Abstract
Introduction
This study aimed to explore the association of serum lactate with clinical outcomes in elderly patients with sepsis based on data from the MIMIC-IV database.
Methods
All elderly patients with sepsis (age ≥ 65 years) were included. Different models were constructed for exploring the relationships between lactate and 28-day mortality. A two-segment linear regression model was performed to verify the threshold effects of lactate on clinical outcomes and smooth curve fitting was performed.
Results
A total of 4199 elderly patients with sepsis were included. The 28-day mortality was 32.22% (n = 1395). After adjustment for all potential cofounders, for each 1 mmol/l increment in lactate, the odds ratio (OR) of 28-day mortality was 1.23 (95% CI 1.18–1.28, P < 0.0001). Smooth fitting curves indicated a non-linear positive relationship between lactate and 28-day mortality. The turning point of lactate level was 5.7 mmol/l: at ≤ 5.7 mmol/l, with each 1 mmol/l increment in lactate, the risk of 28-day mortality increased significantly (OR 1.32, 95% CI 1.25–1.38, P < 0.0001); the significantly positive relationship was still present at lactate > 5.7 mmol/l (OR 1.10, 95% CI 1.04–1.18, P = 0.0019). The area under the ROC curve (AUC) of lactate was 0.618 (95% CI 0.599–0.635) and the cutoff value of lactate was 2.4 mmol/l with a sensitivity of 0.483 and a specificity of 0.687.
Conclusion
In elderly patients with sepsis, a non-linear positive relationship was discovered between serum lactate and 28-day mortality. Physicians should be alert to lactate assessment at admission and pay more attention to those patients with higher levels of lactate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why was the study carried out? |
Elderly patients with sepsis were more likely to have an increased risk of mortality. |
The study aimed to explore the association of serum lactate with clinical outcomes in elderly patients with sepsis based on a large-scale public database in order to aid in risk stratification of poor prognosis. |
What was learned from the study? |
In elderly patients with sepsis, for each 1 mmol/l increment in lactate, the OR of 28-day mortality was 1.23 (95% CI 1.18–1.28, P < 0.0001). |
A prognostic value of lactate for prognosis in elderly patients with sepsis was identified. |
Monitoring lactate level is helpful for dynamically identifying those patients with higher risk of worse outcomes. |
Introduction
Lactate is an easily and simply accessible laboratory parameter and could be an objective biomarker for tissue perfusion, which is superior to urine output and physical examination [1,2,3]. Previous studies proved that elevated levels of lactate indicated lower oxygen supply in tissues and organs, increased aerobic glycolysis, or decreased lactate clearance due to liver or kidney dysfunctions [4,5,6]. Lactate level was utilized for risk-stratifying disease severity and elevated levels of lactate partly revealed the poorer prognosis in various diseases [7,8,9]. Hence, monitoring lactate levels is helpful for dynamically identifying those patients with a higher risk of worse outcomes.
The Surviving Sepsis Campaign Guidelines 2016 recommended that fluid resuscitation should be done until lactate level normalized in patients with sepsis and higher levels of lactate [10]. A recent meta-analysis of randomized controlled trials with 16 studies and 5968 patients with sepsis concluded that lactate-guided therapy was associated with lower mortality [11]. As a result of the aging of society, the number of elderly patients with sepsis has been increasing significantly [12, 13]. Compared to young adult patients, elderly patients were more likely to have comorbidities, chronic diseases, and decreased functional reserve, leading to an increased risk of mortality [14, 15].
As a result of the significance of serum lactate in sepsis, our study aimed to explore the association of serum lactate with clinical outcomes in elderly patients with sepsis based on a large-scale public database in order to aid in risk stratification of poor prognosis.
Methods
Database, Definition, and Study Cohort
This was a retrospective study based on the Medical Information Mart for Intensive Care (MIMIC)-IV database (version 1.0, https://mimic.mit.edu/iv/), which included the medical records of all the patients admitted to the intensive care unit (ICU) in the Beth Israel Deaconess Medical Center from 2008 to 2019 [16, 17]. To apply for access to the database, the author (N.D.) passed the Protecting Human Research Participants exam (No. 32900964).
Elderly patients with sepsis in MIMIC-IV were enrolled in our research. The diagnosis of sepsis was confirmed according to the Sepsis-3 definition [18]. When an acute change in sequential organ failure assessment (SOFA) score ≥ 2 points resulted from the infection, sepsis was identified. Inclusion criteria were (1) age ≥ 65 years old; (2) diagnosis of sepsis in the database. Exclusion criteria were (1) missing data of lactate; (2) missing data of individual variables > 5%.
Compliance with Ethics Guidelines
This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. MIMIC-IV is an anonymized public database. The project was approved by the institutional review boards of the Massachusetts Institute of Technology (MIT) and Beth Israel Deaconess Medical Center (BIDMC) and was given a waiver of informed consent.
Variables
General characteristics including age, gender, and comorbidities were extracted. Vital signs and laboratory variables of each patient in the 24 h after admission were included. Only the first value of the variable which was recorded in 24 h was utilized for analysis.
The following data were used in our research: systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate (HR), respiratory rate (RR), anion gap (AG), alanine aminotransferase (ALT), red blood cell (RBC), white blood cell (WBC), sodium, creatinine, chloride, total bilirubin, prothrombin time (PT), international normalized ratio (INR), urea nitrogen, platelet (PLT), and glucose. SOFA and acute physiology and chronic health evaluation (APACHE II) scores were collected. Variables of clinical outcomes were extracted and calculated as follows: days of length of stay (LOS) in ICU and hospital and 28-day mortality.
Data Extraction and Statistical Analysis
Data was extracted from the MIMIC-IV database using PgAdmin4 which was applied to run structure query language (SQL). We used the software packages R (http://www.R-project.org) and EmpowerStats (http://wwwempowerstats.com) for data analysis. Statistically significant was defined as a P value < 0.05.
All elderly patients with sepsis were distributed into four groups based on the quartiles of lactate level (Q1, < 1.5 mmol/l; Q2, 1.5–2.0 mmol/l; Q3, 2.1–3.0 mmol/l; Q4, > 3.0 mmol/l). Different variables were reported as follows: (1) continuous variables as medians; (2) categories variables as percentages or frequencies. Chi-squared test and Mann–Whitney U test were applied for data analysis.
First, we compared the different variables between the four groups (Q1–Q4). Second, we implemented univariate and multivariate analyses to investigate the association of different variables with 28-day mortality by logistic regression. We evaluated the odds ratio (OR) with 95% confidence interval (CI) for each variable. Third, the following three different models were constructed to explore the relationships between lactate and clinical outcomes: (1) crude model adjusted for none; (2) model I adjusted for age and gender; (3) model II adjusted for all potential cofounders. In addition, lactate as a categorical parameter based on quartiles (Q1–Q4) and categorial (Q1 (≤ 2.0 mmol/l), Q2 (> 2.0, ≤ 4.0 mmol/l), Q3 (> 4.0 mmol/l)) were analyzed in three models and the values of p for trend of categorized lactate in all three different models were statistically calculated. Moreover, Kaplan–Meier analysis for cumulative hazard in 28-day mortality based on quartiles and categorial groups were constructed to compare the different mortality risks between different groups. Fourth, we compared two models (model A, the linear model; and model B, the two-segment non-linear model) for displaying the relationship between lactate and 28-day mortality. The log-likelihood ratio tests were applied to select the better one between the two models. When a P value is less than 0.05, model B is significantly better than model A. The threshold effects of lactate on 28-day mortality in model B were analyzed and smooth fitting curves were generated by the generalized additive model. If a non-linear association of lactate and clinical outcomes was found, the turning point of lactate was confirmed by recursive algorithm. Finally, the receiver operating characteristic (ROC) analysis of lactate for predicting 28-day mortality was performed. The predictive performances including specificity, sensitivity, cutoff value, positive predictive value (PPV), and negative predictive value (NPV) were analyzed.
Results
General Description of the Cohort of Elderly Patients with Sepsis
A total of 4199 patients with a median age of 76 years were included in our research (Supplementary Fig. 1 and Table 1). The 28-day mortality was 32.22% (n = 1395). The numbers of men and women was 2289 (54.51%) and 1910 (45.49%), respectively. The median days of LOS in ICU and hospital were 3.78 and 9.53, respectively.
In Table 1, the whole cohort is divided into four groups based on the quartiles of lactate level: Q1 (< 1.5 mmol/l, n = 1019), Q2 (1.5–2.0 mmol/l, n = 1016), Q3 (2.1–3.0 mmol/l, n = 1063), and Q4 (> 3.0 mmol/l, n = 1101). Different clinical and laboratory variables were compared between the four groups. The 28-day mortalities in the Q1–Q4 groups were as follows: 23.65% (n = 241), 28.54% (n = 290), 32.46% (n = 345), and 47.14% (n = 519), respectively (P < 0.001).
Univariate and Multivariate Analyses of Variables for 28-Day Mortality
Table 2 summarizes the univariate and multivariate analyses of variables for 28-day mortality in elderly patients with sepsis. Multivariate analysis showed that age (P < 0.0001), renal disease (P = 0.0001), HR (P = 0.0025), creatinine (P < 0.0001), urea nitrogen (P < 0.0001), and lactate (P < 0.0001) were significantly associated with 28-day mortality in elderly patients with sepsis.
Relationship Between Lactate and 28-Day Mortality
Table 3 summarizes the three models, namely crude model, model I, and model II, that were constructed to explore the association between lactate and 28-day mortality. In model II after adjustment for all potential cofounders, for each 1 mmol/l increment in lactate, the OR of 28-day mortality was 1.23 (95% CI 1.18–1.28, P < 0.0001). Categorial variables including Q1–Q4 based on quartiles of lactate were compared in the three models. In the Q4 group (lactate > 3 mmol/l), the risk of 28-day mortality in model II increased the most: OR 2.52 (95% CI 2.03–3.13, P < 0.0001). The values of P for trend in the three models were statistically significant (all P < 0.0001).
Moreover, we divided the cohort into three group based on cutoff values of lactate (2.0 mmol/l and 4.0 mmol/l): Q1 (≤ 2.0 mmol/l, n = 2166), Q2 (> 2.0, ≤ 4.0 mmol/l, n = 1378), and Q3 (> 4.0 mmol/l, n = 655). Compared to the Q1 group, the risk of 28-day mortality in model II significantly increased the most in the Q3 group: OR 3.05 (95% CI 2.46–3.79, P < 0.0001).
Figure 1 shows the Kaplan–Meier analysis for cumulative hazard in 28-day mortality. Figure 1a shows that on the basis of the quartiles of lactate level, the risk of 28-day mortality was the highest in the Q4 group (> 3.0 mmol/l) (P < 0.001). Figure 1b revealed that compared to the Q1 group (≤ 2.0 mmol/l), the risk of 28-day mortality was the highest in the Q3 group (> 4.0 mmol/l) (P < 0.001).
Kaplan–Meier analysis for 28-day survival probability in elderly patients with sepsis. a Groups based on quartiles of lactate level (Q1, < 1.5 mmol/l; Q2, 1.5–2.0 mmol/l; Q3, 2.1–3.0 mmol/l; Q4, > 3.0 mmol/l). b Groups based on category of lactate level (Q1, ≤ 2.0 mmol/l; Q2, > 2.0 and ≤ 4.0 mmol/l; Q3, > 4.0 mmol/l)
Non-linear Relationship Between Lactate and 28-Day Mortality
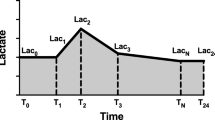
Two different models, namely the linear model (model A) and the two-segment non-linear model (model B), were constructed and analyzed as summarized in Table 4. Comparing the two models, the P value was < 0.001 and model B was the better one for indicating the relationship. The turning point of lactate level was 5.7 mmol/l. At lactate level ≤ 5.7 mmol/l, with each 1 mmol/l increment in lactate, the risk of 28-day mortality increased significantly (OR 1.32, 95% CI 1.25–1.38, P < 0.0001). The significantly positive relationship remained at lactate > 5.7 mmol/l (OR 1.10, 95% CI 1.04–1.18, P = 0.0019). Smooth curve fitting was performed to indicate the relationship between lactate and 28-day mortality (Fig. 2).
Predictive Performance of Lactate for 28-Day Mortality
Table 5 and Supplementary Fig. 2 summarize the predictive performance of lactate. The area under the ROC curve (AUC) of lactate was 0.618 (95% CI 0.599–0.635) and the cutoff value of lactate was 2.4 mmol/l with a sensitivity of 0.483 and a specificity of 0.687.
Discussion
In this study, we found a non-linear positive relationship between lactate and 28-day mortality in elderly patients with sepsis. In addition, a prognostic value of lactate was identified. To the best of our knowledge, this was the first study to explore the association of serum lactate with clinical outcomes in elderly patients with sepsis based on MIMIC-IV.
Lactate level is associated with mortality in sepsis, which should be evaluated within 1 h after admission [18]. Much evidence was accumulated clarifying that there is a significant prognostic value of lactate in sepsis [19,20,21]. One study in adult sepsis showed that for predicting mortality, the cutoff value of lactate was 1.6 mmol/l with a sensitivity of 79.59% and a specificity of 32.10% [22]. In pediatric sepsis, initial lactate level > 2 mmol/l was significantly related to 30-day mortality (OR 3.26, 95% CI 1.16–9.16) [23]. In addition, lactate level > 2 mmol/l was also able to provide sufficient sensitivity for predicting mortality in elderly sepsis admitted to the emergency department [24], a result which was partly consistent with ours. One large retrospective study found that lactate ≥ 4 mmol/l was associated not only with short-term outcomes but also with 1-year mortality in sepsis (OR 1.80, 95% CI 1.40–2.60) [25]. Recent machine learning research on elderly sepsis demonstrated that lactate level was one of most important variables in the prognostic model [26].
Our study showed that after adjustment for all potential cofounders, for each 1 mmol/l increment in lactate, the OR of 28-day mortality was 1.23 (95% CI 1.18–1.28, P < 0.0001). Kaplan–Meier analysis for cumulative hazard in 28-day mortality also indicated that the higher the level of lactate was, the higher the risk of 28-day mortality in elderly patients with sepsis was. Elevated level of lactate caused by sepsis could be explained with several mechanisms. Sepsis usually leads to adrenergic stimulation, which results in activation of some enzymes and acceleration of glycolysis tissues, resulting in excess production of lactate [27]. Moreover, mitochondrial function, which normally converts lactate into energy, is impaired by sepsis, potentially causes lactate accumulation and hyperlactatemia [28]. Inflammatory response can activate immune cells, which is another source of lactate in sepsis [29].
The strength of the present study is that the results could enable physicians to perform risk stratification for elderly patients with sepsis based on the different lactate levels. However, some limitations also should be discussed. First, as a result of the lack of some data, some factors including interventions and drugs which might affect the prognosis were not enrolled for the study. Second, this was a retrospective study from a US public database. Bias could not be avoided and the generalizability of our conclusion might not be suitable for patients in other countries or regions.
Conclusion
In elderly patients with sepsis, a non-linear positive relationship was discovered between serum lactate and 28-day mortality. Physicians should be alert to lactate assessment at admission and pay more attention to those patients with higher levels of lactate.
References
Urushidani S, Kuriyama A, Matsumura M. Blood gas analysis results and serum lactate levels in patients with psychogenic hyperventilation and urinary tract infection with suspected sepsis: a retrospective comparative study. Intern Med. 2021. https://doi.org/10.2169/internalmedicine.8434-21.
Webb AL, Kramer N, Rosario J, et al. Delta lactate (three-hour lactate minus initial lactate) prediction of in-hospital death in sepsis patients. Cureus. 2020;12(4):e7863.
Weinberger J, Klompas M, Rhee C. What is the utility of measuring lactate levels in patients with sepsis and septic shock? Sem Respir Crit Care Med. 2021;42(5):650–61.
Gupta MK, Yadav G, Singh Y, Bhalekar A. Correlation of the changing trends of red cell distribution width and serum lactate as a prognostic factor in sepsis and septic shock. J Anaesthesiol Clin Pharmacol. 2020;36(4):531–4.
Yoon S, Choi B, Eun S, Bae G, Koo C, Kim M. Using the lactate-to-albumin ratio to predict mortality in patients with sepsis or septic shock: a systematic review and meta-analysis. Eur Rev Med Pharmacol Sci. 2022;26(5):1743–52.
Jouffroy R, Vivien B. Initial antimicrobial management of sepsis: increased prehospital blood lactate levels for identifying sicker patients who may benefit from prehospital antibiotic therapy initiation. Crit Care. 2021;25(1):377.
Zhang M, Zhang Q, Yu Y, An L, Qi Z, Li C. Effects of early hemodynamics, oxygen metabolism, and lactate dynamics on prognosis of post-cardiac arrest syndrome. Chin Med J. 2021;135(3):344–6.
Çınar E, Usul E, Demirtaş E, Gökçe A. The role of trauma scoring systems and serum lactate level in predicting prognosis in thoracic trauma. Turk J Trauma Emerg Surg. 2021;27(6):619–23.
Gao Y, Zhang H, Zhong H, Yang S, Wang Q. Lactate and blood ammonia on admission as biomarkers to predict the prognosis of patients with acute mushroom poisoning and liver failure: a retrospective study. Toxicol Res. 2021;10(4):850–5.
Hotchkiss R, Moldawer L, Opal S, Reinhart K, Turnbull I, Vincent J. Sepsis and septic shock. Nat Rev Dis Primers. 2016;2:16045.
Ding XF, Yang ZY, Xu ZT, et al. Early goal-directed and lactate-guided therapy in adult patients with severe sepsis and septic shock: a meta-analysis of randomized controlled trials. J Transl Med. 2018;16(1):331.
Hernández-Quiles R, Merino-Lucas E, Boix V, et al. Bacteraemia and quick Sepsis Related Organ Failure Assessment (qSOFA) are independent risk factors for long-term mortality in very elderly patients with suspected infection: retrospective cohort study. BMC Infect Dis. 2022;22(1):248.
Cuijpers ACM, Coolsen MME, Schnabel RM, et al. Self-perceived recovery and quality of life in elderly patients surviving ICU-admission for abdominal sepsis. J Intensive Care Med. 2021. https://doi.org/10.1177/08850666211052460.
Zincircioğlu Ç, Rollas K, Güldoğan I, et al. Diagnostic value of procalcitonin and C reactive protein for infection and sepsis in elderly patients. Turk J Med Sci. 2021. https://doi.org/10.3906/sag-2007-268.
Devia Jaramillo G, Ibáñez Pinilla M. Quick sequential organ failure assessment, sequential organ failure assessment, and procalcitonin for early diagnosis and prediction of death in elderly patients with suspicion of sepsis in the emergency department, based on Sepsis-3 definition. Gerontology. 2022;68(2):171–80.
Johnson A, Stone D, Celi L, Pollard T. The MIMIC code repository: enabling reproducibility in critical care research. J Am Med Inf Assoc. 2018;25(1):32–9.
Johnson A, Pollard T, Shen L, et al. MIMIC-III, a freely accessible critical care database. Sci Data. 2016;3: 160035.
Evans L, Rhodes A, Alhazzani W, et al. Surviving Sepsis Campaign: international guidelines for management of sepsis and septic shock 2021. Crit Care Med. 2021;49(11):e1063–143.
Sauer C, Gómez J, Botella M, et al. Understanding critically ill sepsis patients with normal serum lactate levels: results from US and European ICU cohorts. Sci Rep. 2021;11(1):20076.
Baysan M, Baroni GD, van Boekel AM, Steyerberg EW, Arbous MS, van der Bom JG. The added value of lactate and lactate clearance in prediction of in-hospital mortality in critically ill patients with sepsis. Crit Care Explor. 2020;2(3): e0087.
Lee SG, Song J, Park DW, et al. Prognostic value of lactate levels and lactate clearance in sepsis and septic shock with initial hyperlactatemia: a retrospective cohort study according to the Sepsis-3 definitions. Medicine (Baltimore). 2021;100(7):e24835.
Charoentanyarak S, Sawunyavisuth B, Deepai S, Sawanyawisuth K. A point-of-care serum lactate level and mortality in adult sepsis patients: a community hospital setting. J Prim Care Community Health. 2021;12:21501327211000230.
Scott HF, Brou L, Deakyne SJ, Kempe A, Fairclough DL, Bajaj L. Association between early lactate levels and 30-day mortality in clinically suspected sepsis in children. JAMA Pediatr. 2017;171(3):249–55.
Cheng HH, Chen FC, Change MW, et al. Difference between elderly and non-elderly patients in using serum lactate level to predict mortality caused by sepsis in the emergency department. Medicine (Baltimore). 2018;97(13):e0209.
Villar J, Short J, Lighthall G. Lactate predicts both short- and long-term mortality in patients with and without sepsis. Infect Dis. 2019;12:1178633719862776.
Zhang L, Huang T, Xu F, et al. Prediction of prognosis in elderly patients with sepsis based on machine learning (random survival forest). BMC Emerg Med. 2022;22(1):26.
Jagan N, Morrow L, Walters R, et al. Sympathetic stimulation increases serum lactate concentrations in patients admitted with sepsis: implications for resuscitation strategies. Ann Intensive Care. 2021;11(1):24.
Iepsen UW, Plovsing RR, Tjelle K, et al. The role of lactate in sepsis and COVID-19: perspective from contracting skeletal muscle metabolism. Exp Physiol. 2021. https://doi.org/10.1113/EP089474.
Weiss S, Henrickson S, Lindell R, et al. Influence of immune cell subtypes on mitochondrial measurements in peripheral blood mononuclear cells from children with sepsis. Shock. 2021. https://doi.org/10.1097/SHK.0000000000001903.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article. The Rapid Service Fee was funded by the authors.
Author Contributions
Conception and design: Ning Ding. Administrative support: Ning Ding, Liudang He. Provision of study materials or patients: Ning Ding, Liudang He. Collection and assembly of data: Ning Ding, Donghua Yang, Qiong Ding. Data analysis and interpretation: Yingjie Su, Ning Ding. Manuscript writing: Ning Ding. Final approval of manuscript: All authors.
Disclosures
All the authors including Liudang He, Donghua Yang, Qiong Ding, Yingjie Su, Ning Ding have nothing to disclose.
Compliance with Ethics Guidelines
This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. MIMIC-IV is an anonymized public database. The project was approved by the institutional review boards of the Massachusetts Institute of Technology (MIT) and Beth Israel Deaconess Medical Center (BIDMC) and was given a waiver of informed consent.
Data Availability
The data that support the findings of this study are available from the Massachusetts Institute of Technology (MIT) and Beth Israel Deaconess Medical Center (BIDMC) but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are, however, available from the authors upon reasonable request and with permission of the Massachusetts Institute of Technology (MIT) and Beth Israel Deaconess Medical Center (BIDMC).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
He, L., Yang, D., Ding, Q. et al. Association Between Lactate and 28-Day Mortality in Elderly Patients with Sepsis: Results from MIMIC-IV Database. Infect Dis Ther 12, 459–472 (2023). https://doi.org/10.1007/s40121-022-00736-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-022-00736-3