Abstract
Introduction
To better understand the conditions associated with pertussis diagnosis among older adults in South Korea, a matched case–control study was conducted of individuals ≥ 50 years diagnosed with pertussis between 2009 and 2018.
Methods
Pertussis cases were identified using the nationwide Health Insurance Review and Assessment service (HIRA) database. Each case was then matched to up to 10 controls identified using the National Health Insurance Service–National Sample Cohort (NHIS-NSC) by age, sex, and geographic region at index date. In the 12 months and 30 days prior to index date, the presence of clinical characteristics previously reported to be related to pertussis and pertussis-like conditions were assessed, respectively. A conditional multivariate logistic regression model was then used to calculate odds ratios (ORs) of pertussis diagnosis, adjusted for each of the characteristics.
Results
Pertussis cases (n = 1004) generally demonstrated a higher prevalence of comorbidities compared to controls (n = 9710). Pre-existing asthma and chronic obstructive pulmonary disease (COPD) within 12 months of index date were associated with a two-fold increased risk of pertussis with adjusted ORs (95% confidence interval) of 2.08 (1.68–2.58) and 2.32 (1.59–3.39), respectively. Gastroesophageal reflux disease [GERD; 2.67 (2.23–3.19)], cancer [1.68 (1.23–2.31)], cardiovascular disease [1.62 (1.31–2.00)], renal disease [1.56 (1.12–2.16)], autoimmune disease [1.50 (1.25–1.79)], and hyperlipidemia [1.43 (1.16–1.77)] were also associated with pertussis diagnosis. Finally, acute respiratory events within 30 days prior to index date, such as pneumonia, acute bronchitis, and upper respiratory tract infection (URTI), were highly associated with increased odds of pertussis diagnosis [adjusted ORs of 8.28 (5.10–13.44), 4.86 (3.84–6.14), and 2.90 (2.30–3.67), respectively].
Conclusions
This study’s findings complement and expand upon previous studies on the adult pertussis population, generating real-world data to describe underlying clinical characteristics of those diagnosed with pertussis in South Korea.
Similar content being viewed by others
Avoid common mistakes on your manuscript.

Why carry out this study? |
A resurgence of pertussis has been reported in South Korea in the last 2 decades, with an increasing proportion of cases reported in older adults. |
There remains a gap in the local data on pertussis in older adults in South Korea, and on whether underlying conditions established as risk factors for pertussis apply to this population. |
What was learned from the study? |
Overall, individuals ≥ 50 years diagnosed with pertussis between 2009 and 2018 in South Korea demonstrated a higher prevalence of comorbidities compared to controls. |
Pre-existing respiratory diseases, such as asthma and chronic obstructive pulmonary disease (COPD), as well as gastroesophageal reflux disease (GERD) and acute respiratory events, were all associated with increased odds of pertussis diagnosis. |
These findings complement and expand upon previous studies on the adult pertussis population, helping to inform the clinical community and public health stakeholders for creation and implementation of more effective pertussis prevention strategies in South Korea. |
Digital Features
This article is published with digital features, including a graphical abstract, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.21710483.
Introduction
Pertussis, or “whooping cough”, is a highly contagious respiratory infection caused by Bordetella pertussis, which is characterized by a prolonged paroxysmal cough lasting several weeks and an inspiratory “whoop” [1]. While the incidence rate of pertussis varies by population and calendar year, epidemiological data in the United States (US) have shown a recent trend towards an increasing proportion of pertussis cases in adults [2]. This, in part, has been attributed to waning immunity occurring in the years following primary childhood immunization, which has also been highlighted in previous studies of pertussis in adults [3, 4].
Pertussis can present atypically in adults, and asymptomatic cases of pertussis in adults are common [5, 6]. However, pertussis can also be debilitating in this population with complications, including pneumonia, fainting, urinary incontinence, rib fracture, encephalopathy, and worsening of underlying respiratory conditions [7, 8]. Adults with pre-existing respiratory conditions may also be at increased risk for pertussis [9] and of severe pertussis requiring hospitalization [10].
A resurgence of pertussis has been reported in South Korea, where local data showed an increase in the number of reported pertussis cases in the early 2000s, which peaked in 2009 among infants aged 12 months or less and in 2011 among those aged 15 years or above [11]. However, there remains a gap in the local data on pertussis in older adults in the South Korean population and on whether the underlying conditions established as risk factors for severe pertussis apply to this population [9, 10, 12].
To better understand the burden of pertussis in adults in South Korea, this study aimed to identify the potential conditions associated with pertussis diagnosis in adults ≥ 50 years.
Methods
Patients
A population-based, matched case–control study was conducted to identify the risk factors and prior conditions associated with pertussis diagnosis among individuals ≥ 50 years in South Korea between 2009 and 2018.
Data Source
The medical claims data of individuals diagnosed with pertussis were retrieved using the South Korea national health insurance claims database operated by the Health Insurance Review and Assessment service (HIRA), with a data period from January 1, 2008 to December 31, 2018. The HIRA database is a repository of claims data collected in the process of triaging reimbursement claims filed by healthcare providers which contains comprehensive information pertaining to all reimbursable healthcare services. As the national health insurance program has achieved universal coverage of the entire population, this database includes 98% of the total population (approximately 50 million as of 2014). All diagnoses are coded using the Korea Standard Classification of Diseases 7th revision, which is based on the International Classification of Diseases, 10th revision (ICD-10) [13].
Due to the HIRA data extraction policy that limits maximum data size to be extracted per request, the National Health Insurance Service-National Sample Cohort (NHIS-NSC) Ver.2.0 was used to identify controls (i.e., individuals without a pertussis diagnosis). The NHIS-NSC is a population-based cohort established by the NHIS in South Korea, which was constructed to provide public health researchers and policy makers with representative information regarding citizens’ utilization of health insurance and health examinations. This cohort includes approximately 1 million subjects (2.2% of the entire population) selected via systemic stratified random sampling from the total eligible population in 2002, and followed until 2015 [14].
This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. As these databases consist of Health Insurance Portability and Accountability Act of 1996 (HIPAA) compliant de-identified data, no ethics committee approval was required.
Study Design
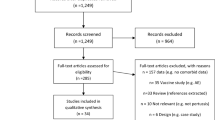
Individuals were included in this analysis if they were aged ≥ 50 years and had been diagnosed with pertussis, as identified using the HIRA by an ICD-10 diagnosis code of pertussis (“A37: Whooping cough”, retrieved up to the 10th position of medical diagnosis) between 2009 and 2018. Information on how diagnosis was made or confirmed (e.g., via laboratory testing) was not available in the database. Individuals were then matched to up to 10 controls identified using the NHIS-NSC by age, sex, and geographic region at the index date (Fig. 1).
The index date for pertussis cases was defined as the date of first pertussis diagnosis (assessed up to the 10th diagnosis position) during the study period. For the matched controls, index date was assigned as the date of a medical visit for any diagnosis that corresponded to the index date of a pertussis case. Due to the limited available data period of NHIS-NSC, pertussis cases diagnosed in 2016–2018 were matched to 2015 NHIS-NSC controls for whom the month and day of the index date was identical to the matched case.
In order to only include cases with a 12-month period preceding index date, pertussis cases diagnosed in 2008 were excluded. Individuals with a history of pertussis within 12 months preceding the pertussis diagnosis were also excluded to only include newly diagnosed cases. Finally, to ensure all controls selected for matching did not have pertussis during the study period, all individuals with ICD-10 “A” code were excluded.
Risk Factors and Associated Conditions Assessed
In the 12 months prior to the index date (baseline period), the presence of conditions previously reported to be related to pertussis were assessed. The conditions assessed were selected a priori via a literature review during the development of the protocol. Firstly, chronic respiratory conditions such as asthma and chronic obstructive pulmonary disease (COPD) were included based on the proposal by Buck et al. 2017 that these may affect risk of pertussis, which is an infection of the respiratory tract [9]. Other medical conditions such as diabetes, hypertension, cardiovascular disease, cerebrovascular disease, hyperlipidemia, and gastroesophageal reflux disease (GERD) were also included as they were among the most common conditions which presented 6 months prior to pertussis diagnosis according to McGuiness et al. 2013 [15]. Neurological disorders, autoimmune disease (e.g., hemolytic anaemia, Crohn’s disease, psoriasis, systemic lupus erythematous, and axial spondylarthritis), and renal disease were included as among the most frequent underlying medical conditions among hospitalized pertussis patients ≥ 65 years [12]. Finally, several conditions included in computing the Charlson Comorbidity Index score among older adults with pertussis (cancer, liver disease, and depression) were also assessed in the 12 months prior to the index date.
In the 30 days prior to the index date, conditions which are pertussis-like or have a clinically meaningful proximal relationship to pertussis were assessed, and were defined as a prescription for cough suppressants or antibiotics accompanied by a diagnosis of acute bronchitis, allergic rhinitis, pneumonia, or upper respiratory tract infection (URTI).
For a full list of the ICD-10 and Anatomical Therapeutic Chemical (ATC) codes used to identify these conditions and associated medications, see Supplementary Table 1.
Statistical Analysis
Baseline characteristics between the cases and controls were compared using the t test for continuous variables and the chi-square test or Fisher’s exact test (expected frequency < 5) for binary variables. To identify potential conditions associated with pertussis diagnosis, a conditional multivariate logistic regression model was used to estimate odds ratios (ORs) with 95% confidence intervals (CIs), adjusted (aORs) for each of the characteristics, including comorbidities and co-medications assessed within 12 months prior to index date and pertussis-like clinical conditions assessed within 30 days of index date. Furthermore, to account for effect modification by age, subgroup analyses were conducted for adults aged 50–64 and ≥ 65 years.
Sensitivity Analyses
To consider the potential effect of different data periods of HIRA (2009–2018; used for extraction of the cases) and NHIS-NSC databases (2009–2015; used for extraction of the controls), the analysis was repeated after truncating the study period from 2009–2018 to 2009–2015, which were the available data periods for the two databases (Supplementary Fig. 1).
As excluding the ICD-10 code “A” may have led to certain individuals with conditions other than pertussis being excluded, a sensitivity analysis where these individuals were included was also conducted.
Lastly, an additional sensitivity analysis which used separate multivariate models for comorbidities and co-medications assessed within 12 months prior to index date and pertussis-like clinical conditions assessed within 30 days of index date was conducted.
Results
Baseline Characteristics of Pertussis Cases and Matched Controls
In 2009–2018, 1011 individuals diagnosed with pertussis ≥ 50 years in South Korea were identified using the HIRA database. The most commonly recorded ICD-10 code was “A37.9 whooping cough, unspecified” (54.9%) and “A37.0 whooping cough due to Bordetella species” (39.3%), followed by “A37.8 whooping cough due to another Bordetella species” (3.7%) and “A37.1 whooping cough due to Bordetella parapertussis” (2.1%).
Of these cases, 1004 were matched with 9,710 controls based on age, sex, and geographic location. Among these individuals, mean age (SD) was 64.5 (10.6) years, 61.4% were women, and most resided in rural (< 1 million population) and urban (≥ 1 million population) compared to metropolitan (capital city, Seoul) areas (39.6% and 38.8% vs. 21.5%, respectively). Among the 1004 pertussis cases, 692 (68.9%) received macrolides on or within 30 days after the pertussis diagnosis. The most frequently prescribed macrolide was azithromycin (466 cases, 46.4%), followed by clarithromycin (193 cases, 19.2%) and erythromycin (33 cases, 3.3%). Table 1 shows the baseline characteristics of the identified pertussis cases and matched controls.
Prevalence of comorbidities in the year prior to the index date was generally higher among pertussis cases compared to controls, including asthma (37.0% vs. 5.9%), cancer (9.7% vs. 3.1%), cardiovascular disease (38.0% vs. 13.2%), cerebrovascular disease (12.1% vs. 5.1%), COPD (10.6% vs. 1.3%), diabetes (29.5% vs. 13.0%), GERD (54.0% vs. 14.1%), hyperlipidemia (48.0% vs. 19.2%), hypertension (49.2% vs. 26.3%), autoimmune disease (49.3% vs. 17.5%), liver disease (32.3% vs. 11.7%), and renal disease (9.6% vs. 3.1%). Furthermore, more individuals diagnosed with pertussis were diagnosed with pertussis-like conditions assessed within 30 days prior to index date, compared with controls.
Potential Risk Factors Associated with Pertussis Diagnosis
Demographic and clinical characteristics assessed 12 months and 30 days prior to the index date that were associated with pertussis diagnosis are presented in Table 2.
Pre-existing respiratory conditions within the 12 months prior to the index date, including asthma and COPD, were associated with increased odds of pertussis diagnosis [aORs (95% CI), 2.08 (1.68–2.58) and 2.32 (1.59–3.39), respectively). Pertussis-like clinical conditions within 30 days prior to the index date were also associated with increased odds of pertussis diagnosis, with the highest odds observed for pneumonia [8.28 (5.10–13.44)], followed by acute bronchitis [4.86 (3.84–6.14)], URTI [2.90 (2.30–3.67)], and allergic rhinitis [1.71 (1.32–2.21)].
Among the other comorbidities under assessment 12 months prior to the index date, patients with past medical history of GERD [aOR 2.67 (2.23–3.19)], cancer [1.68 (1.23–2.31)], cardiovascular disease [1.62 (1.31–2.00)], renal disease [1.56 (1.12–2.16)], autoimmune disease [1.50 (1.25–1.79)], or hyperlipidemia [1.43 (1.16–1.77)] were at increased odds for pertussis diagnosis.
Subgroup Analyses
Among the 558 pertussis cases and 5,452 matched controls aged 50–64 years, pre-existing respiratory conditions such as asthma and COPD within 12 months prior to index date and pertussis-like conditions within 30 days prior to the index date were consistently associated with increased odds of pertussis diagnosis. However, fewer comorbidities under assessment 12 months prior to the index date showed statistically significant increased odds of pertussis diagnosis, including GERD [2.44 (1.94–3.07)], autoimmune disease [1.56 (1.24–1.95)], and hyperlipidemia [1.39 (1.06–1.83); Supplementary Table 2].
Among the 446 pertussis cases and 4,258 controls aged ≥ 65 years, results from the subgroup analysis were largely consistent with the combined group analysis findings. In addition, use of immunosuppressive drugs within 12 months prior to index date was associated with increased odds of pertussis diagnosis [3.82 (1.24–11.75); Supplementary Table 3].
Sensitivity Analysis
To validate the main findings, sensitivity analysis was carried out by only including the cases diagnosed between 2009 and 2015 to match the data period of NHIS-NSC in which the controls were retrieved. Of the 1,004 pertussis cases included in the main analysis, 558 cases were subsequently excluded, resulting in 446 cases and 4,451 matched controls between 2009 and 2015 (Supplementary Table 4). Similar to the results of the main analysis, individuals with pre-existing respiratory conditions within 12 months prior to the index date had increased odds of pertussis diagnosis. However, the majority of assessed comorbidities showed null association, except for cardiovascular disease and GERD (Table 3). This trend was also seen in the subgroup analyses, in which past medical histories of COPD, asthma, and GERD, and cardiovascular disease were consistently associated with an increased risk of pertussis diagnosis (Supplementary Tables 5 and 6).
Findings from the sensitivity analysis where individuals with the ICD-10 “A” code were not excluded from control group selection (cases: n = 1,005; controls: n = 9,718) were also in line with those of the main analysis. The presence of asthma, COPD, and other comorbidities consistently increased the odds of pertussis diagnosis.
When separate multivariate models were used for comorbidities assessed within 12 months prior to index date and pertussis-like conditions assessed within 30 days prior to index date, factors significantly associated with a pertussis diagnosis were largely consistent with the main results. However, the magnitude of association differed for some variables after using two separate models. For instance, aORs (95% CI) of pertussis diagnosis for asthma more than doubled from 2.08 (1.68–2.58) to 4.59 (3.86–5.45; Supplementary Table 7).
Discussion
In view of the relatively limited data on the characteristics of adults with pertussis in South Korea, a matched case–control study design was utilized to identify risk factors associated with pertussis diagnosis among individuals ≥ 50 years. After matching based on age, sex, and geographic region, substantial differences in the clinical characteristics between cases and controls were identified, with pertussis cases generally demonstrating a higher prevalence of comorbidities.
Pre-existing respiratory diseases within 12 months prior to index date, such as asthma and COPD, were associated with a roughly two-fold risk of pertussis diagnosis. As pertussis is an infection of the respiratory tract, patients with these underlying respiratory conditions may be at increased risk for pertussis.
Several studies have examined the relationship between asthma and pertussis. A study during a pertussis outbreak in Canada documented that adolescent pertussis cases had relatively higher asthma prevalence of 24%, compared with 12% in the general population [7]. A population-based cohort study in Australia also showed pre-existing asthma as a significant predictor of pertussis [16].
Conversely, the association between COPD and pertussis has been explored less. A study in Switzerland confirmed pertussis as an underlying cause of acute exacerbation in 19% of COPD patients but remained inconclusive on whether COPD independently increases the risk of pertussis [8]. However, this preliminary finding was later confirmed by a retrospective cohort study in the US, where the relative risks of pertussis was increased among individuals with COPD compared with those without [9].
Asthma and COPD have not only been linked to risk of pertussis but also to the severity of pertussis disease. For example, among adolescent and adult patients with pertussis-related hospitalization in the US, 29.3% and 15.7%, respectively, were found to have a history of asthma or COPD, much higher than the background prevalence of 10% and 8% for asthma among US adults and adolescents, respectively, and 6.4% for COPD among US adults (no data reported for adolescents) [10]. Moreover, patients with both asthma and COPD have been linked to increased healthcare resource utilization among pertussis patients [9]. Therefore, the findings of the current study confirm those of previous studies that asthma is a significant risk factor for pertussis and contribute to the real-world data on the increased risk of pertussis among those with pre-existing COPD.
Acute respiratory events within 30 days prior to index date, such as pneumonia, acute bronchitis, and URTI were also associated with increased odds of pertussis diagnosis. In fact, almost half of study participants presented with at least one pertussis-related diagnosis in the 6 months preceding pertussis diagnosis. Similar findings to these have been previously reported, with a recent cohort study on pertussis patients aged ≥ 50 years in the US reporting over half (57%) of the patients presented with at least one pertussis-like diagnosis such as acute bronchitis [15].
However, these initial diagnoses may have been made while waiting for laboratory confirmation of etiology or may simply represent misdiagnoses. The latter is plausible, given that adult patients with pertussis usually present in an atypical manner [17]. Therefore, the trends in pertussis-like conditions shown in this study require careful interpretation, as they may be subject to bias from reverse causation. In particular, pneumonia is a known complication of pertussis, and has been previously shown to occur in around 5–9% of pertussis cases in adults ≥ 30 years, increasing with age [7]. Similarly, pertussis may be initially misdiagnosed as asthma or remain undetected during acute exacerbations of COPD [8, 18, 19].
Among the clinical characteristics assessed 12 months prior to the index date, diagnosis of GERD was also associated with pertussis diagnosis across all analyses. GERD is a common disorder with an estimated prevalence of 7.3% in 2008 in South Korea [20]. The association of GERD with pulmonary diseases has been established previously [21], and a retrospective cohort study in Taiwan showed that the risk of pneumonia was significantly higher in GERD patients [22]. However, to the best of our knowledge, there has not been a consensus as to whether individuals with GERD have an increased risk for pertussis diagnosis. Data analysis of community-acquired pneumonia cases in New Zealand showed B. pertussis was identified along with other respiratory pathogens such as Streptococcus pneumoniae, Haemophilus influenzae, respiratory syncytial virus, and influenza A virus [23]. Therefore, GERD as a risk factor for pertussis diagnosis may be in part attributable to GERD patients being susceptible to respiratory complications, and therefore being more likely to have B. pertussis detected. GERD in adults is also a common cause of chronic cough [24], and so it is possible that GERD diagnosis is evoked first, with a pertussis diagnosis established later.
Similar results were seen across the subgroup analysis that accounted for effect modification by age and the sensitivity analysis which accounted for the potential effect of different database periods. Notably, mean age was lower for the sensitivity analysis, which used an earlier data period (2009–2015). This may reflect reports by the Korea Disease Control Prevention Agency (KDCA) which show an increasing proportion of pertussis cases in older individuals [adults ≥ 50 years accounting for 3.7% (½7) of pertussis cases in 2010 and 38.2% (47/123) of cases in 2020] [25].
Interestingly, decreased odds of pertussis diagnosis were seen for individuals with pre-existing diabetes across the sensitivity analysis. While the reason for this trend is unclear, it could be attributed to the current adult immunization schedule recommended by the Korean Society of Infectious Diseases and endorsed by the Korean Diabetes Association, which recommends the tetanus, reduced diphtheria, acellular pertussis (TdaP)/tetanus and diphtheria toxoid (Td), pneumococcal, and annual influenza vaccines for patients with diabetes [26]. Assuming adequate vaccination rate in this population, these patients may benefit from TdaP vaccination in preventing pertussis.
Limitations
This study represents the first of its kind to investigate the risk factors of pertussis among adults in South Korea. A robust methodology was used as well as a comprehensive dataset, courtesy of the HIRA database which is internationally recognized and representative of the entire South Korean population. However, when interpreting the study findings, limitations pertaining to the use of administrative claims data should be considered.
As medical claims data of HIRA were collected mainly for reimbursement purposes and not for research, there are inbuilt limitations such as incomplete, inaccurate, or missing data. Specifically, as this study relied on the diagnostic codes from the procured data to measure the exposure, outcome, and covariates, potential miscoding or misdiagnosis may consequently lead to underestimation or overestimation of the true occurrence of variables assessed. However, case definitions validated in past studies and subsequently reviewed by clinical experts were used for asthma and COPD, thereby minimizing overestimation of true rates of these conditions.
It should additionally be noted that only diagnosed pertussis cases were included in this analysis. While pertussis is a communicable disease that requires mandatory reporting to the KDCA, it is likely that pertussis is underdiagnosed in the adult South Korean population, as indicated by the rates of seroprevalence, which are far higher than expected given reported cases [27]. Therefore, it is likely that a number of pertussis cases which were not diagnosed were not included in this analysis.
Information was also unavailable on the diagnostic methods of pertussis cases in this database, and thus an ICD-10 code-based case definition was used. In South Korea, pertussis is mandated to be reported by healthcare providers upon diagnosis, and cases are typically confirmed either via laboratory testing [most commonly using polymerase chain reaction or clinical presentation (cough lasting more than a week and at least one of the following conditions: paroxysmal cough, inspiratory whoop, post-tussive vomiting]. Data from a 2012 ad hoc active sentinel surveillance in South Korea showed that only 13% of the pertussis cases reported in the active sentinel surveillance centers were laboratory confirmed [28]. Therefore, we assumed that the majority of pertussis cases identified in this study were clinically diagnosed.
Similarly, the bacterial etiology of pertussis cases could not be confirmed as this information was not available in the database. From the ICD-10 codes used, we estimated that < 6% of whooping cough cases were due to a pathogen other than B. pertussis. However, these cases would likely have little impact on results given the similar clinical presentations of these different strains, with B. parapertussis likely to be lower in severity than B. pertussis. Recent studies have also suggested that the pertussis vaccine may induce cross-immunity against B. parapertussis, further suggesting phenotypic similarities between the two pathogens [29].
Clinical presentation of pertussis may have also coincided with that of other comorbidities in the 12 months prior to index date, such as asthma, leading to an incorrect diagnosis. However, to avoid this, strict case definitions were used. For example, diagnosis of asthma was defined by one inpatient or at least two outpatient diagnoses, as well as a prescription record for at least one asthma medication. Moreover, the other conditions assessed in the 12 months prior to the index date were mostly chronic medical conditions that are somewhat less symptomatic compared to the abrupt and acute symptoms related to pertussis.
In addition, there may have been potential selection bias which is inherent in case–control studies. As comorbidities (including asthma, COPD, cardiovascular disease, hyperlipidemia, and autoimmune disease) may increase healthcare-seeking activities and the opportunity for diagnosis, this may have resulted in an increased effect size in pertussis cases compared with controls. Patients with chronic respiratory illness who present with an exacerbation of symptoms may also be more likely to undergo diagnostic work-up compared to those without. To mitigate the effect of selection bias, ORs were adjusted for each of the comorbidities and co-medications. However, a confounding factor not matched for or included in the database could have influenced results.
Lastly, the use of ICD-10 codes masks the presence of communicable infectious diseases, and thus excludes individuals with “A” codes (e.g., pertussis [A37] or who are at potentially higher risk for infectious disease (e.g., have immunocompromising conditions or other comorbidities). As a result, the control group may have been healthier than cases in the matched case–control analysis. However, this study performed additional sensitivity analysis that included controls with ICD-10 “A” codes, in which findings were generally consistent with the main analysis. Similarly, in a multivariate analysis of the chronic conditions and recent conditions, the risk factors for pertussis diagnosis were largely consistent with the main results.
Conclusions
In this population-based matched case–control analysis of individuals ≥ 50 years in South Korea, several chronic medical conditions were found to increase the odds for pertussis diagnosis, including chronic respiratory conditions such as asthma and COPD, as well as acute respiratory and pertussis-like symptoms. While these conditions represent potential risk factors for pertussis diagnosis, they also represent potential misdiagnoses. Therefore, increased awareness of pertussis among adults in South Korea is important to support efficient patient management and pertussis prevention.
Current strategies to prevent pertussis include TdaP vaccination. The 2022 report for the Global Initiative for Chronic Obstructive Lung Disease strategy for prevention, diagnosis, and management of COPD, refer to the US Advisory Committee on Immunization Practices for TdaP vaccination [30]. These state that persons ≥ 19 years who have never received TdaP should receive a dose of this vaccine, with a booster dose every 10 years [31]. These guidelines are similar to the current adult immunization schedule recommended by the Korean Society of Infectious Diseases [26]. The US CDC also strongly recommends the Tdap vaccine, among others, for patients with lung diseases including asthma [32].
Overall, the present study’s findings complement and expand upon previous studies on the adult pertussis population in South Korea, generating real-world data to describe underlying clinical characteristics of those at increased risk for pertussis, and helping to inform the clinical community and public health stakeholders for the creation of more effective pertussis prevention strategies, including vaccination for at-risk populations.
References
Jenkinson D. Natural course of 500 consecutive cases of whooping cough: a general practice population study. BMJ. 1995;310(6975):299–302.
Pertussis—United States, 2001-2003. MMWR Morb Mortal Wkly Rep. 2005;54(50):1283-6
Kilgore PE, Salim AM, Zervos MJ, Schmitt HJ. Pertussis: microbiology, disease, treatment, and prevention. Clin Microbiol Rev. 2016;29(3):449–86.
Lambert HJ. Epidemiology of a small pertussis outbreak in Kent County, Michigan. Public Health Rep (1896). 1965;80(4):365–9.
Zepp F, Heininger U, Mertsola J, et al. Rationale for pertussis booster vaccination throughout life in Europe. Lancet Infect Dis. 2011;11(7):557–70.
Mannerstedt G. Pertussis in adults. J Pediatr. 1934;5:596–600.
De Serres G, Shadmani R, Duval B, et al. Morbidity of pertussis in adolescents and adults. J Infect Dis. 2000;182(1):174–9.
Bonhoeffer J, Bär G, Riffelmann M, Solèr M, Heininger U. The role of Bordetella infections in patients with acute exacerbation of chronic bronchitis. Infection. 2005;33(1):13–7.
Buck PO, Meyers JL, Gordon LD, et al. Economic burden of diagnosed pertussis among individuals with asthma or chronic obstructive pulmonary disease in the USA: an analysis of administrative claims. Epidemiol Infect. 2017;145(10):2109–21.
Mbayei SA, Faulkner A, Miner C, et al. Severe pertussis infections in the United States, 2011–2015. Clin Infect Dis. 2019;69(2):218–26.
Choe YJ, Park Y-J, Jung C, Bae G-R, Lee D-h. National pertussis surveillance in South Korea 1955–2013;2011: epidemiological and clinical trends. Int J Infect Dis. 2012;16(12):e850–4.
Jenkins VA, Savic M, Kandeil W. Pertussis in high-risk groups: an overview of the past quarter-century. Hum Vaccin Immunother. 2020;16(11):2609–17.
Kim JA, Yoon S, Kim LY, Kim DS. Towards Actualizing the Value Potential of Korea Health Insurance Review and Assessment (HIRA) Data as a Resource for Health Research: Strengths, Limitations, Applications, and Strategies for Optimal Use of HIRA Data. J Korean Med Sci. 2017;32(5):718–28.
Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort Profile: The National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017;46(2): e15.
McGuiness CB, Hill J, Fonseca E, et al. The disease burden of pertussis in adults 50 years old and older in the United States: a retrospective study. BMC Infect Dis. 2013;13:32.
Liu BC, McIntyre P, Kaldor JM, et al. Pertussis in older adults: prospective study of risk factors and morbidity. Clin Infect Dis. 2012;55(11):1450–6.
Tozzi AE, Pastore Celentano L, Ciofi degli Atti ML, Salmaso S. Diagnosis and management of pertussis. CMAJ. 2005;172(4):509–15.
Ristić M, Radosavljević B, Stojanović VD, Đilas M, Petrović V. Performance of the new clinical case definitions of pertussis in pertussis suspected infection and other diagnoses similar to pertussis. PLoS ONE. 2018;13(9): e0204103.
Weinberger M, Abu-Hasan M. Pseudo-asthma: when cough, wheezing, and dyspnea are not asthma. Pediatrics. 2007;120(4):855–64.
Kim K-M, Cho YK, Bae SJ, et al. Prevalence of gastroesophageal reflux disease in Korea and associated health-care utilization: A national population-based study. J Gastroenterol Hepatol. 2012;27(4):741–5.
Gaude GS. Pulmonary manifestations of gastroesophageal reflux disease. Ann Thorac Med. 2009;4(3):115–23.
Hsu WT, Lai CC, Wang YH, et al. Risk of pneumonia in patients with gastroesophageal reflux disease: a population-based cohort study. PLoS ONE. 2017;12(8): e0183808.
Beynon KA, Young SA, Laing RT, et al. Bordetella pertussis in adult pneumonia patients. Emerg Infect Dis. 2005;11(4):639–41.
Harding SM. Gastroesophageal reflux and chronic cough GI Motility online 2006.
Korea Disease Control and Prevention Agency. Infectious Disease Portal. http://www.kdca.go.kr/npt/biz/npp/ist/bass/bassSexdstnAgeStatsMain.do. Accessed 3 Aug 2021 (Internet).
Recommended immunization schedule for adults in Korea. by the Korean Society of Infectious Diseases, 2012. Clin Exp Vaccine Res. 2014;3(1):110–2.
Mungall BA, Kim H, Oh KB. A systematic review of the burden of pertussis in South Korea. Hum Vaccin Immunother. 2021;17(6):1747–56.
Choe YJ, Kim JW, Park YJ, Jung C, Bae GR. Burden of pertussis is underestimated in South Korea: a result from an active sentinel surveillance system. Jpn J Infect Dis. 2014;67(3):230–2.
Liko J, Robison SG, Cieslak PR. Do pertussis vaccines protect against bordetella parapertussis? Clin Infect Dis. 2017;64(12):1795–7.
Global Initiative for Chronic Obstructive Lung Disease. Global Initiative for Chronic Obstructive Lung Disease. 2022. https://goldcopd.org/2022-gold-reports-2/. Accessed 10 Jan 2022 (Internet).
Havers FP, Moro PL, Hunter P, Hariri S, Bernstein H. Use of tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccines: updated recommendations of the advisory committee on immunization practices—United States, 2019. MMWR Morb Mortal Wkly Rep. 2020;69(3):77–83.
Centers for Disease Control and Prevention. Vaccine information for adults—lung disease including asthma and adult vaccination. https://www.cdc.gov/vaccines/adults/rec-vac/health-conditions/lung-disease.html. Accessed 5 July 2022 (Internet).
Acknowledgements
Funding
Sponsorship for this study and Rapid Service Fee was provided by GlaxoSmithKline Biologicals SA.
Medical Writing, Editorial, and Other Assistance
The authors acknowledge Kyu-Bin Oh, GSK, Singapore, and Bruce A. Mungall, formerly GSK, Korea, for contributions to the design of the study, Ahhyung Choi, Sungkyunkwan University, Suwon, South Korea, for contributions to the analysis and interpretation of the data, and Roeland Van Kerckhoven, GSK, Belgium, for publication management. The authors also thank Costello Medical for editorial assistance and publication coordination, on behalf of GSK, and acknowledge Kaity McCafferty Layte, Costello Medical, UK for medical writing and editorial assistance based on authors’ input and direction funded by GlaxoSmithKline Biologicals SA in accordance with Good Publication Practice 2022 guidelines (https://www.ismpp.org/gpp-2022).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authors’ Contributions
Substantial contributions to study conception and design: Hyungwoo Kim, Ju-Young Shin, Jing Chen, Ju Hwan Kim, Yunha Noh, Hee Jin Cheong, Yeon-Mok Oh, Adrienne Guignard, Sumitra Shantakumar; substantial contributions to analysis and interpretation of the data: Hyungwoo Kim, Ju-Young Shin, Jing Chen, Ju Hwan Kim, Yunha Noh, Hee Jin Cheong, Yeon-Mok Oh, Adrienne Guignard, Sumitra Shantakumar; drafting the article or revising it critically for important intellectual content: Hyungwoo Kim, Ju-Young Shin, Jing Chen, Ju Hwan Kim, Yunha Noh, Hee Jin Cheong, Yeon-Mok Oh, Adrienne Guignard, Sumitra Shantakumar; final approval of the version of the article to be published: Hyungwoo Kim, Ju-Young Shin, Jing Chen, Ju Hwan Kim, Yunha Noh, Hee Jin Cheong, Yeon-Mok Oh, Adrienne Guignard, Sumitra Shantakumar.
Disclosures
Hyungwoo Kim: employed by the GSK group of companies; Ju-Young Shin: research funding from the Ministry of Food and Drug Safety, Ministry of Health and Welfare, Government-wide R&D Fund project for Infectious Disease Research (GFID) and National Research Foundation of South Korea and grants from GSK, Amgen, Pfizer, Hoffmann-La Roche, Dong-A ST, and Yungjin, outside the submitted work; Jing Chen, Adrienne Guignard, Sumitra Shantakumar: employed by the GSK group of companies and hold GSK shares; Ju Hwan Kim, Yunha Noh, Hee Jin Cheong: report nothing to disclose; Yeon-Mok Oh: personal fees from Boehringer Ingelheim, Boehringer Ingelheim Korea, GSK Korea and Novartis Korea, outside the submitted work.
Compliance with Ethics Guidelines
This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. As the databases used for this study consist of Health Insurance Portability and Accountability Act of 1996 (HIPAA) compliant de-identified data, no ethics committee approval was required.
Data Availability
The datasets generated during and/or analyzed during the current study are not publicly available as they are owned by the statutory health insurances. Permission to access these data was granted to the study team between January 2021–January 2023 (approval number: M20200622614). Applications to access the databases used in this study can be made via the HIRA Open data portal (https://opendata.hira.or.kr/home.do). The datasets supporting the conclusions of this article are included within the article and its additional files.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kim, H., Shin, JY., Chen, J. et al. Risk Factors of Pertussis Among Older Adults in South Korea: A Nationwide Health Data-Based Case–Control Study. Infect Dis Ther 12, 545–561 (2023). https://doi.org/10.1007/s40121-022-00747-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-022-00747-0