Abstract
Introduction
Talaromyces marneffei (T. marneffei), a dimorphic fungus, causes local or disseminated infection in humans. We aimed to analyze the clinical characteristics, prognostic factors, and survival outcomes of patients with T. marneffei infection and compare the differences between human immunodeficiency virus (HIV)-positive and HIV-negative subgroups.
Methods
We retrospectively analyzed 241 patients with T. marneffei infection at the First Affiliated Hospital of Guangxi Medical University between January 2012 and January 2022. The overall population was stratified into HIV-positive (n = 98) and HIV-negative (n = 143) groups according to HIV status. Kaplan–Meier analysis and multivariate Cox regression models were used to determine the prognostic factors for overall survival (OS) and progression-free survival (PFS).
Results
With a median follow-up time of 58.9 months, 120 patients (49.8%) experienced disease progression and 85 patients (70.8%) died. The 5-year rates of OS and PFS were 61.4% (95% CI 55.0–68.6%) and 47.8% (95% CI 41.5–55.1%), respectively. As an independent factor, patients who were HIV positive had better PFS (HR 0.50, 95% CI 0.31–0.82; p < 0.01) than patients who were HIV negative. Compared with patients who were HIV positive, patients who were HIV negative were older and had more probabilities of underlying diseases, chest involvement, bone destruction, and higher count of neutrophils (all p < 0.05). Hemoglobin (PFS: HR 0.62; 95% CI 0.39–1.00; p < 0.05; OS: HR 0.45; 95% CI 0.22–0.89; p = 0.02) and lymphocyte count (PFS: HR 0.06; 95% CI 0.01–0.26; p < 0.01; OS: HR 0.08; 95% CI 0.01–0.40; p < 0.01) were independent prognostic factors for PFS and OS in patients who were HIV negative.
Conclusions
Patients with T. marneffei infection have a poor prognosis. Patients who are HIV positive and HIV negative have relatively independent clinical characteristics. Multiple organ involvement and disease progression are more common in patients who are HIV negative.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
T. marneffei infection in humans remains neglected owing to the lack of competent knowledge of disease performance and prognosis. |
We systematically analyzed the clinical characteristics, prognostic factors, and survival outcomes of 241 patients infected with T. marneffei and compared the differences between individuals who were HIV positive and HIV negative. |
Clinical features of T. marneffei differ in patients who are HIV positive and HIV negative. |
Patients who are HIV negative with T. marneffei infection have a higher neutrophil count, more organ damage, and present a higher mortality. |
Introduction
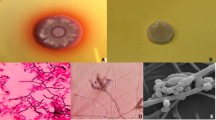
Talaromyces marneffei (T. marneffei), a thermally dimorphic fungus, is mainly prevalent in the tropical areas of South and Southeast Asia [1], especially in Thailand, India, Vietnam, and southern China. The occurrence of T. marneffei infections in humans is mainly caused by inhaling spores in the surroundings [2]. T. marneffei spores transform into the pathogenic yeast form in macrophages after entering the human body, leading to localized or severe disseminated infection [3]. Disseminated T. marneffei infections may involve multiple organs and systems, and present with fever, anemia, bone marrow involvement, lymphadenopathy, skin lesions, hepatosplenomegaly, respiratory symptoms, and weight loss [4]. Patients with disseminated T. marneffei infection display high rates of mortality and relapse after treatment, especially in patients without human immunodeficiency virus (HIV) [5].
Previously, T. marneffei infection was regarded as an acquired immune deficiency syndrome (AIDS)-defining disease in South and Southeast Asia [6]. In northern Thailand, disseminated T. marneffei infection is the third most frequent opportunistic infection among patients infected with HIV, ranking just below tuberculosis and Cryptococcus spp. [7]. Over the past few decades, the prevalence of T. marneffei infections in patients who are HIV positive has decreased dramatically by using powerful antiretroviral therapy and controlling the epidemic of HIV/AIDS [1, 8]. A growing number of patients who are HIV negative with impaired cell-mediated immunity have been reported to experience T. marneffei infection [9, 10]. However, T. marneffei infection in humans remains neglected owing to the lack of competent knowledge of disease diagnosis and therapy. A previous study also revealed that patients who are HIV negative with T. marneffei infection have a higher mortality than patients who are infected with HIV due to misdiagnosis or delayed diagnosis [11].
The improvement in understanding of T. marneffei infection in both patients who are HIV positive and HIV negative is equally important for the clinician. Therefore, we systematically analyzed the clinical characteristics, prognostic factors, and survival outcomes of 241 patients with T. marneffei infection and compared the differences between HIV-positive (n = 98) and HIV-negative (n = 143) subgroups in a 10-year retrospective cohort. This study might provide the new recognition of T. marneffei infection for the clinician and contribute to early diagnosis of T. marneffei infection.
Methods
Study Participants
We retrospectively collected 241 patients with T. marneffei infection at the First Affiliated Hospital of Guangxi Medical University between January 2012 and January 2022. The diagnostic criteria of T. marneffei infection were the positive culture of pathogens from sputum, blood, bone marrow, or other clinical specimens using the standard culture method. All data were obtained from the medical record system or telephonic follow-up after patients were diagnosed with T. marneffei infection, including demographic information, clinical manifestations, laboratory findings, imaging findings, pathological features, treatments, and survival outcomes. The study was approved by the Medical Ethics Committee of the First Affiliated Hospital of Guangxi Medical University (approval no. KY-E-2019-038; approval no. KY-E-2020-173) and conformed to the Declaration of Helsinki. Informed consent was obtained from all patients for the acquisition and use of clinical information and survival outcome.
Statistical Analysis
All statistical analyses were performed using R software (version 4.0.5, https://www.r-project.org/). A threshold of p < 0.05 was considered to be statistically significant. The primary endpoints were progression-free survival (PFS) and overall survival (OS). Disease progression was defined as severe opportunistic infections (e.g., T. marneffei reinfection, mycobacterium tuberculosis infection, or non-tuberculous mycobacterium infection, etc.) or death after antifungal treatment.
The baseline demographic and clinical characteristics were comprehensively evaluated and compared according to disease severity (with progression versus without progression) and survival outcome (survival versus death). The optimal cutoff value for continuous variables was calculated using the Maxstat algorithm [12]. Categorical variables were compared according to chi-squared test or Fisher’s exact test. PFS and OS were analyzed with the Kaplan–Meier method. Multivariate Cox analysis with the forward method was used to identify these independent prognostic factors for PFS and OS.
Subgroup Analysis
To explore whether HIV infection affected the prognosis of patients infected with T. marneffei, the entire population was classified into HIV-positive and HIV-negative groups to create the subgroup datasets. Additionally, we performed subgroup analysis to compare the differences between HIV-positive (n = 98) and HIV-negative (n = 143) subgroups. We also performed multivariate Cox analysis to identify these independent prognostic factors for patients in HIV-positive (n = 98) and HIV-negative (n = 143) subgroups, respectively.
Results
Patient Characteristics
As shown in Supplementary Fig. S1, 241 patients with confirmed T. marneffei infection between January 2012 and January 2022 were included in the study. The median follow-up time was 58.9 months. At the last follow-up, 120 patients experienced disease progression and 85 died. An overview of patient demographics and clinical characteristics is shown in Table 1. The median age was 49.0 (range 0.3–82.0) years, and the study population included 178 (73.9%) male and 63 (26.1%) female patients. Approximately seven-tenths (68.9%) of the patients lived in rural areas and one-third (34.9%) had a history of smoking. Underlying diseases were identified in 42 (17.4%) patients, including malignancies (n = 15), diabetes (n = 12), autoimmune diseases (n = 12), chronic kidney diseases (n = 2), and post-transplant (n = 1). Of these 241 patients, bone destruction occurred in 61 (25.3%), chest involvement in 229 (95.0%), lymph node enlargement in 194 (80.5%), and skin lesions in 141 (58.5%). More than half of the patients (53.9%) received oxygen therapy, and 18 (7.5%) were admitted to the intensive care unit (ICU).
Treatment Outcome
Progression-Free Survival
Of the 241 patients, 120 showed disease progression in the follow-up period. These patients suffered from severe opportunistic infections or death despite antifungal treatment. The most frequent opportunistic infections were T. marneffei reinfection, and non-tuberculous mycobacterium infection. Compared with patients in the disease-progression subgroup, those in the non-progression subgroup had a higher incidence of HIV coinfection (54.5% versus 26.7%, p < 0.01, Table 1) and a lower incidence of bone destruction (18.2% versus 32.5%, p = 0.02), underlying diseases (14.0% versus 20.8%, p = 0.22), oxygen therapy (40.5% versus 67.5%, p < 0.01), and admission to ICU (0.8% versus 14.2%, p < 0.01). As shown in Fig. 1A, Kaplan–Meier curve analysis revealed that the 1-year, 3-year, and 5-year PFS rates were 65.9% (95% CI 60.1–72.2%), 54.6% (95% CI 48.5–61.4%), and 47.8% (95% CI 41.5–55.1%), respectively. On the basis of the univariable Cox analysis (Supplementary Table S1), six candidate variables with a p-value < 0.05 were further entered into the multivariable Cox analysis, including hemoglobin, neutrophil count, prothrombin time, bone destruction, HIV coinfection, and underlying diseases. As shown in Fig. 2A, hemoglobin (HR 0.66, 95% CI 0.45–0.97; p = 0.04), prothrombin time (HR 1.78, 95% CI 1.13–2.80; p = 0.01), and HIV coinfection (HR 0.50, 95% CI 0.31–0.82; p < 0.01) remained the independent prognostic factors for PFS.
Overall Survival
Of 241 patients, 85 died in the follow-up period. Compared with the patients in the death subgroup, those in the survival subgroup had a higher incidence of combination antifungal therapy with amphotericin B (AMB) and triazoles (66.7% versus 43.5%, p < 0.01), and a lower incidence of underlying diseases (13.5% versus 24.7%, p = 0.04), oxygen therapy (44.2% versus 71.8%, p < 0.01), and admission to ICU (1.9% versus 17.6%, p < 0.01). As shown in Fig. 1B, Kaplan–Meier curve analysis revealed that the 1-year, 3-year, 5-year OS rates were 79.6% (95% CI 74.7–84.9%), 69.1% (95% CI 63.4–75.4%), and 61.4% (95% CI 55.0–68.6%), respectively. On the basis of the univariable Cox analysis (Supplementary Table S1), 11 candidate variables with a p-value < 0.05 were fitted into the multivariable Cox analysis, including residence, smoking history, hepatosplenomegaly, hemoglobin, neutrophil count, lymphocyte count, prothrombin time, underlying diseases, oxygen therapy, admission to ICU, and antifungal therapy. As shown in Fig. 2B, smoking history (HR 1.72, 95% CI 1.08–2.72; p = 0.02), hemoglobin (HR 0.48, 95% CI 0.29–0.80; p < 0.01), lymphocyte count (HR 0.48, 95% CI 0.24–0.95; p = 0.04), prothrombin time (HR 2.06, 95% CI 1.17–3.63; p = 0.01), oxygen therapy (HR 2.14, 95% CI 1.24–3.69; p < 0.01), and admission to ICU (HR 2.64, 95% CI 1.33–5.22; p < 0.01) remained independent prognostic factors for OS.
Subgroup Analysis
Patient Characteristics
Of the 241 patients, 98 (40.7%) had HIV coinfection during the follow-up period, the majority of whom were male (84.7%, Table 2). Among these patients, more than one-fifth (21.4%) were found to contract HIV infection before infection with T. marneffei, while most (78.6%) were found to be coinfected with T. marneffei when they were detected as HIV positive for the first time. Compared with patients in the HIV-positive subgroup, those in the HIV-negative subgroup were older (p < 0.01) and had a higher incidence of underlying diseases (25.9% versus 5.1%, p < 0.01), chest involvement (97.9% versus 90.8%, p = 0.03), bone destruction (42.0% versus 1.0%, p < 0.01), oxygen therapy (69.2% versus 31.6%, p < 0.01), and admission to ICU (11.9% versus 1.0%, p < 0.01). In terms of laboratory examinations, patients in the HIV-negative group had remarkedly higher levels of neutrophil count and lymphocyte count (all p < 0.01), whereas those in the HIV-positive group had a higher incidence of receiving combination antifungal therapy with AMB and triazoles (66.3% versus 53.1%, p = 0.01).
Treatment Outcome
HIV-Negative Group
Of the 241 patients, 143 (59.3%) were not infected with HIV. On the basis of Kaplan–Meier method, the 1-year, 3-year, and 5-year PFS rates were 57.8% (95% CI 50.2–66.5%), 43.1% (95% CI 35.4–52.5%), and 32.7% (95% CI 24.7–43.3%), respectively; the 1-year, 3-year, and 5-year OS rates were 79.6% (95% CI 73.3–86.5%), 66.5% (95% CI 58.8–75.1%), and 54.4% (95% CI 45.2–65.4%), respectively. Further multivariate analysis (Fig. 3) presented that hemoglobin (HR 0.62; 95% CI 0.39–1.00; p < 0.05), and lymphocyte count (HR 0.06; 95% CI 0.01–0.26; p < 0.01) were independent prognostic factors for PFS; hemoglobin (HR 0.45; 95% CI 0.22–0.89; p = 0.02), lymphocyte count (HR 0.08; 95% CI 0.01–0.40; p < 0.01), and admission to ICU (HR 2.80; 95% CI 1.31–5.99; p < 0.01) were independent prognostic factors for OS. The results of univariable Cox analysis are shown in Supplementary Table S2.
HIV-Positive Group
Of the 241 patients, 98 (40.7%) were infected with HIV. On the basis of Kaplan–Meier method, the 1-year, 3-year, and 5-year PFS rates were 77.6% (95% CI 69.7–86.3%), 69.1% (95% CI 60.5–79.0%), and 66.5% (95% CI 57.7–76.8%), respectively; the 1-year, 3-year, and 5-year OS rates were 79.6% (95% CI 72.0–88.0%), 71.2% (95% CI 62.7–80.8%), and 68.6% (95% CI 59.8–78.7%), respectively. Further multivariate analysis (Fig. 4) showed that lymphocyte count (HR 0.40; 95% CI 0.17–0.93; p = 0.03), prothrombin time (HR 6.28; 95% CI 2.39–16.50; p < 0.01), and combination antifungal therapy with AMB and triazoles (HR 0.27; 95% CI 0.12–0.64; p < 0.01) were independent prognostic factors for PFS; prothrombin time (HR 3.21; 95% CI 1.01–10.14; p < 0.05) and combination antifungal therapy with AMB and triazoles (HR 0.37; 95% CI 0.15–0.95; p = 0.04) were independent prognostic factors for OS. The results of univariable Cox analysis are shown in Supplementary Table S3.
Discussion
In this retrospective study, we analyzed the clinical characteristics, prognostic factors, and survival outcomes of patients infected with T. marneffei. The 5-year OS and PFS rates of overall population were 61.4% and 47.8%, respectively. Patients who were HIV positive and HIV negative have different clinical characteristics. Multiple organ involvement and disease progression are more common in patients who are HIV negative. Our findings would help clinicians diagnose and treat T. marneffei infection.
As an intracellular pathogen, T. marneffei infection in humans predominantly involves organs rich in monocytes/macrophages [6, 13], leading to localized and disseminated infection. After infection with T. marneffei, macrophages phagocytize the fungi and reproduce prolifically. The macrophages carry fungi that contribute to causing systemic disseminated infection via lymphatic and blood circulation, reaching lungs, lymph nodes, skin, liver, spleen, and bone marrow [14]. Consistent with the previous study [6], the common clinical features of infected patients were fever, anemia, bone marrow involvement, lymphadenopathy, skin lesions, hepatosplenomegaly, respiratory symptoms, and weight loss. Chest involvement exhibits varied imaging abnormalities, including pulmonary consolidations, cavities, atelectasis, interstitial infiltrates, pneumonectomies, pleural effusion, hydropericardium, and mediastinal lymphadenopathies. Due to lack of specific imaging manifestations, T. marneffei infection is easily misdiagnosed as tuberculosis, pulmonary cryptococcosis, aspergillosis, and malignant pulmonary tumors. As a result, many patients did not receive timely diagnosis and effective antifungal therapy at the early stage of the disease.
In our study, more than half (59.3%) of patients infected with T. marneffei were HIV negative. These patients had significantly higher neutrophil and lymphocyte counts than patients who were HIV positive. Similar to the finding of a retrospective study conducted in northern Thailand [15], we also found that patients who were HIV negative were older and more likely to have chest involvement, underlying diseases, and bone destruction, indicating more organ damage. Notably, the incidence of bone destruction apparently increases in patients who are HIV negative (60% versus 1%, p < 0.01). We found that bone destruction often occurred in the ribs, skull, spine, ilium, and humerus. Patients with bone destruction are often accompanied by bone pain, and have a much higher risk of occurring fractures. Kudeken et al. [16, 17] found that bone destruction could be caused by leukocyte hydrolase released in the lesion, and was closely correlated with a potent autoimmune response induced by leukocytes. The deficient number and abnormal function of leukocytes may explain why bone destruction is less likely to occur in patients who are HIV positive [18]. T. marneffei infection with bone destruction often results in more severe conditions and a higher relapse rate. Therefore, these patients should receive prolonged antifungal therapy, together with periodic surveillance for routine blood examination and bone imaging [19].
In our study, the 5-year OS rates of overall population and patients who were HIV negative and HIV positive were 61.4%, 54.4%, and 68.6%, respectively. In other research involving 116 patients who were HIV positive and 34 patients who were HIV negative in Northern Thailand, mortality was 20.7% and 29.4%, respectively [15]. These data showed that patients infected with T. marneffei have a poor prognosis. For patients with AIDS, the reduction and dysfunction of CD4+ T lymphocyte (CD4) contributes to the development of a variety of infections, particularly tuberculosis, Cryptococcus spp., and disseminated T. marneffei infection [7]. Currently, using powerful antiretroviral therapy for patients with AIDS, as well as receiving anti-infection treatment if they experience severely opportunistic infection, can remarkably increase long-term survival and improve prognosis. Patients who are HIV negative are more likely to be misdiagnosed and receive inappropriate treatment because the early clinical symptoms are atypical. Additionally, patients who are HIV negative tend to be complicated, with underlying diseases such as neoplasms, rheumatic diseases, and other immunodeficiency diseases. Qiu et al. have proved that patients who are HIV negative with underlying diseases had a significantly higher mortality (44.4% versus 12.0%) than those without underlying diseases [20]. These reasons may explain why patients who are HIV negative have a worse prognosis.
Current studies showed that adult-onset acquired immunodeficiency mediated by anti-IFN-γ autoantibodies (AIGAs) had a strong association with T. marneffei infection in patients who are HIV negative [21,22,23]. Infected patients are more prone to suffering from relapse, disseminated opportunistic infections, or severe infection resulting from multiple intracellular pathogens, particularly non-tuberculous mycobacterium infection, varicella zoster virus, and mycobacterium tuberculosis [3, 24, 25], leading to accelerated disease progression. In this study, we also found that patients who were HIV negative had significantly lower 5-year PFS rate (32.7% versus 66.5%) than patients who were HIV positive, which indicated that patients who were HIV negative were more likely to experience disease progression. The potential reason may be related to AIGAs. Currently, the underlying mechanism of AIGAs in patients who are HIV negative have rarely been reported. Therefore, our research group has conducted an ongoing study on this topic. At present, 44 patients with T. marneffei infection who are HIV negative have been tested for anti-IFN gamma autoantibodies in plasma used by enzyme-linked immunosorbent assays. Among these patients, 31 (70.5%) were positive for anti-IFN-γ autoantibodies.
AMB and triazoles are considered the mainstay therapies for talaromycosis. Some reports recommend intravenous AMB (0.7–1 mg/kg daily for 2 weeks) as induction therapy for talaromycosis, followed by oral itraconazole (400 mg/day) for 10 weeks [26, 27]. Several studies have proven that AMB has good clinical effect for treatment of T. marneffei infection. In 2017, a multicenter randomized controlled trial in Vietnam showed that induction treatment with AMB was associated with significantly faster fungal clearance and lower rates of relapse and immune reconstitution inflammatory syndrome than itraconazole [28]. As induction therapy for talaromycosis, AMB was superior to itraconazole, with significantly lower 6-month mortality (11.3% versus 21.0%) [28]. A retrospective study performed in Guangdong (2011–2017) showed that triazole monotherapy in the treatment of T. marneffei independently predicted a poor prognosis [29]. In this study, we also found that patients who had ever been treated with AMB in the long-term course of triazole antifungals had a lower risk of death (HR 0.37, p = 0.04) and disease progression (HR 0.27, p < 0.01) than triazole monotherapy for those patients who were HIV positive. Despite the survival benefit, the adverse effects of AMB (e.g., renal failure and hematologic and infusion-related toxic effects) should be considered in some patients. Close monitoring is required in patients receiving AMB therapy.
There are several limitations in this study. First, it is a retrospective study, and some important laboratory examinations were not performed in patients who were HIV negative previously due to lack of understanding of T. marneffei infection, such CD4 count, so we cannot compare the data between groups. Second, the relatively small number of patients may cause a selection bias to a certain extent. Moreover, this was a single-center cohort study; more extrapolating studies are needed for other endemic areas in China.
Conclusions
T. marneffei infection in patients has the potential to cause systemic involvement with high mortality. The clinical manifestations differ between patients who are HIV positive and HIV negative. Our study may provide a better understanding of T. marneffei infection for clinicians.
References
Cao C, Xi L, Chaturvedi V. Talaromycosis (penicilliosis) due to Talaromyces (Penicillium) marneffei: insights into the clinical trends of a major fungal disease 60 years after the discovery of the pathogen. Mycopathologia. 2019;184(6):709–20.
Li Y, Luo H, Fan J, et al. Genomic analysis provides insights into the transmission and pathogenicity of Talaromyces marneffei. Fungal Genet Biol. 2019;130:54–61.
Guo J, Ning XQ, Ding JY, et al. Anti-IFN-gamma autoantibodies underlie disseminated Talaromyces marneffei infections. J Exp Med. 2020;217(12).
Pan M, Qiu Y, Zeng W, Tang S, Wei X, Zhang J. Disseminated Talaromyces marneffei infection presenting as multiple intestinal perforations and diffuse hepatic granulomatous inflammation in an infant with STAT3 mutation: a case report. BMC Infect Dis. 2020;20(1):394.
Ding X, Huang H, Zhong L, et al. Disseminated Talaromyces marneffei infection in a non-HIV infant with a homozygous private variant of RELB. Front Cell Infect Microbiol. 2021;11: 605589.
Vanittanakom N, Cooper CR Jr, Fisher MC, Sirisanthana T. Penicillium marneffei infection and recent advances in the epidemiology and molecular biology aspects. Clin Microbiol Rev. 2006;19(1):95–110.
Supparatpinyo K, Khamwan C, Baosoung V, Nelson KE, Sirisanthana T. Disseminated Penicillium marneffei infection in southeast Asia. Lancet. 1994;344(8915):110–3.
Pongpom M, Vanittanakom P, Nimmanee P, Cooper Jr CR, Vanittanakom N. Adaptation to macrophage killing by Talaromyces marneffei. Future Sci OA. 2017;3(3):FSO215.
Chen M, Houbraken J, Pan W, et al. Pulmonary fungus ball caused by Penicillium capsulatum in a patient with type 2 diabetes: a case report. BMC Infect Dis. 2013;13:496.
Ye F, Luo Q, Zhou Y, et al. Disseminated Penicilliosis marneffei in immunocompetent patients: a report of two cases. Indian J Med Microbiol. 2015;33(1):161–5.
Chan JF, Lau SK, Yuen KY, Woo PC. Talaromyces (Penicillium) marneffei infection in non-HIV-infected patients. Emerg Microbes Infect. 2016;5: e19.
Xu G, Jiang L, Ye C, et al. The ratio of CD86+/CD163+ macrophages predicts postoperative recurrence in stage II–III colorectal cancer. Front Immunol. 2021;12: 724429.
Youngchim S, Vanittanakom N, Hamilton AJ. Analysis of the enzymatic activity of mycelial and yeast phases of Penicillium marneffei. Med Mycol. 1999;37(6):445–50.
Zeng W, Qiu Y, Lu D, Zhang J, Zhong X, Liu G. A retrospective analysis of 7 human immunodeficiency virus-negative infants infected by Penicillium marneffei. Medicine (Baltimore). 2015;94(34): e1439.
Kawila R, Chaiwarith R, Supparatpinyo K. Clinical and laboratory characteristics of penicilliosis marneffei among patients with and without HIV infection in Northern Thailand: a retrospective study. BMC Infect Dis. 2013;13:464.
Kudeken N, Kawakami K, Saito A. Cytokine-induced fungicidal activity of human polymorphonuclear leukocytes against Penicillium marneffei. FEMS Immunol Med Microbiol. 1999;26(2):115–24.
Kudeken N, Kawakami K, Saito A. Mechanisms of the in vitro fungicidal effects of human neutrophils against Penicillium marneffei induced by granulocyte-macrophage colony-stimulating factor (GM-CSF). Clin Exp Immunol. 2000;119(3):472–8.
Wei HY, Liang WJ, Li B, et al. Clinical characteristics and risk factors of Talaromyces marneffei infection in human immunodeficiency virus-negative patients: a retrospective observational study. World J Emerg Med. 2021;12(4):281–6.
Liang X, Si L, Li Y, et al. Talaromyces marneffei infection relapse presenting as osteolytic destruction followed by suspected nontuberculous mycobacterium infection during 6 years of follow-up: a case update. Int J Infect Dis. 2020;93:208–10.
Qiu Y, Liao H, Zhang J, Zhong X, Tan C, Lu D. Differences in clinical characteristics and prognosis of Penicilliosis among HIV-negative patients with or without underlying disease in Southern China: a retrospective study. BMC Infect Dis. 2015;15:525.
Su SS, Zhang SN, Ye JR, et al. Disseminated Talaromyces marneffei and mycobacterium avium infection accompanied sweet’s syndrome in a patient with anti-interferon-gamma autoantibodies: a case report. Infect Drug Resist. 2019;12:3189–95.
Chen ZM, Li ZT, Li SQ, et al. Clinical findings of Talaromyces marneffei infection among patients with anti-interferon-gamma immunodeficiency: a prospective cohort study. BMC Infect Dis. 2021;21(1):587.
Shi N, Kong J, Wang K, Cao C. Coinfection with Talaromyces marneffei and other pathogens associated with acquired immunodeficiency. JAMA Dermatol. 2019;155(10):1195–7.
Zeng W, Qiu Y, Tang S, Zhang J, Pan M, Zhong X. Characterization of anti-interferon-gamma antibodies in HIV-negative patients infected with disseminated Talaromyces marneffei and cryptococcosis. Open Forum Infect Dis. 2019;6(10):ofz208.
Hoflich C, Sabat R, Rosseau S, et al. Naturally occurring anti-IFN-gamma autoantibody and severe infections with Mycobacterium cheloneae and Burkholderia cocovenenans. Blood. 2004;103(2):673–5.
Kaplan JE, Benson C, Holmes KK, et al. Guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. MMWR Recomm Rep. 2009;58(RR-4):1–207 (quiz CE1–4).
Nelson M, Dockrell D, Edwards S, et al. British HIV Association and British Infection Association guidelines for the treatment of opportunistic infection in HIV-seropositive individuals 2011. HIV Med. 2011;12(Suppl 2):1–140.
Le T, Kinh NV, Cuc NTK, et al. A trial of itraconazole or amphotericin B for HIV-associated talaromycosis. N Engl J Med. 2017;376(24):2329–40.
Ying RS, Le T, Cai WP, et al. Clinical epidemiology and outcome of HIV-associated talaromycosis in Guangdong, China, during 2011–2017. HIV Med. 2020;21(11):729–38.
Acknowledgements
Funding
This work was supported by Education Department of Guangxi Zhuang Autonomous Region (no. 02304001023C) and Guangxi Zhuang Region Health Committee (G202002002). The funding source had no role in the design of this study and will not have any role during its execution, analyses, interpretation of the data, or decision to submit results. The journal’s Rapid Service Fee has been funded by the authors.
Author Contributions
Zhiyi He and Xiaokai Feng designed the study and had the full responsibility for the facticity of data. Xiaona Liang, Siqiao Liang, Nan Ma, Siyao Wu and Yan Ning collected clinical data and contributed to following up patients. QingLiang Yu, Meifang Wei and Rong Xiao performed the statistical analyses and contributed to writing of the manuscript. Jingmin Deng, Meiling Yang, Quanfang Chen, Wen Zeng, Meihua Li, Xiaokai Feng, Zhiyi He revised the manuscript. All authors read and approved the final manuscript.
Disclosures
QingLiang Yu, Meifang Wei, Rong Xiao, Xiaona Liang, Siqiao Liang, Nan Ma, Siyao Wu, Yan Ning, Jingmin Deng, Meiling Yang, Quanfang Chen, Wen Zeng, Meihua Li, Xiaokai Feng, and Zhiyi He have nothing to disclose.
Compliance with Ethics Guidelines
This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. All subjects were provided informed consent to participate in the study. The study was approved by the Medical Ethics Committee of the First Affiliated Hospital of Guangxi Medical University (approval no. KY-E-2019-038; approval no. KY-E-2020-173).
Data Availability
The information has not previously been presented at any meetings. The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Yu, Q., Wei, M., Xiao, R. et al. Clinical Characteristics, Course, and Long-Term Outcomes in Patients with Talaromyces marneffei Infection: A 10-Year Retrospective Cohort Study. Infect Dis Ther 12, 1283–1297 (2023). https://doi.org/10.1007/s40121-023-00801-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-023-00801-5