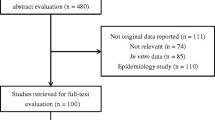
Abstract
Introduction
High-dose daptomycin-based combinations are recommended for vancomycin-resistant Enterococcus (VRE) bloodstream infection (BSI). Preclinical data have shown a synergistic effect of daptomycin/fosfomycin combinations against VRE. However, clinical studies comparing daptomycin monotherapy with daptomycin/fosfomycin combinations are unavailable.
Methods
An observational study of VRE-BSI was performed between 2010–2021 on patients receiving daptomycin monotherapy (≥ 8 mg/kg) or daptomycin combined with intravenous fosfomycin. Patients treated with concomitant β-lactam combinations were excluded. The primary outcome was in-hospital mortality. Outcomes were analyzed using multivariable logistic regression and augmented inverse probability weighting (AIPW) analyses.
Results
Among 224 patients, 176 received daptomycin monotherapy, and 48 received fosfomycin combinations. The median daptomycin and fosfomycin doses were 9.8 mg/kg and 12 g/day, respectively. In-hospital mortality was 77.3% and 47.9% in the daptomycin monotherapy and fosfomycin combination groups (P < 0.001), respectively. Multivariable logistic regression analysis predicted lower mortality with fosfomycin combination treatment (adjusted odds ratio, 0.35; 95% confidence interval (CI), 0.17–0.73; P = 0.005). AIPW demonstrated a 17.8% reduced mortality with fosfomycin combinations (95% CI, − 30.6– − 4.9%; P = 0.007). The survival benefit was significant, especially among patients with a lower Pitt bacteremia score or fosfomycin minimum inhibitory concentration (MIC) ≤ 64 mg/l. Fosfomycin combination resulted in higher hypernatremia (10.4% vs. 2.8%, P = 0.04) and hypokalemia (33.3% vs. 15.3%, P = 0.009) compared to daptomycin monotherapy.
Conclusion
The combination of high-dose daptomycin with fosfomycin improved the survival rate of patients with VRE-BSI compared to daptomycin alone. The benefit of the combination was most pronounced for VRE with fosfomycin MIC ≤ 64 mg/l and for patients with a low Pitt bacteremia score.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Clinical studies comparing daptomycin monotherapy with daptomycin/fosfomycin combinations for vancomycin-resistant Enterococcus (VRE) bloodstream infection (BSI) are unavailable. |
We compared the clinical effectiveness of high-dose daptomycin monotherapy with high-dose daptomycin and fosfomycin combinations for vancomycin-resistant Enterococcus bloodstream infection. |
What was learned from the study? |
The combination of high-dose daptomycin with fosfomycin improved the survival rate of patients with VRE-BSI compared to daptomycin alone. |
The overall in-hospital mortality rates were 77.3% and 47.9% in the daptomycin monotherapy and fosfomycin combination groups, respectively (P < 0.001). |
Multivariable logistic regression showed that fosfomycin combination was an independent predictor of lower mortality (adjusted odds ratio, 0.35; 95% confidence interval 0.17–0.73; P = 0.005). |
Introduction
Bloodstream infections (BSIs) with vancomycin-resistant enterococci (VRE) are of great concern because of their high morbidity and mortality. Linezolid and daptomycin are among the few antimicrobial agents that can effectively treat VRE BSI [1, 2]. Linezolid was initially preferred over daptomycin because of its lower associated mortality [3, 4], but high-dose daptomycin has been found to be at least as effective as linezolid [5, 6].
High-dose daptomycin has become an attractive option because of its bactericidal activity and concentration-dependent effect [7]. Several studies have validated its role in in treatment of VRE BSI [8, 9]. However, the mortality rate associated with VRE BSI remains high. It is doubtful that an adequate pharmacodynamic effect can be achieved against VRE with high daptomycin minimum inhibitory concentrations (MICs) even with high-dose daptomycin [10]. VRE isolates with higher daptomycin MICs, although still susceptible, are associated with increased microbiological failure [11]. It has been suggested that β-lactam antibiotics might be considered for treatment of VRE BSI [12], since β-lactam antibiotics combined with daptomycin further enhance its antimicrobial activity [13, 14]. Nonetheless, the inherent resistance of VRE to β-lactams and suboptimal patient outcomes warrant the investigation of other alternative combinations.
Fosfomycin has broad-spectrum bactericidal activity. It has been extensively evaluated for treatment of patients with gram-positive and -negative BSI [15]. Combinations of fosfomycin with daptomycin have been reported to be synergistic against methicillin-resistant Staphylococcus aureus (MRSA) [16]. A randomized controlled trial found the combination to be superior to daptomycin monotherapy for microbiological outcomes in MRSA BSI [17], though the treatment success rate was not significantly different. Daptomycin with fosfomycin has also been shown to be synergistic against VRE in in vitro studies [18,19,20]. The combination was found to be a potent and safe treatment option for VRE BSI in our previous observational cohort study [21]. However, the study did not include the daptomycin monotherapy group as a control group. In view of these promising observations, further studies are needed to determine whether the combination of fosfomycin and daptomycin is clinically superior to daptomycin alone.
We hypothesized that combination of fosfomycin and daptomycin might improve the survival of patients with VRE BSI compared to daptomycin alone. We conducted this observational study to compare the clinical efficacy of high-dose daptomycin monotherapy with high-dose daptomycin and fosfomycin combinations for VRE BSI. We also evaluated the safety of daptomycin and fosfomycin combinations compared to daptomycin monotherapy.
Methods
Hospital Setting and Patients
This study is a subgroup analysis of the previously published cohort [22]. The retrospective cohort study was conducted at the National Taiwan University Hospital (NTUH), the NTUH-Hsin-Chu Branch, and the NTUH-Yun-Lin Branch. The VRE BSI patients were prospectively identified per institution routine. For this study, a subcohort was retrieved and analyzed retrospectively. The Research Ethics Committee of the NTUH (201606064RINB) approved the study protocol and waived the requirement for informed consent. Since (1) this is a retrospective study and the research would not be practicable to carry out without the waiver, (2) the research has important social value, and (3) the research poses no more than minimal risks to participants, the committee waived the requirement for informed consent. The study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments.
Patients with VRE BSI between January 2010 and December 2021 were enrolled. VRE BSI was defined as the growth of VRE in at least one set of blood cultures. The inclusion criteria were as follows: The patients were hospitalized, aged ≥ 18 years, and had received ≥ 8 mg/kg daptomycin. Patients who received daptomycin and β-lactam combinations were excluded [23]. Only the first episode of VRE BSI was included among patients with two or more episodes within the cohort period. Addition of fosfomycin within 24 h of daptomycin was a required criterion for receipt of fosfomycin combinations. The duration of fosfomycin administration was not limited to avoid an immortal time bias. The selection of patients to be treated with fosfomycin and daptomycin alone or together, dosage, and laboratory tests were based on the clinical judgment of the primary care physicians. In our hospital, fosfomycin is given in 2–3 divided doses, and the daily maximum dose is adjusted according to renal function: decreased to 70%, 60%, 40%, and 20% when the estimated creatinine clearance (CrCl) falls to 30–40, 20–30, 10–20, and ≤ 10 ml/min, respectively. For patients on hemodialysis, 2 g of fosfomycin is administered after hemodialysis.
Microbiological Studies and Antimicrobial Susceptibility Testing
The blood cultures were processed at the clinical microbiology laboratory. Before 2017, Enterococcus spp. were identified using the VITEK 2 identification system (bioMérieux, Marcy l'Etoile, France). Subsequently, Enterococcus spp. were identified using matrix-assisted laser desorption ionization-time-of-flight mass spectrometry (Bruker Biotyper system, MicroFlex LT; Bruker Daltonik GmbH, Bremen, Germany). Vancomycin-resistant enterococci were defined as Enterococcus isolates with a vancomycin MIC ≥ 32 mg/l. The MIC of daptomycin was determined by the broth microdilution method. Cation-Adjusted Mueller-Hinton Broth (Becton Dickinson, Le Pont-de-Claix, France) supplemented with 50 mg/l calcium was used. The fosfomycin MIC was determined using the agar dilution method in a medium supplemented with 25 mg/l glucose-6-phosphate. MIC for fosfomycin was interpreted based on the criteria for Enterococcus faecalis urinary tract isolates [24].
Clinical Data Collection and Definitions
Patients’ baseline characteristics were obtained from their electronic medical records. Primary bacteremia was defined as the absence of an otherwise identified infection focus. Catheter-related infections were defined according to previously published guidelines [25]. Source control was defined as central venous catheter removal for catheter-related infections and image-guided aspiration, drainage, or surgical drainage for intra-abdominal infections [21]. Immunosuppressive agent use was defined as the prescription of antineoplastic medications, cyclophosphamide, or other immunosuppressants within 6 weeks or prednisolone over 20 mg/day for ≥ 2 weeks or 30 mg/day for ≥ 1 week before the onset of VRE BSI [26]. The Charlson comorbidity index was calculated to adjust for the underlying conditions [27], and the Pitt bacteremia score was considered to evaluate BSI severity [28]. The following adverse events were recorded during the treatment: creatine kinase (CK) elevation was defined as a serum CK level > 250 U/l. Thrombocytopenia was defined as a platelet count < 50,000/μl. Hypernatremia was defined as serum sodium level > 155 mEq/l and hypokalemia as serum potassium level < 3 mEq/l [29]. CrCl was estimated using the Cockcroft-Gault equation. Acute kidney injury was defined as CrCl reduction > 50% or serum creatinine level elevation by at least two-fold if baseline CrCl ≥ 60 ml/min, CrCl reduction > 20%, or serum creatinine level elevation by at least 1.5-fold if baseline CrCl < 60 ml/min [22].
The primary outcome was in-hospital mortality. The secondary outcomes were 28- and 14-day all-cause mortality, microbiological failure, and clinical failure. Microbiological failure was defined as VRE isolation in follow-up blood cultures ≥ 4 days after the onset of VRE BSI or mortality within 7 days of VRE BSI without documented bloodstream VRE clearance [9]. Clinical failure was defined as either mortality within 14 days or microbiological failure [9]. In the sensitivity analysis of the primary outcome, patients receiving fosfomycin before documented bloodstream VRE clearance were selected in the fosfomycin combination group [21].
Statistical Analysis
For categorical variables, percentages were presented, and a two-tailed Fisher’s exact test was performed for comparisons. The median and interquartile range (IQR) were presented for continuous variables, and a Mann-Whitney U test was used for comparisons. Multivariable logistic regression was performed for the outcome analysis. Variables with a P-value ≤ 0.1 in the univariable regression were included in the multivariable analysis. Multivariable models were developed using backward stepwise minimization of Akaike’s information criterion (AIC). Significant differences might be present in the baseline characteristics of the daptomycin monotherapy and daptomycin fosfomycin combination groups. Multivariable logistic regression generated by backward stepwise minimizing AIC with covariates with a P value ≤ 0.1 was applied to identify independent predictors for daptomycin monotherapy or daptomycin and fosfomycin combination. Propensity score was calculated according to the regression model, and augmented inverse probability weighting (AIPW) was used to estimate the average treatment effect [30]. The interactions between the fosfomycin combination and Pitt bacteremia score on the outcome were examined by marginal effects analysis. Stata software (v. 17; StataCorp, College Station, TX, USA) was used for statistical analysis. Two-sided P values ≤ 0.05 were considered significant in all analyses.
Results
Study Participants
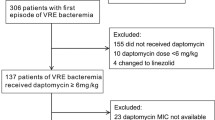
A total of 1425 episodes of VRE BSI were identified within the study period, among which 224 patients met the inclusion criteria for the analysis. Among these cases, 176 received daptomycin monotherapy, and 48 received the daptomycin and fosfomycin combination (Fig. 1). All isolates showed the presence of E. faecium. Among these, 204 were available for the MIC determination. Daptomycin MIC was ≤ 1 mg/l, 2 mg/l, and ≥ 4 mg/l in 21 (10.3%), 109 (53.4%), and 74 (36.3%) isolates, respectively. In contrast, fosfomycin MIC was ≤ 32 mg/l, 64 mg/l, and ≥ 128 mg/l in 9 (4.4%), 99 (48.5%), and 96 (47.1%) isolates, respectively (Table 1).
Among the 224 patients, the median (IQR) age and Pitt bacteremia score were 66.9 (58.5–78.3) years and 2 (0–4) points, respectively (Table 1). The median source control was 0 (-10–7) days and 1 (0–2) days after the onset of VRE BSI for patients with intra-abdominal and catheter-related infections, respectively. The interval to daptomycin initiation from the onset of VRE BSI was 2 (2–3) days. The daptomycin dose was 9.8 (9.0–10.4) mg/kg. The fosfomycin combination dose was 12 (6–21) g/day. The duration of daptomycin treatment was 8.5 (3–14) days. The duration of fosfomycin treatment was 7.5 (3–14) days. The overall in-hospital mortality was 71.0%. The mortality rate was 76.9% for the period of 2010–15 and 70.2% for the period of 2016–21 (P = 0.48).
The demographics and clinical characteristics of patients with VRE BSI treated with daptomycin monotherapy or fosfomycin combinations are summarized in Table 1. The overall in-hospital mortality rates were 77.3% and 47.9% in the daptomycin monotherapy and fosfomycin combination groups, respectively (P < 0.001). The Pitt bacteremia score was significantly higher in the daptomycin monotherapy group than in the fosfomycin combination group (2 vs. 1, P = 0.008). The daptomycin dose was 9.7 and 10.1 mg/kg, respectively (P = 0.04). Daptomycin and fosfomycin MICs were not significantly different between the two groups.
Association Between Fosfomycin Combination and Mortality
The underlying factors associated with mortality were also analyzed (Table 2). Daptomycin dose was not significantly different between survivors and non-survivors (10.0 vs. 9.7 mg/kg, P = 0.45). Among the daptomycin monotherapy group, the mortality rate was not different between daptomycin MIC of < 4 and ≥ 4 mg/l (78/99 vs. 47/61, P = 0.80). Fosfomycin combination is associated with less mortality than daptomycin alone among daptomycin MIC of < 4 mg/l (14/31 vs. 78/99, P < 0.001) and daptomycin MIC of ≥ 4 mg/l (6/13 vs. 47/61, P = 0.03). Multivariable logistic regression (Table 3) showed that fosfomycin combination was an independent predictor of lower mortality [adjusted odds ratio (aOR), 0.35; 95% confidence interval (CI) 0.17–0.73; P = 0.005]. Compared to the daptomycin monotherapy, the fosfomycin combination significantly showed a lower mortality with a fosfomycin MIC of ≤ 64 mg/l (136/176 vs. 12/28; aOR, 0.28; 95% CI, 0.11–0.68; P = 0.005) but not with a fosfomycin MIC of ≥ 128 mg/l (136/176 vs. 8/16; aOR, 0.45; 95% CI, 0.14–1.47; P = 0.19). The Kaplan-Meier survival curves of daptomycin monotherapy versus fosfomycin combinations are shown in Fig. 2a, b. Fosfomycin combination was associated with a lower mortality rate than daptomycin monotherapy (hazard ratio, 0.59; 95% CI, 0.38–0.91; P = 0.02).
Comparison of Kaplan-Meier survival curves between (A) daptomycin monotherapy and daptomycin and fosfomycin combination and (B) daptomycin monotherapy and daptomycin and fosfomycin combination with different minimum inhibitory concentrations in patients with vancomycin-resistant enterococcal bloodstream infection. DAP daptomycin, FOS fosfomycin, Gr group, HR hazard ratio, MIC minimum inhibitory concentration
Multivariable logistic regression analysis of the factors associated with fosfomycin combinations with P ≤ 0.1 and backward stepwise AIC method is presented in Table 4. Peptic ulcer disease (aOR, 0.21, P = 0.04), malignancy (aOR 0.42, P = 0.01), and Pitt bacteremia score (aOR 0.80, P = 0.005) were significantly different between the two groups; they were therefore included to calculate propensity score. With the balance of AIPW, the standardized mean mortality of daptomycin monotherapy and fosfomycin combinations was 75.4% and 57.6%, respectively. Fosfomycin combination exhibited an average 17.8% reduction in mortality (95% CI, − 30.6– − 4.9%; P = 0.007).
In addition, we used propensity score for matching. The baseline characteristics, especially the Pitt bacteremia score, of the fosfomycin combination and the daptomycin monotherapy groups were relatively similar among the propensity score-matched cohort (Supplementary Table S1). The fosfomycin combination group had lower mortality than the daptomycin monotherapy group (47.9% vs. 70.8%, P = 0.02).
Interaction Between the Fosfomycin Combination and Pitt Bacteremia Score
The marginal effects analysis of the interaction between fosfomycin combinations and Pitt bacteremia score on mortality is shown in Fig. 3. For lower Pitt bacteremia scores, fosfomycin combinations provided a significant survival benefit compared to that by daptomycin monotherapy. The benefit became insignificant as the Pitt bacteremia score increased.
Sensitivity Analysis
The sensitivity analysis included 176 and 41 patients who received daptomycin monotherapy and fosfomycin combinations, respectively, before documented bloodstream VRE clearance. This result supports the finding of a primary comparison. Fosfomycin combinations were independently associated with lower overall mortality in the multivariable logistic regression (aOR, 0.37; 95% CI, 0.17–0.82; P = 0.01).
Secondary Outcomes
The secondary outcomes are presented in Table 5. Twenty-eight-day mortality (61.9% vs. 43.8%, P = 0.02), clinical failure (63.6% vs. 45.8%, P = 0.03), and microbiological failure (50.0% vs. 24.2%, P = 0.008) were significantly higher in the daptomycin monotherapy group. As for adverse events, the hypernatremia rate (2.8% vs. 10.4%, P = 0.04) and hypokalemia rate (15.3% vs. 33.3%, P = 0.009) were significantly higher in the fosfomycin combination group. The new-onset thrombocytopenia rate was borderline higher in the monotherapy group (27.6 vs. 17.1%, P = 0.05). CK elevation and acute kidney injury rates were not significantly different between the two groups. Only one patient in the daptomycin monotherapy group discontinued antibiotic treatment because of adverse event of elevated CK (1714 U/l).
Discussion
Linezolid or high-dose daptomycin combined with β-lactams is currently recommended for treatment of VRE BSI. Combinations of daptomycin with fosfomycin are being evaluated because of suboptimal outcomes and poor prognosis with current therapy [31, 32]. In this observational study, we found on multivariable logistic regression analysis that daptomycin/fosfomycin was associated with lower in-hospital mortality than daptomycin alone. We also observed a significant reduction in the average treatment effect favoring daptomycin/fosfomycin in the AIPW analysis. The combination of daptomycin and fosfomycin was also significantly associated with lower secondary outcomes, including 28-day mortality, microbiological failure, and clinical failure, but with higher rates of hypernatremia and hypokalemia than daptomycin alone.
The potential efficacy of combinations of daptomycin and fosfomycin against enterococci is supported by several in vitro and in vivo studies [18,19,20]. The synergistic mechanism against VRE is attributed to the ability of fosfomycin to imbalance the bacterial membrane potential and thereby reduce surface charge. This effect enhances cationic binding of daptomycin to the cell surface and facilitates bactericidal activity [19]. Several case reports and an observational study found combination therapy to be a promising approach to treatment of VRE BSI [21, 33]. The current observational study provides further support for the concept that daptomycin/fosfomycin combinations are more effective than high-dose daptomycin monotherapy for VRE BSI.
We recently reported that high-dose daptomycin was associated with better clinical outcomes in VRE BSI than lower doses combined with fosfomycin [21]. In the current study we maximized the daptomycin dose effect on the outcome by including only those patients who received a dose of ≥ 8 mg/kg. We did not find an association within the range of high doses of daptomycin with clinical outcomes. This was probably due to the similar high dose ranges of the cohort (all ≥ 8 mg/kg, median 9.8 mg/kg) and the relatively small sample size. The lower mortality associated with the fosfomycin combination became insignificant as the Pitt bacteremia score worsened. This is not surprising since severity of infection is the major limitation for all antibiotics regardless of their antimicrobial activity for patients with major underlying diseases and shortened life expectancies.
Fosfomycin has been shown to have both direct antibacterial and synergistic activity with daptomycin against VRE [21]. The efficacy of the daptomycin/fosfomycin combination against VRE BSI is strongly dependent on susceptibility to fosfomycin [21]. Thirty-four cases were included in both previous and present studies. In the current study we found that only patients with isolates exhibiting low fosfomycin MICs benefited from the combination with daptomycin. The combination was not more effective than daptomycin alone in 16 patients with a fosfomycin MIC ≥ 128 mg/l. This suggests but does not prove that fosfomycin exerts and an additive rather synergistic effect in combination with daptomycin.
Though the duration of the antibiotic is an important variable, there might be reverse causation bias. Patients who lived longer received longer treatment. The direction of the causal relationship could not be confirmed using the current observational approach. In addition, survivors had a longer time to daptomycin treatment than non-survivors (3 vs. 2, P = 0.01). However, the result should be interpreted with caution. The association might be a result of confounding by indication. Patients with more severe VRE BSI might be associated with a higher bacterial burden and shorter time to blood culture positivity [34, 35]. Therefore, these more severe patients might have a shorter time to daptomycin treatment. We should not overlook the importance of early antimicrobial treatment.
Hypokalemia was the most common adverse event among patients who received combinations of daptomycin and fosfomycin. This is a known complication of fosfomycin therapy [32]. It appears to be related to increased renal excretion of fosfomycin in the distal tubules. Hypokalemia might be prevented by an extended infusion period [36]. The high sodium salt content of fosfomycin might have contributed to the significantly higher rate of hypernatremia. We recommend frequent serum electrolyte monitoring during fosfomycin administration. We found a borderline significantly higher frequency of new-onset thrombocytopenia in the daptomycin monotherapy group. This might be related to significantly higher Pitt bacteremia scores among patients who received daptomycin monotherapy or reflects a better prognosis for patients in the daptomycin/fosfomycin combination group.
The strengths of this study include use of high-dose daptomycin in both arms of the study. We excluded β-lactam combinations to minimize treatment heterogeneity and facilitate a fair comparison of the two arms of the study. We used two independent statistical methods, multivariable logistic regression and AIPW, to show the benefit of addition of fosfomycin to high-dose daptomycin. The AIPW estimates the average treatment effect and potential outcome means from observational data. The AIPW combines aspects of regression adjustment and inverse-probability-weighted methods and has a double-robust property [30, 37].
This study has several limitations. Although we used a multivariable logistic regression approach to control for possible confounders, non-observable confounders remain despite our endeavors to minimize them by applying the AIPW balance. Blood cultures were obtained based on the judgment of the primary care physician. Thus, we could not control some misclassifications in estimating some of the microbiological outcomes. Misclassification may have been non-differential and could bias the results towards null [38]. We collected only the first isolate per patient. Therefore, we cannot show the development of daptomycin resistance and compare the developed resistance in different treatment groups. The optimal fosfomycin dose for the combination is unknown and may have been underestimated for patients with less susceptible isolates.
Conclusions
This study provides clinical evidence that the combination of high-dose daptomycin with fosfomycin improved the survival of patients with VRE BSI compared to daptomycin alone. The benefit of the combination was most pronounced for VRE with fosfomycin MIC ≤ 64 mg/l and for patients with less severe BSI, as determined by the Pitt bacteremia score. Randomized controlled trials are needed to provide further evidence for the therapeutic benefit of this combination.
References
Arias CA, Contreras GA, Murray BE. Management of multidrug-resistant enterococcal infections. Clin Microbiol Infect. 2010;16(6):555–62. https://doi.org/10.1111/j.1469-0691.2010.03214.x.
Wang JL, Hsueh PR. Therapeutic options for infections due to vancomycin-resistant enterococci. Expert Opin Pharmacother. 2009;10(5):785–96. https://doi.org/10.1517/14656560902811811.
Balli EP, Venetis CA, Miyakis S. Systematic review and meta-analysis of linezolid versus daptomycin for treatment of vancomycin-resistant enterococcal bacteremia. Antimicrob Agents Chemother. 2014;58(2):734–9. https://doi.org/10.1128/AAC.01289-13.
Chuang YC, Wang JT, Lin HY, Chang SC. Daptomycin versus linezolid for treatment of vancomycin-resistant enterococcal bacteremia: systematic review and meta-analysis. BMC Infect Dis. 2014;14:687. https://doi.org/10.1186/s12879-014-0687-9.
Chuang YC, Lin HY, Chen PY, Lin CY, Wang JT, Chang SC. Daptomycin versus linezolid for the treatment of vancomycin-resistant enterococcal bacteraemia: implications of daptomycin dose. Clin Microbiol Infect. 2016;22(10):890. https://doi.org/10.1016/j.cmi.2016.07.018.
Britt NS, Potter EM, Patel N, Steed ME. Comparison of the effectiveness and safety of linezolid and daptomycin in vancomycin-resistant enterococcal bloodstream infection: a national cohort study of veterans affairs patients. Clin Infect Dis. 2015;61(6):871–8. https://doi.org/10.1093/cid/civ444.
French GL. Bactericidal agents in the treatment of MRSA infections—the potential role of daptomycin. J Antimicrob Chemother. 2006;58(6):1107–17. https://doi.org/10.1093/jac/dkl393.
Britt NS, Potter EM, Patel N, Steed ME. Comparative effectiveness and safety of standard-, medium-, and high-dose daptomycin strategies for the treatment of vancomycin-resistant enterococcal bacteremia among veterans affairs patients. Clin Infect Dis. 2017;64(5):605–13. https://doi.org/10.1093/cid/ciw815.
Chuang YC, Lin HY, Chen PY, et al. Effect of daptomycin dose on the outcome of vancomycin-resistant, daptomycin-susceptible enterococcus faecium bacteremia. Clin Infect Dis. 2017;64(8):1026–34. https://doi.org/10.1093/cid/cix024.
Avery LM, Kuti JL, Weisser M, et al. pharmacodynamic analysis of daptomycin-treated enterococcal bacteremia: it is time to change the breakpoint. Clin Infect Dis. 2019;68(10):1650–7. https://doi.org/10.1093/cid/ciy749.
Shukla BS, Shelburne S, Reyes K, et al. Influence of minimum inhibitory concentration in clinical outcomes of enterococcus faecium bacteremia treated with daptomycin: is it time to change the breakpoint? Clin Infect Dis. 2016;62(12):1514–20. https://doi.org/10.1093/cid/ciw173.
Mercuro NJ, Davis SL, Zervos MJ, Herc ES. Combatting resistant enterococcal infections: a pharmacotherapy review. Expert Opin Pharmacother. 2018;19(9):979–92. https://doi.org/10.1080/14656566.2018.1479397.
Smith JR, Barber KE, Raut A, Aboutaleb M, Sakoulas G, Rybak MJ. beta-Lactam combinations with daptomycin provide synergy against vancomycin-resistant enterococcus faecalis and enterococcus faecium. J Antimicrob Chemother. 2015;70(6):1738–43. https://doi.org/10.1093/jac/dkv007.
Chuang YC, Chen PY, Lin CY, Chen YC, Wang JT, Chang SC. A retrospective clinical comparison of daptomycin vs daptomycin and a beta-lactam antibiotic for treating vancomycin-resistant Enterococcus faecium bloodstream infections. Sci Rep. 2018;8(1):1632. https://doi.org/10.1038/s41598-018-19986-8.
Michalopoulos AS, Livaditis IG, Gougoutas V. The revival of fosfomycin. Int J Infect Dis. 2011;15(11):e732–9. https://doi.org/10.1016/j.ijid.2011.07.007.
de la Garcia MC, Gasch O, Garcia-Gonzalez J, et al. The combination of daptomycin and fosfomycin has synergistic, potent, and rapid bactericidal activity against methicillin-resistant staphylococcus aureus in a rabbit model of experimental endocarditis. Antimicrob Agents Chemother. 2018. https://doi.org/10.1128/AAC.02633-17.
Pujol M, Miro JM, Shaw E, et al. Daptomycin plus fosfomycin versus daptomycin alone for methicillin-resistant staphylococcus aureus bacteremia and endocarditis: a randomized clinical trial. Clin Infect Dis. 2021;72(9):1517–25. https://doi.org/10.1093/cid/ciaa1081.
Descourouez JL, Jorgenson MR, Wergin JE, Rose WE. Fosfomycin synergy in vitro with amoxicillin, daptomycin, and linezolid against vancomycin-resistant Enterococcus faecium from renal transplant patients with infected urinary stents. Antimicrob Agents Chemother. 2013;57(3):1518–20. https://doi.org/10.1128/AAC.02099-12.
Hall Snyder AD, Werth BJ, Nonejuie P, et al. Fosfomycin enhances the activity of daptomycin against vancomycin-resistant enterococci in an in vitro pharmacokinetic-pharmacodynamic model. Antimicrob Agents Chemother. 2016;60(10):5716–23. https://doi.org/10.1128/AAC.00687-16.
Antonello RM, Principe L, Maraolo AE, et al. Fosfomycin as partner drug for systemic infection management a systematic review of its synergistic properties from in vitro and in vivo studies. Antibiotics. 2020. https://doi.org/10.3390/antibiotics9080500.
Chuang YC, Tseng TC, Wang JT, et al. Influence of daptomycin dose and fosfomycin susceptibility on outcome of vancomycin-resistant Enterococcus faecium bloodstream infections treated with daptomycin and fosfomycin combination. J Antimicrob Chemother. 2022;77(5):1436–43. https://doi.org/10.1093/jac/dkac023.
Chuang YC, Lin HY, Yang JL, et al. Influence of daptomycin doses on the outcomes of VRE bloodstream infection treated with high-dose daptomycin. J Antimicrob Chemother. 2022;77(8):2278–87. https://doi.org/10.1093/jac/dkac164.
Casapao AM, Jacobs DM, Bowers DR, Beyda ND, Dilworth TJ. Early administration of adjuvant beta-lactam therapy in combination with vancomycin among patients with methicillin-resistant staphylococcus aureus bloodstream infection: a retrospective, multicenter analysis. Pharmacotherapy. 2017;37(11):1347–56. https://doi.org/10.1002/phar.2034.
Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing: 31st Edition, M100. Wayne: CLSI; 2021.
O’Grady NP, Alexander M, Burns LA, et al. Summary of recommendations: guidelines for the prevention of intravascular catheter-related infections. Clin Infect Dis. 2011;52(9):1087–99. https://doi.org/10.1093/cid/cir138.
Chuang YC, Sheng WH, Li SY, et al. Influence of genospecies of Acinetobacter baumannii complex on clinical outcomes of patients with acinetobacter bacteremia. Clin Infect Dis. 2011;52(3):352–60. https://doi.org/10.1093/cid/ciq154.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83. https://doi.org/10.1016/0021-9681(87)90171-8.
Chow JW, Yu VL. Combination antibiotic therapy versus monotherapy for gram-negative bacteraemia: a commentary. Int J Antimicrob Agents. 1999;11(1):7–12. https://doi.org/10.1016/s0924-8579(98)00060-0.
Iarikov D, Wassel R, Farley J, Nambiar S. Adverse events associated with fosfomycin use: review of the literature and analyses of the FDA adverse event reporting system database. Infect Dis Ther. 2015;4(4):433–58. https://doi.org/10.1007/s40121-015-0092-8.
Robins JM, Rotnitzky A, Zhao LP. Estimation of regression coefficients when some regressors are not always observed. J Am Stat Assoc. 1994;89(427):846–66. https://doi.org/10.2307/2290910.
Miller WR, Murray BE, Rice LB, Arias CA. Vancomycin-resistant enterococci: therapeutic challenges in the 21st century. Infect Dis Clin North Am. 2016;30(2):415–39. https://doi.org/10.1016/j.idc.2016.02.006.
Falagas ME, Vouloumanou EK, Samonis G, Vardakas KZ. Fosfomycin. Clin Microbiol Rev. 2016;29(2):321–47. https://doi.org/10.1128/CMR.00068-15.
Khatri AM, Anderson AD, Camargo JF. Addition of oral fosfomycin to antimicrobial salvage therapy for persistent vancomycin-resistant enterococcal bacteremia. Clin Infect Dis. 2022;74(9):1710–1. https://doi.org/10.1093/cid/ciab832.
Chuang YC, Lin HY, Chen PY, et al. Survival of patients with vancomycin-resistant enterococcus faecium bacteremia treated with conventional or high doses of daptomycin or linezolid is associated with the rate of bacterial clearance. Crit Care Med. 2018;46(10):1634–42. https://doi.org/10.1097/CCM.0000000000003264.
Oldberg K, Thoren R, Nilson B, Gilje P, Inghammar M, Rasmussen M. Short time to blood culture positivity in Enterococcus faecalis infective endocarditis. Eur J Clin Microbiol Infect Dis. 2021;40(8):1657–64. https://doi.org/10.1007/s10096-021-04210-9.
Florent A, Chichmanian RM, Cua E, Pulcini C. Adverse events associated with intravenous fosfomycin. Int J Antimicrob Agents. 2011;37(1):82–3. https://doi.org/10.1016/j.ijantimicag.2010.09.002.
Funk MJ, Westreich D, Wiesen C, Sturmer T, Brookhart MA, Davidian M. Doubly robust estimation of causal effects. Am J Epidemiol. 2011;173(7):761–7. https://doi.org/10.1093/aje/kwq439.
Gustafson P, Greenland S. Misclassification. In: Ahrens W, Pigeot I, editors. Handbook of epidemiology. New York: Springer; 2014. p. 639–58. https://doi.org/10.1007/978-0-387-09834-0_58.
Acknowledgements
The authors thank the Third Core Facility at the National Taiwan University Hospital for technical assistance and support. We thank Dr. Calvin M. Kunin for his critical review of the manuscript.
Funding
This work was partially supported by the Ministry of Science and Technology, Taiwan (110-2628-B-002-059, 110-2326-B-002-003-MY3, and 111-2314-B-002-209), the Ministry of Health and Welfare, Taiwan (MOHW111-TDU-B-211-134002), and National Taiwan University Hospital (NTUH. 110-S4901). The study and the journal’s Rapid Service Fee were funded by the funders.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Tai-Chung Tseng, Yu-Chung Chuang, Jann-Tay Wang, Yee-Chun Chen, and Shan-Chwen Chang conceived and designed the study. Yu-Chung Chuang, Jia-Ling Yang, Chi-Ying Lin, and Sung-His Huang collected the data. Tai-Chung Tseng, Yu-Chung Chuang and Jann-Tay Wang performed data analysis and interpretation. Tai-Chung Tseng and Yu-Chung Chuang wrote the manuscript. All authors reviewed and approved the final version of the report.
Disclosures
Tai-Chung Tseng, Yu-Chung Chuang, Jia-Ling Yang, Chi-Ying Lin, Sung-Hsi Huang, Jann-Tay Wang, Yee-Chun Chen, and Shan-Chwen Chang have nothing to disclose.
Compliance with Ethics Guidelines
The Research Ethics Committee of the NTUH (201606064RINB) approved the study protocol and waived the requirement for informed consent. Since (1) this is a retrospective study and the research would not be practicable to carry out without the waiver, (2) the research has important social value, and (3) the research poses no more than minimal risks to participants, the committee waived the requirement for informed consent. The study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments.
Data Availability
The datasets generated during and analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Tseng, TC., Chuang, YC., Yang, JL. et al. The Combination of Daptomycin with Fosfomycin is More Effective than Daptomycin Alone in Reducing Mortality of Vancomycin-Resistant Enterococcal Bloodstream Infections: A Retrospective, Comparative Cohort Study. Infect Dis Ther 12, 589–606 (2023). https://doi.org/10.1007/s40121-022-00754-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-022-00754-1