Abstract
Introduction
The clinical, social, and economic burden of epilepsy is undeniable. Local guidance on epilepsy management is limited and needed to address the both use of anti-seizure medication (ASM) and switching practices which influence clinical outcomes.
Areas Covered
An expert panel composed of practicing neurologists and epileptologists from countries of the Gulf Cooperation Council (GCC) met in 2022 to discuss local challenges in the management of epilepsy and formulate recommendations for clinical practice. Published literature on the outcomes of ASM switching was reviewed along with clinical practice/gaps, international guidelines, and local treatment availabilities.
Expert Opinion
Improper ASM use and inappropriate brand-name-to-generic or generic-to-generic switching can contribute to worsening clinical outcomes in epilepsy. ASMs should be used for the management of epilepsy based on patient clinical profile, underlying epilepsy syndrome, and drug availability to ensure optimal and sustainable treatment. Both first-generation and newer ASMs can be considered; appropriate use is recommended from the beginning of treatment. It is critical to avoid inappropriate ASM switching to avoid breakthrough seizures. All generic ASMs should fulfill strict regulatory requirements. If needed, ASM changes should always be approved by the treating physician. ASM switching (brand-name-to-generic, generic-to-generic, generic-to-brand-name) should be avoided in epilepsy patients who have achieved control but can be considered for those uncontrolled on current medication.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Improper anti-seizure medication (ASM) use and inappropriate brand-name-to-generic or generic-to-generic switching can lead to worsening clinical outcomes in epilepsy patients in the Gulf. |
Both first-generation and newer ASMs can be considered and should be used appropriately from the beginning of treatment to ensure optimal clinical outcomes. |
Inappropriate ASM switching should be avoided to prevent breakthrough seizures. |
ASM switching (brand-name-to-generic, generic-to-generic, generic-to-brand name) can be considered for patients who are uncontrolled on current medication, but not for those who are in remission (controlled). |
Introduction
Epilepsy remains one of the most common neurological diseases worldwide across all age groups [1]. In 2016, there were close to 46 million patients with all-active epilepsy (both idiopathic and secondary epilepsy) globally [2]. People with epilepsy are at a significantly higher risk of premature mortality [1]. In 2019, about 114,000 deaths were attributed to idiopathic epilepsy worldwide [3]. Health outcomes in persons with epilepsy are further worsened by comorbid physical and psychiatric conditions, which occur in around 50% of this patient population [1]. Epilepsy is a treatable condition, with up to 70% of people with epilepsy having the potential to become seizure free should adequate diagnosis and anti-seizure medicines (ASMs) be used [1]. Epidemiological data are generally lacking in the Arab world [4, 5], but the age-standardized prevalence of idiopathic epilepsy was estimated to be between 330 and 430 per 100,000 population in countries of the Gulf Cooperation Council (GCC) [2]. In 2019, there were an estimated 811 deaths and 115,789 disability-adjusted life-years due to idiopathic epilepsy in GCC countries. The number of deaths due to epilepsy has remained relatively stable from 1990 up to 2019, but the number of disability-adjusted life-years has increased [3].
Despite this background, epilepsy services are underdeveloped in the Gulf region. The majority of hospitals have no adult or pediatric neurologists/epileptologists, and although epilepsy monitoring units are available, they are unequally distributed in the region, with reported underutilization [6, 7]. Moreover, epilepsy carries a significant social and economic burden that is evident at several levels, but most notably a social stigma and loss of productivity [1]. Social stigma is particularly evident in the GCC region. Poor knowledge and socio-cultural/socio-religious beliefs drive negative attitudes towards people with epilepsy; according to these beliefs, the etiology of epilepsy is often linked to psychological disorders, evil eye (envy), and spirit possession. Such negative attitudes carry notable implications for people with epilepsy, often in the form of social disadvantages/discrimination in marriage, child-bearing, and employment, as well as decreased quality of life, depression, and anxiety [8,9,10,11,12].
In addition to the social implications of epilepsy, this condition carries a significant economic burden. The cost of ASMs, particularly the newer, is one of the major contributors to the cost of epilepsy [13,14,15]. Moreover, the cost of many common brand-name ASMs can be tenfold higher per pill day than their generic equivalents [16]. Consequently, there is an urgent need to evaluate any incremental benefits derived from newer ASMs against their cost-effectiveness [17]. Generics and authorized generics offer significant cost savings without compromising clinical efficacy and safety [18, 19]. While authorized generics are identical to their brand-name equivalents, generics are similar to brand-name drugs with demonstrated bioequivalence within the permitted range of variability. Indeed, the pharmacokinetic (PK) parameters reflecting the bioavailability of generics can vary between 80% and 125% of the original brand-name drug. There is currently no compelling evidence of a high risk of non-bioequivalence or clinically relevant changes in efficacy among approved generic products subject to strict regulatory requirements [20]. Despite that, barriers to generic substitution persists around the world, with the most notable being mistrust of regulatory control and quality of generic ASMs as well as lack of education on generics [21].
Clinical experience in GCC countries has shown that improper use of ASMs and ASM switching lead to worsened clinical outcomes. ASM accessibility also plays a significant role. The above evidence, compounded by the absence of local guidance on epilepsy management, reveals the need to establish consensus guidance common to the Gulf region. By establishing such guidelines, the clinical approach and treatment goals for epilepsy management can be aligned in the region. In particular, these guidelines will focus on the medical impact of ASM choice and treatment changes [from brand-name ASM to generic ASM (brand-name–generic), from generic ASM to another generic ASM (generic–generic), or from brand-name ASM to a different brand-name ASM (brand-name–brand-name)], bearing in mind socio-economic considerations. This work is intended to guide both local practitioners as well as key opinion leaders and healthcare authorities regarding appropriate healthcare strategies for epilepsy patients in GCC countries. This paper mainly addresses adult epilepsy and does not apply properly to pediatric epilepsy in general, but only to pediatric patients with focal epilepsy that behaves as in adults.
Methodology
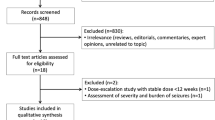
The expert panel comprised practicing neurologists and epileptologists from GCC countries who met in 2022 to initiate the discussion on the topic and relevant aspects of local challenges. All authors were experts participating on the panel. A literature search was conducted in the Medline and PubMed databases, with no limits on date or language, using various combinations of keywords including ‘anticonvulsants/antiepileptic drugs/antiseizure medications,’ ‘bioequivalence,’ and ‘generic anticonvulsants/antiepileptic drugs/anti-seizure medications.’ Further references were identified by searching the reference lists of retrieved articles and from the authors’ knowledge of the field. Published literature was reviewed taking into consideration clinical practice, international guidelines, best practices, clinical gaps, and local treatment availabilities. Two authors performed the literature review and a third reviewer was called in to handle any conflicts that arose.
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Results
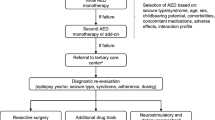
Selecting an ASM
Both older and newer generations of ASMs are effective for managing epilepsy, albeit with better tolerability associated with the newer ASMs [22]. A network meta-analysis based on randomized controlled trials (RCTs) confirmed that for people with focal seizures and for people with generalized seizures, first-generation ASMs [phenobarbitone (adults only, not applicable to children) and phenytoin] provide better seizure control when indicated than other ASMs, but at the cost of the highest rates of treatment discontinuation. Sodium valproate was suggested as ASM to ensure the best control and remission of generalized tonic–clonic seizures, with lamotrigine and levetiracetam shown to be suitable alternatives. Carbamazepine and lamotrigine are appropriate first-treatment options for the management of focal-onset seizures, with possible substitution by levetiracetam [22]. First-generation ASMs should therefore remain part of the armamentarium against epilepsy. The SANAD II phase IV trial actually demonstrated that levetiracetam was neither non-inferior nor cost-effective compared to valproate in patients with generalized and unclassifiable epilepsy [17]. In newly diagnosed focal epilepsy, the SANAD II trial findings support lamotrigine, but not levetiracetam or zonisamide, as a first-line treatment option [23].
Local insights on ASM usage are limited and as follows. One study from Qatar reported that levetiracetam is the most frequently prescribed drug (41% of subjects), with an average seizure freedom rate of 54% [24]. A study carried out in the UAE reported that approximately a quarter of patients initially receive a nonspecific ASM, of whom around 64% are poorly controlled [25]. In the same study, the use of broad-spectrum ASMs led to seizure control in patients who were previously on narrow-spectrum or no ASM [25]. The authors of one study from Saudi Arabia noted the increased use of ASMs, particularly new ASMs (i.e., levetiracetam and lamotrigine), during pregnancies in patients with epilepsy, with a higher rate of maternal complications observed with first-generation ASMs (i.e., carbamazepine and valproate) [26]. Several variables should be considered when choosing an ASM, including comorbidities, age, sex, underlying profile (metabolic, psychiatric), as well as cost. Addressing psychiatric comorbidities, such as depression and anxiety, as well as physical (somatic) symptoms could be necessary interventions to improve treatment adherence and clinical outcomes among local patients with epilepsy [27, 28]. In another study from Saudi Arabia, the authors reported that proper seizure control is needed to improve patients’ quality of life, regardless of the medication class used [29]. It should also be noted that the efficacy and tolerability of a drug is greatly affected by appropriate clinical practice. It is therefore necessary to use available ASMs appropriately from the beginning of treatment to ensure optimal clinical outcomes and avoid causing stigma among patients.
Drug availability remains a prevailing clinical challenge in GCC countries, with the exception of Qatar. Although drug availability is not a major issue in Qatar, the choice of ASM reportedly remains dependent on the availability of drugs in the patient’s native country [30]. In general, drug availability in the region has been governed in recent years by a tender-based system as opposed to medical evidence-based system. Changes in medication availability are based on policies and economic decisions with no involvement from epileptologists or medical professionals. It is recommended that changes in ASM availability should never be sudden or imposed for economic reasons. If necessary, use of appropriate treatment alternatives (in terms of spectrum of efficacy and in compliance with local/international guidelines and regulations) is recommended when faced with interrupted ASM supply. The specific choice of alternative treatment is left to the discretion of the treating physician.
Switching ASM
The expert panel is not opposed to ASM switching from brand-name ASM to generic ASM or between generic ASMs. However, switching ASMs has been predominately imposed on physicians practicing in the GCC (with the exception of Qatar). Anecdotal insights from local practice suggest that arbitrary ASM switching has medical consequences, namely breakthrough seizures and increased visits to the clinic. Neurologists generally have positive attitudes towards generics when initiating new anti-seizure treatment, and when looking to reduce treatment costs [31]. Patient preference to remain on a brand-name drug treatment is a major driver of switch avoidance [31]. In addition, neurologists remain concerned about any deterioration in seizure control when considering a switch from a brand-name ASM to a generic ASM [31]. Findings in the literature support the possible implications of treatment uncertainties and generic skepticism on clinical outcomes [32]. Patient adherence to recommended medical treatment is often reliant on the shape and color of the medication, and generic substitution could lead to changes in patient behavior [33, 34]. Moreover, people with epilepsy are generally skeptic towards generic ASMs and their attitudes are dependent on prior experience with generic substitutions [35, 36].
Changes in clinical efficacy have also been observed with the use of generics; anecdotal evidence from some centers using the generic levetiracetam revealed a possible increase in seizure pattern, although relevant literature does not consistently reflect this increase [37,38,39,40,41,42,43,44]. An overview of relevant published studies on clinical outcomes after ASM switch is provided in section ASM Switching: Current Body of Evidence (summarized in Table 1).
It should be noted that regardless of the findings reported above, the use of generics should be carefully regulated in any country to ensure clinical efficacy and safety. Patient counseling is recommended when a switch to generic ASM is necessary in order to not only limit any possible deterioration of clinical outcomes, but also prevent litigation for medical negligence [45]. The medical implications of introducing a generic ASM by policy-makers could be limited across the region. Purely economic-driven policies should not be adopted for epilepsy management, and the switch from a brand-name ASM to a generic ASM or between generic ASMs should never be allowed without the approval of the attending physician.
ASM Switching: Current Body of Evidence
RCTs on ASM Switching
To date, three RCTs have reported the bioequivalence of generics to brand-name drugs, confirming the results of bioequivalence studies conducted in healthy volunteers [46]. That being said, these RCTs were conducted in a small number of patients with epilepsy and only reported on switching between brand-name and generic lamotrigine. The BioEquivalence in Epilepsy Patients (BEEP) study demonstrated the bioequivalence of generic lamotrigine to brand-name Lamictal [47]. The trial included 34 patients that were deemed “generic brittle,” i.e., patients who are expected to experience issues with generic switching due to a history of reported prior exacerbation of seizures or side effects following changes in ASM formulation, or intolerable ASM side effects or refractory seizures within the last year prior to study. Patients were switched between generic and brand-name medication every 2 weeks, and bioequivalence of the generic to the branded ASM was demonstrated in terms of PK parameters [area under the concentration–time curve (AUC), maximum plasma concentration reached (Cmax), and minimum blood plasma concentration reached (Cmin)]. The within-subject variability (WSV) of the generic and brand-name drug was also similar. Moreover, no adverse events were linked to the allowable PK differences between the generic and branded drug, which supports the soundness of the US Food and Drug Administration (FDA) bioequivalence standards in controlled clinical conditions [47]. Generic-to-generic lamotrigine switches in people with epilepsy were evaluated as part of the EQUIGEN trial [48]. In this trial, 35 eligible patients, namely adults already receiving immediate-release lamotrigine at doses ranging from 100 mg up to 400 mg twice daily, were randomized. Two lamotrigine generics were used, and switches were done every 14 days, for 2 months. The study assessed and demonstrated bioequivalence between the generic products (via Cmax and AUC), confirming the appropriateness of US Food and Drug Administration bioequivalence standards. The study also reported no serious adverse events, and no significant change in seizure frequency or adverse events [48]. The EQUIGEN trial also compared brand-name lamotrigine to two generics, lamotrigine-high and lamotrigine-low [49]. The study included 50 patients on concomitant ASM and not currently receiving lamotrigine. A single subtherapeutic dose of lamotrigine was administered in a blinded sequence, and PK bioequivalence (Cmax and AUC) was evaluated on the same day, then daily through outpatient samples over a 4-day period. Each drug was tested twice throughout the study, with a washout period between each drug administration. The study demonstrated the bioequivalence of generic lamotrigine-high and generic lamotrigine-low to brand-name lamotrigine in patients with epilepsy on concomitant ASM. The results of this study also supported the FDA bioequivalence standards [49].
Non-randomized and Retrospective/Real-World Data
Non-randomized studies of the effect of ASM switching are available and offer insights into a wide range of ASMs. However, the results of these studies have been conflicting, with evidence both supporting and cautioning against switching from a brand-name ASM to a generic sASM.
The longest follow-up data are from a prospective observational real-life study which reported the safety and efficacy of switching from brand-name to generic levetiracetam [41]. A total of 125 patients were included in this study, and follow-up data were obtained for up to 4 years after the switch. The study showed no significant change in the frequency of seizures nor in drug-related adverse events, irrespective of the epilepsy syndrome. It should be noted that adverse effects were reported in close to 25% of patients receiving the generic levetiracetam, with some leading to treatment discontinuation both during the initial study period as well as during the long-term follow-up [41]. These results were consistent with those reported from other studies which found minimal or no risk of increased seizure frequency after substituting brand-name levetiracetam with generic levetiracetam [37,38,39,40,41,42,43,44]. Contradictory results were reported from a very recent retrospective study which evaluated the switch of patients with stable seizure frequency from brand-name levetiracetam to generic ASM [50]. The switch period was 6 months, after which patients were returned to brand-name levetiracetam. Of the 75 patients included in the study, seizure frequency was found to significantly increase in patients who were previously controlled. Moreover, 8% experienced adverse events after the switch from brand-name levetiracetam to generic levetiracetam. Recurrent seizures or adverse events were observed as early as 14 days after the transition to the generic ASM and changes in therapy were needed in 22 cases [50].
Recently, Lang et al. [51] examined whether manufacturer switch of the same ASM would have a detrimental effect on seizure-free children and adolescents. The authors could not demonstrate any significant effect of manufacturer change on seizure control rate. This was applicable to any type of ASM included, namely, first-generation ASM, new-generation ASM, generic ASM, and brand-name ASM. The only factor found to affect the risk of seizure recurrence in a seizure-free group was changing the dosage of the ASM [51]. This result was in contrast to that of a previous nationwide study of prescription data from adults, which had reported a significantly higher risk of seizure recurrence following manufacturer switch of ASM in previously seizure-free patients with epilepsy [52]. A total of 3530 people with epilepsy were included in the study, and the increased risk of seizure recurrence was observed in both brand-name-to-generic switches, and generic-to-generic switches [52]. A population-based case-crossover study investigated whether switching to a different generic manufacturer would affect the risk of seizure-related events (seizure-related hospital admission or emergency room) [32]. Among the 83,000 patients on generic ASM included in the study, generic ASMs were found to lead to a 8% increase in the odds of seizure-related events, but the switch to a different generic manufacturer was not associated with increased risk [32]. An earlier case–control study found a modest association between switching bioequivalent ASMs (brand-name–generic, generic–brand-name, generic–generic) and seizure-related events. The risk of seizure-related events persisted even after controlling for individual medication effects (e.g., first- vs. new-generation ASM) [53]. The authors also emphasized the potential implication of the behavior of switching ASM itself as well as other environmental characteristics rather than the type of ASM or switch [53]. These results were consistent with those from previous studies [54, 55], but in contrast to the findings of other studies which reported no increased risk with bioequivalent ASM switching [56,57,58].
Conclusion
Epilepsy carries a notable social and economic burden in the GCC region. The improper use of ASMs and inappropriate brand-name-to-generic or generic-to-generic switching are two of the most prominent contributors to worsening clinical outcomes in epilepsy patients. ASMs should be used for the management of epilepsy based on a patient’s clinical profile and drug availability to ensure optimal and sustainable treatment. Both first-generation and newer ASMs can be considered and should be used appropriately from the beginning of treatment to ensure optimal clinical outcomes. International guidelines align with the present expert panel’s emphasis of the need to avoid inappropriate ASM switching to avoid breakthrough seizures. Strict regulatory requirements and monitoring should be enforced for all generic ASM. If needed, changes in ASM should always be approved by the treating physician. ASM switching (brand-name–generic, generic–generic, generic–brand-name) should be avoided in epilepsy patients who are in clinical remission (controlled) but could be considered for patients who are uncontrolled on current medication.
Expert Opinion
Recommendations
-
Both first- and newer generation ASMs should be considered for the management of epilepsy.
-
The choice of ASM should depend on the patient’s clinical profile and drug availability to ensure optimal and sustainable treatment.
-
Available and accessible ASMs should be used appropriately from the beginning of treatment to ensure optimal clinical outcomes and avoid causing stigma among patients.
-
Patients should be counseled on the nature of generics, the strict regulatory conditions governing their use, and the efficacy and safety of appropriate generic use to alleviate/prevent patient anxiety related to generic prescription.
-
Strict regulatory conditions and monitoring should be enforced for all generic ASMs.
-
Changes in ASM should never be made without the approval of the treating physician.
-
If for clinical reasons brand-name-to-generic substitution is contraindicated, this should be clearly indicated in the prescription.
-
When changes in the packaging, form, and color of ASM are implicated in generic substitution, patients should be informed of these changes.
-
It is preferable to avoid ASM switch (brand-name–generic, generic–generic, generic–brand-name) in epilepsy patients who are in clinical remission (controlled).
-
ASM switch (brand-name–generic, generic–generic, generic–brand-name) could be considered for patients who are uncontrolled on current medication.
Epilepsy can be a treatable chronic brain disorder in almost 70% of cases. In general, selecting the appropriate recommended ASM is fundamental to achieve a seizure-free state. The ASM should be chosen through a patient-centric approach, based on clinical profile, comorbidities, as well the cost and the availability of the chosen ASM. That being said, drug-resistant epilepsy remains a notable concern in at least 30% of cases and could be driven by the underlying pathogenesis of epilepsy and other factors unrelated to the inappropriate use of ASM. In all cases, careful selection of the ASM is critical to assure patient compliance, which can be a real challenge for patients with epilepsy, noting that only 30–60% of patients with epilepsy are compliant with their treatment. This challenge is further complicated in our GCC region where stigma of this disorder, along with continuing misconceptions among different communities, have affected and will continue to affect patients’ attitude toward accepting and continuing the recommended therapy. Furthermore, access to various ASMs is not equally distributed among citizens and residents of these countries. It is not, therefore, very surprising the decision to start or switch to a specific ASM is driven by costs only. Different regularity bodies among the GCC countries have taken upon themselves the role to regulate the access and availability of these ASMs and have, to a great extent, both influenced the decisions on which generation of ASMs to include in drug formularies and directed the direction of switching brand names for generics. Unfortunately, these steps were taken without requesting inputs from the practicing physicians and experts in the field.
This report is an attempt to address some of the gaps in managing epilepsy in our GCC region and to try to shed light on some of the unmet needs, taking into consideration the variability of cultural, religious, and socio-economic status of citizens and residents of our region. Experts participating in our expert panel were carefully chosen based on recommendations of their respective local neurological societies and were tasked to come up with clear recommendations on how to select the appropriate ASM and to thoroughly review the literature on the consequences of brand-name-to-generic and generic-to-generic switch. We strongly believe that treating physicians should have the final call on how and when to make that switch, if indicated. Future local and regional research in this area, based on well-designed, large sample RCTs, is strongly needed to address the safety, feasibility, and drawbacks, if any, on this matter. Unfortunately, all of the published reports on this topic have been carried out in Western societies where genetic, socio-economic, and educational differences may affect the outcome of these studies and, therefore, may not be applicable to our region. Furthermore, epidemiological studies reporting rates and types of injuries associated with different seizure types as well the risk factors to these injuries are very limited in our region. These studies are expected to help us understand the variable risk factors, including the clinical profiles, demographics, and compliance rates among our patients in this region. On another note, and despite the high prevalence of various neuropsychiatric comorbidities among patients with epilepsy in our region, a significant segment of these patients is not screened for these disorders [61]. Failure to identify these patients could render them resistant to treatment or make them more prone to experience undesirable adverse effects. Educating all community physicians on the importance of this practice is critical to assure better outcome. Moreover, developing nationwide and regional practice guidelines that include specific practice parameters and address different aspects of the management of patients with epilepsy, on which our physicians will be regularly audited by local licensing bodies, is one of the best approaches to improve patients’ care and to achieve our ultimate goal of improving the quality of lives of our patients with epilepsy.
Finally, the art of ASM selection and profiling the right candidates for ASM switching can be fine-tuned by future pharmacogenomic studies that would allow us to map out the right patient for the appropriate ASM. These studies are expected to predict the response rates and the risks of developing adverse events among various ASM based on genetic and ethnic backgrounds and gender of the patient. Local authorities, with support of all relevant bodies, are encouraged to include practicing physicians and experts in the field in their committees to steer future efforts in accessing various ASM, monitoring the practices of physicians, and adopting the protocols that govern the switch between different ASM formulations.
Data availability
Data sharing is not applicable to this article as no datasets were generated or analyzed.
References
World Health Organization, International League Against Epilepsy, International Bureau for Epilepsy. Epilepsy: a public health imperative. 2019. https://www.ilae.org/files/dmfile/19053_Epilepsy_A-public-health-imperative-For-Web.pdf. Accessed 16 Oct 2022.
Beghi E, Giussani G, Abd-Allah F, et al. Global, regional, and national burden of epilepsy, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18:357–75..
Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) cause and risk summary. 2020. Seattle: IHME, University of Washington. https://vizhub.healthdata.org/gbd-results/. Accessed 16 Oct 2022.
Idris A, Alabdaljabar MS, Almiro A, et al. Prevalence, incidence, and risk factors of epilepsy in Arab countries: a systematic review. Seizure. 2021;92:40–50.
Bhalla D, Lotfalinezhad E, Timalsina U, et al. A comprehensive review of epilepsy in the Arab world. Seizure. 2016;34:54–9.
Aljafen BN, Alfayez SM, Alanazy MH, et al. Epilepsy monitoring units in Saudi Arabia: Where do we stand compared to developed countries? Neurosciences (Riyadh). 2018;23:244–9.
Alfayez SM, Aljafen BN. Epilepsy services in Saudi Arabia. Quantitative assessment and identification of challenges. Neurosciences (Riyadh). 2016;21:326–30.
Al-Hashemi E, Ashkanani A, Al-Qattan H, et al. Knowledge about epilepsy and attitudes toward students with epilepsy among middle and high school teachers in Kuwait. Int J Pediatr. 2016;2016:1–15.
Abduelkarem AR. Societal problems that patients with epilepsy are facing in Sharjah, UAE. Epilepsy Behav. 2016;59:142–6.
AlHarbi FA, Alomari MS, Ghaddaf AA, et al. Public awareness and attitudes toward epilepsy in Saudi Arabia: a systematic review and meta-analysis. Epilepsy Behav. 2021;124.
Abdel Ghaffar NF, Asiri RN, AL-Eitan LN, et al. Improving public stigma, sociocultural beliefs, and social identity for people with epilepsy in the Aseer region of Saudi Arabia. Epilepsy Behav Reports. 2021;16.
Alsaadi T, El Hammasi K, Shahrour TM, et al. Prevalence of depression and anxiety among patients with epilepsy attending the epilepsy clinic at Sheikh Khalifa Medical City, UAE: a cross-sectional study. Epilepsy Behav. 2015;52:194–9.
Al-Zakwani I, Hanssens Y, Deleu D, et al. Annual direct medical cost and contributing factors to total cost of epilepsy in Oman. Seizure. 2003;12:555–60.
Begley C, Wagner RG, Abraham A, et al. The global cost of epilepsy: a systematic review and extrapolation. Epilepsia. 2022;63:892–903.
Gao L, Xia L, Pan SQ, et al. Burden of epilepsy: a prevalence-based cost of illness study of direct, indirect and intangible costs for epilepsy. Epilepsy Res. 2015;110:146–56.
Terman SW, Lin CC, Kerr WT, et al. Changes in the use of brand name and generic medications and total prescription cost among medicare beneficiaries with epilepsy. Neurology. 2022;99:E751–61.
Marson A, Burnside G, Appleton R, et al. The SANAD II study of the effectiveness and cost-effectiveness of valproate versus levetiracetam for newly diagnosed generalised and unclassifiable epilepsy: an open-label, non-inferiority, multicentre, phase 4, randomised controlled trial. Lancet. 2021;397:1375–86.
Tian Y, Reichardt B, Dunkler D, et al. Comparative effectiveness of branded vs. generic versions of antihypertensive, lipid-lowering and hypoglycemic substances: a population-wide cohort study. Sci Rep 2020;10:1–12.
Desai RJ, Sarpatwari A, Dejene S, et al. Comparative effectiveness of generic and brand-name medication use: a database study of US health insurance claims. PLoS Med. 2019;16.
Odi R, Franco V, Perucca E, et al. Bioequivalence and switchability of generic antiseizure medications (ASMs): a re-appraisal based on analysis of generic ASM products approved in Europe. Epilepsia. 2021;62:285–302.
Niyongere J, Welty TE, Bell MW, et al. Barriers to generic antiseizure medication use: results of a global survey by the International League Against Epilepsy Generic Substitution Task Force. Epilepsia Open. 2022;7:260–70.
Nevitt SJ, Sudell M, Cividini S, et al. Antiepileptic drug monotherapy for epilepsy: a network meta-analysis of individual participant data. Cochrane Database Syst Rev. 2022;6(6):CD011412. https://doi.org/10.1002/14651858.CD011412.pub4.
Marson A, Burnside G, Appleton R, et al. The SANAD II study of the effectiveness and cost-effectiveness of levetiracetam, zonisamide, or lamotrigine for newly diagnosed focal epilepsy: an open-label, non-inferiority, multicentre, phase 4, randomised controlled trial. Lancet. 2021;397:1363–74.
Haddad N, Melikyan G, Al Hail H, et al. Epilepsy in Qatar: causes, treatment, and outcome. Epilepsy Behav. 2016;63:98–102.
Alsaadi T, Taha H, Al Hammadi F. Choice of antiepileptic drugs in idiopathic generalized epilepsy: UAE experience. Epilepsy Res Treat. 2015;2015:1–4.
Alsfouk BA, Almarzouqi MR, Alageel S, et al. Patterns of antiseizure medication prescription in pregnancy and maternal complications in women with epilepsy: a retrospective study in Saudi Arabia. Saudi Pharm J. 2022;30:205–11.
Alsaadi T, Kassie S, El Hammasi K, et al. Potential factors impacting health-related quality of life among patients with epilepsy: results from the United Arab Emirates. Seizure. 2017;53:13–7.
Almwled AS, Almuhaydili AO, Altamimi SM, et al. Prevalence and biopsychosocial factors associated with treatment adherence among people with epilepsy in a tertiary care hospital in Riyadh, Saudi Arabia. Neurosciences (Riyadh). 2022;27:94–103.
Tayeb HO, Alsawwaf Y, Khoja AA, et al. Determinants of health-related quality of life of epilepsy patients in Jeddah, Saudi Arabia. Cureus. 2022;14.
Wilkins SS, Mesraoua B, Palomo GA, et al. Characteristics of patients with confirmed epilepsy and psychogenic nonepileptic seizures in Qatar. Epilepsy Behav. 2018;85:218–21.
Olsson P, Freij J, Compagno Strandberg M, et al. Physicians’ attitudes toward generic substitutions of antiseizure drugs in epilepsy. Acta Neurol Scand. 2021;144:600–7.
Das S, Jiang X, Jiang W, et al. Relationship of antiepileptic drugs to generic brittleness in patients with epilepsy. Epilepsy Behav. 2020;105:106936.
Barenie RE, Kesselheim AS, Gagne JJ, et al. Preferences for and experiences with pill appearance changes: national surveys of patients and pharmacists. Am J Manag Care. 2020;26:340–7.
Sarpatwari A, Gagne JJ, Lu Z, et al. A survey of patients’ perceptions of pill appearance and responses to changes in appearance for four chronic disease medications. J Gen Intern Med. 2019;34:420–8.
Rathe J, Andersen M, Jarbøl DE, et al. Generic switching and non-persistence among medicine users: a combined population-based questionnaire and register study. PLoS ONE. 2015;10:e0119688.
Olsson P, Pearson K, Reimers A, et al. Widespread skeptic attitudes among people with epilepsy toward generic antiseizure drugs—a Swedish survey study. Epilepsy Behav. 2021;114.
Gha-Hyun L, Dae SJ. Brand name to generic substitution of levetiracetam in patients with epilepsy. Seizure. 2018;60:127–31.
Bosak M, Słowik A, Turaj W. Safety of switching from brand-name to generic levetiracetam in patients with epilepsy. Drug Des Devel Ther. 2017;11:2287–91.
Liang MJ, Qiu WF, Zhang JW, et al. Efficacy and safety of switching from brand-name to domestic generic levetiracetam in children with epilepsy. Zhongguo Dang Dai Er Ke Za Zhi. 2022;24:285–9.
Vari MS, Pinto F, Mencaroni E, et al. Safety of overnight switch from brand-name to generic levetiracetam. Clin Drug Investig. 2016;36:87–91.
Trimboli M, Russo E, Mumoli L, et al. Brand-to-generic levetiracetam switching: a 4-year prospective observational real-life study. Eur J Neurol. 2018;25:666–71.
Markoula S, Chatzistefanidis D, Gatzonis S, et al. Brand-to-generic levetiracetam switch in patients with epilepsy in a routine clinical setting. Seizure. 2017;48:1–6. https://pubmed.ncbi.nlm.nih.gov/28363098/.
Reimers A, Olsson P, Nilsson J, et al. Impact of generic substitution on levetiracetam serum concentration—a prospective study in an outpatient setting. Epilepsy Res. 2017;134:54–61.
Fanella M, Morano A, Fattouch J, et al. Switch from originator to equivalent drug in the era of generic antiepileptic drugs: study of Keppra Versus Epitiram clinical equivalence. Clin Neuropharmacol. 2017;40:239–42..
Beran RG. Generic substitution and advice to patients -potential legal medicine consequences—from A (Australia) to U (United Kingdom or United States of America). Seizure. 2021;91:515–9.
Srichaiya A, Longchoopol C, Oo-Puthinan S, et al. Bioequivalence of generic lamotrigine 100-mg tablets in healthy Thai male volunteers: a randomized, single-dose, two-period, two-sequence crossover study. Clin Ther. 2008;30:1844–51.
Ting TY, Jiang W, Lionberger R, et al. Generic lamotrigine versus brand-name Lamictal bioequivalence in patients with epilepsy: a field test of the FDA bioequivalence standard. Epilepsia. 2015;56:1415–24..
Privitera MD, Welty TE, Gidal BE, et al. Generic-to-generic lamotrigine switches in people with epilepsy: the randomised controlled EQUIGEN trial. Lancet Neurol. 2016;15:365–72.
Berg M, Welty TE, Gidal BE, et al. Bioequivalence between generic and branded lamotrigine in people with epilepsy: the EQUIGEN randomized clinical trial. JAMA Neurol. 2017;74:919–26.
Tharavichitkun J, Yadee T, Angkaow P, et al. Evaluating therapeutic equivalence of generic and original levetiracetam in patients with epilepsy: a retrospective study. Neurol Int. 2022;14:271–83.
Lang JD, Kostev K, Reindl C, et al. Manufacturer switch of anti-seizure drugs may not increase the risk of seizure recurrence in Children: a nationwide study of prescription data in Germany. Epilepsy Behav. 2021;115.
Lang JD, Kostev K, Onugoren MD, et al. Switching the manufacturer of antiepileptic drugs is associated with higher risk of seizures: a nationwide study of prescription data in Germany. Ann Neurol. 2018;84:918–25.
Hansen RN, Nguyen HP, Sullivan SD. Bioequivalent antiepileptic drug switching and the risk of seizure-related events. Epilepsy Res. 2013;106:237–43..
Hansen RN, Campbell JD, Sullivan SD. Association between antiepileptic drug switching and epilepsy-related events. Epilepsy Behav. 2009;15:481–5.
Zachry WM, Doan QD, Clewell JD, et al. Case-control analysis of ambulance, emergency room, or inpatient hospital events for epilepsy and antiepileptic drug formulation changes. Epilepsia. 2009;50:493–500.
Devine ST, Weisbart E, Barron J, et al. Acute epilepsy exacerbations in patients switched between A-rated anti-epileptic drugs. Curr Med Res Opin. 2010;26:455–63.
Gagne JJ, Avorn J, Shrank WH, et al. Refilling and switching of antiepileptic drugs and seizure-related events. Clin Pharmacol Ther. 2010;88:347–53.
Erickson SC, Le L, Ramsey SD, et al. Clinical and pharmacy utilization outcomes with brand to generic antiepileptic switches in patients with epilepsy. Epilepsia. 2011;52:1365–71.
Kesselheim AS, Bykov K, Gagne JJ, et al. Switching generic antiepileptic drug manufacturer not linked to seizures: a case-crossover study. Neurology. 2016;87:1796–801.
Polard E, Nowak E, Happe A, et al. Brand name to generic substitution of antiepileptic drugs does not lead to seizure-related hospitalization: a population-based case-crossover study. Pharmacoepidemiol Drug Saf. 2015;24:1161–9.
Alsaadi T, Kassie S, Ali OM, et al. Psychiatric comorbidity in neurological disorders: towards a multidisciplinary approach to illness management in the United Arab Emirates. Front Psychiatry. 2019;10:263.
Acknowledgements
Funding
The authors retained control over the editorial process, including the discussion at all times. There was no financial reward associated with writing the paper. GSK has had no influence over the content other than a review of the paper for medical accuracy.
Medical Writing and Editorial Assistance
The authors wish to thank Nancy Al Akkary MSc, BSc, and Racha Aaraj, Pharm D, MSc, MPH from Phoenix Clinical Research for the writing and editorial support in the preparation of this manuscript. Writing/editorial assistance and publication charges was funded by GSK. The views and opinions expressed are those of the authors.
Author Contributions
The primary author was responsible for the concept of the paper and led the project. Taoufik Alsaadi, Abubaker Almadani, Jasem Al-Hashel, Abdullah Al Salti, Gayane Melikyan and Riaz Ahmed Khan have written parts of and have reviewed the whole manuscript.
Disclosures
Abubaker Almadani, Jasem Al-Hashel, Abdullah Al Salti, Gayane Melikyan, and Riaz Ahmed Khan have nothing to declare. Taoufik Alsaadi has no conflicts of interest to declare. This work was not undertaken as part of his role in the Emirati League Against Epilepsy.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Alsaadi, T., Almadani, A., Al-Hashel, J. et al. Commentary: Consensus Guidelines on the Appropriate Use of Brand-Name and Generic Anti-Seizure Medication for the Management of Epilepsy in the Gulf Region. Neurol Ther 12, 1015–1031 (2023). https://doi.org/10.1007/s40120-023-00491-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40120-023-00491-8