Abstract
Introduction
Molnupiravir is an oral antiviral drug that received special approval for emergency use in Japan on December 24 2021 for infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). This post-marketing surveillance (PMS) is underway to investigate the safety and effectiveness of molnupiravir in daily clinical practice in Japan. The interim PMS data collected from December 27 2021 to June 15 2022 are reported in this publication.
Methods
This survey included adult Japanese patients treated with molnupiravir. For safety, adverse drug reactions (ADR) were assessed by physicians. Effectiveness was assessed by the composite endpoint of (1) hospitalization or (2) death in outpatients and by the composite endpoint of (3) death or (4) initiation of oxygen administration/mechanical ventilation in inpatients hospitalized for any reasons and without oxygen administration at the start of molnupiravir administration. The observation period was through 29 days from the start of molnupiravir administration.
Results
Of the 1031 patients in the safety analysis set, 68 (6.60%) patients reported ADRs and four (0.39%) patients reported serious ADRs. The main ADRs observed were diarrhoea [26 patients (2.52%)], rash [six patients (0.58%)], dizziness [five patients (0.48%)], and faeces soft [four patients (0.39%)]. In the effectiveness analysis from the start date of molnupiravir administration to day 29, there were 16/612 (2.61%) hospitalizations and no deaths. Oxygen administration was newly initiated in 9/199 (4.52%) inpatients after the initiation of molnupiravir administration; 2/199 (1.01%) inpatients died.
Conclusion
This interim analysis of molnupiravir in daily clinical practice use in Japan supports the safety and effectiveness profile of molnupiravir under pandemic conditions in which Omicron was the dominant SARS-CoV-2 variant. The results of this PMS will provide valuable information for daily clinical practice use.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why this survey was conducted? |
Molnupiravir is an oral antiviral drug that received special approval for emergency use in 2021, for infectious disease caused by SARS-CoV-2. |
This PMS was conducted to obtain data regarding the safety and effectiveness of molnupiravir in Japanese patients, obtained under clinical practice. |
What was learned from the survey? |
This interim analysis is the first report of the safety and effectiveness of molnupiravir in over 1000 patients, reflecting a real-world setting in Japan, and is significant in that it provides detailed large-scale information on the background of patients prescribed molnupiravir in Japan, the actual administration status, safety, and to a limited extent, effectiveness. |
This analysis of molnupiravir in daily clinical practice use in Japan supports the safety and effectiveness profile of molnupiravir in treating COVID-19, under pandemic conditions in which Omicron was the dominant SARS-CoV-2 variant. |
Introduction
In mid-2021, several COVID-19 treatments for patients with mild-to-moderate disease were available, such as remdesivir and monoclonal antibodies. There are, however, potential difficulties associated with both of these treatment categories. The continued efficacy of monoclonal antibodies remains a challenge due to mutations in the viral spike protein, leading to a loss of efficacy. Additionally, there are also difficulties associated with administering intravenous antiviral drugs on continuous days in outpatient settings. As many COVID-19 patients are being treated as outpatients there was, therefore, a strong need to develop COVID-19 treatments that could be administered orally. As such nirmatrelvir/ritonavir received special approval as an oral antiviral drug, in February of the following year, thereby increasing patient options. Nirmatrelvir/ritonavir is a drug combination that shows a good efficacy profile, despite having drug–drug interaction limitations [1]. In these circumstances, capsule formulation molnupiravir (LAGEVRIO®) was developed and received special approval for emergency use on December 24 2021 in Japan [2].
Molnupiravir is a small-molecule ribonucleoside pro-drug of N-hydroxycytidine (NHC), which has activity against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and other RNA viruses, and a high resistance to the development of resistance [2,3,4,5,6,7,8,9]. Also, similar antiviral effects have been observed against the SARS-CoV-2 variant strains of concern in vitro [10], including Omicron evaluated in a clinical trial [11]. In Japan, the indication for molnupiravir use is “infectious disease caused by SARS-CoV-2” [2].
Administration of molnupiravir does not require dose adjustment in patients with renal or hepatic impairment. In vitro studies indicate that molnupiravir and NHC are not substrates, inhibitors, or inducers of CYP3A4 enzymes [2], and it is not, therefore, expected that molnupiravir will have drug–drug interactions. Also, in vivo preclinical studies indicate that molnupiravir is not mutagenic or genotoxic in mammalian systems [2].
The efficacy and safety of molnupiravir were investigated in the phase III part of the global MOVe-OUT study in outpatients with mild-to-moderate COVID-19 who were at risk for severe disease, at a dose of 800 mg twice daily for 5 days [12]. The results showed that molnupiravir significantly reduced the rate of hospitalization or death compared with the placebo group. The most common adverse drug reactions (ADRs) to molnupiravir (incidence ≥ 1%) reported were diarrhea, nausea, and dizziness. These results should be placed in the context that the MOVe-OUT study was conducted before the emergence of the Omicron SARS-CoV-2 strain. The MOVe-OUT study had eligibility criteria for enrollment, including unvaccinated patients with increasing risk(s) of severe illness and cases within 5 days from onset of COVID-19. Overall, there is a lack of data in a large number of Japanese patients regarding the safety and efficacy of molnupiravir.
It is of urgent importance to obtain data regarding effectiveness and safety in Japanese patients, obtained under Japanese clinical practice. This post-marketing surveillance (PMS) is the first large-scale survey (more than 1000 patients) to investigate molnupiravir in a real-world setting conducted at medical institutions in Japan.
Methods
Patient Population
This PMS was initiated on December 27 2021 and it is planned to enroll 3000 patients with “infection caused by SARS-CoV-2” that are treated with molnupiravir, in principle within 5 days of COVID-19 diagnosis, in the 3-year period to December 2024. This interim analysis includes data collected from December 27 2021 to June 15 2022 at 151 enrolled medical institutions. Of the enrolled medical institutions, survey forms were collected from 120 institutions. This paper only contains data on patients from whom informed consent was obtained.
In this survey, it was planned to enroll a population of Japanese patients with “infection caused by SARS-CoV-2,” with risk factors for illness progression. These risk factors included age ≥ 65 years, malignant tumor, chronic obstructive pulmonary disease (COPD), chronic kidney disease, type 2 diabetes mellitus, hypertension, dyslipidemia, immunodeficiency after solid-organ transplantation, obesity [body mass index (BMI) ≥ 30 kg/m2], smoking, and others. Patients were enrolled regardless of outpatient or inpatient status, vaccination status, or history of medical complications. The inpatient population included cases of onset during hospitalization for reasons other than COVID-19 infection; and cases hospitalized for COVID-19 isolation, treatment, etc. Some patients were classified as others and included nursing home residents and patients receiving home-visit medical care, etc. In principle, patients were administered molnupiravir within 5 days of SARS-CoV-2 infection. Data was collected in a single-arm observational design by the continuous registration method. To reduce selection bias, patients who received molnupiravir were consecutively enrolled without selecting cases, and as such did include patients without risk factors for disease progression. The observation period was through 29 days from the start of molnupiravir administration.
Compliance with Ethics Guidelines
This PMS was conducted in accordance with the Ministry of Health, Labour, and Welfare (MHLW) ordinance for Good Post-marketing Study Practice (GPSP). The survey protocol was approved by the Pharmaceuticals and Medical Devices Agency (PMDA). Additionally, this survey was conducted in accordance with the protocol; the Helsinki Declaration of 1964, and its later amendments; and all other applicable regulations. Institutional review board (IRB) approval was not mandatory for this survey according to the GPSP.
The physician in charge of the survey explained to the patient or his/her legally acceptable representative the objective of the survey, the information to be collected through the survey, and the uses of the survey results, and obtained informed consent from the patient or his/her legally acceptable representative.
Data Collection and Assessment
Safety Assessments
All reported adverse events (AEs) were collected through the observation period. ADRs were defined as AEs for which the causal relationship to molnupiravir could not be ruled out by an attending physician. These ADRs were classified according to the Medical Dictionary for Regulatory Activities/Japanese version [MedDRA/J version (25.0)]. Additionally, the survey physicians assessed all ADRs for seriousness.
Additionally, patient background characteristics were captured. Information on concomitant treatments were collected from the same day as molnupiravir administration and continued thereafter. The severity of COVID-19 and risk factors for severe COVID-19 illness in this survey were reported by the physicians with reference to the “Clinical Management of Patients with COVID-19” [13] (Supplementary Material: Table S1).
Effectiveness Assessments
Due to the different backgrounds of outpatients, inpatients without oxygen or mechanical ventilation at the start of molnupiravir administration, and patients classified as others, the analysis focused on the number and frequency of events of composite effectiveness endpoints experienced by inpatients and outpatients only, during the observation period assessed according to the following definitions:
Outpatient endpoint: hospitalization (i.e., for reasons other than pre-planned admission prior to the start of molnupiravir, such as isolation and hospitalization for examination) or death through 29 days from the start of molnupiravir administration.
Inpatient endpoint: patients that were not receiving oxygen or mechanical ventilation [including extracorporeal membrane oxygenation (ECMO)] at the start of molnupiravir administration that required the initiation of oxygen/mechanical ventilation or died through the 29 day observation period from the start of administration.
Statistical Analysis
The safety analysis set included all patients for whom the survey form was collected, and excluded patients that were not administrated molnupiravir.
The effectiveness analysis set included all patients in the safety analysis set and excluded the following patients: outside the dosage and administration instructions, and effectiveness not evaluable due to loss to follow-up, etc.
Descriptive statistics were summarized for continuous variables. Kaplan–Meier plots were used to describe the effectiveness endpoints. All statistical tests were calculated using SAS Release 9.4 (SAS Institute, Inc., Cary, NC, USA) and considered statistically significant at P < 0.05.
Results
Patient Disposition
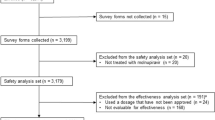
As shown in Fig. 1, of 1236 enrolled patients, a total of 1031 patients were included in the safety analysis set [case report forms (CRFs) were not collected from 202 patients; and three patients were excluded from the safety analysis set as molnupiravir was not administered]. Whilst in principle, patients were administered molnupiravir within 5 days of SARS-CoV-2 infection, 41 patients (3.98%) were enrolled 6 days or more after infection.
Of the 1031 patients included in the safety analysis, 884 patients were included in the effectiveness analysis set, and 147 patients were excluded for the following reasons: outside the dosage and administration instructions in 18 patients, effectiveness not evaluable in 133 patients, and four patients were excluded as they met both exclusion criteria.
Patient Characteristics
As shown in Fig. 2 and Table 1 the safety analysis set comprised predominantly older aged patients. The median age of patients was 68.0 years (range: 18–107 years) [Table 1]: 57.23% of the population was ≥ 65 years and 45.30% were aged 70 years or older (Fig. 2). As presented in Table 1, 53.06% of patients were male.
In the safety analysis set, 689 (66.83%) were outpatients, 294 (28.52%) were inpatients, and 48 (4.66%) were other patients.
The reason for the use of the molnupiravir, in all 1031 patients, was infection due to SARS-CoV-2 as judged by a physician, and most patients had COVID-19 symptoms at the start of treatment (97.28%).
At the start of administration of the drug, 862 (83.61%) patients had received at least one vaccine dose against SARS-CoV-2, and 657 (63.72%) patients were vaccinated twice.
The severity of COVID-19, before molnupiravir treatment based on the clinical management of patients with COVID-19 (Supplementary material: Table S1) was mild in 87.88%, moderate I in 9.60%, and moderate II in 2.23% of the patients.
At the start of molnupiravir treatment (Table 2), 96.80% patients had risk factors for severe COVID-19 illness. The most frequent risk factor for progression to severe COVID-19 (Table 2) was “elderly ≥ 65 years,” which was recorded in 590 patients (57.23%). The second most observed risk factor was hypertension, followed by smoking. Three hundred twenty-three (31.33%) patients had one risk factor; 330 (32.01%) patients had two risk factors, 210 (20.37%) patients had three risk factors, 93 (9.02%) patients had four risk factors, and 42 (4.07%) patients had five risk factors or more. In the analysis populations, however, 33 (3.20%) patients without such risk factors were also included.
At the start of molnupiravir treatment (Table 1), 863 patients (83.71%) had comorbidities (including diseases with risk factor for severe COVID-19 illness) and 153 patients (14.84%) had no underlying comorbid diseases. The most common comorbidities were hypertension (45.00%), type 2 diabetes mellitus/diabetes mellitus (22.31%), and dyslipidemia (20.17%).
Regarding treatment practice, molnupiravir was started at a median of 1–2 days from COVID-19 symptom onset. For most patients (93.11%), molnupiravir was started within 5 days. For approximately half of the patients (50.53%), molnupiravir was started 1–2 days from the symptom onset. The median time from positive SARS-CoV-2 virus test results to molnupiravir administration was 1 day (range: 1–9 days). After molnupiravir treatment started, 96.61% of patients completed treatment.
Safety
Of 1031 patients in the safety analysis population, the frequency of ADRs was 78 events in 68 patients (6.60%). A list of all ADRs observed in this survey is presented in Table S2 (Supplementary Material). Among the ADRs that occurred, four events in four patients (0.39%) were serious ADRs. Furthermore, the ADR rate observed in patients aged 65 years and above was 5.25% (31/590).
ADRs that occurred in three or more patients were diarrhoea in 26 patients (2.52%), rash in six patients (0.58%), dizziness in five patients (0.48%), faeces soft in four patients (0.39%), and vomiting and headache in three patients each (0.29%) (Table 3).
Most ADRs occurred soon after molnupiravir administration, and 34 ADRs were observed in 32 patients, 1–2 days after the start of administration.
A total of 35 patients (3.39%) in the safety analysis set discontinued molnupiravir administration. Twenty-one patients discontinued molnupiravir due to the onset of AEs, two patients discontinued administration due to lack of effectiveness, and 12 patients for other reasons (patient request, patient lost to follow-up, etc.). Among the 21 patients that discontinued the administration due to AEs, a total of 16 patients experienced 19 ADRs. The ADRs that led to discontinuations were as follows: diarrhea (four cases), rash (three cases), vomiting (two cases), drug eruption (two cases), and other events (one case each).
ADRs were assessed by physicians and serious ADRs were observed in four patients (four events) including rash, hepatic function abnormality, COVID-19 (aggravation), and interstitial pneumonia (aggravation) observed in one patient each.
There were seven deaths (Table 4) [no outpatients, three inpatients (one with and two without oxygen or mechanical ventilation at the start of molnupiravir administration), and four other patients in nursing homes, etc.]. The causal relationships of all deaths were judged by physicians not to be related to molnupiravir. Six of the recorded deaths were observed in patients aged 80 years or greater, and the age of one patient that died was unknown. All cases of death had risk factors for severe COVID-19 illness. The causes of death were as follows: COVID-19 (including complications related to COVID-19 and death due to associated symptom) in three patients; and urinary tract infection/sepsis, diabetic ketoacidosis, senescence, and unknown (with comorbidities of chronic kidney disease and high blood pressure, and a recorded AE term of respiratory disorder) in one patient each.
Effectiveness
Of the 1031 patients included in the safety analysis, 884 patients were included in the effectiveness analysis set. Among these, 612 (69.23%) were outpatients, 227 (25.68%) were inpatients, and 45 (5.09%) were classified as other. In the effectiveness analysis set, outpatients (612 patients, 69.23%) and inpatients without oxygen or mechanical ventilation at the start of molnupiravir administration (199 patients, 22.51%) were assessed for the frequency of the composite effectiveness endpoint (hospitalization or death, and initiation of oxygen/mechanical ventilation or death, respectively).
Among outpatients, 16/612 patients (2.61%) were hospitalized, for all causes, through 29 days from the start of administration (Fig. 3a). As presented in Table 5, among outpatients 12/16 were over 60 years old; 14/16 patients had presence of comorbidities including risk factors for severe COVID-19 illness; 10/13 (missing data for three patients) patients had received concomitant medications for COVID-19; and 16/16 had risk factors for severe COVID-19 illness. Twelve of the 16 patients (1.96%) had COVID-19-related hospitalization, and no deaths were reported in outpatients.
Frequency of effectiveness endpoints through 29 days after the start of molnupiravir administration. a Hospitalization or death in the outpatients at the start of molnupiravir administration and b death, start of oxygen administration, or mechanical ventilation (including ECMO) through 29 days after the start of molnupiravir administration in inpatients without oxygen administration at the start of molnupiravir administration. The inset displays the same data on an enlarged vertical axis. CI confidence interval, ECMO extracorporeal membrane oxygenation
Among inpatients (without oxygen at start of molnupiravir administration), 9/199 patients (4.52%) started oxygen administration through 29 days from the start of administration (Fig. 3b). No patient was placed on mechanical ventilation (including ECMO). Two inpatients died [2/199 (1.01%)] within 29 days from the start of administration. For inpatients the composite endpoint [death, start of oxygen, or mechanical ventilation (including ECMO)] frequency was 5.03%.
The use of oxygen administration in the effectiveness analysis set is presented in Table S3 (Supplementary Material). Of the 884 patients in the effectiveness analysis set, 12 patients (1.36%) initiated oxygen therapy after molnupiravir administration, including nine inpatients, one outpatient, and two other categorized patients. The median volume of oxygen supply was 2 L/min (range: 1–15 L/min) in ten patients, which excludes two patients who had unknown oxygen supply volumes. A total of 15 L/min of oxygen mask with reservoir was supplied to the fatal case with urinary tract infection/sepsis.
The frequency of all-cause death was 0.79% (7/884) in the effectiveness analysis population, and the frequency of death caused by COVID-19 was 0.34% (3/884).
In the effectiveness analysis set, 84.05% had comorbidities and the vaccination rate was 83.37%. Additionally, as characteristic of the aging Japanese population, 65.16% of the analysis set were aged 60 years or older, and a further 43.44% of patients were aged 70 years or older.
Discussion
Principal Findings
This interim analysis is the first report of the safety and effectiveness of molnupiravir in over 1000 patients, reflecting a real-world setting in Japan. It is significant in that it provides detailed large-scale information on the background of patients prescribed molnupiravir in Japan, as well as the actual administration status, safety, and to a limited extent, effectiveness.
This PMS included approximately 84% of patients who had comorbidities, 84% who were vaccinated, and 45% aged 70 years or older, reflecting the aging society of Japan. As defined in large-scale surveys, age and comorbidities were reported to increase the probability of developing severe COVID-19 illness [14]. Older people generally have multiple age-related comorbidities, and such patients are expected to be at a high risk of developing severe COVID-19 illness.
This survey was conducted while Omicron was the dominant SARS-CoV-2 variant, and as vaccine availability was widespread, the majority of the survey population had been vaccinated. In the period when Omicron was the dominant SARS-CoV-2 variant compared with the period when Delta was dominant, the Government Advisory Board data [15] suggested a decrease in deaths due to respiratory failure caused by severe COVID-19 pneumonia. Additionally in the periods January–February 2022 and March–April 2022, during the time period that data was collected in this PMS, the MHLW reported [16, 17] in certain prefectures of Japan that the death rate was higher in older age patients. In these data, regardless of inpatient or outpatient status, the death rate was 0.01% in patients aged 50 years or younger and 1.99% in patients aged over 60 years (January–February 2022); and 0.01% in patients aged 50 years or younger, and 1.13% in those aged over 60 years (March–April 2022). Additionally, by age group, the death rates (%) were 0.29/0.10, 1.23/0.94, 3.67/2.67, and 6.21/4.05 (January–February/March–April) in patients aged in their 60s, 70s, 80s, or 90s or over, respectively. This demonstrates the importance of focusing on the care of older age patients and patients with comorbidities.
Considering the high proportion of patients aged 65 years or greater in the survey population, the low number of deaths is particularly noteworthy. Seven deaths [0.79% (7/884)] were observed, which were all unrelated to molnupiravir, as presented in Table 4.
In the safety analysis set, the frequency of reported ADRs was low. Additionally, molnupiravir was well tolerated by patients aged 65 years and older. While the types of ADRs to molnupiravir observed in this survey are similar to those in the phase III MOVe-OUT randomized clinical trial (RCT) (diarrhoea, nausea, dizziness, etc.) the incidences of these ADRs were lower (apart from diarrhea) than in the MOVe-OUT study [12].
Regarding treatment adherence, after molnupiravir treatment started, 96.61% of patients completed treatment, suggesting that there are minimal barriers for patients to complete administration of the treatment formulation and that molnupiravir was well tolerated.
Among outpatients in the effectiveness analysis set, a small percentage of patients (2.61%) were hospitalized, and no deaths were reported. These results support the effectiveness of molnupiravir in this survey. Whilst not directly comparable, the efficacy of molnupiravir was reported in the MOVe-OUT RCT (molnupiravir administered to outpatients with mild or moderate COVID-19 symptoms), in which 7.3% of patients were hospitalized or died through 29 days.
Additionally, recent data has been reported from several real-world clinical studies conducted in various countries including Japan [18][Suzuki et al.], Hong Kong [19], Israel [20] [Arbel et al. preprint], Italy [21], and a clinical trial in the UK [22] [Butler et al.]. In common with our PMS, many of these studies were retrospective cohort studies that included vaccinated patients with mild and moderate disease, and were conducted when the predominant SARS-CoV-2 viral strain was Omicron. Wong et al. reported that in an outpatient population during the Omicron wave, the crude incidence rate of all-cause mortality was 4.2 per 100,000 person-days lower in the molnupiravir group (17.9) compared with matched controls (22.1) [19]. Arbel et al. reported that in high-risk outpatients infected when the Omicron SARS-CoV-2 viral strain was predominant, individuals aged 65 years and older treated with molnupiravir experienced a significant reduction in hospitalization and mortality [20] [Arbel et al. preprint]. The present results cannot be directly compared with these previous studies, as the characteristics of patients included in our PMS and the conditions of molnupiravir use differ from the clinical trial and overseas real-world clinical studies; however, evidence supporting the safety and effectiveness of molnupiravir is increasing.
The UK-based PANORAMIC study was a national, multigroup, prospective, platform adaptive randomized clinical study. In the two arms of this study, usual care and 800 mg molnupiravir was administered twice daily for 5 days, or usual care only was provided. In the preliminary report of the PANORAMIC study, Butler et al. [22] presented secondary endpoint results of time-to-first-recovery (patient-reported outcomes), in addition to the primary endpoint results of death and hospitalization. The patient-reported outcomes and symptom data will be important in assessing the clinical effectiveness of molnupiravir in the future.
Limitations
There are some limitations to be considered. This survey is not a RCT and has no control group, and therefore, the results cannot compare the safety or effectiveness outcomes with those who did not receive any treatment.
In general, conducting long-term examinations in outpatients is difficult due to the high rate of loss to follow-up. In this context, investigating patient follow-up using the continuous registration method implemented in this survey provides extremely important safety and effectiveness data on patients that have been prescribed therapeutics, despite the fact that there is no control group as in randomized clinical trials. In the effectiveness analysis set, approximately 15% of patients were lost to follow up; however, in this survey, follow-up was limited because this was a noninterventional observational survey in an outpatient setting under conditions of real-world clinical use.
The number of sites that participated in this survey is limited compared with the number of sites in Japan, and there are, therefore, limitations in the evaluation of these results.
Finally, as SARS-CoV-2 strains transition sequentially from prevalent strains at the time of the survey, the results of this survey should be interpreted from the viewpoint that during this survey Omicron was the main SARS-CoV-2 variant.
Conclusion
This interim analysis of molnupiravir in daily clinical practice use in Japan supports the safety and effectiveness profile of molnupiravir under pandemic conditions in which Omicron was the dominant SARS-CoV-2 variant.
References
Pfizer Japan Inc. Paxlovid package insert (Japanese). https://www.pmda.go.jp/PmdaSearch/iyakuDetail/ResultDataSetPDF/672212_62501B5X1020_1_05. Accessed Mar 9, 2023.
MSD K.K. LAGEVRIO® Interview Form (Japanese). https://www.msdconnect.jp/wp-content/uploads/sites/5/2022/09/if_lagevrio_cap200.pdf. Accessed Nov 17, 2022.
Yoon JJ, Toots M, Lee S, et al. Orally efficacious broad-spectrum ribonucleoside analog inhibitor of influenza and respiratory syncytial viruses. Antimicrob Agents Chemother. 2018;62(8):e00766-e818. https://doi.org/10.1128/aac.00766-18.
Cox RM, Wolf JD, Plemper RK. Therapeutically administered ribonucleoside analogue MK-4482/EIDD-2801 blocks SARS-CoV-2 transmission in ferrets. Nat Microbiol. 2021;6(1):11–8. https://doi.org/10.1038/s41564-020-00835-2.
Sheahan TP, Sims AC, Zhou S, et al. An orally bioavailable broad-spectrum antiviral inhibits SARS-CoV-2 in human airway epithelial cell cultures and multiple coronaviruses in mice. Sci Transl Med. 2020;12(541): eabb5883. https://doi.org/10.1126/scitranslmed.abb5883.
Wahl A, Gralinski LE, Johnson CE, et al. SARS-CoV-2 infection is effectively treated and prevented by EIDD-2801. Nature. 2021;591(7850):451–7. https://doi.org/10.1038/s41586-021-03312-w.
Abdelnabi R, Foo CS, De Jonghe S, Maes P, Weynand B, Neyts J. Molnupiravir inhibits replication of the emerging SARS-CoV-2 variants of concern in a hamster infection model. J Infect Dis. 2021;224(5):749–53. https://doi.org/10.1093/infdis/jiab361.
Agostini ML, Pruijssers AJ, Chappell JD, et al. Small-molecule antiviral β-d-N(4)-hydroxycytidine inhibits a proofreading-intact coronavirus with a high genetic barrier to resistance. J Virol. 2019;93(24):e01348-e1419. https://doi.org/10.1128/jvi.01348-19.
Urakova N, Kuznetsova V, Crossman DK, et al. β-d-N(4)-hydroxycytidine is a potent anti-alphavirus compound that induces a high level of mutations in the viral genome. J Virol. 2018;92(3):e01965-e2017. https://doi.org/10.1128/jvi.01965-17.
Uraki R, Kiso M, Iida S, et al. Characterization and antiviral susceptibility of SARS-CoV-2 Omicron BA.2. Nature. 2022;607(7917):119–27. https://doi.org/10.1038/s41586-022-04856-1.
Zou R, Peng L, Shu D, et al. Antiviral efficacy and safety of molnupiravir against omicron variant infection: a randomized controlled clinical trial. Front Pharmacol. 2022;13: 939573. https://doi.org/10.3389/fphar.2022.939573.
Jayk Bernal A, Gomes da Silva MM, Musungaie DB, et al. Molnupiravir for oral treatment of Covid-19 in nonhospitalized patients. N Engl J Med. 2022;386(6):509–20. https://doi.org/10.1056/NEJMoa2116044.
Ministry of Health, Labour and Welfare. Clinical management of patients with COVID-19. https://www.mhlw.go.jp/content/000936655.pdf. Accessed Nov 17, 2022.
Terada M, Ohtsu H, Saito S, et al. Risk factors for severity on admission and the disease progression during hospitalisation in a large cohort of patients with COVID-19 in Japan. BMJ Open. 2021;11(6): e047007. https://doi.org/10.1136/bmjopen-2020-047007.
COVID-19 Advisory Board. Analysis of mortality cases based on the COVID-19 registry (Japanese). https://covid-registry.ncgm.go.jp/achievements/documents/220907.pdf. Accessed Nov 17, 2022.
Ministry of Health, Labour and Welfare. Eleven things you need to know NOW about COVID-19 (As of August 2022). https://www.mhlw.go.jp/content/aug2022.pdf. Accessed Nov 17, 2022.
Ministry of Health, Labour and Welfare. Eleven things you need to know NOW about COVID-19 (As of October 2022). https://www.mhlw.go.jp/content/oct2022.pdf. Accessed Nov 17, 2022.
Suzuki Y, Shibata Y, Minemura H, et al. Real-world clinical outcomes of treatment with molnupiravir for patients with mild-to-moderate coronavirus disease 2019 during the Omicron variant pandemic. Clin Exp Med. 2022. https://doi.org/10.1007/s10238-022-00949-3.
Wong CKH, Au ICH, Lau KTK, Lau EHY, Cowling BJ, Leung GM. Real-world effectiveness of molnupiravir and nirmatrelvir plus ritonavir against mortality, hospitalisation, and in-hospital outcomes among community-dwelling, ambulatory patients with confirmed SARS-CoV-2 infection during the omicron wave in Hong Kong: an observational study. Lancet. 2022;400(10359):1213–22. https://doi.org/10.1016/s0140-6736(22)01586-0.
Arbel R, Sagy YW, Battat E, et al. Molnupiravir use and severe Covid-19 outcomes during the omicron surge (Preprint). 2022. https://doi.org/10.21203/rs.3.rs-2115769/v1.
Vena A, Traman L, Bavastro M, et al. Early clinical experience with molnupiravir for mild to moderate breakthrough COVID-19 among fully vaccinated patients at risk for disease progression. Vaccines. 2022;10(7):1141. https://doi.org/10.3390/vaccines10071141.
Butler CC, Hobbs R, Gbinigie A, et al. Molnupiravir plus usual care versus usual care alone as early treatment for adults with COVID-19 at increased risk of adverse outcomes (PANORAMIC): an open-label, platform-adaptive randomised controlled trial. Lancet. 2023;401(10373):281–93. https://doi.org/10.1016/S0140-6736(22)02597-1.
Acknowledgements
Funding
This work was supported by MSD K.K., Tokyo, Japan. All authors are employed by MSD K.K. MSD K.K. provided support in the form of salaries for authors. MSD K.K provided support for this journal’s rapid service fee.
Medical Writing and/or Editorial Assistance
Statistical analysis and data management were provided by CMIC HOLDINGS Co., Ltd. Medical writing support was provided by Robert Phillips and Emiko Sato at Clinical Study Support, Inc. (Nagoya, Japan). Both statistical and medical writing supports were funded by MSD K.K. (Tokyo, Japan). The authors would like to thank all investigators who conducted this survey and provided necessary data on patients treated for COVID-19.
Author Contributions
Masahiro Kimata, Asuka Watanabe, Yukiko Yanagida, Daisuke Kinoshita and Shinichiroh Maekawa made substantial contributions to all of the following: (1) the conception and design of the survey, or acquisition of data, or analysis and interpretation of data, (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted and meet the ICMJE authorship criteria.
Disclosures
Masahiro Kimata, Asuka Watanabe, Yukiko Yanagida, Daisuke Kinoshita and Shinichiroh Maekawa, are all employees of MSD K.K.
Compliance with Ethics Guidelines
This PMS was conducted in accordance with the MHLW ordinance for GPSP. The survey protocol was approved by the Pharmaceuticals and Medical Devices Agency (PMDA). Additionally, this survey was conducted in accordance with the protocol; the Helsinki Declaration of 1964, and its later amendments; and all other applicable regulations. IRB approval was not mandatory for this survey according to the GPSP. The physician in charge of the survey explained to the patient or his/her legally acceptable representative the objective of the survey, the information to be collected through the survey and the uses of the survey results and obtained informed consent from the patient or his/her legally acceptable representative.
Data Availability
The datasets generated during and/or analyzed during the current survey are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kimata, M., Watanabe, A., Yanagida, Y. et al. Safety and Effectiveness of Molnupiravir (LAGEVRIO®) Capsules in Japanese Patients with COVID-19: Interim Report of Post-marketing Surveillance in Japan. Infect Dis Ther 12, 1119–1136 (2023). https://doi.org/10.1007/s40121-023-00782-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-023-00782-5