Abstract
Cerebral venous thrombosis (CVT) is a rare entity that remains a diagnostic challenge due to various clinical manifestations and a wide variety of causative agents. Local infections, such as acute (AOM) or chronic otitis media, can play a role in the pathogenesis of CVT. The proximity of the tympanic cavity and temporal bone air cells to the dural venous sinuses predisposes them to secondary thrombosis. The release of inflammatory cytokines and activation of the coagulation pathway in the middle ear space in response to infection may trigger the thrombotic mechanism in venous sinuses of the central nervous system. There is no consensus in the literature concerning the treatment of otogenic cerebral venous sinus thrombosis (CVST). Both the extent of the surgery and the use of anticoagulants are disputable. The aim of the study was to provide a thorough analysis of the literature concerning CVST in patients with AOM and acute mastoiditis (AM). The current surgical and conventional treatment strategies are presented. Special attention has been attached to the predisposing factors, the extent of the surgery, and the role of anticoagulants in the treatment of septic otogenic CVST.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Each pediatric patient without typical otomastoid complaints but presenting symptoms of raised intracranial pressure and otitis media should be suspected for otogenic CVST (OCVST). |
The extent of the sigmoid sinus pathology is not proportional to the involvement of the bony sinus plate. |
The role of contralateral compensatory drainage as a factor predisposing to OCVST needs further studies. |
The routine screening for thrombophilia is disputable and requires further objective verification. |
The benefits of anticoagulant therapy appear to outweigh the potential risks, but there is no established regimen concerning indications, the duration, or form of the treatment. |
Introduction
Cerebral venous thrombosis (CVT) is a rare entity but with the potentially serious consequences. Headaches, neurologic deficits, and seizures have been reported in more than 50% of children, whereas death has occurred in 9–29% of pediatric cases [1,2,3]. CVT remains a diagnostic challenge due to various clinical manifestations and a wide variety of causative agents. Local infections, such as acute (AOM) or chronic otitis media (COM), can play a role in the pathogenesis of CVT. It is considered that CVT may be triggered by the release of inflammatory cytokines and the activation of the coagulation pathway in the middle ear space in response to infection [4]. The proximity of the tympanic cavity and temporal bone air cells to the dural venous sinuses predisposes them to secondary thrombosis [5]. The incidence of acute mastoiditis (AM) is estimated at 3.5–4.2 per 100,000 people/year. Septic lateral sinus thrombosis (LST) develops in 0–3% of patients with AM [6,7,8,9]. Among all the pediatric patients with CVT, otogenic causes are responsible for less than 10% of cases. In contrast, a primary thrombus formation within the dural sinus is called a nonseptic LST [5, 10]. This difference is of utmost importance, as the therapy strategies are not the same. There is no consensus in the literature concerning the treatment of otogenic cerebral venous sinus thrombosis (OCVST). Both the extent of the surgery and the use of anticoagulants are disputable.
The aim of this study was to provide a thorough analysis of the literature concerning cerebral venous sinus thrombosis (CVST) in patients with AOM and AM. The current surgical and conventional treatment strategies have been presented. Special attention has been attached to the role of anticoagulants in septic CVST.
Methods
A review of the literature concerning cases with OCVST was carried out. PubMed database was searched for literature published in English on the subject. Databases were searched using Medical Subject Headings (MeSH) terms “acute otitis media” or “mastoiditis” with one of the following terms: “cerebral venous thrombosis”, “lateral sinus thrombosis”, “sigmoid sinus thrombosis”, “transverse sinus thrombosis” or “petrosal sinus thrombosis” and combined with the term “children”. The following exclusion criteria were implemented: publication before 2000, isolated case reports, and series of cases of < 5 patients, primary CVT, reports concerning solely adult patients, studies providing no data or insufficient data on the type of intracranial complication, studies providing no data or insufficient data on the method of treatment, animal reports, non-English language, or only abstract available.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Results
The search process in the PubMed database identified a total of 204 results. Forty-four of them met the inclusion criteria and were included for further analysis (Fig. 1). The main disputable issues concerning pediatric OCVST have been identified, discussed, and summarized. The list of the most important articles included in our analysis is presented in Table 1.
Discussion
Nomenclature
The literature analysis revealed a significant inconsistency in the nomenclature regarding the cerebral venous system. Many authors customarily used the term “lateral sinus” to describe the sigmoid sinus (SS) or the transverse sinus (TS). The term lateral sinus (LS) was also used as a description of a complex of sigmoid and transverse sinuses. Such an inconsistency influences the unequivocal interpretation of the published data. According to Tubbs [13], the sigmoid sinus and the transverse sinus are anatomically different structures and terms. Therefore, these terms should be distinguished and the nomenclature respected in further studies.
General Characteristic and Demographics
Septic otogenic CVST in children is a rare entity but with potential devastating neurological consequences. Nevertheless, only one mortality was reported in a group of reviewed 104 patients [14]. Wong et al. stressed that CVST was twice as common in males [9]. The lateral sinus thrombosis is thought to occur slightly more commonly on the right side [9, 14]. The average time from the onset of symptoms to hospital admission was 11 days [14].
Symptoms and Clinical Findings
The symptomatology of septic CVST is uncharacteristic. Severe headache is the most common presenting symptom. Except from that, otalgia, “picket-fence” fever, vomiting, pain in the neck or neck stiffness, and papilloedema may be observed [5, 14, 15]. Typical otoscopic findings confirm AOM, whereas an oedema in the postauricular region with tenderness over mastoid are pathognomonic of mastoiditis. Internal jugular vein thrombosis can be suspected during the palpation of the neck along the sternocleidomastoid muscle [5]. Examining the fundus oculi reveals papilloedema, and sometimes retinal hemorrhage. Symptoms of intracranial hypertension in the case of CVT include headache, vision deterioration, and vomiting [15]. Strabismus and sixth cranial nerve palsy were also reported among neurologic findings [15].
A wide variety of bacterial flora including bacteroides, Staphylococcus, Enterobacteriaceae, Proteus, Pseudomonas, and other species have been identified as etiological factors [5]. The conclusion from the review by Au et al. was that only 46% of cultures were positive [14]. Vishawanatha et al. stated that a high percentage of negative cultures could stem from preadmission antimicrobial therapy [5], which may mask the typical symptoms of septic CVST.
Recent studies of Coudert et al. have revealed a significant association between Fusobacterium necrophorum and thrombotic complications of AM [16]. F. necrophorum presented a specific prothrombotic activity by producing cytokines and hemagglutinin supporting inflammation and aggregation of platelets [17, 18]. Ziv et al. revealed that F. necrophorum was statistically associated with multiple intracranial complications of AM [19]. Ichord regarded F. necrophorum as a main risk factor for CVST in children [20].
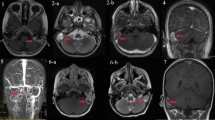
Imaging
Many researchers agree that magnetic resonance imaging or magnetic resonance venography (MRI or MRV) should become a gold standard in cases suspected of CVT [8, 21,22,23]. According to a study by Au et al., MRI is more specific than CT in thrombus detection (sensitivity 100% vs 87%) [14]. Due to the essential role of surgery in treatment of AM and OCVST, it seems reasonable to perform MRI with contrast-enhanced CT for the supreme evaluation of both cerebral and otologic pathology [5]. Moreover, MRI enables the differential diagnosis and visualization of some dural venous sinus anatomical variants, including not only hypoplasia or aplasia of the sinus but more challenging cases with intrasinus septum or prominent arachnoid granulations [8]. The importance of serial imaging with MRI, MRV, or CT venography in patients suspected of thrombus progression is emphasized [24].
Unfortunately, the main disadvantage is the availability of the emergency MRI which has been highlighted in the literature by numerous authors [1, 11, 25]. Ghosh et al. stressed that the high index of suspicion is required in children with raised intracranial pressure (ICP) and a history of prior ear pain or AOM even in the absence of typical otomastoid complaints [8]. This remark is extremely important to make clinicians aware that AM is not necessary for OCVST to occur.
Predisposing Factors and Controversies
Knowing that sigmoid sinus thrombosis may be a silent complication [24, 26], the predisposing factors should be taken into consideration.
Venous Drainage Pattern Asymmetry (VDPA)
VDPA is frequently revealed on imaging. Csákányi et al. claim that atresia or hypoplasia of the transverse sinuses is not uncommon [11]. In cases of a dominant sinus occlusion, the clinical signs of elevated ICP are more severe. Durgun et al. reported that right-sided sinuses are the dominant ones in 41% of the population [27]. Similar observations were published by Widjaja and Gritffiths [28]. The anatomic study conducted by Leach et al. revealed asymmetric transverse sinuses were in 49% of participants, with a complete or partial absence of one transverse sinus in 20% of individuals [29]. The other attribute of cerebral sinuses influencing the potential course of the CVT is the lack of valves, which favors thrombus propagation to other sinuses and to the internal jugular vein [25]. Zanoletti et al. regard the form of protective mechanism as showing that the cerebral sinuses invert their venous flow when an acute obstruction occurs in the sigmoid-jugular system [6]. They claim that a compensatory drainage guarantees the function of the whole system. Moreover, the authors conclude that very few cases of unplanned sigmoid sinus occlusion have had serious clinical consequences, and even unplanned sacrifice of the sigmoid sinus has never reportedly been a problem per se [6].
Thrombophilia
Some authors have claimed that 50% of patients with CVST had a previously asymptomatic prothrombotic state related to one or more of the following: protein C and S deficiency, anticardiolipin antibodies, antithrombin III, or prothrombotic gene mutations (MTHFR, factor V Leiden, prothrombin 20210) [3, 30]. In contrast, the favored role of thrombophilia in CVST was considered controversial in other studies [8, 31, 32]. Scorpecci et al. reported that more than 90% of children in their study had genetic abnormalities associated with thrombophilia [12]. Other authors have assessed the prevalence of thrombophilia among children with OLST ranging from 10 to 78% [33] or even higher [34]. Some authors consider the favored role of polymorphism of the MTHFR gene still controversial [8, 31, 32], but others recognize it as a significant prothrombotic factor in OLST [34, 35]. The type of thrombophilia did not appear to be predictive of short- or long-term OLST resolution [12].
Others
A few more preoperative non-anatomical conditions have been indicated in the literature as factors predisposing to OCVST: cardiac disease, collagen tissue disorders, and other than thrombophilia hematological abnormalities [3, 24].
Treatment
The literature review revealed no controlled studies concerning this issue of OCVST. Due to the lack of evidence-based reports, Scorpecci et al. are skeptical to recommend surgical treatment [9, 12]. Christensen et al. considered the variable clinical manifestation and the rarity of CVST unfavorable factors in establishing the optimal therapeutic management in these patients [36].
Surgical Treatment
Most authors consider surgery to be mandatory [11, 32, 37], but the extent of the surgery differs between them. Many ENT surgeons have performed prompt cortical mastoidectomy with removal of the SS plate (or its remnants) and granulation tissue adjacent to the SS [11, 14, 36], with subsequent conservative therapy [11, 37,38,39]. In contrast, Scorpecci et al. stated that mastoidectomy should no longer be indicated in cases where lateral sinus thrombosis is associated with a non-erosive mastoiditis [12]. It sounds controversial in relation to the study of Ooi [37]. That author highlighted that the extent of the SS pathology is not proportional to the involvement of the bony sinus plate. These observations are consistent with the results of Csákányi al., as they revealed that an epidural abscess can frequently be identified under an apparently intact SS plate [11]. The facts mentioned above shed a new light on the potential recommendations concerning the extent of the surgical procedure with the obligatory decompression of the SS during mastoidectomy.
Surprisingly, one of the studies reported that < 50% of patients had concurrent myringotomy with ventilation tube insertion [14]. The reason is unclear as this procedure is considered a natural step in the treatment of AM.
Au et al. reported surgical manipulations of the thrombosed sinus in almost 50% of individuals [14]. In that group, a needle aspiration was performed in 54.9% of patients, thrombectomy in 47.1%, and internal jugular vein ligation in 7.8%. Recently, the role of these procedures has apparently diminished. Csákányi et al. argued that surgical confirmation of the thrombus was unnecessary in children without persisting septicemia because of the wide availability of imaging [11]. In cases of signs of persisting septicemia, some authors advise removal of the infected clot [38].
The literature also indicates the marginal role of internal jugular vein (IJV) ligation. Recent authors consider IJV ligation redundant in cases of mastoidectomy and SS exposition supported by adequate antibiotic therapy [23]. Some authors see the role of IJV ligation in cases of embolization or septicemia not responding to conventional and initial surgical treatment [5].
Conventional Treatment and Anticoagulants
Some authors support a less invasive therapeutic approach [40] or even question operative management [12].
Guidance on the management of CVST in children was published by the British Society of Haematology in 2009 [33]. Anticoagulation treatment with low-molecular-weight heparin (LMWH) was recommended in each case apart from the situation of associated intracranial hemorrhage. Researchers have stressed that anticoagulants prevented thromboembolic events, decreased the risk of death and severe neurologic consequences, and reduced the recurrence of thrombosis within 6 months [32, 41, 42]. Nevertheless, the guidance of the British Society of Haematology refers to all causes of pediatric CVST and is unspecific as to otological cause, which is the major limitation of this document.
Anticoagulation with heparin followed by oral anticoagulation is considered the traditional therapy for CVT [24], and is recommended by pediatric neurologists and hematologists [31,32,33]. Surprisingly, a recent systematic review revealed that only 60% of children with OLST received anticoagulation [9], and, in the report by Au et al., 57.4% patients received it [14]. The routine use in otogenic septic CVST is still disputable among otorhinolaryngologists [8, 14].
A distinctive position on this issue was presented by Scorpecci et al. [14]. The authors proposed a treatment protocol including intravenous broad-spectrum antibiotics and anticoagulation with LMWH in all patients. They recommended mastoidectomy only on a case-to-case basis because of insufficient evidence on the effectiveness of surgical treatment [14].
Several authors have questioned the importance of anticoagulation, due to the possible risk for hemorrhage [8, 31, 32, 39]. Other researchers recommend their use only in cases of OCVST with proximal (to IJV) or retrograde thrombus progression (to TS, petrosal sinus or cavernous sinus) or the presence on initial imaging [37, 43]. Bradley et al. suggested introducing anticoagulants in the presence of persistent fever, neurologic changes, and embolic events [43].
The recommended therapy duration with anticoagulants is still disputable in the literature. Scorpecci et al. suggested continuing the treatment for at least 2 months to the first MRI control [14]. They advised basing the decision of treatment duration on comprehensive thrombophilia screening (including MTHFR mutations) in patients with OCVST. This allows the estimation of the risk for thrombosis recurrence and establishes future antithrombotic prophylaxis [14]. Coudert et al. claim that the duration of therapy should depend on the initial extent of the thrombosis and imaging studies performed 6 and 12 weeks after surgery [16]. Nevertheless, the type of thrombophilia does not influence the perspectives of otogenic CVST resolution, hence international guidelines do not recommend any modifications of treatment protocols [1, 33].
Endovascular Treatment
The endovascular treatment of CVST using thrombolysis (urokinase, streptokinase) and mechanical thrombectomy have been reported in a few case reports or small case series. Dentali et al. claim that there is a severe risk of intracranial hemorrhage and mortality in this method [44]. Capecchi et al. indicated that the published data were unconvincing regarding the safety of thrombolysis and endovascular treatment in cases of CVST [45]. No data concerning endovascular treatment of otogenic CVST are available in the literature.
Treatment Outcome and Recanalization
Zanoletti et al. claim that symptoms of CVST are usually self-limiting and rarely life-threatening, with a good response to conservative treatment [6, 24]. Many authors have reported the rapid resolution of symptoms after initial treatment [14, 26]. An interesting observation was published by Rosdy et al. in 2014. The authors revealed that clinical signs of elevated intracranial pressure had transiently worsened postoperatively [25]. Considering the results of these studies, a more reliable indicator of recovery should be sought. Recanalization of the affected venous sinus after 6 months seems to be widely recognized in the literature. In the majority of cases, recanalization may be expected in 2–5 months [11]. Scorpecci et al. proposed scheduled postoperative monitoring with imaging studies to assess the resolution of thrombosis [14].
Some authors have stated that sinuses usually recanalize spontaneously even without clot evacuation after simple mastoidectomy and antimicrobial treatment [46]. According to a study published by Neilan et al., spontaneous sinus recanalization was observed in 52.9% of cases. These rates were higher (although insignificantly) for patients with additional anticoagulation in their group (66.7%) [46]. Au et al. presented higher percentages of 75% and 84% for non-anticoagulated and additionally anticoagulated patients, respectively [14]. In contrast, Chalmers et al. stated that there was no evidence that anticoagulation improves the rate of recanalization [33]. Nevertheless, some limitations for the interpretation of these data exist. The degree of recanalization (partial or complete), unstandardized timing of imaging during follow-up, and the lack of standard protocols for anticoagulation treatment should be taken into consideration.
Conclusions and Future Studies
The extent of sigmoid sinus pathology is not proportional to the involvement of the bony sinus plate. Each pediatric patient without typical otomastoid complaints but presenting symptoms of raised intracranial pressure and otitis media should be suspected for otogenic CVST. The role of contralateral compensatory drainage as a factor predisposing to OCVST needs further studies. The routine screening for thrombophilia is disputable and requires further objective verification. The use of anticoagulant therapy in otogenic CVST remains controversial. The benefits appear to outweigh the potential risks, but there is no established regimen concerning indications, the duration, and the form of the treatment.
References
Monagle P, Chan AKC, Goldenberg NA, Ichord RN, Journeycake JM, Nowak-Göttl U, Vesely SK. Antithrombotic therapy in neonates and children: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e737S–801S. https://doi.org/10.1378/chest.11-2308(Erratum in: Chest. 2014; 146(6):1694. Dosage error in article text. Erratum in: Chest. 2014; 146(5):1422).
deVeber G, Andrew M, Adams C, Bjornson B, Booth F, Buckley DJ, Camfield CS, David M, Humphreys P, Langevin P, MacDonald EA, Gillett J, Meaney B, Shevell M, Sinclair DB, Yager J, Canadian Pediatric Ischemic Stroke Study Group. Cerebral sinovenous thrombosis in children. N Engl J Med. 2001;345(6):417–23. https://doi.org/10.1056/NEJM200108093450604.
Sébire G, Tabarki B, Saunders DE, Leroy I, Liesner R, Saint-Martin C, Husson B, Williams AN, Wade A, Kirkham FJ. Cerebral venous sinus thrombosis in children: risk factors, presentation, diagnosis and outcome. Brain. 2005;128(Pt 3):477–89. https://doi.org/10.1093/brain/awh412.
Levi M, Keller TT, van Gorp E, ten Cate H. Infection and inflammation and the coagulation system. Cardiovasc Res. 2003;60(1):26–39. https://doi.org/10.1016/s0008-6363(02)00857-x.
Viswanatha B, Thriveni CN, Naseeruddin K. Nonseptic and septic lateral sinus thrombosis: a review. Indian J Otolaryngol Head Neck Surg. 2014;66(Suppl 1):10–5. https://doi.org/10.1007/s12070-011-0422-4.
Zanoletti E, Cazzador D, Faccioli C, Sari M, Bovo R, Martini A. Intracranial venous sinus thrombosis as a complication of otitis media in children: critical review of diagnosis and management. Int J Pediatr Otorhinolaryngol. 2015;79(12):2398–403. https://doi.org/10.1016/j.ijporl.2015.10.059.
Anthonsen K, Høstmark K, Hansen S, Andreasen K, Juhlin J, Homøe P, Caye-Thomasen P. Acute mastoiditis in children: a 10-year retrospective and validated multicenter study. Pediatr Infect Dis J. 2013;32(5):436–40. https://doi.org/10.1097/INF.0b013e31828abd13.
Ghosh PS, Ghosh D, Goldfarb J, Sabella C. Lateral sinus thrombosis associated with mastoiditis and otitis media in children: a retrospective chart review and review of the literature. J Child Neurol. 2011;26(8):1000–4. https://doi.org/10.1177/0883073811401745.
Wong BY, Hickman S, Richards M, Jassar P, Wilson T. Management of paediatric otogenic cerebral venous sinus thrombosis: a systematic review. Clin Otolaryngol. 2015;40(6):704–14. https://doi.org/10.1111/coa.12504.
Rosen A, Scher N. Nonseptic lateral sinus thrombosis: the otolaryngologic perspective. Laryngoscope. 1997;107(5):680–3. https://doi.org/10.1097/00005537-199705000-00023.
Csákányi Z, Rosdy B, Kollár K, Móser J, Kovács E, Katona G. Timely recanalization of lateral sinus thrombosis in children: should we consider hypoplasia of contralateral sinuses in treatment planning? Eur Arch Otorhinolaryngol. 2013;270(7):1991–8. https://doi.org/10.1007/s00405-012-2258-2.
Scorpecci A, Massoud M, Giannantonio S, Zangari P, Lucidi D, Martines F, Foligno S, Di Felice G, Minozzi A, Luciani M, Marsella P. Otogenic lateral sinus thrombosis in children: proposal of an experience-based treatment flowchart. Eur Arch Otorhinolaryngol. 2018;275(8):1971–7. https://doi.org/10.1007/s00405-018-5033-1.
Anatomy, imaging and surgery of the intracranial dural venous sinuses—Ed. R. Shane Tubbs. Elsevier; 2020.
Au JK, Adam SI, Michaelides EM. Contemporary management of pediatric lateral sinus thrombosis: a twenty year review. Am J Otolaryngol. 2013;34(2):145–50. https://doi.org/10.1016/j.amjoto.2012.09.011.
Havalı C, İnce H, Gündoğdu EB, Gürkaş E, Karal Y, Ekici A, Gündoğdu E. The management of elevated intracranial pressure and sinus vein thrombosis associated with mastoiditis: the experience of eighteen patients. Childs Nerv Syst. 2022;38(2):421–8. https://doi.org/10.1007/s00381-021-05402-6.
Coudert A, Fanchette J, Regnier G, Delmas J, Truy E, Nicollas R, Akkari M, Couloignier V, Ayari-Khalfallah S. Fusobacterium necrophorum, a major provider of sinus thrombosis in acute mastoiditis: a retrospective multicentre paediatric study. Clin Otolaryngol. 2020;45(2):182–9. https://doi.org/10.1111/coa.13478.
Holm K, Frick IM, Björck L, Rasmussen M. Activation of the contact system at the surface of Fusobacterium necrophorum represents a possible virulence mechanism in Lemièrre’s syndrome. Infect Immun. 2011;79(8):3284–90. https://doi.org/10.1128/IAI.05264-11. (Erratum in: Infect Immun. 2015; 83(11):4451).
Shamriz O, Engelhard D, Temper V, Revel-Vilk S, Benenson S, Brooks R, Tenenbaum A, Stepensky P, Koplewitz B, Kaufmann M, Averbuch D. Infections caused by Fusobacterium in children: a 14-year single-center experience. Infection. 2015;43(6):663–70. https://doi.org/10.1007/s15010-015-0782-x.
Ziv O, Sapir A, Leibovitz E, Kordeluk S, Kaplan DM, El-Saied S. Post-operative clinical course in children undergoing mastoidectomy due to complicated acute mastoiditis. Eur Arch Otorhinolaryngol. 2022;279(8):3891–7. https://doi.org/10.1007/s00405-021-07149-x.
Ichord R. Cerebral sinovenous thrombosis. Front Pediatr. 2017;5:163. https://doi.org/10.3389/fped.2017.00163.
Vieira JP, Luis C, Monteiro JP, Temudo T, Campos MM, Quintas S, Nunes S. Cerebral sinovenous thrombosis in children: clinical presentation and extension, localization and recanalization of thrombosis. Eur J Paediatr Neurol. 2010;14(1):80–5. https://doi.org/10.1016/j.ejpn.2008.12.004.
Dlamini N, Billinghurst L, Kirkham FJ. Cerebral venous sinus (sinovenous) thrombosis in children. Neurosurg Clin N Am. 2010;21(3):511–27. https://doi.org/10.1016/j.nec.2010.03.006.
Viswanatha B. Lateral sinus thrombosis with cranial nerves palsies. Int J Pediatr Otorhinolaryngol Extra. 2007;2(3):165–8. https://doi.org/10.1016/j.pedex.2007.05.001.
Zanoletti E, Cazzador D, Faccioli C, Martini A, Mazzoni A. Closure of the sigmoid sinus in lateral skull base surgery. Acta Otorhinolaryngol Ital. 2014;34(3):184–8.
Rosdy B, Csákányi Z, Kollár K, Móser J, Mellár M, Kulcsár A, Kovács É, Várallyay G, Katona G. Visual and neurologic deterioration in otogenic lateral sinus thrombosis: 15 year experience. Int J Pediatr Otorhinolaryngol. 2014;78(8):1253–7. https://doi.org/10.1016/j.ijporl.2014.05.001.
Zanoletti E, Marioni G. Pediatric otogenic lateral sinus thrombosis: focus on the prognostic role of contralateral venous drainage. Eur Arch Otorhinolaryngol. 2019;276(3):919–20. https://doi.org/10.1007/s00405-019-05316-9.
Durgun B, Ilglt ET, Cizmeli MO, Atasever A. Evaluation by angiography of the lateral dominance of the drainage of the dural venous sinuses. Surg Radiol Anat. 1993;15(2):125–30. https://doi.org/10.1007/BF01628311.
Widjaja E, Griffiths PD. Intracranial MR venography in children: normal anatomy and variations. Am J Neuroradiol. 2004;25(9):1557–62.
Leach JL, Fortuna RB, Jones BV, Gaskill-Shipley MF. Imaging of cerebral venous thrombosis: current techniques, spectrum of findings, and diagnostic pitfalls. Radiographics. 2006; 26 Suppl 1:S19–41; discussion S42–3. doi: https://doi.org/10.1148/rg.26si055174. PMID: 17050515.
Galgano MA, Deshaies EM. An update on the management of pseudotumor cerebri. Clin Neurol Neurosurg. 2013;115(3):252–9. https://doi.org/10.1016/j.clineuro.2012.11.018.
Sitton MS, Chun R. Pediatric otogenic lateral sinus thrombosis: role of anticoagulation and surgery. Int J Pediatr Otorhinolaryngol. 2012;76(3):428–32. https://doi.org/10.1016/j.ijporl.2011.12.025.
Novoa E, Podvinec M, Angst R, Gürtler N. Paediatric otogenic lateral sinus thrombosis: therapeutic management, outcome and thrombophilic evaluation. Int J Pediatr Otorhinolaryngol. 2013;77(6):996–1001. https://doi.org/10.1016/j.ijporl.2013.03.030.
Chalmers E, Ganesen V, Liesner R, Maroo S, Nokes T, Saunders D, Williams M, British Committee for Standards in Haematology. Guideline on the investigation, management and prevention of venous thrombosis in children. Br J Haematol. 2011;154(2):196–207. https://doi.org/10.1111/j.1365-2141.2010.08543.x.
Oestreicher-Kedem Y, Raveh E, Kornreich L, Yaniv I, Tamary H. Prothrombotic factors in children with otitis media and sinus thrombosis. Laryngoscope. 2004;114(1):90–5. https://doi.org/10.1097/00005537-200401000-00015.
Ulanovski D, Yacobovich J, Kornreich L, Shkalim V, Raveh E. Pediatric otogenic sigmoid sinus thrombosis: 12-Year experience. Int J Pediatr Otorhinolaryngol. 2014;78(6):930–3. https://doi.org/10.1016/j.ijporl.2014.03.016.
Christensen N, Wayman J, Spencer J. Lateral sinus thrombosis: a review of seven cases and proposal of a management algorithm. Int J Pediatr Otorhinolaryngol. 2009;73(4):581–4. https://doi.org/10.1016/j.ijporl.2008.12.004.
Ooi EH, Hilton M, Hunter G. Management of lateral sinus thrombosis: update and literature review. J Laryngol Otol. 2003;117(12):932–9. https://doi.org/10.1258/002221503322683795.
Lee JH, Choi SJ, Park K, Choung YH. Managements for lateral sinus thrombosis: does it need the ligation of internal jugular vein or anticoagulants? Eur Arch Otorhinolaryngol. 2009;266(1):51–8. https://doi.org/10.1007/s00405-008-0724-7.
Seven H, Ozbal AE, Turgut S. Management of otogenic lateral sinus thrombosis. Am J Otolaryngol. 2004;25(5):329–33. https://doi.org/10.1016/j.amjoto.2004.04.005.
Manolidis S, Kutz JW Jr. Diagnosis and management of lateral sinus thrombosis. Otol Neurotol. 2005;26(5):1045–51. https://doi.org/10.1097/01.mao.0000170536.49646.ec.
Groth A, Enoksson F, Hultcrantz M, Stalfors J, Stenfeldt K, Hermansson A. Acute mastoiditis in children aged 0–16 years–a national study of 678 cases in Sweden comparing different age groups. Int J Pediatr Otorhinolaryngol. 2012;76(10):1494–500. https://doi.org/10.1016/j.ijporl.2012.07.002.
Ropposch T, Nemetz U, Braun EM, Lackner A, Walch C. Low molecular weight heparin therapy in pediatric otogenic sigmoid sinus thrombosis: a safe treatment option? Int J Pediatr Otorhinolaryngol. 2012;76(7):1023–6. https://doi.org/10.1016/j.ijporl.2012.03.024.
Bradley DT, Hashisaki GT, Mason JC. Otogenic sigmoid sinus thrombosis: what is the role of anticoagulation? Laryngoscope. 2002;112(10):1726–9. https://doi.org/10.1097/00005537-200210000-00003.
Dentali F, Squizzato A, Gianni M, De Lodovici ML, Venco A, Paciaroni M, Crowther M, Ageno W. Safety of thrombolysis in cerebral venous thrombosis. A systematic review of the literature. Thromb Haemost. 2010;104(5):1055–62. https://doi.org/10.1160/TH10-05-0311.
Capecchi M, Abbattista M, Martinelli I. Cerebral venous sinus thrombosis. J Thromb Haemost. 2018;16(10):1918–31. https://doi.org/10.1111/jth.14210.
Neilan RE, Isaacson B, Kutz JW Jr, Lee KH, Roland PS. Pediatric otogenic lateral sinus thrombosis recanalization. Int J Pediatr Otorhinolaryngol. 2011;75(6):850–3. https://doi.org/10.1016/j.ijporl.2011.03.024.
Acknowledgements
Funding
No funding or sponsorship was received for this study. The journal’s fee was funded by the authors.
Author Contributions
Conceptualization: Michal Kotowski, Jaroslaw Szydlowski; Methodology: Michal Kotowski; Formal analysis and investigation: Michal Kotowski; Writing—original draft preparation: Michal Kotowski; Writing—review and editing: Michal Kotowski; Resources: Michal Kotowski, Jaroslaw Szydlowski; Supervision: Jaroslaw Szydlowski. All authors read and approved the final manuscript.
Disclosures
Michal Kotowski and Jaroslaw Szydlowski declare that they have no competing interests.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kotowski, M., Szydlowski, J. Otogenic Cerebral Sinus Thrombosis in Children: A Narrative Review. Neurol Ther 12, 1069–1079 (2023). https://doi.org/10.1007/s40120-023-00499-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40120-023-00499-0