Abstract
Nontuberculous mycobacteria (NTM) are a group of atypical bacteria that may cause a spectrum of clinical manifestations, including pulmonary, musculoskeletal, skin and soft tissue, and cardiac infections. Antimycobacterial medication regimens for NTM infections require multiple agents with prolonged treatment courses and are often associated with poor tolerance in patients and suboptimal clinical outcomes. This review summarizes NTM pharmacotherapy, including treatment concepts, preferred medication regimens according to NTM species and site of infection, and emerging treatment methods for difficult-to-treat species.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Mycobacterial infections constitute a substantial worldwide problem because of their ubiquitous nature, inherent drug resistance, and increasing incidence. |
Designing safe and effective nontuberculous mycobacterial infection treatments is challenging because of variability in treatment regimens for different mycobacterial species, infection sites, and disease severity, in addition to medication adverse effects, the prolonged duration of therapy, and common patient comorbid conditions. |
Nontuberculous mycobacterial treatment regimen framework designs generally include the use of at least two drugs, which may include an intensive stage followed by a maintenance stage, and drug choices are often informed by microbiologic data. |
Emerging treatments include tetracycline derivatives, oxazolidinones, combination β-lactams, β-lactamase inhibitors, and phage therapy. |
Introduction
As a human pathogen, Mycobacterium tuberculosis (which causes tuberculosis) is familiar to clinicians, but infections caused by nontuberculous mycobacteria (NTM) may be less well known. NTM most commonly cause pulmonary infections, especially among patients with structural airway disease (e.g., cystic fibrosis and bronchiectasis), but can also cause lymphadenitis, skin and soft tissue infection (SSTI), cardiac infection, bone and joint infections, and disseminated disease [1, 2].
Mycobacteria are aerobic organisms known for their acid-fastness and thick, lipid-rich cell walls [3]. Cell wall impermeability, along with biofilm formation, contributes to the antimicrobial, high-temperature, and disinfectant resistance of mycobacteria [4]. NTM are ubiquitous in the environment and commonly found in water and soil reservoirs. Inhalation and ingestion are the purported leading routes of transmission, and direct person-to-person transmission is rare, unlike that of M. tuberculosis. NTM commonly colonize hot tubs, peat-based potting soils, hemodialysis clinics, fish tanks, and domestic water systems, and have been linked to nosocomial outbreaks [5, 6].
More than 190 NTM species and subspecies have been identified to date, many of which were recently discovered because of advances in culture techniques and molecular diagnostics [7, 8]. Classically, NTM have been divided into rapid (≤ 7 days for mature colony formation in solid media) and slow (> 7 days for colonization) growers. Of the NTM species known to cause human disease, notable rapid growers include Mycobacterium abscessus complex (Mabs, comprising M. abscessus subsp. abscessus, M. abscessus subsp. bolletii, and M. abscessus subsp. massiliense), Mycobacterium fortuitum, and Mycobacterium chelonae. Slow growers known to cause human disease include Mycobacterium avium complex (MAC, comprising Mycobacterium avium, Mycobacterium intracellulare, and Mycobacterium chimaera), Mycobacterium kansasii, and Mycobacterium xenopi. Among both rapid and slow growers, MAC is the most common cause of NTM pulmonary disease in the US, followed by M. kansasii and Mabs [8].
NTM infections appear to be increasing worldwide, with an estimated incidence of 4.1–14.1 cases per 100,000 patient-years [9, 10]. Proposed reasons for this increase include higher air pollution levels, a population increasing in age and comorbid conditions, use of immunosuppressive therapies, and chronic use of inhaled corticosteroids [9, 10]. However, improved diagnostics may also contribute to the apparent increase in NTM infections [6, 11]. Diagnosis of NTM infections is based on a combination of clinical, microbiologic, and radiographic criteria that often involve infectious diseases and/or pulmonary specialists. NTM diagnostic criteria and the decision to initiate treatment are described in detail elsewhere and are considered outside the scope of this pharmacotherapy review [8, 12].
Mycobacterial infections pose a substantial problem because of their widespread prevalence worldwide and their increasing incidence [13]. Treatment of these infections is challenged by the need for multiple antimicrobial agents, varying resistance patterns among mycobacterial species, and long duration of therapy. Here, we review current and emerging approaches to pharmacologic management of NTM infections.
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Current Treatments
Treatment Concepts
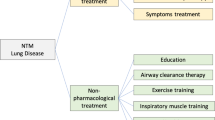
Antimycobacterials are often used in combination with bronchial hygiene/clearance regimens and/or surgical resection to decrease bacterial burden [8]. However, designing safe and effective pharmacotherapy for NTM disease is complex, in part because of treatment regimen variability based on different NTM species, infection sites, and disease severities. Patient-specific factors can increase this complexity, including advanced patient age, body weight extremes, and comorbid conditions. NTM treatment commonly requires the administration of multiple drugs for long durations, accompanied by clinical and laboratory monitoring. In addition to the lack of association between in vitro and in vivo activity for most antimicrobials, systematic controlled trials of first-line treatment regimens, including preferred drug choice, dose, and duration, for various NTM species and diseases are also sparse [12].
Despite these challenges, a general framework for NTM treatment can be useful after reaching a definitive diagnosis and should contain the following elements:
-
1.
At least 2 drugs with likely or confirmed activity against the isolated NTM species should be used. Combination therapy prevents emergent resistance, and certain drug pairings can be synergistic. Disease severity and infection location guide the number of drugs initially used. Up to 4 drugs are commonly used for severe disease, such as fibrocavitary and pulmonary MAC infection, whereas 2 drugs may be used for uncomplicated NTM SSTI.
-
2.
For infections caused by certain species, such as Mabs, treatment may occur in 2 stages: an initial, intensive phase lasting approximately 1–3 months, followed by a prolonged maintenance phase. The initial phase typically contains more drugs and intravenous (IV) administration when indicated. The maintenance phase ideally involves only orally administered drugs and may include as few as 2 drugs. Total treatment duration is guided by clinical response and patient tolerability. Treatment duration is best defined for pulmonary NTM infection as continuing for 12 months after sputum culture conversion to negative [8].
-
3.
Mycobacterium species identification and susceptibility testing guide drug choice. Data showing an association between in vivo clinical outcomes and in vitro susceptibility test results are lacking for most NTM infections, although amikacin and clarithromycin are notable exceptions for MAC and Mabs infections, as well as rifampin for M. kansasii infection. Nevertheless, performing susceptibility testing is generally recommended. Empiric treatment based on usual susceptibility patterns is often initiated for severe and/or disseminated disease while awaiting further microbiologic test results. Macrolides, except when resistance is evident, are a backbone of most NTM treatment regimens [12].
Patients should be counseled about the NTM disease process, goals of therapy, chances of treatment success, medication administration and adverse effects, and laboratory monitoring requirements before committing to NTM therapy. A multidisciplinary team supporting the patient is key to success and may include infectious diseases and pulmonary physicians, advanced practitioners, pharmacists, surgeons, respiratory therapists, nurses, dieticians, microbiologists, and radiologists.
Common Pharmacotherapeutics for MAC
Because MAC infections are overwhelmingly the most common NTM infection type, MAC is the most extensively studied NTM species. Many studies have aimed to determine optimal MAC treatment, and uniform treatment regimens are supported by high-level evidence from randomized, controlled trials. In contrast, treatment recommendations for other species are less extensively investigated. Therefore, the following discussion focuses on MAC treatment recommendations. Other species and active antimicrobial agents are summarized in Table 1.
Guidelines for pulmonary MAC recommend a three-drug regimen consisting of a macrolide (azithromycin or clarithromycin), ethambutol, and a rifamycin (rifampin or rifabutin) [8]. Macrolides are generally regarded as the cornerstone of MAC treatment, and clinical outcomes do not differ between azithromycin and clarithromycin treatment [8]. Azithromycin may be favored more than clarithromycin because azithromycin is associated with fewer drug–drug interactions, better patient tolerance, and a lower pill burden [8].
Hallmark adverse effects of macrolides include gastrointestinal and taste disturbances, QTc prolongation, other cardiac disturbances, and auditory toxicities [8]. Because ethambutol helps prevent the development of macrolide resistance in MAC infections, it is the preferred second agent. Notable adverse effects of ethambutol include ocular toxicity and peripheral neuropathy [8]. The addition of a rifamycin to macrolide/ethambutol combination treatment may provide further protection against macrolide resistance [8]. Rifampin causes many drug–drug interactions by inducing several cytochrome P450 enzymes, most notably CYP3A4, and UDP-galactose transporter. Rifampin also causes red–orange discoloration of bodily secretions (e.g., urine, saliva, perspiration, and tears), hepatotoxicity, and cytopenia [8].
The aminoglycoside amikacin has considerable activity against most NTM species, including MAC. IV amikacin is a potential fourth drug in macrolide-nonsusceptible and cavitary MAC disease, although some experts may recommend an inhaled route for noncavitary disease [8, 14]. Inhaled or IV amikacin are both options for refractory pulmonary disease [8]. Both formulations are associated with a risk of kidney, vestibular, and auditory toxicity, although these risks are considerably lower with inhalation [8, 14]. Medications with activity against MAC and other NTM species are listed in Table 1.
Therapeutic Drug Monitoring
Therapeutic drug monitoring (TDM) is standard for patients receiving IV amikacin because of its drug toxicity risks. An extrapolated peak of 35–45 mcg/mL and trough of less than 5 mcg/mL are targeted with daily administration of IV amikacin (15–20 mg/kg ideal body weight) [8]. Amikacin peaks can be extrapolated with 2- and 6-h postinfusion concentrations to avoid sampling before reaching serum–tissue drug equilibrium. If two serum concentrations are not readily available, an approximate peak can be measured 1 h after the end of infusion, with a peak goal of 25–35 mcg/mL. A 3timesaweek IV amikacin dose of 25 mg/kg, with a peak goal of 65–80 mcg/mL and undetectable trough, is an alternative dosing strategy for pulmonary NTM infection [8, 20].
Serum TDM of oral NTM agents is not well established but is considered in certain circumstances, such as concern for adequate drug absorption (e.g., a history of Roux-en-Y procedure, graft-versus-host disease of the gut, and severe gastrointestinal disease such as Crohn’s disease), pharmacokinetic drug interactions, kidney or liver dysfunction, or a lack of clinical/microbiologic response to therapy. Measuring serum drug levels at two time points, typically at 2–3 h after drug administration and again at 6 h after administration, is generally used with oral TDM to assess for potential delayed drug absorption [15]. Table 2 includes the target Cmax concentrations (i.e., peak blood/serum drug concentrations) for TDM during NTM infection treatment.
Alternative NTM Pharmacotherapy Agents
Treating mycobacterial infections is challenging because of the complexity of the disease and therapeutics used. NTM harbor intrinsic resistance and also quickly acquire resistance, which renders many antimicrobial classes ineffective. Medication tolerability issues with traditional NTM pharmacotherapeutics can arise, especially because long-term treatment courses are generally required. Relatively established alternative NTM agents with distinct pharmacologic considerations are summarized in Table 3. Studies of select alternative pharmacotherapy agents are reviewed in Table 2.
Bedaquiline
Bedaquiline is a diarylquinoline antibiotic that inhibits the proton pump of mycobacterial ATP synthase, which is conserved across mycobacterial species [33]. Bedaquiline is used to treat pulmonary multidrug-resistant tuberculosis [34] and has a dose-dependent bacteriostatic effect against MAC and Mabs in vitro and synergism with clofazimine [35]. Bedaquiline was added as off-label salvage therapy for 10 patients with treatment-refractory MAC or Mabs lung infections. Despite a modest microbiologic and clinical response, no cures were reported [23]. Bedaquiline is administered as a daily 400mg dose for 2 weeks, followed by 200 mg administered 3 times per week (with food) and taken in combination with other drugs for at least 6 months [34].
Bedaquiline is metabolized via CYP3A4, and potential drug interactions should be assessed, particularly with CYP3A4 inducers. Substantially decreased serum concentrations of bedaquiline occur with coadministration of rifamycins [36], which limits the usefulness of bedaquiline for MAC treatment. Extreme caution must be used when substituting a rifamycin with moxifloxacin because both medications can prolong the QTc interval, which increases risk of ventricular arrhythmia [37]. Electrocardiographic monitoring of patients treated with bedaquiline is recommended. Adverse effects include hepatotoxicity, peripheral neuropathy, otovestibular toxicity, anemia, thrombocytopenia, neutropenia, and kidney impairment [37, 38]. A clinical trial comparing bedaquiline with a rifamycin in a treatment regimen for pulmonary MAC infection is ongoing and has an estimated completion date in late 2024 (clinicaltrials.gov, NCT04630145).
Clofazimine
Clofazimine is an antimicrobial phenazine dye that inhibits bacterial proliferation by binding to DNA. It also acts on the bacterial cell wall to generate toxic lysophospholipids [39]. It has in vitro bacteriostatic activity against MAC and Mabs and synergism with amikacin and/or clarithromycin [40]. Substituting rifampin with clofazimine in ethambutol/clarithromycin-containing regimens enhanced bacterial clearance in a murine model of pulmonary MAC infection, and this substitution led to equivalent patient outcomes in retrospective analyses [24, 41]. Addition of clofazimine and/or aerosolized amikacin to drug regimens for macrolide-resistant pulmonary MAC infection is recommended, although prospective studies have not been performed [14]. In a murine model of pulmonary Mabs infection, administration of clofazimine increased bacterial clearance, which was enhanced by the addition of bedaquiline [42]. Retrospective analyses of infection in humans show moderate effectiveness against Mabs when clofazimine is combined with other antibiotics [25].
Adverse effects of clofazimine include discoloration of the conjunctiva and skin (orange to brownish-black) that may not reverse for months to years after discontinuation. Crystallization of the drug in tissues such as the intestinal mucosa may cause abdominal pain with nausea and vomiting and can rarely lead to intestinal obstruction. Clofazimine may increase concentrations of CYP3A4/5 substrates. QTc prolongation is not a major risk but may be enhanced in combination with certain medications; thus, electrocardiographic monitoring is recommended [26]. Aluminum/magnesium antacids may interfere with clofazimine oral absorption. Clofazimine (50–100 mg) should be taken 2 times daily with a meal and separately from aluminum/magnesium-containing antacids.
Rifabutin
Rifabutin, similar to rifampin, is a semisynthetic rifamycin antibiotic that inhibits the bacterial DNA-dependent RNA polymerase, which inhibits transcription of bacterial RNA and leads to cell death. Rifabutin has in vitro activity against most NTM species and is recommended for pulmonary MAC, M. kansasii, and Mycobacterium xenopi infections [8]. In a preclinical murine model, daily rifabutin (10 mg/kg) for 10 days reduced Mabs concentration by 1 log, which is similar to that with clarithromycin [43]. Rifabutin is usually orally administered as a daily 150 to 300mg dose or 3 times a week at 300 mg, depending on indication and potential drug–drug interactions [8].
Rifabutin adverse effects include orange-brown discoloration of body fluids, rash, gastrointestinal symptoms (e.g., nausea and diarrhea), and neutropenia [44]. Rifabutin induces CYP3A4 activity and therefore reduces the concentrations of many drugs, although typically to a lesser extent than does rifampin. However, rifabutin is also metabolized by CYP3A4 and thus has greater potential for bidirectional drug interactions than does rifampin [44].
Linezolid
Linezolid is an oxazolidinone antibiotic that binds to bacterial 23S ribosomal RNA of the 50S subunit to inhibit bacterial protein synthesis and has in vitro activity against most mycobacterial species [45,46,47]. Clinical outcomes data in humans are most readily available for Mabs and M. chelonae infections [27, 28, 48]. Linezolid is also considered an alternative treatment option for MAC [28]. Long-term tolerability is limited by hematologic and neurologic toxicities, including pancytopenias and peripheral and optic neuropathies. A daily 600mg dose of linezolid is often used for mycobacterial infections to improve long-term tolerability, although outcomes studies directly comparing 1- vs. 2-time daily dosing are not available [49]. Other methods to limit drug toxicities, including pyridoxine (vitamin B6) supplementation, were not beneficial [28].
Linezolid has reversible, weak inhibitory properties against monoamine oxidase, which led to labeling precautions for serotonin syndrome when it is combined with other serotonergic agents and for hypertensive crisis with tyramine-rich foods. Serotonin syndrome risk, although low overall, may increase with concomitant administration of serotonergic agents and according to their serotonergic potential [50,51,52].
Emerging Treatments
NTM treatment outcomes remain suboptimal with established regimens. This highlights the need for developing novel therapeutics and repurposing currently approved therapeutics for antimycobacterial management. Studies of such emerging treatments are reviewed in Table 2.
Tetracycline Derivatives
Tetracyclines reversibly bind to the bacterial 30S ribosomal subunit and inhibit protein synthesis. Tigecycline is a third-generation tetracycline approved for complicated skin and intra-abdominal infections. It also has been studied for its efficacy against NTM disease and is currently recommended as a preferred IV antimycobacterial agent for Mabs in multiple NTM treatment guidelines [8, 53,54,55]. However, tigecycline use is associated with dose-limiting nausea and vomiting and has a boxed warning for increased risk of death. This boxed warning resulted from outcomes in patients treated for bacterial bloodstream infections [56]. Tigecycline is available only as an IV formulation because of its poor oral absorption [57].
Omadacycline was recently approved for bacterial pneumonia and SSTI, and eravacycline was approved for complicated intra-abdominal infections. Both drugs are better tolerated than their predecessor tigecycline [58] and are attractive therapeutic options for NTM disease. Two in vitro studies reported eravacycline activity against NTM [59, 60], and several in vitro [60,61,62,63,64] and in vivo case reports/series described the use of omadacycline [29,30,31, 65] in combination therapy for Mabs infection. Omadacycline is under investigation in a phase 2 clinical trial for NTM infection treatment (clinicaltrials.gov, NCT04922554).
Omadacycline is the only novel tetracycline derivative available as an oral formulation. Administering food 2 h before oral omadacycline reduced omadacycline concentrations by 40–63% in clinical trials [66]. Therefore, fasting is recommended for oral omadacycline administration, with no food or drink, except water, consumed 4 h before or 2 h after administration. Absorption is further impaired by antacids containing polyvalent cations, such as calcium or aluminum. Dairy products, antacids, and multivitamins should not be consumed for at least 4 h after omadacycline administration. Although the approved dosing for oral omadacycline includes a loading dose, omitting the loading dose in NTM treatment may increase gastrointestinal tolerability [29]. Eravacycline is a CYP3A4 substrate that can interact with CYP3A4 inducers such as rifampin. Because both omadacycline and eravacycline depress plasma prothrombin activity, concomitant anticoagulant treatment may require dose reduction.
Tedizolid
Tedizolid is a novel oxazolidinone antibiotic that inhibits bacterial protein synthesis in a similar mechanism to that of linezolid. In vitro activity of tedizolid is reported for many slow-growing and rapid-growing NTM species, including MAC, M. kansasii, Mabs, M. chelonae, M. fortuitum, Mycobacterium marinum, Mycobacterium smegmatis group, and Mycobacterium immunogenum. Minimum inhibitory concentrations (MICs) for tedizolid are generally comparable to or several dilutions lower than those of linezolid [67,68,69,70,71]. Clinical evidence for tedizolid use for NTM treatment is limited. Discrepant effectiveness and safety findings of tedizolid in comparison with linezolid are reported [32, 72, 73]. Two case reports describe successful tedizolid use for NTM infection in patients with previous linezolid-induced cytopenia [72, 73]. Tedizolid has greater antibacterial potency, better pharmacokinetic/pharmacodynamic profiles, and lower hematologic and neurologic toxicity than does linezolid [74, 75]. The relatively weak monoamine oxidase inhibition and poor central nervous system penetration of tedizolid may also lead to fewer drug interactions with serotonergic agents [76, 77]. The improved long-term safety, high bioavailability, and daily dosing regimen are favorable factors for tedizolid use in NTM therapy.
Combination β-Lactams
Dual β-lactam combination therapy is an evolving area of interest, in which two β-lactam agents are used to induce synergistic bactericidal activity. Such combinations are most extensively studied for Mabs infections, which often have limited treatment options and poorer clinical outcomes than infections with other NTM species, with culture conversion rates of 25–42% among macrolide-resistant isolates [16]. In vitro synergistic activity is reported for several combinations, including imipenem/ceftaroline, ceftazidime/ceftaroline, imipenem/cefoxitin, imipenem/cefdinir, and imipenem/doripenem [78,79,80,81,82]. Imipenem/ceftaroline synergism was also replicated in an in vivo mouse model of pulmonary Mabs infection [83].
Several possible mechanisms of synergy have been proposed. Both cefoxitin and imipenem are slowly hydrolyzed by the Mabs class A β-lactamase (BlaMab). In the absence of readily available inhibitors of BlaMab, dual β-lactam combination therapy may overwhelm BlaMab to allow more drug to reach the target binding site. Cephalosporins and carbapenems have different binding affinities to Mabs l,d-transpeptidase proteins LdtMab1–5 [84, 85]. These different affinities may provide greater saturation of molecular targets with both drugs than with either agent alone. This mechanism is analogous to ampicillin and third-generation cephalosporin synergy against Enterococcus faecalis infection [86]. Molecular simulation studies suggest that LdtMab2 undergoes ligand-induced conformational changes in which initial imipenem docking may alter or open additional binding sites for ceftaroline [85].
β-Lactamase Inhibitors
Although imipenem and cefoxitin are often recommended as first-line IV NTM therapy [8], the presence of BlaMab renders them inactive [87]. However, in vitro models suggest that novel β-lactamase inhibitors may block BlaMab and restore β-lactam activity. Relebactam and avibactam (diazabicyclooctane β-lactamase inhibitors) and vaborbactam (boronic acid β-lactamase inhibitor) have been studied in various combinations. Relebactam and vaborbactam (4 mcg/mL) reduce the MIC of M abscessus subsp. abscessus when combined with oral and IV carbapenems and cephalosporins [88]. Another in vitro study assessed different ratios of β-lactam to β-lactamase inhibitor for efficacy against M abscessus subsp. abscessus, M abscessus subsp. bolletii, and M abscessus subsp. massiliense. Although the currently available dose/ratio of imipenem/relebactam was optimized, no combination of ceftazidime/avibactam was effective. However, triple-combination imipenem, relebactam, and meropenem resulted in the lowest MICs and minimum bactericidal concentrations for all three subspecies [89]. Other studies have shown that the addition of ampicillin to imipenem/relebactam, and to a lesser extent to ceftazidime/avibactam, can result in lower Mabs MICs [89, 90]. Currently, all three β-lactamase inhibitors are available only in coformulations with β-lactams: imipenem/cilastatin with relebactam, ceftazidime with avibactam, and meropenem with vaborbactam. To achieve potentially active combinations that include meropenem or ampicillin, the patient must also receive noncontributory β-lactams, such as ceftazidime.
Thus far, β-lactam and β-lactamase inhibitor combinations have been studied only in vitro, and the optimal combination, dose, and tolerability in humans are unknown. The risk of bone marrow suppression with long-term β-lactam use is a theoretical concern and may be exacerbated by overlapping drug toxicity profiles. Therefore, caution is needed when using these combinations in clinical practice.
Phage Therapy
Mycobacteriophages are viruses that infect mycobacterial hosts. Phage therapy uses bacteriophages to specifically target and lyse pathogenic bacteria [91] and is an emerging strategy to combat multidrug-resistant infections, including mycobacterial infections [92]. Successful phage therapy for nonmycobacterial infections has been described [93].
Dedrick et al. [91] reported a case of a 15-year-old patient with cystic fibrosis who had a disseminated Mabs infection after lung transplant and was successfully treated with phage therapy. A 2022 report describes the use of phage therapy in 20 patients with drug-resistant mycobacterial disease [94]. Therapy was administered by IV infusion, aerosolization, or both. No adverse reactions were reported, and favorable clinical or microbiological responses occurred in 11 patients. These data suggest that phage therapy is a strategy for NTM infections without other viable treatment options [94, 95]. Challenges for the broader use of this therapy include the limited availability of therapeutically useful bacteriophages, variability in bacteriophage susceptibility among clinical isolates, unclear dosing and route of administration, lack of understanding of the added benefit of cotreatment with antimicrobials or antiinflammatory agents, and the need to counter bacteriophage resistance. More research is needed to establish best practices for using this evolving technology.
Experimental and Preclinical Therapies
The repurposing of commercially available antibiotics with in vitro antimycobacterial activity has expanded the available therapeutic options. In addition, several antimycobacterial agents are currently undergoing first-in-human testing in phase I and II clinical trials [96]. Addition of inhaled nitric oxide or granulocyte–macrophage colony-stimulating factor has been used as adjunctive therapy for patients with pulmonary NTM infections [97, 98]. Nonpharmacologic interventions, such as host modulation with stem cells, photodynamic therapy, antibiofilm therapy, nanoparticles, vaccines, and antimicrobial peptides, are also currently in development [99].
Conclusion
NTM infections are increasingly common and pose a substantial problem worldwide. Strategies used to treat NTM infections include multidrug therapy, modification of existing antibiotic classes, and phage therapy. Although further evidence is needed to establish novel treatments as a standard of care, a multidisciplinary management approach can optimize treatment for the breadth of NTM infections.
References
Griffith DE, Aksamit TR. Managing Mycobacterium avium complex lung disease with a little help from my friend. Chest. 2021;159(4):1372–81. https://doi.org/10.1016/j.chest.2020.10.031.
Winthrop KL, McNelley E, Kendall B, et al. Pulmonary nontuberculous mycobacterial disease prevalence and clinical features: an emerging public health disease. Am J Respir Crit Care Med. 2010;182(7):977–82. https://doi.org/10.1164/rccm.201003-0503OC.
Chan ED, Iseman MD. Underlying host risk factors for nontuberculous mycobacterial lung disease. Semin Respir Crit Care Med. 2013;34(1):110–23. https://doi.org/10.1055/s-0033-1333573.
Jarlier V, Nikaido H. Mycobacterial cell wall: structure and role in natural resistance to antibiotics. FEMS Microbiol Lett. 1994;123(1–2):11–8. https://doi.org/10.1111/j.1574-6968.1994.tb07194.x.
Falkinham JO. Growth in catheter biofilms and antibiotic resistance of Mycobacterium avium. J Med Microbiol. 2007;56(Pt 2):250–4. https://doi.org/10.1099/jmm.0.46935-0.
van Ingen J, Hoefsloot W, Dekhuijzen PN, Boeree MJ, van Soolingen D. The changing pattern of clinical Mycobacterium avium isolation in the Netherlands. Int J Tuberc Lung Dis. 2010;14(9):1176–80. https://www.ncbi.nlm.nih.gov/pubmed/20819265.
Johnson MM, Odell JA. Nontuberculous mycobacterial pulmonary infections. J Thorac Dis. 2014;6(3):210–20. https://doi.org/10.3978/j.issn.2072-1439.2013.12.24.
Daley CL, Iaccarino JM, Lange C, et al. Treatment of nontuberculous mycobacterial pulmonary disease: an official ATS/ERS/ESCMID/IDSA clinical practice guideline. Eur Respir J. 2020. https://doi.org/10.1183/13993003.00535-2020.
Kirschner RA Jr, Parker BC, Falkinham JO 3rd. Epidemiology of infection by nontuberculous mycobacteria. Mycobacterium avium, Mycobacterium intracellulare, and Mycobacterium scrofulaceum in acid, brown-water swamps of the southeastern United States and their association with environmental variables. Am Rev Respir Dis. 1992;145(Pt 1):271–5. https://doi.org/10.1164/ajrccm/145.2_Pt_1.271.
Larsson LO, Polverino E, Hoefsloot W, et al. Pulmonary disease by non-tuberculous mycobacteria—clinical management, unmet needs and future perspectives. Expert Rev Respir Med. 2017;11(12):977–89. https://doi.org/10.1080/17476348.2017.1386563.
Al-Houqani M, Jamieson F, Mehta M, Chedore P, May K, Marras TK. Aging, COPD, and other risk factors do not explain the increased prevalence of pulmonary Mycobacterium avium complex in Ontario. Chest. 2012;141(1):190–7. https://doi.org/10.1378/chest.11-0089.
Pennington KM, Vu A, Challener D, et al. Approach to the diagnosis and treatment of non-tuberculous mycobacterial disease. J Clin Tuberc Other Mycobact Dis. 2021;24:100244. https://doi.org/10.1016/j.jctube.2021.100244.
Honda JR, Virdi R, Chan ED. Global environmental nontuberculous mycobacteria and their contemporaneous man-made and natural niches. Front Microbiol. 2018;9:2029. https://doi.org/10.3389/fmicb.2018.02029.
Kwon YS, Koh WJ, Daley CL. Treatment of Mycobacterium avium complex pulmonary disease. Tuberc Respir Dis (Seoul). 2019;82(1):15–26. https://doi.org/10.4046/trd.2018.0060.
Peloquin C. The role of therapeutic drug monitoring in mycobacterial infections. Microbiol Spectr. 2017. https://doi.org/10.1128/microbiolspec.TNMI7-0029-2016.
Griffith DE, Daley CL. Treatment of Mycobacterium abscessus pulmonary disease. Chest. 2022;161(1):64–75. https://doi.org/10.1016/j.chest.2021.07.035.
Kasperbauer SH, De Groote MA. The treatment of rapidly growing mycobacterial infections. Clin Chest Med. 2015;36(1):67–78. https://doi.org/10.1016/j.ccm.2014.10.004.
Philley JV, Griffith DE. Treatment of slowly growing mycobacteria. Clin Chest Med. 2015;36(1):79–90. https://doi.org/10.1016/j.ccm.2014.10.005.
van Ingen J, Egelund EF, Levin A, et al. The pharmacokinetics and pharmacodynamics of pulmonary Mycobacterium avium complex disease treatment. Am J Respir Crit Care Med. 2012;186(6):559–65. https://doi.org/10.1164/rccm.201204-0682OC.
Peloquin CA, Berning SE, Nitta AT, et al. Aminoglycoside toxicity: daily versus thrice-weekly dosing for treatment of mycobacterial diseases. Clin Infect Dis. 2004;38(11):1538–44. https://doi.org/10.1086/420742.
Egelund EF, Fennelly KP, Peloquin CA. Medications and monitoring in nontuberculous mycobacteria infections. Clin Chest Med. 2015;36(1):55–66. https://doi.org/10.1016/j.ccm.2014.11.001.
Shulha JA, Escalante P, Wilson JW. Pharmacotherapy approaches in nontuberculous mycobacteria infections. Mayo Clin Proc. 2019;94(8):1567–81. https://doi.org/10.1016/j.mayocp.2018.12.011.
Philley JV, Wallace RJ Jr, Benwill JL, et al. Preliminary results of bedaquiline as salvage therapy for patients with nontuberculous mycobacterial lung disease. Chest. 2015;148(2):499–506. https://doi.org/10.1378/chest.14-2764.
Jarand J, Davis JP, Cowie RL, Field SK, Fisher DA. Long-term follow-up of Mycobacterium avium complex lung disease in patients treated with regimens including Clofazimine and/or Rifampin. Chest. 2016;149(5):1285–93. https://doi.org/10.1378/chest.15-0543.
Yang B, Jhun BW, Moon SM, et al. Clofazimine-containing regimen for the treatment of Mycobacterium abscessus lung disease. Antimicrob Agents Chemother. 2017. https://doi.org/10.1128/AAC.02052-16.
Martiniano SL, Wagner BD, Levin A, Nick JA, Sagel SD, Daley CL. Safety and effectiveness of clofazimine for primary and refractory nontuberculous mycobacterial infection. Chest. 2017;152(4):800–9. https://doi.org/10.1016/j.chest.2017.04.175.
Parize P, Hamelin A, Veziris N, et al. Induction therapy with linezolid/clarithromycin combination for Mycobacterium chelonae skin infections in immunocompromised hosts. J Eur Acad Dermatol Venereol. 2016;30(1):101–5. https://doi.org/10.1111/jdv.12965.
Winthrop KL, Ku JH, Marras TK, et al. The tolerability of linezolid in the treatment of nontuberculous mycobacterial disease. Eur Respir J. 2015;45(4):1177–9. https://doi.org/10.1183/09031936.00169114.
Pearson JC, Dionne B, Richterman A, et al. Omadacycline for the treatment of Mycobacterium abscessus disease: a case series. Open Forum Infect Dis. 2020;7(10):ofaa415. https://doi.org/10.1093/ofid/ofaa415.
Morrisette T, Alosaimy S, Philley JV, et al. Preliminary, real-world, multicenter experience with omadacycline for Mycobacterium abscessus infections. Open Forum Infect Dis. 2021;8(2):ofab002. https://doi.org/10.1093/ofid/ofab002.
Duah M, Beshay M. Omadacycline in first-line combination therapy for pulmonary Mycobacterium abscessus infection: a case series. Int J Infect Dis. 2022;122:953–6. https://doi.org/10.1016/j.ijid.2022.06.061.
Poon YK, La Hoz RM, Hynan LS, Sanders J, Monogue ML. Tedizolid vs linezolid for the treatment of nontuberculous mycobacteria infections in solid organ transplant recipients. Open Forum Infect Dis. 2021;8(4):ofab093. https://doi.org/10.1093/ofid/ofab093.
Andries K, Verhasselt P, Guillemont J, et al. A diarylquinoline drug active on the ATP synthase of Mycobacterium tuberculosis. Science. 2005;307(5707):223–7. https://doi.org/10.1126/science.1106753.
Conradie F, Diacon AH, Ngubane N, et al. Treatment of Highly drug-resistant pulmonary tuberculosis. N Engl J Med. 2020;382(10):893–902. https://doi.org/10.1056/NEJMoa1901814.
Ruth MM, Sangen JJN, Remmers K, et al. A bedaquiline/clofazimine combination regimen might add activity to the treatment of clinically relevant non-tuberculous mycobacteria. J Antimicrob Chemother. 2019;74(4):935–43. https://doi.org/10.1093/jac/dky526.
Svensson EM, Murray S, Karlsson MO, Dooley KE. Rifampicin and rifapentine significantly reduce concentrations of bedaquiline, a new anti-TB drug. J Antimicrob Chemother. 2015;70(4):1106–14. https://doi.org/10.1093/jac/dku504.
Borisov SE, Dheda K, Enwerem M, et al. Effectiveness and safety of bedaquiline-containing regimens in the treatment of MDR- and XDR-TB: a multicentre study. Eur Respir J. 2017. https://doi.org/10.1183/13993003.00387-2017.
Division of Tuberculosis Elimination, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. Provisional CDC guidelines for the use and safety monitoring of bedaquiline fumarate (Sirturo) for the treatment of multidrug-resistant tuberculosis. MMWR Morb Mortal Wkly Rep. 2013;62(RR09):1–12. https://www.cdc.gov/mmwr/preview/mmwrhtml/rr6209a1.htm.
Arbiser JL, Moschella SL. Clofazimine: a review of its medical uses and mechanisms of action. J Am Acad Dermatol. 1995;32(2 Pt 1):241–7. https://doi.org/10.1016/0190-9622(95)90134-5.
Ferro BE, Meletiadis J, Wattenberg M, et al. Clofazimine prevents the regrowth of Mycobacterium abscessus and Mycobacterium avium type strains exposed to amikacin and clarithromycin. Antimicrob Agents Chemother. 2016;60(2):1097–105. https://doi.org/10.1128/AAC.02615-15.
Lee JM, Park J, Choi S, et al. A clofazimine-containing regimen confers improved treatment outcomes in macrophages and in a murine model of chronic progressive pulmonary infection caused by the Mycobacterium avium complex. Front Microbiol. 2020;11:626216. https://doi.org/10.3389/fmicb.2020.626216.
Obregon-Henao A, Arnett KA, Henao-Tamayo M, et al. Susceptibility of Mycobacterium abscessus to antimycobacterial drugs in preclinical models. Antimicrob Agents Chemother. 2015;59(11):6904–12. https://doi.org/10.1128/AAC.00459-15.
Dick T, Shin SJ, Koh WJ, Dartois V, Gengenbacher M. Rifabutin is active against Mycobacterium abscessus in mice. Antimicrob Agents Chemother. 2020. https://doi.org/10.1128/AAC.01943-19.
Crabol Y, Catherinot E, Veziris N, Jullien V, Lortholary O. Rifabutin: where do we stand in 2016? J Antimicrob Chemother. 2016;71(7):1759–71. https://doi.org/10.1093/jac/dkw024.
Alcala L, Ruiz-Serrano MJ, Perez-Fernandez Turegano C, et al. In vitro activities of linezolid against clinical isolates of Mycobacterium tuberculosis that are susceptible or resistant to first-line antituberculous drugs. Antimicrob Agents Chemother. 2003;47(1):416–7. https://doi.org/10.1128/AAC.47.1.416-417.2003.
Brown-Elliott BA, Crist CJ, Mann LB, Wilson RW, Wallace RJ Jr. In vitro activity of linezolid against slowly growing nontuberculous mycobacteria. Antimicrob Agents Chemother. 2003;47(5):1736–8. https://doi.org/10.1128/AAC.47.5.1736-1738.2003.
Wallace RJ Jr, Brown-Elliott BA, Ward SC, Crist CJ, Mann LB, Wilson RW. Activities of linezolid against rapidly growing mycobacteria. Antimicrob Agents Chemother. 2001;45(3):764–7. https://doi.org/10.1128/AAC.45.3.764-767.2001.
Brown-Elliott BA, Wallace RJ Jr, Blinkhorn R, Crist CJ, Mann LB. Successful treatment of disseminated Mycobacterium chelonae infection with linezolid. Clin Infect Dis. 2001;33(8):1433–4. https://doi.org/10.1086/322523.
Graciaa DS, Kipiani M, Magee MJ, et al. Linezolid exposure is associated with cytopenias in patients treated for multidrug-resistant tuberculosis. Antimicrob Agents Chemother. 2022. https://doi.org/10.1128/aac.00408-22.
Butterfield JM, Lawrence KR, Reisman A, Huang DB, Thompson CA, Lodise TP. Comparison of serotonin toxicity with concomitant use of either linezolid or comparators and serotonergic agents: an analysis of phase III and IV randomized clinical trial data. J Antimicrob Chemother. 2012;67(2):494–502. https://doi.org/10.1093/jac/dkr467.
Gatti M, Raschi E, De Ponti F. Serotonin syndrome by drug interactions with linezolid: clues from pharmacovigilance-pharmacokinetic/pharmacodynamic analysis. Eur J Clin Pharmacol. 2021;77(2):233–9. https://doi.org/10.1007/s00228-020-02990-1.
Lodise TP, Patel N, Rivera A, et al. Comparative evaluation of serotonin toxicity among veterans affairs patients receiving linezolid and vancomycin. Antimicrob Agents Chemother. 2013;57(12):5901–11. https://doi.org/10.1128/AAC.00921-13.
Floto RA, Olivier KN, Saiman L, et al. US Cystic Fibrosis Foundation and European Cystic Fibrosis Society consensus recommendations for the management of non-tuberculous mycobacteria in individuals with cystic fibrosis. Thorax. 2016;71(Suppl 1):i1-22. https://doi.org/10.1136/thoraxjnl-2015-207360.
Haworth CS, Banks J, Capstick T, et al. British Thoracic Society guidelines for the management of non-tuberculous mycobacterial pulmonary disease (NTM-PD). Thorax. 2017;72(Suppl 2):ii1–64. https://doi.org/10.1136/thoraxjnl-2017-210927.
Longworth SA, Daly JS, AST Infectious Diseases Community of Practice. Management of infections due to nontuberculous mycobacteria in solid organ transplant recipients—guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin Transplant. 2019;33(9):e13588. https://doi.org/10.1111/ctr.13588.
Prasad P, Sun J, Danner RL, Natanson C. Excess deaths associated with tigecycline after approval based on noninferiority trials. Clin Infect Dis. 2012;54(12):1699–709. https://doi.org/10.1093/cid/cis270.
Stein GE, Craig WA. Tigecycline: a critical analysis. Clin Infect Dis. 2006;43(4):518–24. https://doi.org/10.1086/505494.
Gotfried MH, Horn K, Garrity-Ryan L, et al. Comparison of omadacycline and tigecycline pharmacokinetics in the plasma, epithelial lining fluid, and alveolar cells of healthy adult subjects. Antimicrob Agents Chemother. 2017. https://doi.org/10.1128/AAC.01135-17.
Chew KL, Octavia S, Go J, et al. In vitro susceptibility of Mycobacterium abscessus complex and feasibility of standardizing treatment regimens. J Antimicrob Chemother. 2021;76(4):973–8. https://doi.org/10.1093/jac/dkaa520.
Kaushik A, Ammerman NC, Martins O, Parrish NM, Nuermberger EL. In vitro activity of new tetracycline analogs omadacycline and eravacycline against drug-resistant clinical isolates of Mycobacterium abscessus. Antimicrob Agents Chemother. 2019. https://doi.org/10.1128/AAC.00470-19.
Bax HI, de Vogel CP, Mouton JW, de Steenwinkel JEM. Omadacycline as a promising new agent for the treatment of infections with Mycobacterium abscessus. J Antimicrob Chemother. 2019;74(10):2930–3. https://doi.org/10.1093/jac/dkz267.
Brown-Elliott BA, Wallace RJ Jr. In vitro susceptibility testing of omadacycline against nontuberculous mycobacteria. Antimicrob Agents Chemother. 2021. https://doi.org/10.1128/AAC.01947-20.
Gumbo T, Cirrincione K, Srivastava S. Repurposing drugs for treatment of Mycobacterium abscessus: a view to a kill. J Antimicrob Chemother. 2020;75(5):1212–7. https://doi.org/10.1093/jac/dkz523.
Shoen C, Benaroch D, Sklaney M, Cynamon M. In vitro activities of omadacycline against rapidly growing mycobacteria. Antimicrob Agents Chemother. 2019. https://doi.org/10.1128/AAC.02522-18.
Minhas R, Sharma S, Kundu S. Utilizing the promise of omadacycline in a resistant, non-tubercular mycobacterial pulmonary infection. Cureus. 2019;11(7):e5112. https://doi.org/10.7759/cureus.5112.
Tzanis E, Manley A, Villano S, Tanaka SK, Bai S, Loh E. Effect of food on the bioavailability of omadacycline in healthy participants. J Clin Pharmacol. 2017;57(3):321–7. https://doi.org/10.1002/jcph.814.
Brown-Elliott BA, Wallace RJ Jr. In vitro susceptibility testing of tedizolid against nontuberculous mycobacteria. J Clin Microbiol. 2017;55(6):1747–54. https://doi.org/10.1128/JCM.00274-17.
Compain F, Soroka D, Heym B, et al. In vitro activity of tedizolid against the Mycobacterium abscessus complex. Diagn Microbiol Infect Dis. 2018;90(3):186–9. https://doi.org/10.1016/j.diagmicrobio.2017.11.001.
Ruth MM, Koeken V, Pennings LJ, et al. Is there a role for tedizolid in the treatment of non-tuberculous mycobacterial disease? J Antimicrob Chemother. 2020;75(3):609–17. https://doi.org/10.1093/jac/dkz511.
Wen S, Gao X, Zhao W, et al. Comparison of the in vitro activity of linezolid, tedizolid, sutezolid, and delpazolid against rapidly growing mycobacteria isolated in Beijing China. Int J Infect Dis. 2021;109:253–60. https://doi.org/10.1016/j.ijid.2021.06.055.
Marfil E, Ruiz P, Martinez-Martinez L, Causse M. Comparative study of in vitro activity of tedizolid and linezolid against Mycobacterium avium complex. J Glob Antimicrob Resist. 2022;30:395–8. https://doi.org/10.1016/j.jgar.2022.07.012.
Shaw TD, Smyth M, Turner G, Hunter M. Prolonged tedizolid use in cutaneous non-tuberculous mycobacterial infection. J Clin Tuberc Other Mycobact Dis. 2021;24:100261. https://doi.org/10.1016/j.jctube.2021.100261.
Yuste JR, Berto J, Del Pozo JL, Leiva J. Prolonged use of tedizolid in a pulmonary non-tuberculous mycobacterial infection after linezolid-induced toxicity. J Antimicrob Chemother. 2017;72(2):625–8. https://doi.org/10.1093/jac/dkw484.
Mensa Vendrell M, Tasias-Pitarch M, Salavert Lletí M, et al. Safety and tolerability of more than six days of tedizolid treatment. Antimicrob Agents Chemother. 2020;64(7):e00356-e420. https://doi.org/10.1128/AAC.00356-20.
Morrisette T, Molina KC, Da Silva B, et al. Real-world use of tedizolid phosphate for 28 days or more: a case series describing tolerability and clinical success. Open Forum Infect Dis. 2022;9(6):ofac028. https://doi.org/10.1093/ofid/ofac028.
Ferrandez O, Urbina O, Grau S. Critical role of tedizolid in the treatment of acute bacterial skin and skin structure infections. Drug Des Devel Ther. 2017;11:65–82. https://doi.org/10.2147/DDDT.S84667.
Flanagan S, Bartizal K, Minassian SL, Fang E, Prokocimer P. In vitro, in vivo, and clinical studies of tedizolid to assess the potential for peripheral or central monoamine oxidase interactions. Antimicrob Agents Chemother. 2013;57(7):3060–6. https://doi.org/10.1128/AAC.00431-13.
Pandey R, Chen L, Manca C, et al. Dual beta-lactam combinations highly active against Mycobacterium abscessus complex in vitro. MBio. 2019. https://doi.org/10.1128/mBio.02895-18.
Lefebvre AL, Dubee V, Cortes M, Dorchene D, Arthur M, Mainardi JL. Bactericidal and intracellular activity of beta-lactams against Mycobacterium abscessus. J Antimicrob Chemother. 2016;71(6):1556–63. https://doi.org/10.1093/jac/dkw022.
Nguyen DC, Dousa KM, Kurz SG, et al. “One-two punch”: synergistic ss-lactam combinations for Mycobacterium abscessus and target redundancy in the inhibition of peptidoglycan synthesis enzymes. Clin Infect Dis. 2021;73(8):1532–6. https://doi.org/10.1093/cid/ciab535.
Story-Roller E, Galanis C, Lamichhane G. Beta-lactam combinations that exhibit synergy against Mycobacteroides abscessus clinical isolates. Antimicrob Agents Chemother. 2021. https://doi.org/10.1128/AAC.02545-20.
Story-Roller E, Maggioncalda EC, Lamichhane G. Select beta-lactam combinations exhibit synergy against Mycobacterium abscessus in vitro. Antimicrob Agents Chemother. 2019. https://doi.org/10.1128/AAC.02613-18.
Story-Roller E, Maggioncalda EC, Lamichhane G. Synergistic efficacy of beta-lactam combinations against Mycobacterium abscessus pulmonary infection in mice. Antimicrob Agents Chemother. 2019. https://doi.org/10.1128/AAC.00614-19.
Kumar P, Chauhan V, Silva JRA, et al. Mycobacterium abscessus l, d-transpeptidases are susceptible to inactivation by carbapenems and cephalosporins but not penicillins. Antimicrob Agents Chemother. 2017. https://doi.org/10.1128/AAC.00866-17.
Dousa KM, Kurz SG, Taracila MA, et al. Insights into the l, d-transpeptidases and d, d-carboxypeptidase of Mycobacterium abscessus: ceftaroline, imipenem, and novel diazabicyclooctane inhibitors. Antimicrob Agents Chemother. 2020;64(8):e00098-e120. https://doi.org/10.1128/AAC.00098-20.
Mainardi JL, Gutmann L, Acar JF, Goldstein FW. Synergistic effect of amoxicillin and cefotaxime against Enterococcus faecalis. Antimicrob Agents Chemother. 1995;39(9):1984–7. https://doi.org/10.1128/AAC.39.9.1984.
Soroka D, Dubee V, Soulier-Escrihuela O, et al. Characterization of broad-spectrum Mycobacterium abscessus class A beta-lactamase. J Antimicrob Chemother. 2014;69(3):691–6. https://doi.org/10.1093/jac/dkt410.
Kaushik A, Ammerman NC, Lee J, et al. In vitro activity of the new beta-lactamase inhibitors relebactam and vaborbactam in combination with beta-lactams against Mycobacterium abscessus complex clinical isolates. Antimicrob Agents Chemother. 2019. https://doi.org/10.1128/AAC.02623-18.
Harrison J, Weaver JA, Desai M, Cox JAG. In vitro efficacy of relebactam versus avibactam against Mycobacterium abscessus complex. Cell Surf. 2021;7:100064. https://doi.org/10.1016/j.tcsw.2021.100064.
Lopeman RC, Harrison J, Rathbone DL, Desai M, Lambert PA, Cox JAG. Effect of amoxicillin in combination with imipenem-relebactam against Mycobacterium abscessus. Sci Rep. 2020;10(1):928. https://doi.org/10.1038/s41598-020-57844-8.
Dedrick RM, Guerrero-Bustamante CA, Garlena RA, et al. Engineered bacteriophages for treatment of a patient with a disseminated drug-resistant Mycobacterium abscessus. Nat Med. 2019;25(5):730–3. https://doi.org/10.1038/s41591-019-0437-z.
Sulakvelidze A, Alavidze Z, Morris JG Jr. Bacteriophage therapy. Antimicrob Agents Chemother. 2001;45(3):649–59. https://doi.org/10.1128/AAC.45.3.649-659.2001.
Schooley RT, Biswas B, Gill JJ, et al. Development and use of personalized bacteriophage-based therapeutic cocktails to treat a patient with a disseminated resistant Acinetobacter baumannii infection. Antimicrob Agents Chemother. 2017;61(10):e00954-e1017. https://doi.org/10.1128/AAC.00954-17.
Dedrick RM, Smith BE, Cristinziano M, et al. Phage therapy of mycobacterium infections: compassionate-use of phages in twenty patients with drug-resistant mycobacterial disease. Clin Infect Dis. 2022. https://doi.org/10.1093/cid/ciac453.
Dedrick RM, Smith BE, Garlena RA, et al. Mycobacterium abscessus strain morphotype determines phage susceptibility, the repertoire of therapeutically useful phages, and phage resistance. MBio. 2021. https://doi.org/10.1128/mBio.03431-20.
World Health Organization. Antibacterial agents in clinical and preclinical development: an overview and analysis. 2021. https://www.who.int/publications/i/item/9789240047655. 5 Dec 2022.
Goldbart A, Gatt D, Golan TI. Non-tuberculous mycobacteria infection treated with intermittently inhaled high-dose nitric oxide. BMJ Case Rep. 2021. https://doi.org/10.1136/bcr-2021-243979.
Scott JP, Ji Y, Kannan M, Wylam ME. Inhaled granulocyte-macrophage colony-stimulating factor for Mycobacterium abscessus in cystic fibrosis. Eur Respir J. 2018. https://doi.org/10.1183/13993003.02127-2017.
Broncano-Lavado A, Senhaji-Kacha A, Santamaria-Corral G, Esteban J, Garcia-Quintanilla M. Alternatives to Antibiotics against Mycobacterium abscessus. Antibiotics (Basel). 2022. https://doi.org/10.3390/antibiotics11101322.
Acknowledgements
Funding
No funding or sponsorship was received for this study or the publication of this article.
Medical Writing and/or Editorial Assistance
Nisha Badders, PhD, ELS, Mayo Clinic, substantively edited the manuscript. The Scientific Publications staff at Mayo Clinic provided proofreading and administrative and clerical support. Dr. Badders and the Scientific Publications staff did not receive funding for their work on the manuscript.
Author Contributions
Christina Rivera provided the idea for the article; Tanner Johnson, Thomas Byrd, Wendi Drummond, Lindsey Childs-Kean, Monica Mahoney, Jeffrey Pearson, and Christina G. Rivera performed the literature search and data analysis; and Tanner Johnson, Thomas Byrd, Wendi Drummond, Lindsey Childs-Kean, Monica Mahoney, Jeffrey Pearson, and Christina G. Rivera drafted and critically revised the work.
Disclosures
Christina G. Rivera discloses receiving speaker fees from Insmed, and Wendi Drummond has served on advisory boards for Insmed. Tanner Johnson, Thomas Byrd, Lindsey Childs-Kean, Monica Mahoney, and Jeffrey Pearson have no relevant disclosures.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Johnson, T.M., Byrd, T.F., Drummond, W.K. et al. Contemporary Pharmacotherapies for Nontuberculosis Mycobacterial Infections: A Narrative Review. Infect Dis Ther 12, 343–365 (2023). https://doi.org/10.1007/s40121-022-00750-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-022-00750-5