Abstract
Introduction
The healthcare situation of multiple sclerosis (MS) and its course are not being thoroughly investigated in Japan. We aimed to examine the current healthcare situation, including treatment and healthcare costs, of MS according to duration since its first diagnosis using Japanese real-world data to determine unidentified healthcare issues at each disease stage.
Methods
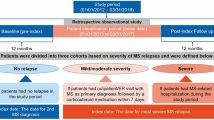
This retrospective, non-comparative, non-interventional study used a Japanese nationwide claims database (April 2008–August 2018) comprising 20 million patients from 329 acute care hospitals (as of June 2018). Treatment patterns, comorbidities, healthcare resource utilization, and healthcare costs were analyzed using longitudinal analyses of patients with MS according to duration since the first diagnosis. The time from diagnosis to first treatment was examined using Kaplan–Meier analysis.
Results
We identified 7067 patients with MS [mean (standard deviation) age at first diagnosis 45.0 (16.2) years]. About 70% of the patients did not receive disease-modifying therapy (DMT) within the first year of diagnosis. The frequency of DMT use decreased in patients with a longer duration since the first diagnosis. MS treatment costs tended to increase with a longer duration from the first diagnosis until 9 years, followed by a tendency to decrease; contrastingly, other healthcare costs tended to increase with duration after decreasing from the year of the first diagnosis to the next year. The frequencies of hospitalizations and hospital visits, healthcare costs—excluding those for MS treatment and tests—and prevalence of comorbidities tended to be higher in patients with a longer duration since the first diagnosis.
Conclusion
A considerable proportion of patients did not receive DMT, suggesting that patients with early-stage MS may lose the opportunity to improve their prognosis through early intervention with DMT. Among patients with a longer duration since the first diagnosis, fewer treatment choices may be available despite the larger clinical and treatment burden.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Patients with multiple sclerosis (MS) commonly experience long and diverse disease courses. However, treatment status and economic burden associated with MS disease courses have been reported mainly in the USA and Europe |
In Japan, novel treatments for MS have been introduced later, and fewer options of disease-modifying therapies (DMTs) are available than in the USA and Europe. Considering the differences between countries, the current healthcare situation in Japan should be investigated to find unidentified healthcare issues at each stage of the disease |
We analyzed the nationwide claims database by duration (in years) since the first diagnosis and by age to assess the current healthcare situation, including prescribed drugs, healthcare resource utilization, costs, and comorbidities of MS over the disease course |
What was learned from the study? |
Use of DMT was observed from the first year of diagnosis; however, about 70% of the patients did not receive treatment with DMT within the first year. The frequency of hospitalizations and hospital visits, healthcare costs—excluding those for MS treatment and tests—and prevalence of comorbidities tended to be higher in patients with a longer duration since the first diagnosis |
A considerable proportion of patients did not receive treatment with DMT, suggesting that patients at an early stage of MS may lose the opportunity to improve their prognosis by early intervention with DMT. In patients with a longer duration since the first diagnosis, it is supposed that fewer treatment choices were available despite suffering from larger clinical and treatment burden |
Introduction
Patients with multiple sclerosis (MS) commonly experience long and diverse disease courses. The majority of patients with MS are diagnosed with relapsing–remitting MS (RRMS), and more than half of those with RRMS are reported to transition to secondary-progressive MS (SPMS) within 15–20 years from disease onset [1, 2]. SPMS is a subtype of the disease characterized by permanent disability progression independent of relapse.
Treatment status and economic burden associated with MS disease course have been reported mainly in the USA and Europe, where high prevalence leads to a high impact on society. MS negatively affects the lives of patients and their families and leads to significant and long-term health and economic burdens [3]. In 2020, the prevalence was reportedly 288 per 100,000 in the USA and ranged from below 40 to more than 300 per 100,000 in European countries [4]. Disease-modifying therapy (DMT) is usually used for patients with RRMS to treat their symptoms of relapse [3]. The first DMT, interferon-β1b, was launched in 1993, and the number of DMTs on the market has been rapidly increasing; the US Food and Drug Administration (FDA) approved 18 DMTs as of 2021 [5].
The findings from other countries may not be directly applied to the situation in Japan, considering the differences in the approved treatments. Although an increase in the prevalence has been reported in Japan [6, 7], it is much lower than in the USA and Europe, that is, 7.7 per 100,000 in 2003 [8] or 15–19 per 100,000 in 2011–2015 [7]. Novel treatments have been introduced later than those in the USA and Europe. Interferon-β1b was released to the market in November 2000 as the first DMT, whereas interferon-β1a (launched in November 2006), fingolimod (November 2011), natalizumab (June 2014), glatiramer acetate (November 2015), and dimethyl fumarate (February 2017) had been available for RRMS treatment. While the efficacy of these DMTs has been proven in RRMS, no DMT had been proven for effectiveness in SPMS [9, 10] until siponimod was approved as the first DMT specifically indicated for SPMS in Japan in June 2020. In the guideline published in 2010, only interferon-β1b was included as DMT, and long-term administration of oral corticosteroid was not denied [11]. Also, in the treatment guidelines in 2017, six DMTs and several immunosuppressants were included for MS treatment, but the oral corticosteroid was not recommended because of lack of evidence [12].
To investigate the current healthcare situation for patients with MS in Japan, a nationwide claims database analysis is suitable considering its low prevalence rate and long and diverse disease course. Several studies using Japanese claims databases provided various types of information regarding treatment for MS in a Japanese real-world setting, including treatment status and costs for all patients and by age groups [13], an increase in prevalence and treatment costs by year [6, 7], and a decrease in the frequency of relapse and hospitalizations by year [6].
Information related to the current healthcare situation of MS, along with the disease course, is important to assess the effect of change on the treatment situation and to find issues along with disease status. However, no claims database includes disease course and disability status information in Japan. Therefore, to provide such information along with MS disease status, we considered referring to disease duration and age as alternative indicators of disease stage. Moreover, no studies have described the treatment situation by disease duration using claims databases in the country. Therefore, we assessed the current healthcare situation, including prescribed drugs, healthcare resource utilization, costs, and comorbidities of MS over the disease course, to clarify unidentified healthcare issues in Japan at each stage based on a claims data analysis by duration (in years) since first diagnosis and age.
Methods
Study Design
This is a retrospective, non-comparative, non-interventional study of patients with MS using a Japanese claims database (April 2008–August 2018). We analyzed treatment patterns, comorbidities, healthcare resource utilization, and healthcare costs by duration since first diagnosis and age.
Data Source and Settings
We used a claims database comprising data collected from acute care hospitals adopting the Japanese Diagnosis and Procedure Combination (DPC)/Per-Diem Payment System (called DPC hospitals) [14]. The Medical Data Vision Co., Ltd provided the database through a contract to Novartis Pharma K.K., and Novartis Pharma K.K. had permission to access and use the data based on the contract. As of April 2018, 1730 DPC hospitals existed, 83% of which were relatively large hospitals with more than 100 beds [15]. The total number of beds in DPC hospitals in Japan was approximately 490,000, covering 55% of all hospital beds for general patients.
The database used in this study included 20 million patients from 329 DPC hospitals as of June 2018. It also included patients who had received any medical practice, regardless of age and type of insurance, and all diagnoses and medical procedures, including prescriptions, clinical tests, and surgeries given to inpatients and outpatients in the hospitals. However, diagnoses or medical procedures given in other settings were not recorded in the database.
The observation period of each patient was from the first record until the last record of their medical visits, and the data collection period was between 2009 and 2018. The results were stratified by year and month of each record with the threshold of November 2011, when fingolimod was launched in Japan. Given that we found some differences in the outcomes in the period before the threshold, we only included records after November 2011 to describe the most recent situation prior to the availability of siponimod. The database had records of the first diagnosis of each disease as “From Date,” which can be outside the observation period of this study, and the earliest From Date of MS was defined as the first diagnosis of MS.
We identified patients with MS based on the algorism validated in a previous study using the same database [13] as presented in Table 1. MS diagnosis was coded as G35 by the International Statistical Classification of Diseases and Related Health Problems, 10th revision (ICD-10) [16]. The diagnosis implies “definitive diagnosis” and does not include “suspected diagnosis” in this study.
Analysis
We assessed treatment patterns, comorbidities, healthcare resource utilization, and healthcare costs by duration (in years) since the first diagnosis through longitudinal analyses from November 2011 to August 2018 or by age through cross-sectional analyses in 2017. The results were assessed on the basis of descriptive statistics.
As the treatment pattern, we calculated the frequency of treatment per patient per month (PPPM) for immunosuppressive/immunomodulatory treatments, including the following classes of treatments: DMTs, oral steroids, relapse treatments, and immunosuppressants. Specifically, DMTs included interferon-β1b, interferon-β1a, fingolimod, natalizumab, glatiramer acetate, and dimethyl fumarate. Supplementary Material Table S1 shows the classification and definitions of the treatments based on the general name for drugs or procedure price table code for procedures. In addition, time from diagnosis to first treatment was analyzed through Kaplan–Meier analyses for DMT, any immunosuppressive/immunomodulatory treatments, or immunosuppressive/immunomodulatory treatments besides relapse treatments. Patients having the first MS diagnosis during the observation period were included in this analysis.
Regarding the comorbidities, we selected remarkable diseases/symptoms that are often present in patients with MS with the help of a medical expert (I.K.). The comorbidities, which may include symptoms of MS with diagnoses other than MS, were defined by ICD-10 code (Supplementary Material Table S2). The prevalence per patient month was calculated for each comorbidity.
We analyzed the prevalence of diseases diagnosed before the first diagnosis of MS by year to examine the changes in diseases before developing MS. Patients having at least 1-month observation periods before the first MS diagnosis were included in this analysis. The diseases were identified on the basis of the standard disease name, which has been used to record diagnoses in Japan. The prevalence of each disease was calculated by year before the first diagnosis. We compared the prevalence in the year before the first diagnosis (year 0, 12 months from the first MS diagnosis) to 1 year prior (year − 1), and calculated the difference as (prevalence in year 0) − (prevalence in year − 1). We calculated the P values by z test to test the null hypothesis that the prevalence in year 0 and year − 1 is equal, and p < 0.05 was defined as statistically significant. We identified the diseases that increased before the first diagnosis, defined as those with larger prevalence in year 0 than year − 1 with statistical significance. The identified diseases were listed in descending order from the largest slope, calculated as the change in prevalence over the change in a year from year − 6 to year 0 using a linear regression model.
We described healthcare resource utilization, including frequency (PPPM) of clinical tests (defined by procedure price table code as shown in Supplementary Material Table S3), hospitalizations, relapse treatments, and hospital visits. As the database did not have a record of relapse, we defined the relapse treatment based on the treatments for relapse, including administration of steroid pulse therapy and plasma purification therapy (see Supplementary Material Table S1). As for the healthcare costs (PPPM), we estimated total costs and their breakdown: MS treatment costs for immunosuppressive/immunomodulatory treatments, clinical test costs (for those defined above), and other healthcare costs.
To assess the effect of aging on other healthcare costs by duration since the first diagnosis, we developed a multivariate model to estimate the other healthcare costs between 12 and 120 months from the first diagnosis of MS as follows:
where X is other healthcare costs and FinFlg is whether in November 2011 or later (1) or not (0). We estimated β1, β2, and β3 and compared them to assess the effect of each parameter.
We conducted the analyses using SAS version 9.4 (SAS Institute Inc., Cary, NC) and Microsoft Excel 2016 (Microsoft, Redmond, WA). The P values were calculated using the t test or the test for the difference in proportions, and p < 0.05 was considered statistically significant.
Ethics Approval and Consent to Participate
The study was approved by Clinical Research Promotion Network Japan (CR-IRB-0094). Clinical trial registration was not required for this study because it did not involve any intervention.
The database includes data collected for secondary use and was provided after anonymization. Therefore, informed consent was not required according to ethical guidelines in Japan.
Results
Patient Identification
In the database, we identified 7067 patients (mean ± standard deviation age at first diagnosis 45.0 ± 16.2; percentage of female patients 65.6%) (Table 1). Among them, 3157 patients had their first MS diagnosis during the observation period. They were included in the Kaplan–Meier analyses to examine the time from diagnosis to first treatment, and 1298 patients had at least 1-month observation periods before the first MS diagnosis and were included to analyze the prevalence of diseases before the first MS diagnosis.
Treatment Pattern
Figure 1 presents the frequency of each treatment by duration (in years) since the first diagnosis. The frequency of DMT use did not change significantly over 15 years from the first diagnosis (p = 0.85) but declined sharply in years 16–20. Meanwhile, the frequency of prednisolone use increased for patients with a longer duration since their first diagnosis (10 years or more). Regarding patients’ age, DMT was often prescribed to patients in their 20s–40s and less often to those aged 50 or above. Prednisolone was the most common treatment for elderly patients (Supplementary Material Fig. S1). Among the DMTs, fingolimod was most frequently administered at 9.7% (PPPM) in the first year, without any significant increase or decrease over the next 10 years (p = 0.43), then gradually decreasing thereafter (Fig. 1).
Treatment pattern by duration (in years) since first diagnosis since November 2011. The percentage for no treatment refers to the percentage of patients without any treatment listed above per patient month, and for each treatment per patient per month. aOral steroid is prednisolone excluding those prescribed within 3 months of prescription with other relapse treatment drug(s) than prednisolone. The colors are assigned for all drugs as the color scale bar. DMT disease-modifying therapy, IFN interferon
Figure 2 shows the time taken to receive the first treatment from the first diagnosis of MS. The percentage of patients who had received any DMT was 27.2% within 6 months and 29.2% within 1 year from the first diagnosis. Only about half of the patients were prescribed DMT over 4 years from the first diagnosis among those prescribed any immunosuppressive/immunomodulatory treatments.
Comorbidities
Among the diseases/symptoms selected as those frequently existing in patients with MS, constipation showed the highest prevalence (Fig. 3). Prevalence tended to increase with a longer duration since the first diagnosis for most diseases/symptoms: excess 25% for constipation and 10% for polyneuropathy, depressive episodes, epilepsy, and neuromuscular dysfunction of the bladder after 10 years since diagnosis. A higher prevalence of constipation was also observed in all age bands (Supplementary Material Fig. S2). Prevalence of these four diseases/symptoms was also high in older age bands (50–59 or higher), while the prevalence of headaches was similar to or higher than in the younger age band.
Diagnoses Before First Multiple Sclerosis Diagnosis
Figure 4 shows the diseases with significantly increased prevalence before the first MS diagnosis. Prevalence of various diseases, including insomnia, intractable reflux esophagitis, and hypertension, increased immediately before the first diagnosis compared to the year prior.
Prevalence of diseases diagnosed before first MS diagnosis. Diseases that significantly increased in prevalence in 1 year before the first diagnosis (year 0) from 1 year prior (year − 1) are listed in descending order from the largest slope. aP value, between 0 and year − 1; bSlope, change in prevalence over the change in year from year − 6 to year 0 using a linear regression model. The colors are assigned according to the color scale bar
Healthcare Resource Utilization and Costs
Clinical tests, hospitalizations, relapse treatments, and hospital visits were the most frequent, and total healthcare costs were the highest in the year of the first diagnosis (Fig. 5). The total healthcare costs were more than Japanese yen (JPY) 160,000 (PPPM, US$ 1487.19, as of June 2020; JPY 1 is equivalent to US$ 0.0093). Then, it decreased to about JPY 92,000 after the first year. MS treatment costs tended to increase with longer duration since the first diagnosis for up to 9 years but tended to decrease later. Other healthcare costs decreased from JPY 107,000 in the year of the first diagnosis to JPY 34,000 after 1 year but tended to increase thereafter. MS treatment costs were higher for patients in their 20s–40s and tended to decrease with age (Supplementary Material Fig. S3). Other healthcare costs tended to increase after age 50. Using a multivariate model, we assessed the effect of aging on the increase in other healthcare costs with duration since the first diagnosis, as shown in Fig. 5.
Healthcare resource utilization and healthcare costs by duration (in years) since the first diagnosis since November 2011. JPY Japanese yen, MRI magnetic resonance imaging, PPPM per patient per month. The colors are assigned by each item group (clinical tests, hospitalization, relapse, hospital visit, or healthcare costs) according to the color scale bar
The coefficient of the multivariate model was calculated as 14.8 (p < 0.001) for β1, 2001.5 (p < 0.001) for β2, and 2192.7 (p < 0.001) for β3. The coefficient of duration since the first diagnosis was significantly higher than that of age at the first diagnosis.
Discussion
In this study, we showed several dimensions of treatment management and healthcare costs for Japanese patients with MS, along with duration since first diagnosis and age. Our results suggested several issues in each stage of MS, including a low proportion of treated patients during several years since the first diagnosis and a decrease in the frequency of DMT use in the later stage of MS.
Although the database did not include information associated with MS disease status, we considered that the healthcare situation by disease course could be assessed on the basis of the analyses of the claims database, including data from DPC hospitals by duration since first diagnosis and age. Nevertheless, when interpreting the results, we should consider some limitations associated with the nature of the study design using this database. We used the duration (in years) since the first diagnosis recorded in the database, not disease duration, as an alternative indicator of disease status because information on the disease onset could not be obtained. Patients assigned to the same duration since the first diagnosis may not always have the same disease duration because the time from disease onset to diagnosis varies from patient to patient. In addition, the database did not have a record of diagnoses and treatments given in other settings; the first diagnosis in the database may not be an exact first diagnosis for some patients, and these patients could be assigned to an earlier duration since the first diagnosis group than the actual duration. However, as MS prevalence is relatively low in Japan, many patients, especially those treated with DMT, may start treatment for MS in relatively large hospitals. A previous study using another Japanese claims database, comprising data from health insurance societies, reported that 46% of patients with MS mainly visited large hospitals with more than 500 beds. Sixty-seven percent visited relatively large hospitals with more than 100 beds [7]. The study also reported that the DMT prescription rate was positively correlated with the number of beds; more than 50% of the patients received DMT in hospitals with more than 500 beds, whereas approximately 20% or 15% of those received DMT in hospitals with fewer than 100 beds or clinics (fewer than 20 beds), respectively [7]. Consequently, this study may describe the current healthcare situation of most patients, and a larger proportion of patients treated with DMT were included than the entire MS population. Notably, higher mean age at first diagnosis in this study (45.0 ± 16.2 years) than the age at the onset of MS in a previous study (32 ± 13 years) [8] may be associated with the gap between MS onset and diagnosis, and the possibility that some patients were given the first diagnosis in other settings prior to visiting the DPC hospitals.
Use of DMT was observed from the same year of the first diagnosis; however, about 70% of patients had not received any DMT 1 year after diagnosis. This proportion is lower compared to the reports from the USA that show that the percentages of patients who received DMT in 2015 were 73% for all patients with MS and 62% for those who were newly diagnosed with MS in 2015 (based on analyses of the Market Scan commercial insurance database) [17]. In the previous study, the percentage of patients who received DMT was calculated on the basis of a snapshot analysis. Specifically, the number of patients who had at least one claim for DMT in a 12-month period in 2015 was divided by the number of patients who were identified with MS in 2015 or any previous year (for all patients) or those identified in 2015 only (for those who were newly diagnosed with MS in 2015). Possible reasons for the lower number of DMT prescriptions include the fact that there are fewer approved types of DMT, and patients with atypical or benign MS, who may be less frequently treated with DMT, seem more common in Japan [18,19,20], rather than in the USA and European countries. The financial aid scheme for incurable diseases, which was reformed in January 2015, may also be associated with a low treatment rate for DMT in Japan at the early stage. It is allowed only for those with severe disease status—meeting either the severity criteria (either Expanded Disability Status Scale [EDSS] ≥ 4.5 or visual disability ≥ II in the severity scale of retinal pigmentary degeneration, or both) or the cost criteria (at least 3 months per year with the total monthly healthcare cost exceeding JPY 33,330) [21]. As newly diagnosed patients do not often meet the criteria for the certification, they may be discouraged from starting DMT at an early stage. Moreover, those who were temporarily given MS diagnosis for differential diagnosis, including clinically isolated syndrome, might remain in the analysis. However, we attempted to exclude such patients by using the algorithm (Table 1) and excluding the suspected diagnosis code of MS.
DMT is usually prescribed in the perspective of preventing relapses but the treatment goal should rather be to reduce disability progression, which is supposed to contribute to long-term clinical and social prognosis [22, 23]. Early intervention with DMT (within 5 years of disease onset) was reported to be associated with a significantly lower risk of conversion to SPMS compared with later intervention (after 5 years of disease onset) [24]. Another report argued that treatment with DMT should begin soon after MS diagnosis and continue unless a suboptimal treatment response or intolerable side effects appear [23]. The Japanese treatment guidelines also recommend early commencement of DMT for patients with RRMS [12]. Considering these facts, our finding of the low treatment rate with DMT in the early stage of MS may suggest that there is still room for improvement in the long-term prognosis by early intervention with DMT in Japan.
Lower frequency of DMT use among patients with a longer duration since the first diagnosis and elderly patients observed in this study may be due to the relatively fewer benefits of the current DMTs for patients at their later stage. Presumably, the frequency of relapse is lower, and possible side effects are higher in later stages than in earlier stages. In the American Academy of Neurology guidelines, continuous use of DMT is recommended for patients with RRMS, even for those with stable MS. However, for patients with SPMS, the likelihood of future relapse considering a patient’s age, duration since the first diagnosis, relapse history, and MRI-detected activity should be assessed; further, discontinuation of DMT may be advised in those without ongoing relapses and those who have not been ambulatory treated for at least 2 years [25]. Our finding may suggest that Japan has fewer treatment options with a favorable risk–benefit balance for patients with late-stage MS during the study period.
It is noteworthy that prednisolone was frequently used for patients in their later stages. This is probably because such patients were diagnosed and started treatment in times when MS and neuromyelitis optica were not clearly differentiated. Previously, oral steroids were frequently used and this older form of treatment may have continued until the patients were in the later stages [26]. Notably, frequent use of prednisolone, more than 30% in 2015 without excluding those for relapse treatment, for all patients was also reported in a previous study using another Japanese claims database, including data of treatments in all settings for patients mostly aged less than 65 years [7].
We observed a higher prevalence of various diseases/symptoms with an extended duration since the first diagnosis. However, aging could be one factor suggesting that the disease burden becomes higher in patients at a later stage. Meanwhile, depression is reported to be a frequent comorbidity for patients with MS [27]. Our results that indicate a higher prevalence of depression in patients with a longer duration since the first diagnosis suggest that more mental healthcare is required for those at the later stage of the disease. However, it should be noted that some diagnoses might be coded to prescribe a specific drug to treat an MS symptom (e.g., antidepressants for pain and antiepileptics for painful muscle spasms).
Interestingly, an increase in the prevalence of some diseases was observed in advance of the MS diagnosis. A prodromal period in MS has been suggested in recent years. A Canadian population-based cohort study reported that patients with MS had more frequent use of healthcare [28] and more psychiatrist and urologist encounters [29] compared with matched controls 5 years before a first demyelinating event. An increase in some diseases, including insomnia and constipation, in the study could also be indicative of such MS prodromes in Japanese patients. We simply examined prevalence of diseases by year before the first MS diagnosis to obtain basic information; further study is needed to confirm the relationship of the increase in these diseases to MS development.
An increase in other healthcare costs in later stages may be related to a trend of increasing healthcare costs with age in general. However, the results of the multivariate analysis indicated higher associations of duration since the first diagnosis with other healthcare costs, compared with the age at first diagnosis. Therefore, the increase in other healthcare costs in later stages may be attributed to the increase in the disability status of MS rather than to the general impact of aging. In previous studies about the relationship between healthcare costs and EDSS in Finland [30], Brazil [31], the Netherlands [32], and Austria [33], costs were strongly associated with disability status. These results indicated that the MS treatment costs increased during the initial period (up to 9 years from the first diagnosis) but decreased later. It was also reported that MS treatment costs are low in patients with higher disability status [30,31,32]. These results are consistent with these reports, given that the duration since the first diagnosis is associated with disability status. Notably, the impact of indirect costs on society has been reported, and the indirect costs related to productivity loss associated with MS were higher in patients with higher EDSS scores [34]. Further research may be needed to assess the comprehensive impact of MS on society, including indirect costs in Japan.
Limitations
There are several limitations in this study. As described previously (second paragraph of the “Discussion” section), we used the duration since the first diagnosis as an alternative indicator of disease status, which started later than disease onset, and the time from onset to the first diagnosis may differ among patients. Moreover, the first diagnosis in the database was not an exact first diagnosis for some previously diagnosed patients in other settings. Therefore, the patients assigned to the same duration since the first diagnosis group may not have a similar disease duration. Next, this study may include more patients who required aggressive treatments than general patients.
As this study is based on secondary use of claims data, the accuracy of the records affects our results. In particular, as mentioned in the “Discussion” section, some diagnoses may be given due to diagnostic tests or prescriptions of particular drugs. Meanwhile, information on treatments and diagnostic tests are assumed to be accurately recorded because claims are generated to claim medical care fees. Subsequently, as the database did not have records of relapses, we defined it based on records for treatments that are usually used for relapses. Therefore, treatments for symptoms other than relapses of MS might have been included, and relapses that may have occurred without treatment were not included. Finally, although we performed longitudinal analyses by duration since the first diagnosis, not all patients have records from their first year since diagnosis; thus, those included in each year were different.
Conclusions
This study showed that the use of DMT was observed from the first year of diagnosis; however, a considerable proportion of patients did not receive treatment with DMT. This finding suggests that patients in Japan at an early stage of MS may lose the opportunity to improve their long-term prognosis through early intervention with DMT. We also demonstrated that patients with a longer duration since the first diagnosis had received less treatment with DMT. They had higher frequencies of hospitalizations and hospital visits, higher miscellaneous costs, and a higher prevalence of comorbidities. The clinical situations in Japan are different from those in the USA and Europe. We believe that this study provides essential information to consider better treatment for patients with MS in Japan through the disease course.
References
Tremlett H, Zhao Y, Devonshire V. Natural history of secondary-progressive multiple sclerosis. Mult Scler. 2008;14:314–24.
Scalfari A, Neuhaus A, Daumer M, Muraro PA, Ebers GC. Onset of secondary progressive phase and long-term evolution of multiple sclerosis. J Neurol Neurosurg Psychiatry. 2014;85:67–75.
Giovannoni G, Butzkueven H, Dhib-Jalbut S, et al. Journal Brain health: time matters in multiple sclerosis. Mult Scler Relat Disord. 2016;9(Suppl 1):S5–48.
MS International Fundation. Atlas of MS 3rd edition. 2020. https://www.msif.org/wp-content/uploads/2020/10/Atlas-3rd-Edition-Epidemiology-report-EN-updated-30-9-20.pdf. Accessed 1 Nov 2021.
National Murtiple Sclerosis Society. Disease-modifying therapies for MS. July 2021. https://www.nationalmssociety.org/NationalMSSociety/media/MSNationalFiles/Brochures/Brochure-The-MS-Disease-Modifying-Medications.pdf. Accessed 1 Nov 2021.
Eskandarieh S, Heydarpour P, Minagar A, Pourmand S, Sahraian MA. Multiple sclerosis epidemiology in East Asia, South East Asia and South Asia: a systematic review. Neuroepidemiology. 2016;46:209–21.
Ogino M, Okamoto S, Ohta H, et al. Prevalence, treatments and medical cost of multiple sclerosis in Japan based on analysis of a health insurance claims database. Clin Exp Neuroimmunol. 2017;8:318–26.
Osoegawa M, Kira J, Fukazawa T, et al. Temporal changes and geographical differences in multiple sclerosis phenotypes in Japanese: nationwide survey results over 30 years. Mult Scler. 2009;15:159–73.
Placebo-controlled multicentre randomised trial of interferon beta-1b in treatment of secondary progressive multiple sclerosis. European Study Group on interferon beta-1b in secondary progressive MS. Lancet. 1998;352:1491–1497.
La Mantia L, Vacchi L, Rovaris M, et al. Interferon beta for secondary progressive multiple sclerosis. Cochrane Database Syst Rev. 2012;1:CD005181.
Treatment Guidelines for Multiple Sclerosis Development Committee. Treatment guidelines for multiple sclerosis. Tokyo: Igaku-Shoin; 2010. (in Japanese).
Multiple Sclerosis and Neuromyelitis Optica Guideline Development Committee. Guidelines for multiple sclerosis and neuromyelitis optica. Tokyo: Igaku-Shoin; 2017. (in Japanese).
Ogino M, Kawachi I, Otake K, et al. Current treatment status and medical cost for multiple sclerosis based on analysis of a Japanese claims database. Clin Exp Neuroimmunol. 2016;7:158–67.
Ishii M. DRG/PPS and DPC/PDPS as prospective payment systems. Japan Med Assoc J. 2012;55:279–91.
Central Social Insurance Medical Council, Ministry of Health, Labor and Welfare. [Estimated scale of DPC hospitals and preparatory hospitals (as of April 1, 2020)]. https://www.mhlw.go.jp/content/12404000/000640465.pdf. Accessed 26 Oct 2021. (in Japanese).
Ministry of Health, Labor and Welfare. Statistical classification of diseases and cause of death 2013. http://www.mhlw.go.jp/toukei/sippei/. Accessed 23 Dec 2020. Japanese.
Pyenson BS, Tomicki S. Multiple sclerosis: new perspectives on the patient journey: 2019 Update. USA Report, Milliman. 2019. https://us.milliman.com/en/insight/multiple-sclerosis-new-perspectives-on-the-patient-journey-2019-update. Accessed 20 Mar 2019.
Matsuoka T, Matsushita T, Kawano Y, et al. Heterogeneity of aquaporin-4 autoimmunity and spinal cord lesions in multiple sclerosis in Japanese. Brain. 2007;130:1206–23.
Piccolo L, Kumar G, Nakashima I, et al. Multiple sclerosis in Japan appears to be a milder disease compared to the UK. J Neurol. 2015;262:831–6.
Yoshimura S, Isobe N, Yonekawa T, et al. Genetic and infectious profiles of Japanese multiple sclerosis patients. PLoS ONE. 2012;7: e48592.
Japan Intractable Diseases Information Center. Information on the financial aid for the patients with the designated incurable diseases. http://www.nanbyou.or.jp/entry/5460. Accessed Dec 25, 2020. (in Japanese).
Costello K, Halper J, Kalb R, Skutnik L, Rapp, R. The use of disease-modifying therapies in multiple sclerosis: principles and current evidence. A Consensus Paper by the Multiple Sclerosis Coalition. 2020. http://www.nationalmssociety.org/NationalMSSociety/media/MSNationalFiles/Brochures/DMT_Consensus_MS_Coalition.pdf. Accessed Dec 25, 2020.
Hart FM, Bainbridge J. Current and emerging treatment of multiple sclerosis. Am J Manag Care. 2016;22:s159-170.
Brown JWL, Coles A, Horakova D, et al. Association of initial disease-modifying therapy with later conversion to secondary progressive multiple sclerosis. JAMA. 2019;321:175–87.
Rae-Grant A, Day GS, Marrie RA, et al. Practice guideline recommendations summary: disease-modifying therapies for adults with multiple sclerosis: report of the guideline development, dissemination, and implementation subcommittee of the American Academy of Neurology. Neurology. 2018;90:777–88.
Kuroiwa Y, Igata A, Itahara K, Koshijima S, Tsubaki T. Nationwide survey of multiple sclerosis in Japan. Clinical analysis of 1,084 cases. Neurology. 1975;25:845–51.
Marrie RA. Comorbidity in multiple sclerosis: implications for patient care. Nat Rev Neurol. 2017;13:375–82.
Wijnands JMA, Kingwell E, Zhu F, et al. Health-care use before a first demyelinating event suggestive of a multiple sclerosis prodrome: a matched cohort study. Lancet Neurol. 2017;16:445–51.
Wijnands JM, Zhu F, Kingwell E, et al. Five years before multiple sclerosis onset: phenotyping the prodrome. Mult Scler. 2019;25:1092–101.
Ruutiainen J, Viita AM, Hahl J, Sundell J, Nissinen H. Burden of illness in multiple sclerosis (DEFENSE) study: the costs and quality-of-life of Finnish patients with multiple sclerosis. J Med Econ. 2016;19:21–33.
da Silva NL, Takemoto MLS, Damasceno A, et al. Cost analysis of multiple sclerosis in Brazil: a cross-sectional multicenter study. BMC Health Serv Res. 2016;16:102.
Karampampa K, Gustavsson A, van Munster ET, et al. Treatment experience, burden, and unmet needs (TRIBUNE) in Multiple Sclerosis study: the costs and utilities of MS patients in the Netherlands. J Med Econ. 2013;16:939–50.
Palmer AJ, Colman S, O’Leary B, et al. The economic impact of multiple sclerosis in Australia in 2010. Mult Scler. 2013;19:1640–6.
Stawowczyk E, Malinowski KP, Kawalec P, Moćko P. The indirect costs of multiple sclerosis: systematic review and meta-analysis. Expert Rev Pharmacoecon Outcomes Res. 2015;15:759–86.
Acknowledgements
Funding
Sponsorship for this study and the journal’s Rapid Service Fee were funded by Novartis Pharma K.K.
Editorial Assistance
Editorial assistance in the preparation of this article was provided by Editage (www.editage.com). Support for this assistance was funded by Novartis Pharma K.K.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work, and have given their approval for this version to be published.
Author Contributions
Izumi Kawachi, Hiromichi Otaka, and Kengo Ueda contributed to the study conception and design. Data analysis was performed by Kosuke Iwasaki. All authors contributed to interpret the data. The first draft of the manuscript was written by Tomomi Takeshima and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Prior Presentation
Parts of this work were presented at the 12th Annual Congress of the Pan-Asian Committee on Treatment and Research in Multiple Sclerosis, Singapore, November 13–15, 2019.
Disclosures
Izumi Kawachi reports funding for research, travel/speaker honoraria or serving on scientific advisory boards from Novartis Pharma K.K., Biogen, Bayer, Mitsubishi Tanabe Pharma, Astellas Pharma Inc., Bristol-Myers Squibb, Takeda Pharmaceutical Company, Japan Blood Product Organization, Chugai Pharmaceutical Co., and Alexion Pharmaceuticals, and research support from a JSPS KAKENHI Grant. Hiromichi Otaka and Kengo Ueda are employees of Novartis Pharma K.K. Kosuke Iwasaki and Tomomi Takeshima are employees of Milliman Inc, which has received consultancy fees from Novartis Pharma K.K.
Compliance with Ethics Guidelines
This study was approved by the Clinical Research Promotion Network Japan (CR-IRB-0094). The database includes data collected for secondary use, and was provided after anonymization. Therefore, informed consent was not required according to ethical guidelines in Japan. The data used in this study was provided by Medical Data Vision Co., Ltd through a contract to Novartis Pharma K.K., and Novartis Pharma K.K. had permission to access and use the data based on the contract.
Data Availability
The data that support the findings of this study are available from Medical Data Vision Co., Ltd., but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. However, the data are available from the authors upon reasonable request and with permission of Medical Data Vision Co., Ltd.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kawachi, I., Otaka, H., Iwasaki, K. et al. Treatment Status and Healthcare Cost Trends for Patients with Multiple Sclerosis in Japan: A Claims Database Analysis. Neurol Ther 11, 1253–1268 (2022). https://doi.org/10.1007/s40120-022-00374-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40120-022-00374-4