Abstract
Introduction
Chronic hepatitis B virus (HBV) infection is associated with significant global morbidity and mortality. Low treatment rates are observed in patients living with HBV; the reasons for this are unclear. This study sought to describe patients’ demographic, clinical and biochemical characteristics across three continents and their associated treatment need.
Methods
This retrospective cross-sectional post hoc analysis of real-world data used four large electronic databases from the United States, United Kingdom and China (specifically Hong Kong and Fuzhou). Patients were identified by first evidence of chronic HBV infection in a given year (their index date) and characterized. An algorithm was designed and applied, wherein patients were categorized as treated, untreated but indicated for treatment and untreated and not indicated for treatment based on treatment status and demographic, clinical, biochemical and virological characteristics (age; evidence of fibrosis/cirrhosis; alanine aminotransferase [ALT] levels, HCV/HIV coinfection and HBV virology markers).
Results
In total, 12,614 US patients, 503 UK patients, 34,135 patients from Hong Kong and 21,614 from Fuzhou were included. Adults (99.4%) and males (59.0%) predominated. Overall, 34.5% of patients were treated at index (range 15.9–49.6%), with nucleos(t)ide analogue monotherapy most commonly prescribed. The proportion of untreated-but-indicated patients ranged from 12.9% in Hong Kong to 18.2% in the UK; almost two-thirds of these patients (range 61.3–66.7%) had evidence of fibrosis/cirrhosis. A quarter (25.3%) of untreated-but-indicated patients were aged ≥ 65 years.
Conclusion
This large real-world dataset demonstrates that chronic hepatitis B infection remains a global health concern; despite the availability of effective suppressive therapy, a considerable proportion of predominantly adult patients apparently indicated for treatment are currently untreated, including many patients with fibrosis/cirrhosis. Causes of disparity in treatment status warrant further investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Chronic hepatitis B infection is a global public health problem, with almost 300 million people globally estimated to be living with the infection in 2016. |
The goal of HBV treatment is to improve patients’ quality of life and survival. |
Whilst clinical practice guidelines provide evidence-based recommendations on treatment, not everyone who could benefit is treated. |
This study sought to leverage routine healthcare data to systematically assess treatment need in chronic HBV patient populations across three continents. |
What was learned from the study? |
A considerable unmet need in terms of undertreatment of chronic HBV infection was observed, with approximately 20% of US and UK patients and between 10 and 15% of Chinese patients potentially undertreated. |
Increasing awareness of clinical practice guidelines and increasing adherence to treatment may overcome undertreatment as well as improving patients’ access to treatment. |
As undertreatment correlates with poor patient outcomes and high societal costs, earlier therapeutic intervention may be warranted for patients with chronic HBV infection. |
Introduction
As of 2016, approximately 292 million people worldwide had chronic hepatitis B virus (HBV) infection [1]. While hepatitis B vaccination has reduced childhood HBV incidence [2], challenges remain for access to anti-HBV treatment for adults and children globally [3]. Without this, complications of chronic HBV infection (e.g. cirrhosis, liver decompensation and hepatocellular carcinoma [HCC]) remain a concern, particularly as they are associated with an increased death risk and substantial societal and economic costs [3,4,5].
Chronic HBV clinical practice guidelines (CPGs) [6,7,8] provide evidence-based recommendations on various aspects of patient care, including screening, diagnosis, surveillance and treatment [9]. The goal of treatment for chronic HBV infection is to improve patients’ quality of life and survival. In the absence of cirrhosis and/or other clinical indications for therapy (e.g. chronic HBV reactivation), CPG recommendations are similar in that routine markers of infection (hepatitis B surface antigen [HBsAg]), replication (hepatitis B e antigen [HBeAg] and HBV DNA) and liver inflammation (alanine aminotransferase [ALT]) generally govern decisions for further investigation (e.g. biopsy) or treatment [6,7,8].
Current CPGs recommend nucleos(t)ide analogues (NAs) as first-line therapy for chronic HBV infection because of their tolerability and efficacy in inhibiting HBV DNA replication. These agents are suppressive rather than curative, and treatment duration is typically prolonged or indefinite [6, 10]. In a systematic review and meta-analysis of HBsAg-positive patients [11], only one quarter were deemed treatment eligible based on CPGs [6, 8, 10, 12]. Another study demonstrated that only 5% of diagnosed HBsAg-positive patients were treated [1, 11, 13]. Consequently, it is necessary to further quantify undertreatment in chronic HBV infection to inform on the extent to which extending treatment eligibility could improve patient outcomes [14].
The current study sought to generate and describe standardized data on the demographic, clinical, biochemical and treatment characteristics of four retrospective cohorts of US, UK and Chinese (Hong Kong [HK] and Fuzhou) patients with chronic HBV infection. An algorithm was then developed to determine treatment eligibility and associated characteristics.
Methods
This was a retrospective post hoc cross-sectional analysis of US, UK and Chinese (HK, and Fuzhou) real-world data. An overview of the data sources and methods applied is provided below, with additional details provided in the Supplementary Methods.
Data Sources
All data were extracted from healthcare or insurance databases. For the US cohort, the subset of Optum’s de-identified Clinformatics® Data Mart (CDM) Database with laboratory data was used. Optum’s CDM is derived from a database of administrative health claims for members of large commercial and Medicare Advantage health plans. The UK cohort was sourced from the National Institute for Health and Care Research Health Informatics Collaborative (NIHR HIC) Viral Hepatitis Theme Database [15, 16]. The NIHR HIC is a collaboration between research-active UK National Health Service (NHS) hospital trusts (i.e. secondary-care setting only). Anonymized HK data were provided by the Clinical Data Analysis and Reporting System, developed by the Hong Kong Hospital Authority and capturing > 90% of the HK population. For Fuzhou, anonymized data were collected from the National Healthcare Big Data Platform (Fuzhou), which covers > 23 million patients (secondary care setting only).
The study sponsor did not have access to individual patient data for any of the cohorts and received only summary tables.
Study Population
Study design for each location is described in Supplementary Fig. 1. Patients in the UK, HK and Fuzhou were identified based on HBV-specific diagnostic codes or laboratory codes/results in 2015 (UK) or 2017 (HK and Fuzhou); the first qualifying date in each year defined the patients’ index date (Table 1). As the UK inclusion criteria did not use diagnostic codes for chronic disease, additional exclusion criteria were employed to minimize the inclusion of cases of acute HBV infection (Table 1). In the US, patients were identified between 1 January 2010 and 1 January 2016 based on HBV-specific diagnostic codes; identified patients who were enrolled on 1 January 2016 were included, with this forming their disease index date.
A minimum 12-month period of historical baseline observation was applied in all studies, with patients aged ≥ 2 years included if they met this criterion (children < 2 years may not have accrued this observation time at diagnosis). The observation period was subsequently extended to 5 years for HK because of a high level of missing data at one year. However, a minimum 12-month baseline period could not be applied in the UK, and applying this criterion had little (US and Fuzhou) or no impact (HK) in the remaining cohorts (Supplementary Table 1).
Demographics (age, sex, ethnicity), clinical characteristics (coinfections, liver fibrosis, cirrhosis, cancer [including HCC], liver transplantation history), laboratory data (HBsAg, HBeAg, HBV DNA, ALT) and treatment at disease index were all described. Initial HK findings revealed that diagnostic codes returned unexpectedly low levels of fibrosis and cirrhosis (0.15% and 2.04%, respectively), based on 5 years of historical data. Post hoc US analyses revealed 1-year baseline levels of 1.14% and 2.81% for fibrosis and cirrhosis, respectively. ICD coding was not used in the UK database and these data were unavailable for Fuzhou. Accordingly, the fibrosis-4 (FIB-4) index and aspartate aminotransferase (AST)-to-platelet ratio index (APRI) scores were calculated to augment ICD-based diagnoses in all studies, with fibrosis defined using cut-offs of > 0.70 and > 2.65 for APRI [17, 18] and FIB-4, respectively, and cirrhosis defined using > 2.0 and > 3.6, respectively [12, 19].
Treatment Eligibility Algorithm Derivation and Application
Each study produced a single anonymized dataset, comprising a count of patients meeting all possible combinations of age, fibrosis, cirrhosis, human immunodeficiency virus (HIV)/HCV coinfection, hepatitis delta virus (HDV) infection, HBsAg, HBeAg, HBV DNA, ALT and treatment status. In HK, this was undertaken on a random 50% sample of the original dataset to further ensure patient confidentiality. These aggregated data outputs were supplied centrally to GSK where the data were standardized, categorized and analysed in Statistical Analysis System (SAS) version 9.4. Patients with missing HBeAg, HBV DNA and ALT data were assumed to have negative, < 2,000 IU/ml and < 2 upper limit of normal (ULN), respectively. These modal values for each variable represented 76.4% (HBeAg), 86.6% (HBV DNA) and 94.0% (ALT) of values among non-missing observations.
Children and adolescents (< 18 years) were excluded from treatment eligibility assessment as they are generally ineligible for treatment [6, 10, 12]. HBsAg-negative patients were also excluded as their status as ‘true’ patients with chronic HBV infection was uncertain. Untreated HBV/HCV coinfected patients with abnormal ALT values or evidence of fibrosis/cirrhosis at index were also excluded as the aetiology of the liver damage was deemed undeterminable. Eligible patients were subsequently classified as ‘treated’, ‘untreated-but-indicated’ or ‘untreated-and-not-indicated’ as per Table 2. Patients in the latter two groups were further classified into chronic HBV disease phases based on their HBeAg status [6]. Finally, patients’ input data were categorized by treatment categories to inform on factors that might drive clinicians’ treatment decisions in each location: for example, the risk of being untreated but indicated for patients with a history of fibrosis/cirrhosis was calculated relative to those patients with no fibrosis/cirrhosis history and the data presented graphically with 95% confidence intervals (CIs).
Data Analysis
All analyses were descriptive. Relative frequencies were calculated for categorical variables, while means ± standard deviation (SD), ranges and median values with interquartile range were calculated for continuous variables; 95% CIs for proportions—reported in square parentheses in this manuscript—were calculated as p ± (1.96*(√((p*(1-p))/N)), where p equalled the sample proportion and N equalled the sample size. If p*N or (1-p)*N was < 10 then exact CIs were calculated using Stata 14.1 (StataCorp, College Station, TX, USA).
Ethics
The studies complied with all applicable laws regarding patient privacy. Ethical approval and informed consent were not required for the analysis of the Health Insurance Portability and Accountability Act (HIPAA)-compliant US data. Over-arching ethical approval for the UK database (REC reference 15/SC/0523) facilitated the use of the anonymized data for analysis without informed consent. The HK study was approved by the institutional review board of the University of Hong Kong and the Hospital Authority Hong Kong West Cluster (reference: UW 18–471). The China study was reviewed and approved by the central China Ethics Committee of Registering Clinical Trials (reference: ChiECRCT-20180222) with an agreement of consent waiver.
Results
The final study population comprised 12,614 patients from the US, 503 from the UK, 34,135 from HK and 21,614 from Fuzhou (Fig. 1). Patients’ baseline characteristics are described in Table 3.
Patient disposition flow chart *Exclusion criteria for the algorithm are not mutually exclusive. The presence of multiple values highlights the number of patients who were excluded by more than one criterion. **Additional step in Hong Kong to protect patient confidentiality. ALT alanine aminotransferase, CHB chronic hepatitis B, HBsAg -ve negative for hepatitis B surface antigen, HCV hepatitis C virus, ULN upper limit of normal
Demographic and Clinical Characteristics
Most patients were adults (≥ 18 years), but more patients in the US (38.1%) and in HK (24.7%) were elderly (≥ 65 years) compared with the UK (7.6%) and Fuzhou (6.1%); there were few pediatric patients (< 18 years of age; range 0.3–1.0%). Males predominated throughout (range 54.3–68.6%), with highest male prevalence in Fuzhou. In the US and the UK, where race/ethnicity data were available and not recorded as ‘unknown’, Asians accounted for 50.0% [49.0–51.0%] and 30.5% [25.9–35.0%] of patients, respectively.
Coinfection with HCV and/or HIV (range 0.08–1.2%) or with HDV (range 0.003–1.8%) was low in the UK, HK and Fuzhou; however, in the US it was 16.0% for HCV and/or HIV and 8.8% for coinfection with HDV. The baseline prevalence of liver fibrosis was consistent in most locations (~ 13%) except the UK, where the excess (21.3%) was mirrored by less cirrhosis (5.2%) than elsewhere (13.1–18.8%). A history of HCC was uncommon (range 0–3.7%), as was a liver transplantation history (range 0–1.7%).
Baseline Laboratory Findings and Treatment Characteristics
Missing baseline data were observed for key laboratory parameters. Over one quarter of HBsAg measurements (26.2%; range 7.3–50.3%), almost half of HBeAg observations (48.3%; range 27.6–69.3%) and nearly two-thirds of HBV DNA values (63.3%; range 32.1–88.1%) were missing. Data on ALT were more complete (89.8%) but a greater percentage was missing in Fuzhou (25.8%) compared with elsewhere (range 2.7–10.5%). Where non-missing data were available, most patients (range 26.5–64.8%) were HBeAg negative, but more Fuzhou patients were HBeAg positive (21.5%) than elsewhere (range 4.2–9.2%). Most patients fell into ‘low’ levels of HBV DNA (< 20,000 IU/ml; range 67.7–81.1%) and ALT (< 2 × ULN; 91.8–96.5%); however, more HK patients (18.8%) had ‘high’ HBV DNA (≥ 2000 IU/ml) compared with other cohorts (range 9.2–12.5%). More UK (8.2% [5.7–10.8%]) and HK (8.0% [7.7–8.3%]) patients had increased ALT levels (≥ 2 × ULN) than US (3.6% [3.2–3.9%]) or Fuzhou (3.5% [3.2–3.8%]) patients. A post hoc analysis of the characteristics of patients with and without laboratory data are provided in Supplementary Table 2. Overall, younger patients (18 – < 65 years) were more likely to have available laboratory data than elderly patients, but these relationships differed by country and treatment status. Treated younger adults tended to have more complete HBeAg, ALT and HBV DNA data and less complete HBsAg data than untreated young adults; treatment-specific differences were less apparent for elderly patients.
Most patients across all locations were untreated at disease index. More Fuzhou patients (49.6% [48.9–50.2%]) were treated than HK patients (31.5% [31.0–32.0%]), who in turn were more often treated than US (17.8% [17.1–18.5%]) and UK patients (15.9% [12.7–19.1%]). NA monotherapy was the most frequently prescribed treatment regimen (range 14.5–43.6%); tenofovir predominated in the US (65.5% [63.5–67.4%]) and the UK (68.5% [57.8–79.1%]), whereas entecavir use was more common in HK (82.6% [81.8–83.3%]) and Fuzhou (79.4% [78.6–80.2%]). Interferons, either alone or in combination, were rarely prescribed (range 0–0.4%).
Algorithm-Derived Treatment Eligibility Status
A total of 9231 patients from the US, 496 from the UK, 16,819 from HK and 21,050 from Fuzhou were included in the treatment algorithm analysis (Table 4). Characteristics of excluded patients are shown in Supplementary Table 3.
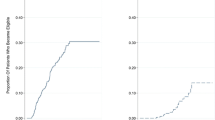
The proportion of ‘untreated-but-indicated’ patients was higher in the US (17.4%) than in Fuzhou (14.6%) and in HK (12.9%); the point estimate for the UK (18.2%) was closer to that of the US, but the 95% CI (14.9–21.8%) marginally overlapped with that for Fuzhou. Most ‘untreated-but-indicated’ patients (range: 53.3–84.2%) would be classified as ‘HBeAg-negative chronic hepatitis B’ patients according to CPGs [6, 8, 10]. The proportion of ‘untreated-and-not-indicated’ patients was highest in the UK (65.7%), followed by the US (61.6%), HK (55.4%) and Fuzhou (35.3%). Most patients in this group were classified as ‘HBeAg-negative chronic HBV infection’ patients according to CPGs [6]. The relationship between the treatment eligibility status and patient characteristics is shown in Fig. 2 (complete data are provided in Supplementary Table 4). Given the construction of the algorithm, the presence of fibrosis/cirrhosis, high HBV DNA and abnormal ALT were consistent drivers for being ‘untreated but indicated’. Almost two thirds of patients in this group (63.1% [61.9–64.2%]; range 61.3–66.7%) had fibrosis/cirrhosis; almost one third (31.9% [30.8–33.0%]) had high HBV DNA and over a fifth (22.2% [21.2–23.2%]) had elevated ALT. Age and HBeAg status were also drivers of undertreatment, but to a lesser extent than the above characteristics, in that the risk of being ‘untreated but indicated’ was higher in older patients (8.9–45.0% of patients in this group were ≥ 65 years) and in HBeAg-positive patients. There was a trend towards HCV/HIV coinfection driving undertreatment in most locations, whereas in the US HCV/HIV coinfected group, patients were more often treated appropriately compared with the UK, HK and Fuzhou.
Relative risk of patients being categorized as “untreated-but-indicated” according to baseline demographic, clinical and biochemical characteristics. The error bars represent 95% CIs. Children and adolescents (< 18 years of age) were excluded from assessment of treatment eligibility as they are generally ineligible for treatment; HBsAg-negative patients were also excluded as their status as ‘true’ patients with chronic HBV infection was uncertain. ALT alanine aminotransferase, CI confidence interval, DNA deoxyribonucleic acid, FZ Fuzhou, China, HBeAg + ve positive for hepatitis B e antigen, HBsAg hepatitis B surface antigen, HBV hepatitis B virus, HCV hepatitis C virus, HIV human immunodeficiency virus, HK Hong Kong, China, UK United Kingdom, ULN upper limit of normal, US United States
Discussion
This study sought to generate standardized demographic, clinical and biochemical data on geographically disparate chronic HBV patients and estimate treatment eligibility with these data. The treatment algorithm developed and applied aligns with clinical practice in the regions studied; hence, the findings are meaningful. To our knowledge, this is the first analysis to systematically compare treatment needs in chronic HBV populations across three continents.
Our study suggests a considerable unmet treatment need in chronic HBV infection. Approximately 20% of US and UK and between 10 and 15% of Chinese patients were potentially undertreated. This suggests a lack of awareness of, and/or adherence to, CPGs by physicians, treatment hesitancy or poor access to treatment. Adherence to CPGs for first-line therapy has been associated with improved clinical outcomes at no increased cost [20]. Despite this, poor guideline adherence in terms of patient monitoring, invasive testing and treatment initiation occurs [21,22,23], with CPG unfamiliarity often blamed for the discrepancy. The complexity of HBV management and confusing nomenclature (e.g. ‘inactive carrier’) may also encourage under-informed treatment decisions.
Considerable patient heterogeneity was observed across locations. Despite these differences, our findings are consistent for undertreated patient populations in each location. A larger proportion of the ‘untreated-but-indicated’ patients was older, suggesting either an age-specific health inequality concerning appropriate care or competing effects of treatment for comorbid conditions. Alternatively, older patients’ may be reluctant to take regular medication to reduce the risk of outcomes that may not occur in their lifespan.
Despite guidelines recommending that patients with cirrhosis/fibrosis receive treatment regardless of laboratory findings [6,7,8, 10], a disquieting proportion of patients with a history of fibrosis and/or cirrhosis were ‘untreated but indicated’. This observation is concerning as an estimated 720,000 viral hepatitis deaths in 2015 were due to cirrhosis [3]. This could reflect a lack of CPG awareness/adherence, as outlined above. Alternatively, the augmentation of code-based definitions with APRI and FIB-4 scores—and specifically the cut-offs applied—may have artificially inflated this patient group. These laboratory scores have high negative predictive value but low positive predictive value in determining fibrosis/cirrhosis [24], making our findings more sensitive than specific (a feature that may be beneficial in this instance as it rules in rather than rules out). However, this is preferential to the only other potential approach, namely relying on diagnostic codes alone (biopsy data are rarely available in routine EHR data). This other approach is inadequate, as diagnostic codes substantially underestimate the predicted prevalence of fibrosis/cirrhosis based on clinical expertise and the published literature (20% cirrhosis by biopsy [UK] [25]; 8–35% cirrhosis in the US [26,27,28]).
It is important to consider the potential benefit of therapy for ‘untreated-but-indicated’ patients. Existing treatment thresholds are arguably too stringent, allowing an unchecked burden of liver disease to emerge in those currently ineligible. Treatment need, as defined by current guidelines, targets those with the highest biochemical and virological activity, where the benefit-to-risk ratio of lifelong therapy is most obvious [7,8,9,10]. Once defined-duration therapies that achieve functional cure become available, they may be indicated for a broader population of individuals living with chronic HBV infection [14, 29]. Future work is needed to evaluate the impact of extending therapy to treat a broader chronic HBV population both to reduce the risk of individual cases of liver disease and to have a population-level benefit in reducing the risk to lower disease incidence.
Although biochemical parameters inform chronic HBV staging, and, in combination with liver disease severity, inform treatment need, many biochemical data were routinely missing [6, 8]. The data in Supplementary Table 2 support the view that patient characteristics, rather than CPGs, appear to dictate laboratory testing/data availability; hence, missing data are largely ‘not tested’ rather than ‘not available’. This creates a paradox: one wants to use the most relevant data to generate the ‘best’ estimates of treatment need, but the data sources which could provide these do not have the observations because the tests do not appear to be warranted in the very patients one is seeking to classify! Consequently, pragmatism is required to deal with missing data, and we believe the approach taken (simple imputation) represents the most objective conservative approach compared to the alternatives. Restricting findings to complete-patient data results in substantial data loss in most geographies (> 60% in the US and Hong Kong, > 40% in the UK and nearly 30% in Fuzhou; Supplementary Table 2), where younger patients are over-represented whilst the untreated elderly patients are often excluded. When the algorithm is applied to these data (Supplementary Table 5; note, ‘treated’ is applied before the need for biochemistry data) the ‘treated’ are unnaturally inflated and the ‘untreated but indicated’ are skewed downwards. In the present study, this is not the case because the complete data effectively capture treatment for each cohort. Multiple imputation may also have been a valid alternative [30], but it relies on the assumption that data are missing at random and should not be applied when there are extensive missing data (recommendations of no more than 10–40% have been suggested) [31]; neither of these are applicable for the present study data. In this study, patients were identified using a mixture of HBsAg data and diagnostic codes, depending on location, and HBsAg data were missing for many patients. While HBsAg represents the gold standard for confirming chronicity of HBV infection [6, 8, 10], these missing data may reflect the fact that HBsAg is not routinely monitored once chronicity is established. Major treatment guidelines reflect this: HBsAg is rarely mentioned and only in the context of anti-HBV therapy where infection would, of course, be established [6, 8, 10].
Several other study design aspects should also be considered. The treatment eligibility estimates, generated from cross-sectional data, may not be widely generalizable to routine clinical practice as the parameters assessed can be modified on a short- (e.g. HBeAg, HBV DNA and ALT) and long-term (e.g. fibrosis/cirrhosis) basis, and can also be modified by treatment. Long-term clinical variability, reflecting the natural history of chronic HBV infection, would ultimately inform treatment decisions. We may also have over-estimated the proportion of ‘untreated-but-indicated’ patients because of the conservative treatment definition applied (an anti-HBV medication prescription covering index). Additionally, while the treatment algorithm was constructed based on recent CPGs, it has not been validated. Although most of the elements of the current approach would receive general clinical acceptance, some parameters (HBV DNA ≥ 20,000 IU/ml or ALT ≥ 2 × ULN for defining ‘untreated but indicated’) may stimulate greater debate [32]. Significant liver damage can be detected in patients with persistently normal ALT (PNALT) and high serum HBV DNA [33], and HBV DNA ≥ 10,000 IU/ml has been associated with an increased risk of HCC [34]. Hence, some researchers recommend initiating treatment in patients with a HBV DNA > 20,000 IU/ml without considering any other criteria [35]. Consequently, including these patients as ‘untreated but indicated’ can be justified. Furthermore, recoding patients with HBV DNA ≥ 20,000 IU/ml as ‘untreated and not indicated’ would not alter our conclusions as a substantial proportion of ‘untreated but indicated’ patients would remain (Supplementary Table 6).
The UK sample size was small and the two Southeast England secondary care sites included may not wholly represent the UK. Similarly, whilst the largely urban Fuzhou data are perhaps less representative of the wider Chinese chronic HBV population, the majority of the Chinese population reside in urban areas [36]; hence, the findings will be generalizable to this setting. Additionally, site-specific cohort construction may have reduced generalizability and limited between-location comparability. The requirement for a chronic HBV-related interaction in the year of interest in most locations may have excluded patients with mild disease who did not require care in that year, limiting generalizability to clinically managed patients. However, the comparison with the US cohort, where all patients with chronic HBV infection identified up to a specific date were included, suggests that this is unlikely, especially as most patients with chronic HBV infection will require routine clinical review at least annually. Finally, the selection of HK patients, in part based on a single positive HBsAg test result, had the potential to include patients with acute HBV infection. However, hepatitis B is a notifiable disease in HK, and only 33 cases of acute hepatitis B infection were reported in 2017, suggesting a negligible impact of this criterion (0.097%).
General limitations that are common to real-world administrative database studies, including the potential for missing or inaccurate diagnostic, procedural or medication codes, are relevant here and may have impacted the findings. Findings from the US may also reflect healthcare provider’s reimbursement claims rather than the patient’s diagnoses.
Conclusions
In conclusion, leveraging the best source of routinely available data that effectively captures the spectrum of patients with chronic HBV infection under clinical care, we show that across multiple geographies a considerable proportion of patients may remain untreated despite meeting accepted treatment thresholds. The undertreatment burden is undoubtedly higher when undiagnosed disease is considered: Polaris collaborators estimated that, globally, 29 million of the 292 million global chronic HBV patients in 2016 were diagnosed, but also that 94 million were treatment eligible [1]. Increasing awareness of CPGs in the healthcare environment and increasing adherence to treatment could overcome undertreatment. Potential differences in access to treatment and patients’ preferences should also be considered as they may exacerbate the issue of undertreatment. Given that low treatment levels correlate with poor patient outcomes and high societal costs, earlier therapeutic intervention for patients with chronic HBV infection may be warranted.
Change history
27 September 2023
A Correction to this paper has been published: https://doi.org/10.1007/s40121-023-00857-3
References
Polaris Observatory Collaborators. Global prevalence, treatment, and prevention of hepatitis B virus infection in 2016: a modelling study. Lancet Gastroenterol Hepatol. 2018;3(6):383–403.
World Health Oragnization. Hepatitis B Fact Sheet. https://www.who.int/news-room/fact-sheets/detail/hepatitis-b.
World Health Organization. Global Hepatitis Report, 2017. 2017.
Sbarigia U, Kariburyo F, Sah J, et al. Evaluating the Effect of Standard of Care Treatment on Burden of Chronic Hepatitis B: A Retrospective Analysis of the United States Veterans Population. Adv Ther. 2020;37(3):1156–72.
Sorrell MF, Belongia EA, Costa J, et al. National Institutes of Health Consensus Development Conference Statement: management of hepatitis B. Ann Intern Med. 2009;150(2):104–10.
European Association for the Study of the Liver. EASL 2017 Clinical Practice Guidelines on the management of hepatitis B virus infection. J Hepatol. 2017;67(2):370–98.
National Institute for Health and Care Excellence (NICE). Hepatitis B (Chronic): Diagnosis and Management of Chronic Hepatitis B in Children, Young People and Adults 2013.
Sarin SK, Kumar M, Lau GK, et al. Asian-Pacific clinical practice guidelines on the management of hepatitis B: a 2015 update. Hepatol Int. 2016;10(1):1–98.
Han SH, Tran TT. Management of Chronic Hepatitis B: An Overview of Practice Guidelines for Primary Care Providers. J Am Board Fam Med. 2015;28(6):822–37.
Terrault NA, Lok ASF, McMahon BJ, et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance. Hepatology. 2018;67(4):1560–99.
Tan M, Bhadoria AS, Cui F, et al. Estimating the proportion of people with chronic hepatitis B virus infection eligible for hepatitis B antiviral treatment worldwide: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2021;6(2):106–19.
World Health Organization. Guidelines for the Prevention, Care and Treatment of Persons with Chronic Hepatitis B Infection. Geneva: World Health Organization; 2015.
Vu VD, Do A, Nguyen NH, et al. Long-term follow-up and suboptimal treatment rates of treatment-eligible chronic hepatitis B patients in diverse practice settings: a gap in linkage to care. BMJ Open Gastroenterol. 2015;2(1): e000060.
McNaughton AL, Lemoine M, van RC, Matthews PC. Extending treatment eligibility for chronic hepatitis B virus infection. Nat Rev Gastroenterol Hepatol. 2020;18(3):146–7.
National Institute for Health Research. Viral Hepatitis. https://hic.nihr.ac.uk/viral+hepatitis.
Smith DA, Wang T, Freeman O, et al. National Institute for Health Research Health Informatics Collaborative: development of a pipeline to collate electronic clinical data for viral hepatitis research. BMJ Health Care Inform. 2020;27(3): e100145.
Kim BK, Kim DY, Park JY, et al. Validation of FIB-4 and comparison with other simple noninvasive indices for predicting liver fibrosis and cirrhosis in hepatitis B virus-infected patients. Liver Int. 2010;30(4):546–53.
Lin ZH, Xin YN, Dong QJ, et al. Performance of the aspartate aminotransferase-to-platelet ratio index for the staging of hepatitis C-related fibrosis: an updated meta-analysis. Hepatology. 2011;53(3):726–36.
Parikh P, Ryan JD, Tsochatzis EA. Fibrosis assessment in patients with chronic hepatitis B virus (HBV) infection. Ann Transl Med. 2017;5(3):40.
Han SH, Jing W, Mena E, et al. Adherence, persistence, healthcare utilization, and cost benefits of guideline-recommended hepatitis B pharmacotherapy. J Med Econ. 2012;15(6):1159–66.
Juday T, Tang H, Harris M, Powers AZ, Kim E, Hanna GJ. Adherence to chronic hepatitis B treatment guideline recommendations for laboratory monitoring of patients who are not receiving antiviral treatment. J Gen Intern Med. 2011;26(3):239–44.
Wu Y, Johnson KB, Roccaro G, et al. Poor adherence to AASLD guidelines for chronic hepatitis B Management and treatment in a large academic medical center. Am J Gastroenterol. 2014;109(6):867–75.
Zhang S, Ristau JT, Trinh HN, Garcia RT, Nguyen HA, Nguyen MH. Undertreatment of Asian chronic hepatitis B patients on the basis of standard guidelines: a community-based study. Dig Dis Sci. 2012;57(5):1373–83.
Xiao G, Yang J, Yan L. Comparison of diagnostic accuracy of aspartate aminotransferase to platelet ratio index and fibrosis-4 index for detecting liver fibrosis in adult patients with chronic hepatitis B virus infection: a systemic review and meta-analysis. Hepatology. 2015;61(1):292–302.
Tedder RS, Rodger AJ, Fries L, et al. The diversity and management of chronic hepatitis B virus infections in the United Kingdom: a wake-up call. Clin Infect Dis. 2013;56(7):951–60.
Serper M, Choi G, Forde KA, Kaplan DE. Care delivery and outcomes among US veterans with hepatitis B: A national cohort study. Hepatology. 2016;63(6):1774–82.
Spradling PR, Xing J, Rupp LB, et al. Infrequent Clinical Assessment of Chronic Hepatitis B Patients in United States General Healthcare Settings. Clin Infect Dis. 2016;63(9):1205–8.
Tong MJ, Blatt LM, Tyson KB, Kao VW. Death From Liver Disease and Development of Hepatocellular Carcinoma in Patients With Chronic Hepatitis B Virus Infection: A Prospective Study. Gastroenterol Hepatol (N Y). 2006;2(1):41–7.
Cornberg M, Lok AS, Terrault NA, Zoulim F. Guidance for design and endpoints of clinical trials in chronic hepatitis B - Report from the 2019 EASL-AASLD HBV Treatment Endpoints Conference. J Hepatol. 2020;72(3):539–57.
Sterne JA, White IR, Carlin JB, et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ. 2009;338: b2393.
Madley-Dowd P, Hughes R, Tilling K, Heron J. The proportion of missing data should not be used to guide decisions on multiple imputation. J Clin Epidemiol. 2019;110:63–73.
Vlachogiannakos J, Papatheodoridis GV. Hepatitis B: Who and when to treat? Liver Int. 2018;38(Suppl 1):71–8.
Ormeci A, Aydin Y, Sumnu A, et al. Predictors of treatment requirement in HBeAg-negative chronic hepatitis B patients with persistently normal alanine aminotransferase and high serum HBV DNA levels. Int J Infect Dis. 2016;52:68–73.
Chen CJ, Yang HI, Su J, et al. Risk of hepatocellular carcinoma across a biological gradient of serum hepatitis B virus DNA level. JAMA. 2006;295(1):65–73.
Özdoğan O, Yaraş S, Köksal AR, et al. A Misleading Parameter in the Diagnosis of Chronic Hepatitis B: Persistently Normal Transaminases. Viral Hepat J. 2018;24(3):79.
United Nations. World Urbanization Prospects. The. Revision. New York: United Nations; 2018. p. 2019.
Acknowledgements
The UK data collection for this research were conducted using NIHR Health Informatics Collaborative (HIC) data resources. Data collection and processing were provided by NIHR Biomedical Research Centres at Imperial College Healthcare NHS Trust and Oxford University Hospitals NHS Foundation Trust.
The authors would like to thank Abdulrahim Mulla (Imperial College Healthcare NHS Trust, London) for his contributions. Abdulrahim Mulla was not directly paid by GSK for his assistance. He was part of the collaboration with NIHR HIC, who were funded to conduct the study.
Optum Clinformatics Data Mart is owned by or licensed to Optum.
Funding
The studies included in these analyses were funded by GSK (Studies 208520; 208521; 212558; 208571). GSK also funded the journal rapid service publication fee. Data collection and processing was funded by NIHR Biomedical Research Centres at Oxford University Hospitals NHS Foundation Trust and Imperial College Healthcare NHS Trust. PCM is funded by a Wellcome intermediate fellowship (ref. 110110/Z/15/Z). KKCM is funded by CW Maplethorpe Fellowship. GSC is supported in part by NIHR Research Professorship.
GSK,208520,208521,212558,208571
Medical Writing and/or Editorial Assistance
Editorial support in the form of development of the initial draft, collating author comments, assembling tables and figures, copyediting and referencing was provided by Appitha Eakin and Sheekha Amin, of Fishawack Indicia Ltd., part of Fishawack Health, and funded by GSK.
Author Contributions
Iain A Gillespie initiated the study. Iain A Gillespie, Eleanor Barnes, Ian CK Wong, Philippa C Matthews, Craig Tipple, Robert C Elston, Tingyan Wang, Kenneth KC Man, Wallis CY Lau, Xing Meng, Luca Mercuri, Naomi Boxall, Sarah Jenner, Jane Dong and Dickens Theodore contributed to the conception or design of these studies/analyses. Eleanor Barnes, Ian CK Wong, Graham S Cooke, Tingyan Wang, Jim Davies, Kinga A Várnai, Oliver Freeman, Ben Glampson and Luca Mercuri contributed to the acquisition and processing of study data. Iain A Gillespie, Eleanor Barnes, Ian CK Wong, Philippa C Matthews, Graham S Cooke, Craig Tipple, Robert C Elston, Yunhao Liu, David A Smith, Kenneth KC Man, Wallis CY Lau, Ben Glampson, Xing Meng, Eleonora Morais, Sen Liu, Naomi Boxall, Sarah Jenner, Stuart Kendrick, Jane Dong and Dickens Theodore contributed to data analysis or interpretation. All authors revised the manuscript critically for important intellectual content and approved the final version for publication.
Prior Publication
Study 208571 data (Fuzhou, China) were presented at The Asian Pacific Association for the Study of the Liver (APASL) 2020 (Abstract #404).
Disclosures
Iain A Gillespie, Robert C Elston, Eleonora Morais, Stuart Kendrick, Jane Dong and Dickens Theodore are employees of GSK and hold stocks/shares in the company. Yunhao Liu, Xing Meng, Craig Tipple and Sen Liu were employees of GSK at the time of study conduct. David A Smith, Luca Mercuri, Wallis CY Lau, Tingyan Wang, Jim Davies, Philippa C Matthews, Oliver Freeman, Kinga A Várnai, Ben Glampson, Sarah Jenner, Eleanor Barnes and Graham S Cooke have no conflicts of interest. Kenneth KC Man, Ian CK Wong and Naomi Boxall received consultancy fees from IQVIA Ltd. Ian CK Wong reports research funding outside the submitted work from Amgen, Bristol-Myers Squibb, Pfizer, Janssen, Bayer, GSK, Novartis, MSD, the Hong Kong Research Grants Council, and the Hong Kong Health and Medical Research Fund, National Institute for Health Research in England, European Commission, National Health and Medical Research Council in Australia, and also received speaker fees from Janssen and Medice consultancy fee from IQVIA in the previous 3 years.
Compliance with Ethics Guidelines
The studies complied with all applicable laws regarding patient privacy. Ethical approval and informed consent were not required for the analysis of the Health Insurance Portability and Accountability Act (HIPAA)-compliant US data. Over-arching ethical approval for the UK database (REC reference 15/SC/0523) facilitates the use of the anonymized data for analysis without informed consent. The HK study was approved by the institutional review board of the University of Hong Kong and the Hospital Authority Hong Kong West Cluster (reference: UW 18–471). The China study was reviewed and approved by the central China Ethics Committee of Registering Clinical Trials (reference: ChiECRCT-20180222) with an agreement of consent waiver.
Data Availability
GSK makes available anonymized individual participant data and associated documents from interventional clinical studies which evaluate medicines, upon approval of proposals submitted to www.clinicalstudydatarequest.com. To access data for other types of GSK sponsored research, for study documents without patient-level data and for clinical studies not listed, please submit an enquiry via the website.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Gillespie, I.A., Barnes, E., Wong, I.C.K. et al. Patient Biochemistry and Treatment Need in Chronic Hepatitis B Virus Infection Across Three Continents: Retrospective Cross-Sectional Cohort Studies. Infect Dis Ther 12, 2513–2532 (2023). https://doi.org/10.1007/s40121-023-00824-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-023-00824-y