Abstract
Legionellosis is the infection caused by bacteria of the genus Legionella, including a non-pneumonic influenza-like syndrome, and Legionnaires’ disease is a more serious illness characterized by pneumonia. Legionellosis is becoming increasingly important as a public health problem throughout the world; although it is an underreported disease, studies have consistently documented a high incidence. In addition, health costs associated with the disease are high. Diagnosis of Legionnaires’ disease is based mainly on the detection of Legionella pneumophila serogroup 1 antigen in urine. However, there have been advances in detection tests for patients with legionellosis. New methodologies show greater sensitivity and specificity, detect more species and serogroups of Legionella spp., and have the potential for use in epidemiological studies. Testing for Legionella spp. is recommended at hospital admission for severe community-acquired pneumonia, and antibiotics directed against Legionella spp. should be included early as empirical therapy. Inadequate or delayed antibiotic treatment in Legionella pneumonia has been associated with a worse prognosis. Either a fluoroquinolone (levofloxacin or moxifloxacin) or a macrolide (azithromycin preferred) is the recommended first-line therapy for Legionnaires’ disease; however, little information is available regarding adverse events or complications, or about the duration of antibiotic therapy and its association with clinical outcomes. Most published studies evaluating antibiotic treatment for Legionnaires’ disease are observational and consequently susceptible to bias and confounding. Well-designed studies are needed to assess the usefulness of diagnostic tests regarding clinical outcomes, as well as randomized trials comparing fluoroquinolones and macrolides or combination therapy that evaluate outcomes and adverse events.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Legionellosis is becoming an important public health threat. The incidence of legionellosis is rising and the health costs associated with the disease are high. |
Diagnosis of Legionnaires’ disease is based mainly on the detection of Legionella pneumophila serogroup 1 antigen in urine. |
Other diagnostic methods such as culture and PCR allow the detection of cases due to most species and serogroups but have some drawbacks. |
Most guidelines recommend the use of Legionella diagnostic tests in patients with severe community-acquired pneumonia or whenever Legionnaires’ disease is suspected based on epidemiological or clinical features. |
Either a fluoroquinolone (levofloxacin or moxifloxacin) or a macrolide (azithromycin preferred) is the recommended first-line therapy for Legionnaires’ disease. |
Delayed antibiotic treatment in Legionella pneumonia is a factor associated with a worse prognosis. |
Randomized trials comparing fluoroquinolones with macrolides and evaluating adverse events in the treatment of Legionella pneumonia are now needed. |
The Scale of the Problem
Legionella is a genus of intracellular, aerobic, non-sporing, Gram-negative bacteria. Legionella species have been found worldwide, mainly from soil and natural or artificial aqueous reservoirs including freshwater streams, lakes, showers, pools, sprinklers, or cooling towers [1, 2]. Most human infections are caused by Legionella pneumophila, but other disease-causing species reported include L. longbeachae in Australia and New Zealand. Numerous serogroups of L. pneumophila and other Legionella spp. have been discovered; currently around 65 species of Legionella have been described [1, 3,4,5,6].
The term legionellosis refers to the infection caused by bacteria of the genus Legionella. The clinical spectrum includes a non-pneumonic, influenza-like syndrome known as Pontiac fever, and Legionnaires’ disease, which is a more severe presentation characterized by pneumonia. Legionella pneumophila associated with human infection was first described in 1977, after an outbreak of severe pneumonia at the American Legion Convention held in 1976 in Philadelphia, USA [1, 2]. Legionnaires’ disease has clinical manifestations like those of other types of pneumonia, and as it lacks a particular pattern, microbiological tests are the key element for its diagnosis. Most cases of Legionnaires’ disease are sporadic, and more than 70% are community-acquired, though some are associated with travel or health care [7]. Legionella spp. are estimated to be the causative agent of 2–10% of community-acquired pneumonia (CAP) cases, with a higher incidence in severe disease [8,9,10,11]. However, studies have shown that adhering to guidelines and recommendations for diagnostic testing results in poor sensitivity for identifying patients with Legionnaires’ disease [12]. Predisposing conditions for legionellosis include advanced age, male sex, immunosuppression, chronic lung disease, alcohol abuse, malignancies, iron overload, anti-tumor necrosis factor (TNF)-alpha treatment and smoking (current or past) [1, 2, 7, 13].
In the present study, we performed a narrative review to update information regarding the diagnosis and treatment of Legionnaires’ disease. This article is based on previously published work and does not contain novel data or information related to human or animal studies; no permission was required from the institutional ethics review board.
Morbidity and mortality in Legionnaires' disease remains high. Intensive care unit (ICU) admission rates reported in studies range from 20 to 27% [1, 7, 14,15,16]. Andrea et al. [14] also found elevated frequency of invasive mechanical ventilation, septic shock, acute respiratory distress syndrome, and acute kidney injury among those patients requiring ICU admission. Moreover, Legionnaires' disease has an overall mortality rate of 4–18% [7, 14,15,16,17,18]. However, mortality is higher in patients with nosocomial Legionella pneumonia, immunocompromised individuals, and those requiring ICU admission. Regueiro-Mira et al. [15] found that mortality was 4.6% in medical wards compared with 23.1% in patients transferred to the ICU. Other studies have documented mortality rates close to 40% in transplant recipients or cases of hospital-acquired infection [1, 13, 19,20,21].
Although information on legionellosis has improved in recent decades, its incidence remains unknown, mainly because it is underdiagnosed and underreported. Countries differ in terms of their level of surveillance, diagnostic methods, and investigation efforts [1, 2, 22, 23]. An increase in the incidence of the condition has been documented, although the causes are not entirely clear. The growth may be due to an increase in infections or an aging population, or perhaps to changes in climate, reporting criteria, or testing practices (for example, the increase in the use of urine antigen testing or polymerase chain reaction), or to a combination of these factors [23, 24]. A study of all cases of legionellosis reported to the US Centers for Disease Control and Prevention from 1990 through 2005 found an increase in reported cases from a mean of 1268 yearly cases before 2003 to more than 2000 from 2003 through 2005 [25]. More recently, 6141 cases were reported in 2016 and 7458 in 2017 [26]. Another retrospective study evaluated Legionnaires’ disease-associated hospitalizations using the US National Hospital Discharge Survey (NHDS) data from 2006 to 2010, and found significant increases in Legionnaires’ over the 5-year study period (from 5.37 per 100,000 population in 2006 to 9.66 in 2010, with a peak in 2009 of 17.07) [22]. Likewise, the European Legionnaires’ disease Surveillance Network (ELDSNet) reported that the notification rates for Legionnaires’ disease have nearly doubled in the past few years, from 1.4 in 2015 to 2.2 per 100,000 population in 2019, and mostly involved men aged 65 years and above. Four countries (France, Germany, Italy, and Spain) accounted for nearly 70% of all reported cases [27]. Similar increases in the incidence of Legionnaires’ disease in recent years have been reported in other studies [28, 29].
Estimates of the costs associated with Legionnaires’ disease could also help to draw attention to the scale of the problem and to the need for prevention and treatment efforts. The studies estimate direct medical costs incurred due to hospitalizations and emergency department visits, and those related to productivity losses caused by absenteeism and premature deaths. Legionnaires’ disease is the second most expensive waterborne disease reported in the United States, with the cost per hospital stay ranging from US$ 7950 to $149,000 in terms of direct health care costs derived from emergency room visits and hospitalizations [30]. Similarly, Baker-Goering et al. [31] assessed productivity losses combined with existing estimates of medical costs of Legionnaires’ disease in the United States for 2014. The economic burden of Legionnaires’ disease was more than double when lifetime productivity losses were added to medical costs and was approximately US$ 835 million, including US$ 21 million caused by absenteeism and US$ 412 million caused by premature deaths. Moreover, a study of Legionnaires’ disease in Belgium evaluated disability-adjusted life year (DALY) rates, with DALYs being the sum of the years of life lost due to premature mortality and the years lived with a disability due to a disease or health condition in a population. One DALY is the loss of the equivalent of 1 year of full health. Legionnaires’ disease caused 3.05 DALYs per case and 8147 total DALYs in Belgium in 2017, which corresponds to 71.9 (95% uncertainty interval: 39.33–109.75) DALYs per 100,000 persons [29].
Given the rising incidence and high costs associated with the disease, legionellosis is gradually becoming a major public health threat. Data on the burden of the disease show the value of studying the epidemiology and of increasing investment in measures to prevent Legionnaires’ disease, such as water management programs and investigations of the outbreaks.
Diagnosis of Legionnaires’ Disease
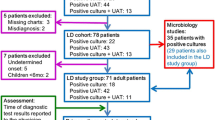
The diagnosis of legionellosis is based on a combination of the presence of clinical and/or radiological symptoms and laboratory tests. These tests are not routinely performed by the clinical microbiology laboratory and therefore must be specifically requested (Table 1). According to a 2019 European Centre for Disease Prevention and Control (ECDC) report, most cases in Europe (90%) are diagnosed using the urine antigen test (UAT) method. This has been a consistent finding over the past decade. Polymerase chain reaction (PCR) detects 9% of the total number of reported cases, and the proportion of cases diagnosed or confirmed by culture is 10% [32]. The species L. pneumophila alone is responsible for more than 90% of cases of Legionnaires’ disease diagnosed worldwide. In Europe, most human cases (80%) are caused solely by L. pneumophila serogroup 1 (Lp1), with other serogroups and species accounting for 16% and 3% of infections, respectively [27]. In Australia and New Zealand, L. longbeachae is the predominant species and in 2019 accounted for up to 60% of the reported cases [4, 5, 33].
Culture of respiratory samples is still considered the gold standard for diagnosis of legionellosis, but it is a very demanding test requiring considerable expertise and growth for several days on complex media. Legionella does not grow on the standard media used in microbiology laboratories, and a specific medium containing yeast extract and activated charcoal (buffered charcoal yeast extract, BCYE) is needed. Legionella has been more successfully isolated from lower respiratory tract samples than from nasopharyngeal or throat swabs, and culture positivity in samples outside the respiratory tract is extremely rare [34]. The main advantage of the culture approach is that it enables isolation of the bacterial strain, which can be used for antibiotic sensitivity testing and for epidemiological typing analyses [35]. The availability of the clinical strain for comparison with environmental strains is one of the key points in epidemiological investigations for understanding the spread of legionellosis—hence the importance of culture in the diagnosis of legionellosis [36]. The disadvantages are of course the slowness of the analysis (which can take up to 14 days), poor sensitivity compared with other techniques, and the restricted availability of suitable clinical material (preferably from the lower respiratory tract) [37]. Some guidelines have recommended the culture of Legionella in patients with severe CAP or whenever Legionnaires’ disease is suspected based on epidemiological or clinical features. In addition, Legionella cultures should be routinely performed on invasive respiratory samples or for patients who have a positive Legionella UAT [38].
The introduction in the late 1990s of enzyme immunoassays for the detection of L. pneumophila antigen in urine made it possible to speed up the diagnosis of Legionnaires’ disease [39]. The antigen detected is a bacterial lipopolysaccharide (LPS), on whose diversity of structure and antigenicity the identification of L. pneumophila serogroups is based. The antigen is detectable in most patients as early as 1–3 days after the onset of symptoms but may persist for several weeks or months [40]. The development and spread of rapid urinary antigen detection kits such as lateral flow immunochromatographic assays or fluorescent immunoassays has revolutionized the diagnosis of legionellosis and allows for early adaptation of the antibiotic therapy. These methods can be implemented in a point-of-care format and today constitute the first-line diagnostic tests for Legionnaires' disease. Commercially available kits mainly detect Lp1 LPS and do not perform as well with strains belonging to other serogroups. The sensitivity therefore depends on the serotype causing the infection and may vary from 86% for Lp1 to 74–79% when considering all serogroups [41].
There are some differences in UAT use criteria between countries. In most guidelines, routine use of the Legionella UAT is not recommended. In this regard, American and European guidelines advise the use of a UAT for Legionnaires' disease only for adults with severe CAP or in patients with risk factors, such as recent travel or a link to a Legionella outbreak. In contrast, other guidelines recommend Legionella UAT for all patients admitted with CAP [42, 43]. An important drawback of UAT is the occurrence of non-specific signals, possibly due to the presence in urine of immunocomplexes that interact with the test and give false positive results [44, 45]. This phenomenon has been known since the 1980s and can be resolved by heating the urine for 5 min at 100 °C [46, 47]. Since the Legionella LPS is heat-stable, heating of the urine sample allows the release of bacterial polysaccharides from antibody complexes and eliminates the nonspecific interferences. This simple heating procedure is recommended for the confirmation of any positive test [39, 48, 49]. Another factor that can cause false positive results is the persistence of Legionella antigen in the urine. Even recent studies have shown that the antigen can still be detected several months (up to 1 year) after the onset of symptoms. This occurs in about 10% of cases and mainly in patients with severe underlying diseases or in immunocompromised individuals [50, 51].
The advantages of urinary antigen detection over other diagnostic methods are considerable. Urine samples are easily obtained, the antigen is detectable very early in the course of the disease, and the test is quick and easy to perform. For the clinician, the test’s usefulness lies in its high positive predictive value. In the presence of suggestive symptoms, while a positive result strongly suggests legionellosis, a negative test does not exclude Legionella spp. as the cause of the pneumonia [52, 53]. In 2019, approximately 90% of reported cases in Europe were diagnosed by urinary antigen. This percentage has increased over the years and has certainly contributed to better diagnosis of the disease [27, 32]. Nevertheless, experts wonder about the importance of cases that are not detected by UAT because they are due to other species or other serogroups for which these tests do not seem to perform as well as for Lp1 [54, 55]. Most commercially available UAT tests are based on lipopolysaccharide detection, which is why they are mainly able to diagnose pneumonia due to L. pneumophila serogroup 1 [41, 56]. Recently, UAT tests based on the detection of other antigens such as ribosomal protein L7/L12 have been developed and launched on the market. Although scientific studies are so far limited, these tests seem very promising and have the capacity to detect other serogroups and even other species [57, 58].
PCR is a method that has the potential to detect all known Legionella species. It is a rapid test with good specificity and sensitivity for Legionella spp., especially when performed on respiratory tract samples (bronchial secretions, bronchoalveolar lavage [BAL], biopsies, or sputum) [59]. The possibility of also performing this assay in materials such as urine or serum would avoid the problem of having to obtain a respiratory sample. Unfortunately, the few studies available that have evaluated PCR in serum and urine have shown low sensitivity [60,61,62,63]. Numerous panels are commercially available and allow the amplification of L. pneumophila and/or Legionella spp. The design of specific PCRs also makes it possible to design specific assays for the detection of particular serogroups [64,65,66] and specific sequence types [67, 68]. In general, Legionella nucleic acid-based detection offers significant advantages in terms of sensitivity and speed. However, there are several disadvantages and limitations. PCR may not be ideal for testing non-lower respiratory tract samples such as urine and serum. In addition, one drawback of all nucleic acid amplification methods is the difficulty in assessing bacterial viability (i.e., after antibiotic treatment) and causing false positive results. Finally, nucleic acid amplification technologies still require specially trained personnel and sophisticated machines, although thanks to the technological advances we have witnessed in recent years, they are increasingly accessible to a wider range of laboratories with a moderate budget [35, 38]. Compared with UAT, PCR offers higher sensitivity. One study revealed an additional diagnosis of 18–30% of LD cases [69]. Similarly, an Italian study showed that the use of real-time PCR in addition to UAT and culture resulted in an increase of 18% of the LD cases [70].
In Europe, the use of PCR seems to have remained quite restricted (< 10%) despite its many advantages [32]. With the increasing use of multi-syndromic PCR panels targeting multiple microorganisms simultaneously, the use of PCR to detect Legionella is expected to increase in the diagnosis of CAP. Some of these PCR panels have been developed for use with BALs, while other tests can also be performed with samples from the upper respiratory tract such as nasopharyngeal smears and sputum [71]. The growth in the popularity of whole-genome sequencing techniques reflects their high diagnostic potential, and they are becoming increasingly affordable. Recent studies also demonstrate their value for microbial identification and in epidemiological studies [72,73,74].
Antimicrobial Treatment
Delayed Therapy and Prognosis
The literature on the association between the time of the onset of therapy and the prognosis in Legionnaires’ disease is scarce [75,76,77,78]. In a retrospective study, Heath et al. [75] reported that the delay in antibiotic initiation after hospital admission and the total delay in appropriate antibiotic initiation after symptoms onset were both factors related to higher mortality in Legionella pneumonia. Following the diagnosis of pneumonia, the median delay before starting therapy was 5 days (range, 1–10 days) for patients who died, and 1 day for those who survived (range, 1–5 days) (p < 0.001). In addition, the total delay after symptom onset in starting therapy ranged from 1 to 12 days (median, 6 days) for survivors and from 8 to 23 days (median, 11 days) for non-survivors (p < 0.001). Another study compared the outcomes of patients with severe Legionella pneumonia requiring ICU care according to the delays in initiating fluoroquinolones and macrolides [76]. After logistic regression analysis, fluoroquinolone administration within 8 h of ICU admission was associated with reduced mortality. Moreover, a recent single-center, retrospective study carried out in Pisa, Italy, showed that delayed macrolide/levofloxacin therapy (> 24 h of hospital admission) was associated with a higher need for ICU admission [77]. The frequency of ICU admission was 54.2% among those who received macrolides/levofloxacin therapy within 24 h of admission and 80.4% in those who initiated therapy later. Interestingly, the investigators also found that the delay in the administration of antibiotics against Legionella was directly correlated with a delay in the performance of the UAT. Similarly, in a study that reported 23% inadequate empirical coverage during the first 2 days of hospitalization in patients diagnosed with Legionella pneumonia, factors related to inadequate coverage were older age, renal replacement therapy, chronic heart failure, nonsmoking status, and having risk for hospital-acquired pneumonia or multidrug-resistant pathogens [9].
These findings indicate that it is necessary to test for Legionella spp. at the time of hospital admission in severe CAP and to decide promptly whether to withdraw or continue antibiotic treatment according to the test results. This strategy improves antimicrobial prescription and prognosis in patients. If the UAT is not available at the time of CAP diagnosis, initial antimicrobial therapy should include a drug with activity against Legionella spp. It is recommended that antibiotics directed against Legionella spp. be included promptly in the empirical therapy of severe cases of CAP and in cases of immunocompromised patients. Inadequate or delayed antibiotic treatments in Legionella pneumonia have been associated with worse prognosis [75,76,77].
Fluoroquinolones or Macrolides
Several studies have evaluated the role of fluoroquinolones or macrolides in Legionella pneumonia. Most of them are observational, and the number of randomized trials is small. The current guidelines for CAP recommend either a fluoroquinolone (levofloxacin or moxifloxacin) or a macrolide (preferably azithromycin) as first-line therapy for Legionnaires’ disease [79, 80].
In this regard, a recent systematic review and meta-analysis compared the effectiveness of fluoroquinolone versus macrolide monotherapy in Legionella pneumonia [81]. A total of 3525 patients from 21 publications were included in this meta-analysis. No difference in mortality was found between patients treated with fluoroquinolones and those treated with macrolides (6.9% vs 7.4%, pooled OR 0.94, 95% CI 0.71–1.25, p = 0.66). Similar results were reported for comparison of fluoroquinolones versus azithromycin and for fluoroquinolones versus clarithromycin. The mortality rates for fluoroquinolones and macrolides in studies that were solely ICU-based was also similar. Moreover, the authors also found no differences in the effect of these antibiotics on clinical cure, length of hospital stay, or the occurrence of complications. Likewise, Kato et al. [82] performed a meta-analysis comparing these treatment groups in terms of their efficacy and safety in Legionella pneumonia, including studies published until January 2020. Seventeen publications met the inclusion criteria. Clinical cure was comparable between the treatment groups, but overall and 30-day mortality was significantly higher for macrolides than for fluoroquinolones. However, in the subgroup analyses, levofloxacin significantly reduced the length of hospital stay compared with two specific macrolides (azithromycin and clarithromycin), although mortality did not differ significantly between the treatment groups. Nor were significant differences found in other outcomes such as time to apyrexia and adverse events.
The results of these systematic reviews and meta-analyses support the present guidelines regarding the use of a fluoroquinolone or a macrolide for the treatment of Legionella pneumonia. However, certain limitations of the current data should be recognized [81,82,83]. First, the usefulness of these antibiotics has not been extensively evaluated in some subgroups of patients, such as immunocompromised patients or those requiring admission to the ICU. Second, the reporting of adverse events or complications varies widely in the currently available studies. Third, the duration of antibiotic therapy and its association with clinical outcomes has not been sufficiently assessed. Fourth, most published studies are observational and are therefore susceptible to bias and confounders. Ideally, randomized trials comparing fluoroquinolones with macrolides for the treatment of Legionella pneumonia should be conducted. Finally, future studies need to evaluate and monitor antibiotic susceptibility data on Legionella spp. Some studies have documented, in general, low values of minimum inhibitory concentrations in environmental and clinical strains, although determinants of resistance to macrolides, such as the LpeAB active efflux system, have also rarely been found [84,85,86].
Combination Therapy
Several in vitro studies suggest a synergistic effect of combination therapy in isolates of Legionella spp. [87,88,89,90]. Martin et al. [87] tested the synergy of erythromycin, clarithromycin, and azithromycin, each in combination with ciprofloxacin and levofloxacin, against 41 isolates of Legionella. The authors did not report any antagonism. Synergy occurred mainly for the clarithromycin-levofloxacin and azithromycin-levofloxacin combinations. Similarly, another study evaluated the susceptibilities of 56 L. pneumophila isolates to levofloxacin, ofloxacin, erythromycin, and rifampin, finding that only levofloxacin plus rifampin demonstrated synergy [88]. Moreover, evaluating the intracellular susceptibility of several antibiotic combinations against L. pneumophila in infected macrophages, Descours et al. [89] found that macrolides, especially azithromycin, were synergistic with rifampicin against Legionella in this in vitro model.
Observational studies have also assessed the synergistic effect of combination therapy in patients with Legionella pneumonia. In a literature review evaluating the role of rifampin in the combination treatment of L. pneumophila pneumonia, Varner et al. [91] concluded that the data on the clinical advantage of rifampin combination therapy are unclear because of the possibility for patient selection bias and the absence of consistent comparators. In an observational cohort study, Grau et al. [92] found that patients who received rifampicin in addition to clarithromycin to treat Legionnaires’ disease had a 50% longer hospital stay and a trend towards elevated bilirubin levels. Combination therapy of clarithromycin and rifampicin had no additional benefit in prognosis compared with clarithromycin monotherapy. Similarly, Blázquez-Garrido et al. [93] compared macrolides versus levofloxacin, in addition to rifampicin, in a prospective, non-randomized study involving 292 patients with Legionella pneumonia. Although the use of levofloxacin was associated with fewer complications and shorter hospital stays compared with macrolides, the addition of rifampicin to the treatment regimen provided no additional benefit. Moreover, the efficacy of combination therapy with macrolides plus quinolones in patients with severe Legionella pneumonia has been reported [94, 95]. In some of the cases described, combination therapy was used because of initial failure with a monotherapy. All the patients survived. Finally, a retrospective study compared the clinical effects of single-agent therapies, fluoroquinolones and macrolides, with combination therapy in the treatment of 22 patients with L. pneumophila pneumonia [96]. A fluoroquinolone combined with a macrolide may be able to improve the inflammation caused by L. pneumophila pneumonia, although there were no significant differences in outcomes.
Based on the literature reviewed here, combination therapy has most often been suggested for use in patients with treatment failure or severe disease, but the data available are limited. Only observational studies evaluating combination therapies in Legionella pneumonia have been performed, with small sample sizes; no randomized trials have been conducted. Nor have the adverse effects and possible drug-drug interactions been adequately evaluated in the studies carried out to date.
Duration of Treatment
According to the guidelines, the duration of antibiotic therapy in CAP should continue until the patient reaches clinical stability and for no less than a total of 5 days [80]. Several meta-analyses have demonstrated the efficacy of shorter courses of antibiotic therapy of 3–7 days [97,98,99]. However, most randomized trials evaluating the duration of antibiotic therapy had a low number of patients with Legionella pneumonia [100,101,102]. In a multicenter, noninferiority randomized clinical trial to validate Infectious Diseases Society of America/American Thoracic Society guidelines for the duration of antibiotic treatment in hospitalized patients with CAP, Uranga et al. [102] found clinical success to be similar between study groups (antibiotics for a minimum of 5 days or according to physicians). Of the 312 patients included in the study, 11 (3.5%) had Legionella pneumonia. Similarly, the number of patients with Legionella pneumonia was zero or not reported in other randomized trials evaluating short courses of antibiotic therapy in CAP [100, 101]. In a retrospective study, Kuzman et al. [103] assessed the clinical usefulness of azithromycin in the treatment of serologically confirmed L. pneumophila pneumonia. The mean age of 16 patients was 42.8 years and they did not have severe chronic cardiac or pulmonary diseases or immunodeficiency. Azithromycin was administered orally for 5 days (first day 500 mg and remaining days 250 mg, once daily) or for 3 days (500 mg once daily). All patients were effectively cured with azithromycin.
The optimal duration of antibiotic therapy for Legionnaires’ disease has not been established, and it may vary according to the antimicrobial agent used, disease severity, and response to therapy. Of note, there are no randomized studies evaluating the duration of antibiotic therapy specifically in patients with Legionella pneumonia. The recommended total duration of antibiotic treatment in mild disease is 3–7 days, and until the patient is clinically stable and afebrile for at least 48 h. However, extended courses of therapy (10–14 days or longer based on clinical response) are reserved for immunocompromised patients, those with complications (e.g., empyema, or extrapulmonary infection), and patients with severe pneumonia or chronic comorbidities [104,105,106]. Levofloxacin or azithromycin for 7–10 days is recommended in cases of moderate to severe Legionella pneumonia. For immunocompromised hosts, a 21-day course of levofloxacin or a 10-day course of azithromycin is usually recommended [105,106,107].
References
Viasus D, Carratalà J. Legionellosis and Legionnaires’ disease. In: Oxford textbook of medicine. 6th ed. Oxford: Oxford University Press; 2020.
Cunha BA, Burillo A, Bouza E. Legionnaires’ disease. Lancet. 2016;387:376–85.
Fields BS, Benson RF, Besser RE. Legionella and Legionnaires’ disease: 25 years of investigation. Clin Microbiol Rev. 2002;15:506–26.
Priest PC, Slow S, Chambers ST, et al. The burden of Legionnaires’ disease in New Zealand (LegiNZ): a national surveillance study. Lancet Infect Dis. 2019;19:770–7.
Chambers ST, Slow S, Scott-Thomas A, Murdoch DR. Legionellosis caused by non-Legionella pneumophila species, with a focus on Legionella longbeachae. Microorganisms. 2021;9:291.
Chauhan D, Shames SR. Pathogenicity and virulence of Legionella: intracellular replication and host response. Virulence. 2021;12(1):1122–44.
Burillo A, Pedro-Botet ML, Bouza E. Microbiology and epidemiology of Legionnaires’ disease. Infect Dis Clin N Am. 2017;31:7–27.
Viasus D, Di Yacovo S, Garcia-Vidal C, et al. Community-acquired Legionella pneumophila pneumonia: a single-center experience with 214 hospitalized sporadic cases over 15 years. Medicine (Baltimore). 2013;92:51–60.
Allgaier J, Lagu T, Haessler S, et al. Risk factors, management, and outcomes of Legionella pneumonia in a large, Nationally representative sample. Chest. 2021;159:1782–92.
Gramegna A, Sotgiu G, Di Pasquale M, GLIMP Study Group, et al. Atypical pathogens in hospitalized patients with community-acquired pneumonia: a worldwide perspective. BMC Infect Dis. 2018;18:677.
Arancibia F, Cortes CP, Valdés M, et al. Importance of Legionella pneumophila in the etiology of severe community-acquired pneumonia in Santiago, Chile. Chest. 2014;145:290–6.
Bellew S, Grijalva CG, Williams DJ, et al. Pneumococcal and Legionella urinary antigen tests in community-acquired pneumonia: prospective evaluation of indications for testing. Clin Infect Dis. 2019;68:2026–33.
Farnham A, Alleyne L, Cimini D, Balter S. Legionnaires; disease incidence and risk factors, New York, New York, USA, 2002–2011. Emerg Infect Dis. 2014;20(11):1795–802.
Andrea L, Dicpinigaitis PV, Fazzari MJ, Kapoor S. Legionella pneumonia in the ICU: a tertiary care center experience over 10 years. Crit Care Explor. 2021;3(8): e0508.
Regueiro-Mira MV, Pita-Fernández S, Pértega-Díaz S, López-Calviño B, Seoane-Pillado T, Fernández-Albalat-Ruiz M. Prognostic factors in adult patients hospitalized for pneumonia caused by Legionella pneumophila. Rev Chilena Infectol. 2015;32(4):435–44.
Wingfield T, Rowell S, Peel A, Puli D, Guleri A, Sharma R. Legionella pneumonia cases over a five-year period: a descriptive, retrospective study of outcomes in a UK district hospital. Clin Med (Lond). 2013;13(2):152–9.
Gershengorn HB, Keene A, Dzierba AL, Wunsch H. The association of antibiotic treatment regimen and hospital mortality in patients hospitalized with Legionella pneumonia. Clin Infect Dis. 2015;60(11):e66-79.
Hung TL, Li MC, Wang LR, Liu CC, Li CW, Chen PL, Syue LS, Lee NY, Ko WC. Legionnaires’ disease at a medical center in southern Taiwan. J Microbiol Immunol Infect. 2018;51(3):352–8.
Dagan A, Epstein D, Mahagneh A, Nashashibi J, Geffen Y, Neuberger A, Miller A. Community-acquired versus nosocomial Legionella pneumonia: factors associated with Legionella-related mortality. Eur J Clin Microbiol Infect Dis. 2021;40(7):1419–26.
Sivagnanam S, Podczervinski S, Butler-Wu SM, Hawkins V, Stednick Z, Helbert LA, Glover WA, Whimbey E, Duchin J, Cheng GS, Pergam SA. Legionnaires' disease in transplant recipients: a 15-year retrospective study in a tertiary referral center. Transpl Infect Dis. 2017;19(5)
Cooley LA, Pondo T, Francois Watkins LK, Shah P, Schrag S, Active Bacterial Core Surveillance Program of the Emerging Infections Program Network. Population-based assessment of clinical risk factors for Legionnaires’ disease. Clin Infect Dis. 2020;70:2428–31.
Mudali G, Kilgore PE, Salim A, McElmurry SP, Zervos M. Trends in Legionnaires’ disease-associated hospitalizations, United States, 2006–2010. Open Forum Infect Dis. 2020;7:ofaa296.
Cassell K, Gacek P, Rabatsky-Ehr T, Petit S, Cartter M, Weinberger DM. Estimating the true burden of Legionnaires’ disease. Am J Epidemiol. 2019;188(9):1686–94.
Walker JT. The influence of climate change on waterborne disease and Legionella: a review. Perspect Public Health. 2018;138:282–6.
Neil K, Berkelman R. Increasing incidence of Legionellosis in the United States, 1990–2005: changing epidemiologic trends. Clin Infect Dis. 2008;47:591–9.
Centers for Disease Control and Prevention. Legionnaires Disease Surveillance Summary Report, United States, 2016–2017. Division of Bacterial Diseases, National Center for Immunization and Respiratory Diseases, CDC. https://www.cdc.gov/legionella/health-depts/surv-reporting/2016-17-surv-report-508.pdf. Accessed 1 Feb 2022.
ECDC. Legionnaires’ disease annual epidemiological report for 2019. https://www.ecdc.europa.eu/en/publications-data/legionnaires-disease-annual-epidemiological-report-2019. Accessed 1 Feb 2022.
Leung YH, Lam CK, Cheung YY, Chan CW, Chuang SK. Epidemiology of Legionnaires’ disease, Hong Kong, China, 2005–2015. Emerg Infect Dis. 2020;26:1695–702.
Fastl C, Devleesschauwer B, van Cauteren D, et al. The burden of Legionnaires’ disease in Belgium, 2013 to 2017. Arch Public Health. 2020;78:92.
Collier SA, Deng L, Adam EA, et al. Estimate of burden and direct healthcare cost of infectious waterborne disease in the United States. Emerg Infect Dis. 2021;27:140–9.
Baker-Goering M, Roy K, Edens C, Collier S. Economic burden of Legionnaires’ disease, United States, 2014. Emerg Infect Dis. 2021;27:255–7.
ECDC. European Centre for Disease Prevention and Control. Annual Epidemiological report for 2019. Legionnaires’ disease. https://www.ecdc.europa.eu/sites/default/files/documents/AER-legionnaires-2019.pdf2021. Accessed 1 Feb 2022.
Kenagy E, Priest PC, Cameron CM, et al. Risk factors for Legionella longbeachae Legionnaires’ disease. N Z Emerg Infect Dis. 2017;23(7):1148–54.
World Health Organization. Legionella and the prevention of Legionellosis. WHO; 2007.
Pierre DM, Baron J, Yu VL, Stout JE. Diagnostic testing for Legionnaires’ disease. Ann Clin Microbiol Antimicrob. 2017;16(1):59.
Essig A, von Baum H, Gonser T, Haerter G, Luck C. Microbiological diagnosis and molecular typing of Legionella strains during an outbreak of legionellosis in Southern Germany. Int J Med Microbiol. 2016;306(2):109–14.
Mercante JW, Winchell JM. Current and emerging Legionella diagnostics for laboratory and outbreak investigations. Clin Microbiol Rev. 2015;28(1):95–133.
Lim WS, Baudouin SV, George RC, Hill AT, Jamieson C, Le Jeune I, Macfarlane JT, Read RC, Roberts HJ, Levy ML, Wani M, Woodhead MA, Pneumonia Guidelines Committee of the BTS Standards of Care Committee. BTS guidelines for the management of community acquired pneumonia in adults: update 2009. Thorax. 2009;64(Suppl 3):iii1-55.
Birtles RJ, Harrison TG, Samuel D, Taylor AG. Evaluation of urinary antigen ELISA for diagnosing Legionella pneumophila serogroup 1 infection. J Clin Pathol. 1990;43(8):685–90.
Williams A, Lever MS. Characterisation of Legionella pneumophila antigen in urine of guinea pigs and humans with Legionnaires’ disease. J Infect. 1995;30(1):13–6.
Kawasaki T, Nakagawa N, Murata M, et al. Diagnostic accuracy of urinary antigen tests for legionellosis: a systematic review and meta-analysis. Respir Investig. 2021;60(2):205–14.
Menéndez R, Torres A, Aspa J, Capelastegui A, Prat C, de Castro FR, Sociedad Española de Neumología y Cirugía Torácica. Community acquired pneumonia. New guidelines of the Spanish Society of Chest Diseases and Thoracic Surgery (SEPAR). Arch Bronconeumol. 2010;46(10):543–58.
Losier A, Dela Cruz CS. New testing guidelines for community-acquired pneumonia. Curr Opin Infect Dis. 2022;35(2):128–32.
Rota MC, Fontana S, Montano-Remacha C, et al. Legionnaires’ disease pseudoepidemic due to falsely positive urine antigen test results. J Clin Microbiol. 2014;52(6):2279–80.
Como J, Moffa MA, Bhanot N, et al. Potential false-positive urine Legionella enzyme immunoassay test results. Eur J Clin Microbiol Infect Dis. 2019;38(7):1377–82.
Doskeland SO, Berdal BP. Bacterial antigen detection in body fluids: methods for rapid antigen concentration and reduction of nonspecific reactions. J Clin Microbiol. 1980;11(4):380–4.
White A, Kohler RB, Wheat LJ, et al. Rapid diagnosis of Legionnaires’ disease. Trans Am Clin Climatol Assoc. 1982;93:50–62.
Beraud L, Gervasoni K, Freydiere AM, et al. Comparison of Sofia Legionella FIA and BinaxNOW(R) Legionella urinary antigen card in two national reference centers. Eur J Clin Microbiol Infect Dis. 2015;34(9):1803–7.
Pontoizeau C, Dangers L, Jarlier V, et al. Ruling out false-positive urinary Legionella pneumophila serogroup 1 and Streptococcus pneumoniae antigen test results by heating urine. J Clin Microbiol. 2014;52(12):4347–9.
Higa F, Fujita J, Koide M, Haranaga S, Tateyama M. Clinical features of two cases of Legionnaires’ disease with persistence of Legionella urinary antigen excretion. Intern Med. 2008;47(3):173–8.
Sopena N, Sabria M, Pedro-Botet ML, Reynaga E, Garcia-Nunez M, Dominguez J, et al. Factors related to persistence of Legionella urinary antigen excretion in patients with Legionnaires’ disease. Eur J Clin Microbiol Infect Dis. 2002;21(12):845–8.
Helbig JH, Uldum SA, Bernander S, et al. Clinical utility of urinary antigen detection for diagnosis of community-acquired, travel-associated, and nosocomial legionnaires’ disease. J Clin Microbiol. 2003;41(2):838–40.
Viasus D, Calatayud L, McBrown MV, Ardanuy C, Carratala J. Urinary antigen testing in community-acquired pneumonia in adults: an update. Expert Rev Anti Infect Ther. 2019;17(2):107–15.
Muyldermans A, Descheemaeker P, Boel A, et al. What is the risk of missing legionellosis relying on urinary antigen testing solely? A retrospective Belgian multicenter study. Eur J Clin Microbiol Infect Dis. 2020;39(4):729–34.
Vaccaro L, Izquierdo F, Magnet A, et al. First case of Legionnaires’ disease caused by Legionella anisa in Spain and the limitations on the diagnosis of Legionella non-pneumophila infections. PLoS ONE. 2016;11(7): e0159726.
Okada C, Kura F, Wada A, Inagawa H, Lee GH, Matsushita H. Cross-reactivity and sensitivity of two Legionella urinary antigen kits, Biotest EIA and Binax NOW, to extracted antigens from various serogroups of L. pneumophila and other Legionella species. Microbiol Immunol. 2002;46(1):51–4.
Ito A, Yamamoto Y, Ishii Y, Okazaki A, Ishiura Y, Kawagishi Y, et al. Evaluation of a novel urinary antigen test kit for diagnosing Legionella pneumonia. Int J Infect Dis. 2020;103:42–7.
Nakamura A, Fukuda S, Kusuki M, Watari H, Shimura S, Kimura K, et al. Evaluation of five Legionella urinary antigen detection kits including new Ribotest Legionella for simultaneous detection of ribosomal protein L7/L12. J Infect Chemother. 2021;27(10):1533–5.
Robert S, Lhommet C, Brun CL, et al. Diagnostic performance of multiplex PCR on pulmonary samples versus nasopharyngeal aspirates in community-acquired severe lower respiratory tract infections. J Clin Virol. 2018;108:1–5.
Diederen BM, de Jong CM, Kluytmans JA, van der Zee A, Peeters MF. Detection and quantification of Legionella pneumophila DNA in serum: case reports and review of the literature. J Med Microbiol. 2006;55(Pt 5):639–42.
Diederen BM, de Jong CM, Marmouk F, Kluytmans JA, Peeters MF, Van der Zee A. Evaluation of real-time PCR for the early detection of Legionella pneumophila DNA in serum samples. J Med Microbiol. 2007;56(Pt 1):94–101.
Matsiota-Bernard P, Waser S, Vrioni G. Detection of Legionella pneumophila DNA in urine and serum samples from patients with pneumonia. Clin Microbiol Infect. 2000;6(4):223–5.
Murdoch DR, Walford EJ, Jennings LC, et al. Use of the polymerase chain reaction to detect Legionella DNA in urine and serum samples from patients with pneumonia. Clin Infect Dis. 1996;23(3):475–80.
Mentasti M, Kese D, Echahidi F, et al. Design and validation of a qPCR assay for accurate detection and initial serogrouping of Legionella pneumophila in clinical specimens by the ESCMID Study Group for Legionella Infections (ESGLI). Eur J Clin Microbiol Infect Dis. 2015;34(7):1387–93.
Benitez AJ, Winchell JM. Clinical application of a multiplex real-time PCR assay for simultaneous detection of Legionella species, Legionella pneumophila, and Legionella pneumophila serogroup 1. J Clin Microbiol. 2013;51(1):348–51.
Merault N, Rusniok C, Jarraud S, et al. Specific real-time PCR for simultaneous detection and identification of Legionella pneumophila serogroup 1 in water and clinical samples. Appl Environ Microbiol. 2011;77(5):1708–17.
Ginevra C, Chastang J, David S, et al. A real-time PCR for specific detection of the Legionella pneumophila serogroup 1 ST1 complex. Clin Microbiol Infect. 2020;26(4):514 e1-e6.
Mentasti M, Cassier P, David S, et al. Rapid detection and evolutionary analysis of Legionella pneumophila serogroup 1 sequence type 47. Clin Microbiol Infect. 2017;23(4):264 e1-e9.
Avni T, Bieber A, Green H, Steinmetz T, Leibovici L, Paul M. Diagnostic accuracy of PCR alone and compared to urinary antigen testing for detection of Legionella spp.: a systematic review. J Clin Microbiol. 2016;54(2):401–11.
Ricci ML, Grottola A, Fregni Serpini G, et al. Improvement of Legionnaires' disease diagnosis using real-time PCR assay: a retrospective analysis, Italy, 2010 to 2015. Euro Surveill. 2018;23(50):1800032.
Rothe K, Spinner CD, Panning M, et al. Evaluation of a multiplex PCR screening approach to identify community-acquired bacterial co-infections in COVID-19: a multicenter prospective cohort study of the German competence network of community-acquired pneumonia (CAPNETZ). Infection. 2021;49(6):1299–306.
Huang Y, Ma Y, Miao Q, et al. Arthritis caused by Legionella micdadei and Staphylococcus aureus: metagenomic next-generation sequencing provides a rapid and accurate access to diagnosis and surveillance. Ann Transl Med. 2019;7(20):589.
Wang Y, Dai Y, et al. Case report: metagenomic next-generation sequencing in diagnosis of Legionella pneumophila pneumonia in a patient after umbilical cord blood stem cell transplantation. Front Med (Lausanne). 2021;8: 643473.
Yue R, Wu X, Li T, Chang L, Huang X, Pan L. Early detection of Legionella pneumophila and Aspergillus by mNGS in a critically ill patient with Legionella Pneumonia after extracorporeal membrane oxygenation treatment: case report and literature review. Front Med (Lausanne). 2021;8: 686512.
Heath CH, Grove DI, Looke DF. Delay in appropriate therapy of Legionella pneumonia associated with increased mortality. Eur J Clin Microbiol Infect Dis. 1996;15:286–90.
Gacouin A, Le Tulzo Y, Lavoue S, et al. Severe pneumonia due to Legionella pneumophila: prognostic factors, impact of delayed appropriate antimicrobial therapy. Intensive Care Med. 2002;28:686–91.
Falcone M, Russo A, Tiseo G, Cesaretti M, Guarracino F, Menichetti F. Predictors of intensive care unit admission in patients with Legionella pneumonia: role of the time to appropriate antibiotic therapy. Infection. 2021;49:321–5.
Chidiac C, Che D, Pires-Cronenberger S, French Legionnaires’ Disease Study Group, et al. Factors associated with hospital mortality in community-acquired legionellosis in France. Eur Respir J. 2012;39:963–70.
Woodhead M, Blasi F, Ewig S, Joint Taskforce of the European Respiratory Society and European Society for Clinical Microbiology and Infectious Diseases, et al. Guidelines for the management of adult lower respiratory tract infections—full version. Clin Microbiol Infect. 2011;17(Suppl 6):E1-59.
Metlay JP, Waterer GW, Long AC, et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019;200:e45–67.
Jasper AS, Musuuza JS, Tischendorf JS, et al. Are fluoroquinolones or macrolides better for treating Legionella Pneumonia? A systematic review and meta-analysis. Clin Infect Dis. 2021;72:1979–89.
Kato H, Hagihara M, Asai N, et al. Meta-analysis of fluoroquinolones versus macrolides for treatment of Legionella pneumonia. J Infect Chemother. 2021;27:424–33.
Torres A, Cillóniz C. Are macrolides as effective as fluoroquinolones in Legionella Pneumonia? Yes, but. Clin Infect Dis. 2021;72:1990–1.
Cocuzza CE, Martinelli M, Perdoni F, Giubbi C, Vinetti MEA, Calaresu E, Frugoni S, Scaturro M, Ricci ML, Musumeci R. Antibiotic susceptibility of environmental Legionella pneumophila strains isolated in Northern Italy. Int J Environ Res Public Health. 2021;18(17):9352.
Edelstein PH. Azithromycin phenotypic versus clinical resistance. Antimicrob Agents Chemother. 2019;64(1):e01986-e2019.
Natås OB, Brekken AL, Bernhoff E, Hetland MAK, Löhr IH, Lindemann PC. Susceptibility of Legionella pneumophila to antimicrobial agents and the presence of the efflux pump LpeAB. J Antimicrob Chemother. 2019;74(6):1545–50.
Martin SJ, Pendland SL, Chen C, Schreckenberger P, Danziger LH. In vitro synergy testing of macrolide-quinolone combinations against 41 clinical isolates of Legionella. Antimicrob Agents Chemother. 1996;40:1419–21.
Baltch AL, Smith RP, Ritz W. Inhibitory and bactericidal activities of levofloxacin, ofloxacin, erythromycin, and rifampin used singly and in combination against Legionella pneumophila. Antimicrob Agents Chemother. 1995;39:1661–6.
Descours G, Ginevra C, Ader F, et al. Rifampicin-macrolide synergy against Legionella pneumophila serogroup 1 in human macrophages using a quantitative real-time PCR assay. Int J Antimicrob Agents. 2011;38:188–9.
Martin SJ, Pendland SL, Chen C, Schreckenberger PC, Danziger LH. In vitro activity of clarithromycin alone and in combination with ciprofloxacin or levofloxacin against Legionella spp.: enhanced effect by the addition of the metabolite 14-hydroxy clarithromycin. Diagn Microbiol Infect Dis. 1997;29:167–71.
Varner TR, Bookstaver PB, Rudisill CN, Albrecht H. Role of rifampin-based combination therapy for severe community-acquired Legionella pneumophila pneumonia. Ann Pharmacother. 2011;45:967–76.
Grau S, Antonio JM, Ribes E, Salvadó M, Garcés JM, Garau J. Impact of rifampicin addition to clarithromycin in Legionella pneumophila pneumonia. Int J Antimicrob Agents. 2006;28:249–52.
Blázquez-Garrido RM, Espinosa-Parra FJ, Alemany-Francés L, et al. Antimicrobial chemotherapy for Legionnaires disease: levofloxacin versus macrolides. Clin Infect Dis. 2005;40:800–6.
Pedro-Botet ML, García-Cruz A, Tural C, et al. Severe Legionnaires’ disease successfully treated with levofloxacin and azithromycin. J Chemother. 2006;18:559–61.
Trübel HK, Meyer HG, Jahn B, Knuf M, Kamin W, Huth RG. Complicated nosocomial pneumonia due to Legionella pneumophila in an immunocompromised child. Scand J Infect Dis. 2002;34:219–21.
Nakamura S, Yanagihara K, Izumikawa K, et al. The clinical efficacy of fluoroquinolone and macrolide combination therapy compared with single-agent therapy against community-acquired pneumonia caused by Legionella pneumophila. J Infect. 2009;59:222–4.
Lan SH, Lai CC, Chang SP, Lu LC, Hung SH, Lin WT. Five-day antibiotic treatment for community-acquired bacterial pneumonia: a systematic review and meta-analysis of randomized controlled trials. J Global Antimicrob Resist. 2020;23:94–9.
Tansarli GS, Mylonakis E. Systematic review and meta-analysis of the efficacy of short-course antibiotic treatments for community-acquired pneumonia in adults. Antimicrob Agents Chemother. 2018;62:e00635-e718.
Dimopoulos G, Matthaiou DK, Karageorgopoulos DE, Grammatikos AP, Athanassa Z, Falagas ME. Short- versus long-course antibacterial therapy for community-acquired pneumonia: a meta-analysis. Drugs. 2008;68:1841–54.
el Moussaoui R, de Borgie CA, van den Broek P, et al. Effectiveness of discontinuing antibiotic treatment after three days versus eight days in mild to moderate-severe community acquired pneumonia: randomised, double blind study. BMJ. 2006;332:1355.
Siegel RE, Alicea M, Lee A, Blaiklock R. Comparison of 7 versus 10 days of antibiotic therapy for hospitalized patients with uncomplicated community-acquired pneumonia: a prospective, randomized, double-blind study. Am J Ther. 1999;6:217–22.
Uranga A, España PP, Bilbao A, et al. Duration of antibiotic treatment in community-acquired pneumonia: a multicenter randomized clinical trial. JAMA Intern Med. 2016;176:1257–65.
Kuzman I, Soldo I, Schönwald S, Culig J. Azithromycin for treatment of community acquired pneumonia caused by Legionella pneumophila: a retrospective study. Scand J Infect Dis. 1995;27:503–5.
Amsden GW. Treatment of Legionnaires’ disease. Drugs. 2005;65:605–14.
Chahin A, Opal SM. Severe pneumonia caused by Legionella pneumophila: differential diagnosis and therapeutic considerations. Infect Dis Clin N Am. 2017;31:111–21.
Lanternier F, Ader F, Pilmis B, Catherinot E, Jarraud S, Lortholary O. Legionnaires’ disease in compromised hosts. Infect Dis Clin N Am. 2017;31:123–35.
Agence française de sécurité sanitaire des produits de santé. Traitement antibiotique de la légionellose chez l’adulte. https://www.infectiologie.com/UserFiles/File/medias/_documents/consensus/2011-afssaps-MAP-legionellose.pdf. Accessed 1 Feb 2022.
Acknowledgements
Funding
Centro de Investigación Biomédica en Red de Enfermedades Infecciosas (CIBERINFEC; CB21/13/00009), Instituto de Salud Carlos III, Madrid, Spain funded this study. No funding or sponsorship was received for the publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work, and have given their approval for this version to be published.
Author Contributions
Diego Viasus: Conceptualization, Investigation, Writing—Original Draft. Valeria Gaia: Investigation, Writing—Original Draft. Carolina Manzur-Barbur: Investigation, Writing—Original Draft. Jordi Carratalà: Conceptualization, Writing—Review and Editing, Supervision.
Disclosures
Diego Viasus, Valeria Gaia, Carolina Manzur-Barbur and Jordi Carratalà confirm that they do not have any relevant financial relationships or conflicts of interest to report.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data Availability
No datasets were generated or analyzed during the current study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visithttp://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Viasus, D., Gaia, V., Manzur-Barbur, C. et al. Legionnaires’ Disease: Update on Diagnosis and Treatment. Infect Dis Ther 11, 973–986 (2022). https://doi.org/10.1007/s40121-022-00635-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-022-00635-7