Abstract
With the increase in the number of cases of autoimmune encephalitis (AE), the cerebrospinal fluid (CSF) of people living with HIV (PLWH) showing abnormal behavior, cognitive impairment or abnormal movements should be actively screened for the antibody panel of AE. Early recognition and treatment can prevent severe seizures or coma and markedly improve the prognosis of patients. The first-line immunotherapy for AE includes intravenous methylprednisolone and immunoglobulin. However, whether long-time immunosuppressive maintenance therapy is needed is debated. For PLWH, immunosuppressive therapy and even steroids could be more challenging. Here, we review and summarize the clinical characteristics often reported cases and report one case from our center to improve the diagnosis and treatment of anti-N-methyl-d-aspartate receptor encephalitis in PLWH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
For people living with HIV (PLWH) with abnormal mental behavior, cognitive or motor disorders, the antibody spectrum of autoimmune encephalitis in cerebrospinal fluid (CSF) should be actively screened for early diagnosis |
Cytokine storm in CSF may be related to anti-NMDA receptor encephalitis |
Dynamic monitoring of CSF cytokines helps guide immunotherapy and evaluate treatment efficacy |
Introduction
Encephalitis is a serious inflammatory disease of the brain that can have infectious or autoimmune etiology. The most common causes of encephalitis are infectious factors [1]. The number of cases of autoimmune encephalitis has been gradually increasing in recent years [2, 3]. Approximately 21% of encephalitis cases in Northern Europe were autoimmune in etiology, and the most common disease was anti-N-methyl-d-aspartate receptor (anti-NMDAR) encephalitis. Furthermore, the disability and mortality rates were higher in patients with an impaired immune system [4]. Anti-NMDAR encephalitis is an acute and subacute brain inflammation thought to be caused by anti-NMDAR [1]. For people living with HIV (PLWH), the interaction and complexity between HIV infection and autoimmune disease are still unclear. Infection with herpes simplex virus (HSV) and other neurogenic viruses have been reported to be the potential triggers of anti-NMDAR encephalitis [5,6,7]. However, whether the HIV is associated with the anti-NMDAR encephalitis and specific underlying pathogenic mechanisms remain unknown. Compared to the general population, the clinical symptoms of anti-NMDAR encephalitis in PLWH are more complex, including abnormal behavior, cognitive impairment and abnormal movements, seizures and even coma [8]. Furthermore, without early treatment, prognosis is poor. Early recognition and treatment can reduce the risk of patients progressing to seizures or coma and markedly improve patient prognosis.
Treatment of anti-NMDAR encephalitis in PLWH is more complex. It is necessary to ensure effective control of HIV replication and the progression of anti-NMDAR encephalitis. Attention also needs to be paid to the drug interaction in the treatment plan to avoid serious adverse drug reactions. First-line immunotherapy for the disease includes intravenous methylprednisolone, intravenous immunoglobulin (IVIG) and plasma exchange (PE) [9]. If the first-line treatment is ineffective, the second-line treatment mainly includes rituximab and mycophenolate- mofetil [10]. However, whether long-time immunosuppressive maintenance therapy is needed is debated. For PLWH, immunosuppressive therapy and even steroids could be more challenging. Therefore, we review and summarize the clinical characteristics of ten reported cases and report one case from our center to improve the diagnosis and treatment of anti-NMDAR encephalitis in PLWH. We believe our findings may serve as a reference for clinical practice.
Case Presentation
A 27-year-old man with HIV infection presented with fever, headache and progressive neuropsychiatric symptoms, including inattention, decreased consciousness, slow reaction, abnormal movements, change of sleep time, abnormal shoulder movements, and fatigue. He was treated with antiretroviral therapy (ART) (tenofovir + lamivudine + efavirenz) for 5 years with undetectable viral load and no AIDS-defining disease. The patient had a history of persistent diarrhea 3 weeks before onset. He had no other past medical history and no history of mental illness or medicine abuse.
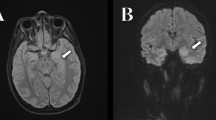
On admission, his body temperature reached a maximum of 39 °C while his vital signs were stable. Physical examination revealed impaired attention, involuntary twitching of the mouth and face, abnormal shoulder movements and myoclonus of both lower limbs. HIV RNA was not detected in plasma, and CD+ 4 T cell count was 694/ul. The blood cell count, liver and kidney function, and thyroid function test results were normal. Bacteria, fungi, mycoplasma and viruses also tested negative. A lumbar puncture was then performed, and the intracranial pressure was 350 mmH20. Cerebrospinal fluid (CSF) analysis showed increased nucleated cells (87 × 106/l) and raised inflammatory cytokines (Table 1). Unbiased metagenomic next-generation sequencing was performed to detect occult pathogens from the CSF sample, and no evidence of pathogen infection was found. This included PCR testing for HSV-1, HSV-2, Epstein-Barr virus (EBV), varicella-zoster virus (VZV), John Cunningham virus, cytomegalovirus, enterovirus, parechovirus and human herpes viruses (HHV6), cryptococcal antigen, mycobacterium culture, nucleic acid amplifcation test (GeneXpert) and bacterial culture. The results of these tests were negative. Electroencephalogram (EEG) was slightly abnormal without epileptiform changes. Cerebral magnetic resonance imaging (MRI) revealed an abnormal signal in the left frontal cortex on T2-weighted fluid-attenuated inversion recovery (FLAIR) image (Figure S1). Luckily, the presence of NMDAR antibodies was identified in the CSF, whereas absence of other antibodies commonly linked to autoimmune encephalitis was observed (Fig. 1). No evidence of tumor was detected by ultrasound and computed tomography examination in the subject. In terms of differential diagnosis, brain tissue biopsy is the gold standard for the diagnosis of CD8 encephalitis, but due to its invasiveness and risks, it is usually only considered when other non-invasive tests cannot confirm the diagnosis. In addition, cognitive dysfunction caused by efavirenz appears earlier or persists, and patient symptoms may improve after discontinuing the drug or reducing the dosage. However, the patient had been using antiviral therapy for 5 years and HIV virus was well controlled. The patient's symptoms improved after receiving hormone combined immunotherapy. Therefore, the patient was diagnosed with autoimmune encephalitis.
Anti-N-methyl-d-aspartate receptor as an antigen of patient CSF autoantibodies: confirmation by a cell-based assay that HEK-293 cells were transfected with the pCMV6-XL5-AK5 plasmid for transient overexpression. Fixed and permeabilized cells were then immunostained with the patient’s CSF and a commercial anti-NMDAR antibody, respectively. Total colocalization between CSF and anti-NMDAR staining was observed. Scale bar = 10 µm
A simplified diagnosis and treatment schema for the patient is shown in Fig. 2. The patient was treated with 5 days of intravenous methylprednisolone (1.5 mg/kg/day) and intravenous immunoglobulin (0.4 g/kg/day) followed by a tapering regimen of methylprednisolone (initial amount 40 mg daily) for 6 months. After 5 days, the patient started to show clinical improvement, and CSF examination revealed a significant decrease in nucleated cells and inflammatory cytokines. There were no headaches or fever, and no abnormal movements after 28 days. With apparent remission according to neuroimaging and CSF analysis, the patient was discharged and received regular follow-ups. During the follow-up period, the CSF examination was done several times to assess cytokine levels to facilitate medication adjustments (Table 1). The patient was stable with no recurrence after 1 year of follow-up.
Informed consent was obtained from the patient for publication of this case report. This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. This study was approved by the Institutional Review Committee of the First Affiliated Hospital of Zhejiang University School of Medicine (no. IIT20220194B-RI).
Discussion
Currently, the publicly reported incidence rate of HIV-positive anti-NMDAR encephalitis is low and misdiagnosis or delayed diagnosis of the condition is common in clinical practice. We reviewed ten previously reported cases [2, 3, 5, 11,12,13,14] and one case from our center and summarized the clinical characteristics of the disease (Table 2).
Anti-NMDAR encephalitis mostly occurs in children and young women. The search for an underlying tumor, particularly ovarian teratoma in women or testicular germ-cell tumor in men, is of paramount importance in the context of an anti-NMDAR encephalitis [3]. Most patients have prodromal symptoms, such as headache, fever and flu-like symptoms. Children often show behavioral abnormalities and abnormal movement, while adults have mental symptoms and seizures. Approximately 35% of patients have brain MRI abnormalities [8]. A literature review showed that among PLWH, anti-NMDAR encephalitis developed mainly in young and middle-aged men (7/10), and no tumors were found (10/10). PLWH may exhibit more complex and severe clinical manifestations due to the coexistence of HIV infection and other opportunistic infections. The most common clinical manifestations of the disease were abnormal behavior and movement disorders. MRI abnormalities were more common (9/10), and EEG abnormalities were rare. A young male patient in our center presented with behavioral abnormalities and autonomic dysfunction. Ultrasound and CT of the body showed no tumors in our patient. An abnormal signal was detected on T2-weighted FLAIR MRI, and EEG showed a slight abnormality without epileptiform changes.
An early study showed that the sensitivity and specificity of antibody detection in the CSF of patients with anti-NMDAR encephalitis were very high, while false-positive or -negative results could be observed in the serum. Approximately 14% of patients with anti-NMDAR encephalitis had antibodies in the CSF but none in the serum [8, 15]. Therefore, it is important to actively screen for the antibody panel of autoimmune encephalitis in cerebrospinal fluid for the diagnosis of anti-NMDAR encephalitis.
Previously, HSV and other neurotropic viruses were thought to be potential triggers of anti-NMDAR encephalitis [7, 8]. It was hypothesized that HSV-induced inflammation and destruction may expose neuronal antigens, thereby triggering humoral autoimmunity. However, the relationships between HIV and autoimmune encephalitis remain poorly defined. Prior reports suggest that HIV may contribute to the generation of NMDAR antibodies. Review of ten prior cases showed that 50% of these patients have high CSF HIV viral loads. It was found that NMDAR was activated by HIV-1 envelope glycoprotein 120 (gp120), which led to neuronal damage after damage to the blood-brain barrier [16]. In addition, increased phosphorylation of NMDAR receptor subunits was detected in human brain tissues with HIV encephalitis infection [17], which could be attributed to HIV Tat protein. All these findings indicate that HIV infection may trigger anti-NMDAR encephalitis; however, the specific mechanism remains to be elucidated. Additionally, the case in our center suggests anti-NMDAR encephalitis occurs despite well-controlled HIV in CSF and plasma, in line with previous studies [2, 13] implying that other factors besides HIV infection are involved in the development of anti-NMDAR encephalitis. Furthermore, because of the patient's history of persistent diarrhea 3 weeks before onset in our center, herpes virus infection could not be ruled out, which then led to an immune response disorder to the opportunistic pathogen. It was observed in our case that white blood cell counts and levels of TNF-α, IL-6, IL-8, and other cytokines in the CSF significantly increased, indicating a potential role of inflammatory cytokine storms in the development of anti-NMDAR encephalitis, which is supported by studies done elsewhere [18].
Once diagnosed, the extraordinary complexity of anti-NMDAR encephalitis therapy remains a major challenge. It is necessary to ensure effective control of HIV replication and the progression of anti-NMDAR encephalitis. Literature review found that 6/10 patients adjusted the ART regimen during hospitalization. Among them, four subjects had low viral load in serum but high viral load in CSF. To reduce the viral load in CSF, they switched to an ART regimen with increased central nervous system (CNS) penetration; the ART regimen was adjusted in another patient because of poor control of HIV in serum and cerebrospinal fluid. The last patient switched his ART regimen but detailed information was not given.
First-line immunotherapy for the condition includes intravenous methylprednisolone and IVIG or plasma exchange [9]. To reduce the risk of intracranial inflammatory reaction and recurrence, a corticosteroid was recommended for maintenance therapy.
Because of their impaired immune status, the patients' treatment response and prognosis for anti-NMDAR encephalitis in PLWH may differ from those of the general population, requiring extra caution during treatment. For PLWH, a long course of high-dose corticosteroid therapy could further inhibit impaired immunity, increasing the risk of opportunistic infections and complexity of the condition [19].
In our case, during maintenance therapy, the amounts of corticosteroid were adjusted in time according to the levels of cytokines IL-6, IL-8, and TNF-α. After 2 months, there were no behavioral abnormalities. Additionally, intracranial pressure and levels of inflammatory cytokine decreased, the nucleated cell count normalized and anti-NMDAR antibody levels in CSF became negative again. Therefore, considering the predictive role of cytokines in the CSF, it was recommended that cytokine levels in the CSF should be checked periodically to guide immunotherapy and assess efficacy.
Conclusion
Anti-NMDAR encephalitis in PLWH can be easily confused with mental diseases, leading to incorrect or delayed diagnoses. It is associated with a high disability rate and seriously affects the quality of life. Therefore, it is necessary to actively screen the antibody panel of autoimmune encephalitis in the CSF for an early diagnosis. In addition, dynamic monitoring of CSF cytokines helps guide immunotherapy and evaluate treatment efficacy.
Data Availability
All data generated or analyzed during this study are included in this published article and supplementary information files.
References
Graus F, Titulaer MJ, Balu R, Benseler S, Bien CG, Cellucci T, et al. A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol. 2016;15(4):391–404.
Patarata E, Bernardino V, Martins A, Pereira R, Loureiro C, Moraes-Fontes MF. Anti-N-methyl-d-aspartate receptor encephalitis in HIV infection. Case Rep Neurol. 2016;8(3):251–7.
Haneche F, Demeret S, Psimaras D, Katlama C, Pourcher V. An anti-NMDA receptor encephalitis mimicking an HIV encephalitis. Clin Immunol (Orlando, FLA). 2018;193:10–1.
Granerod J, Ambrose HE, Davies NW, Clewley JP, Walsh AL, Morgan D, et al. Causes of encephalitis and differences in their clinical presentations in England: a multicentre, population-based prospective study. Lancet Infect Dis. 2010;10(12):835–44.
Moloney PB, Hutchinson S, Heskin J, Mulcahy F, Langan Y, Conlon NP, et al. Possible N-methyl-d-aspartate receptor antibody-mediated encephalitis in the setting of HIV cerebrospinal fluid escape. J Neurol. 2020;267(5):1348–52.
Schäbitz WR, Rogalewski A, Hagemeister C, Bien CG. VZV brainstem encephalitis triggers NMDA receptor immunoreaction. Neurology. 2014;83(24):2309–11.
Ioannidis P, Papadopoulos G, Koufou E, Parissis D, Karacostas D. Anti-NMDA receptor encephalitis possibly triggered by measles virus. Acta Neurol Belg. 2015;115(4):801–2.
Dutra LA, Abrantes F, Toso FF, Pedroso JL, Barsottini OGP, Hoftberger R. Autoimmune encephalitis: a review of diagnosis and treatment. Arq Neuropsiquiatr. 2018;76(1):41–9.
Nosadini M, Eyre M, Molteni E, Thomas T, Irani SR, Dalmau J, et al. Use and safety of immunotherapeutic management of N-methyl-d-aspartate receptor antibody encephalitis: a meta-analysis. JAMA Neurol. 2021;78(11):1333–44.
Chinese Society of Neuroinfectious Diseases and Cerebrospinal Fluid Cytology. Chinese expert consensus on the diagnosis and management of autoimmune encephalitis (2022 edition). Chin J Neurol. 2022;55(9):931–49.
Arboleya S, Clemente A, Deng S, Bedmar M, Salvador I, Herbera P, et al. Anti-NMDAR antibodies in new-onset psychosis. Positive results in an HIV-infected patient. Brain Behav Immunity. 2016;56:56–60.
Anguizola-Tamayo D, Bocos-Portillo J, Pardina-Vilella L, Rodriguez-Sainz A, Vicente-Olabarria I, Martínez E, et al. Psychosis of dual origin in HIV infection: viral escape syndrome and autoimmune encephalitis. Neurol Clin Pract. 2019;9(2):178–80.
Pinzon-Charry A, Wallace G, Clark JE, Nourse C. Anti-NMDA-receptor encephalitis in an adolescent with HIV infection and review of the literature. Pediatr Infect Dis J. 2019;38(8):e169–71.
Cunill V, Arboleya S, Jiménez ML, Campins A, Herbera P, Mestre L, et al. Neuronal surface antibodies in HIV-infected patients with isolated psychosis. J Neuroimmunol. 2016;301:49–52.
Gresa-Arribas N, Titulaer MJ, Torrents A, Aguilar E, McCracken L, Leypoldt F, et al. Antibody titres at diagnosis and during follow-up of anti-NMDA receptor encephalitis: a retrospective study. Lancet Neurol. 2014;13(2):167–77.
Louboutin JP, Strayer DS. Blood-brain barrier abnormalities caused by HIV-1 gp120: mechanistic and therapeutic implications. Sci World J. 2012;2012: 482575.
King JE, Eugenin EA, Hazleton JE, Morgello S, Berman JW. Mechanisms of HIV-tat-induced phosphorylation of N-methyl-d-aspartate receptor subunit 2A in human primary neurons: implications for neuroAIDS pathogenesis. Am J Pathol. 2010;176(6):2819–30.
Byun JI, Lee ST, Moon J, Jung KH, Sunwoo JS, Lim JA, et al. Distinct intrathecal interleukin-17/interleukin-6 activation in anti-N-methyl-d-aspartate receptor encephalitis. J Neuroimmunol. 2016;297:141–7.
Damba JJ, Laskine M, Peet MM, Jin Y, Sinyavskaya L, Durand M. Corticosteroids use and incidence of severe infections in people living with HIV compared to a matched population. J Int Assoc Prov AIDS Care. 2022;21:23259582221107196.
Medical Writing and Editorial Assistance
The authors did not use any medical writing or editorial assistance for this article.
Funding
Sponsorship for this study and Rapid Service Fee were funded by the project of NINGBO Leading Medical & Health Discipline, Project Number: 2022-x05.
Author information
Authors and Affiliations
Contributions
Jiangjin Hui wrote the manuscript; Jinhua Wang and Zhikai Wan collected the basic information of the patients and edited the manuscirpt; Qing Cao, Bohao Dai and Haiyan Lou were responsible for imaging data and processing; Biao Zhu reviewed and edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Jiangjin Hui, Qing Cao, Zhikai Wan, Bohao Dai, Haiyan Lou and Biao Zhu have no relevant financial or non-financial interests to disclose.
Ethical Approval
Informed consent was obtained from the patient for publication of this case report. This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. This study was approved by the Institutional Review Committee of the First Affiliated Hospital of Zhejiang University School of Medicine (no. IIT20220194B-RI).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Hui, J., Wang, J., Wan, Z. et al. Anti-N-methyl-d-aspartate Receptor Encephalitis in People Living with HIV: Case Report and Literature Review. Neurol Ther 13, 907–916 (2024). https://doi.org/10.1007/s40120-024-00594-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40120-024-00594-w