Abstract
Introduction
The objective of the study was to investigate long-term food intake patterns and establish possible associations between the inferred dietary habits and levels of reported symptoms among people with multiple sclerosis (MS) in Denmark.
Methods
The present study was designed as a prospective cohort study. Participants were invited to register daily food intake and MS symptoms and were observed during a period of 100 days. Dropout and inclusion probabilities were addressed using generalized linear models. Dietary clusters were identified among 163 participants using hierarchical clustering on principal component scores. Associations between the dietary clusters and the levels of self-assessed MS symptoms were estimated using inverse probability weighting. Furthermore, the effect of a person’s position on the first and second principal dietary component axis on symptom burden was investigated.
Results
Three dietary clusters were identified: a Western dietary cluster, a plant-rich dietary cluster and a varied dietary cluster. Analyses further indicated a vegetables-fish-fruit-whole grain axis and a red-meat-processed-meat axis. The plant-rich dietary cluster showed reduction in symptom burden in nine pre-defined MS symptoms compared to the Western dietary cluster (between 19 and 90% reduction). This reduction was significant for pain and bladder dysfunction as well as across all nine symptoms (pooled p value = 0.012). Related to the two dietary axes, high intake of vegetables resulted in 32–74% reduction in symptom burden compared to low levels of vegetable intake. Across symptoms, this was significant (pooled p value = 0.015), also regarding walking difficulty and fatigue.
Conclusions
Three dietary clusters were identified. Compared to levels of self-assessed MS-related symptoms, and adjusted for potential confounders, the results suggested less symptom burden with increased intake of vegetables. Although the research design limits the possibilities of establishing causal inference, the results indicate that general guidelines for healthy diet may be relevant as a tool in coping with MS symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
More knowledge is needed regarding dietary habits and their potential impact among people with multiple sclerosis |
Very brief background leading to the study is provided, including for example disease population, economic burden and/or unmet need |
The impact of diet on MS symptomatology and disease progression is actively discussed, not least among patients. Research within the field is centered around either studies using food frequency questionnaires or intervention studies, both research designs entailing methodological challenges within the MS population |
The study adds to the existing knowledge within the field by having systematically collected real-world observational data on food intake and MS-related symptoms over a significant period of time |
What was learned from the study? |
The results suggested three dietary clusters among people with multiple sclerosis and an overall negative association between affiliation to the plant-rich dietary cluster and levels of symptom burden, with less symptom burden with increased intake of vegetables |
Although statistically complex, a prospective cohort study based on real-world data from daily registrations offers unique insight into dietary habits and possible associations to MS symptomatology |
Introduction
Multiple sclerosis (MS) is an chronic, autoimmune, demyelinating disease of the central nervous system. Medical treatment can halt the progress of the disease in some cases, and certain complications can be treated medically. However, treatments are only partially effective and may cause a number of side effects. Two out of three persons with MS (pwMS) are women [1].
MS often entails many accompanying symptoms [2], and many pwMS in Denmark engage in daily self-care activities with the aim of alleviating symptoms [3]. Such activities comprise conventional activities as well as activities within the complementary field, and the purpose of such activities is mainly non-specific and preventive [3,4,5,6]. Self-care activities most often carried out among pwMS are physical exercise, brain exercise and dietary intervention [3]. A range of more or less specific MS diets exist and are frequently used by pwMS, including Swank’s, Wahl’s, Jelinek’s, anti-inflammatory, vegetarian and ketogenic diets [7]. The use of such diets is to a wide extent based on patient-experienced benefits, very often anecdotal and non-systematized.
While many studies have investigated the effect of physical exercise and cognitive interventions on the symptomatology in pwMS, a limited number of studies have explored possible associations between food intake and disease expression. Specific nutritional perspectives, such as low sodium intake, intake of coconut oil as well as intake of specific fatty acids and vitamin D, have been suggested as being associated with slower disease progression, better quality of life, lower levels of depression and/or lower level of MS-related symptoms. However, results are somewhat conflicting [8,9,10,11,12,13,14]. It has been argued that more studies on diet are needed rather than studies targeting individual nutrients [15]. Some case-control studies have indicated that diet may be a relevant component in reducing MS risk [16,17,18,19,20,21] while other studies have not been able to confirm this hypothesis [22, 23]. Cross-sectional studies investigating possible associations between diet and symptom severity and/or disability among pwMS have indicated the relevance of a healthy diet [7, 18, 20, 24,25,26,27,28,29]. However, such studies are most often based on food frequency questionnaires and thereby entail methodological challenges, e.g. due to recall bias within a patient group where cognitive impairment is highly prevalent [30]. Furthermore, observational studies may suffer from uncontrolled confounding. High-quality clinical trials are rare within the field of MS and diet, not least due to challenges in maintaining pwMS on a specific diet during a long period of time. Fatigue, impairment in motor skills and children in the household with specific dietary habits constitute some of these challenges [31,32,33]. Pilot studies and small-scale trials [14, 34,35,36,37,38,39,40,41,42] have been conducted as well as a few medium-scale trials [43,44,45,46,47], but although suggesting that diet may play a relevant role in the management of MS symptomatology, recent reviews conclude that evidence is uncertain [48,49,50,51].
In the present study, our aim has been to supplement the existing knowledge within the field by systematically collecting real-world observational data on food intake and MS-related symptoms over a significant period of time. We utilize the collected real-world dataset to investigate long-term food intake patterns and establish possible associations between the inferred dietary habits and levels of reported MS-related symptoms. Hence, the digital study design accommodates some of the main methodological challenges observed in previous studies. The study addresses the long-term (equilibrium state) association between dietary habits and levels of MS symptoms. Short-term or lagged effects of diet on MS symptoms are not addressed in the current study. Hence, the objective of the study was to investigate long-term food intake patterns and establish possible associations between the inferred dietary habits and levels of reported symptoms among people with multiple sclerosis (MS) in Denmark based on daily registrations of food intake and MS symptoms.
Methods
Study Design
The present study was designed as a prospective cohort study. Participants were observed during a period of 100 days. Food intake and levels of MS symptoms were registered daily. The study was not designed to investigate a possible effect of one or more specific diets, but to explore dietary patterns among pwMS and establish possible associations between such patterns and long-term levels of MS symptoms among the participants.
Study Population and Participant Flow
From November 2017 to March 2018, pwMS were invited to participate in the study, which entailed performing daily registrations on diet intake and MS symptoms. Invitations were emailed to all members of the Danish MS Society who had provided an email, indicated MS diagnosis, were > 18 years old and had agreed to receive information from the patient society. Additionally, invitations to the study were posted in magazines and on social media pages. Individuals diagnosed with MS who were not members of the society were permitted to participate.
Invitations were sent out to 7249 people and 689 people accepted the invitation, and an additional 46 people signing up to the study without having received the original invitation. Of 735 people who signed up for the study, 550 downloaded the study platform app and filled out the consent form and baseline questionnaire.
Of the 550 registered participants, 413 downloaded the diet tracker app, set up data exchange between their diet tracker app profile and study server, and had at least one active day as a participant. An active day was defined as a day on which the participant had registered food intake and reported symptom burden. Among 413 participants, median number of active days (interquantile limits Q1, Q3) were 25 (2, 65), with 16% of participants having zero active days (left censoring) and 0.5% having 100 active days (right censoring).
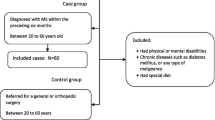
Missing entry percentages for background variables were 5.3% for work status, 7.0% for MS type and 1.0% for age. Among the 413 participants, 163 fulfilled the inclusion criteria of at least 21 active and 3 weekly registrations in average between first and final registration. All 163 of the included participants had complete background information available, with a median number of active days and interquantile limits (Q1, Q3) of 73.0 (53.0, 69.1) and lower levels of left (0.6% with 21 active days) and right (1.2% with 100 active days) censoring. Furthermore, all 163 of the included participants had signed up and initiated daily registrations during the first three enrolment months between November 2017 and January 2018. In Fig. 1, the participant flow is illustrated. Participant flow and attrition are further described as supplementary material (Table S2), where we have listed frequencies and percentages in the varying categories of the included and available background variable, including demographic variables, MS type, aid, disease-modifying treatment, etc., for each step in the participant flow.
Collected Background Data
For all participants, the following 11 background variables were collected as self-reported data at baseline: gender (male, female), civil status (single, married/in couple), work status (employed/working, under education, early retirement, otherwise), education (primary school, high school, vocational education, short higher education, bachelor's degree, master's degree or higher), MS type (relapsing-remitting MS, secondary progressive MS, primary progressive MS), use of aid equipment (yes, no), disease-modifying treatment (yes, no), smoking (never smoked, previous smoker, current smoker (on the day of filling out the questionnaire), sequelae (none, 1–2, 3 or more) as indicated by medicinal drug usage, region (Copenhagen and surrounding, Seeland, Northern and Middle Jutland, Southern Danmark, other). Furthermore, age and time since diagnosis were discretized into the following categories: age < 43 years, 43–51 years, > 51 years; time since diagnosis 0–4 years, 5–9 years, 10–14 years and ≥ 15 years.
Data on side effects (such as fatigue or taste change) due to use of medication were not collected in the study. Data on weight/obesity were optional in the questionnaire and were not included in the analyses because of limited response.
The current study’s nature as an observational, prospective cohort study based on participant self-reported data collected via digital apps entailed some restrictions regarding the inclusion of clinical data. For example, reliable EDSS values would have required a clinical assessment at study entrance by a clinician. Self-reporting of often non-updated EDSS assessments might have been too error prone or misleading. However, we might argue that some of the background variables included in the current study, and reported by the participants, may carry important information on the MS disease progression state and hence are expected to be proxies for clinical measures as EDSS, at least in combination. These background variables are time since diagnosis, use of aid equipment (aid) and number of sequelae.
Data Collection
Participants downloaded a platform app, constructed specifically for the project and linking to the diet tracker FatSecret, daily questionnaires for symptom registration, a questionnaire regarding background information as well as general guidance. Informed participation consent was obtained (including consent for participation and publication), and participants completed a baseline questionnaire before initiating registrations. Participants were encouraged to register diet and symptoms for up to 100 days but were informed that a shorter interval would also benefit the study.
Diet data for all participants were extracted daily from FatSecret servers to a server at University of Copenhagen. By the end of the data collection, data were transferred as XML files that were pre-processed for analysis. The data extract from FatSecret contained information on Food ID, registration timestamps, participant ID, name and description of food ID, units, meal and nutritional content.
Food IDs were coded and grouped in three levels with each food ID being assigned a food category, food group and food item. Items were coded according to a food coding framework used in the Danish Diet, Cancer, and Health prospective cohort 1993–1997 [52]. All food IDs were coded into categories, followed by a coding of each category into food groups, and finally into food items as exemplified in Fig. 2. The entire list of food group items is presented as supplementary material Table S1.
Daily self-reported measures of symptoms provided the main outcome for the work reported in this article. Clinical tests, such as EDSS, were not performed on the participants. The exploratory, real-world study design, following people with MS' everyday dietary habits and development in MS symptoms, imposed a rather large burden of registration on the participants. Additional clinical tests and evaluations would have entailed the risk of imposing an unfeasible trial burden.
Due to a lack of suitable MS-specific scales for assessing daily changes in symptoms, a scale was developed specifically for the project [53, 54]. Items were constructed based on interviews with individuals with MS, and health professionals provided feedback on scale drafts. The final version of the scale has gone through validation testing in cognitive interviews and a pilot study that tested response scale sensitivity and face validity [53, 54]. As part of the pilot study, data were collected over a week for each participant to test day-to-day sensitivity, and the scale showed satisfactory results for both internal consistency (Cronbach’s alpha) and content validity. A separate, complete scale validation is in progress.
The MS scale consists of nine symptoms and seven functions that individuals with MS consider important for their everyday ability to be active and engaged in daily life. In this article, we report on results using the nine MS symptoms as outcome variables. The nine symptoms are fatigue, pain, spasticity, muscle weakness, walking difficulty, dizziness, sensory disturbances, bladder problems and bowel problems. Each item is assessed on a numerical rating scale ranging from 0 (symptom not present) to 10 (symptom presents worst imaginable).
Furthermore, FatSecret was chosen as the diet tracker used in the study. The diet tracker allows users to track food intake by adding food items from the app’s food database or to create food items themselves. As part of the logging, participants are asked to estimate weight/amount of a logged food item. As part of an exploratory, real-world study, this standard food app database approach to diet tracking decreases the food logging burden for participants, and the content of the app food database has previously shown comparable to reference methods [55, 56].
Attrition Analyses
Prospective observational studies are vulnerable to selection bias especially because of an increased risk of non-random dropout or differential contribution from study participants eventually leading to attrition and/or contribution bias [57]. For example, among the 163 participants passing the inclusion criterion, considerable variation in contribution with data among participants remained, with response rates, i.e., number of active days out of the 100 possible observation days, ranging from 21 to 100% with median (Q1, Q3) rates of 73% (53%, 69%). We therefore investigated both dropout and differential response rates as a function of the 11 background variables using the following four models. Model I addressed the dropout probability among the 550 registered participants. Model IIa and IIb addressed the response rate and inclusion probability, respectively, among the 413 participants after dropout. Finally, model III addressed the response rate among the 163 in-study participants. Dropout and inclusion probabilities were modeled using binomial logistic regression, while response rates were modeled using quasi-binomial logistic regression to account for over-dispersion due to left and right censoring. To address whether participants with different dietary patterns contributed with differing data entry intensity, model III included dietary cluster membership (see below) as a 12th explanatory variable. In all models, we used a step-wise downward selection strategy dropping at each step the model term with largest Wald test p-value until only significant model terms were retained.
Dietary Cluster Derivation and Characterization
Initial analyses indicated that only few respondents consistently followed well-defined diets. Using a threshold of at least 85% of observation days as a diet consistency indicator, only 2.5%, 1.8% and 0.0% of the respondents followed the anti-inflammatory, vegetarian and Swank’s diet, respectively. Hence, to identify dietary patterns among the participants, we performed hierarchical clustering on principal component scores (HCPC) derived from participants’ individual food category mean daily portions (dp) calculated over the study period. HCPC provides a means of representing participants and correlated food categories in a lower dimensional space, while simultaneously achieving a denoised cluster solution [58]. In the principal component analysis (PCA) on the square-root transformed data, we identified seven components with an eigenvalue > 1 explaining a total of 67% of the variance of the data. We then used hierarchical clustering on the seven first principal component scores using Ward’s linkage to minimize the total within-cluster variance. Using the tau index [59] we identified three dietary clusters. Dietary clusters were then characterized by calculating median and interquantile ranges of mean dp intake for all food categories and by calculating percentage distributions of demographic characteristics, testing group differences using chi-square tests. We used the false discovery rate multiple testing correction at a family-wise significance level of 5%. As dietary cluster membership is sensitive to the chosen clustering method and cluster selection index, we also quantified its position on the first and second principal components axes for each person by discretizing first and second principal component scores into tertile classes.
Statistical Analyses of Symptoms as a Function of Diet
Analysis of treatment effects from observational data may be biased because of imbalance in observed and/or unobserved confounders [60]. We used the following strategy to address the risk of bias in the association between dietary patterns and self-reported symptom burden in pwMS: (1) We identified a minimal total adjustment set [61], i.e., a minimal but sufficient set of potential confounders [61], among all observed background variables using a putative directed acyclic graph (DAG) that describes the complex interrelations among background variables, exposure (dietary cluster) and outcome (symptom burden); see supplementary materials, Figure S1. The putative DAG was tested against the current data using local conditional independence tests and combining test probabilities using Fisher’s C according to Shipley [62]; see supplementary materials, Table S3. We sequentially added variable relationships with smallest local test p values until the DAG no longer was rejected at a 5% level (Fisher’s C, p = 0.14). In all DAG analyses, symptom burden was quantified as the quintile-discretized sum of symptoms scores across all nine symptoms. The identified minimal total adjustment set of the final DAG consisted of Aid, DMT (Disease Modifying Treatment), DiagnTime (Time of Diagnosis), Education, MStype (relapse-remitting, primary progressive or secondary progressive), Sequelae and Work status. (2) We estimated propensity scores for dietary cluster membership using generalized boosted modeling (with default settings in the weightit R function) on the identified adjustment set and investigated the obtained balance in the inverse propensity score weighted adjustment set using the Kolmogorov-Smirnov (KS) statistic [63]. The KS statistic is sample size dependent, and hence we used a KS threshold for balance of KSthreshold = 0.27 corresponding to a 5% type I error rate for the average cluster size of n = 54.3. (3) We then used inverse probability weighting (IPW, [60]) to model each of the nine log-transformed symptoms as a function of the dietary cluster indicator variable and using the inverse propensity scores as observation weights. (4) We used sensitivity analysis to address the effect of a potential omitted variable bias following Cinelli et al. [64]. Cinelli et al. [64] define a robustness parameter RVq that expresses how strong (quantified in percentage of the residual variance of both the treatment and outcome) the unobserved confounder bias must be to bring the point estimate of the treatment to zero. (5) The nine symptom outcomes may be considered as correlated evidence factors, with each outcome potentially being vulnerable to different biases or to biases to different degrees. We combined the evidence from the dependent set of evidence factors by pooling the single outcome p values while taking the correlation structure into account following Cinar and Viechtbauer [65] using Fisher’s method, the sample correlation matrix of the outcome variables (see supplementary materials, Table S4) and the Nyholt method for adjustment of test dependency. (6) Using the described procedures, we also investigated the effect of a person’s position on the first and second principal component axis on symptom burden as a different quantification of dietary patterns may show different sensitivities to measured and unmeasured biases. We used tertile discretization of the first and second axis.
Ethical Consideration and Data Agency
In this study, no biological material or medical devices were used, and the participants were not subjected to any kind of diagnostics or treatment. Consequently, approval from the Danish National Committee on Health Research Ethics was not required, which is the case for all studies only involving interviews and questionnaires. The study was registered and approved by the Danish Data Protection Agency (2016-41-4723). Informed participation consent was obtained (including consent for participation and publication) for all participants.
Results
Attrition and Response Rate
Attrition model I found no significant association between any of the background variables and the probability of dropout among the 550 registered participants (p > 0.05), except for the effect of primary school education (p = 0.019). When excluding participants with primary school as their highest educational level, significance disappeared (p = 0.14). This may indicate that younger participants, as indicated by educational level, dropped out to a lesser degree than the remaining participants (OR 0.52 for non-primary school vs. primary school). Model IIa found that among the 413 participants the response rate was significantly affected by MS type (p = 0.024), sequelae (p = 0.034), and age (p < 0.001), with OR 0.68 and 0.64 for secondary progressive MS and primary progressive MS, respectively, vs. relapsing-remitting MS, OR 1.5, for three or more sequelae vs. none, and OR 1.4 and 1.5 for 43–51 years and > 51 years of age, respectively, vs. < 43 years of age. This indicates that willingness to contribute with data during the surveillance period is positively associated with more progressive or severe MS. Model IIb found that the probability of inclusion into the study significantly was affected only by sequelae (p = 0.021), with OR 2.5 for three or more sequelae vs. none. Finally, model III indicated no significant effects of any of the background variables or dietary cluster membership (p = 0.24) on response rates within the in-study cohort of 163 participants. In short, attrition analyses indicated that initial dropout was probably affected by age-related aspects, presumably related to technical aspects, while contribution intensity was affected by MS severity. Hence, the study population might be biased towards pwMS with more progressive or severe MS.
Dietary Clusters
The HCPC analysis identified three dietary clusters; see Fig. 3. The cluster dendrogram on the first seven principal component scores showed a clear segregation in three main groups (agglomerative coefficient AC = 0.87), with the ratio of average within-cluster distance over average between-cluster distance being 0.85. The first two varimax-rotated dimensions of the PCA indicated a vegetables-fish-fruit-wholegrain axis (PC1) and a red-meat-processed-meat axis (PC2). The biplot suggested a group with elevated intake of red meat and processed meat products (hereafter called Western dietary cluster), a group with elevated intake of vegetables, vegetable oils and fruit (hereafter called plant-rich dietary cluster) and finally a group placed in the central portion of the biplot (hereafter called Varied dietary cluster). Tables 1 and 2 summarize the three dietary clusters in terms of their background and dietary characteristics, respectively. The Western dietary cluster is exclusively characterized by high intake of red meat (0.98 dp) and processed meat (0.70 dp). The dietary cluster varied by dairy products (1.55 dp) and coffee (1.14 dp) and the plant-rich dietary cluster by vegetables (3.67 dp) and vegetable oils (0.32 dp). The Western and plant-rich dietary clusters were clearly distinct concerning background variables (Table 1): while the former was found to consist of pwMS that were less educated, mainly living in rural areas of Danmark (Table 1), the latter was associated with younger, higher-educated pwMS living in the capital region of Denmark, with work status ‘student’ or ‘otherwise/not working’ and not using aid equipment. Participant enrollment month was not associated with any of the dietary clusters. Furthermore, 9 out of 163 participants experience > 1 more days with a self-reported, MS-related relapse during the 100-day period. Relapses occurred among participants in all three dietary clusters.
Results of HCPC analysis showing biplot of the first two varimax-rotated dimensions of the principal component analysis (PCA) (left panel) and the hierarchical clustering tree derived from hierarchical clustering on the first seven principal components scores (right panel); see text for details. Identified dietary clusters are indicated by color. Anti-inflammatory and vegetarian diets are indicated for subjects with at least 75% of observation days in correspondence with the diet. In the biplot, group centroids and for dietary clusters 80% confidence ellipses are shown. Correlations of food categories with principal axes are shown as arrows, indicating a vegetables-fish-fruit-whole grain axis (PC1) and a red-meat-processed-meat axis (PC2). Stippled lines delineate tertiles in the vegetable axis (PC1) and meat axis (PC2)
Neither vegetarians nor Swank diet followers were recovered as distinct groups in the cluster analysis. The single participant following an anti-inflammatory diet could not be determined.
MS-Related Symptoms as Function of Dietary Patterns
Observed and model-adjusted estimates of symptom burden for the three dietary clusters as well the tertile-discretized first and second axis (vegetable intake axis and meat intake axis, respectively) are shown in Tables 3 and 4. After IPW adjustment, the plant-rich dietary cluster showed reduction in symptom burden in all nine symptoms compared to the Western dietary cluster (between 19 and 90% reduction, Table 3). This reduction was significant for pain and bladder dysfunction as well as across all nine symptoms (pooled p value = 0.012). IPW adjustment achieved balance in all background variables in the adjustment set, as assessed by KS < KSthreshold, except aid, which showed a KS of 0.32; none in the plant-rich group received aid (Table 1). Therefore, a different characterization of dietary patterns was assessed by dividing the first two axes of the PCA into tertiles and investigating whether membership within a tertile bin of the first and second axis, representing vegetable and meat intake, respectively, might explain differences in symptom burden (Table 4). This resulted in IPW adjustments with fully balanced adjustment sets (all KS < KSthreshold). However, high intake of vegetables was still resulting in 32–74% reduction in symptom burden when compared to low levels of vegetable intake (Table 4). Across symptoms, this was significant (pooled p value = 0.015), also regarding walking difficulty and fatigue (fatigue being borderline significant). Interestingly, no overall significance was found for the effect of meat intake. However, muscle weakness was significantly associated with meat intake (p = 0.032) with increased muscle weakness in both the high and low meat intake groups, but reduced muscle weakness with medium levels of meat intake (Table 4).
Discussion
Main Findings
Three dietary clusters were detected among the participants; a Western dietary cluster characterized by an elevated intake of red meat and processed meat products, a plant-rich dietary cluster characterized by an elevated intake of vegetables and vegetable oils and a varied dietary cluster characterized by an elevated intake of dairy products and by being placed in the central portion of the biplot. Compared to levels of self-assessed MS-related symptoms, and adjusted for potential confounders, the results suggested an overall negative association between affiliation to the plant-rich dietary cluster and levels of symptom burden, with less symptom burden with increased intake of vegetables. We also addressed the relative importance of increased levels of vegetable intake versus decreased intake of red meat and meat products by investigating the significance of membership within tertile bins of the first and second PC axis that represented vegetable and meat intake, respectively, and found that high intake of vegetables resulted in substantial reduction in symptom burden compared to low levels of vegetable intake, while no overall significance was found for the effect of meat intake.
Comparison with Previous Research
In a study from 2021 among PwMS within 5 years from diagnosis, Simpson-Yap et al. identified three major dietary patterns [24]. Similar to the findings by lw-Yap, we found three dietary clusters in our study, of which one was characterized by a high intake of fruits, vegetables and whole grains and one characterized by a high intake of meat. Also similar to the findings of Simpson-Yap et al. in the before-mentioned study, as well as in another cohort study from 2022 [29], we found a high intake of vegetables to be negatively associated with MS burden (lower relapse risk and reduced disability progression in the studies by Simpson-Yap et al. and lower overall level of MS symptoms in our study). Simpson-Yap et al. found a low intake of meat to be associated with reduced disability progression [29], whereas we did not find clear associations between meat intake and levels of MS symptoms. This latter difference may partly be explained by the rigorous analytical approach in the present study; the initiary IPW-adjusted analyses indicated clear associations among the Western diet, high level of meat intake and higher symptom levels. However, respecting the lack of KS balance in background variables, a supplemental approach was applied, questioning the impact of meat.
Clear associations between food intake and MS symptomatology are yet to be established. A recent study by Fitzgerald et al., based on a dietary screening questionnaire among a large number of participants, suggested that a healthy dietary pattern is associated with less disability and symptom burden among pwMS [7]. Fitzgerald et al. found that a diet that is overall high in fruits, vegetables, legumes and whole grain and lower in added sugars, sweetened beverages and red meat is associated with lower disability levels. Another recent study based on dietary adherence indicated that MS-related symptoms were significantly higher among participants who had a high intake of red meat and lower if a high intake of fish was the case [66]. Similar results were found by Moravejolahkami et al. in another cross-sectional study that showed associations between adherence to a healthy dietary pattern and lower systemic inflammation, severity of fatigue, MS attacks, improved quality of life and balanced weight [27]. These findings are generally supported by a review by Stoiloudes et al. from 2022, stating that a balanced diet involving high amounts of fruit, vegetables and low fat may have an add-on value in more efficient management of the disease overall and that diet may play a role in MS pathogenesis and course [51]. De Majo et al. argue in their study from 2022 that combining the Mediterranean and ketogenic diets is relevant in a dietary protocol for PwMS [67]. Whereas a high intake of vegetables is consistently accentuated in all studies on diet and MS, the intake of fat is more debated. Hence, the ketogenic diet is high in fat, and Stoiloudes et al. emphasize a low intake of fat as recommendable in their review. The results of the present study support the emphasis on vegetable intake as being positively associated with lower levels of MS burden. The results of the present study also support the unclear status of fat; increased muscle weakness in both the high and low meat intake groups was found, whereas reduced muscle weakness was associated with medium levels of meat intake. Moreover, different types of fat should be considered—in the present study, the plant-rich cluster was characterized by a high intake of vegetable oils and the Western dietary cluster by a high intake of butter, snack foods and animal fat. In a review from 2019, AlAmmer et al. emphasize the role of specifically omega-3 fatty acids and fish oils as beneficial for PwMS [, p. 3].13
Based on data from interviews and questionnaires, Jakimovski et al. found unhealthy diet preferences to be associated with MS lesion accrual [28]. In their study, healthy dietary preferences were compatible with the Mediterranean diet, including high consumption of fruits, vegetables, whole grains and reduced consumption of sugary beverages and red meat. In their study, Black et al. found that a healthy diet, high in poultry, fish, eggs, vegetables and legumes, was associated with a decreased risk of a first clinical diagnosis [68]. In a study from 2022, Noormohammadi et al. showed that a high intake of green leafy vegetables, other vegetables and beans seems to decrease the odds of MS [20]. The present study includes solely MS symptomatology, and not risk factors, but it may be emphasized that a high intake of vegetables is highlighted in all three above-mentioned studies, and the potentially overall positive role of a high intake of vegetables among PwMS is supported be the results of the present study.
Intervention studies have established associations between specific diets and MS symptomatology. Yadav et al. found indications that a low-fat, plant-based diet could improve self-reported fatigue [42]. Katz et al. found that a Mediterranean diet reduced fatigue, impact of MS symptoms and disability among pwMS [34]. The diet was characterized by a high intake of fish, fresh fruits, vegetables and whole grain but low in meat, dairy products and processed foods. Lee et al. found in their study that a modified Paleolithic diet, e.g., high in fruits and vegetables as well as plant and animal protein and low in gluten-containing grains, eggs and casein, was associated with reduced fatigue and better maintenance of cognitive function [69]. Mousavi-Shirazi-Fard et al. found in their study that an anti-inflammatory diet, high in fruits, vegetables, whole grain, legumes, plant proteins, essential oils, fish, poultry and low in red meat, eggs, refined carbohydrates and sucrose-containing products, led to improvement in fatigue and in physical and mental components of measured quality of life [44]. In their study, Fellows Maxwell et al. found a diet high in fruits and vegetables, animal and plant protein and low in gluten-containing grains, dairy products and eggs to be associated with improvements in fatigue among pwMS [38]. In a study from 2021, Wahls et al. found both the Swank and Wahls elimination diets have a positive impact on fatigue and quality of life [47], and Brenton et al. found in a study from 2022 that a ketogenic diet may improve fatigue, depression, QoL and neurological disability among PwMS [46].
Although limited in number of participants (n = 61, n = 36, n = 15, n = 100, n = 18, n = 87, n = 65 respectively), these intervention studies suggest that a healthy diet may have a positive impact regarding MS symptomatology among pwMS. All seven studies emphasize fatigue as one of the MS symptoms that may be positively affected by a dietary intervention. In the present study, we found indications of an association between high intake of vegetables and lower levels of fatigue, hereby supporting the trend identified in the pilot studies.
The present study did not find associations between specific food categories and MS symptomatology as was the case in the pilot studies mentioned above, e.g., regarding gluten, dairy products and eggs. However, the pilot studies are all based on pre-defined diets, and the associations between the specific food categories and MS symptomatology should be regarded as part of an overall diet and not as effects of single dietary elements. In the present study, possible associations among gluten, dairy, eggs and levels of MS symptoms were investigated and no associations were found. Similarly, Fitzgerald et al. [7] as well as Simpson-Yap et al. [24] and Black et al. [68] did not, applying similar explorative approach as in the present, find any of the three food categories to be negatively associated with MS symptomatology, relapse rate or MS risk in their studies.
Digital Tools for Data Collection
In the present study, digital tools were used to collect patient-reported data daily with the aim to investigate possible associations between symptom levels and a specific dietary behavior. A large variety of digital tools for data registration has been developed over the past 5–10 years, regarding both manifestation of symptoms and health behavior. Within the field of MS, a range of such tools has been investigated [70,71,72,73,74,75,76,77,78]. Such digital tools may play an important role within the concept of ecological momentary assessment (EMA), where the aim is to collect data on subjects' behavior and experiences in real time and their natural environments [79, 80]. While such tools may serve one purpose for MS patients in supporting and motivating consecutive disease management [74, 75, 81,82,83,84,85,86] and/or for improving dialogue between patients and HCPs [87, 88], other demands must be made when applying digital tools for data collection in research. Within the field of MS, the majority of studies have reported positive experiences regarding the use of digital tools in collecting data for research, e.g., when studying associations between physical activity and MS symptoms [72, 89], physical activity and self-regulatory strategies [90], tracking daily fatigue fluctuations [70], possible associations between cortisol and fatigue [91] as well as depression and fatigue [71]. Several tools for registration of MS symptoms have been tested and/or validated, focusing for example on symptoms in general [76, 78, 92] and fatigue specifically [73]. Motl et al. argue that commercially available accelerometry could profitably be applied as an outcome measure within MS research with the aim of strengthening the understanding of ambulatory impairments in real-world conditions [77]. Thus, while it should be taken into consideration that the use of digital tools in research may entail several challenges linked to validity of measurements [93], adherence [94] and burden of registration [78], for example, it should also be noticed that such tools may offer a valid and valuable way to gain insight into everyday life with MS within real-world settings.
Methodological Strengths and Limitations
The present results are limited regarding causal inference as, for example, no temporal elements are integrated in the analytical design. Any causal interpretation of the found associations among dietary patterns and symptom burdens relies therefore on further assumptions. For example, within-participant dietary patterns and symptom burdens must be assumed to be sufficiently time invariant and their relationship approximately in equilibrium. Under these assumptions, the associations found may be interpreted as long-term effects of dietary patterns on symptom burden in pwMS.
Furthermore, observational studies, as ours, may suffer from bias due to uncontrolled confounders, thereby distorting estimates of causal relationships. For example, dietary patterns may be associated with background variables such as age, education and MS severity, which in itself may influence MS symptom burden. To reduce the potential impact of this limitation, we used inverse probability weighting, thereby providing estimates that are controlled for potential confounding among dietary cluster membership and observed background variables. We also used Cinelli et al.'s [64] sensitivity analysis approach to quantify how strong an unobserved confounder must be to bring the estimated effects down to zero.
It should also be considered that both food intake and symptom levels are self-reported. Recall bias constitutes a major challenge in studies on dietary habits [30], but due to daily digital registrations, this challenge is expected to be reduced in the present study. Digital self-report studies often suffer from response bias in the form of non-random dropout and non-random missing data [95]. Our analyses indicate that initial dropout was affected by age, probably indicating that app-based self-reporting may include technical barriers for people less familiar with digital tools. Furthermore, self-reported daily dietary intake is a time-consuming task, and diet diaries are known to be prone to under-reporting [96]. Our analyses indicate that participants’ motivation to contribute with data and hence achieve inclusion in our study may have been influenced by MS severity. Thus, our study population may be biased towards people with more severe MS compared to the Danish population of people with MS. However, we found no evidence that response rates differed among dietary clusters. While the exploratory design strengthened an everyday and real-world perspective on dietary habits, and their possible associations with MS symptoms, the design did not enable clinical features (e.g., EDSS score) to be included in the study. Furthermore, because participants received standard care and treatment as usual, medical treatment of symptoms may have influenced both presence and rating of symptoms.
Conclusions
Three dietary clusters were identified. Compared to levels of self-assessed MS-related symptoms, and adjusted for potential confounders, the results suggested less symptom burden with increased intake of vegetables. Although the research design limits the possibilities of establishing causal inference, the results indicate that general guidelines for healthy diet may be relevant as a tool in coping with MS symptoms.
Perspectives
The results of the present study add to the growing knowledge concerning the impact of diet on MS symptomatology. While explorative studies such as this contribute to a better understanding of the complexity within which combinations of diet elements may affect MS symptoms rather than single food items affecting them through linear correlations, strong causal associations are still to be established. Large intervention studies, entailing altering of dietary habits for entire families over long periods, are challenging to conduct among PwMS, not least because of the widespread impairments regarding cognitive functions, motor skills and energy levels. Explorative study designs should be further developed with the aim of generating better and more individualized knowledge on correlations between diet and MS symptomatology, combining tools that allow for non-comprehensive daily registrations over a significant period of time and analytical approaches that integrate temporal elements and thereby strengthen the understanding of possible causal relations.
References
Dobson R, Giovannoni G. Multiple sclerosis—a review. Eur J Neurol. 2019;26(1):27–40. https://doi.org/10.1111/ene.13819.
Barin L, et al. The disease burden of multiple sclerosis from the individual and population perspective: which symptoms matter most? Mult Scler Relat Disord. 2018;25:112–21. https://doi.org/10.1016/j.msard.2018.07.013.
Lynning M, Hanehøj K, Karnøe Knudsen A, Skovgaard L. Self-Care activities among people with multiple sclerosis in denmark: use and user characteristics. Complement Med Res. 2017;24(4):240–5. https://doi.org/10.1159/000478262.
Skovgaard L. Use and users of complementary and alternative medicine among people with multiple sclerosis in Denmark. Dan Med J. 2016;63(1):B5159.
Skovgaard L, et al. Differences between users and non-users of complementary and alternative medicine among people with multiple sclerosis in Denmark: a comparison of descriptive characteristics. Scand J Public Health. 2013;41(5):492–9. https://doi.org/10.1177/1403494813481646.
Bergien SO, Petersen CM, Lynning M, Kristiansen M, Skovgaard L. Use of natural medicine and dietary supplements concomitant with conventional medicine among people with Multiple Sclerosis. Mult Scler Relat Disord. 2020;44:102197. https://doi.org/10.1016/j.msard.2020.102197.
Fitzgerald KC, et al. Diet quality is associated with disability and symptom severity in multiple sclerosis. Neurology. 2018;90(1):e1–11. https://doi.org/10.1212/WNL.0000000000004768.
Fitzgerald KC, et al. Sodium intake and multiple sclerosis activity and progression in BENEFIT. Ann Neurol. 2017;82(1):20–9. https://doi.org/10.1002/ana.24965.
Farinotti M, Vacchi L, Simi S, Di Pietrantonj C, Brait L, Filippini G. Dietary interventions for multiple sclerosis. Cochrane Database Syst Rev. 2012;12:CD004192. https://doi.org/10.1002/14651858.CD004192.pub3.
Lucas RM, Byrne SN, Correale J, Ilschner S, Hart PH. Ultraviolet radiation, vitamin D and multiple sclerosis. Neurodegen Dis Manag. 2015;5(5):413–24. https://doi.org/10.2217/nmt.15.33.
van der Mei IAF, Simpson SJ, Stankovich J, Taylor BV. Individual and joint action of environmental factors and risk of MS. Neurol Clin. 2011;29(2):233–55. https://doi.org/10.1016/j.ncl.2010.12.007.
Jelinek GA, Hadgkiss EJ, Weiland TJ, Pereira NG, Marck CH, van der Meer DM. Association of fish consumption and Ω 3 supplementation with quality of life, disability and disease activity in an international cohort of people with multiple sclerosis. Int J Neurosci. 2013;123(11):792–800. https://doi.org/10.3109/00207454.2013.803104.
AlAmmar WA, Albeesh FH, Ibrahim LM, Algindan YY, Yamani LZ, Khattab RY. ‘Effect of omega-3 fatty acids and fish oil supplementation on multiple sclerosis: a systematic review. Nutr Neurosci. 2021;24(7):569–79. https://doi.org/10.1080/1028415X.2019.1659560.
Platero JL, et al. The impact of coconut oil and epigallocatechin gallate on the levels of IL-6, anxiety and disability in multiple sclerosis patients. Nutrients. 2020. https://doi.org/10.3390/nu12020305.
Tredinnick AR, Probst YC. Evaluating the effects of dietary interventions on disease progression and symptoms of adults with multiple sclerosis: an umbrella review. Adv Nutr. 2020;11(6):1603–15. https://doi.org/10.1093/advances/nmaa063.
Gianfrancesco MA, et al. Obesity during childhood and adolescence increases susceptibility to multiple sclerosis after accounting for established genetic and environmental risk factors. Obes Res Clin Pract. 2014;8(5):e435-447. https://doi.org/10.1016/j.orcp.2014.01.002.
Abdollahpour I, et al. Dietary inflammatory index and risk of multiple sclerosis: findings from a large population-based incident case-control study. Clin Nutr. 2020;39(11):3402–7. https://doi.org/10.1016/j.clnu.2020.02.033.
Black LJ, Baker K, Ponsonby A-L, van der Mei I, Lucas RM, Pereira G. A higher Mediterranean diet score, including unprocessed red meat, is associated with reduced risk of central nervous system demyelination in a case-control study of Australian adults. J Nutr. 2019;149(8):1385–92. https://doi.org/10.1093/jn/nxz089.
Langer-Gould A, et al. Seafood, fatty acid biosynthesis genes, and multiple sclerosis susceptibility. Mult Scler. 2020;26(12):1476–85. https://doi.org/10.1177/1352458519872652.
Noormohammadi M, et al. MIND diet adherence might be associated with a reduced odds of multiple sclerosis: results from a case-control study. Neurol Ther. 2022;11(1):397–412. https://doi.org/10.1007/s40120-022-00325-z.
Rezaeimanesh N, Moghadasi AN, Sahraian MA, Eskandarieh S. Dietary risk factors of primary progressive multiple sclerosis: a population-based case-control study. Mult Scler Relat Disord. 2021. https://doi.org/10.1016/j.msard.2021.103233.
Rubin KH, et al. Intake of dietary fibre, red and processed meat and risk of late-onset Chronic Inflammatory Diseases: a prospective Danish study on the “diet, cancer and health” cohort. Int J Med Sci. 2020;17(16):2487–95. https://doi.org/10.7150/ijms.49314.
Pommerich UM, et al. Diet quality is not associated with late-onset multiple sclerosis risk—a Danish Cohort Study. Mult Scler Relat Disord. 2020;40:101968. https://doi.org/10.1016/j.msard.2020.101968.
Simpson-Yap S, et al. High Prudent diet factor score predicts lower relapse hazard in early multiple sclerosis. Mult Scler. 2020. https://doi.org/10.1177/1352458520943087.
Albrechtsen MT, Langeskov-Christensen M, Jørgensen MLK, Dalgas U, Hansen M. ‘Is diet associated with physical capacity and fatigue in persons with multiple sclerosis?—results from a pilot study. Mult Scler Relat Disord. 2020;40:101921. https://doi.org/10.1016/j.msard.2019.101921.
Black LJ, et al. Higher fish consumption and lower risk of central nervous system demyelination. Eur J Clin Nutr. 2020;74(5):818–24. https://doi.org/10.1038/s41430-019-0476-z.
Moravejolahkami AR, Paknahad Z, Chitsaz A. Association of dietary patterns with systemic inflammation, quality of life, disease severity, relapse rate, severity of fatigue and anthropometric measurements in MS patients. Nutr Neurosci. 2020;23(12):920–30. https://doi.org/10.1080/1028415X.2019.1580831.
Jakimovski D, et al. Dietary and lifestyle factors in multiple sclerosis progression: results from a 5-year longitudinal MRI study. J Neurol. 2019;266(4):866–75. https://doi.org/10.1007/s00415-019-09208-0.
Simpson-Yap S, Nag N, Probst Y, Jelinek G, Neate S. Higher-quality diet and non-consumption of meat are associated with less self-determined disability progression in people with multiple sclerosis: a longitudinal cohort study. Eur J Neurol. 2022;29(1):225–36. https://doi.org/10.1111/ene.15066.
Zuniga K, McAuley E. Considerations in selection of diet assessment methods for examining the effect of nutrition on cognition. J Nutr Health Aging. 2015;19(3):333–40. https://doi.org/10.1007/s12603-014-0566-5.
Plow M, Finlayson M. A qualitative study of nutritional behaviors in adults with multiple sclerosis. J Neurosci Nurs. 2012;44(6):337–50. https://doi.org/10.1097/JNN.0b013e3182682f9b.
Cordeiro F, et al. Barriers and negative nudges: exploring challenges in food journaling. In: Proceedings of the 33rd annual ACM conference on human factors in computing systems—CHI ’15, Seoul. Republic of Korea: ACM Press, pp. 1159–1162 (2015). https://doi.org/10.1145/2702123.2702155
Roman SN, Fitzgerald KC, Beier M, Mowry EM. Safety and feasibility of various fasting-mimicking diets among people with multiple sclerosis. Mult Scler Relat Disord. 2020;42:102149. https://doi.org/10.1016/j.msard.2020.102149.
Katz Sand I, et al. Randomized-controlled trial of a modified Mediterranean dietary program for multiple sclerosis: a pilot study. Mult Scler Relat Disord. 2019;36:101403. https://doi.org/10.1016/j.msard.2019.101403.
Reginald McDaniel H, et al. The effect of a polysaccharide-based multinutrient dietary supplementation regimen on infections and immune functioning in multiple sclerosis. J Diet Suppl. 2020;17(2):184–99. https://doi.org/10.1080/19390211.2018.1495675.
Lee D, Newell R, Ziegler L, Topping A. Treatment of fatigue in multiple sclerosis: a systematic review of the literature. Int J Nurs Pract. 2008;14(2):81–93. https://doi.org/10.1111/j.1440-172X.2008.00670.x.
Benlloch M, et al. Satiating effect of a ketogenic diet and its impact on muscle improvement and oxidation state in multiple sclerosis patients. Nutrients. 2019. https://doi.org/10.3390/nu11051156.
Fellows Maxwell K, et al. Lipid profile is associated with decreased fatigue in individuals with progressive multiple sclerosis following a diet-based intervention: results from a pilot study. PLoS ONE. 2019;14(6): e0218075. https://doi.org/10.1371/journal.pone.0218075.
Bromley L, Horvath PJ, Bennett SE, Weinstock-Guttman B, Ray AD. Impact of nutritional intake on function in people with mild-to-moderate multiple sclerosis. Int J MS Care. 2019;21(1):1–9. https://doi.org/10.7224/1537-2073.2017-039.
Azary S, et al. Contribution of dietary intake to relapse rate in early paediatric multiple sclerosis. J Neurol Neurosurg Psychiatry. 2018;89(1):28–33. https://doi.org/10.1136/jnnp-2017-315936.
Chen J, et al. Multiple sclerosis patients have a distinct gut microbiota compared to healthy controls. Sci Rep. 2016;6(1):28484. https://doi.org/10.1038/srep28484.
Yadav V, et al. Low-fat, plant-based diet in multiple sclerosis: a randomized controlled trial. Mult Scler Relat Disord. 2016;9:80–90. https://doi.org/10.1016/j.msard.2016.07.001.
Coe S, et al. A randomised double-blind placebo-controlled feasibility trial of flavonoid-rich cocoa for fatigue in people with relapsing and remitting multiple sclerosis. J Neurol Neurosurg Psychiatry. 2019;90(5):507–13. https://doi.org/10.1136/jnnp-2018-319496.
Mousavi-Shirazi-Fard Z, Mazloom Z, Izadi S, Fararouei M. The effects of modified anti-inflammatory diet on fatigue, quality of life, and inflammatory biomarkers in relapsing-remitting multiple sclerosis patients: a randomized clinical trial. Int J Neurosci. 2020. https://doi.org/10.1080/00207454.2020.1750398.
Bock M, Karber M, Kuhn H. Ketogenic diets attenuate cyclooxygenase and lipoxygenase gene expression in multiple sclerosis. EBioMedicine. 2018;36:293–303. https://doi.org/10.1016/j.ebiom.2018.08.057.
Brenton JN, et al. Phase II study of ketogenic diets in relapsing multiple sclerosis: safety, tolerability and potential clinical benefits. J Neurol Neurosurg Psychiatry. 2022;93(6):637–44. https://doi.org/10.1136/jnnp-2022-329074.
Wahls TL, et al. Impact of the Swank and Wahls elimination dietary interventions on fatigue and quality of life in relapsing-remitting multiple sclerosis: the WAVES randomized parallel-arm clinical trial. Mult Scler J Exp Transl Clin. 2021;7(3):20552173211035400. https://doi.org/10.1177/20552173211035399.
Esposito S, Bonavita S, Sparaco M, Gallo A, Tedeschi G. The role of diet in multiple sclerosis: a review. Nutr Neurosci. 2018;21(6):377–90. https://doi.org/10.1080/1028415X.2017.1303016.
Parks NE, Jackson-Tarlton CS, Vacchi L, Merdad R, Johnston BC. Dietary interventions for multiple sclerosis-related outcomes. Cochrane Database Syst Rev. 2020;5(5):CD004192. https://doi.org/10.1002/14651858.CD004192.pub4.
Valburg C, Sonti A, Stern JN, Najjar S, Harel A. Dietary factors in experimental autoimmune encephalomyelitis and multiple sclerosis: a comprehensive review. Mult Scler. 2020. https://doi.org/10.1177/1352458520923955.
Stoiloudis P, et al. The role of diet and interventions on multiple sclerosis: a review. Nutrients. 2022. https://doi.org/10.3390/nu14061150.
Halkjaer J, Tjønneland A, Overvad K, Sørensen TIA. Dietary predictors of 5-year changes in waist circumference. J Am Diet Assoc. 2009;109(8):1356–66. https://doi.org/10.1016/j.jada.2009.05.015.
Karnoe A. Development and feasibility test of a scale for patient-reported outcome measures in multiple sclerosis. Mult Scler J. 2019. https://doi.org/10.1177/1352458519844447.
Karnoe AK, Kayser L, Skovgaard L. Development and feasibility test of a scale assessing self-reported scale for assessing symptoms and functions in multiple sclerosis. Manuscript.
Fallaize R, Zenun Franco R, Pasang J, Hwang F, Lovegrove JA. Popular nutrition-related mobile apps: an agreement assessment against a UK reference method. JMIR Mhealth Uhealth. 2019;7(2): e9838. https://doi.org/10.2196/mhealth.9838.
Turner-McGrievy GM, Yang C-H, Monroe C, Pellegrini C, West DS. Is burden always bad? Emerging low-burden approaches to mobile dietary self-monitoring and the role burden plays with engagement. J Technol Behav Sci. 2021;6(3):447–55. https://doi.org/10.1007/s41347-021-00203-9.
Hammer GP, du Prel JB, Blettner M. Avoiding bias in observational studies: part 8 in a series of articles on evaluation of scientific publications. Dtsch Arztebl Int. 2009;106(41):664–8. https://doi.org/10.3238/arztebl.2009.0664
Meyer A, Spielmann L, Séverac F. ‘On how to not misuse hierarchical clustering on principal components to define clinically meaningful patient subgroups. Response to: “On using machine learning algorithms to define clinical meaningful patient subgroups” by Pinal-Fernandez and Mammen. Ann Rheum Dis. 2020;79(10):e129. https://doi.org/10.1136/annrheumdis-2019-215868.
Charrad M, Ghazzali N, Boiteau V, Niknafs A. NbClust: an R package for determining the relevant number of clusters in a data set. J Stat Softw. 2014;61:1–36.
Brumback BA. Fundamentals of causal inference, with R, vol. New York: CRC Press; 2022.
Textor J, van der Zander B, Gilthorpe MS, Liskiewicz M, Ellison GT. Robust causal inference using directed acyclic graphs: the R package “dagitty.” Int J Epidemiol. 2016;45(6):1887–94. https://doi.org/10.1093/ije/dyw341.
Shipley B. Cause and correlation in biology: a user’s guide to path analysis, structural equations and causal inference with R. Cambridge: Cambridge University Press; 2016.
Greifer N. WeightIt: weighting for covariate balance in observational studies. [Online]. https://cran.r-project.org/web/packages/WeightIt/index.html. Accessed 28 Jun 2022.
Cinelli C, Ferwerda J, Hazlett C. sensemakr: sensitivity analysis tools for regression models. [Online]. https://cran.r-project.org/web/packages/sensemakr/index.html. Accessed 8 Oct 2021.
Cinar O, Viechtbauer W. The poolr package for combining independent and dependent p values. J Stat Softw. 2022;101:1–42.
Ertaş Öztürk Y, Helvaci EM, Sökülmez Kaya P, Terzi M. Is Mediterranean diet associated with multiple sclerosis related symptoms and fatigue severity? Nutr Neurosci. 2022. https://doi.org/10.1080/1028415X.2022.2034241.
Di Majo D, et al. Ketogenic and modified mediterranean diet as a tool to counteract neuroinflammation in multiple sclerosis: nutritional suggestions. Nutrients. 2022. https://doi.org/10.3390/nu14122384.
Black LJ, Rowley C, Sherriff J, Pereira G, Ponsonby A-L, Lucas RM. A healthy dietary pattern associates with a lower risk of a first clinical diagnosis of central nervous system demyelination. Mult Scler. 2019;25(11):1514–25. https://doi.org/10.1177/1352458518793524.
Lee JE, Titcomb TJ, Bisht B, Rubenstein LM, Louison R, Wahls TL. A modified MCT-based ketogenic diet increases plasma β-hydroxybutyrate but has less effect on fatigue and quality of life in people with multiple sclerosis compared to a modified paleolithic diet: a waitlist-controlled, randomized pilot study. J Am Coll Nutr. 2020. https://doi.org/10.1080/07315724.2020.1734988.
Powell DJH, Liossi C, Schlotz W, Moss-Morris R. Tracking daily fatigue fluctuations in multiple sclerosis: ecological momentary assessment provides unique insights. J Behav Med. 2017;40(5):772–83. https://doi.org/10.1007/s10865-017-9840-4.
Romberg A, Ruutiainen J, Puukka P, Poikkeus L. Fatigue in multiple sclerosis patients during inpatient rehabilitation. Disabil Rehabil. 2008;30(19):1480–5. https://doi.org/10.1080/09638280701623687.
Kratz AL, Murphy SL, Braley TJ. Pain, fatigue, and cognitive symptoms are temporally associated within but not across days in multiple sclerosis. Arch Phys Med Rehabil. 2017;98(11):2151–9. https://doi.org/10.1016/j.apmr.2017.07.003.
Kim E, Lovera J, Schaben L, Melara J, Bourdette D, Whitham R. Novel method for measurement of fatigue in multiple sclerosis: Real-Time Digital Fatigue Score. J Rehabil Res Dev. 2010;47(5):477–84. https://doi.org/10.1682/jrrd.2009.09.0151.
Giunti G, Mylonopoulou V, Rivera Romero O. More stamina, a gamified mHealth solution for persons with multiple sclerosis: research through design. JMIR Mhealth Uhealth. 2018;6(3): e51. https://doi.org/10.2196/mhealth.9437.
Babbage DR, et al. MS energize: field trial of an app for self-management of fatigue for people with multiple sclerosis. Internet Interv. 2019;18: 100291. https://doi.org/10.1016/j.invent.2019.100291.
Greenhalgh J, Ford H, Long AF, Hurst K. The MS Symptom and Impact Diary (MSSID): psychometric evaluation of a new instrument to measure the day to day impact of multiple sclerosis. J Neurol Neurosurg Psychiatry. 2004;75(4):577–82. https://doi.org/10.1136/jnnp.2003.020529.
Motl RW, et al. Exercise in patients with multiple sclerosis. Lancet Neurol. 2017;16(10):848–56. https://doi.org/10.1016/S1474-4422(17)30281-8.
Westergaard K, Reitzel SB, Krogh C, Lynning M, Olsgaard SB, Skovgaard L. Potentials and barriers of using digital tools for collecting daily measurements in multiple sclerosis research. Digit Health. 2021;7:205520762110555. https://doi.org/10.1177/20552076211055552.
McKeon A, McCue M, Skidmore E, Schein M, Kulzer J. Ecological momentary assessment for rehabilitation of chronic illness and disability. Disabil Rehabil. 2018;40(8):974–87. https://doi.org/10.1080/09638288.2017.1280545.
Dunton GF. Ecological momentary assessment in physical activity research. Exerc Sport Sci Rev. 2017;45(1):48–54. https://doi.org/10.1249/JES.0000000000000092.
Wendrich K, van Oirschot P, Martens MB, Heerings M, Jongen PJ, Krabbenborg L. Toward digital self-monitoring of multiple sclerosis. Int J MS Care. 2019;21(6):282–91. https://doi.org/10.7224/1537-2073.2018-083.
Brichetto G, Pedullà L, Podda J, Tacchino A. Beyond center-based testing: understanding and improving functioning with wearable technology in MS. Mult Scler. 2019;25(10):1402–11. https://doi.org/10.1177/1352458519857075.
Damanabi S, Salimzadeh Z, Kalankesh LR, Shaafi S, Ferdousi R. Exploring self-management needs of persons with multiple sclerosis: a qualitative study for mobile application development. Int J MS Care. 2022;24(1):1–7. https://doi.org/10.7224/1537-2073.2019-129.
Stephens S, Schneiderman JE, Finlayson M, Berenbaum T, Motl RW, Yeh EA. Feasibility of a theory-informed mobile app for changing physical activity in youth with multiple sclerosis. Mult Scler Relat Disord. 2022;58:103467. https://doi.org/10.1016/j.msard.2021.103467.
Ayobi A. Informing the design of personal informatics technologies for unpredictable chronic conditions. In: Extended abstracts of the 2018 CHI conference on human factors in computing systems, Montreal, QC, Canada: ACM, Apr. 2018, pp. 1–4. https://doi.org/10.1145/3170427.3173025.
van Oirschoti P, et al. Self-monitoring of mobility, signal processing speed, physical activity and sleep by persons with multiple sclerosis. 2018.
Ziebland S, et al. Examining the role of patients’ experiences as a resource for choice and decision-making in health care: a creative, interdisciplinary mixed-method study in digital health. Southampton: NIHR Journals Library; 2016. https://doi.org/10.3310/pgfar04170.
Gulick EE, Namey M, Halper J. Monitoring my multiple sclerosis: a patient-administered health-assessment scale. Int J MS Care. 2011;13(3):137–45. https://doi.org/10.7224/1537-2073-13.3.137.
Kratz AL, Fritz NE, Braley TJ, Scott EL, Foxen-Craft E, Murphy SL. Daily temporal associations between physical activity and symptoms in multiple sclerosis. Ann Behav Med. 2019;53(1):98–108. https://doi.org/10.1093/abm/kay018.
Cederberg KL, Balto JM, Motl RW. Self-regulatory strategies as correlates of physical activity behavior in persons with multiple sclerosis. Arch Phys Med Rehabil. 2018;99(5):920–6. https://doi.org/10.1016/j.apmr.2017.12.037.
Powell DJH, Moss-Morris R, Liossi C, Schlotz W. Circadian cortisol and fatigue severity in relapsing-remitting multiple sclerosis. Psychoneuroendocrinology. 2015;56:120–31. https://doi.org/10.1016/j.psyneuen.2015.03.010.
Zhang Y, Taylor BV, Simpson SJ, Blizzard L, Palmer AJ, van der Mei I. Validation of 0–10 MS symptom scores in the Australian multiple sclerosis longitudinal study. Mult Scler Relat Disord. 2019;39:101895. https://doi.org/10.1016/j.msard.2019.101895.
Maddocks M, Granger CL. Measurement of physical activity in clinical practice and research: advances in cancer and chronic respiratory disease. Curr Opin Support Palliat Care. 2018;12(3):219–26. https://doi.org/10.1097/SPC.0000000000000372.
Kocherginsky M, Huisingh-Scheetz M, Dale W, Lauderdale DS, Waite L. Measuring physical activity with hip accelerometry among U.S. older adults: how many days are enough? PLoS ONE. 2017;12(1):e0170082. https://doi.org/10.1371/journal.pone.0170082.
Rosenman R, Tennekoon V, Hill LG. Measuring bias in self-reported data. Int J Behav Healthc Res. 2011;2(4):320–32. https://doi.org/10.1504/IJBHR.2011.043414.
De Castro JM. Methodology, correlational analysis, and interpretation of diet diary records of the food and fluid intake of free-living humans. Appetite. 1994;23(2):179–92. https://doi.org/10.1006/appe.1994.1045.
Acknowledgements
We acknowledge all the participants who have invested a large amount of energy in the registration of diet and symptom data.
Funding
This study was funded by The Danish MS Society and The Innovation Fund Denmark (grant: 5016-00143B). The publication fee was funded by the authors.
Author Contributions
Lasse Skovgaard: drafting/revising the manuscript, study concept or design, analysis or interpretation of data, accepts responsibility for conduct of research and final approval, study supervision. Philipp Trénel: revising the manuscript, analysis or interpretation of data, accepts responsibility for conduct of research and final approval, statistical analysis. Lasse Skovgaard and Philipp Trénel share the first authorship. Katrine Westergaard: revising the manuscript, analysis or interpretation of data, accepts responsibility for conduct of research and final approval, statistical analysis. Astrid Karnøe Knudsen: revising the manuscript, analysis or interpretation of data, accepts responsibility for conduct of research and final approval, study supervision.
Disclosures
Lasse Skovgaard has nothing to disclose. Philipp Trénel has nothing to disclose. Katrine Westergaard has nothing to disclose. Astrid Karnøe Knudsen has nothing to disclose.
Compliance with Ethics Guidelines
In this study, no biological material or medical devices were used and the participants were not subjected to any kind of diagnostics or treatment. The study was registered and approved with the Danish Data Protection Agency. Informed participation consent was obtained (including consent for participation and publication) for all participants.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Skovgaard, L., Trénel, P., Westergaard, K. et al. Dietary Patterns and Their Associations with Symptom Levels Among People with Multiple Sclerosis: A Real-World Digital Study. Neurol Ther 12, 1335–1357 (2023). https://doi.org/10.1007/s40120-023-00505-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40120-023-00505-5