Abstract
Introduction
The characteristics of patients across different sleep clinics may vary because they selectively visit specific specialists on the basis of their primary symptoms. This study aimed to compare the clinical and polysomnography (PSG) features of patients with suspected obstructive sleep apnea (OSA) at three sleep specialty clinics (otolaryngology [ENT], neurology [NR], and psychiatry [PSY]).
Methods
We retrospectively analyzed the medical records and PSG reports of adult patients who underwent full-night PSG between January 2022 and June 2023 at a tertiary medical center. The demographic, questionnaire, and PSG variables were compared.
Results
Of the 407 patients, 83.0% exhibited sleep-disordered breathing (apnea–hypopnea index ≥ 5) with varying severity among the specialty pathways. Patients in the ENT group (n = 231) were the youngest and had the shortest sleep latency and most severe OSA markers with the highest positive airway pressure (PAP) acceptance, while those in the NR group (n = 79) had similar OSA-related PSG parameters to those in the ENT group but were older and had more OSA-related comorbidities, although their PAP acceptance was relatively low. The PSY group (n = 97) included a significant proportion of patients with normal or mild OSA, a female majority, high levels of depression, and subjective sleep distress.
Conclusion
Our results highlight the multidisciplinary aspects of sleep medicine and diverse patients, and specialist needs for diagnosing sleep disorders and PAP acceptance. Exploring the potential differences in prognosis and treatment responses across various sleep specialty clinics would facilitate the development of personalized strategies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
South Korea has faced a surge in the demand for sleep-related evaluations in recent years; however, comprehensive research and real-world practice on the patterns of polysomnography (PSG) utilization, which is the gold standard for diagnosing obstructive sleep apnea (OSA), are lacking. |
We hypothesized that patient demographics and PSG characteristics would vary depending on the sleep clinic they visited and aimed to characterize these differences. |
Significant differences were observed in the severity of OSA, PAP acceptance, incidence of comorbidities, mood disorders, and sleepiness among patients from different sleep specialty clinics. |
Patients undergoing sleep studies can have significantly different characteristics depending on the clinical pathway and primary symptoms that require a sleep study. |
Patient differences should be considered in the diagnosis and treatment of OSA. |
Introduction
A spectrum of sleep disorders, including sleep apnea, insomnia, parasomnia, hypersomnia, and sleep-related movement disorders, lead to the referral of patients to sleep clinics via various pathways, including otolaryngologists, pulmonologists, neuropsychiatrists, neurologists, pediatricians, and dentists. Moreover, professionals have differing expertise and practices, and are influenced by their specific sleep medicine training and experience. Moreover, sleep-related symptoms, such as frequent awakening during sleep, non-restorative sleep, and impaired daytime functioning, are common and may overlap in different sleep disorders. Therefore, increasing the diagnostic accuracy of sleep studies is of the utmost importance to ensure optimal patient management. Polysomnography (PSG) is the gold standard for diagnosing obstructive sleep apnea (OSA) and can be used to evaluate other sleep disorders, including rapid eye movement (REM) behavior disorders and periodic limb movements during sleep (PLMS) in adults [1]. Although a routine diagnosis of primary insomnia is not required, PSG may be considered upon clinical suspicion of another sleep disorder to identify a treatable cause.
Since the expansion of National Health Insurance (NHI) service coverage for suspected OSA in South Korea in July 2018, the demand for sleep-related evaluations over the past few years has surged considerably [2]. NHI coverage for PSG and PAP (positive airway pressure) therapy was introduced on the basis of a shift in public health authorities’ perception of OSA, driven by the understanding that sleep apnea, a recognized risk factor for chronic conditions such as cardiovascular diseases and hypertension, not only affects individual patients but also imposes a significant long-term financial burden on medical insurance due to the development of these chronic conditions. Accordingly, the accessibility to diagnose sleep disorders through PSG has quickly improved across various departments specializing in sleep disorders.
The South Korean NHI covers PSG for patients exhibiting symptoms of suspected OSA, along with associated comorbidities, adhering to the similar clinical symptom criteria outlined in the third edition of the International Classification of Sleep Disorders [3]. However, comprehensive research and real-world practice on PSG utilization patterns in South Korea remain lacking.
To elucidate patterns of PSG utilization, we compared and characterized a patient population requesting in-laboratory full-night PSG studies at three distinct sleep specialty clinics: otolaryngology (ENT), neurology (NR), and psychiatry (PSY). In this study, we hypothesized that there are fundamental differences among patients with suspected OSA who underwent PSG at different sleep clinics within a single tertiary center.
Methods
Study Population
This retrospective study was conducted at a single tertiary center in Ulsan Metropolitan City. Patients who underwent sleep laboratory tests for suspected OSA between January 2022 and June 2023 were included. To meet the criteria for insurance coverage for suspected OSA in South Korea, individuals must satisfy either conditions A plus B or A plus C:
-
(A)
Presence of one or more symptoms such as daytime sleepiness, habitual snoring, sleep apnea, non-restorative sleep, choking during sleep, restless sleep, or frequent awakening during sleep.
-
(B)
Positive findings on physical examination, including a modified Mallampati score greater than grade 3, Friedman staging tonsil size greater than grade 2–3 (grade 3 for those ≤ 13 years old and grade 2 for those > 13 years old), or observation of upper airway obstruction during the Müller maneuver.
-
(C)
Presence of hypertension, heart disease, cerebrovascular disease, diabetes mellitus, or a body mass index (BMI) equal to or greater than 30 kg/m2.
The exclusion criteria included patients aged < 18 years; those with a total sleep time < 120 min; cases involving postsurgical PSG; those who underwent a multiple sleep latency test (MSLT)-paired PSG for suspected hypersomnia; and cases from departments other than the ENT, NR, or PSY clinics. This study was approved by the Institutional Review Board of Ulsan University Hospital (IRB No. 2023-10-014), and the procedures followed were in accordance with the principles of the 1964 Helsinki Declaration and its later amendments. The requirement for informed consent was waived because of the retrospective nature of the study, and patient identities were maintained anonymously.
PSG Preparation and Collection of Sleep-Related Information
PSG preparations involved standard patient instructions. Psychiatric medication was maintained if previously prescribed, and zolpidem 6.25 mg was administered to patients experiencing difficulty sleeping to minimize interference with sleep architecture and muscle tone. The patients refrained from napping during the day and were advised against consuming heavy meals. A standardized questionnaire was completed to record their sleep schedule, daytime sleepiness, symptoms such as snoring, witnessed apnea, insomnia, demographic data, BMI, comorbidities (diabetes mellitus, hypertension, cardiovascular or cerebrovascular diseases such as coronary heart disease, heart failure, arrhythmia, and stroke), and psychiatric comorbidities. Structured questionnaires related to sleep quality, daytime sleepiness, and emotional state, including the Epworth Sleepiness Scale (ESS), Pittsburgh Sleep Quality Index (PSQI), and Beck Depression Inventory (BDI-II), were administered. The ESS is an eight-item questionnaire that assesses the extent of subjective daytime sleepiness; a cutoff of ≥ 11 points indicates excessive daytime sleepiness, whereas a score ≤ 5 points indicates lower normal daytime sleepiness. The PSQI is a widely used short self-report questionnaire for measuring subjective sleep quality and disturbances, with higher scores representing worse sleep quality. BDI-II is scored from 0 to 63, with a higher score indicating a more depressed mood. Inaccurate self-reported checklist data were cross-verified using electronic medical charts.
Full-Night in-Laboratory PSG and Diagnosis of OSA
This study solely included patients who underwent in-laboratory PSG, as reimbursement excludes home sleep apnea testing. Full-night PSG was conducted using the Xltek® Brain Monitor with Natus® SleepWorks™ Middleton, USA, PSG software at the Ulsan University Hospital Sleep Lab Unit. All data were uniformly analyzed by a central team, ensuring consistency across all clinics. This team comprised two experienced and skilled technicians along with the sole supervising physician, Dr. Eunmi Lee. Certified as a polysomnography instructor with sleep fellowship experience, Dr. Lee provided training and ensured the accuracy of the final readings and interpretation. The following measures were obtained during the sleep study: electroencephalography, electrooculography, electromyography (submental and bilateral anterior tibialis muscles), electrocardiography, nasal and oral airflow (nasal airflow pressure sensor, nasal and oral airflow thermal sensor), chest and abdominal respiratory muscle effort (impedance belts), oxygen saturation measured with pulse oximetry (SpO2), snoring volume (tracheal microphone), and sleep position (body position sensors). The American Academy of Sleep Medicine (AASM) v2.6 guidelines were followed for PSG interpretation [4]. Apnea was defined as the absence of airflow for ≥ 10 s and classified as obstructive, mixed, or central. Hypopnea was defined as a > 30% decrease in airflow lasting at least 10 s and associated with ≥ 3% SpO2 desaturation or arousal. Respiratory effort-related arousal (RERA) was defined as arousal from sleep that did not technically meet the definition of apnea or hypopnea without apnea or hypopnea. The apnea–hypopnea index (AHI) was calculated as the number of apneas and hypopneas per hour of sleep, and the respiratory disturbance index (RDI) was calculated as the number of respiratory events (AHI + RERA). The oxygen desaturation index (ODI) obtained from the PSG was defined as the frequency of oxygen saturation decrease by ≥ 3%/h during sleep. Sleep apnea was defined as AHI ≥ 5/h. OSA severity was categorized on the basis of AHI into normal (AHI < 5), mild (AHI 5–15), moderate (AHI 15–30), and severe (AHI ≥ 30). The presence of PLMS was defined as the number of leg movements per hour (periodic leg movement index [PLMI] ≥ 15).
The following PSG variables were measured and categorized into five domains based on a previous study [5]: (1) sleep structure parameters of total sleep time (TST, min), sleep latency (SL, min), sleep efficacy (SE, %), rapid eye movement (REM) latency (min), waking after sleep onset (WASO, min), and sleep-stage percentages (stages N1, N2, N3, and R); (2) OSA frequency metrics of AHI and RDI; (3) hypoxemic parameters of ODI, minimum oxygen saturation (minO2), and percentage of sleep time (%) spent with oxygen saturation below 90% (T < 90%); (4) limb movement parameters of PLMI; and (5) arousal parameters of total arousal index (TArI), respiratory arousal index (RArI), and spontaneous arousal index (SArI). Additionally, the rates of in-laboratory positive airway pressure (PAP) testing for each sleep specialty group and their subsequent PAP therapy acceptance were analyzed. To be eligible for a PAP prescription, individuals had to satisfy one of the following conditions:
-
(A)
Moderate-to-severe OSA (AHI ≥ 15), even in the absence of symptoms.
-
(B)
Mild OSA (AHI 10–15) with any one of the following symptom-based conditions: insomnia, daytime sleepiness, cognitive disorder, mood disorder.
-
(C)
Mild OSA (AHI 5–10) with any one of the following: hypertension, ischemic CVD, history of stroke, or min SpO2 < 85%.
The PAP device had fixed and auto-adjusting PAP modes. The prescribed mode was determined on the basis of the discretion of the individual sleep specialist and patient preferences. If the in-laboratory manual PAP titration was successful, a fixed-pressure CPAP mode was offered on the basis of the titration results. Where manual titration was refused, failed, or unselected by the physician, Auto-PAP, which has a wide range of therapeutic pressures that can be automatically adjusted while the patient is sleeping, was prescribed.
Statistical Analysis
Demographic and PSG parameters were compared among the ENT, NR, and PSY groups. Categorical data are presented as counts and percentages, whereas continuous data are expressed as mean and standard deviation (SD) or median and interquartile ranges [IQR] for normally and non-normally distributed data, respectively. The Mann–Whitney rank sum test was used to analyze sex differences in each group. For comparisons between groups, we performed the chi-square test for categorical variables. Normally distributed continuous variables were analyzed using Welch’s analysis of variance (ANOVA) with pairwise t tests for post hoc analysis (Holm-adjusted). The Kruskal–Wallis test with pairwise Wilcoxon tests for post hoc analysis (Holm-adjusted) was used for non-parametric continuous data. Multiple logistic regression analysis using a backward step was performed to identify the potential demographic and PSG variables predictive of PAP acceptance. These results are presented as odds ratios (ORs) and 95% confidence intervals (CIs).
In cases where REM sleep was not obtained or sleep questionnaires were inaccurate (poorly completed, incomplete or not completed), these parameters were treated as missing values. Statistical analyses were conducted using SPSS data editor software for Windows, version 25.0 (IBM SPSS Statistics, IBM Corp., Armonk, NY, USA). P < 0.05 was considered statistically significant for all statistical tests.
Results
General Characteristics of the Study Population
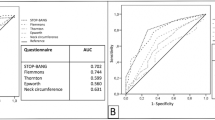
We reviewed the records of 445 patients and excluded 38 patients aged < 18 years (n = 2), with sleep time < 120 min (n = 1), postsurgical PSG (n = 3), MSLT-paired PSG for suspected hypersomnia (n = 20), and testing at a different sleep specialty clinic (n = 12). Missing REM sleep parameter values were observed in 20 patients. Finally, 407 patients who underwent PSG were analyzed. The majority of patients were referred by the ENT clinic (56.8%), followed by the PSY (23.8%) and NR (19.4%) clinics. In-laboratory zolpidem was administered to 151 patients, with 86 patients (37.2%) in the ENT group, 30 patients (38.0%) in the NR group, and 35 patients (36.1%) in the PSY group. For patients using self-administered daily hypnotics during PSG, 10 patients (4.3%) were in the ENT group, 7 patients (8.9%) in the NR group, and 52 patients (53.6%) in the PSY group. The patients were predominantly male (68.1%), with an average BMI of 25.1 kg/m2, including 17.2% with obesity (BMI ≥ 30 kg/m2). Hypertension was the most common comorbidity (33.7%). A considerable proportion of patients (24.8%) scored ≥ 11 on the ESS. Most patients (83.0%) met the criteria for OSA diagnosis (AHI ≥ 5/h), with 26%, 21.1%, and 35.9% of patients in the mild, moderate, and severe categories, respectively. The severity of OSA based on AHI was higher in men, regardless of the sleep specialty clinics they visited. Of the 338 patients diagnosed with OSA, 173 underwent in-laboratory PAP titration and 195 received PAP therapy. Further details of the study population are presented in Table 1 and Fig. 1.
Stacked bar graph showing the distribution of the obstructive sleep apnea severity according to sleep clinic pathway (normal, AHI < 5; mild, AHI 5–15; moderate, AHI 15–30; and severe, AHI ≥ 30). AHI apnea–hypopnea index, ENT otolaryngology, NR neurology, PAP positive airway pressure, PSY psychiatry. a Total population (n = 407), b PAP acceptance population (n = 195)
Group Comparison According to Sleep Clinic Pathway
The group characteristics are outlined in Table 1. There were significant differences between the three groups. The ENT group was the youngest in age and had the highest daytime sleepiness, AHI, RDI, ODI, hypoxemic parameters, sleep efficiency, and shortest sleep latency. The NR group shared similarities with the ENT group in terms of male predominance, BMI, and occurrence of moderate-to-severe OSA, but showed intermediate characteristics in OSA-related PSG parameters (ENT > NR > PSY; AHI, RDI, ODI, minO2, T < 90%, RArI) between the ENT and PSY groups. Additionally, the NR group had the highest prevalence of hypertension (45.6%) and cardio- or cerebrovascular diseases (27.8%). The PSY group, predominantly female (53.6%), had the lowest BMI, highest incidence of depression, and lowest subjective sleep quality, mildest OSA, and lowest rate of hypoxia, and showed a similarly low ESS as the NR group. Most sleep structure variables did not show significant differences between the NR and PSY groups except shortened N1 sleep in the PSY group. The ENT group had the highest number of requests for in-laboratory PAP titration studies (82.7%) and PAP prescriptions (73.8%). In comparison, of the NR and PSY groups, only 13.4% and 4.0% underwent an in-laboratory PAP titration study, and among those who met the diagnostic criteria for sleep apnea with an AHI ≥ 5, 13.3% and 12.8% were prescribed PAP, respectively.
Analysis of Patients with Moderate-to-Severe OSA According to Sleep Clinic Pathway
The characteristics of patients with moderate-to-severe OSA in each group are presented in Table 2. Patients with moderate-to-severe OSA accounted for 57.0% of the total study population. The distribution according to the sleep clinic pathway was as follows: ENT (67.2%) NR, (19.0%) and PSY (13.8%). The ENT group had the worst OSA severity, whereas the NR group had the highest comorbidity rates for hypertension and cardiovascular or cerebrovascular disease and shared similar BMI and PSG parameters to those of patients with severe OSA in the ENT group. Both the NR and PSY groups had a significantly older average age, reduced propensity for sleepiness, and higher rate of moderate-to-severe depression (> 30%) compared with the ENT group. The PSY group exhibited the least severe OSA among the three groups, with the lowest AHI, hypoxia, BMI, and the occurrence of obesity. The PAP acceptance rates in patients with AHI ≥ 15 were notably higher in the ENT group (80.1%) than in the NR (56.8%) and PSY (56.3%) groups.
Factors Affecting PAP Acceptance
Independent factors associated with PAP acceptance are presented in Table 3. The analysis revealed that the sleep clinic pathway significantly predicted the acceptance of PAP. Patients diagnosed with OSA in the NR and PSY groups were less likely to have been prescribed PAP therapy than those in the ENT group (p < 0.001 and p = 0.05, respectively). Moreover, a higher ODI and lower minO2 were associated with a higher likelihood of receiving PAP therapy (p = 0.003 and p = 0.003, respectively). Other clinical factors, such as age ≥ 60 years, sex, BMI, ESS, PSQI, BDI-II, and AHI, did not independently predict PAP acceptance.
Discussion
The present study is the first to compare the differences among patients requesting PSG for suspected OSA from three sleep specialty clinics within a single tertiary center. This investigation provides critical insights into the clinical and PSG characteristics of patients with suspected and confirmed OSA. We found that patients from different sleep clinics had distinct differences in OSA severity, mood, daytime sleepiness, and comorbidities. These distinct patient characteristics underscore the multidimensional nature of OSA and its association with other medical and psychiatric disorders. Understanding and accounting for these variations in patients are pivotal for improving OSA management. The ENT group accounted for over half of all the referrals in this study. Additionally, the acceptance of PAP treatment was highest in the ENT group, perhaps as a result of referral by an otolaryngologist and the original presentation of an upper respiratory tract issue.
We believe that our results reflect recent shifts in clinical practice after the introduction of NHI coverage of PSG for OSA in South Korea in July 2018. An initial comprehensive national data analysis indicated a fourfold increase in patients undergoing in-laboratory sleep PSG immediately after the implementation of NHI coverage, which was attributed to enhanced medical accessibility and a reduced cost of approximately 130 USD [2]. The nationwide rate of PAP prescriptions revealed that medical specialists diagnosing and managing sleep apnea were exclusively concentrated in three departments: ENT (66.6%), NR (18.7%), and PSY (10.3%) [2]. This split in sleep studies by clinic is consistent with our observations. Clinical practice in sleep clinics is influenced by patient preferences and individual symptomatology related to specific disorders. Patients often choose specialized sleep clinics on the basis of their primary complaint, and OSA is traditionally diagnosed and managed by otolaryngologists. However, the emerging trends in this study suggest that there is potential for an increase in diagnoses from sleep clinics specializing in insomnia treatment or from internal medicine sleep specialists interested in managing OSA-related medical comorbidities.
Our study particularly emphasizes the marked increase in sleep studies of psychiatric patients within our tertiary center. The prevalence of PSG in PSY clinic may be due to diverse complaints of psychiatric disorders. The multifaceted and subjective symptoms of psychiatric disorders pose a diagnostic challenge, emphasizing the need for psychiatric professionals to exclude secondary sleep disorders. Even among patients tentatively diagnosed with primary or secondary insomnia accompanying chronic psychiatric disorders, there is a substantial demand for PSG upon reasonable clinical suspicion of breathing or movement disorders, uncertain initial diagnosis, treatment failures, or precipitous arousals occurring with violent or injurious behaviors [6]. Utilizing PSG benefits psychiatrists in excluding OSA, aiding in chronic insomnia treatment strategies such as Cognitive Behavioral Therapy for Insomnia (CBT-I), and safe use of sedative hypnotics [7]. One-third of the PSY group in our study presented with moderate-to-severe sleep apnea, despite its lower severity compared to the other groups, indicating a non-negligible prevalence of OSA, particularly in the older population.
Notably, both the NR and PSY groups predominantly consisted of older patients with similar low or no sleepiness characteristics and comparable sleep structures irrespective of OSA severity. Advancing age, male sex, and higher BMI are known to increase OSA prevalence by up to 49% with advanced age [8,9,10]. Previous reports have emphasized that the older population may be less obese, with less sleepiness and less severe OSA but more insomnia symptoms [11, 12].
OSA is a highly heterogeneous condition involving individual combinations of pathophysiological, polysomnographic, and clinical symptom-based traits. Recent guidelines have highlighted numerous symptoms linked to OSA and more variations beyond these descriptions may exist [13]. Clinical examination, sleep apnea-focused questionnaires, and clinical prediction algorithms alone are limited in their ability to diagnose OSA, and direct objective sleep apnea testing should be conducted [14, 15]. Recent cluster analyses in patients with moderate-to-severe OSA revealed three consistent groups: excessive sleepiness, disturbed sleep, and minimal symptoms, irrespective of the patient’s AHI [16,17,18]. These findings highlight the lack of a direct correlation between symptoms and OSA severity, with typical excessive daytime sleepiness being present in only a subset of patients. These studies have reported that the minimally symptomatic phenotype accounts for 25–56% of patients and is more prevalent among older individuals, which potentially delays OSA diagnosis. We observed similar characteristics in patients with moderate-to-severe OSA in the NR and ENT groups with similar OSA severity and hypoxic burden. However, no sleep propensity in daily life, as indicated by the ESS score ≤ 5, was observed in 60.5% of the NR group, almost double the rate of the ENT group. Additionally, the NR group had the highest prevalence of comorbidities and older patients. These findings support previous studies and indicate the need for comprehensive sleep evaluation, particularly in asymptomatic or minimally symptomatic elderly patients with medical comorbidities. PAP treatment is recommended as the first-line treatment modality in cases of AHI ≥ 15 [19]. This study reports a positive effect of the ENT sleep clinic pathway, BMI, and OSA severity metrics on the likelihood of PAP acceptance. The higher acceptance of PAP therapy in the ENT group may be attributed to their younger age and more severe OSA, which is a factor linked to increased adherence. The younger age of the ENT group may also contribute to their higher acceptance, possibly as a result of more active engagement with updated health-related information through the media and internet. The ENT group might have had a higher awareness of OSA, a more positive attitude toward treatment, and a greater willingness to actively pursue therapeutic interventions. As our study was conducted at a single tertiary center, it is likely that patients with relatively severe OSA in the community were referred to the ENT sleep clinic, offering both surgical and non-surgical treatment options. Contrastingly, the NR and PSY groups primarily focused on exams confirming or excluding OSA due to insomnia or comorbidities, and so might be less receptive to treatment based solely on physician recommendations, especially if coupled with lower awareness of OSA and PAP therapy. We did not identify a significant influence of daytime sleepiness, sleep quality complaints, or AHI on acceptance of PAP therapy. This suggests that commonly used questionnaires, such as the ESS and PSQI, may not accurately reflect patient symptoms. Instead, our results, as depicted in Table 3, emphasize the importance of hypoxemic parameters with PAP acceptance, highlighting the role of the hypoxic burden in modifying OSA severity. Hypoxic burden has been suggested to be as effective or even superior to AHI in predicting adverse medical outcomes [14, 20]. We also did not observe any influence of age on PAP acceptance. There is ongoing debate regarding PAP adherence between younger and older individuals, which potentially contributes to reduced adherence among older individuals [12, 21]. Moreover, in the older population, there may be instances of minimally symptomatic yet severe OSA, leading individuals to refuse PSG and not being evaluated for treatment. The low rate of acceptance of PAP in the PSY and NR groups in this study indicates that a non-uniform, personalized approach to treatment may be necessary for some patients. Alternatively, these groups may be unaware of the importance of treating OSA.
This study has several limitations. First, as it was exclusively conducted at a single tertiary center in South Korea, our findings may have been influenced by referral bias. There could also be a significant bias in patient selection due to specific insurance coverage criteria for PSG and PAP therapy within the healthcare system, which could have influenced the composition of the study sample, potentially limiting the generalizability of the results. Second, we did not investigate long-term acceptance of PAP treatment. Previous observational studies have suggested that the long-term maintenance of PAP therapy is influenced by socioeconomic factors and the healthcare system [22]. Findings from recent Korean observational studies suggest improved long-term compliance with PAP therapy up to 9 months post-implementation of the NHI [23]. Third, as we only focused on patients undergoing PSG, we may have underestimated the overall prevalence of sleep disorders owing to cases in which patients declined evaluation. Finally, we were unable to investigate individual reasons for refusal to undergo PAP treatment because of the retrospective nature of the study. Future prospective multicenter studies are needed to verify the long-term efficacy of NHI coverage on OSA diagnosis and PAP therapy.
Conclusion
This study elucidated the distinct patient characteristics and PSG findings of individuals who underwent overnight PSG for suspected OSA from three distinct sleep specialty clinical pathways. Our findings illustrate the real-world practice of PSG utilization within a tertiary center for patients with various primary complaints. We also highlight the multifaceted needs of sleep specialists and patients for diagnosing sleep disorders using PSG. Our findings could be valuable reference material for future research assessing the appropriateness of policies in other countries considering implementation of NHI coverage for PSG and PAP therapy. Further large-scale, longitudinal studies are needed to understand the differences in patient populations among various sleep specialty clinics and identify the most effective strategies tailored to individual needs.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Markun LC, Sampat A. Clinician-focused overview and developments in polysomnography. Curr Sleep Med Rep. 2020;6:309–21. https://doi.org/10.1007/s40675-020-00197-5.
Kim M, Baek H, Lee SY. Trends of clinical practice for obstructive sleep apnea following the change in the national health insurance coverage. J Sleep Med. 2020;17:122–7.
Sateia MJ. International classification of sleep disorders. Chest. 2014;146:1387–94.
Berry RB, Abrue A, Quan SF. The AASM Manual for the scoring of sleep and associated events rules, terminology, and technical specifications. Version 2.6.0. Darien, (IL). American Academy of Sleep Medicine: 2020.
Kim JW, Won TB, Rhee CS, Park YM, Yoon IY, Cho SW. Polysomnographic phenotyping of obstructive sleep apnea and its implications in mortality in Korea. Sci Rep. 2020;10:13207. https://doi.org/10.1038/s41598-020-70039-5.
Schutte-Rodin S, Broch L, Buysse D, Dorsey C, Sateia M. Clinical guideline for the evaluation and management of chronic insomnia in adults. J Clin Sleep Med. 2008;4:487–504.
Janssen H, Venekamp LN, Peeters GAM, Pijpers A, Pevernagie DAA. Management of insomnia in sleep disordered breathing. Eur Respir Rev. 2019. https://doi.org/10.1183/16000617.0080-2019.
Jung Y, Junna MR, Mandrekar JN, Morgenthaler TI. The national healthy sleep awareness project sleep health surveillance questionnaire as an obstructive sleep apnea surveillance tool. J Clin Sleep Med. 2017;13:1067–74.
Heinzer R, Vat S, Marques-Vidal P, et al. Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med. 2015;3:310–8. https://doi.org/10.1016/S2213-2600(15)00043-0.
Senaratna CV, Perret JL, Lodge CJ, et al. Prevalence of obstructive sleep apnea in the general population: a systematic review. Sleep Med Rev. 2017;34:70–81. https://doi.org/10.1016/j.smrv.2016.07.002.
Onen F, Moreau T, Gooneratne NS, Petit C, Falissard B, Onen SH. Limits of the Epworth sleepiness scale in older adults. Sleep Breath. 2013;17:343–50. https://doi.org/10.1007/s11325-012-0700-8.
Lammintausta A, Anttalainen U, Basoglu ÖK, et al. Clinical characteristics and positive airway pressure adherence among elderly European sleep apnoea patients from the ESADA cohort. ERJ Open Res. 2023;9:00506–2022.
Patil SP, Ayappa IA, Caples SM, Kimoff RJ, Patel SR, Harrod CG. Treatment of adult obstructive sleep apnea with positive airway pressure: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2019;15:335–43. https://doi.org/10.5664/jcsm.7640.
Malhotra A, Ayappa I, Ayas N, et al. Metrics of sleep apnea severity: beyond the apnea-hypopnea index. Sleep. 2021. https://doi.org/10.1093/sleep/zsab030.
Kapur VK, Auckley DH, Chowdhuri S, et al. Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2017;13:479–504. https://doi.org/10.5664/jcsm.6506.
Ye L, Pien GW, Ratcliffe SJ, et al. The different clinical faces of obstructive sleep apnoea: a cluster analysis. Eur Respirat J. 2014;44:1600–7.
Keenan BT, Kim J, Singh B, et al. Recognizable clinical subtypes of obstructive sleep apnea across international sleep centers: a cluster analysis. Sleep. 2018;41:Zsx214. https://doi.org/10.1093/sleep/zsx214.
Kim J, Keenan BT, Lim DC, Lee SK, Pack AI, Shin C. Symptom-based subgroups of Koreans with obstructive sleep apnea. J Clin Sleep Med. 2018;14:437–43. https://doi.org/10.5664/jcsm.6994.
Adult Obstructive Sleep Apnea Task Force of the American Academy of Sleep Medicine. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5:263–76.
Cao W, Luo J, Xiao Y. A review of current tools used for evaluating the severity of obstructive sleep apnea. Nat Sci Sleep. 2020;12:1023–31. https://doi.org/10.2147/NSS.S275252.
Martinez-Garcia MA, Valero-Sánchez I, Reyes-Nuñez N, et al. Continuous positive airway pressure adherence declines with age in elderly obstructive sleep apnoea patients. ERJ Open R es. 2019;5:00178–2018.
Pandey A, Mereddy S, Combs D, et al. Socioeconomic inequities in adherence to positive airway pressure therapy in population-level analysis. J Clin Med. 2020;9:442. https://doi.org/10.3390/jcm9020442.
Choi W, Bae M, Chung Y. The impact of national health insurance coverage on compliance with positive airway pressure therapy in patients with obstructive sleep apnea. Clin Exp Otorhinolaryngol. 2022;15:100–6. https://doi.org/10.21053/ceo.2020.02362.
Acknowledgements
Medical Writing and Editorial Assistance
The authors declare there is no medical writing. We would like to thank Editage (www.editage.co.kr) for English language editing.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Funding
No funding or sponsorship was received for this study or publication of this article. The Rapid Service Fee was funded by the authors.
Author information
Authors and Affiliations
Contributions
Eunmi Lee designed the study concept, data collection, statistical analysis, interpretation of data and drafted main manuscript. Hyunjo Lee assisted data collection and interpretation of data. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflicts of interest.
Ethical Approval
This study was approved by the Institutional Review Board of Ulsan University Hospital (IRB No. 2023-10-014), and the procedures followed were in accordance with the principles of the 1964 Helsinki Declaration and its later amendments. The requirement for informed consent was waived because of the retrospective nature of the study, and patient identities were maintained anonymously. The K-BDI-II incorporating the standardized scale questionnaire since August 1, 2020 has been officially integrated into the medical insurance fee as outlined in the Ministry of Health and Welfare’s directive No. 2020–163 in South Korea. At our healthcare institution, we utilize the Korean version of the K-BDI-II provided by the Korean Psychology Corporation. We use this version for assessments, billing purposes, and the results are transcribed and attached to the medical records after score conversion. The result form captures details such as the name, gender, age, and examination date of the respondent. Each page of the questionnaire explicitly notes that all rights are reserved by Aaron T. Beck. The medical institution claims the comprehensive fee code, 너701나FY752060, covering the cost of the BDI-II for the subjects, and receives reimbursement from the National Health Insurance.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Lee, E., Lee, H. Clinical and Polysomnographic Characteristics of Adult Patients with Suspected Obstructive Sleep Apnea from Different Sleep Clinics at a Single Tertiary Center. Neurol Ther 13, 399–414 (2024). https://doi.org/10.1007/s40120-024-00581-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40120-024-00581-1