not used to code all adverse events in all studies. As such, re-coding was carried out according to MedDRA version 21.0.
The solicited injection site reactions for participants 12–23 months of age included injection tenderness, erythema and swelling (Table S1), and for participants ≥ 2 years, injection site pain, erythema and swelling (Table S2 and S3). The solicited systemic reactions for participants 12–23 months of age included fever, vomiting, abnormal crying, drowsiness, appetite loss and irritability (Table S4), and for participants ≥ 2 years, fever, headache, malaise and myalgia (Table S5).
Important potential risks for MenACYW-TT during the clinical development program included anaphylaxis (based on risks for any vaccine), Guillain-Barré Syndrome (GBS) and Bell’s palsy (risks identified from post-marketing experience of other meningococcal vaccines) [6, 10, 32]. Post-marketing data for meningococcal vaccines have shown these events to occur at very low frequencies. There were no events of anaphylaxis or Bell’s palsy attributed to MenACYW-TT and no events of GBS reported during pivotal MenACYW-TT clinical trials [11,12,13,14,15].
Data Sources and Analysis
The key data sources were six pivotal clinical trials of MenACYW-TT [11,12,13,14,15] (Table 1). Included studies were conducted between 2015 and 2017 in toddlers at sites across Europe (Spain, Germany, Hungary and Finland) and in children, adolescents, adults and older adults at sites across the US and Puerto Rico. All clinical studies evaluating MenACYW-TT were conducted in accordance with the Declaration of Helsinki and the Quality Standards of the International Conference on Harmonization Good Clinical Practices. For the individual clinical trials, statistical software SAS® version 9.4 or later was used. All trials included in the benefit-risk assessment measured immunogenicity (seroresponse and seroprotection) on Day 30 after initial vaccination and had similar procedures for collection of safety data, and similar primary endpoints, allowing an integrated and pooled analysis.
This analysis is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Display Results
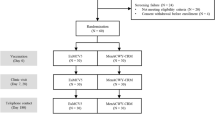
The criteria selected for this benefit-risk assessment were outlined in the value tree (Fig. 1), with the key dimensions of the evaluation and related evidence and uncertainties described for the six pivotal trials within the FDA framework table (Table 3) [33,34,35]. Forest plots are shown as key outputs of the structured benefit-risk assessment.
For each age group (toddlers 12–23 months, children 2–9 years, adolescents 10–17 years, adults 18–55 years and older adults ≥ 56 years), differences in rates of effects were calculated for benefits as (benefit rate for MenACYW-TT) − (benefit rate for comparator) and for risk as (risk rate for comparator) − (risk rate for MenACYW-TT), with 95% confidence intervals (CI) calculated using the Wilson score method without continuity correction. Separate analyses were conducted by baseline meningococcal vaccination status: those who were meningococcal vaccine-naïve and those who were meningococcal vaccine-primed (with MCV4 [adolescents and adults]). Meningococcal vaccine-naïve was defined as participants without a prior history of meningococcal vaccination. Meningococcal-primed individuals were defined as those who had received prior vaccination with any meningococcal vaccine. Toddlers were either meningococcal vaccine-naïve or MenC conjugate (MCC) vaccine-primed (≥ 1 dose of MCC prior to 12 months of age). In toddlers who had received a MenC vaccination during their first year of life, the numbers who had received previous vaccination with either MenC-TT (NeisVac-C™; Pfizer Ltd, Kent, UK) or MenC-CRM (Menjugate®; GlaxoSmithKline Vaccines Srl, Siena, Italy) were relatively small; therefore, the benefit-risk plots for this age group are presented for the combined population of meningococcal vaccine-naïve and MCC-primed and for the meningococcal vaccine-naïve toddlers.
Graphical representation of the data was done using forest plots. Each forest plot represents the summary of benefit-risk for a single dose of MenACYW-TT in each age group. The plots are divided into two portions, with the top (in blue) presenting the evidence supporting the efficacy of MenACYW-TT and the bottom (in red) presenting the evidence evaluating the safety. The plots are configured so that all point estimates to the left of the middle line for both efficacy and safety are favorable to MenACYW-TT. The point estimates to the right of the middle line favor the comparator. There is a favorable effect for MenACYW-TT when the lower limit of the 95% CI is to the left of the middle line. Point estimates are comparable when there is no difference between MenACYW-TT and the comparator vaccine if the 95% CIs crosses the middle line.
Results
Meningococcal Vaccine-Naïve Participants
Toddlers (12–23 Months)
Regarding the benefits criteria (Fig. 2; blue points), the comparison of MenACYW-TT with MCV4-TT showed no difference between vaccines for serogroups A, Y and W, while there was a favorable effect for MenACYW-TT for serogroup C in terms of seroresponse and seroprotection. Regarding the risks criteria (Fig. 2; red points), there was no difference between MenACYW-TT and MCV4-TT.
Rate difference for benefits and risks for MenACYW-TT compared to MCV4-TT in meningococcal vaccine-naïve toddlers (MET51 study). Blue point estimate: (benefit rate for MenACYW-TT) − (benefit rate for comparator). Red point estimate: (risk rate for comparator) − (risk rate for MenACYW-TT). CI confidence interval, MenACYW-TT MenQuadfi®, MCV4-TT Nimenrix®
Children (2–9 Years)
Regarding the benefits criteria (Fig. 3; blue points), the comparison of MenACYW-TT with MCV4-CRM showed favorable effects for MenACYW-TT for all serogroups, with a higher effect for serogroup C in terms of seroresponse and seroprotection. Regarding the risks criteria (Fig. 3; red points), there was a favorable effect for MenACYW-TT for the solicited injection site reactions (all and grade 3) while there was no difference between the vaccines for the other risks criteria.
Rate difference for benefits and risks for MenACYW-TT compared to MCV4-CRM in meningococcal vaccine-naïve children (MET35 study). Blue point estimate: (benefit rate for MenACYW-TT) − (benefit rate for comparator). Red point estimate: (risk rate for comparator) − (risk rate for MenACYW-TT). CI confidence interval, MenACYW-TT MenQuadfi®, MCV4-CRM Menveo®
Adolescents (10–17 Years)
Regarding the benefits criteria, the comparison of MenACYW-TT with MCV4-DT (Fig. 4; blue points) and MCV4-CRM (Fig. 5; blue points) showed a favorable effect for MenACYW-TT for all four serogroups, with a higher effect for serogroup C, in terms of both seroresponse and seroprotection. Regarding the risks criteria (Figs. 4, 5; red points), the comparison with MCV4-DT showed a favorable effect for MenACYW-TT for solicited injection site and systemic reactions of any intensity (Fig. 4), while there was no difference between MenACYW-TT and MCV4-CRM for solicited reactions. There was no difference for SAEs between MenACYW-TT and either MCV4-DT or MCV4-CRM.
Rate difference for benefits and risks for MenACYW-TT compared to MCV4-DT in Meningococcal vaccine-naïve adolescents (MET43 study). Blue point estimate: (benefit rate for MenACYW-TT) − (benefit rate for comparator). Red point estimate: (risk rate for comparator) − (risk rate for MenACYW-TT). CI confidence interval, MenACYW-TT MenQuadfi®, MCV4-DT Menactra®
Rate difference for benefits and risks for MenACYW-TT compared to MCV4-CRM in Meningococcal vaccine-naïve adolescents (MET50 study). Blue point estimate: (benefit rate for MenACYW-TT) − (benefit rate for comparator). Red point estimate: (risk rate for comparator) − (risk rate for MenACYW-TT). CI confidence interval, MenACYW-TT MenQuadfi®, MCV4-CRM Menveo®
Adults (18–55 Years)
Regarding the benefits criteria (Fig. 6; blue points), the comparison of MenACYW-TT with MCV4-DT showed favorable effects for MenACYW-TT for all four serogroups in terms of seroresponse and seroprotection, with a larger effect for the seroresponse to serogroup C. Regarding the risks criteria (Fig. 6; red points), there was a favorable effect for MCV4-DT for solicited injection site reactions of any intensity, while there was no difference between the vaccines for the other risks, including injection site reactions of Grade 3 intensity.
Rate difference for benefits and risks for MenACYW-TT compared to MCV4-DT in meningococcal vaccine-naïve adults (MET43 study). Blue point estimate: (benefit rate for MenACYW-TT) − (benefit rate for comparator). Red point estimate: (risk rate for comparator) − (risk rate for MenACYW-TT). CI confidence interval, MenACYW-TT MenQuadfi®, MCV4-DT Menactra®
Older Adults (≥ 56 Years)
Regarding the benefits criteria (Fig. 7; blue points), the comparison of MenACYW-TT with MPSV4 showed favorable effects for MenACYW-TT for all four serogroups, with larger effects for serogroups Y and C, in terms of both seroresponse and seroprotection. Regarding the risks criteria (Fig. 7; red points), there was a favorable effect for MPSV4 for solicited systemic and injection site reactions of any intensity, particularly for injection site reactions. There was no difference between the vaccines for the other risks, including solicited reactions of grade 3 intensity.
Rate difference for benefits and risks for MenACYW-TT compared to MPSV4 in meningococcal vaccine-naïve older adults (MET49 study). Blue point estimate: (benefit rate for MenACYW-TT) − (benefit rate for comparator). Red point estimate: (risk rate for comparator) − (risk rate for MenACYW-TT). CI confidence interval, MenACYW-TT MenQuadfi®, MPSV4 Menomune®
Vaccine-Naïve and MCC-Primed Toddlers (12–23 Months)
Regarding the benefit criteria (Fig. 8; blue points), the comparison of MenACYW-TT with MCV4-TT for the combined population of meningococcal vaccine-naïve or MCC-primed individuals showed favorable effects for MenACYW-TT for serogroup C, in terms of seroresponse and seroprotection, and no difference between vaccines for serogroups A and W. For serogroup Y, the comparison showed a favorable effect for MenACYW-TT in terms of seroresponse and no difference in terms of seroprotection. Regarding the risk criteria (Fig. 8; red points), there was no difference between MenACYW-TT and MCV4-TT.
Rate difference for benefits and risk for MenACYW-TT compared to MCV4-TT in meningococcal vaccine-naïve and vaccine-primed toddlers (MET51 study). Blue point estimate: (benefit rate for MenACYW-TT) − (benefit rate for comparator). Red point estimate: (risk rate for comparator) − (risk rate for MenACYW-TT). CI confidence interval, MenACYW-TT MenQuadfi®, MCV4-TT Nimenrix®
MCV4-Primed Participants
Analysis for MCV4 primed participants was performed in adolescents and adults ≥ 15 years of age. Regarding the benefit criteria (Fig. 9; blue points), the comparison of MenACYW-TT with MCV4-DT showed a favorable effect for MenACYW-TT for serogroups A, C and W in terms of seroresponse, and no difference between vaccines for serogroup Y, in terms of seroresponse and for all four serogroups in terms of seroprotection.
Rate difference for benefits and risks for MenACYW-TT compared to MCV4-DT in meningococcal vaccine-primed adults and adolescents (MET56 study). Blue point estimate: (benefit rate for MenACYW-TT) − (benefit rate for comparator). Red point estimate: (risk rate for comparator) − (risk rate for MenACYW-TT). CI confidence interval, MenACYW-TT MenQuadfi®, MCV4-DT Menactra®
Regarding the risk criteria (Fig. 9; red points), there was no difference between MenACYW-TT and MCV4-DT.
Discussion
This structured, semi-quantitative benefit-risk assessment of MenACYW-TT was based on data from six pivotal, randomized, active-controlled clinical trials using licensed active comparators (MCV4-CRM, MCV4-DT, MCV4-TT and MPSV4) in participants aged 12 months or older. This study illustrates the steps and methodology used for the benefit-risk assessment of a medicinal product and in this specific case, a vaccine. Although structured benefit-risk methodologies and frameworks have been widely discussed and presented in the regulatory landscape [21, 26], there are limited published examples.
The immunogenicity and safety findings from each of these pivotal clinical trials have been previously published [11,12,13,14,15,16]. These studies individually demonstrated immune non-inferiority of MenACYW conjugate vaccine for all four serogroups across all age groups and versus all comparators, using hSBA vaccine seroresponse for individuals aged ≥ 2 years or hSBA seroprotection rates in toddlers (12–24 months old).
In toddlers 12–23 months of age, the benefit-risk profile of MenACYW-TT was generally comparable relative to the comparator MCV4-TT, with no difference for all risk criteria. A favorable effect for MenACYW-TT was found for serogroup C in vaccine-naïve participants and in the combined population of either meningococcal vaccine-naïve or MCC-primed participants. Similar immunogenic outcomes were found for serogroup C in vaccine-naïve toddlers when administered with MenACYW-TT or MCV4-TT and NeisVac-C® as a single dose [39].
In individuals ≥ 2 years, regardless of priming status, the benefit-risk profile of MenACYW-TT is favorable relative to the licensed comparator vaccines used in children (MCV4-CRM), adolescents (MCV4-CRM and MCV4-DT), adults (MCV4-DT) and older adults (MSPV4). MenACYW-TT was well tolerated when given as a single dose across all age groups, had no vaccine-related SAEs and had a similar safety profile to that of the standard-of-care MCV4 vaccines. The most common reactions were non-serious, self-limiting and similar in type and frequency to those observed with the comparator meningococcal vaccines [6, 8,9,10, 32]. Important potential risks were the same as those identified with standard-of-care MCV4 vaccines or other vaccines given in the same age group [6,7,8]. In older adults, the rate of solicited reactions, particularly injection site reactions, favored the comparator MPSV4; however, there was no difference in reactions of Grade 3 intensity between both vaccines. This increased frequency of solicited reactions can likely be attributed to the formulation of the vaccines, with MenACYW-TT being conjugated to tetanus toxoid and with no protein carrier with MPSV4. These risks can be managed through routine pharmacovigilance and risk minimization measures.
While our findings are based on the results of pivotal studies that support the initial licensure of MenACYW-TT, more recent studies confirm these findings for immunogenicity and safety of a MenACYW-TT booster dose in children [17], adolescents and young adults [36] and older adults [37] primed with MenACYW-TT or another MCV4 vaccine.
As well as the favorable immunogenicity and safety findings, MenACYW-TT is available in a ready-to-use liquid formulation allowing healthcare providers to avoid vaccine reconstitution as compared to non-fully liquid MCV4-TT and MCV4-CRM [6,7,8, 38]. Therefore, reducing steps in the vaccine preparation subsequently reduces the preparation time and decreases the opportunities for immunization errors and thus might impact safety.
Limitations
While this analysis used data from six clinical trials across a range of age groups and comparators, there are still limitations. Each type of MCV4 was not used as a comparator vaccine to MenACYW-TT across all the age groups. MCV4-TT was not used as a comparator in studies conducted in the US since it is not licensed there for any age group. Similarly, MCV4-DT was not used as a comparator in any study conducted in Europe since it is not licensed for use in that region. The hSBA ≥ 1:8 threshold, referred to as seroprotection, is widely used as serological surrogate of protection and is accepted globally by health regulatory agencies, but the absolute clinical benefit of protective titers is yet to be determined [27,28,29,30, 40]. Using a hSBA threshold of at least 1:8 is a conservative estimate of protection, and therefore this structured benefit-risk assessment may underestimate the true benefit-risk ratio for MenACYW-TT. Five of the included studies were double-blind studies, while MET50 (in adolescents; vs. MCV4-CRM) had an open-label study design, which is potentially open for bias; however, the laboratory technicians who performed the hSBA were blinded to vaccine allocation to reduce bias. Additionally, the clinical relevance of the unfavorable effect of MenACYW-TT for serogroup A in the MCC-primed toddlers is unknown and should be interpreted with caution as it was restricted only to a very small number of toddlers primed with a MenC-CRM vaccine.
There were also potential limitations to the benefit-risk assessment approach used that must be considered. In terms of the methodology used, we chose a descriptive structured benefit-risk assessment following the key steps of a Benefit-risk Action Team (BRAT) framework and US FDA recommendations [41, 42]. This framework provides qualitative stepwise instructions for the benefit-risk evaluation. While it allows for structured benefit-risk evaluation, it does not offer the possibility to account for the importance of each benefit and risk by weighting the key criteria. This is inherent to this framework. In contrast, fully quantitative frameworks, such as Multi-Criteria Decision Analysis (MCDA) [43], provide explicit methods for weighting criteria and balancing the benefits and the risks. MCDA is however used for more complex decisions with higher uncertainty which was not the case in our assessment. The second limitation is related to patient perspective. The regulatory perspective was taken for this structured benefit-risk assessment. Key benefits and risks considered for this assessment were based on clinical outcomes from trials and did not include patient outcomes. Integrating patient perspectives is recently becoming an important part of the regulatory decision-making process, and pharmaceutical industries actively engage patients to collect their perspectives throughout the development and life cycle of medical products [44]. Patients not only contribute to the evaluation of benefit-risk during regulatory approval but also during the development phase, helping to identify unmet medical needs and to better understand the acceptability of benefits and risks [21, 45].
Conclusion
The structured benefit-risk approach facilitates the identification of critical issues regarding benefit-risk and improves the transparency of the assumptions used by the marketing authorization holder to evaluate the benefit-risk profile of a drug or a biological product.
The MenACYW-TT vaccine has shown consistent and robust immunogenicity across all four serogroups in individuals from 12 months of age and older, demonstrating strong evidence towards benefit for the vaccine vs. comparators, alongside comparable risk of solicited adverse events and SAEs. Based on the overall favorable benefit-risk profile across age groups ranging from toddlers 12 months old through older adults ≥ 56 years of age, combined with the convenience of a ready-to-use liquid formulation, MenACYW-TT vaccine is expected contribute in the prevention and control of IMD associated with vaccine serogroups A, C, W and Y because of the demonstrated immunogenicity across a broad age range, while also generating higher immune responses without additional safety concerns. Ongoing Phase 3 trials are investigating the use of MenACYW-TT in infants as young as 6 weeks of age to better address the global need for meningococcal disease prevention throughout life.
Data Availability
Qualified researchers may request access to patient-level data and related documents [including, e.g., the clinical study report, study protocol with any amendments, blank case report form, statistical analysis plan, and dataset specifications]. Patient-level data will be anonymized, and study documents will be redacted to protect the privacy of trial participants. Further details on Sanofi’s data sharing criteria, eligible studies, and process for requesting access can be found at https://vivli.org/.
References
Nadel S, Ninis N. Invasive meningococcal disease in the vaccine era. Front Pediatr. 2018;6:321.
Mbaeyi S, Duffy J, McNamara LA. Meningococcal disease. Centres for Disease Control and Prevention (CDC); 2021.
Centers for Disease Control and Prevention. Surveillance. Antibiotic-resistant Neisseria meningitidis serogroup Y2019.
Krone M, Gray S, Abad R, Skoczynska A, Stefanelli P, van der Ende A, et al. Increase of invasive meningococcal serogroup W disease in Europe, 2013 to 2017. Euro Surveill. 2019;24(14):1800245.
Public Health England. Invasive meningococcal disease in England: annual laboratory confirmed reports for epidemiological year 2016/2017. Health Protection Report (2017). 2018.
Menveo®. Summary of product characteristics. 2020.
European Centre for Disease Prevention and Control (ECDC). Factsheet about meningococcal disease. European Centre for Disease Prevention and Control (ECDC); 2019.
Nimenrix®. Summary of product characteristics. 2021.
(CDC) CfDCaP. Clinical update. 2017.
U.S Food and Drug Administration. Menomune-A/C/Y/W-135-prescribing information. 2019.
van der Vliet D, Vesikari T, Sandner B, Martinón-Torres F, Muzsay G, Forsten A, et al. Immunogenicity and safety of a quadrivalent meningococcal tetanus toxoid-conjugate vaccine (MenACYW-TT) vs. a licensed quadrivalent meningococcal tetanus toxoid-conjugate vaccine in meningococcal vaccine-naïve and meningococcal C conjugate vaccine-primed toddlers: a phase III randomised study. Epidemiol Infect. 2021;149:e50.
Baccarini CI, Simon MW, Brandon D, Christensen S, Jordanov E, Dhingra MS. Safety and immunogenicity of a quadrivalent meningococcal conjugate vaccine in healthy meningococcal-Naïve children 2–9 years of age: a phase III, randomized study. Pediatr Infect Dis J. 2020;39:955–60.
Chang LJ, Hedrick J, Christensen S, Pan J, Jordanov E, Dhingra MS. A Phase II, randomized, immunogenicity and safety study of a quadrivalent meningococcal conjugate vaccine, MenACYW-TT, in healthy adolescents in the United States. Vaccine. 2020;38:3560–9.
Áñez G, Hedrick J, Simon MW, Christensen S, Jeanfreau R, Yau E, et al. Immunogenicity and safety of a booster dose of a quadrivalent meningococcal tetanus toxoid-conjugate vaccine (MenACYW-TT) in adolescents and adults: a Phase III randomized study. Hum Vaccin Immunother. 2020;16:1292–8.
Esteves-Jaramillo A, Koehler T, Jeanfreau R, Neveu D, Jordanov E, Singh DM. Immunogenicity and safety of a quadrivalent meningococcal tetanus toxoid-conjugate vaccine (MenACYW-TT) in ≥56-year-olds: a phase III randomized study. Vaccine. 2020;38:4405–11.
Vesikari T, Borrow R, Forsten A, Findlow H, Dhingra MS, Jordanov E. Immunogenicity and safety of a quadrivalent meningococcal tetanus toxoid-conjugate vaccine (MenACYW-TT) in healthy toddlers: a PHASE II randomized study. Hum Vaccin Immunother. 2020;16:1306–12.
Piazza FM, Virta M, Paassilta M, Ukkonen B, Ahonen A, Esteves-Jaramillo A, et al. Immunogenicity and safety of an investigational quadrivalent meningococcal conjugate vaccine administered as a booster dose in children vaccinated against meningococcal disease 3 years earlier as toddlers: a phase III, open-label, multi-center study. Hum Vaccin Immunother. 2022;18(1):1–10.
Dhingra MS, Namazova-Baranova L, Arredondo-Garcia JL, Kim KH, Limkittikul K, Jantarabenjakul W, et al. Immunogenicity and safety of a quadrivalent meningococcal tetanus toxoid-conjugate vaccine administered concomitantly with other paediatric vaccines in toddlers: a phase III randomised study. Epidemiol Infect. 2021;149: e90.
Kirstein J, Pina M, Pan J, Jordanov E, Dhingra MS. Immunogenicity and safety of a quadrivalent meningococcal tetanus toxoid-conjugate vaccine (MenACYW-TT) in adults 56 years of age and older: a phase II randomized study. Hum Vaccin Immunother. 2020;16:1299–305.
Dhingra MS, Peterson J, Hedrick J, Pan J, Neveu D, Jordanov E. Immunogenicity, safety and inter-lot consistency of a meningococcal conjugate vaccine (MenACYW-TT) in adolescents and adults: a phase III randomized study. Vaccine. 2020;38:5194–201.
U.S Food and Drug Administration. Benefit-risk assessment for new drug and biological products. 2021.
European Medicines Agency (EMA). Benefit-risk methodology project-work package 2 report: applicability of current tools and processes for regulatory benefit-risk assessment. 2010.
U.S Food and Drug Administration. About CBER. 2018.
Arlegui H, Bollaerts K, Salvo F, Bauchau V, Nachbaur G, Bégaud B, et al. Benefit-risk assessment of vaccines. Part I: a systematic review to identify and describe studies about quantitative benefit-risk models applied to vaccines. Drug Saf. 2020;43:1089–104.
Mt-Isa S, Hallgreen CE, Wang N, Callréus T, Genov G, Hirsch I, et al. Balancing benefit and risk of medicines: a systematic review and classification of available methodologies. Pharmacoepidemiol Drug Saf. 2014;23:667–78.
Hughes D, Waddingham E, Mt-Isa S, Goginsky A, Chan E, Downey GF, et al. Recommendations for benefit-risk assessment methodologies and visual representations. Pharmacoepidemiol Drug Saf. 2016;25:251–62.
Andrews N, Borrow R, Miller E. Validation of serological correlate of protection for meningococcal C conjugate vaccine by using efficacy estimates from postlicensure surveillance in England. Clin Diagn Lab Immunol. 2003;10:780–6.
(WHO) WHO. Meningococcal vaccines: WHO position paper. Releve epidemiologique hebdomadaire. 2011;86:521–39.
Gill CJ, Ram S, Welsch JA, Detora L, Anemona A. Correlation between serum bactericidal activity against Neisseria meningitidis serogroups A, C, W-135 and Y measured using human versus rabbit serum as the complement source. Vaccine. 2011;30:29–34.
Findlow J, Balmer P, Borrow R. A review of complement sources used in serum bactericidal assays for evaluating immune responses to meningococcal ACWY conjugate vaccines. Hum Vaccin Immunother. 2019;15:2491–500.
World Health Organization (WHO). The immunological basis for immunization series—module 15: meningococcal disease (updated 2020). 2020.
U.S Food and Drug Administration. Menactra® highlights of prescribing information. 2018.
Maiden MC, Ibarz-Pavón AB, Urwin R, Gray SJ, Andrews NJ, Clarke SC, et al. Impact of meningococcal serogroup C conjugate vaccines on carriage and herd immunity. J Infect Dis. 2008;197:737–43.
Kristiansen PA, Jørgensen HJ, Caugant DA. Serogroup A meningococcal conjugate vaccines in Africa. Expert Rev Vaccin. 2015;14:1441–58.
Balmer P, Burman C, Serra L, York LJ. Impact of meningococcal vaccination on carriage and disease transmission: a review of the literature. Hum Vaccin Immunother. 2018;14:1118–30.
Zambrano B, Peterson J, Deseda C, Julien K, Spiegel CA, Seyler C et al. Quadrivalent meningococcal tetanus toxoid-conjugate booster vaccination in adolescents and adults: phase III randomized study. Pediatr Res. 2023;94(3):1035–43.
Robertson CA, Jacqmein J, Selmani A, Galarza K, Oster P. Immunogenicity and safety of a quadrivalent meningococcal conjugate vaccine (MenACYW-TT) administered as a booster to adults aged 59 years: a phase III randomized study. Human Vaccines Immunother. 2023;19(1):2160600.
MENQUADFI™—highlights of prescribing information. 2020.
Knuf M, Rämet M, Breinholt Stærke N, Bertrand-Gerentes I, Thollot Y, B’Chir S, et al. Comparing the meningococcal serogroup C immune response elicited by a tetanus toxoid conjugate quadrivalent meningococcal vaccine (MenACYW-TT) versus a quadrivalent or monovalent C tetanus toxoid conjugate meningococcal vaccine in healthy meningococcal vaccine-naïve toddlers: a randomised, controlled trial. Hum Vaccin Immunother. 2022;18:2052657.
Rivero-Calle I, Raguindin PF, Gómez-Rial J, Rodriguez-Tenreiro C, Martinón-Torres F. Meningococcal Group B vaccine for the prevention of invasive meningococcal disease caused by Neisseria meningitidis serogroup B. Infect Drug Resist. 2019;12:3169–88.
U.S Food and Drug Administration. Structured approach to benefit-risk assessment in drug regulatory decision-making: draft PDUFA V implementation plan—February 2013 (FISCAL YEARS 2013–2017). 2013.
U.S Food and Drug Administration (Center for Drug Evaluation and Research; Center for Biologics Evaluation and Research). Benefit-risk assessment for new drug and biological products. 2021.
Guo JJ, Pandey S, Doyle J, Bian B, Lis Y, Raisch DW. A review of quantitative risk-benefit methodologies for assessing drug safety and efficacy-report of the ISPOR risk-benefit management working group. Value Health. 2010;13:657–66.
U.S Food and Drug Administration. Benefit-risk assessment in drug regulatory decision-making: draft PDUFA VI implementation plan (FY 2018–2022). 2018. Available at https://www.fda.gov/files/about%20fda/published/Benefit-Risk-Assessment-in-Drug-Regulatory-Decision-Making.pdf. Accessed October 03, 2022.
de Bekker-Grob EW, Berlin C, Levitan B, Raza K, Christoforidi K, Cleemput I, et al. Giving patients’ preferences a voice in medical treatment life cycle: the PREFER public-private project. Patient. 2017;10:263–6.
Rüggeberg JU, Gold MS, Bayas J-M, Blum MD, Bonhoeffer J, Friedlander S, et al. Anaphylaxis: case definition and guidelines for data collection, analysis, and presentation of immunization safety data. Vaccine. 2007;25:5675–84.
Sejvar JJ, Kohl KS, Gidudu J, Amato A, Bakshi N, Baxter R, et al. Guillain–Barré syndrome and Fisher syndrome: case definitions and guidelines for collection, analysis, and presentation of immunization safety data. Vaccine. 2011;29:599–612.
Rath B, Gidudu JF, Anyoti H, Bollweg B, Caubel P, Chen Y-H, et al. Facial nerve palsy including Bell’s palsy: case definitions and guidelines for collection, analysis, and presentation of immunisation safety data. Vaccine. 2017;35:1972–83.
Acknowledgements
The authors thank Jean-Sébastien Persico for editorial assistance and manuscript coordination on behalf of Sanofi.
Medical Writing and Editorial Assistance
Medical writing and editorial assistance was funded by Sanofi.
Funding
Sanofi funded this study. Sanofi also funded the medical writing, editorial assistance, and the journal’s Rapid Service Fee.
Author information
Authors and Affiliations
Contributions
All authors attest they meet the ICMJE criteria for authorship. All authors made significant contributions to the conception and design of the study and were involved in the analysis and interpretation of the data. Aiying Chen, Mandeep Singh Dhingra, Marie-Laure Kürzinger, David Neveu, Betzana Zambrano and Lydie Marcelon were involved in the acquisition of the data.
Corresponding author
Ethics declarations
Conflict of Interest
David Neveu, Tamala Mallett Moore, Betzana Zambrano, Marie-Laure Kürzinger, Lydie Marcelon and Mandeep Singh Dhingra are Sanofi employees and may hold stocks/shares. Aiying Chen was an employee of Sanofi at the time of the study was conducted, and held stocks during her employment at Sanofi; she is currently employed at Daiichi Sankyo, New Jersey, United States of America.
Ethical Approval
This analysis is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors. All clinical studies evaluating MenACYW-TT were conducted in accordance with the Declaration of Helsinki as well as in accordance with the Quality Standards of the International Conference on Harmonization Good Clinical Practices.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Aiying Chen: Affiliation at time of study conduct.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Neveu, D., Mallett Moore, T., Zambrano, B. et al. Structured Benefit-Risk Assessment of a New Quadrivalent Meningococcal Conjugate Vaccine (MenACYW-TT) in Individuals Ages 12 Months and Older. Infect Dis Ther 12, 2367–2386 (2023). https://doi.org/10.1007/s40121-023-00864-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-023-00864-4