Abstract
The highest incidence of meningococcal disease occurs in infants younger than 1 year of age. However, in the US, prior to June 2012, there was no meningococcal vaccine licensed for use in this age group. In the US, where both serogroups C and Y contribute substantially to the overall epidemiology of invasive meningococcal disease, a vaccine combining these capsular polysaccharides was developed. We review the newly licensed HibMenCY-TT (MenHibrix™, GlaxoSmithKline Biologicals, Rixensart, Belgium), a novel vaccine containing Haemophilus influenzae type b (Hib) and serogroups C and Y Neisseria meningitidis conjugated to tetanus toxoid. We describe the vaccine, summarize the clinical trial data, and describe the patient populations recommended to receive HibMenCY-TT as their primary vaccination against Hib. Phase II and III clinical trials found HibMenCY-TT to be well tolerated, safe, and immunogenic when administered at 2, 4, 6, and 12–15 months of age for primary vaccination against both Hib and serogroups C and Y meningococcal disease. In October 2012, the Advisory Committee on Immunisation Practice in the US recommended HibMenCY-TT vaccination for infants at increased risk of meningococcal disease. HibMenCY-TT may be given concomitantly with other routine infant vaccines. It induces antibodies against Hib as well as bactericidal activity against meningococcal serogroup C and Y without increasing the number of injections required. As meningococcal disease epidemiology is dynamic, global surveillance remains essential. In the future, other countries may also benefit from the addition of HibMenCY-TT into their vaccine armamentarium against meningococcal disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neisseria meningitidis (Nm) and Haemophilus influenzae type b (Hib) are polysaccharide-encapsulated bacteria capable of rapid invasion and fulminant disease. Even with readily available and affordable therapy, meningococcal disease has a mortality rate of 8–12% and up to 20% of survivors develop permanent sequelae such as amputations, hearing loss, and neurodevelopmental disabilities [1, 2]. Even in the absence of epidemics, more than 500,000 cases of invasive meningococcal disease (IMD) occur annually worldwide of which approximately 50,000 (10%) result in death [3].
Nm is classified based on the chemical composition of the polysaccharide capsule. There are 13 antigenically distinct serogroups; A, B, C, D, E-29, H, I, K, L, W-135, X, Y, and Z, of which six; A, B, C, W-135, X, and Y, cause virtually all invasive diseases [4]. The incidence of IMD may be up to 100 per 100,000 in an epidemic season in the African meningitis belt but endemic disease incidence tends to lie between 1 to 2 per 100,000 in UK, Europe, and Australia and 0.5 to 1.5 per 100,000 in the US [5]. The relative contribution of each serogroup to all IMD is dynamic and varies both geographically and temporally [5, 6]. The majority of invasive diseases in Africa are caused by serogroup A, and in most developed countries, serogroups B and C. Over the past decade, serogroup Y has become a major contributor to IMD in the US and is steadily increasing in importance in some Nordic countries [5, 7]. Recently, there also has been a significant increase in the incidence of serogroup W-135 in both South Africa and South America, demonstrating the propensity for strain dominance to change in unpredictable ways [8, 9]. The frequency of IMD also varies by age. The highest burden of Nm is in young children, especially infants, and a second smaller peak occurs in adolescence.
The routine use of polysaccharide-protein conjugate vaccines in infant schedules has resulted in dramatic country-specific declines in disease burden and mortality caused by these encapsulated bacteria [10–12]. Hib, once the major causative organism of bacterial meningitis in children under 5 years of age, has been practically eliminated by routine use in many countries [13]. The control of IMD, however, has been more challenging.
In the late 1990s, the emergence of a hypervirulent meningococcal serogroup C (MenC) strain prompted the rapid development and licensure of a monovalent meningococcal conjugate vaccine. England and Wales were the first to introduce MenC conjugate vaccine in their National Immunization Program (as a three-dose infant schedule) and simultaneously commenced a catch-up program for all children and young adults to 18 years of age (and later 24 years of age). The program was a great success; MenC disease fell by 81% in the targeted age group (<18 years of age) [10]. The vaccine was also shown to reduce carriage [14], with subsequent herd protection against disease evidenced by a 67% decrease in attack rate among the unvaccinated population [15].
Following this success in the UK, and faced with a similarly increasing burden of serogroup C meningococcal disease, other European countries, Australia, and Canada also incorporated MenC conjugate vaccine into their National Immunization Programs with similar success [16, 17]. Today in the post-MenC era, the vast majority of ongoing Nm disease is attributed to serogroup B in these developed countries [5, 18]. In the UK, between 2006 and 2010 serogroup B accounted for 94% of Nm disease in children less than 5 years of age [5]. In Australia in 2011, 91% of Nm disease in this same age group was due to serogroup B, with no cases of serogroup C reported [18].
Similar to other regions, the highest incidence of Nm disease in the US occurs in infants younger than 12 months of age (5.38 cases per 100,000 population between 1998 and 2007) [19]. However, what differentiates the US from other countries is the extremely high contribution of serogroup Y disease to all cause IMD. Between 1998 and 2007, serogroup Y was responsible for 34.8% of all meningococcal isolates (serogroup B, 29.9%, serogroup C, 28.8% and W-135, 2.5%) [19]. An efficacious monovalent MenC conjugate vaccine would combat only one of the three most prevalent serogroups.
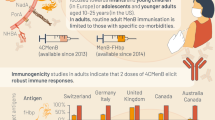
However, the past decade has seen great advances in quadrivalent meningococcal conjugate vaccines. In 2005, the first quadrivalent meningococcal conjugate vaccine, MenACWY-D (Menactra™, Sanofi Pasteur Inc., Swiftwater, PA, USA), containing Nm serogroup A, C, W-135, and Y polysaccharides individually conjugated to diphtheria toxoid, was licensed by the US Food and Drug Administration (FDA) for use in persons 11–55 years of age. License indications have since expanded, and as of April 2011 include administration as a 2-dose series in toddlers from 9–23 months of age. However, MenACWY-D is only poorly immunogenic in infancy when efficacy against MenC and Y in the US are needed most [20]. Another quadrivalent meningococcal conjugate vaccine, MenACWY-CRM197 (Menveo™, Novartis Vaccines, Cambridge, MA, USA), using C-reactive protein (a mutant of diphtheria toxoid) as the carrier protein, was licensed by the US FDA in 2010, and in January 2011 its use was expanded to include children 2–10 years of age. Phase II clinical trials of MenACWY-CRM197 vaccine in infants have demonstrated good immunogenicity in this age group following a 3-dose schedule [21]. A phase III clinical trial has recently been completed [22].
In summary, prior to June 2012, there was no vaccine licensed in the US for the prevention of meningococcal disease in infants. The combination of Nm serogroups C and Y polysaccharides together was specifically chosen for development to meet a need in the US for prevention of MenC and MenY IMD in infants and was manufactured together with Hib to obviate an additional injection at each infant vaccination [23].
The Vaccine
HibMenCY-TT is a combination of three discrete polysaccharide–protein conjugates. Each 0.5 mL dose of HibMenCY-TT contains 2.5 μg of Hib capsular polysaccharide (polyribosylribitol phosphate [PRP]) and 5 μg each of MenC and MenY polysaccharide individually conjugated or bound to tetanus toxoid. The total amount of tetanus toxoid is approximately 17.75 μg. HibMenCY-TT does not contain adjuvant or preservative. HibMenCY-TT is supplied as a single-dose vial of lyophilized vaccine to be reconstituted with the accompanying vial of saline diluent [24].
Mechanism of Action
Due to the low incidence of meningococcal disease, as for other novel meningococcal vaccines, efficacy trials of HibMenCY-TT were impractical and effectiveness was inferred based on demonstration of immunogenicity and achievement of presumed correlates of protection [25]. Serum bactericidal activity (SBA) is a functional assay that measures killing of Nm by antibodies contained in the patient’s serum in the presence of complement. The complement source may be human (hSBA) or rabbit (rSBA). For hSBA, a titer of ≥4 is the accepted correlate of protection for serogroup C based on clinical effectiveness [26]. For rSBA, a more conservative titer of ≥8 has been found to be most consistent with clinical efficacy of conjugate vaccines against serogroup C disease [25, 27]. Of note, this low bactericidal titer (with rabbit complement) does not necessarily indicate that bactericidal activity is the mechanism of immune protection (e.g., it may be a marker for an alternative mechanism such as human complement-enhanced opsonic antibody [28]). For serogroup Y, no true correlate of protection exists and the same hSBA and rSBA titers as for MenC have been accepted as surrogates of protection [27].
Due to the virtual elimination of Hib disease through routine vaccination, efficacy trials of novel Hib vaccines are not feasible. Effectiveness of the Hib polysaccharide in HibMenCY-TT was inferred based on comparative trials with other licensed Hib vaccines with non-inferiority of immunogenicity as the end-point. Based on an efficacy trial with Hib polysaccharide vaccine in Finland, it has been widely accepted that an anti-PRP antibody concentration of ≥0.15 μg/ml is adequate to confer short-term protection, and an anti-PRP concentration of ≥1.0 μg/ml is required for long-term protection (or protection for the following 12 months) [29, 30].
Clinical Trial Data
Phase II Clinical Trials
There have been six published phase II and III clinical trials investigating the safety and immunogenicity of HibMenCY-TT (Table 1) [31–37]. The initial phase II/dose-finding comparative studies were performed in between 2003 and 2004 in Australia [31] and Belgium and Germany [32]. The Australian study compared three doses of different formulations of HibMenCY-TT with licensed Hib-TT and MenC-CRM in infants at 2, 4, and 6 months of age [31]. The Belgium and German study compared three doses of different formulations of HibMenCY-TT with Hib-MenC-TT or DTap-HepB-IPV/Hib-TT and MenC-CRM [32] in infants at 2, 3, and 4 months, followed by a booster dose of HibMenCY-TT at 12–18 months. These phase II studies showed similar PRP and MenC seroprotection rates post primary [31, 32] and post fourth dose [32] and similar safety profiles after receipt of three or four doses of HibMenCY-TT compared with licensed control vaccines. Almost all infants (>97%) developed functional antibodies (rSBA titer ≥8) against MenY [31, 32]. The 2.5/5/5 μg formulation of HibMenCY-TT, was selected for further clinical development as it was the least reactogenic and was the only formulation that did not show any statistically significant difference in the proportion of infants with rSBA titer ≥128 compared with MenC-CRM controls [32].
Two phase II/safety and immunogenicity studies were performed between 2004 and 2007. A US study compared the Hib immune response after three doses of HibMenCY-TT compared with Hib-TT at 2, 4, and 6 months and compared MenCY immune responses with that of a toddler control group who received MenACWY-PS at 3–5 years of age [33]. A second phase of this study compared the immunogenicity and safety of a fourth dose of HibMenCY-TT compared with Hib-TT in a subset of infants at 12–15 months who had previously been primed with three doses of HibMenCY-TT or Hib-TT, respectively [34]. A third paper published data from these two clinical trials on the immune response to antigens administered concomitantly with HibMenCY-TT both at priming and at the fourth booster dose [35]. The US infant study showed that MenC and Y antibody responses were higher in infants vaccinated with HibMenCY-TT than in the control 3- to 5-year-old children who received a single dose of MenACWY-PS vaccine [33]. Higher antibody titers of MenC and Y were also observed post fourth dose of HibMenCY-TT as compared with a single dose of HibMenCY at 12–15 months, providing evidence of immune memory [34]. There was no immune interference to any concomitantly administered antigens with HibMenCY-TT in infancy (Streptococcus pneumoniae serotypes contained in PCV7 or diphtheria, tetanus, pertussis, hepatitis B, and poliovirus antigens contained in DTPa-HBV-IPV) or in anti-pneumococcal antibody concentrations after the fourth HibMenCY-TT dose [35].
A large phase II/safety and immunogenicity study undertaken in Australia randomized more than 1,100 participants to receive three doses of HibMenCY-TT at 2, 4, and 6 months compared with Hib-TT + MenC-CRM or Hib-TT alone [36]. At 12–15 months, a fourth dose of HibMenCY-TT was given to both the HibMenCY-TT and MenC-CRM primed children and Hib-OMP was given to the Hib-TT primed children. Post third and fourth doses of HibMenCY-TT, the safety and reactogenicity profiles were similar and MenC and Hib antibody responses were noninferior. However, at 12 months, persistence of MenC and Hib was better after priming with HibMenCY-TT compared with children primed with Hib and MenC monovalent vaccines [36]. Importantly, this study also assessed the immunogenicity after two doses of HibMenCY-TT in infancy and found rSBA titers ≥8 against MenC and Y in 94% and 83%, respectively, suggesting protection from serogroups C and Y meningococcal disease may be afforded as early as 5 months of age with this schedule. However, for all three HibMenCY antigens a 6-month dose still has immunologic value suggested by marked rises in anti-PRP GMC and MenC and Y GMTs after the third dose [36].
Phase III Clinical Trials
The phase III/pivotal clinical trial evaluated the safety, immunogenicity, and lot-to-lot consistency of HibMenCY-TT in 4,180 infants in three cohorts, across 91 centers in three countries [37]. Cohort one included only US infants for immunogenicity and safety (n = 991), cohort two included children in the US, Australia, and Mexico for safety endpoints only (n = 2,989), and cohort three, Mexican infants for immunogenicity and safety (n = 200). As there was no licensed MenC vaccine available to use as a control in this age group in the US, all infants were randomized to receive three doses of HibMenCY-TT or Hib-TT at 2, 4, and 6 months and HibMenCY-TT or Hib-OMP at 12–15 months (monovalent MenC was administered to Australian children after the study completion in accordance with their National Immunisation Program) [37].
Immunogenicity Against Nm Serogroups C and Y
The proportion of participants with hSBA titers ≥8 was 99% and 96% after the third dose and 99% after dose 4, for both MenC and MenY, respectively. MenC and Y hSBA titers increased 12-fold from pre- to post-fourth dose levels [37].
Immunogenicity Against Hib
The proportion of participants with anti-PRP antibody concentrations ≥1.0 μg/ml was noninferior (96% in the HibMenCY-TT group vs. 91% the Hib-TT group post dose 3 and 99% post dose 4 for both HibMenCY-TT and control Hib-OMP groups) [37]. As in phase II studies, PRP GMCs were significantly higher after three doses of HibMenCY-TT than Hib-TT [33, 36, 37] and also pre-dose 4 and 1 month after the fourth dose compared with after monovalent Hib vaccine [34, 36, 37]. Further, a booster response to the fourth dose of HibMenCY-TT was observed [34, 36].
Concomitant Vaccine Administration
Co-administration of HibMenCY-TT with DTPa-HBV-IPV and PVC7 at 2, 4, and 6 months did not cause immune interference to any concomitantly administered antigens [35]. Further, a pooled analysis of 1,257 toddlers found non inferiority of immune responses to measles, mumps and rubella, and varicella antigens when administered concomitantly with a fourth dose of HibMenCY-TT compared to Hib-OMP vaccine at 12–15 months of age [38].
Safety and Tolerability
Despite the addition of MenC and Y antigens, the reactogenicity of HibMenCY-TT does not differ from that associated with administration of Hib-TT vaccine [33, 36, 37]. A pooled safety analysis that included more than 8,500 participants from two primary vaccination and two-fourth dose phase III clinical trials found the incidence of serious adverse events, adverse events and solicited local and general systemic symptoms were similar following HibMenCY-TT and licensed Hib vaccines [39]. Rates of pain at the injection site and irritability were significantly lower following HibMenCY-TT than commercially available Hib vaccines [39].
Licensure, Schedule, and Recommendations for Use
On June 14, 2012, HibMenCY-TT became the first meningococcal vaccine licensed by the FDA for use in infants, age 2–8 months in the US. It was approved for use in children age 6 weeks to 18 months for the prevention of invasive Hib and serogroup C and Y meningococcal disease [24].
Recommendations for Use
Phase II and III clinical trials have found HibMenCY-TT vaccine to be well tolerated, safe, and immunogenic in infants for primary vaccination against both Hib and serogroups C and Y meningococcal disease. Routine use in the US would prevent a substantial proportion of IMD in infants without increasing the number of injections required at each vaccination visit.
However, in October 2012, rather than recommending universal Nm serogroup C and Y infant vaccination, the ACIP voted to recommend vaccination only for infants at increased risk of meningococcal disease [40]. The ACIP primarily based its recommendations on the current epidemiology of meningococcal disease in the US, which is at an historic low. The incidence of Nm in the US has been decreasing since 2000 and was only 0.21 cases per 100,000 population in 2011. Whilst young children (<5 years of age) still accounted for the highest age incidence of disease between 1993 and 2007 in the US (1.74 per 100,000 population), approximately 60% of disease in that age group was caused by serogroup B. Further, the highest incidence in children aged less than 5 years is in those in the first 6 months of life when most infants would still be too young to have received two or three doses of vaccine required for adequate protection [40]. Cost-effectiveness estimates are unfavorable. In October 2011, the CDC calculated the cost per quality-adjusted life year (QALY) averted for infant meningococcal vaccination in the US to be $3.6 million per case [41]. Accordingly, the ACIP concluded that the present low burden of disease, combined with the lack of efficacy of conjugate meningococcal vaccines against serogroup B, limits the potential impact of a routine infant meningococcal program in the US [40]. While the report did not raise the issues of programmatic implications, routine use of HibMenCY-TT would preclude many other Hib combination vaccines presently licensed for use in the infant schedule.
Recommended Schedule
HibMenCY-TT is recommended for use in infants as a 4-dose series (3 primary doses and a single booster), each 0.5 mL dose given by intramuscular injection at 2, 4, 6, and 12–15 months of age. The first dose may be given as early as 6 weeks. The fourth dose may be given as late as 18 months of age [24].
The ACIP has recommended HibMenCY-TT be used in infants at increased risk of meningococcal disease, including those with persistent complement component pathway deficiencies or functional or anatomical asplenia. Additionally, some infants with complex congenital heart disease may have asplenia and infants recognized with sickle cell disease through newborn screening warrant vaccination as they often develop functional asplenia during early childhood. HibMenCY-TT vaccination of healthy infants (6 weeks to 18 months) may also be infrequently recommended, e.g., during a community or organization outbreak of MenC or MenY disease. Finally, despite not receiving ACIP recommendation for universal use, HibMenCY-TT may still be used in the US (for those who can afford to pay) in any infant for routine vaccination against Hib and at the same time affording some protection against serogroups C and Y meningococcal disease (Table 2) [40, 42].
Children recognized in early infancy as being at increased risk for meningococcal disease should receive a four-dose series as outlined above. The ACIP recommends the following alternative schedules for use in the following circumstances [40]: If an infant at risk of meningococcal disease falls behind in their Hib vaccine doses, HibMenCY-TT may be given as per the recommended Hib catch-up schedule. If, however, the first dose of HibMenCY-TT is given after 12 months of age, two doses should be given at least 8 weeks apart to ensure adequate protection against Nm serogroups C and Y. For infants at risk of meningococcal disease who have received or are going to receive a different Hib vaccine product, they should receive MenACWY-D if they are between 9–23 months of age or MenACWY-CRM or MenACWY-D from 24 months of age.
HibMenCY-TT may be given concomitantly with other routine infant vaccines, including 7- or 13-valent pneumococcal conjugate vaccines [33, 35, 37, 40]. It may also be given concomitantly with MMR and varicella vaccine [37]. As HibMenCY-TT incudes Hib, it should not be administered concomitantly with other Hib-containing vaccines.
It is important to note that HibMenCY-TT affords no protection against serogroups A, B, or W-135 meningococcal disease. For infants traveling to the Hajj or to the ‘meningitis belt’ of sub-Saharan Africa, who need protection against MenA and MenW-135, a quadrivalent meningococcal conjugate vaccine may be offered (MenACWY-D is currently licensed for children ≥9 months of age in the US). There is currently no licensed quadrivalent meningococcal vaccine for infants under 9 months of age. Earlier this year, a non-strain specific meningococcal vaccine against serogroup B disease was licensed in Europe (Bexsero™, Novartis Vaccines, Cambridge, MA, USA) [43].
As meningococcal disease epidemiology is dynamic, global surveillance of capsular switching and serogroup replacement will remain essential. If the increase in serogroup Y disease in some European countries continues, re-evaluation of meningococcal C vaccine strategies will be necessary that may warrant expansion of coverage to include C and Y. Quadrivalent MenACWY-CRM vaccine and possibly MenACWY-TT are also likely to be available for use in infants in the future adding to choice, but at present add marginal benefit to the monovalent MenC or bivalent MenCY vaccine in most developed countries given low levels of serogroup A and W-135 disease. Ultimately, global control of IMD will require the addition of broad strain coverage serogroup B vaccines, although the effectiveness of the first of these vaccines remains to be determined.
References
Kirsch EA, Barton RP, Kitchen L, Giroir BP. Pathophysiology, treatment and outcome of meningococcemia: a review and recent experience. Pediatr Infect Dis J. 1996;15:967–78 quiz 979.
Center for Disease Control and Prevention. Meningococcal disease. The pink book: course textbook. 12th ed. Atlanta: Center for Disease Control and Prevention; 2012.
Tikhomirov E, Santamaria M, Esteves K. Meningococcal disease: public health burden and control. World Health Stat Q. 1997;50:170–7.
Rosenstein, Perkins BA, Stephens DS, Popovic T, Hughes JM. Meningococcal disease. N Engl J Med. 2001;344:1378–88.
Halperin SA, Bettinger JA, Greenwood B. The changing and dynamic epidemiology of meningococcal disease. Vaccine. 2012;30:B26–36.
Pollard AJ. Global epidemiology of meningococcal disease and vaccine efficacy. Pediatr Infect Dis J. 2004;23:S274–9.
Center for Disease Control and Prevention. ABCs Report: Neisseria meningitides. CDC, Atlanta, GA; 2009.
Efron AM, Sorhouet C, Salcedo C, Abad R, Regueira M, Vázquez JA. W135 invasive meningococcal strains spreading in South America: significant increase in incidence rate in Argentina. J Clin Microbiol. 2009;47:1979–80.
von Gottberg A, du Plessis M, Cohen C, et al. Emergence of endemic serogroup W135 meningococcal disease associated with a high mortality rate in South Africa. Clin Infect Dis. 2008;46:377–86.
Miller E, Salisbury D, Ramsay M. Planning, registration, and implementation of an immunisation campaign against meningococcal serogroup C disease in the UK: a success story. Vaccine. 2001;20:S58–67.
Whitney CG, Farley MM, Hadler J, et al. Decline in invasive pneumococcal disease after the introduction of protein-polysaccharide conjugate vaccine. N Engl J Med. 2003;348:1737–46.
Ramsay ME, McVernon J, Andrews NJ, Heath PT, Slack MP. Estimating Haemophilus influenzae type b vaccine effectiveness in England and Wales by use of the screening method. J Infect Dis. 2003;188:481–5.
World Health Organization. WHO position paper on Haemophilus influenzae type b conjugate vaccines. Wkly Epidemiol Rec. 2006;81:445–52.
Maiden MC, Stuart JM, UK Meningococcal Carraige Group. Carriage of serogroup C meningococci 1 year after meningococcal C conjugate polysaccharide vaccination. Lancet. 2002;359:1829–31.
Ramsay ME, Andrews NJ, Trotter CL, Kaczmarski EB, Miller E. Herd immunity from meningococcal serogroup C conjugate vaccination in England: database analysis. BMJ. 2003;326:365–6.
de Greeff, de Melker HE, Spanjaard L, Schouls LM, van Derende A. Protection from routine vaccination at the age of 14 months with meningococcal serogroup C conjugate vaccine in the Netherlands. Pediatr Infect Dis J. 2006;25:79–80.
Tapsall J, Australian Meningococcal Surveillance Programme. Annual report of the Australian Meningococcal Surveillance Programme, 2008. Commun Dis Intell Q Rep. 2009;33:259–67.
Lahra MM, Enriquez RP. Annual report of the Australian Meningococcal Surveillance Programme, 2011. Commun Dis Intell Q Rep. 2012;36:E251–62.
Cohn AC, MacNeil JR, Harrison LH, et al. Changes in Neisseria meningitidis disease epidemiology in the United States, 1998–2007: implications for prevention of meningococcal disease. Clin Infect Dis. 2010;50:184–91.
Rennels M, King J Jr, Ryall R, Papa T, Froeschle J. Dosage escalation, safety and immunogenicity study of four dosages of a tetravalent meninogococcal polysaccharide diphtheria toxoid conjugate vaccine in infants. Pediatr Infect Dis J. 2004;23:429–35.
Klein NP, et al. Safety and immunogenicity of a novel quadrivalent meningococcal CRM-conjugate vaccine given concomitantly with routine vaccinations in infants. Pediatr Infect Dis J. 2012;31:64–71.
Novartis Vaccines. A study to evaluate the safety and immunogenicity of 4 doses of MenACWY conjugate vaccine, administered concomitantly with routine vaccines, among infants aged 2 months. http://clinicaltrials.gov/show/NCT01000311. Last Accessed 15 May 2013.
Bryant KA, Marshall GS. Haemophilus influenzae type b-Neisseria meningitidis serogroups C and Y tetanus toxoid conjugate vaccine for infants and toddlers. Expert Rev Vaccin. 2011;10:941–50.
Food and Drug Administration. FDA Package insert for MenHibrix (Meningococcal groups C and Y and Haemophilus b tetanus toxoid conjugate vaccine). 2012; www.fda.gov/downloads/BiologicsBloodVaccines/Vaccines/ApprovedProducts/UCM308577.pdf. Last Accessed 15 May 2013.
Borrow R, Balmer R, Miller E. Meningococcal surrogates of protection—serum bactericidal antibody activity. Vaccine. 2005;23:2222–7.
Goldschneider I, Gotschlich EC, Artenstein MS. Human immunity to the meningococcus. I. The role of humoral antibodies. J Exp Med. 1969;129:1307–26.
Andrews N, Borrow R, Miller E. Validation of serological correlate of protection for meningococcal C conjugate vaccine by using efficacy estimates from postlicensure surveillance in England. Clin Diagn Lab Immunol. 2003;10:780–6.
Plotkin SA, Orenstein WA, Offit PA. Vaccines. 5th ed. Philadelphia: Elsevier, Saunders; 2008.
Käyhty H, Peltola H, Karanko V, Mäkelä PH. The protective level of serum antibodies to the capsular polysaccharide of Haemophilus influenzae type b. J Infect Dis. 1983;147:1100.
Anderson P. The protective level of serum antibodies to the capsular polysaccharide of Haemophilus influenzae type b. J Infect Dis. 1984;149:1034–5.
Nolan T, Lambert S, Roberton D, et al. A novel combined Haemophilus influenzae type b-Neisseria meningitidis serogroups C and Y-tetanus-toxoid conjugate vaccine is immunogenic and induces immune memory when co-administered with DTPa-HBV-IPV and conjugate pneumococcal vaccines in infants. Vaccine. 2007;25:8487–99.
Habermehl P, Leroux-Roels G, Sänger R, Mächler G, Boutriau D. Combined Haemophilus influenzae type b and Neisseria meningitidis serogroup C (HibMenC) or serogroup C and Y-tetanus toxoid conjugate (and HibMenCY) vaccines are well-tolerated and immunogenic when administered according to the 2, 3, 4 months schedule with a fourth dose at 12–18 months of age. Hum Vaccin. 2010;6:640–51.
Marchant CD, et al. Randomized trial to assess immunogenicity and safety of Haemophilus influenzae type b and Neisseria meningitidis serogroups C and Y-tetanus toxoid conjugate vaccine in infants. Pediatr Infect Dis J. 2010;29(1):48–52.
Marshall GS, et al. Immune response and one-year antibody persistence after a fourth dose of a novel Haemophilus influenzae type b and Neisseria meningitidis serogroups C and Y-tetanus toxoid conjugate vaccine (HibMenCY) at 12 to 15 months of age. Pediatr Infect Dis J. 2010;29(5):469–71.
Marshall GS, Marchant CD, Blatter M, Friedland LR, Aris E, Miller JM. Co-administration of a novel Haemophilus influenzae type b and Neisseria meningitidis serogroups C and Y-tetanus toxoid conjugate vaccine does not interfere with the immune response to antigens contained in infant vaccines routinely used in the United States. Hum Vaccin. 2011;7:258–64.
Nolan T, Richmond P, Marshall H, et al. Immunogenicity and safety of an investigational combined Haemophilus influenzae type B-Neisseria meningitidis serogroups C and Y-tetanus toxoid conjugate vaccine. Pediatr Infect Dis J. 2011;30:190–6.
Bryant KA, Marshall GS, Marchant CD, et al. Immunogenicity and safety of H influenzae type b-N meningitidis C/Y conjugate vaccine in infants. Pediatrics. 2011;127:e1375–85.
Bryant K, McVernon J, Marchant C, et al. Immunogenicity and safety of measles-mumps-rubella and varicella vaccines coadministered with a fourth dose of Haemophilus influenzae type b and Neisseria meningitidis serogroups C and Y-tetanus toxoid conjugate vaccine in toddlers: a pooled analysis of randomized trials. Hum Vaccin Immunother. 2012;8:1036–41.
Rinderknecht S, Bryant K, Nolan T, et al. The safety profile of Haemophilus influenzae type b-Neisseria meningitidis serogroups C and Y tetanus toxoid conjugate vaccine (HibMenCY). Hum Vaccin Immunother. 2012;8:304–11.
Infant meningococcal vaccination. Advisory Committee on Immunization Practices (ACIP) recommendations and rationale. MMWR Morb Mortal Wkly Rep. 2013;62:52–4.
Pichichero M. Infant meningococcal vaccine: why not? www.pediatricnews.com/index.php?id=7989&type=98&tx_ttnews%5Btt_news%5D=137807&cHash=da03e20e36. Last Accessed 15 May 2013.
Center for Disease Control and Prevention. Advisory Committee on Immunization Practices. Vaccines for children program. Vaccines to prevent meningococcal disease. 2012. www.cdc.gov/vaccines/programs/vfc/downloads/resolutions/1012-2-mening-mcv.pdf. Last Accessed 15 May 2013.
Novartis. Novartis receives EU approval for Bexsero®, first vaccine to prevent the leading cause of life-threatening meningitis across Europe. http://www.novartis.com/newsroom/media-releases/en/2013/1672036.shtml. Last Accessed 15 May 2013.
Acknowledgments
Dr. K. Perrett received funding from an Australian National Health and Medical Research Council (NHMRC) research fellowship. Dr. K. Perrett is the guarantor for this article and takes responsibility for the integrity of the work as a whole.
Conflict of Interest
Dr T. Nolan’s institution (MCRI) has received research grants from GSK, Novartis, CSL, Pfizer, and Sanofi Pasteur. He has received past payment for a role (now completed) as a member of the independent data and safety monitoring board for GSK Vaccine’s HPV vaccine. He chairs the Australian Government’s Technical Advisory Group on Immunisation (ATAGI) and is a member of the World Health Organisation Strategic Advisory Group of Experts (SAGE) on Immunization. Dr J. McVernon has been an investigator on vaccine and epidemiological studies sponsored by a range of vaccine manufacturers and in this role has received support for conference attendance, presentation of data, and membership of vaccine advisory boards. She is currently a member of the Australian Technical Advisory Group on Immunisation. Dr. K. Perrett has received support from Novartis for conference attendance and presentation of data and honoraria from Pfizer for educational lectures.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Perrett, K.P., Nolan, T.M. & McVernon, J. A Licensed Combined Haemophilus influenzae Type b-Serogroups C and Y Meningococcal Conjugate Vaccine. Infect Dis Ther 2, 1–13 (2013). https://doi.org/10.1007/s40121-013-0007-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-013-0007-5