Abstract
Vaccination is a critical component for ensuring the health of those living with the human immunodeficiency virus (HIV) by protection against vaccine-preventable diseases. Since HIV-infected persons may have reduced immune responses and shorter durations of protection post-vaccination, HIV-specific guidelines have been published by global and national advisory organizations to address these potential concerns. This article provides a comprehensive review of the current guidelines and evidence-based data for vaccinating HIV-infected adults, including guidance on modified vaccine dosing and testing strategies, as well as safety considerations, to enhance protection among this vulnerable population. In the current article, part I of the two-part series, inactivated vaccines with broad indications as well as vaccines for specific risk and age groups will be discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Importance of Vaccinations
HIV-infected persons are at an increased risk for a wide variety of infections. For example, HIV-infected persons have a markedly higher risk and severity of pneumonia from pneumococcal disease and influenza [1]. Similarly, salmonellosis causing typhoid fever occurs at higher rates in exposed HIV-infected persons [2]. Acquisition of hepatitis B virus (HBV) and human papillomavirus (HPV) infections are common in this population given their shared routes of transmission, and HIV-infected persons are at risk for more rapid progression to significant liver disease (cirrhosis, hepatocellular carcinoma) and genital (cervical and anal cancers), respectively, compared with HIV-uninfected persons [3,4,5]. Strategies for reducing the risk of concurrent infectious diseases among HIV-infected persons include receipt of antiretroviral therapy to enhance immune protective responses; behavioral modifications (e.g., smoking cessation to reduce pneumococcal and influenza pneumonia, safe sex to reduce HBV and HPV, etc.); prophylactic antibiotics depending on the CD4 cell count and geographic location; and vaccination. As such, vaccination is a key component to ensure the health of all persons living with HIV by preventing infectious complications. Since HIV-infected patients who are born in other countries may have had incomplete or varying vaccinations, special attention should be given to ensure all vaccines (including those generally given in childhood) are up to date. This review, part I of a two-part series (doi:10.1007/s40121-017-0165-y), will highlight the importance of vaccination as a critical preventive strategy among HIV-infected adults and provide a summary of the current evidence-based recommendations.
Overview of Vaccine Recommendations
Vaccine recommendations for HIV-infected adults have been published by various advisory groups including the World Health Organization (WHO) [6, 7], British HIV Association (BHIVA) [8], and US-based groups such as the US Centers for Disease Control and Prevention (CDC) and the Advisory Committee on Immunization Practices (ACIP) [9,10,11]. Additionally, the European AIDS Clinical Society (EACS) [12] and The HIV Medicine Association of the Infectious Diseases Society of America (HIVMA) [13] contain specific recommendations for vaccinating HIV-infected persons. Specific countries (e.g., France) also have published guidance on vaccinating HIV-infected adults [14]. While the WHO had previously issued specific vaccination guidelines for HIV-infected adults [6], more recently guidance has been based on standard vaccinations recommended by the national immunization schedules with specific sections containing guidance for HIV-infected persons [7].
The BHIVA guidelines were published in 2015 [8], while the EACS guidelines were published in 2017 [12] and French guidelines in 2016 [14]. US guidelines specifically for HIV-infected persons were published in 2013 [10, 13], and national guidelines (which include guidance for HIV-infected persons) are published annually, including in 2017 [9]. Additionally, there are country-specific immunization guidelines that include recommendations for HIV-infected persons, and readers are encouraged to refer to national or local guidance in their geographic region regarding best vaccine practices.
While vaccine guidelines for HIV-infected adults are often similar to those for HIV-uninfected persons, there are important differences as HIV can affect both the efficacy and safety of vaccines. For example, the recommended dosage, number, and timing of specific vaccines may differ by HIV status, and some vaccines (e.g., live) are contraindicated among HIV-infected persons with specific clinical and laboratory characteristics (e.g., symptomatic disease, CD4 count <200 cells/mm3).
This overview will provide summary data regarding vaccinations for the HIV-infected adult from the major advisory groups (WHO, BHIVA, CDC/ACIP) [6,7,8,9,10] and include recommendations from other organizations [12, 14]. While the published guidelines are overall similar in many of their recommendations, there are notable differences. Some of these differences are related to the paucity of, or conflicting, efficacy data regarding specific vaccines among HIV-infected adults in various geographic areas. Additionally, there may be competing health priorities as well as differing local epidemiologic disease trends within specific countries and regions. This review provides overall vaccine recommendations by various advisory groups with differences in guidelines concisely summarized in Tables 1, 2, 3. Although this article includes current recommendations, changes are anticipated over time given the evolving epidemiology of the causative pathogens and surveillance data, emerging vaccine-related effectiveness data, and the development of newly approved vaccines.
Most vaccines can be administered at or shortly after HIV diagnosis especially among early diagnosed persons. However, in cases of late diagnoses with low CD4 counts, postponing vaccination may be advised until antiretroviral therapy (ART) is initiated and immune reconstitution is achieved; further details will be discussed for each vaccine below. The timing of vaccination should be contextualized for each individual HIV-positive person balancing the risks of potential exposures with improved vaccine responses post-ART initiation. There are no clear data for the upper limit on the number of vaccines that can be administered at one visit, however practical limitations should be considered including the number of desirable anatomic sites to administer vaccines and patient comfort considerations. Additionally, live vaccines should be administered on the same day or separated by at least 28 days.
Vaccines will be categorized into inactivated vaccines with broad indications [influenza, pneumococcal, HBV, and tetanus-diphtheria (Td)/tetanus-diphtheria-pertussis (Tdap)] followed by vaccines targeted among those with additional risk factors or specific age groups [hepatitis A virus (HAV), HPV, and meningococcal]. These vaccines will be reviewed in the current article, which is part I of the two-part series. Additional vaccines will be covered in part II of the series, including live vaccines [varicella, zoster, and measles-mumps-rubella (MMR)], as these may be considered among at-risk, non-pregnant, HIV-infected persons who are clinically stable with low level immunosuppression (CD4 count ≥200 cells/mm3). Travel-related vaccines [polio, typhoid, yellow fever, rabies, Japanese encephalitis virus (JEV), cholera, and tick-borne encephalitis (TBE)], vaccines to protect against specific occupational or exposure risks (anthrax, smallpox), and additional vaccines [Hemophilus influenzae serotype b (Hib) and Bacille Calmette-Guerin (BCG)] will also be reviewed in part II of the series.
For each vaccine, the importance of each infectious agent in the context of HIV infection will be briefly described followed by the current recommendations (WHO, BHIVA, EACS, French, and US guidelines, respectively). Data regarding post-vaccination immune responses and durability in the HIV-infected adult as well as safety data will be provided. This article represents a review article, is based on previously conducted studies, and does not involve any new studies of human or animal subjects performed by either of the authors.
Inactivated Vaccines with Overall Broad Indications
Influenza
HIV-infected adults have an elevated risk of severe infections and complications from influenza and hence are considered a key target population for vaccination [15,16,17,18,19,20,21]. Further, HIV-infected pregnant women are at particular risk for severe disease and represent an important group for targeted vaccination. Although ART is associated with a reduction in hospitalizations due to influenza, HIV-infected adults remain at higher risk than the general population; hence, vaccination is advocated to reduce influenza infections and related complications [17]. All major advisory groups recommend HIV-infected adults receive annual influenza vaccination regardless of CD4 count [8,9,10,11,12,13,14] (Table 1).
There are two overall types of influenza vaccines, a live attenuated influenza vaccine (LAIV) and an inactivated influenza vaccine (IIV). The LAIV is administered as a nasal spray, but is generally avoided among HIV-infected adults because of the theoretical risk of prolonged viral shedding and/or disease acquisition in the setting of underlying immunosuppression; however, this concern has not been clearly demonstrated [22,23,24]. Hence, guidelines recommend using the inactivated vaccine (IIV), which is typically administered by intramuscular injection. There are two main types of inactivated vaccines, which can be categorized into trivalent (containing two A viruses and one B virus) and quadrivalent (containing an additional B virus) forms.
The WHO recommends influenza vaccination to be determined by national capacity and resources, with pregnant women having the highest priority followed by additional risk groups including those with specific chronic medical conditions such as HIV [7].
The BHIVA recommends using IIV and suggests using the quadrivalent form if available to provide the maximal anti-influenza virus coverage [8]. The EACS simply recommends an annual influenza vaccine and cites the BHIVA for further guidance [12]. The French guidelines recommend IIV, but also note that LAIV may be considered if the CD4 count is >200 cells/mm3 [14].
In the US, the IIV is recommended for annual administration. LAIV is contraindicated since it is a live vaccine, and there is an inactivated vaccine (i.e., IIV) available. Further, the lack of efficacy of LAIV among the US general population during recent seasons has resulted in this vaccine not currently being recommended for any population group [9]. US guidelines do not indicate a preference for the specific type of IIV among HIV-infected persons [9].
In addition to the standard-dose inactivated vaccine, a high-dose vaccine (containing four times the hemagglutinin antigenic content, Fluzone® high-dose) is available in the US (where it is approved for persons ≥65 years of age) and other geographic locations including Canada. This vaccine elicits improved antibody responses and greater effectiveness at protecting against influenza in select groups, and it has been shown to be cost-effective and prevent more deaths compared with the standard-dosed vaccine among the elderly [25,26,27]. Currently, the vaccine does not have a specific indication for younger HIV-infected adults in any of the guidelines.
The efficacy of influenza vaccination among HIV-infected persons is reduced compared with HIV-uninfected persons [28,29,30,31,32]. Poorer responses among HIV-infected persons may partly be attributed to reduced CD4 counts and HIV viremia [29]. However, studies among patients with well-controlled HIV have demonstrated poorer post-vaccination responses versus HIV-uninfected persons [28] suggesting that additional HIV-related factors, including heightened immune activation and inhibition of B cell and cytotoxic T-cell immune responses, may be responsible [29, 33, 34]. Additionally, HIV appears to worsen age-associated deficits of immune responses post-influenza vaccination [33]. A recent meta-analysis incorporating findings from several studies (i.e., three randomized-controlled trials and three cohort studies, n = 1562) confirmed that vaccination among HIV-infected adults reduces laboratory-confirmed influenza with a pooled efficacy of 85% (95% CI 22–97%); however, there were wide variations between the study results, and vaccination did not show a benefit for secondary outcomes [e.g., influenza-like illness (ILI)] [35]. A randomized trial among HIV-infected pregnant women noted a vaccine efficacy of 58% [36].
Given these data [28, 29, 37], improving the immune responses generated after influenza vaccination is of clinical interest. In one study, the administration of a second dose of influenza vaccine (this study utilized the H1N1 influenza vaccine) significantly increased seroprotective responses (from 68% to 92% after the second dose); however, the study utilized an adjuvant plus vaccine [38]. Current guidelines do not recommend additional doses of influenza vaccination during the same season. Another potential strategy is the utilization of vaccines with higher antigen content. The use of a high-dose vaccine (Fluzone®, which contains 60 mcg of antigen per strain vs. 15 mcg) was evaluated among 190 HIV-infected adults. In this study, seroprotection rates were greater in the high-dose group for H1N1 (96% vs. 87%, p = 0.03) and influenza B (91% vs. 80%, p = 0.03) and similar for H3N2 (96% vs. 92%, p = 0.30) strains [39]. However, a more recent, smaller study of HIV-infected children and young adults did not show improved antibody responses with high-dose vaccination [40]. Intradermal vaccines have been studied, and although they allow for the use of smaller antigenic doses, they do not appear to elicit greater immune responses and may be associated with more local and systemic side effects [41, 42]. Finally, the use of adjuvanted vaccines (e.g., with AS03® or MF59® adjuvants) have generally produced greater immune responses post-vaccination [38, 43,44,45]. An adjuvanted vaccine is now available in the US (Fluad™) and is targeted for persons ≥65 years, but has not been studied or approved specifically for HIV-infected adults. Although the aforementioned studies suggest the potential for improvement in antibody responses using these alternate vaccine approaches, studies have been limited and have not evaluated effectiveness in preventing clinical influenza; hence, none of these strategies are currently recommended by guidelines [7,8,9,10,11,12].
Some health care providers have wondered if HIV-infected persons should be preferentially vaccinated later in influenza season because of concerns regarding possible reduced durability of protection. Vaccination generally elicits immune protection 2 weeks after vaccination, but the duration of protection has been questioned. A recent study among the general population found waning of effectiveness over time with ~7% loss of efficacy per month, although most recipients remained protected during the influenza season (October–April in the Northern hemisphere) post-vaccination [46]. Among immunocompromised hosts, however, durability may be shortened given lower post-vaccination antibody responses [47]. A retrospective study among HIV-infected persons in the US showed that those who received influenza vaccine early in the season were more likely to develop influenza or an ILI than those vaccinated later in the season (i.e., after 15 November) [48]. Additional data from Canada also suggest that waiting later (mid-November to early December) [49] is preferred. As such, the BHIVA recommends vaccine administration between September and early November [8], while US guidelines do not advocate for a specific timeframe for influenza vaccination among HIV-infected adults [9, 10, 13]. Vaccination can continue until March [8] and until community influenza activity has ended. Of note, defining narrow windows for vaccination must be weighed against the possibility of influenza occurring early in the season and missed vaccination opportunities.
Despite challenges in the efficacy and durability of influenza vaccination, guidelines recommend the use of the influenza vaccine since it provides some level of protection and reduces severe complications [17]. Despite these recommendations, vaccine coverage remains suboptimal among HIV-infected adults in many locations including the US (average 38% coverage, range 26–50%) [50]; therefore, targeted efforts for optimizing vaccine rates are advocated.
Influenza vaccination has been shown to be safe overall with local reactions being the most common reaction. Pregnant women can receive the inactivated vaccines with studies demonstrating safety in this group [36]. No long-term negative effects on CD4 counts, HIV RNA levels, or progression to AIDS or death have been noted [51]. Persons with mild egg allergies (only hives without other allergic symptoms) may receive the inactivated vaccine per the US CDC guidelines [9]. A recombinant vaccine (not made using eggs or egg proteins, FluBlok®) is also available in some countries (e.g., US, Mexico) for those with more severe forms of egg allergy [9]. For those with an allergy to the vaccine itself or with a history of severe reactions (e.g., Guillain-Barré syndrome), vaccination should be avoided unless deemed safe by an expert in this field (e.g., allergy/immunology specialist). For those not able to receive vaccination, anti-viral prophylaxis may be warranted, especially among those at high risk of exposure and severe disease. Additionally, those exposed and not vaccinated or those who may not have generated an adequate post-vaccination response (e.g., CD4 count <200 cells/mm3) should be considered for antiviral prophylaxis (e.g., with oseltamivir). Finally, vaccinating close contacts to reduce the possibility of influenza exposure is recommended.
Pneumococcal
HIV-infected persons have been recognized to be at risk for pneumococcal disease since the beginning of the epidemic [52] and continue to have an elevated risk (20- to 40-fold higher) despite the use of ART [1, 53,54,55]. The elevated risk is due to immunodeficiency as well as the concurrent high rate of adverse health behaviors (smoking, drug use) in this population. Infections caused by Streptococcus pneumoniae include invasive disease (e.g., meningitis, bacteremia) and pneumonia. There are currently two main types of pneumococcal vaccination—the polysaccharide pneumococcal vaccine (PPV), which contains 23 serotypes (covering ~85% to 90% of the strains leading to invasive disease), and the conjugate pneumococcal vaccine (PCV) containing up to 13 serotypes depending on the valency (the same serotypes are also included in PPV except 6A).
The current WHO guidelines (published in 2012) do not recommend PPV for HIV-infected adults residing in resource-limited settings given competing health priorities and a low level of evidence to support its use in this setting (Table 1) [7]. The conjugate vaccine, PCV, is not discussed in the WHO guidelines for HIV-infected adults [7]; however, recommendations were published prior to the availability of several studies regarding this vaccine in adults.
British and US guidelines [8,9,10,11, 13] recommend pneumococcal vaccination among HIV-infected adults, although the type and number of vaccinations differ by guideline (Table 1). The BHIVA guidelines recommend that HIV-infected adults receive 1 dose of PCV given its proven immunogenicity and efficacy in HIV-infected persons [8]. This recommendation is largely based on a randomized, double-blind, placebo-controlled trial (using PCV-7) among HIV-infected adults in Malawi, which showed a 74% efficacy against vaccine-type invasive pneumococcal disease, with good efficacy even at CD4 counts <200 cells/mm3 [56]. Hence, BHIVA guidelines recommend a single dose of PCV among HIV-infected adults irrespective of CD4 count, HIV viral load, or ART use. The BHIVA currently recommends PPV only among HIV-infected persons who are >65 years or among younger adults with a concurrent comorbidity (e.g., asplenia) requiring vaccination based on the national program recommendations. This represents a change from the prior BHIVA guideline in 2008 that had recommended PPV for all HIV-infected adults. When both PPV and PCV vaccines are administered, BHIVA guidelines recommend that doses be separated by at least 3 months. Repeat doses of either vaccine (PCV or PPV) are not currently recommended [8]. Similar to the BHIVA guidelines, the EACS guidelines also recommend a dose of PCV-13 instead of PPV and state no recommendations for booster doses [12]. The French guidelines differ by advising both vaccines with an initial dose of PCV followed by PPV at least 2 months later; among those already having received PPV, at least 3 years should elapse, and then administering PCV followed by PPV 2 months later is recommended [14].
US recommendations advise the administration of both PPV and PCV among HIV-infected adults regardless of concurrent comorbidities. PCV (i.e., Prevnar-13®) is recommended at HIV diagnoses regardless of CD4 count [9,10,11, 13]. The use of PCV as the initial vaccination is based on its excellent priming ability and efficacy [56]. The continued recommendation for PPV among HIV-infected adults is based on the additive risk that HIV conveys for the development of invasive pneumococcal disease, studies that show PPV reduces pneumococcal bacteremia and death [55, 57, 58], and the additional serotypes covered compared with PCV-13. This recommendation is also supported by studies showing that a PCV prime followed by a PPV boost strategy may enhance both the breadth and magnitude of antibody responses among HIV-infected adults [59, 60], although the clinical impact of this strategy remains unclear [61, 62]. Overall, US guidelines recommend PCV followed by PPV administered ≥8 weeks later in pneumococcal vaccine-naïve persons. The delay in the timing between the vaccinations is to reduce hyporesponsiveness [30, 59, 61]. Since HIV-infected persons with CD4 counts <200 cells/mm3 may have poorer vaccine responses to PPV, vaccination can be deferred until the CD4 count is ≥200 cells/mm3 if ART will be initiated soon [10]; alternatively, if administered before immune reconstitution, revaccination may be offered after a CD4 count >200 cells/mm3 has been achieved [13]. Revaccination with PPV is also recommended at 5 years after the initial PPV dose and then again at age ≥65 years (≥5 years should separate each PPV dose). If a newly diagnosed HIV-infected adult has already received PPV, a single dose of PCV is administered ≥1 year after the last PPV dose and then another PPV dose ≥5 years after the initial PPV vaccination [9, 63]. Although US guidelines recommend repeated PPV doses, it only recommends a single dose of PCV.
The divergent guidance regarding pneumococcal vaccination by various advisory groups is likely reflective of the timing of the publication of each guideline, the pros and cons of each type of vaccine (e.g., PCV has improved immunogenicity, but covers fewer serotypes), the paucity of large, randomized clinical efficacy studies on pneumococcal vaccinations among HIV-infected adults, and divergent results from studies conducted in the developed vs. developing world. For example, PPV efficacy is mainly based on observational data that have shown divergent results [55, 57, 64,65,66], and a randomized, double-blind, placebo-controlled trial in Uganda found a higher risk of pneumonia following PPV administration in HIV-infected adults not receiving ART [67] (although additional follow-up noted a decrease in all-cause mortality post-vaccination) [58]. Further, there are no current head-to-head trials comparing PPV with PCV among HIV-infected adults. A recent systematic review of the existing data (including 1 randomized trial and 15 observational studies) in HIV-infected adults concluded there was moderate evidence to support PPV use [68]. In summary, the US and French guidelines currently recommend both PPV and PCV in distinction to the WHO, BHIVA, and EACS guidelines. Even though the former approach may provide the most anti-pneumococcal protection to HIV-infected persons if doses are appropriately sequenced, the overall cost-effectiveness and efficacy compared with simpler strategies (i.e., a single PCV dose) remain unclear.
Updates to current pneumococcal vaccine guidelines are anticipated as further data on vaccine efficacy become available as well as the patterns of disease and causative serotypes change over time. For example, since the introduction of PCV among infants is associated with herd protection, a shift of invasive infections due to replacement strains (not contained in PCV) is emerging [69]. As such, surveillance data on the serotypes causing disease among HIV-infected adults in diverse geographic locations are needed to inform future vaccine guidelines. Further, a conjugate vaccine containing additional serotypes (beyond those in PCV-13) is desirable, but not yet available.
Regarding PPV23 immunogenicity, data have shown reduced immune responses to PPV among HIV-infected persons compared with HIV-uninfected persons, with some studies demonstrating poorer responses at lower CD4 counts [70, 71]. Regarding efficacy, observational studies have shown varying results with a 20–79% effectiveness of PPV for preventing invasive disease and 20–35% for pneumonia [8], although some studies have shown no benefit. As noted above, a review found moderate evidence for a reduced risk of invasive disease after PPV administration among HIV-infected adults [68], although further data on clinical efficacy are needed.
Due to concerns regarding the limited durability of immune responses after PPV among immunosuppressed persons [72], revaccination with a second dose of PPV at 5 years has demonstrated increased antibody responses, although the magnitude and breath of responses were reduced compared with those originally observed after the first dose [73]. Although immunogenicity studies have been performed, we are unaware of any clinical efficacy data to support the use of repeated PPV doses among HIV-infected adults. Hence, whether repeated PPV vaccinations are clinically beneficial and the ideal timing for revaccination remain unknown. At this time, US guidelines recommend PPV vaccination with a booster at 5 years and again at age 65 years (assuming 5 years has elapsed from the prior dose) for a total of three doses over time, but BHIVA and EACS guidelines do not recommend doses (either initial or booster) of PPV for HIV-infected adults without additional indications (beyond HIV infection alone).
Regarding PCV immunogenicity, HIV-infected persons generate reduced antibody levels compared with HIV-uninfected persons after vaccination [74, 75], similar to those noted for PPV. Regarding efficacy, as noted above, a randomized trial demonstrated a 74% efficacy at reducing invasive disease [56]. Although this trial utilized two doses of PCV, the additional dose may provide little, if any, additional benefit [76, 77]. BHIVA, EACS, French, and US guidelines [8,9,10, 12] recommend a single dose of PCV among HIV-infected adults; no additional PCV doses are recommended by any guideline.
Both PPV and PCV have shown no serious safety concerns, with the most common reported adverse event of local reactions, with fevers or myalgias reported in <1%. Some data suggest more local pain at the injection site after PCV vaccination than after PPV, perhaps given the greater immunogenicity of the former vaccine [61, 78].
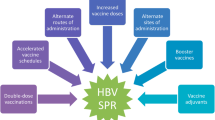
Hepatitis B Virus
HBV is important among HIV-infected persons given the viruses’ shared routes of transmission. Additionally, HIV-infected persons have both a higher risk of HBV infection after exposure and an increased risk for progression to cirrhosis and HBV-related complications after infection [3, 79]. Further, chronic HBV infection is associated with poorer HIV outcomes, with a nearly two-fold higher risk of AIDS and/or death [80, 81].
All guidelines included in this review recommend that non-immune HIV-infected persons be vaccinated against HBV (Table 2). This is because vaccination has been shown to reduce the risk of both newly acquired HBV infections and the development of chronic infections among those newly infected [82].
Testing for HBV infection and immunity is recommended among HIV-infected adults. In resource-limited settings, testing prior to vaccination can be deferred if not available [7]. Although the exact tests to evaluate for HBV immunity vary by guideline, obtaining hepatitis B surface antigen (HBsAg), antibody to hepatitis B core antigen (anti-HBc), and antibody to hepatitis B surface antigen (anti-HBs) provides the most complete picture of HBV status [10]. The presence of anti-HBs at levels of ≥10 mIU/ml is consistent with seroprotection, and vaccination is not required. Some people have an isolated positive anti-HBc (HBsAg negative and anti-HBs negative). This pattern represents: (1) a false positive test, (2) a resolved infection with waning anti-HBs over time, or (3) a chronic HBV infection with an undetectable HBsAg. The latter group may have chronic inactive infection (HBV DNA is undetectable) or ‘occult’ infection (HBV DNA is detectable). Among those with an isolated anti-HBc, testing for HBV DNA is recommended by the US guidelines and, if negative, then the HBV vaccine series administered [13]. The BHIVA guidelines suggest administration of a single dose of vaccine rather than DNA testing to evaluate for an anamnestic response, and if a response is detected (anti-HBs ≥10 mIU/ml), no further vaccination is needed; if the anti-HBs are <10 mIU/ml, then completion of a series is advised [8]. Of note, studies among HIV-infected persons with an isolated anti-HBc have generally shown a low rate of anamnestic responses, suggesting that a full vaccine series is often needed [83, 84]. The French guidelines are similar to the BHIVA guidelines [14]. Contrary to the US and BHIVA guidelines, the EACS guidelines currently state that given the lack of data on the impact of immunization in isolated anti-HBc positive persons, vaccination is not presently recommended for this group [12].
Among HIV-infected adults requiring vaccination, the WHO guidelines recommend the use of standard dosing (20 mcg) with either a schedule of 0, 1, and 6 months or 0, 1, 2, and 12 months for those with a CD4 count >500 cells/mm3 [6]. Those with lower CD4 counts (200–500 cells/mm3) are advised to receive the latter more intensive schedule. The WHO recommends deferring vaccination among those with a CD4 count <200 cells/mm3 until ART has been started, and the CD4 count has risen to >200 cells/mm3. These recommendations are based on studies showing a strong association between pre-vaccination CD4 counts and ART use on post-vaccine immune responses [85, 86]. If a person does not respond to vaccination (anti-HBs <10 mIU/ml measured ≥4–8 weeks after the series), then booster doses or initiation of a new vaccination series using higher doses (40 mcg) in a four-dose series is advised; of note, varying strategies have been cited in different WHO protocols [6, 7, 87].
The BHIVA recommends that non-immune persons receive a non-adjuvanted vaccine (e.g., Engerix B® or HBvaxPRO®) at a dose of 40 mcg or an adjuvanted vaccine (i.e., Fendrix®) at a 20 mcg dose [8]. Each are recommended as a four-dose series (0, 1, 2, and 6 months). An ultra-rapid course [using 3 standard doses (not higher doses given lack of data) over 3 weeks] can be considered if there is an urgency to ensure rapid completion of the series, but is not recommended among those with CD4 counts <500 cells/mm3. For those not responding to the initial series, three more doses are recommended (Engerix B®, HBvaxPRO®, or Fendrix® with a slight preference for Fendrix®) [88] with doses given at monthly intervals. Among non-responders to the initial series with low CD4 counts, delaying the revaccination series until a CD4 count of >350 cells/mm3 and viral load suppression on ART have been achieved can be considered. Finally, those with a low protective level after the initial series (defined as ≥10, but <100 mIU/ml) are to be offered a single dose booster based on data showing that this group will have a titer <10 mIU/ml in the near future [89]. Similarly, the EACS and French guidelines recommend vaccination among those without anti-HBs [12, 14]. The EACS suggests that among initial non-responders, re-vaccination should be considered using the double-dose vaccine (40 mcg) at 3–4 time points (months 0, 1, 6, and 12) to help to improve response rates [12]. The French guidelines recommend initial HBV vaccination using 40 mcg at four time points (0, 1, 2, and 6 months) and recommend that initial non-responders receive high-dose (40 mcg) vaccination every 1–2 months until a protective titer has been achieved, but without exceeding six injections in total [14]. Further guidance is based on national guidelines [12].
In the US, Engerix-B® (20 mcg/ml) or Recombivax HB® (10 mcg/ml) as a three-dose series (0, 1, and 6 months) or Engerix-B® (40 mcg/ml) or Recombivax HB® (20 mcg/ml) as a four-dose (0, 1, 2, and 6 months) series is recommended. Guidelines have increasingly recommended higher doses of HBV vaccine among immunosuppressed persons including those with HIV [10, 13]. Similar to other guidelines, seroprotection should be measured 4 weeks after the initial vaccine series, and those with anti-HBs <10 mIU/ml should be revaccinated with a second series with advisement for the higher dose series (e.g., 40 mcg/ml Engerix-B® at 0, 1, 2, and 6 months). In addition, consideration for delaying the revaccination series until CD4 count improvement and ART receipt is suggested, but must be balanced with data suggesting that a longer time to revaccination may predict non-response to the second series [90] and that they may be at risk for newly acquired HBV infection.
Regarding HBV vaccine interruption, a real-life situation given the need for multiple vaccine doses over a 6-month period, the vaccine series can simply be resumed. The use of tracking and electronic (including text) reminders may be useful for ensuring series completion [91].
Regarding vaccine immunogenicity, seroprotective HBV vaccine responses are lower among HIV-infected compared with HIV-uninfected persons, with rates of 18–71% and 60–95%, respectively [11, 92,93,94,95,96]. Patients vaccinated prior to HIV infection have seroprotective responses similar to HIV-uninfected persons [97], suggesting that completion of the vaccine series prior to HIV infection is optimal. Among those already HIV-infected, receiving at least three doses, not using the accelerated schedule, higher CD4 counts, lower HIV viral loads, and receipt of ART have been associated with improved post-vaccination responses [85, 98, 99].
Given the lower seroconversion rates among HIV-infected persons, higher doses of HBV vaccine (40 vs. 20 mcg/ml) for the initial vaccine series have been advocated. For example, HIV-infected persons randomized to a standard dose (20 mcg/ml) vs. double dose (40 mcg/ml) of recombinant hepatitis B vaccine found seroconversion rates of 34% vs. 47%, respectively (p = 0.07) [100]. Interestingly, higher seroconversion rates were noted among those with CD4 counts ≥350 cells/mm3, but not with lower CD4 counts. In another study, the percentage of responders was 82% in the group receiving 40 mcg/ml (using a 4-dose vaccine series) and 65% in the 20 mcg/ml group (using a 3-dose vaccine series) (p < 0.001) [101]. Finally, a meta-analysis including five clinical studies (n = 883 HIV-infected persons, most of whom were vaccine naïve) found a significant increase in response rates using the higher dose vaccine (OR 1.96, 95% CI 1.47–2.61) [102].
Response rates to a second vaccine series vary, but have been reported as 36–85% [98, 103, 104]. Since vaccine response rates are correlated with the immunocompetence of the host, some experts suggest delaying the second vaccine series until receipt of ART and achievement of a higher CD4 count. Some, but not all, studies have found superior response rates for high-dose versus standard-dose revaccination series [105,106,107]. Importantly, persons who were non-responders to primary vaccination series but who responded to revaccination lost protective anti-HB concentrations faster than those who responded after the first vaccination cycle; hence, this group may benefit from closer follow-up evaluations of protective anti-HB levels [103, 108]. Overall, the varying guidelines’ recommendations exemplify the less than ideal vaccine responses and somewhat conflicting data for the best approaches for HBV vaccination among HIV-infected persons; however, all guidelines recommend vaccination in an effort to protect non-immune persons.
Among those who receive a second vaccine series, a post-vaccination level should again be measured 4–8 weeks after the series per all the guidelines; among those who still do not have an anti-HBs >10 mIU/ml, the benefit of additional doses is unclear, and they are generally not recommended. These persons should be advised of their risk for HBV infection and counseled on appropriate precautions. In addition, those who do not respond to the revaccination series should be tested for HBsAg to exclude chronic infection. Some guidelines (e.g., BHIVA, WHO) also recommend annual HbsAg testing [8], or HbsAg and anti-HBc testing [6, 87], among non-responders to evaluate for potential newly acquired HBV infections over time. Of note, HIV-infected persons receiving antiretroviral therapy with tenofovir (either TDF or TAF), emtricitabine, or lamivudine may have additional protection against HBV infection given the anti-HBV activity of these agents [82, 109, 110].
The durability of the immune responses after HBV vaccination and the significance of seroreversion remain important questions. In the general population, initial vaccine responses appear to predict life-long HBV immunity, and retesting is generally not recommended [111]. Although few data exist among HIV-infected persons, the anti-HBs level measured 4 weeks after vaccine series completion appears to predict the durability of seroprotection [89, 112]. For example, those with a level 10–100 mIU/ml, 100–1000 mIU/ml, and >1000 mIU/ml had a mean time to loss of a seroprotective anti-HBs level of 2, 3.7, and 4.4 years, respectively, in one study [112]. While US guidelines do not specifically recommend follow-up testing among vaccinees with an initial titer antiHBs >10 mIU/ml [10, 13], the WHO, BHIVA, and French guidelines recommend regular testing of anti-HBs levels (e.g., every 1–4 years depending on the specific guideline and based on both the initial antibody level and HIV control over time) [6, 8, 14, 87]; of note, studies have found a relationship between suppressed HIV viral loads and improved anti-HB levels over time [89, 113]. Those whose anti-HBs level becomes <10 mIU/ml are recommended to receive a booster dose [6, 8, 14].
HBV vaccines are considered safe with the most common side effect being local site reactions. Studies have found significantly higher rates of local adverse reactions [107] and pain at the injection site with high dose (40 mcg) compared to standard dose (20 mcg) [114].
Tetanus, Diphtheria, and Pertussis
Since these diseases do not have elevated incidence rates and are not known to be associated with poorer outcomes among HIV-infected adults, vaccination recommendations mirror those for the general population. All major guidelines advise receipt of these vaccinations among HIV-infected adults stating that the primary doses are generally given during infancy, with boosters administered periodically to adults over time (Table 1). Specific guidance regarding those with an unknown or incomplete receipt of the primary series is addressed in each guideline [6,7,8,9].
For those having received the primary vaccination series, WHO recommends tetanus toxoid (TT) and/or tetanus-diphtheria (Td) vaccines given to HIV-infected adults using the same schedule and doses as for HIV-uninfected persons [6]. The guidelines stress the importance of vaccination especially among illicit drug users to prevent tetanus, especially in areas without needle exchange programs. Tdap vaccination is not specifically mentioned in the context of HIV-infected adults, but is recommended among pregnant women (during the 2nd or 3rd trimesters) and for healthcare workers caring for those at risk for disease (e.g., infants).
The BHIVA guidelines recommend giving a Td booster every 10 years, especially among those at risk for exposure (e.g., travel to an area where post-exposure prophylaxis would be difficult to receive after a tetanus-prone injury), among those who received the full primary vaccination series (5 doses) [8]. Among those >50 years, shortening the interval for booster doses to every 5 years is suggested. Regarding pertussis, BHIVA recommends following the national guidelines, which currently recommend pertussis vaccination (e.g., Boostrix®) among pregnant women (28–32 weeks) and during an outbreak. Vaccination among those meeting indications is advised regardless of the CD4 count, HIV viral load, or ART use [8]. There are no specific EACS guidelines as HIV-infected persons should follow country guidance [12]. Similarly, French guidelines recommend following national vaccination recommendations including the administration of dTP boosters every 10 years without altered schedules among HIV-infected persons [14].
The US guidelines similarly recommend that previously vaccinated HIV-infected adults receive booster doses of Td every 10 years [9]. A single dose of Tdap (tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis; Boostrix® or Adacel®) is advised to replace a dose of Td if the person has not previously received Tdap. Additionally, HIV-infected adults who become pregnant should receive Tdap during each pregnancy (at 27–36 weeks). Also, HIV-infected adults caring for infants aged less than 12 months (at work or home) should also be considered for Tdap vaccination [9].
Compared with HIV-uninfected adults, studies have shown lower antibody responses after tetanus and diphtheria vaccination among HIV-infected persons [30, 115, 116]. For example, one study showed protective antibodies among 83–100% and 61–73% for tetanus and diphtheria, respectively, with variation by CD4 counts [115]. Durability is poorly studied, but a study among HIV-infected children found that response rates after tetanus vaccination waned quickly [117], raising the question whether Td boosters every 10 years are adequate. Further, seroprotective responses among older adults may be suboptimal [118]; hence, the BHIVA guidelines recommend considering more frequent booster dosing among those >50 years [8]. There are no current data regarding responses to the pertussis vaccination among HIV-infected adults, but antibody titers are lower than expected among HIV-infected children [119].
Vaccination is overall safe with no increased adverse events noted among HIV-infected adults.
Inactivated Vaccines for HIV-Infected Adults who Have Additional Risk Factors or Specific Age Groups
Hepatitis A Virus
HIV-infected adults who are illicit drug users and men who have sex with men (MSM) are at risk for HAV infection [120, 121]. The presence and severity of symptomatic HAV infection increases with age; however, HIV infection per se does not predict a more severe course, although prolonged viremia has been described [120, 122].
Guidelines recommend HAV vaccination among non-immune HIV-infected persons who have specific risks such as drug use (both injection and non-injection) and among MSM [8, 9, 14]. In addition, those traveling to countries endemic for the disease and potential household or occupational exposures are also mentioned in some of the guidelines (Table 3). Recent guidelines from the HIV Medicine Association of the Infectious Diseases Society of America also recommend considering vaccination for all nonimmune HIV-positive persons regardless of risk factors [13]; however, other guidelines (e.g., BHIVA, WHO, and the US CDC) do not contain this specific recommendation [6,7,8,9].
Prevaccination screening for HAV IgG to determine whether a person is already immune can be considered. Its cost effectiveness is based on the existence of risk factors for prior HAV infection such as being born or living for extensive periods in areas of high endemicity and those >50 years [8]. Prior infection confers lifelong protection, and vaccination is not needed in this group.
WHO guidelines recommend a two-dose vaccine series given at 0 and 6–12 months [6] among HIV-infected persons who are in one or more of the following risk groups: MSM, drug users, chronic liver disease (such as HCV and HBV-coinfected), clotting factor disorders, occupational risks, or traveling to a country with high or intermediate risk of HAV infection. For the HIV-infected person, the use of the inactivated (vs. live) vaccine is recommended. While post-vaccination testing is not recommended given the vaccine’s excellent immunogenicity and durability in the general population, the guideline does not specifically address post-vaccination testing and repeat doses for the HIV-infected adult.
The BHIVA guideline recommends HAV vaccination among those with risk factors of HAV acquisition. These are similar to the WHO guidelines, although BHIVA does not mention chronic liver disease, but does additionally include household or sexual contacts of infected persons, individuals at risk of infection during outbreaks, and persons with special needs living in residential institutions [8]. A two-dose vaccine series at 0 and 6 months is advised for those with a CD4 count >350 cells/mm3 and a three-dose series at 0, 1, and 6 months for those with a CD4 <350 cells/mm3. The reason for this recommendation is the poorer vaccine responses at lower CD4 counts and studies showing improved seroconversion rates and higher antibody titers using the three-dose strategy [123, 124]. Additionally, they recommend using the monovalent vaccine (rather than the combined HAV/HBV vaccine) because of superior responses noted in at least one study [125] and because the combination vaccine typically contains only 720 ELISA units of HAV antigen (versus 1440). The BHIVA guidelines recommend that if the risk factor for HAV persists, persons should be revaccinated with a single dose of the HAV vaccine every 10 years, although evidence for this recommendation is limited [8]. Similarly, the EACS and French guidelines recommend vaccination of HIV-infected persons based on their risk profile (e.g., MSM, travel, IVDU, active hepatitis B or C infection) if anti-HAV IgG seronegative [12, 14]. The French guidelines recommend administering two doses (0, 6–12 months) and, if the post-series titer is <20 mIU/ml, then a third dose is given [14].
In the US, non-immune persons at risk for HAV infection (similar to risk factors noted above) should receive a two-dose series (Havrix® at 0 and 6–12 months or Vaqta® at 0 and 6–18 months) [9]. Unlike the other guidelines, the US CDC recommends that the antibody response (total or IgG anti-HAV) be assessed 1 month after completion of the series and, if negative, revaccination provided preferably after the CD4 count is >200 cells/mm3 [10]. Monitoring antibody levels over time for vaccine seroprotection durability is not mentioned in the current US guidelines.
Regarding vaccine immunogenicity, seroresponses post-vaccination are lower among HIV-infected persons compared with HIV-uninfected persons in whom ~95% respond [126]. While the majority of HIV-infected adults develop antibody responses to HAV vaccination, overall seroconversion rates are 50–96% and vary by CD4 count [123, 126,127,128,129,130,131]. For example, in a study of early diagnosed HIV-infected persons, those with a CD4 cell count ≥300 cells/mm3 had a seroconversion rate of 100% vs. 87% among those with a CD4 count of <300 cells/mm3 [131]. The use of an accelerated (0, 7, 21 days, and 6 months) vs. standard dosing (0, 6 months) schedule also is associated with poorer immune responses [128].
To potentially improve vaccine responses in HIV-infected adults, one study examined three vs. two doses with seroconversion rates (defined as an anti-HAV antibody ≥20 mIU/ml) of 83% and 69%, respectively (p = 0.13) [123]. In addition, a study that followed anti-HAV antibody titers over 5 years in HIV-positive persons noted that three- versus two-dose series resulted in higher antibody titers and more durable responses over time [132]. Given the overall paucity of data in this area, only BHIVA currently recommends the three-dose series among those at risk for poor vaccine responses (CD4 count <350 cells/mm3) [8]. The US guidelines address this concern by advocating for checking the post-vaccination HAV IgG antibody levels among HIV-infected persons and revaccinating if needed [10, 13].
Regarding the durability of HAV vaccine responses, one study showed that 85% of HIV-infected adults maintained a seropositive response at 6–10 years after a two-dose vaccine series [133], while another study showed 76% had seropositive responses at 5 years [130]. To date, there are no uniform guidelines regarding monitoring anti-HAV levels over time. Regarding revaccination with additional HAV vaccine doses over time among HIV-infected adults, the BHIVA recommends every 10 years among those remaining at risk, but data are limited to support this recommendation [8].
HAV vaccination has been found to be safe. Adverse events are typically minor with local site reactions being commonly reported followed by mild systemic side effects including self-limited headache and fever [131].
Human Papillomavirus (HPV)
HPV is the most common sexually transmitted infection (STI) in the world. There are over 150 HPV types with HPV 6 and 11 accounting for 90% of genital warts and HPV 16 and 18 for >60% of associated cancers in the general population. HIV-infected persons have an elevated risk of HPV infections and persistence as well as the subsequent development of HPV-related cancers (e.g., cervical, anal) [4, 5]. For example, HIV-infected MSM have an anal cancer incidence of 131/100,000 vs. 46/100,000 in non-MSM HIV-infected men and 2/100,000 in HIV-negative men [134]. Despite the use of ART, a higher risk for HPV-related disease persists [134]. As such, HIV-infected adolescents and adults, especially MSM, are important target groups for vaccination. In spite of the high occurrence of HPV and sequelae in the MSM population, there is a general lack of knowledge regarding the importance of HPV vaccination in this group. Opportunities to optimize HPV vaccination by improving awareness through public health campaigns and bundling of HPV vaccination with other health visits are advocated [135, 136].
The optimal timing of HPV vaccination is prior to sexual debut as the HPV vaccine is designed to prevent initial HPV infection. Nonetheless, a sizable proportion of HIV-infected persons may benefit from vaccination especially when considering all serotypes contained within the newer vaccines. A cross-sectional study in HIV-infected men and women (median age of 47 years) found that 73% were infected with at least one HPV vaccine type (HPV 16: 64%; HPV 6: 39%; HPV 18: 31%; HPV 11: 8%); however, most had not been exposed to all currently available vaccine serotypes [137]. Since rates of concurrent HPV infections vary by age, gender, sexual history, and geographic region, population-specific data are needed to inform vaccine guidance.
There are three available vaccines: a bivalent vaccine, Cervarix®, which has coverage against two high-risk HPV serotypes (HPV 16 and 18); a quadrivalent vaccine, Gardasil-4®, which protects against four serotypes (HPV 6, 11, 16, and 18); a nine-valent vaccine (Gardasil-9®), which also covers 31, 33, 45, 52, and 58 (covering an additional 14% of female cancers and 4% of male cancers) [10]. Cervarix® is approved for women, while Gardasil-4® and Gardasil-9® are approved for both men and women. Vaccines are administered at 0, 1–2, and 6 months, and the series can simply be continued if interruption occurs. Recent data suggest that vaccination in the general population can be given as a two-dose series (0 and 6 months) if begun before age 15 years, but data for this strategy among HIV-infected persons are lacking; hence, a three-dose series is recommended for this group. It is not necessary to screen for HPV infection prior to vaccination, and a history of genital warts, abnormal cytology, or positive HPV DNA test results is not a contraindication to vaccination.
The WHO recommends targeted HPV vaccination for young females (9–13 years of age) regardless of HIV status (Table 3) [7]. If resources allow, vaccination of older adolescent and young women is advised, with additional coverage of males thereafter. Among HIV-infected persons, guidelines recommend using a three-dose schedule (0, 1–2, and 6 months). Vaccination is advised irrespective of receipt of ART.
The BHIVA guidelines recommend HPV vaccination for HIV-infected men and women ages 9–26 years, mirroring general population guidelines [8]. They also recommend vaccination up to the age of 40 years among HIV-positive MSM and HIV-positive women, albeit at a lower level of evidence rating. A recent study found that vaccinating HIV-infected MSM up to the age of 40 years is cost-effective [138]. HPV vaccination can be given regardless of HIV control status, but may be deferred among those with a CD4 count <200 cells/mm3 until after ART initiation. The guideline states a preference for Gardisal-9® if available given its more extended serotype coverage. Regarding the number of doses, BHIVA recommends continuing to utilize the three-dose vaccine series among HIV-infected persons given the current lack of data for fewer doses in this population. Finally, vaccination is also recommended for HIV-infected persons with a history of high-grade HPV disease given evidence that vaccination may reduce the risk of future recurrences [139]. EACS do not have specific guidelines for HIV-infected persons [12]. The French guidelines recommend HPV vaccination (3-dose schedule at 0, 2, and 6 months) among females and males (quadrivalent formulation specifically recommended for males) aged 11–19 years and MSM who are ≤26 years, similar to US guidelines [14].
In the US, HPV vaccination is recommended for HIV-infected persons (male and female) aged 9–26 years using a three-dose series [9]. The higher valency vaccines are preferred to cover additional serotypes [13]. The vaccine can be administered regardless of CD4 count or HIV viral load. No recommendations have been made regarding vaccinating older (i.e., >26 years) HIV-infected adults.
Immunogenicity studies among HIV-infected persons are becoming increasing available for both men and women of a variety of ages [140,141,142,143,144,145,146]. For example, in a study of adult HIV-infected men, seroconversion rates of ≥95% were found for each of the four main HPV types (HPV 6, 11, 16, and 18) [141]. In a study of HIV‐infected women aged 13–45 years, seroconversion 4 weeks after the third dose of the quadrivalent vaccine containing types 6, 11, 16, and 18 was 96, 98, 99, and 91%, respectively, at CD4 count >350 cells/mm3; 100, 98, 98, and 85%, respectively, at CD4 count 201–350 cells/mm3; 84, 92, 93, and 75%, respectively, at CD4 count ≤200 cells/mm3 [143]. Another study evaluated HIV-positive women (aged 15–66 years old) who received three doses of the quadrivalent vaccine and found seroconversion rates at month 24 to be 93, 94, 98, and 67% for HPV types 6, 11, 16, and 18, respectively [146]. Overall, post-vaccination responses are excellent among HIV-infected persons, albeit slightly lower than HIV-uninfected comparators with seroconversion rates 1 month after administration of the third vaccine dose, being 85% in the HIV-infected and 91% in the HIV-uninfected group (p = 0.52) [145]. Studies generally have shown that post-vaccination seroconversion rates and geometric mean titers post-vaccination are higher than after natural infection and are improved among those with high CD4 counts, suppressed HIV viral loads, and ART use [143]. HPV vaccination has excellent efficacy in preventing clinical disease (intraepithelial neoplasia, Pap abnormalities, and genital warts) in the general population [147, 148], but data on its clinical efficacy are currently lacking among HIV-infected persons. Regarding durability, protection is maintained for at least 10 years among HIV-uninfected persons; however, data among HIV-infected persons are needed. As universal early adolescent HPV vaccination is being rolled out in many countries (e.g., the US, Australia, and many European countries), data on the need and timing of boosters among adults, including those with HIV infection, are recommended.
The vaccine is generally safe and well tolerated. The most common side effect reported is local pain, and the most frequent systemic side effect is headache [145]. A double-blind, controlled trial that randomized HIV-positive adults to receive three doses of Cervarix® or Gardasil® found mild infection site reactions to be more common in the Cervarix® group versus the Gardasil® group (91% vs. 70%, p = 0.02) [149]. Both the quadrivalent and nine-valent vaccines are contraindicated in those with a history of immediate hypersensitivity to yeast. HPV vaccination is generally avoided during pregnancy; however, data to date do not suggest adverse outcomes [150], and pre-vaccination pregnancy testing is not advised among women who are not known to be pregnant per the US guidelines [9].
Meningococcal
Invasive meningococcal disease among HIV-infected persons has been recognized since the early epidemic [151], with outbreaks among MSM in a variety of large cities including New York City, Los Angeles, and Berlin [152,153,154]. An epidemiologic study recently estimated the risk of invasive disease among HIV-infected persons as ten-fold higher compared with the overall general population, with the greatest risk among those with CD4 counts <200 cells/mm3 [155]. In addition to the higher risk for disease [155, 156], HIV-infected persons with meningococcal disease have a higher risk of death with a case-fatality ratio of 20% among HIV-infected compared with 11% among HIV-uninfected individuals [157].
Available quadrivalent meningococcal vaccines include polysaccharide (Menomune®) and conjugate (Menactra® and Menveo®) vaccines for protection against serogroups A, C, Y, and W. In addition, single serogroup vaccines are available such as MenC (Meningitec®, Menjugate®, NeisVac-C®) and MenA (MenAfriVac®). Most recently, serogroup B vaccines have become available including MenB-4C (Bexsero®) and MenB-FHbp (Trumenba®) given as two doses (Bexsero® at 0 and ≥1 months apart; Trumenba® at 0 and 6 months). Given the evolving epidemiology of meningococcal disease, updated national guidelines should be consulted for the most recent guidance.
WHO recommends that countries with high (>10 cases/100,000 population/year) or intermediate endemic rates (2–10 cases/100,000 population/year) of invasive meningococcal disease and countries with frequent epidemics should introduce appropriate large-scale meningococcal vaccination programs (Table 3). These are typically focused among infants and young children, but can be extended to young adults, as exemplified by the large-scale MenA vaccine (MenAfriVac®) campaigns in the meningitis belt of Africa. In countries where the disease occurs less frequently (<2 cases per 100,000 population/year), vaccination is recommended for defined risk groups: those residing in closed communities (e.g., boarding schools or military camps); laboratory workers at risk of exposure to meningococcus; travelers to high-endemic areas; persons with immunodeficiency, including asplenia, terminal complement deficiencies, or advanced HIV infection. For each country, the choice of vaccine depends on the locally prevalent serogroup(s) of N. meningitidis with a preference for conjugate vaccine. The potential need for booster doses for long-term protection in adults is not specifically defined by current WHO guidelines, which note that further studies are needed to determine the frequency of repeated doses of vaccines among immunodeficient persons [7].
BHIVA guidelines recommend using national guidelines to inform meningococcal vaccination among HIV-infected persons. Specifically, HIV-infected persons <25 years of age not previously vaccinated, those with uncertain vaccine history, or who received the MenC at <10 years of age should be vaccinated with MenACWY and possibly MenB. In addition, HIV-infected persons with a history of asplenia, complement deficiency disorders, or risk for exposure via travel or outbreaks should be vaccinated. Two doses of MenACWY given 2 months apart is recommended as well as revaccination every 5 years if the risk remains [8]. Similarly, the EACS recommends vaccination as for the general population based on national guidance using a conjugate meningococcal vaccine (2 doses, 1–2 months apart) with boosters every 5 years if exposure continues; serotype B vaccination is not specifically mentioned [12]. French guidelines recommend meningococcal C vaccination (2 doses given 6 months apart) for those ≤24 years of age or among those with additional risk factors similar to the general population. In addition, a single dose of meningococcal C vaccine is advised among previously unvaccinated MSM >24 years, especially among those who frequent meeting places such as bars. The meningococcal B vaccine is not specifically recommended for HIV-infected adults [14]. Finally, HIV-infected adults exposed to a person with the disease should be provided antibiotic prophylaxis and appropriate vaccination [8].
In the US, guidelines have been recently updated to include HIV infection as an indication for MenACWY vaccination regardless of other specific indications [9]. Vaccination is given as a two-dose series (2 months apart) of the conjugate quadrivalent vaccination (e.g., Menactra®, Menveo®), and revaccination is recommended every 5 years. Meningococcal B vaccination is not specifically recommended for HIV-infected adults unless additional risk factors for serogroup B disease are present, as meningococcal disease in HIV-infected US adults is mainly caused by serogroups C, W, and Y.
Regarding immunogenicity, HIV-infected compared with HIV-uninfected persons have poorer responses especially among those with more advanced disease; hence, HIV-infected persons are often advised to have two vaccine doses (vs. a single dose) to improve post-vaccination immune responses as recommended by some guidelines (BHIVA, US). For example, in a study of HIV-positive youth, after one dose of the meningococcal serogroup C conjugate vaccine, 72% of the HIV-infected group and 100% of the HIV-uninfected group were protected; an additional dose in HIV-infected persons increased the response rate to 81% [158]. Regarding immune responses for each serogroup, the poorest responses are typically to serogroup C (seroconversion to A: 68%; C: 52%; Y: 73%; W: 63%); hence, a second dose may be especially important for protecting against disease from this serogroup [158,159,160]. Follow-up testing for post-vaccination immune responses is not currently recommended or widely available. Studies among HIV-infected persons are needed regarding clinical efficacy and durability as well as responses among older patients.
Regarding safety, no adverse signals have been reported among vaccinated HIV-infected persons.
Summary
Vaccination is a key component for preventing infectious complications among HIV-infected adults. Similar to the importance of ART and the achievement of robust immunologic responses in reducing subsequent infections, vaccines are also an essential component for ensuring the health of those living with HIV. Strategies to ensure vaccine coverage, for both the initial vaccination and subsequent boosters when applicable, are advocated. Since HIV-infected persons may have blunted post-vaccination immune responses and shorter durations of seroprotection, specific guidelines have been published to address these concerns. The current article serves to provide a concise summary of global and national recommendations for inactivated vaccinations among HIV-infected persons. While guidelines may contain varying vaccine recommendations for HIV-infected adults, this article serves to provide a concise summary of current recommendations in an effort to bolster strategies to protect HIV-infected adults from vaccine-preventable diseases.
References
Yin Z, Rice BD, Waight P, et al. Invasive pneumococcal disease among HIV-positive individuals, 2000–2009. AIDS. 2012;26:87–94.
Gordon MA. Invasive nontyphoidal Salmonella disease: epidemiology, pathogenesis and diagnosis. Curr Opin Infect Dis. 2011;24:484–9.
Thio CL, Seaberg EC, Skolasky R Jr, et al. Multicenter AIDS Cohort Study. HIV-1, hepatitis B virus, and risk of liver-related mortality in the Multicenter Cohort Study (MACS). Lancet. 2002;360:1921–6.
Palefsky JM, Holly EA, Ralston ML, Jay N. Prevalence and risk factors for human papillomavirus infection of the anal canal in human immunodeficiency virus (HIV)-positive and HIV-negative homosexual men. J Infect Dis. 1998;177:361–7.
Chaturvedi AK, Madeleine MM, Biggar RJ, Engels EA. Risk of human papillomavirus-associated cancers among persons with AIDS. J Natl Cancer Inst. 2009;101:1120–30.
World Health Organization Europe. Edited by Irina Eramova, Srdan Matic and Monique Munz. HIV/AIDS treatment and care: clinical protocols for the WHO European region. 2007. http://www.euro.who.int/__data/assets/pdf_file/0004/78106/E90840.pdf. Accessed Mar 30, 2017.
World Health Organization. Vaccine position papers. http://www.who.int/immunization/documents/positionpapers/en/. Accessed Mar 30, 2017.
British HIV Association Guidelines on the Use of Vaccines in HIV-Positive Adults 2015. http://www.bhiva.org/documents/Guidelines/Immunisation/consultation/BHIVA-Immunisation-Guidelines-2015-Consultation.pdf. Accessed Mar 30, 2017.
Kim DK, Riley LE, Harriman KH, Hunter P, Bridges CB; on behalf of the Advisory Committee on Immunization Practices. Recommended immunization schedule for adults aged 19 years or older, United States, 2017. Ann Intern Med. 2017;166:209–19.
Panel on Opportunistic Infections in HIV-Infected Adults and Adolescents. Guidelines for the prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. https://aidsinfo.nih.gov/contentfiles/lvguidelines/adult_OI.pdf. Accessed Mar 30, 2017.
Rubin LG, Levin MJ, Ljungman P, et al. 2013 IDSA clinical practice guideline for vaccination of the immunocompromised host. Clin Infect Dis. 2014;58:309–18.
European AIDS Clinical Society (EACS) Guidelines for the treatment of HIV. Version 8.2. January 2017. http://www.eacsociety.org/guidelines/eacs-guidelines/eacs-guidelines.html. Accessed Mar 30, 2017.
Aberg JA, Gallant JE, Ghanem KG, Emmanuel P, Zingman BS, Horberg MA. Primary care guidelines for the management of persons infected with HIV: 2013 update by the HIV medicine association of the Infectious Diseases Society of America. Clin Infect Dis. 2014;58:e1–34.
Frésard A, Gagneux-Brunon A, Lucht F, Botelho-Nevers E, Launay O. Immunization of HIV-infected adult patients—French recommendations. Hum Vaccin Immunother. 2016;12:2729–41.
Abadom TR, Smith AD, Tempia S, Madhi SA, Cohen C, Cohen AL. Risk factors associated with hospitalisation for influenza-associated severe acute respiratory illness in South Africa: a case-population study. Vaccine. 2016;34:5649–55.
Lin JC, Nichol KL. Excess mortality due to pneumonia or influenza during influenza seasons among persons with acquired immunodeficiency syndrome. Arch Intern Med. 2001;161:441–6.
Kunisaki K, Janoff E. Influenza in immunosuppressed populations: a review of infection frequency, morbidity, mortality, and vaccine responses. Lancet Infect Dis. 2009;9:493–504.
Radwan HM, Cheeseman SH, Lai KK, Ellison RT III. Influenza in human immunodeficiency virus-infected patients during the 1997–1998 influenza season. Clin Infect Dis. 2000;31:604–6.
Safrin S, Rush JD, Mills J. Influenza in patients with human immunodeficiency virus infection. Chest. 1990;98:33–7.
Cohen C, Moyes J, Tempia S, et al. Mortality amongst patients with influenza-associated severe acute respiratory illness, South Africa, 2009–2013. PLoS One. 2015;10:e0118884.
Sheth AN, Althoff KN, Brooks JT. Influenza susceptibility, severity, and shedding in HIV-infected adults: a review of the literature. Clin Infect Dis. 2011;52:219–27.
King JC Jr, Treanor J, Fast PE, et al. Comparison of the safety, vaccine virus shedding, and immunogenicity of influenza virus vaccine, trivalent, types A and B, live cold-adapted, administered to human immunodeficiency virus (HIV)-infected and non-HIV-infected adults. J Infect Dis. 2000;181:725–8.
King JC Jr, Fast PE, Zangwill KM, et al. Safety, vaccine virus shedding and immunogenicity of trivalent, cold-adapted, live attenuated influenza vaccine administered to human immunodeficiency virus infected and noninfected children. Pediatr Infect Dis J. 2001;20:1124–31.
Levin MJ, Song LY, Fenton T, et al. Shedding of live vaccine virus, comparative safety, and influenza-specific antibody responses after administration of live attenuated and inactivated trivalent influenza vaccines to HIV-infected children. Vaccine. 2008;26:4210–7.
DiazGranados CA, Dunning AJ, Kimmel M, et al. Efficacy of high-dose versus standard-dose influenza vaccine in older adults. N Engl J Med. 2014;371(17):635–45.
Falsey AR, Treanor JJ, Tornieporth N, et al. Randomized, double-blind controlled phase 3 trial comparing the immunogenicity of high-dose and standard-dose influenza vaccine in adults 65 years of age and older. J Infect Dis. 2009;200:172–80.
Shay DK, Chillarige Y, Kelman J, et al. Comparative effectiveness of high-dose versus standard-dose influenza vaccines among US Medicare beneficiaries in preventing postinfluenza deaths during 2012–2013 and 2013-2014. J Infect Dis. 2017;215:510–7.
Crum-Cianflone NF, Eberly LE, Duplessis C, et al. Immunogenicity of a monovalent 2009 influenza A (H1N1) vaccine in an immunocompromised population: a prospective study comparing HIV-infected adults with HIV-uninfected adults. Clin Infect Dis. 2011;52:138–46.
Tebas P, Frank I, Lewis M, et al. Center for AIDS Research and Clinical Trials Unit of the University of Pennsylvania. Poor immunogenicity of the H1N1 2009 vaccine in well controlled HIV-infected individuals. AIDS. 2010;24:2187–92.
Kroon FP, van Dissel JT, de Jong JC, van Furth R. Antibody response to influenza, tetanus and pneumococcal vaccines in HIV-seropositive individuals in relation to the number of CD4+ lymphocytes. AIDS. 1994;8:469–76.
Nelson KE, Clements ML, Miotti P, Cohn S, Polk BF. The influence of human immunodeficiency virus (HIV) infection on antibody responses to influenza vaccines. Ann Intern Med. 1988;109:383–8.
Tiu CT, Lin YS, Pagala M, et al. Antibody response to inactivated influenza A (H1N1) 2009 monovalent vaccine in patients with and without HIV. J Acquir Immune Defic Syndr. 2011;58:e99–102.
George VK, Pallikkuth S, Parmigiani A, et al. HIV infection worsens age-associated defects in antibody responses to influenza vaccine. J Infect Dis. 2015;211:1959–68.
Parmigiani A, Alcaide ML, Freguja R, et al. Impaired antibody response to influenza vaccine in HIV-infected and uninfected aging women is associated with immune activation and inflammation. PLoS One. 2013;8:e79816.
Remschmidt C, Wichmann O, Harder T. Influenza vaccination in HIV-infected individuals: systematic review and assessment of quality of evidence related to vaccine efficacy, effectiveness and safety. Vaccine. 2014;32:5585–92.
Madhi SA, Cutland CL, Kuwanda L, Maternal Flu Trial (Matflu) Team, et al. Influenza vaccination of pregnant women and protection of their infants. N Engl J Med. 2014;371:918–31.
Beck CR, McKenzie BC, Hashim AB, Harris RC, University of Nottingham Influenza and the ImmunoCompromised (UNIIC) Study Group, Nguyen-Van-Tam JS. Influenza vaccination for immunocompromised patients: systematic review and meta-analysis by etiology. J Infect Dis. 2012;206:1250–9.
Bickel M, von Hentig N, Wieters I, et al. Immune response after two doses of the novel split virion, adjuvanted pandemic H1N1 influenza A vaccine in HIV-1-infected patients. Clin Infect Dis. 2011;52:122–7.
McKittrick N, Frank I, Jacobson JM, et al. Improved immunogenicity with high-dose seasonal influenza vaccine in HIV-infected persons: a single-center, parallel, randomized trial. Ann Intern Med. 2013;158:19–26.
Hakim H, Allison KJ, Van de Velde LA, Tang L, Sun Y, Flynn PM, McCullers JA. Immunogenicity and safety of high-dose trivalent inactivated influenza vaccine compared to standard-dose vaccine in children and young adults with cancer or HIV infection. Vaccine. 2016;34:3141–8.
Seo YB, Lee J, Song JY, Choi HJ, Cheong HJ, Kim WJ. Safety and immunogenicity of influenza vaccine among HIV-infected adults: conventional vaccine vs. intradermal vaccine. Hum Vaccin Immunother. 2016;12:478–84.
Ansaldi F, Valle L, de Florentiis D, et al. Phase 4 randomized trial of intradermal low-antigen-content inactivated influenza vaccine versus standard-dose intramuscular vaccine in HIV-1-infected adults. Hum Vaccin Immunother. 2012;8:1048–52.
Durier C, Desaint C, Lucht F, ANRS 151 study group and the REIVAC network, et al. Long-term immunogenicity of two doses of, A/H1N1v vaccine with and without AS03(A) adjuvant in HIV-1-infected adults. AIDS. 2009;2013(27):87–93.
Iorio AM, Francisci D, Camilloni B, et al. Antibody responses and HIV-1 viral load in HIV-1-seropositive subjects immunised with either the MF59-adjuvanted influenza vaccine or a conventional non-adjuvanted subunit vaccine during highly active antiretroviral therapy. Vaccine. 2003;21:3629–37.
Cooper C, Klein M, Walmsley S, Phac Cihr Influenza Research Network, et al. High-level immunogenicity is achieved vaccine with adjuvanted pandemic H1N1(2009) and improved with booster dosing in a randomized trial of HIV-infected adults. HIV Clin Trials. 2012;13:23–32.
Ferdinands JM, Fry AM, Reynolds S, et al. Intraseason waning of influenza vaccine protection: evidence from the US Influenza Vaccine Effectiveness Network, 2011–2012 through 2014–2015. Clin Infect Dis. 2017;64:544–50.
Crum-Cianflone NF, Iverson E, Defang G, et al. Durability of antibody responses after receipt of the monovalent 2009 pandemic influenza A (H1N1) vaccine among HIV-infected and HIV-uninfected adults. Vaccine. 2011;29:3183–91.
Glinka ER, Smith DM, Johns ST. Timing matters—influenza vaccination to HIV-infected patients. HIV Med. 2016;17:601–4.
Werker GR, Sharif B, Sun H, Cooper C, Bansback N, Anis AH. Optimal timing of influenza vaccination in patients with human immunodeficiency virus: a Markov cohort model based on serial study participant hemoagglutination inhibition titers. Vaccine. 2014;32:677–84.
Durham MD, Buchacz Arnon, et al. Seasonal influenza vaccination rates in the HIV Outpatient Study-United States, 1999–2013. Clin Infect Dis. 2015;60:976–7.
Sullivan PS, Hanson DL, Dworkin MS, Jones JL, Ward JW. Adult and Adolescent Spectrum of HIV Disease Investigators. Effect of influenza vaccination on disease progression among HIV-infected persons. AIDS. 2000;14:2781–5.
Redd SC, Rutherford GW 3rd, Sande MA, Lifson AR, Hadley WK, Facklam RR, Spika JS. The role of human immunodeficiency virus infection in pneumococcal bacteremia in San Francisco residents. J Infect Dis. 1990;162:1012–7.
Nunes MC, von Gottberg A, de Gouveia L, et al. The impact of antiretroviral treatment on the burden of invasive pneumococcal disease in South African children: a time series analysis. AIDS. 2011;25:453–62.
Heffernan RT, Barrett NL, Gallagher KM, et al. Declining incidence of invasive Streptococcus pneumoniae infections among persons with AIDS in an era of highly active antiretroviral therapy, 1995–2000. J Infect Dis. 2005;191:2038–45.
Grau I, Pallares R, Tubau F, Spanish Pneumococcal Infection Study Network (G03/103), et al. Epidemiologic changes in bacteremic pneumococcal disease in patients with human immunodeficiency virus in the era of highly active antiretroviral therapy. Arch Intern Med. 2005;165:1533–40.
French N, Gordon SB, Mwalukomo T, et al. A trial of a 7-valent pneumococcal conjugate vaccine in HIV-infected adults. N Engl J Med. 2010;362:812–22.
Hung CC, Chen MY, Hsieh SM, Hsiao CF, Sheng WH, Chang SC. Clinical experience of the 23-valent capsular polysaccharide pneumococcal vaccination in HIV-1-infected patients receiving highly active antiretroviral therapy: a prospective observational study. Vaccine. 2004;22:2006–12.
Watera C, Nakiyingi J, Miiro G, et al. 23-Valent pneumococcal polysaccharide vaccine in HIV-infected Ugandan adults: 6-year follow-up of a clinical trial cohort. AIDS. 2004;18:1210–3.
Lesprit P, Pédrono G, Molina JM, ANRS 114-Pneumovac Study Group, et al. Immunological efficacy of a prime-boost pneumococcal vaccination in HIV-infected adults. AIDS. 2007;21:2425–34.
Sadlier C, O’Dea S, Bennett K, Dunne J, Conlon N, Bergin C. Immunological efficacy of pneumococcal vaccine strategies in HIV-infected adults: a randomized clinical trial. Sci Rep. 2016;6:32076.
Feikin DR, Elie CM, Goetz MB, et al. Randomized trial of the quantitative and functional antibody responses to a 7-valent pneumococcal conjugate vaccine and/or 23-valent polysaccharide vaccine among HIV-infected adults. Vaccine. 2001;20:545–53.
Ho YL, Brandão AP, de Cunto Brandileone MC, Lopes MH. Immunogenicity and safety of pneumococcal conjugate polysaccharide and free polysaccharide vaccines alone or combined in HIV-infected adults in Brazil. Vaccine. 2013;31:4047–53.
Glesby MJ, Watson W, Brinson C, et al. Immunogenicity and safety of 13-valent pneumococcal conjugate vaccine in HIV-infected adults previously vaccinated with pneumococcal polysaccharide vaccine. J Infect Dis. 2015;212:18–27.
Dworkin MS, Ward JW, Hanson DL, Jones JL, Kaplan JE. Pneumococcal disease among human immunodeficiency virus-infected persons: incidence, risk factors, and impact of vaccination. Clin Infect Dis. 2001;32:794–800.
Peñaranda MM, Falco V, Payeras A, et al. Effectiveness of polysaccharide pneumococcal vaccine in HIV-infected patients: a case–control study. Clin Infect Dis. 2007;45:e82–7.
Lopez-Palomo C, Martin-Zamorano M, Benitez E, et al. Pneumonia in HIV-infected patients in the HAART era: incidence, risk, and impact of the pneumococcal vaccination. J Med Virol. 2004;72:517–24.
French N, Nakiyingi J, Carpenter LM, et al. 23-valent pneumococcal polysaccharide vaccine in HIV-1-infected Ugandan adults: double-blind, randomised and placebo controlled trial. Lancet. 2000;355:2106–11.
Pedersen RH, Lohes N, Østergaard L, Søgaard OS. The effectiveness of pneumococcal polysaccharide vaccination in HIV-infected adults: a systematic review. HIV Medicine. 2011;12:323–33.
Cohen AL, Harrison LH, Farley MM, Active Bacterial Core Surveillance Team, et al. Prevention of invasive pneumococcal disease among HIV-infected adults in the era of childhood pneumococcal immunization. AIDS. 2010;24:2253–62.
Rodriguez-Barradas MC, Alexandraki I, Nazir T, et al. Response of human immunodeficiency virus-infected patients receiving highly active antiretroviral therapy to vaccination with 23-valent pneumococcal polysaccharide vaccine. Clin Infect Dis. 2003;37:438–47.
Rodriguez-Barradas MC, Serpa JA, Munjal I, et al. Quantitative and qualitative antibody responses to immunization with the pneumococcal polysaccharide vaccine in HIV-infected patients after initiation of antiretroviral treatment: results from a randomized clinical trial. J Infect Dis. 2015;211:1703–11.
Hung CC, Chang SY, Su CT, et al. A 5-year longitudinal follow-up study of serological responses to 23-valent pneumococcal polysaccharide vaccination among patients with HIV infection who received highly active antiretroviral therapy. HIV Med. 2010;11:54–63.
Tasker SA, Wallace MR, Rubins JB, Paxton WB, O’Brien J, Janoff EN. Reimmunization with 23-valent pneumococcal vaccine for patients infected with human immunodeficiency virus type 1: clinical, immunologic, and virologic responses. Clin Infect Dis. 2002;34:813–21.
Chen M, Ssali F, Mulungi M, et al. Induction of opsonophagocytic killing activity with pneumococcal conjugate vaccine in human immunodeficiency virus-infected Ugandan adults. Vaccine. 2008;26:4962–8.
Crum-Cianflone NF, Huppler Hullsiek K, Roediger M, Infectious Disease Clinical Research Program HIV Working Group, et al. A randomized clinical trial comparing revaccination with pneumococcal conjugate vaccine to polysaccharide vaccine among HIV-infected adults. J Infect Dis. 2010;202:1114–25.
Cheng A, Chang SY, Tsai MS, et al. Long-term immune responses and comparative effectiveness of one or two doses of 7-valent pneumococcal conjugate vaccine (PCV7) in HIV-positive adults in the era of combination antiretroviral therapy. J Int AIDS Soc. 2016;19:20631.
Bhorat AE, Madhi SA, Laudat F, et al. Immunogenicity and safety of the 13-valent pneumococcal conjugate vaccine in HIV-infected individuals naive to pneumococcal vaccination. AIDS. 2015;29:1345–54.
Ahmed F, Steinhoff MC, Rodriguez-Barradas MC, et al. Effect of human immunodeficiency virus type 1 infection on the antibody response to a glycoprotein conjugate pneumococcal vaccine: results from a randomized trial. J Infect Dis. 1996;173:83–90.
Hadler SC, Judson FN, O’Malley PM, et al. Outcome of hepatitis B virus infection in homosexual men and its relation to prior human immunodeficiency virus infection. J Infect Dis. 1991;163:454–9.
Chun HM, Roediger MP, Hullsiek KH, Infectious Disease Clinical Research Program HIV Working Group, et al. Hepatitis B virus coinfection negatively impacts HIV outcomes in HIV seroconverters. J Infect Dis. 2012;205:185–93.
Nikolopoulos GK, Paraskevis D, Hatzitheodorou E, et al. Impact of hepatitis B virus infection on the progression of AIDS and mortality in HIV-infected individuals: a cohort study and meta-analysis. Clin Infect Dis. 2009;48:1763–71.
Kellerman SE, Hanson DL, McNaghten AD, Fleming PL. Prevalence of chronic hepatitis B and incidence of acute hepatitis B infection in human immunodeficiency virus-infected subjects. J Infect Dis. 2003;188:571–7.
Gandhi RT, Wurcel A, Lee H, et al. Response to hepatitis B vaccine in HIV-1-positive subjects who test positive for isolated antibody to hepatitis B core antigen: implications for hepatitis B vaccine strategies. J Infect Dis. 2005;191:1435–41.
Piroth L, Launay O, Michel ML, ANRS HB EP03 CISOVAC Study Group, et al. Vaccination Against Hepatitis B Virus (HBV) in HIV-1-Infected Patients with Isolated Anti-HBV Core Antibody: the ANRS HB EP03 CISOVAC Prospective Study. J Infect Dis. 2016;213:1735–42.
Landrum ML, Huppler Hullsiek K, Ganesan A, et al. Hepatitis B vaccine responses in a large US military cohort of HIV-infected individuals: another benefit of HAART in those with preserved CD4 count. Vaccine. 2009;27:4731–8.
Bailey CL, Smith V, Sands M. Hepatitis B vaccine: a seven-year study of adherence to the immunization guidelines and efficacy in HIV-1-positive adults. Int J Infect Dis. 2008;12:e77–83.
World Health Organization. Protocol 8. Prevention of Hepatitis A, B, C and other Hepatotoxic Factors in People Living with HIV/AIDS. http://www.euro.who.int/__data/assets/pdf_file/0010/91945/E90840_Chapter_8.pdf?ua=1. Accessed June 1, 2017.
de Silva TI, Green ST, Cole J, Stone BJ, Dockrell DH, Vedio AB. Successful use of Fendrix in HIV-infected non-responders to standard hepatitis B vaccines. J Infect. 2014;68:397–9.
Powis JE, Raboud J, Ostrowski M, Loutfy MR, Kovacs C, Walmsley SL. The recombinant hepatitis B surface antigen vaccine in persons with HIV: is seroconversion sufficient for long-term protection? J Infect Dis. 2012;205:1534–8.
Irungu E, Mugo N, Ngure K, et al. Immune response to hepatitis B virus vaccination among HIV-1 infected and uninfected adults in Kenya. J Infect Dis. 2013;207:402–10.
Rock C, de Barra E, Sadlier C, et al. Impact of a new vaccine clinic on hepatitis B vaccine completion and immunological response rates in an HIV-positive cohort. J Infect Public Health. 2013;6:173–8.
van den Berg R, van Hoogstraten I, van Agtmael M. Non-responsiveness to hepatitis B vaccination in HIV seropositive patients; possible causes and solutions. AIDS Rev. 2009;11:157–64.
Kim HN, Harrington RD, Crane HM, Dhanireddy S, Dellit TH, Spach DH. Hepatitis B vaccination in HIV-infected adults: current evidence, recommendations and practical considerations. Int J STD AIDS. 2009;20:595–600.
Collier AC, Corey L, Murphy VL, Handsfield HH. Antibody to human immunodeficiency virus (HIV) and suboptimal response to hepatitis B vaccination. Ann Intern Med. 1988;109:101–5.
Paitoonpong L, Suankratay C. Immunological response to hepatitis B vaccination in patients with AIDS and virological response to highly active antiretroviral therapy. Scand J Infect Dis. 2008;40:54–8.
Pasricha N, Datta U, Chawla Y, et al. Immune responses in patients with HIV infection after vaccination with recombinant hepatitis B virus vaccine. BMC Infect Dis. 2006;6:65.
Landrum ML, Hullsiek KH, Chun HM, et al. The timing of hepatitis B virus (HBV) immunization relative to human immunodeficiency virus (HIV) diagnosis and the risk of HBV infection following HIV diagnosis. Am J Epidemiol. 2011;173:84–93.
Whitaker JA, Rouphael NG, Edupuganti S, Lai L, Mulligan MJ. Strategies to increase responsiveness to hepatitis B vaccination in adults with HIV-1. Lancet Infect Dis. 2012;12:966–76.
Okulicz JF, Mesner O, Ganesan A, et al. Hepatitis B vaccine responsiveness and clinical outcomes in HIV controllers. PLoS One. 2014;9:1–8.
Fonseca MO, Pang LW, de Paula Cavalheiro N, Barone AA, Heloisa Lopes M. Randomized trial of recombinant hepatitis B vaccine in HIV-infected adult patients comparing a standard dose to a double dose. Vaccine. 2005;23:2902–8.
Launay O, van der Vliet D, Rosenberg AR, et al. Safety and immunogenicity of 4 intramuscular double doses and 4 intradermal low doses vs standard hepatitis B vaccine regimen in adults with HIV-1: a randomized controlled trial. JAMA. 2011;305:1432–40.
Ni JD, Xiong YZ, Wang XJ, Xiu LC. Does increased hepatitis B vaccination dose lead to a better immune response in HIV-infected patients than standard dose vaccination: a meta-analysis? Int J STD AIDS. 2013;24:117–22.
Rey D, Krantz V, Partisani M, et al. Increasing the number of hepatitis B vaccine injections augments anti-HBs response rate in HIV-infected patients. Effects on HIV-1 viral load. Vaccine. 2000;18:1161–5.
de Vries-Sluijs TE, Hansen BE, van Doornum GJ, et al. A prospective open study of the efficacy of high-dose recombinant hepatitis B rechallenge vaccination in HIV-infected patients. J Infect Dis. 2008;197:292–4.
Psevdos G, Kim JH, Groce V, Sharp V. Efficacy of double-dose hepatitis B rescue vaccination in HIV-infected patients. AIDS Patient Care STDS. 2010;24:403–7.
Chatkittikunwong G. Khawcharoenporn. Hepatitis B revaccination in HIV-infected vaccine non-responders: is double dosing always necessary? Int J STD AIDS. 2016;27:850–5.
Rey D, Piroth L, Wendling MJ, ANRS HB04 B-BOOST study group, et al. Safety and immunogenicity of double-dose versus standard-dose hepatitis B revaccination in non-responding adults with HIV-1 (ANRS HB04 B-BOOST): a multicentre, open-label, randomised controlled trial. Lancet Infect Dis. 2015;15:1283–91.
Cruciani M, Mengoli C, Serpelloni G, et al. Serologic response to hepatitis B vaccine with high dose and increasing number of infections in HIV infected adult patients. Vaccine. 2009;27:17–22.
Shilaih M, Marzel A, Scherrer AU, Swiss HIV Cohort Study a.; Swiss HIV Cohort Study, et al. Dually active HIV/HBV antiretrovirals as protection against incident hepatitis B infections: potential for prophylaxis. J Infect Dis. 2016;214:599–606.
Seremba E, Ssempijja V, Kalibbala S, et al. Hepatitis B incidence and prevention with antiretroviral therapy among HIV-positive individuals in Uganda. AIDS. 2017;31:781–6.
Poovorawan Y, Chongsrisawat V, Theamboonlers A, Crasta PD, Messier M, Hardt K. Long-term anti-HBs antibody persistence following infant vaccination against hepatitis B and evaluation of anamnestic response: a 20-year follow-up study in Thailand. Hum Vaccin Immunother. 2013;9:1679–84.
Lopes VB, Hassing RJ, de Vries-Sluijs TE, et al. Long-term response rates of successful hepatitis B vaccination in HIV-infected patients. Vaccine. 2013;31:1040–4.
O’Bryan TA, Rini EA, Okulicz J, et al. HIV viraemia during hepatitis B vaccination shortens the duration of protective antibody levels. HIV Med. 2015;16:161–7.
Chaiklang K, Wipasa J, Chaiwarith R, et al. Comparison of immunogenicity and safety of four doses and four double doses vs. standard doses of hepatitis B vaccination in HIV-infected adults: a randomized, controlled trial. PLoS One. 2013;8:1–10.
Kroon FP, van Dissel JT, Labadie J, van Loon AM, van Furth R. Antibody response to diphtheria, tetanus, and poliomyelitis vaccines in relation to the number of CD4+ T lymphocytes in adults infected with human immunodeficiency virus. Clin Infect Dis. 1995;21:1197–203.
Bonetti TC, Succi RC, Weckx LY, Tavares-Lopes L, de Moraes-Pinto MI. Tetanus and diphtheria antibodies and response to a booster dose in Brazilian HIV-1-infected women. Vaccine. 2004;22:3707–12.
Rosenblatt HM, Song LY, Nachman SA, Pediatric AIDS Clinical Trials Group 377 Study Team, et al. Tetanus immunity after diphtheria, tetanus toxoids, and acellular pertussis vaccination in children with clinically stable HIV infection. J Allergy Clin Immunol. 2005;116:698–703.
Andrade RM, Andrade AF, Lazaro MA, et al. Failure of highly active antiretroviral therapy in reconstituting immune response to Clostridium tetani vaccine in aged AIDS patients. J Acquir Immune Defic Syndr. 2010;54:10–7.
de Martino M, Podda A, Galli L, et al. Acellular pertussis vaccine in children with perinatal human immunodeficiency virus-type 1 infection. Vaccine. 1997;15:1235–8.
Ida S, Tachikawa N, Nakajima A, et al. Influence of human immunodeficiency virus type 1 infection on acute hepatitis A virus infection. Clin Infect Dis. 2002;34:379–85.
Fonquernie L, Meynard JL, Charrois A, Delamare C, Meyohas MC, Frottier J. Occurrence of acute hepatitis A in patients infected with human immunodeficiency virus. Clin Infect Dis. 2001;32:297–9.
Costa-Mattioli M, Allavena C, Poirier AS, Billaudel S, Raffi F, Ferré V. Prolonged hepatitis A infection in an HIV-1 seropositive patient. J Med Virol. 2002;68:7–11.
Launay O, Grabar S, Gordien E, HEPAVAC Study Group1, et al. Immunological efficacy of a three-dose schedule of hepatitis A vaccine in HIV-infected adults: HEPAVAC study. J Acquir Immune Defic Syndr. 2008;49:272–5.
Tseng YT, Chang SY, Liu WC, et al. Comparative effectiveness of two doses versus three doses of hepatitis A vaccine in human immunodeficiency virus-infected and -uninfected men who have sex with men. Hepatology. 2013;57:1734–41.
Jimenez HR, Hallit RR, Debari VA, Slim J. Hepatitis A vaccine response in HIV-infected patients: are TWINRIX and HAVRIX interchangeable? Vaccine. 2013;31:1328–33.
Overton ET, Nurutdinova D, Sungkanuparph S, Seyfried W, Groger RK, Powderly WG. Predictors of immunity after hepatitis A vaccination in HIV-infected persons. J Viral Hepatitis. 2007;14:189–93.
Kemper CA, Haubrich R, Frank I, California Collaborative Treatment Group, et al. Safety and immunogenicity of hepatitis A vaccine in human immunodeficiency virus-infected patients: a double-blind, randomized, placebo-controlled trial. J Infect Dis. 2003;187:1327–31.
Mena G, García-Basteiro AL, Llupià A, et al. Factors associated with the immune response to hepatitis A vaccination in HIV-infected patients in the era of highly active antiretroviral therapy. Vaccine. 2013;31:3668–74.
Kourkounti S, Papaizos V, Leuow K, Kordosis T, Antoniou C. Hepatitis A vaccination and immunological parameters in HIV-infected patients. Viral Immunol. 2013;26:357–63.
Jabłonowska E, Kuydowicz J. Durability of response to vaccination against viral hepatitis A in HIV-infected patients: a 5-year observation. Int J STD AIDS. 2014;25:745–50.
Wallace MR, Brandt CJ, Earhart KC, et al. Safety and immunogenicity of an inactivated hepatitis A vaccine among HIV-infected subjects. Clin Infect Dis. 2004;39:1207–13.
Cheng A, Chang SY, Sun HY, et al. Long-term durability of responses to 2 or 3 doses of hepatitis A vaccination in HIV-positive adults on antiretroviral therapy. J Infect Dis. 2017;215:606–13.
Crum-Cianflone NF, Wilkins K, Lee AW, et al. Long-term durability of immune responses after hepatitis A vaccination among HIV-infected adults. J Infect Dis. 2011;203:1815–23.
Silverberg MJ, Lau B, Justice AC, North American AIDS Cohort Collaboration on Research and Design (NA-ACCORD) of IeDEA, et al. Risk of anal cancer in HIV-infected and HIV-uninfected individuals in North America. Clin Infect Dis. 2012;54:1026–34.
Fontenot HB, Fantasia HC, Vetters R, Zimet GD. Increasing HPV vaccination and eliminating barriers: recommendations from young men who have sex with men. Vaccine. 2016;34:6209–16.
Kahle EM, Meites E, Sineath C, et al. Sexually transmitted disease testing and uptake of human papillomavirus vaccine in a large online survey of US men who have sex with men at risk for HIV infection, 2012. Sex Transm Dis. 2017;44:63–7.
Tamalet C, Obry-Roguet V, Ressiot E, Bregigeon S, Del Grande J, Poizot-Martin I. Distribution of human papillomavirus genotypes, assessment of HPV 16 and 18 viral load and anal related lesions in HIV positive patients: a cross-sectional analysis. J Med Virol. 2014;86:419–25.
Lin A, Ong KJ, Hobbelen P, et al. Impact and cost-effectiveness of selective human papillomavirus vaccination of men who have sex with men. Clin Infect Dis. 2017;64:580–8.
Deshmukh AA, Chhatwal J, Chiao EY, Nyitray AG, Das P, Cantor SB. Long-term outcomes of adding HPV vaccine to the anal intraepithelial neoplasia treatment regimen in HIV-positive men who have sex with men. Clin Infect Dis. 2015;61:1527–35.
Levin MJ, Moscicki AB, Song LY, et al. Safety and immunogenicity of a quadrivalent human papillomavirus (types 6, 11, 16, and 18) vaccine in HIV-infected children 7 to 12 years old. J Acquir Immune Defic Syndr. 2010;55:197–204.
Wilkin T, Lee JY, Lensing SY, et al. Safety and immunogenicity of the quadrivalent human papillomavirus vaccine in HIV-1-infected men. J Infect Dis. 2010;202:1246–53.
Kahn JA, Xu J, Kapogiannis BG, Rudy B, et al. Immunogenicity and safety of the human papillomavirus 6, 11, 16, 18 vaccine in HIV-infected young women. Clin Infect Dis. 2013;57:735–44.
Kojic EM, Kang M, Cespedes MS, et al. Immunogenicity and safety of a quadrivalent human papillomavirus vaccine in HIV-1-infected women. Clin Infect Dis. 2014;59:127–35.
Denny L, Hendricks B, Gordon C, et al. Safety and immunogenicity of the HPV-16/18 AS04-adjuvanted vaccine in HIV-positive women in South Africa: a partially-blind randomised placebo-controlled study. Vaccine. 2013;31:5745–53.
Giacomet V, Penagini F, Trabattoni D, et al. Safety and immunogenicity of a quadrivalent human papillomavirus vaccine in HIV-infected and HIV-negative adolescents and young adults. Vaccine. 2014;32:5657–61.
Money DM, Moses E, Blitz S, et al. HIV viral suppression results in higher antibody responses in HIV-positive women vaccinated with the quadrivalent human papillomavirus vaccine. Vaccine. 2016;34:4799–806.
Harper DM, Franco EL, Wheeler CM, HPV Vaccine Study group, et al. Sustained efficacy up to 4.5 years of a bivalent L1 virus-like particle vaccine against human papillomavirus types 16 and 18: follow-up from a randomised control trial. Lancet. 2006;367:1247–55.
Wheeler CM, Skinner SR, Del Rosario-Raymundo MR, VIVIANE Study Group, et al. Efficacy, safety, and immunogenicity of the human papillomavirus 16/18 AS04-adjuvanted vaccine in women older than 25 years: 7-year follow-up of the phase 3, double-blind, randomised controlled VIVIANE study. Lancet Infect Dis. 2016;16:1154–68.
Toft L, Storgaard M, Muller M, et al. Comparison of the immunogenicity and reactogenicity of Cervarix and Gardasil human papillomavirus vaccines in HIV-infected adults: a randomized, double-blind clinical trial. J Infect Dis. 2014;209:1165–73.
Scheller NM, Pasternak B, Mølgaard-Nielsen D, Svanström H, Hviid A. Quadrivalent HPV vaccination and the risk of adverse pregnancy outcomes. N Engl J Med. 2017;376:1223–33.
Nitta AT, Douglas JM, Arakere G, Ebens JB. Disseminated meningococcal infection in HIV-seropositive patients. AIDS. 1993;7:87–90.
Simon MS, Weiss D, Gulick RM. Invasive meningococcal disease in men who have sex with men. Ann Intern Med. 2013;159:300–1.
Hellenbrand W, Claus H, Schink S, Marcus U, Wichmann O, Vogel U. Risk of invasive meningococcal disease in men who have sex with men: lessons learned from an outbreak in Germany, 2012–2013. PLoS One. 2016;11:e0160126.
Centers for Disease Control and Prevention (CDC). Notes from the field: serogroup C invasive meningococcal disease among men who have sex with men—New York City, 2010–2012. MMWR Morb Mortal Wkly Rep. 2013;61:1048.
Miller L, Arakaki L, Ramautar A, et al. Elevated risk for invasive meningococcal disease among persons with HIV. Ann Intern Med. 2014;160:30–7.
Simmons RD, Kirwan P, Beebeejaun K, et al. Risk of invasive meningococcal disease in children and adults with HIV in England: a population-based cohort study. BMC Med. 2015;13:297.
Cohen C, Singh E, Wu HM, Group for Enteric, Respiratory and Meningeal disease Surveillance in South Africa (GERMS-SA), et al. Increased incidence of meningococcal disease in HIV-infected individuals associated with higher case-fatality ratios in South Africa. AIDS. 2010;24:1351–60.
Bertolini DV, Costa LS, van der Heijden IM, Sato HK, Marques HH. Immunogenicity of a meningococcal serogroup C conjugate vaccine in HIV-infected children, adolescents, and young adults. Vaccine. 2012;30:5482–6.
Lujan-Zilbermann J, Warshaw MG, International Maternal Pediatric Adolescent AIDS Clinical Trials Group P1065 Protocol Team, et al. Immunogenicity and safety of 1 vs 2 doses of quadrivalent meningococcal conjugate vaccine in youth infected with human immunodeficiency virus. J Pediatr. 2012;161:676–81.
Siberry GK, Warshaw MG, Williams PL, IMPAACT P1065 Protocol Team, et al. Safety and immunogenicity of quadrivalent meningococcal conjugate vaccine in 2- to 10-year-old human immunodeficiency virus-infected children. Pediatr Infect Dis J. 2012;31:47–52.
Acknowledgements
No funding or sponsorship was received for this study or publication of this article. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
Disclosures
Nancy F. Crum-Cianflone and Eva Sullivan have nothing to disclose, and both contributed to the writing of this manuscript.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by either of the authors.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/61E8F06021EA7287.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Crum-Cianflone, N.F., Sullivan, E. Vaccinations for the HIV-Infected Adult: A Review of the Current Recommendations, Part I. Infect Dis Ther 6, 303–331 (2017). https://doi.org/10.1007/s40121-017-0166-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-017-0166-x