Abstract
Introduction
We aimed to elucidate the impact of metabolic syndrome (MS) and nonalcoholic fatty liver disease (NAFLD) on treatment-naïve patients with chronic hepatitis B (CHB) and normal alanine aminotransferase (ALT).
Methods
We analyzed the clinical characteristics of a cross-sectional cohort of treatment-naïve patients with CHB and ALT in the upper limit of normal (ULN) from October 2018 to July 2021. ALT ≤ 0.5 ULN was stratified as low-normal ALT (LNALT) and 0.5 ULN < ALT ≤ ULN as high-normal ALT (HNALT). Transient elastography (TE) was used to evaluate liver steatosis and fibrosis.
Results
Among 733 patients with CHB enrolled, 23.1% of them had MS, 37.2% of them had NAFLD, and 5.9% of them had significant fibrosis. The proportions of patients with MS, steatosis, and significant fibrosis in the HNALT group were higher than those in the LNALT group (31.4% vs. 14.1%, p < 0.001; 48.7% vs. 25.2%, p < 0.001; and 8.0% vs. 3.6%, p = 0.013, respectively). Multiple linear regression showed that steatosis (beta = 0.098, p = 0.001) and MS (beta = 0.092, p = 0.002) were independently related to ALT levels in the normal range. Multivariate logistic regression showed that age (OR 1.049, 95% CI 1.012–1.087, p = 0.010), aspartate aminotransferase (AST) (OR 1.059, 95% CI 1.005–1.115, p = 0.030), and severe steatosis (OR 2.559, 95% CI 1.212–5.403, p = 0.014) were independently associated with significant fibrosis. When analyzed in the subgroup of CHB with NAFLD, age (OR 1.060, 95% CI 1.006–1.117, p = 0.029) and severe steatosis (OR 2.962, 95% CI 1.126–7.792, p = 0.028) were still statistically significant.
Conclusion
The accumulation of MS components exacerbated hepatic steatosis. Severe NAFLD was independently associated with significant fibrosis. This emphasizes the importance of screening for MS and NAFLD in patients with CHB and normal ALT, where a more active intervention may apply.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Chronic hepatitis B virus (CHB) infection with normal alanine aminotransferase (ALT) levels progress insidiously, and some of the affected patients develop adverse outcomes such as liver fibrosis. |
We aimed to compare the clinical characteristics by ALT levels and explore the roles of metabolic syndrome (MS) and controlled attenuation parameter (CAP)-identified steatosis in a treatment-naïve ALT-normal CHB population. |
What was learned from the study? |
Treatment-naïve patients with CHB and normal ALT levels were not completely disease-free and deserved close clinical attention. |
Patients with CHB and high normal ALT need aggressive control of MS or fatty liver to reduce the risk of liver fibrosis. |
Introduction
Approximately 686,000 patients die from hepatitis B virus (HBV)-related diseases worldwide every year, of which 46.0% and 44.0% die from cirrhosis and hepatocellular carcinoma (HCC), respectively [1]. Currently, most of the authoritative guidelines regard an abnormal alanine aminotransferase (ALT) level as a major marker of chronic hepatitis B (CHB) disease activity and one of the key references for recommending antiviral treatment [2,3,4]. However, studies have shown that 40–70% of patients with chronic HBV infection have persistently normal ALT levels [5, 6]. They may still have hepatic inflammation and fibrosis, which can further progress insidiously to cirrhosis and HCC, while prompt treatment can delay disease progression and improve outcomes [7,8,9]. A study from China retrospectively included hepatitis B envelope antigen (HBeAg)-negative ALT-normal patients with CHB who underwent liver biopsy, showing that 37.3% of the study patients had liver necroinflammation and 53.2% had liver fibrosis [7].
Nonalcoholic fatty liver disease (NAFLD) is becoming the most commonly seen chronic liver disease globally, mainly as a result of lifestyle and diet [10]. Because of the sedentary lifestyle and general overnutrition of the public, metabolic syndrome (MS) is becoming a modern health epidemic. Approximately one-fourth of world's adult population have MS [11]. MS is a pathological state manifested as obesity, insulin resistance, dyslipidemia, and hypertension. As all components of MS correlate with liver fat content, NAFLD is considered as the liver manifestation of MS [12]. Although a few types of NAFLD associated with certain genetic factors including the I148M PNPLA3 variant are not accompanied by MS and insulin resistance, occurrence and worsening of MS and its components not only increase the risk of NAFLD but also are independent predictors of overall and liver-related mortality in patients with NAFLD [13].
There are also a considerable proportion of patients with MS and NAFLD in the CHB population with normal ALT. The overall prevalence of NAFLD has reached approximately 30%, even in Asian populations, and has grown steadily in recent decades [14, 15]. Furthermore, the overlapping occurrences of CHB and NAFLD are frequently seen in clinical practice. According to recent literature, the incidence of hepatic steatosis in patients with CHB ranges from 14% to 60% [16,17,18]. Coexisting steatosis could promote the initiation and progression of fibrosis and HCC in patients with CHB [16, 19]. However, most of these patients had ALT levels fluctuating within the normal range, so the previously defined upper limit of normal (ULN) cannot completely identify these patients [20].
Experts from several countries and regions believe that the current ULN of ALT may not facilitate early diagnosis and treatment [2, 21]. In most clinical studies in patients with CHB and normal ALT, subjects with steatosis are excluded [6, 7]. Whereas, the significant proportion of steatosis in the CHB population emphasizes that this population cannot be ignored. Moreover, the roles of MS and its components in patients with CHB require further clarification. In the present study, we established a cross-sectional cohort to characterize the clinical features of treatment-naïve ALT-normal patients with CHB, especially focusing on the impact of concomitant metabolic characteristics and NAFLD.
Methods
Patients
The study included outpatients who underwent transient elastography (TE) at the Department of Infectious Disease, Tongji Hospital, Wuhan, China from October 2018 to July 2021. All patients were over 18 years of age. We excluded patients who were not positive for the hepatitis B surface antigen (HBsAg) for at least 6 months, had excessive alcohol consumption (≥ 30 g/day for men, ≥ 20 g/day for women), had CHB but had already received any antiviral treatment or had an ALT exceeding the ULN (40 U/L). Patients who had been coinfected with hepatitis C virus (HCV) or schistosoma or reported HCC history were also excluded from the study cohort.
Of the 2136 patients who underwent TE from October 2018 to July 2021, 1403 of them were excluded from the final study cohort. Forty-nine participants were excluded for excessive alcohol consumption, 94 for not having a chronic infection with HBV, 1 for HCV coinfection, 14 for schistosoma coinfection, 8 for HCC history, 1061 due to having received antiviral treatment, 173 with ALT > ULN, and 3 with ALT absence (Fig. 1). Finally, 733 treatment-naïve patients with CHB and normal ALT were included and stratified into a low-normal ALT (LNALT, ALT ≤ 20 U/L) group and a high-normal ALT (HNALT, 20 U/L < ALT ≤ 40 U/L) group.
All procedures performed in this study involving human participants were approved by the local ethical review board (the Human Ethics Committee of Tongji Medical College, Huazhong University of Science and Technology, China) and complied with the 1964 Declaration of Helsinki and its later amendments. Written informed consent was obtained from all study participants.
Clinical Data
Researchers collected comprehensive clinical data including demographic characteristics, laboratory tests, and transient elastography results of all the study participants at the time of transient elastography. The demographic characteristics included age, sex, body height, body weight, body mass index (BMI), waist circumference, hip circumference, waist-to-hip ratio, systolic blood pressure, diastolic blood pressure, and medical history.
Diabetes mellitus and hypertension were defined according to reported medical history or specific treatment. MS was defined as the presence of any three of five conditions (elevated waist circumference, elevated serum triglyceride, reduced high-density lipoprotein [HDL], elevated blood pressure, and elevated fasting glucose) using the International Diabetes Federation (IDF) and the American Heart Association/National Heart, Lung, and Blood Institute (AHA/NHLBI) criteria [22]. Metabolic disorder (MD) was defined as the presence of any one of the five aforementioned components.
Laboratory Tests
Laboratory tests involved liver and renal function tests, blood lipids, fasting blood glucose, and virological factors. Liver and renal function tests (ALT, aspartate aminotransferase [AST], alkaline phosphatase [ALP], γ-glutamyl transferase [GGT], albumin, total bilirubin, urea, creatinine, uric acid, and estimated glomerular filtration rate [eGFR]), blood lipids (total cholesterol, triglyceride, HDL-cholesterol, and low-density lipoprotein [LDL]-cholesterol) and fasting blood glucose were tested with an automated clinical chemistry analyzer (Roche Cobas 8000; Basel, Switzerland). The ULN of ALT was defined as 40 U/L according to the APASL guidelines [4]. HBsAg and HBeAg levels were determined by chemiluminescent assay (Kemei Biological Technology Co., Ltd., Beijing, China). The hepatitis B virus deoxyribonucleic acid (HBV DNA) level was measured by a real-time PCR kit with a lower detection limit of 20 IU/mL (Roche Diagnostics, Penzberg, Germany) or with a lower detection limit of 100 IU/mL (Tianlong Technology Co., Ltd., Xi’an, China).
Transient Elastography
Transient elastography (FibroScan, Echosens, Paris, France) was performed to assess liver stiffness measurement (LSM) and controlled attenuation parameters (CAP). An experienced technician obtained a final result fulfilling the following criteria: at least 10 valid shots, a success rate above 60%, and an interquartile range (IQR) less than 30% of the median (M) LSM value (IQR/M ≤ 0.30). An XL probe was used to evaluate patients with BMI above 30.0 kg/m2; otherwise, an M probe was used routinely [23]. All participants in this study underwent ultrasonography at the same time as transient elastography.
Significant fibrosis was defined as LSM > 9.0 kPa in patients with normal ALT according to the European Association for the Study of the Liver/Asociacion Latinoamericana para el Estudio del Higado guidelines [23]. Liver steatosis was defined as CAP ≥ 248 dB/m, in which 248 dB/m ≤ CAP < 268 dB/m was defined as mild, 268 dB/m ≤ CAP < 280 dB/m was defined as moderate , and CAP ≥ 280 dB/m was defined as severe [24].
Statistical Analysis
The results were shown as the median (lower quartile to upper quartile) (M [Q1–Q3]) for continuous variables or frequency (percentage) for categorical variables. Levels of HBV DNA and HBsAg were transferred to log10 IU/mL and log10 ng/mL, respectively. Student’s t test was used for the comparisons of normal continuous variables. The Mann–Whitney U test was the nonparametric test used for abnormal continuous data. The chi-square test was used for categorical variables. A univariate analysis was first performed to determine if any clinical variables were associated with outcome variables with the criteria of p < 0.10. Multivariate logistic regression or multiple linear regression was then used to determine whether those identified variables were independently associated with outcome variables. A two-tailed p value less than 0.05 was considered statistically significant. All data were analyzed using the SPSS statistical package (version 25.0; SPSS, Inc., Chicago, IL).
Results
Clinical Characteristics of all the Study Patients
Patient disposition of the present study is depicted in Fig. 1. A total of 733 participants were analyzed, as depicted in Table 1, among which 357 patients (48.7%) had low-normal ALT levels and 376 patients (51.3%) had high-normal ALT levels. The M (Q1–Q3) of age was 42 (34–49) years old. Moreover, 454 (61.9%) men and 279 (38.1%) women made up the whole study population. The majority of participants (662, 92.2%) had a negative HBeAg, with M (Q1–Q3) of HBsAg at 2.9 (1.6–3.6) log10 ng/mL. Only 195 (26.9%) recruited patients were HBV DNA-negative (HBV DNA < 20–100 IU/mL), with the M (Q1–Q3) of quantitative DNA at 2.9 (2.0–4.0) log10 IU/mL.
Regarding metabolic characteristics and steatosis, 273 (37.2%) patients with CHB had coexisting NAFLD, of whom 106 (14.5%) were defined as mild, 51 (7.0%) moderate, and 116 (15.8%) severe on the basis of CAP. There were also 187 (25.5%), 38 (5.2%), and 163 (23.1%) patients who suffered from hypertension, diabetes, and MS, respectively. By assessing LSM, there were 43 significant fibrosis participants, which accounted for 5.9% of the whole (Table 1).
Comparisons of Clinical Characteristics Between the LNALT Group and HNALT Group
Comparisons of clinical characteristics between the LNALT group and HNALT group are depicted in Table 1. No significant differences were seen in age between the two groups. The proportion of male patients was significantly higher in the HNALT group than in the LNALT group (80.3% vs 42.6%, p < 0.001). Anthropometric characteristics, including BMI, waist circumference, hip circumference, waist-to-hip ratio, systolic blood pressure, and diastolic blood pressure, were obviously higher in the HNALT group when compared to those in the LNALT group (p < 0.001 for each comparison). In addition, the HNALT group had significantly higher ALT, AST, ALP, GGT, albumin, total bilirubin, triglyceride, and fasting glucose levels than the LNALT group (p < 0.05 for each comparison). The HNALT group had significantly lower HDL-cholesterol (p < 0.001). Additionally, creatinine and uric acid were also higher in the HNALT group (p < 0.001 for each comparison). However, there were no significant differences in total cholesterol, LDL-cholesterol, urea, or eGFR.
The HNALT group had higher HBV DNA levels and a lower proportion of negative HBV DNA (3.0 vs. 2.8 log10 IU/mL, p = 0.003; 22.4% vs. 31.5%, p = 0.005), while HBsAg levels and HBeAg negative rates were statistically comparable. The HNALT group had more hypertension, MS, and steatosis (31.4% vs. 19.3%, p < 0.001; 31.4% vs. 14.1%, p < 0.001; 48.7% vs. 25.2%, p < 0.001), and the same was true after adjusting for age and sex (Table S1). When analyzing subgroups by the degree of steatosis, the difference in hepatosteatosis between the two groups was reflected in the severe steatosis subgroup (Fig. 2). Significant fibrosis was also significantly different (8.0% vs. 3.6%, p = 0.013), and the same was true after adjusting for age and sex (Table S1), which occurred mainly in the CHB with NAFLD subgroup but not in the CHB without NAFLD subgroup (Fig. 3). Furthermore, the CAP and LSM of the patients with HNALT were higher (246 vs. 215 dB/m, p < 0.001; 5.1 vs. 4.8 kPa, p < 0.001) (Table 1).
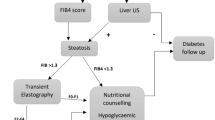
Relationship Among Metabolic Syndrome, Steatosis, and Significant Fibrosis
In the study population, CAP values (p < 0.001) increased with the accumulation of MS components, and LSM values (p < 0.001) increased with the increasing steatosis grading. When they were divided into a “None" group (patients with neither MD nor NAFLD), MD group (patients with MD but no NAFLD), and MD + NAFLD group (patients with both MD and NAFLD), the LSM values of the three groups increased successively (p < 0.001) and the prevalence of significant fibrosis also increased (p < 0.05) (Fig. 4).
Relationship among metabolic syndrome, steatosis, and significant fibrosis. The relationship between metabolic syndrome components and CAP (a); the relationship between steatosis grading and LSM (b); the changes in LSM (c); and the incidence of significant fibrosis (d) in None group, MD group, and MD + NAFLD group. The CAP values and LSM values were depicted as mean ± standard deviation in the graph. Metabolic syndrome components including elevated waist circumference, elevated serum triglyceride, reduced high-density lipoprotein, elevated blood pressure, and elevated fasting glucose. Metabolic disorder (MD) was defined as the presence of any 1 of 5 of the aforementioned conditions. The dotted lines in a indicated steatosis (CAP ≥ 248 dB/m) and severe steatosis (CAP ≥ 280 dB/m). The dotted lines in b and c indicate abnormal LSM (LSM > 6 kPa) and significant fibrosis (LSM > 9 kPa). None group: patients with neither MD nor NAFLD; MD group: patients with MD but no NAFLD; MD + NAFLD group: patients with both MD and NAFLD. CAP controlled attenuation parameter, LSM liver stiffness measurement, MD metabolic disorder, NAFLD nonalcoholic fatty liver disease
Factors Associated with ALT Elevation in the Normal Range
By univariate analysis, significant fibrosis, steatosis, and MS were positively correlated with ALT elevation in the normal range, as well as age, male sex, AST, ALP, GGT, albumin, total bilirubin, and HBV DNA load (Table 2). Multivariate linear regression showed that age (beta = − 0.152, p < 0.001), male sex (beta = 0.303, p < 0.001), AST (beta = 0.444, p < 0.001), GGT (beta = 0.198, p < 0.001), HBV DNA load (beta = 0.127, p < 0.001), steatosis (beta = 0.098, p = 0.001), and MS (beta = 0.092, p = 0.002) were independent variables positively correlated with ALT levels (Table 2). When independent variables were analyzed separately whether or not combined with NAFLD, age, sex, AST, GGT, and MS were significant in both groups, whereas the HBV DNA load was significant only in the CHB without NAFLD group (Tables S2 and S3).
Factors Associated with Significant Fibrosis with Normal ALT
Univariate analysis showed that significant fibrosis with normal ALT correlated with age, ALT, AST, ALP, GGT, albumin, and severe steatosis (p < 0.05 for each comparison). Multivariate logistic analysis showed that age (OR 1.049, 95% CI 1.012–1.087, p = 0.010), AST (OR 1.059, 95% CI 1.005–1.115, p = 0.030), and severe steatosis (OR 2.559, 95% CI 1.212–5.403, p = 0.014) were significantly and independently associated with significant fibrosis (Table 3). NAFLD-specific multivariate analysis showed that age (OR 1.060, 95% CI 1.006–1.117, p = 0.029) and severe steatosis (OR 2.962, 95% CI 1.126–7.792, p = 0.028) were still significantly associated with significant fibrosis in the CHB with NAFLD group, whereas AST (OR 1.256, 95% CI 1.097–1.437, p = 0.001) and GGT (OR 1.044, 95% CI 1.011–1.078, p = 0.008) were significantly associated with significant fibrosis in the CHB without NAFLD group (Tables S4 and S5).
Discussion
Patients with CHB combined with MS or NAFLD, whose population is large, often have insidious disease progression and are not easily detected in the presence of normal ALT. Our study showed that 23.1% of patients with CHB and normal ALT had MS. This observed prevalence is consistent with those in reports of other Asian populations, in which MS incidence ranged from 18.6% to 23.4% [25, 26]. The HNALT group had a significantly worse metabolic condition compared to that in the LNALT group. In our ALT-normal CHB cohort, severe liver steatosis determined by CAP was found to be an independent risk factor for significant fibrosis. With the increase of MS components, steatosis tended to be worse. We also found that with the increase of steatosis severity, the stiffness of the liver rose accordingly and severe steatosis was positively correlated with significant fibrosis. It highlights the importance of MS and NAFLD intervention in reducing the risk of liver fibrosis in ALT-normal patients with CHB.
Studies have shown that fatty liver alone is no longer considered a benign lesion of the liver and is strongly associated with adverse regressions such as liver fibrosis, cirrhosis, and HCC [27]. However, the relationship between steatosis and HBV-related disease remains controversial. In a recent study of 420 North American patients with chronic HBV infection who underwent liver biopsy, one-third of them had coexisting steatosis, and it was shown that NAFLD increased the rate of incident fibrosis [28]. Yuen et al. repeatedly reported that TE-identified steatosis was positively associated with liver fibrosis, but increased the HBsAg seroclearance rate [16, 29, 30]. However, some studies have shown inconsistent findings. A study from Shandong, China, claimed that fatty liver was significantly associated with lower cirrhosis and HCC risk in patients with CHB [31]. Choi et al. reported that patients with CHB, high viral load, and no significant ALT elevation can benefit from antiviral treatment [32]. Therefore, we need follow up to clarify the role of antiviral therapy in ALT-normal patients with CHB, especially those combined with MS or NAFLD.
ALT within the normal range does not mean an individual is “disease-free”. Among these patients with CHB, more than 30% were proven to have abnormal liver histology, including significant necroinflammation and fibrosis. The proportion of patients with significant liver fibrosis ranged from 8.8% to 53.2% according to a series of studies [7, 33, 34]. In our study, 5.9% of patients with normal ALT had TE-identified significant fibrosis. The discrepancies in diagnostic standards, antiviral therapy, viral load, HBeAg status, and HBV genotype may partly explain why the results fluctuated. One study from Hong Kong showed 4.4% of patients had severe fibrosis and 2.0% with cirrhosis in a similar treatment-naïve population and the same diagnostic method as the present research [29]. We also found that the incidence of significant fibrosis was higher in the HNALT group when compared with that in the LNALT group. We also performed a gender-based subgroup analysis with a cutoff value of 30 IU/L for male patients or 19 IU/L for female patients. Interestingly, we found a higher viral load, a higher proportion of patients with MS, as well as higher CAP and LSM values in the HNALT group than the LNALT group, in both subgroups, which was consistent with the results from the whole study population. However, these differences did not reach to statistical significance (data not shown), most likely because of the limited sample size in subgroups. We suggest that hepatoprotective therapy, bringing ALT down to LNALT levels in ALT-normal patients with CHB combined with MS or NAFLD, could reduce the risk of liver fibrosis.
Currently, there is no agreement on whether HBV DNA levels are associated with the risk of liver fibrosis from studies on patients with CHB and normal ALT. Some studies have shown that elevated HBV DNA loads were independently associated with significant liver histopathology [7]. However, other researchers have suggested that liver histopathological changes of patients with CHB were associated with age, transaminases, platelet, and GGT, but not HBV DNA [35, 36]. We had similar findings that HBV DNA did not play a role in increasing the incidence of fibrosis. Studies have confirmed that excessive advanced glycation end products and free fatty acids, in the presence of MS and simple fatty liver, can activate hepatic stellate cells (HSC) [37]. Meanwhile, the function of hepatocytes, hepatic macrophages, and HSC was also affected by hepatic mitochondrial dysfunction, endoplasmic reticulum stress, oxidative stress, and inflammatory cytokine release, which in turn promote the liver fibrosis [38]. Therefore, we speculated that in ALT-normal patients with CHB, the inflammatory damage and the stimulation of HSC may come mainly from metabolic factors. In this regard, we need more in-depth studies to evaluate the role of MS and NAFLD control in ALT-normal patients with CHB.
In a recent study based on data surveyed from the employees of a German chemical company, male individuals, manual workers, overweight or obesity, alcohol drinking, diabetes, and seasons contributed to the elevation of ALT [39]. Lin et al., carrying out related research in a Chinese population, also showed that male sex, older age, and higher HBV DNA load were risk factors for HNALT [40]. MS was independently associated with higher ALT levels longitudinally in a largely Asian CHB cohort [26]. Obviously, in addition to demographic and virological factors, metabolic factors and steatosis have clinical implications for ALT elevation in chronic liver disease. As expected, in our study the ALT level was associated with risk factors, including younger age, male sex, AST, GGT, higher viral load, steatosis, and MS. This highlights the importance of comprehensive monitoring of the metabolic status in patients with CHB.
Interestingly, AST rather than ALT was an independent risk factor for fibrosis in the total study population and the subgroup of CHB without NAFLD. In line with our findings, a previous prospective cohort study showed that baseline and changes in AST levels were associated with the progression of fibrosis stage by two liver biopsies in patients with NAFLD [41]. Another study pointed out that AST could predict histologically significant abnormalities in HBeAg-positive patients with CHB and predict significant inflammation in HBeAg-negative patients [33]. AST mainly exists in the mitochondria of liver cells, while ALT exists in the cytoplasm. Advanced liver disease may cause mitochondrial damage leading to increased AST release, which is more marked than ALT [42]. In addition, fibrosis progression may result in significant retardation of the plasma clearance of AST [43]. Both mechanisms synergistically cause the elevation of AST levels. This suggests that AST may provide much more specific prediction performance for liver fibrosis than traditionally valued ALT does.
Liver biopsy is still the gold standard to define histological abnormalities by invasive examination. But in clinical practice, steatosis can be identified by imaging methods, because they are more widely available, economical, and safer than liver biopsy. Ultrasound was considered as the preferred first-line diagnostic procedure for imaging of NAFLD by the EASL–EASD–EASO Clinical Practice Guidelines. However, ultrasound does not reliably detect steatosis when lower than 20% and is imprecise in estimating the extent of steatosis [12]. These limitations could be complemented by CAP values, although there is still ongoing debating. One meta-analysis concluded that CAP should be cautiously considered as a noninvasive substitute for liver biopsy because of the effect of geographic regions, cutoffs, age, and BMI [44]. Whereas another meta-analysis confirmed that the correlation between CAP and histologically determined steatosis is very good, and established cutoffs on the basis of comprehensive data, which enabled the routine use of CAP. This study also proposed that sex and age played a much small role when interpreting CAP [24]. To sum up, CAP provides an estimate of the percentage of steatotic hepatocytes which is more accurate than ultrasound, whereas the liver biopsy provides histological evaluation on the pathological changes in liver parenchyma. Noninvasive CAP may be a good choice to screen for hepatic steatosis whenever an invasive procedure is not available or not feasible.
Our study had some limitations. First, the inherent cross-sectional nature impedes a firm causal conclusion. Second, liver biopsy was not available to assess fibrosis and steatosis. However in real-world practice, TE is becoming popular owing to its noninvasiveness, reliability, and repeatability [23]. Thirdly, we only included treatment-naïve patients, and most of them were HBeAg negative. Thus, when applied to on-treatment or HBeAg-positive patients, one should interpret the conclusions with caution. Despite these limitations, our data with a large population of 733 patients stands to provide solid information on the clinical features of treatment-naïve patients with CHB and normal ALT. To further validate the results, a prospective and multicenter study on a larger scale is needed.
Conclusions
ALT-normal treatment-naïve patients with CHB may have metabolic abnormalities, steatosis, and significant fibrosis. MS was independently associated with ALT elevation and led to increasing risk of NAFLD. The latter increased the risk of significant fibrosis in patients with CHB and normal ALT levels. Moreover, AST levels may be useful in predicting the risk of liver fibrosis in this population. Our study highlights the importance of MS and NAFLD screening and management in patients with CHB and normal ALT.
References
Mohsen N, Haidong W, Rafael L, et al. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385:117–71.
Terrault NA, Lok ASF, McMahon BJ, et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance. Hepatology. 2018;67:1560–99.
Lampertico P, Agarwal K, Berg T, et al. EASL 2017 Clinical Practice Guidelines on the management of hepatitis B virus infection. J Hepatol. 2017;67:370–98.
Sarin SK, Kumar M, Lau GK, et al. Asian-Pacific clinical practice guidelines on the management of hepatitis B: a 2015 update. Hepatol Int. 2016;10:1–98.
Tseng TC, Liu CJ, Hsu CY, et al. High level of hepatitis B core-related antigen associated with increased risk of hepatocellular carcinoma in patients with chronic HBV infection of intermediate viral load. Gastroenterology. 2019;157:1518–29 (e1513).
Tan YW, Zhou XB, Ye Y, He C, Ge GH. Diagnostic value of FIB-4, aspartate aminotransferase-to-platelet ratio index and liver stiffness measurement in hepatitis B virus-infected patients with persistently normal alanine aminotransferase. World J Gastroenterol. 2017;23:5746–54.
Duan M, Chi X, Xiao H, Liu X, Zhuang H. High-normal alanine aminotransferase is an indicator for liver histopathology in HBeAg-negative chronic hepatitis B. Hepatol Int. 2021;15:318–27.
Li Q, Lu C, Li W, Huang Y, Chen L. The independent predictors of significant liver histological changes in chronic hepatitis B virus infection patients with persistently high-normal or low-normal alanine transaminase levels. Discov Med. 2017;23:19–25.
Chan AW, Wong GL, Chan HY, et al. Concurrent fatty liver increases risk of hepatocellular carcinoma among patients with chronic hepatitis B. J Gastroenterol Hepatol. 2017;32:667–76.
Wang FS, Fan JG, Zhang Z, Gao B, Wang HY. The global burden of liver disease: the major impact of China. Hepatology. 2014;60:2099–108.
O’Neill S, O’Driscoll L. Metabolic syndrome: a closer look at the growing epidemic and its associated pathologies. Obes Rev. 2015;16:1–12.
European Association for the Study of the Liver (EASL), European Association for the Study of Diabetes (EASD), European Association for the Study of Obesity (EASO). EASL-EASD-EASO clinical practice guidelines for the management of non-alcoholic fatty liver disease. Diabetologia. 2016;59:1121–40.
Stepanova M, Rafiq N, Younossi ZM. Components of metabolic syndrome are independent predictors of mortality in patients with chronic liver disease: a population-based study. Gut. 2010;59:1410–5.
Li J, Zou B, Yeo YH, et al. Prevalence, incidence, and outcome of non-alcoholic fatty liver disease in Asia, 1999–2019: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2019;4:389–98.
Zhou F, Zhou J, Wang W, et al. Unexpected rapid increase in the burden of NAFLD in China from 2008 to 2018: a systematic review and meta-analysis. Hepatology. 2019;70:1119–33.
Mak LY, Hui RW, Fung J, et al. Diverse effects of hepatic steatosis on fibrosis progression and functional cure in virologically quiescent chronic hepatitis B. J Hepatol. 2020;73:800–6.
Wong VW, Wong GL, Chu WC, et al. Hepatitis B virus infection and fatty liver in the general population. J Hepatol. 2012;56:533–40.
Tsochatzis E, Papatheodoridis GV, Manesis EK, Chrysanthos N, Kafiri G, Archimandritis AJ. Hepatic steatosis in chronic hepatitis B develops due to host metabolic factors: a comparative approach with genotype 1 chronic hepatitis C. Dig Liver Dis. 2007;39:936–42.
Choi HSJ, Brouwer WP, Zanjir WMR, et al. Nonalcoholic steatohepatitis is associated with liver-related outcomes and all-cause mortality in chronic hepatitis B. Hepatology. 2020;71:539–48.
Chang Y, Ryu S, Sung E, Jang Y. Higher concentrations of alanine aminotransferase within the reference interval predict nonalcoholic fatty liver disease. Clin Chem. 2007;53:686–92.
Tanaka K, Hyogo H, Ono M, et al. Upper limit of normal serum alanine aminotransferase levels in Japanese subjects. Hepatol Res. 2014;44:1196–207.
Alberti KG, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–5.
Laurent C, Henry LYC, Marco A, et al. EASL-ALEH clinical practice guidelines: non-invasive tests for evaluation of liver disease severity and prognosis. J Hepatol. 2015;63:237–64.
Karlas T, Petroff D, Sasso M, et al. Individual patient data meta-analysis of controlled attenuation parameter (CAP) technology for assessing steatosis. J Hepatol. 2017;66:1022–30.
Choi JS, Han KJ, Lee S, et al. Serum HBV surface antigen positivity is associated with low prevalence of metabolic syndrome in Korean adult men. J Epidemiol. 2015;25:74–9.
Khalili M, Shuhart MC, Lombardero M, et al. Relationship between metabolic syndrome, alanine aminotransferase levels, and liver disease severity in a multiethnic North American cohort with chronic hepatitis B. Diabetes Care. 2018;41:1251–9.
Wong VW, Wong GL, Choi PC, et al. Disease progression of non-alcoholic fatty liver disease: a prospective study with paired liver biopsies at 3 years. Gut. 2010;59:969–74.
Khalili M, Kleiner DE, King WC, et al. Hepatic steatosis and steatohepatitis in a large North American cohort of adults with chronic hepatitis B. Am J Gastroenterol. 2021;116:1686–97.
Seto WK, Hui RWH, Mak LY, et al. Association between hepatic steatosis, measured by controlled attenuation parameter, and fibrosis burden in chronic hepatitis B. Clin Gastroenterol Hepatol. 2018;16:575-583.e572.
Mak LY, Seto WK, Hui RW, et al. Fibrosis evolution in chronic hepatitis B e antigen-negative patients across a 10-year interval. J Viral Hepat. 2019;26:818–27.
Li J, Yang HI, Yeh ML, et al. Association between fatty liver and cirrhosis, hepatocellular carcinoma, and hepatitis B surface antigen seroclearance in chronic hepatitis B. J Infect Dis. 2021;224:294–302.
Choi GH, Kim GA, Choi J, Han S, Lim YS. High risk of clinical events in untreated HBeAg-negative chronic hepatitis B patients with high viral load and no significant ALT elevation. Aliment Pharmacol Ther. 2019;50:215–26.
Liao B, Wang Z, Lin S, et al. Significant fibrosis is not rare in Chinese chronic hepatitis B patients with persistent normal ALT. PLoS ONE. 2013;8: e78672.
Tan Y, Ye Y, Zhou X, Chen L, Wen D. Age as a predictor of significant fibrosis features in HBeAg-negative chronic hepatitis B virus infection with persistently normal alanine aminotransferase. PLoS ONE. 2015;10: e0123452.
Wang H, Ru GQ, Yan R, Zhou Y, Wang MS, Cheng MJ. Histologic disease in Chinese chronic hepatitis B patients with low viral loads and persistently normal alanine aminotransferase levels. J Clin Gastroenterol. 2016;50:790–6.
Cheng JL, Wang XL, Yang SG, Zhao H, Wu JJ, Li LJ. Non-ALT biomarkers for markedly abnormal liver histology among Chinese persistently normal alanine aminotransferase-chronic hepatitis B patients. World J Gastroenterol. 2017;23:2802–10.
Lanthier N, Horsmans Y, Leclercq IA. The metabolic syndrome: how it may influence hepatic stellate cell activation and hepatic fibrosis. Curr Opin Clin Nutr Metab Care. 2009;12:404–11.
Luangmonkong T, Suriguga S, Mutsaers HAM, Groothuis GMM, Olinga P, Boersema M. Targeting oxidative stress for the treatment of liver fibrosis. Rev Physiol Biochem Pharmacol. 2018;175:71–102.
Claus M, Antoni C, Hofmann B. Factors associated with elevated alanine aminotransferase in employees of a German chemical company: results of a large cross-sectional study. BMC Gastroenterol. 2021;21:25.
Lin CL, Liao LY, Liu CJ, et al. Hepatitis B viral factors in HBeAg-negative carriers with persistently normal serum alanine aminotransferase levels. Hepatology. 2007;45:1193–8.
Kleiner DE, Brunt EM, Wilson LA, et al. Association of histologic disease activity with progression of nonalcoholic fatty liver disease. JAMA Netw Open. 2019;2: e1912565.
Nalpas B, Vassault A, Le Guillou A, et al. Serum activity of mitochondrial aspartate aminotransferase: a sensitive marker of alcoholism with or without alcoholic hepatitis. Hepatology. 1984;4:893–6.
Kamimoto Y, Horiuchi S, Tanase S, Morino Y. Plasma clearance of intravenously injected aspartate aminotransferase isozymes: evidence for preferential uptake by sinusoidal liver cells. Hepatology. 1985;5:367–75.
Pu K, Wang Y, Bai S, et al. Diagnostic accuracy of controlled attenuation parameter (CAP) as a non-invasive test for steatosis in suspected non-alcoholic fatty liver disease: a systematic review and meta-analysis. BMC Gastroenterol. 2019;19:51.
Acknowledgements
We thank the participants of the study.
Funding
This study was funded by the General Program of National Natural Science Foundation of China (NSFC82170596) and the National Key Research and Development Program of China (2021YFC2600200). Qin Ning funded the journal’s Rapid Service Fees.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All authors contributed to the study conception and design. Patient enrollment and clinical data collection were performed by Yuting Diao, Danqing Hu and Xue Hu. Data analysis and correction were performed by Yuting Diao and Peng Wang. The first draft of the manuscript was written by Yuting Diao. Xiaojing Wang, Xiaoping Luo, Hongwu Wang and Qin Ning made critical revisions of the manuscript. The study was supervised by Hongwu Wang and Qin Ning. All authors approved the final manuscript and agreed to be accountable for all aspects of the work.
Disclosures
The authors Yuting Diao, Danqing Hu, Xue Hu, Peng Wang, Xiaojing Wang, Xiaoping Luo, Hongwu Wang and Qin Ning declare that they have no conflicts of interest.
Compliance with Ethics Guidelines
All procedures performed in this study involving human participants were approved by the local ethical review board (the Human Ethics Committee of Tongji Medical College, Huazhong University of Science and Technology, China) and complied with the 1964 Declaration of Helsinki and its later amendments. Written informed consent was obtained from all study participants.
Data Availability
All data generated or analyzed during this study are included in this published article and supplementary information files.
Author information
Authors and Affiliations
Corresponding authors
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Diao, Y., Hu, D., Hu, X. et al. The Role of Metabolic Factors and Steatosis in Treatment-Naïve Patients with Chronic Hepatitis B and Normal Alanine Aminotransferase. Infect Dis Ther 11, 1133–1148 (2022). https://doi.org/10.1007/s40121-022-00629-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-022-00629-5