Abstract
Introduction
Galcanezumab, a humanized monoclonal antibody against calcitonin gene-related peptide, is a preventive migraine treatment. In global, randomized, placebo-controlled trials, galcanezumab reduced migraine headache severity and the frequency of migraine headaches associated with nausea and/or vomiting, photophobia and phonophobia, prodromal symptoms, or aura. We report secondary analyses from a Japanese phase 2 trial that assessed the effect of galcanezumab on migraine headache severity, frequency of migraine-associated symptoms, and frequency of migraine headaches during menstrual periods in Japanese patients with episodic migraine.
Methods
Adults with migraine (International Classification of Headache Disorders, 3rd edition; 4–14 migraine headache days/month) were randomized (2:1:1) to a monthly placebo (n = 230), 120 mg galcanezumab (240 mg loading dose; n = 115), or 240 mg galcanezumab (n = 114) for 6 months (double-blind). Patients recorded migraine headache days, severity, and symptoms in an electronic diary. Changes from baseline were analyzed (mixed model for repeated measures).
Results
Both galcanezumab doses significantly reduced the number of monthly moderate-to-severe and severe migraine headache days compared with placebo, overall (difference in least-squares mean change from baseline, 120 mg/240 mg versus placebo: moderate-to-severe, −1.9/−1.8 days; severe: −0.4/−0.4 days) and in each month; mean severity score was significantly reduced in the 240 mg group. Both galcanezumab doses significantly reduced the number of migraine headache days with nausea/vomiting (−1.1/−1.0 days), photophobia/phonophobia (−2.3/−1.7 days), prodromal symptoms (−0.7/−0.8 days), and aura (−0.7/−0.7 days). In most cases, the proportion of migraine headache days with these symptoms was reduced by galcanezumab. Both galcanezumab doses reduced the number of migraine headache days occurring during menstrual periods (n = 269; −0.8/−0.9 days).
Conclusion
Once-monthly galcanezumab significantly reduced the frequency of migraine headache days with moderate-to-severe or severe headache, migraine headache days with migraine-associated symptoms, and migraine headache days during menstrual periods in Japanese patients with episodic migraine, consistent with results from global studies.
Trial Registration: ClinicalTrials.gov (NCT02959177).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Global, randomized, placebo-controlled trials have demonstrated that galcanezumab, a once-monthly preventive treatment for migraine, significantly reduces the number of monthly migraine headache days, the severity of migraine headaches, and the frequency of migraine-associated symptoms. |
In this study, we analyzed data from a Japanese randomized, placebo-controlled trial to assess the effect of 6 months of galcanezumab treatment on migraine headache severity, frequency of migraine-associated symptoms, and frequency of migraine headaches during menstrual periods. |
What was learned from the study? |
Both 120 mg and 240 mg doses of galcanezumab significantly reduced the severity of migraine headaches, the frequency of migraine-associated symptoms, and the frequency of migraine headaches during menstrual periods in Japanese patients with episodic migraine. |
These results indicate that galcanezumab treatment not only reduces the frequency of migraine headaches in Japanese patients (as demonstrated previously), but also reduces other important aspects of migraine, such as headache severity, migraine-associated symptoms, and migraine headaches during menstrual periods, that adversely affect quality of life. |
Introduction
Migraine affects more than 1 billion people worldwide [1] and is the second most common cause of disability [2]. Although migraine attacks are primarily characterized by headache, other symptoms such as nausea, vomiting, photophobia, and phonophobia are common [3]. The headache phase is often preceded by prodromal symptoms (e.g., yawning, fatigue, mood changes), and about a third of people experience aura before and/or during headache [4, 5]. Migraine is most prevalent among young adult women, and migraine attacks are often associated with menstrual periods [2, 6]. Although preventive treatments for migraine reduce the frequency of migraine headache, their effects on the severity of migraine headaches or on the frequency of migraine-associated symptoms are not well documented.
Galcanezumab is a humanized monoclonal antibody directed against calcitonin gene-related peptide (CGRP) that is approved in many countries as a once-monthly preventive treatment for migraine [7, 8]. Global phase 3 randomized, placebo-controlled trials have demonstrated that galcanezumab significantly reduces the number of monthly migraine headache days in people with episodic [9, 10] or chronic [11] migraine. In 2021, galcanezumab was approved in Japan [12], where migraine is estimated to affect 6.0–8.4% of the population [13, 14]. A phase 2 randomized, placebo-controlled trial has demonstrated the efficacy and safety of monthly galcanezumab in Japanese patients with episodic migraine [15]. Over the 6-month treatment period of the trial, the number of monthly migraine headache days was reduced to a significantly greater extent by both 120 mg (following a 240 mg loading dose; mean change from baseline: −3.60 days) and 240 mg (−3.36 days) doses of galcanezumab compared with placebo (−0.59 days) [15]. Treatment-emergent adverse events were numerically more frequent with galcanezumab than with placebo, with injection-site reactions the most common adverse event across all treatment groups; the full safety results of this phase 2 trial have been reported in the primary publication [15].
A subsequent analysis of the global trials reported that galcanezumab significantly reduced the number of moderate-to-severe migraine headache days, the number of severe migraine headache days, and the number of migraine headache days associated with nausea and/or vomiting, photophobia and phonophobia, prodromal symptoms, or aura [16]. We hypothesized that galcanezumab would have similar effects on migraine headache severity and symptoms in Japanese patients. In addition, we aimed to determine for the first time whether galcanezumab could reduce the frequency of migraine headaches during menstrual periods. In this report, we present secondary analyses from the Japanese phase 2 trial that assessed the effect of galcanezumab on the severity of migraine headaches, the frequency of migraine-associated symptoms, and the frequency of migraine headaches during menstrual periods in Japanese people with episodic migraine.
Methods
Study Design
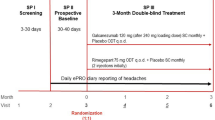
This was an analysis of data from a phase 2 randomized, placebo-controlled trial of galcanezumab in patients with episodic migraine in Japan (ClinicalTrials.gov: NCT02959177); the primary results have been published previously [15]. The trial was conducted at 40 sites in Japan between December 2016 and January 2019 and in accordance with the Declaration of Helsinki, Good Clinical Practice, and the Council for International Organizations of Medical Sciences International Ethical Guidelines. The protocol was approved by local ethics review boards (Table S1), and all patients provided written informed consent before any study procedures. The study consisted of a screening and washout period (≥ 30 days or ≥ 4 months for patients using botulinum toxin A or B), a prospective baseline period of 30–40 days, a 6-month double-blind treatment period, and a 4-month follow-up period.
Study Population
Detailed inclusion and exclusion criteria have been reported previously [15]. In brief, patients were eligible for the study if they were aged 18–65 years, had a diagnosis of migraine based on the International Classification of Headache Disorders, 3rd edition (beta version) criteria [3], and had 4–14 migraine headache days per month and ≥ two migraine attacks per month in the previous 3 months. A migraine headache day was defined as a calendar day when the patient recorded having a migraine headache or probable migraine headache. Patients were excluded if they were currently using migraine preventive treatment, had persistent daily headache, cluster headache, or migraine subtypes, had ≥ 15 headache days per month or suspected chronic migraine, or had failed to respond to ≥ three adequately dosed migraine preventive treatments from different classes.
Treatment Protocol
After the baseline period, patients were randomized (2:1:1) to placebo, 120 mg galcanezumab, or 240 mg galcanezumab. Randomization was stratified by baseline monthly migraine frequency (< 8 versus ≥ 8 monthly migraine headache days) and implemented using a computer-generated random sequence with an interactive web-response system.
Study drug was administered subcutaneously once per month. The 120 mg galcanezumab group received a loading dose of 240 mg at the first injection.
Outcome Measures
Patients recorded migraine headache data using an electronic diary (eDiary) during the baseline, treatment, and follow-up periods. Headache data included the occurrence and severity (mild, moderate, or severe) of a migraine (or probable migraine) headache and the presence or absence of migraine-associated symptoms (nausea, vomiting, photophobia, phonophobia, prodromal symptoms, aura). Menstrual periods were also recorded in the eDiary throughout the study; there was no set definition of a “menstrual period,” although this is usually considered to be from the first day of bleeding to when bleeding has stopped or almost stopped. Patient demographic data and years since migraine diagnosis were collected at baseline.
The primary endpoint of the trial was the overall mean change from the baseline period in the number of monthly migraine headache days averaged over the 6 months of the double-blind period, which was estimated as the main treatment effect from a mixed model for repeated measures (MMRM) analysis [15]. Prespecified (except where noted) analyses of secondary and exploratory endpoints reported herein include the following: for each month and for the overall double-blind period (average per month for months 1–6), the monthly mean change in the number of moderate-to-severe migraine headache days (secondary), severe migraine headache days (post hoc), migraine headache days with nausea and/or vomiting (exploratory), migraine headache days with photophobia or phonophobia (exploratory), migraine headache days with prodromal symptoms (exploratory), migraine headache days with aura (exploratory), and migraine headache days during menstrual periods (secondary); for the overall double-blind period, the change in mean severity score of migraine headache days (secondary; for analysis, severity was converted to a 3-point scale, where 1 = mild, 2 = moderate, and 3 = severe, and mean severity score was calculated as the sum of the severity scores of migraine headache days during the period divided by the number of migraine headache days during the period), proportion of migraine headache days with nausea and/or vomiting (post hoc), proportion of migraine headache days with photophobia and phonophobia (post hoc), and proportion of migraine headache days during menstrual periods (post hoc).
Statistical Analysis
As reported previously [15], the planned sample size of 451 patients was based on an effect size of 0.36 and a 15% discontinuation rate, and would provide 88% power to detect a significant difference between galcanezumab and placebo for the primary endpoint. The intent-to-treat population, defined as all randomized patients who received ≥ one dose of study drug, was used for all analyses. Baseline demographic and clinical characteristics are reported as mean [standard deviation (SD)] or n (%). Changes from the baseline period were analyzed using a restricted maximum likelihood-based MMRM with treatment, month, treatment-by-month interaction, baseline value, baseline-by-month interaction, and baseline migraine headache days category (< 8 versus ≥ 8) as factors. MMRM provides an unbiased estimator under the assumption of missing at random, whereas analysis of covariance (ANCOVA) with a last observation carried forward imputation method cannot. As stated, potential baseline confounders were included in the MMRM as covariates, and the model terms would be similar between ANCOVA and MMRM (both include baseline value and baseline migraine headache days category). The overall change from baseline for months 1–6 was the average of the changes from baseline for each month. Changes from baseline are presented as least-squares (LS) means with standard errors (SE); differences in LS means compared with placebo are presented with 95% confidence intervals (CIs). No multiplicity adjustments were made. The change in the proportion of monthly migraine headache days with symptoms was calculated by subtracting the proportion at baseline (number of monthly migraine headache days with symptom during the baseline period/total number of monthly migraine headache days during the baseline period ×100) from the proportion at each month (number of monthly migraine headache days with symptom during the month/total number of monthly migraine headache days during the month × 100). Statistical tests were two-sided with a significance level of 5%. Analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Demographic and Baseline Clinical Characteristics
As reported previously [15], 459 patients were randomized to placebo (n = 230), 120 mg galcanezumab (n = 115), or 240 mg galcanezumab (n = 114); of these, 440 patients completed the study. All patients received all doses of study drug. Most patients were female, with mean age approximately 44 years and a mean of approximately 21 years since migraine diagnosis (Table 1). The mean (SD) number of monthly migraine headache days was 8.7 (2.9). Of these, a mean of 6.0 (3.3) days were with moderate-to-severe migraine headache and a mean of 1.0 (1.4) day was with severe migraine headache. The mean (SD) severity score of migraine headaches on a 3-point scale was 1.77 (0.37). Symptoms associated with migraine headache were common (Table 1). The mean (SD) number of monthly migraine headache days with nausea and/or vomiting was 3.0 (3.1), with photophobia and phonophobia was 5.1 (4.0), with prodromal symptoms was 2.4 (3.2), and with aura was 3.0 (3.5). The mean (SD) number of monthly migraine headache days during menstrual periods (n = 269) was 2.4 (1.7).
Migraine Headache Severity
Moderate-to-Severe Migraine Headache Days
Both 120 mg and 240 mg doses of galcanezumab significantly reduced the number of monthly moderate-to-severe migraine headache days compared with placebo (Fig. 1). Statistically significant differences between each dose of galcanezumab and placebo were seen at each month (Fig. 1a) and overall for months 1–6 (Fig. 1b). The overall difference in LS mean (95% CI) change from baseline in the number of monthly moderate-to-severe migraine headache days compared with placebo was −1.9 (−2.5 to −1.2) days in the 120 mg galcanezumab group and −1.8 (−2.5 to −1.2) days in the 240 mg galcanezumab group.
Severe Migraine Headache Days
Both 120 mg and 240 mg doses of galcanezumab significantly reduced the number of monthly severe migraine headache days compared with placebo (Fig. 2). Statistically significant differences between each dose of galcanezumab and placebo were seen at each month (Fig. 2a) and overall for months 1–6 (Fig. 2b). The overall difference in LS mean (95% CI) change from baseline in the number of monthly severe migraine headache days compared with placebo was −0.4 (−0.6 to −0.2) days in both the 120 mg and 240 mg galcanezumab groups.
Migraine Headache Severity Score
The overall LS mean (SE) severity score of migraine headache days across months 1–6 was reduced by −0.11 (0.02), −0.17 (0.03), and −0.20 (0.03) points for placebo, 120 mg galcanezumab, and 240 mg galcanezumab, respectively. The LS mean change difference (95% CI) versus placebo was statistically significant for the 240 mg dose (−0.09 [−0.16 to −0.03], p = 0.005), but not for the 120 mg dose [−0.06 (−0.13 to 0.00), p = 0.055].
Symptoms Associated with Migraine
Nausea and/or Vomiting
Significantly greater reductions in the number of monthly migraine headache days with nausea and/or vomiting were observed in both galcanezumab groups compared with placebo at every month (Fig. 3a) and overall across 6 months (Fig. 3b). The overall difference in LS mean (95% CI) change from baseline in the number of monthly migraine headache days with nausea and/or vomiting compared with placebo was −1.1 (−1.7 to −0.6) and −1.0 (−1.5 to −0.4) days in the 120 mg and 240 mg galcanezumab groups, respectively.
In the baseline period, the mean (SD) proportion of monthly migraine headache days with nausea and/or vomiting across all groups was 32.7% (30.2). The overall LS mean (SE) monthly reduction in the proportion of migraine headache days with nausea and/or vomiting was numerically greater in both the 120 mg [−3.7% (2.6)] and 240 mg [−7.7% (2.7)] galcanezumab groups than in the placebo group [−0.4% (1.9)]; the difference was statistically significant for 240 mg galcanezumab versus placebo (p = 0.02), but not for 120 mg galcanezumab versus placebo (p = 0.31).
Photophobia and Phonophobia
Similarly, the reduction from baseline in the number of monthly migraine headache days with photophobia and phonophobia was significantly greater in both galcanezumab groups than in the placebo group at each month (Fig. 4a) and overall (Fig. 4b). The overall difference in LS mean (95% CI) change from baseline in the number of monthly migraine headache days with photophobia and phonophobia compared with placebo was −2.3 (−3.0 to −1.6) and −1.7 (−2.4 to −1.1) days in the 120 mg and 240 mg galcanezumab groups, respectively.
In the baseline period, the mean (SD) proportion of monthly migraine headache days with photophobia and phonophobia across all groups was 55.7% (37.7). The overall LS mean (SE) monthly reduction in the proportion of migraine headache days with photophobia and phonophobia was numerically greater in both the 120 mg [−6.4% (2.8)] and 240 mg [−3.2% (2.8)] galcanezumab groups than in the placebo group [increase of +1.1% (2.1)]; the difference was statistically significant for 120 mg galcanezumab versus placebo (p = 0.03), but not for 240 mg galcanezumab versus placebo (p = 0.21).
Prodromal Symptoms
Significantly greater reductions in the number of monthly migraine headache days with prodromal symptoms were observed in both galcanezumab groups compared with placebo at most months (Fig. 5a) and overall for months 1–6 (Fig. 5b). Differences from placebo were not statistically significant for the 120 mg dose group at month 6 or for the 240 mg dose group at month 4 (Fig. 5a). The overall difference in LS mean (95% CI) change from baseline in the number of monthly migraine headache days with prodromal symptoms compared with placebo was −0.7 (−1.3 to −0.2) and −0.8 (−1.4 to −0.3) days in the 120 mg and 240 mg galcanezumab groups, respectively.
Aura
Significantly greater reductions in the number of monthly migraine headache days with aura were seen in both galcanezumab groups compared with placebo at most months (Fig. 6a) and overall for months 1–6 (Fig. 6b). Differences from placebo were not statistically significant for the 240 mg dose group at month 4, the 120 mg dose group at month 5, or for either dose group at month 6 (Fig. 6a). The overall difference in LS mean (95% CI) change from baseline in the number of monthly migraine headache days with aura compared with placebo was −0.7 (−1.2 to −0.2) days in both the 120 mg and 240 mg galcanezumab groups.
Change in Migraine Headache Days during Menstrual Periods
Among 269 women who recorded ≥ one menstrual period during the study, significantly greater reductions in the number of monthly migraine headache days during menstrual periods were observed in both galcanezumab groups compared with placebo at every month (Fig. 7a) and overall across 6 months (Fig. 7b). The overall difference in LS mean (95% CI) change from baseline in the number of monthly migraine headache days during menstrual periods compared with placebo was −0.8 (−1.2 to −0.5) and −0.9 (−1.2 to −0.6) days in the 120 mg and 240 mg galcanezumab groups, respectively.
In the baseline period, the mean (SD) proportion of monthly migraine headache days during menstrual periods (n = 269 women with ≥ one menstrual period during the study) was 27.6% (19.3) across all groups. During the double-blind phase, the proportion decreased by a mean (SE) of −3.6% (1.6) and −5.5% (1.6) in the galcanezumab 120 mg and 240 mg groups, respectively, compared with a mean decrease of −1.5% (1.1) in the placebo group (p = 0.28 for 120 mg galcanezumab versus placebo; p = 0.04 for 240 mg galcanezumab versus placebo).
Discussion
In this 6-month study, once-monthly galcanezumab significantly reduced the frequency of moderate-to-severe and severe migraine headache days, the severity of headaches, the frequency of headache days with migraine-associated symptoms, and the frequency of headache days during menstrual periods in Japanese patients with episodic migraine. These results indicate that galcanezumab treatment of Japanese patients not only reduces the number of migraine headaches, as previously demonstrated [15], but also reduces the frequency of moderate and severe headaches and migraine-associated symptoms. This is the first study to evaluate the effect of galcanezumab on migraine headache severity and associated symptoms in Japanese patients, and the first to examine galcanezumab effects on migraine headaches during menstrual periods in any population.
Consistent with analyses of global trials [16], both 120 mg and 240 mg doses of galcanezumab were effective in reducing the number of moderate-to-severe and severe migraine headache days. The headache severity score was also reduced, similar to findings in global trials [17], although statistical significance was only achieved in the 240 mg group. Significant reductions in moderate-to-severe and severe headache days were observed in the first month of treatment and were sustained throughout the 6-month study. Over the 6 months, galcanezumab treatment resulted in a mean reduction of nearly 3 days per month with moderate-to-severe migraine headache, which corresponds to approximately half the baseline mean of 6 days per month. Severe migraine headache days were reduced by approximately 0.6 days per month, more than half the baseline mean of 1 day per month. Although the absolute reduction in number of days may seem small, this is because the baseline number of days within each subcategory of migraine headache is also small. Moreover, the number of moderate-to-severe or severe migraine headache days was reduced by approximately 50% relative to baseline, which meets the American Headache Society’s criteria for successful migraine prevention [4]. Other antibodies directed against CGRP or the CGRP receptor have also been shown to reduce the frequency of moderate-to-severe headache days (fremanezumab [18]) or the severity of breakthrough migraine headaches (erenumab [19]) in patients with episodic migraine. Migraine headache frequency and severity are both important contributors to overall migraine-associated disability [20]. Thus, treatments that effectively reduce both the occurrence of migraine headache and the intensity of headaches can help reduce the burden of disease in people with migraine. Indeed, previous analyses of this Japanese trial have demonstrated that galcanezumab was associated with improved quality of life [21] and treatment satisfaction [22].
In addition to headache, migraine-associated symptoms are common, can adversely affect quality of life [23, 24], and can be associated with progression to chronic migraine [25]. In an analysis of the 2017 Japanese National Health and Wellness Survey, more than half of patients with migraine reported experiencing nausea/vomiting (59.3%), photophobia (57.4%), or phonophobia (54.5%), and 22.5% reported having aura [26]. In this study, during the baseline period, approximately one-third (mean 32.7%) of migraine headache days were accompanied by nausea and/or vomiting and more than half (mean 55.7%) by photophobia and phonophobia. Both doses of galcanezumab reduced the number of monthly migraine headache days with nausea and/or vomiting, photophobia and phonophobia, prodromal symptoms, and aura. Additionally, the proportion of migraine headache days with nausea and/or vomiting and with photophobia and phonophobia was lower with galcanezumab, although the difference from placebo was not always statistically significant. Although fremanezumab has been reported in a phase 2 randomized trial to reduce the number of days per week with nausea/vomiting and with photophobia/phonophobia, the effect on migraine headache days with these symptoms was not assessed [18]. Interestingly, a recent case report described the disappearance of aura in a patient treated with galcanezumab and reduced duration and intensity of aura in a patient treated with erenumab [27]; another case report also reported reduced aura after erenumab treatment [28]. A physician survey conducted in Germany has reported that erenumab reduced nausea/vomiting, photophobia/phonophobia, and aura [29]. A post hoc analysis of four randomized, placebo-controlled trials indicated that although erenumab reduced the number of monthly migraine headache days in patients with or without aura, it did not significantly reduce the number of monthly aura days [30]. Galcanezumab is the only CGRP antibody currently shown in clinical trials to reduce migraine headache days with prodromal symptoms and with aura. Overall, our results are consistent with those of the global galcanezumab trials [16], indicating that galcanezumab is equally effective at reducing migraine-associated symptoms in Japanese patients.
In women of reproductive age, migraine attacks disproportionately occur during or just before menstrual periods, suggesting there may be hormonal triggers for migraine onset [6, 31]. In women with menstrual-related migraine, migraine attacks that occur during menstrual periods have been reported to last longer, cause greater disability, and respond less well to acute treatments compared with migraine attacks that occur at other times [32, 33]. In this study, galcanezumab was effective in reducing the number of migraine headache days by approximately 45%, as well as the proportion of migraine headache days, that occurred during menstrual periods. Although the absolute reduction in the number of migraine headache days during menstrual periods was small, the impact is likely to be clinically meaningful because of the greater severity and duration of headaches that occur at this time [32, 33]. The effect of galcanezumab on migraine at the time of menstrual periods was not evaluated in the global galcanezumab trials [9,10,11, 16, 17]. A post hoc analysis of data from a phase 3 randomized trial indicated that erenumab reduced monthly migraine headache days compared with placebo in women with a history of menstrual migraine; however, unlike our study, the analysis did not specifically investigate migraine headaches occurring during menstrual periods separately from migraine headaches occurring outside of the 5-day perimenstrual window [34]. A real-world observational study conducted at a single center in Italy reported that CGRP/CGRP receptor antibodies, including galcanezumab, reduced the frequency, intensity, and duration of menstrual-related migraines occurring during the 5-day perimenstrual window in 40 women with ≥ three previous treatment failures [35]. Together, these results suggest that galcanezumab may be an effective preventive treatment for women experiencing migraine during menstrual periods.
Our study is a detailed analysis of data from a phase 2 multicenter, randomized placebo-controlled trial of galcanezumab in Japanese patients with episodic migraine, and is the first analysis of the effect of galcanezumab on the frequency of migraine headache days during menstrual periods. Although the primary endpoint of the trial was the reduction in overall number of migraine headache days [15], most of the secondary analyses reported here were prespecified, while some were post hoc. As a limitation, the sample size was based on the primary endpoint and may not have provided sufficient statistical power for all analyses. Additionally, the presence of aura was reported by patients and may not correspond to clinically defined aura. Similarly, patients recorded whether they had their menstrual period, with no set definition. Finally, although head-to-head comparisons between galcanezumab and other preventive medications for migraine would be useful, these trials have not yet been completed. Future investigations specifically designed to examine the effect of galcanezumab on migraine-associated symptoms, including aura, and on migraine headaches during menstrual periods are required.
Conclusion
This analysis indicates that once-monthly galcanezumab is effective at reducing the frequency of moderate-to-severe and severe migraine headache days, the severity of headaches, the frequency of migraine headache days with associated symptoms, and the frequency of migraine headache days during menstrual periods in Japanese patients with episodic migraine.
References
Safiri S, Pourfathi H, Eagan A, et al. Global, regional, and national burden of migraine in 204 countries and territories, 1990 to 2019. Pain. 2022;163(2):e293–309.
Steiner TJ, Stovner LJ, Jensen R, Uluduz D, Katsarava Z, Lifting The Burden: the Global Campaign against Headache. Migraine remains second among the world’s causes of disability, and first among young women: findings from GBD2019. J Headache Pain. 2020;21(1):137.
Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia. 2013;33(9):629–808.
American Headache Society. The American Headache Society position statement on integrating new migraine treatments into clinical practice. Headache. 2019;59(1):1–18.
Laurell K, Artto V, Bendtsen L, et al. Premonitory symptoms in migraine: a cross-sectional study in 2714 persons. Cephalalgia. 2016;36(10):951–9.
Vetvik KG, MacGregor EA. Menstrual migraine: a distinct disorder needing greater recognition. Lancet Neurol. 2021;20(4):304–15.
EMGALITY® (galcanezumab) [package insert]. Indianapolis, IN: Eli Lilly and Company; 2019.
Kielbasa W, Helton DL. A new era for migraine: pharmacokinetic and pharmacodynamic insights into monoclonal antibodies with a focus on galcanezumab, an anti-CGRP antibody. Cephalalgia. 2019;39(10):1284–97.
Skljarevski V, Matharu M, Millen BA, Ossipov MH, Kim BK, Yang JY. Efficacy and safety of galcanezumab for the prevention of episodic migraine: results of the EVOLVE-2 phase 3 randomized controlled clinical trial. Cephalalgia. 2018;38(8):1442–54.
Stauffer VL, Dodick DW, Zhang Q, Carter JN, Ailani J, Conley RR. Evaluation of galcanezumab for the prevention of episodic migraine: the EVOLVE-1 randomized clinical trial. JAMA Neurol. 2018;75(9):1080–8.
Detke HC, Goadsby PJ, Wang S, Friedman DI, Selzler KJ, Aurora SK. Galcanezumab in chronic migraine: the randomized, double-blind, placebo-controlled REGAIN study. Neurology. 2018;91(24):e2211–21.
EMGALITY® (galcanezumab) [package insert]. Kobe, Japan: Eli Lilly Japan K.K.; 2021.
Sakai F, Igarashi H. Prevalence of migraine in Japan: a nationwide survey. Cephalalgia. 1997;17(1):15–22.
Takeshima T, Ishizaki K, Fukuhara Y, et al. Population-based door-to-door survey of migraine in Japan: the Daisen study. Headache. 2004;44(1):8–19.
Sakai F, Ozeki A, Skljarevski V. Efficacy and safety of galcanezumab for prevention of migraine headache in Japanese patients with episodic migraine: a phase 2 randomized controlled clinical trial. Cephalalgia Rep. 2020;3:1–10.
Ament M, Day K, Stauffer VL, et al. Effect of galcanezumab on severity and symptoms of migraine in phase 3 trials in patients with episodic or chronic migraine. J Headache Pain. 2021;22(1):6.
Ailani J, Andrews JS, Rettiganti M, Nicholson RA. Impact of galcanezumab on total pain burden: findings from phase 3 randomized, double-blind, placebo-controlled studies in patients with episodic or chronic migraine (EVOLVE-1, EVOLVE-2, and REGAIN trials). J Headache Pain. 2020;21(1):123.
Silberstein SD, Rapoport AM, Loupe PS, et al. The effect of beginning treatment with fremanezumab on headache and associated symptoms in the randomized phase 2 study of high frequency episodic migraine: post-hoc analyses on the first 3 weeks of treatment. Headache. 2019;59(3):383–93.
Lipton RB, Dodick DW, Kudrow D, et al. Reduction in migraine pain intensity in patients treated with erenumab: a post hoc analysis of two pivotal randomized studies. Cephalalgia. 2021;41(14):1458–66.
Stewart WF, Lipton RB, Kolodner K. Migraine disability assessment (MIDAS) score: relation to headache frequency, pain intensity, and headache symptoms. Headache. 2003;43(3):258–65.
Shibata M, Nakamura T, Ozeki A, Ueda K, Nichols RM. Migraine-Specific Quality-of-Life Questionnaire (MSQ) version 2.1 score improvement in Japanese patients with episodic migraine by galcanezumab treatment: Japan Phase 2 study. J Pain Res. 2020;13:3531–8.
Tatsuoka Y, Takeshima T, Ozeki A, Matsumura T. Treatment satisfaction of galcanezumab in Japanese patients with episodic migraine: a Phase 2 randomized controlled study. Neurol Ther. 2021;10(1):265–78.
Hanson LL, Ahmed Z, Katz BJ, et al. Patients with migraine have substantial reductions in measures of visual quality of life. Headache. 2018;58(7):1007–13.
Lipton RB, Buse DC, Saiers J, Fanning KM, Serrano D, Reed ML. Frequency and burden of headache-related nausea: results from the American Migraine Prevalence and Prevention (AMPP) study. Headache. 2013;53(1):93–103.
Reed ML, Fanning KM, Serrano D, Buse DC, Lipton RB. Persistent frequent nausea is associated with progression to chronic migraine: AMPP study results. Headache. 2015;55(1):76–87.
Kikui S, Chen Y, Todaka H, Asao K, Adachi K, Takeshima T. Burden of migraine among Japanese patients: a cross-sectional National Health and Wellness Survey. J Headache Pain. 2020;21(1):110.
Albanese M, Mercuri NB. Could the new anti-CGRP monoclonal antibodies be effective in migraine aura? Case reports and literature review. J Clin Med. 2022;11(5):1228.
Matteo E, Pensato U, Favoni V, Giannini G, Pierangeli G, Cevoli S. Do anti-CGRP drugs have a role in migraine aura therapy? J Neurol. 2021;268(6):2273–4.
Straube A, Stude P, Gaul C, Schuh K, Koch M. Real-world evidence data on the monoclonal antibody erenumab in migraine prevention: perspectives of treating physicians in Germany. J Headache Pain. 2021;22(1):133.
Ashina M, Goadsby PJ, Dodick DW, et al. Assessment of erenumab safety and efficacy in patients with migraine with and without aura: a secondary analysis of randomized clinical trials. JAMA Neurol. 2022;79(2):159–68.
Cupini LM, Corbelli I, Sarchelli P. Menstrual migraine: what it is and does it matter? J Neurol. 2021;268(7):2355–63.
Granella F, Sances G, Allais G, et al. Characteristics of menstrual and nonmenstrual attacks in women with menstrually related migraine referred to headache centres. Cephalalgia. 2004;24(9):707–16.
MacGregor EA, Victor TW, Hu X, et al. Characteristics of menstrual vs nonmenstrual migraine: a post hoc, within-woman analysis of the usual-care phase of a nonrandomized menstrual migraine clinical trial. Headache. 2010;50(4):528–38.
Pavlovic JM, Paemeleire K, Göbel H, et al. Efficacy and safety of erenumab in women with a history of menstrual migraine. J Headache Pain. 2020;21(1):95.
Silvestro M, Orologio I, Bonavita S, et al. Effectiveness and safety of CGRP-mAbs in menstrual-related migraine: a real-world experience. Pain Ther. 2021;10(2):1203–14.
Acknowledgements
The authors would like to thank all study participants.
Funding
This study was funded by Eli Lilly Japan K.K., Kobe, Japan, manufacturer/licensee of galcanezumab in Japan. Eli Lilly Japan K.K. and Daiichi Sankyo Company, Limited funded the journal’s Rapid Service Fee.
Medical Writing Assistance
Medical writing assistance was provided by Rebecca Lew, PhD, CMPP, and Prudence Stanford, PhD, CMPP, of ProScribe—Envision Pharma Group, and was funded by Eli Lilly Japan K.K. and Daiichi Sankyo Company, Limited. ProScribe’s services complied with international guidelines for Good Publication Practice.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Hisaka Igarashi and Mamoru Shibata were investigators in the study, and participated in the interpretation of study results and in the drafting, critical revision, and approval of the final version of the manuscript. Akichika Ozeki was involved in the study design and statistical analysis, and participated in the interpretation of study results and in the drafting, critical revision, and approval of the final version of the manuscript. Taka Matsumura participated in the interpretation of study results and in the drafting, critical revision, and approval of the final version of the manuscript.
Prior Presentation
This manuscript contains some data that were previously presented at the 50th Annual Meeting of the Japanese Headache Society, Tokyo, Japan (November 25–26, 2022).
Disclosures
Hisaka Igarashi received personal fees for speaker and consulting services from Eli Lilly Japan K.K., Amgen K.K., Otsuka Pharmaceutical Co., Ltd, Eisai Co., Ltd., Lundbeck Japan K.K., Pfizer Japan Inc., Sawai Pharmaceutical Co., Ltd., Takeda Pharmaceutical Company Limited, and Daiichi Sankyo Company, Limited. Mamoru Shibata received personal fees for consulting services from Eli Lilly Japan K.K. and Otsuka Pharmaceutical Co., Ltd, and honoraria from Amgen K.K. Akichika Ozeki and Taka Matsumura are employees of Eli Lilly Japan K.K. and minor shareholders in Eli Lilly and Company.
Compliance with Ethics Guidelines
The protocol was approved by the local institutional review boards (Table S1). All patients provided written informed consent before any study procedures. The study was conducted in accordance with the Declaration of Helsinki, Good Clinical Practice, and the Council for International Organizations of Medical Sciences International Ethical Guidelines.
Data Availability
Eli Lilly and Company provides access to all individual participant data collected during the trial, after anonymization, with the exception of pharmacokinetic or genetic data. Data are available to request 6 months after the indication studied has been approved in the United States and the European Union and after primary publication acceptance, whichever is later. No expiration date of data requests is currently set once data are made available. Access is provided after a proposal has been approved by an independent review committee identified for this purpose and after receipt of a signed data sharing agreement. Data and documents, including the study protocol, statistical analysis plan, clinical study report, blank or annotated case report forms, will be provided in a secure data sharing environment. For details on submitting a request, see the instructions provided at www.vivli.org.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Igarashi, H., Shibata, M., Ozeki, A. et al. Galcanezumab Effects on Migraine Severity and Symptoms in Japanese Patients with Episodic Migraine: Secondary Analysis of a Phase 2 Randomized Trial. Neurol Ther 12, 73–87 (2023). https://doi.org/10.1007/s40120-022-00410-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40120-022-00410-3