Abstract
Introduction
Levodopa remains the cornerstone treatment for Parkinson’s disease (PD) but its use is associated with the development of ‘wearing-off’ fluctuations and other motor and non-motor complications over time. Adding a catechol-O-methyltransferase (COMT) inhibitor to levodopa/dopa decarboxylase (DDC) inhibitor therapy reduces fluctuations in the profile of plasma levodopa levels following oral dosing, and can therefore be beneficial for the management of motor complications. The objective of the EPSILON study is to investigate the efficacy of opicapone (OPC; a third-generation, once-daily COMT inhibitor) in enhancing the clinical benefit of levodopa in patients in earlier stages of PD, without end-of-dose motor fluctuations.
Methods
EPSILON is a phase III, double-blind, randomised, placebo-controlled and parallel-group study, designed to evaluate the efficacy and safety of OPC as add-on to levodopa/DDC inhibitor therapy in patients with early PD who do not exhibit signs of motor complications. Eligible patients will be randomised (1:1) to receive OPC 50 mg or placebo, in addition to their existing levodopa/DDC inhibitor therapy, over a 24-week, double-blind treatment period, after which they will have the option of entering an additional 1-year, open-label extension period, during which all patients will receive OPC 50 mg.
Planned Outcomes
The primary efficacy endpoints are change in Movement Disorders Society Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) Part III total score from baseline to the end of the double-blind period (double-blind phase) and change in MDS-UPDRS Part IV total score from open-label baseline to the end of the open-label period (open-label phase). Secondary outcomes during the double-blind phase will include other measures of PD symptoms, including quality of life, non-motor symptoms, and development of motor fluctuations. Safety assessments will include evaluation of treatment-emergent adverse events, laboratory safety parameters, suicidality and impulse control disorders.
Trial Registration
European Union Drug Regulating Authorities Clinical Trials Database (number 2020-005011-52).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Levodopa remains the cornerstone treatment for Parkinson’s disease (PD) but its use is associated with the development of wearing-off fluctuations and other motor and non-motor complications. |
The addition of a catechol-O-methyltransferase (COMT) inhibitor to levodopa therapy increases plasma levodopa levels and reduces fluctuations following oral dosing. |
Opicapone (OPC; a third-generation, once-daily COMT inhibitor) ensures a substantial and prolonged inhibition of COMT over 24 h and increases the overall systemic exposure to levodopa. |
EPSILON is a phase III, randomised, double-blind, placebo-controlled trial and open-label extension study that will evaluate the efficacy of OPC in enhancing the clinical benefit of levodopa in patients in the early stages of PD, without end-of-dose motor fluctuations. |
What will be learned from the study? |
EPSILON will evaluate the impact of adding OPC to levodopa therapy on motor symptoms in patients with early PD who do not exhibit signs of motor complications. |
Introduction
Parkinson’s disease (PD) is a progressive neurodegenerative disorder, presenting with a variety of motor and non-motor symptoms [1]. It is the second most common neurodegenerative disease (after Alzheimer’s disease) [2], affecting an estimated 6 million people globally [3]. PD has a particularly debilitating effect on patients’ health-related quality of life, with a significant impact on areas such as psychosocial functioning and mobility [4]. Thus, identification, diagnosis and effective treatment strategies in the early stages of the disease are essential.
Dopamine substitution is still the primary strategy for symptomatic treatment of PD [5], with levodopa remaining the cornerstone therapeutic agent [6]. While levodopa is well tolerated and efficacious, it is extensively metabolised in the periphery by dopa decarboxylase (DDC) and catechol-O-methyltransferase (COMT), and consequently only 1% of an oral dose of levodopa reaches the brain [7, 8]. In addition, with disease progression the duration of each levodopa dose becomes shorter, with use of levodopa being associated with the development of motor complications (fluctuations of motor function and dyskinesias) and non-motor fluctuations [9]. Evidence suggests that the appearance of motor complications is associated with loss and decreased buffering capacity of striatal dopamine nerve terminals, as well as non-physiological, pulsatile stimulation of dopamine receptors, resulting from intermittent oral dosing with levodopa [10, 11]. A therapy providing a continuous delivery of levodopa (‘continuous dopamine stimulation’) might help restore dopamine at a more physiological level, thereby facilitating the management of motor complications, and this concept has been validated in advanced patients undergoing levodopa jejunal infusions [12]. Within this context, the addition of a COMT inhibitor to levodopa/DDC inhibitor therapy may help to reduce fluctuations in plasma levodopa levels following oral dosing and extend the benefit of each levodopa dose, without the necessity for increasing the dose or frequency of levodopa administration [10, 11, 13]. There has therefore been a long-standing debate regarding the potential role of COMT inhibitors as early adjunctive therapy to prevent or delay the development of wearing-off. Results of a meta-analysis of entacapone studies demonstrated that the use of the triple therapy of levodopa/carbidopa/entacapone resulted in significant improvements in Unified Parkinson’s Disease Rating Scale (UPDRS) Parts II and III scores in patients with early PD (although associated with more adverse events [AEs] than levodopa/carbidopa alone) [14]. However, when levodopa/carbidopa/entacapone was compared with levodopa/carbidopa in non-fluctuating patients initiating levodopa therapy in the prospective STalevo Reduction In Dyskinesia Evaluation in PD (STRIDE-PD) study, it was associated with a shorter time to onset and increased frequency of dyskinesia, compared with levodopa/carbidopa alone [15]. Potential reasons for the failure of this study have been proposed: the dosing schedule used (four daily doses administered every 3.5 h) may not have provided stable and continuous levodopa plasma levels, despite administration with entacapone; compliance may not have been optimal in the early, non-fluctuating patients enrolled in the study; and the daily levodopa load was higher in the levodopa/carbidopa/entacapone group than the levodopa/carbidopa group [16]. Further studies are therefore required in order to validate the use of a COMT inhibitor as an adjunctive therapy to levodopa plus a DDC inhibitor in early PD.
Opicapone (OPC) is a third-generation COMT inhibitor [7, 8, 17] which was developed to improve the toxicity limitations of other COMT inhibitors in a convenient, once-daily dosage regimen [17]. It was evaluated in two pivotal trials in patients with PD and end-of-dose motor fluctuations (BIPARK-I and II), and the results demonstrated an acceptable tolerability profile, combined with efficacy in reducing OFF-time [18, 19]. These studies led to the approval of OPC in the European Union, USA, Japan, Australia and other countries as adjunctive therapy to preparations of levodopa/DDC inhibitor in patients with PD and end-of-dose motor fluctuations[20] or OFF episodes [21]. In the recent guidelines from the Movement Disorders Society (MDS), OPC was deemed efficacious, with no safety concerns and no need for specialised monitoring [22], and it may, therefore, represent a suitable candidate for add-on COMT inhibition with levodopa/DDC inhibitor therapy in patients with early or stable PD. Although the mean disease duration of patients enrolled in the BIPARK studies was approximately 8 years and the mean duration of motor fluctuations was approximately 3 years [23], the studies did include patients with end-of-dose motor fluctuations in early stages of PD. Recently, a post hoc analysis of the BIPARK studies has demonstrated that OPC was efficacious over the entire course of motor fluctuation evolution in patients with PD, with enhanced efficacy in patients who were earlier, in comparison to later, in both their disease course and levodopa treatment pathway, supporting its use as an early adjunct to levodopa in PD [24].
Given the acceptable safety profile and encouraging efficacy observed in studies of OPC in patients with PD and end-of-dose motor fluctuations, including evidence demonstrating its specific efficacy in those who are relatively early in their disease course and levodopa treatment pathway, the EPSILON (Early ParkinSon wIth Levodopa/DDC inhibitor and OpicapoNe) study is a phase III, double-blind, randomised, placebo-controlled, parallel-group trial that has been designed to explore the potential of OPC to enhance the clinical benefit of levodopa in patients in the early stages of PD, without end-of-dose motor fluctuations.
Methods
Study Design
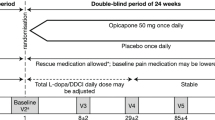
EPSILON is a phase III, double-blind, randomised, placebo-controlled and parallel-group study to evaluate the efficacy and safety of OPC as add-on to levodopa and a DDC inhibitor in patients with early idiopathic PD who do not exhibit signs of any motor complication (consisting of fluctuations in the motor response and/or involuntary movements or dyskinesias). After a screening period of up to 4 weeks, eligible patients will be randomised in a 1:1 ratio to receive treatment with either OPC 50 mg or placebo, in addition to their existing levodopa/DDC inhibitor therapy, and enter a 24-week, double-blind treatment period (Fig. 1). At the end of the double-blind period, and at the discretion of both the investigator and patient, participants may enter an additional 1-year, open-label extension period, during which all patients will receive OPC 50 mg, irrespective of their prior treatment group. A post-study visit (PSV) will be performed approximately 2 weeks after the end-of-study visit (EOS) or early discontinuation visit (EDV). The study is registered on the European Union Drug Regulating Authorities Clinical Trials Database (EudraCT; number 2020-005011-52).
Treatment Allocation
Subjects will be centrally assigned to randomised study treatment using an Interactive Voice Response System/Interactive Web Response System (IVRS/IWRS). Eligible patients will be randomly assigned (1:1) at baseline using a proprietary computer-generated scheme (IQVIA Holdings Inc. and its subsidiaries, USA) to once-daily OPC 50 mg or matching placebo, using a sequential, non-stratified, dummy block approach.
Treatment Groups and Duration
The estimated duration of individual patient participation in the double-blind period is 28 weeks (including a 4-week screening period, and 24-week maintenance treatment period). An additional 2-week follow-up period will be performed if the patient does not enter the open-label period. The estimated duration of individual patient participation in the open-label period is 54 weeks (including a 52-week treatment period, and 2-week follow-up period).
Dose Regimen
Study treatment (OPC or matching placebo) will be taken orally once daily in the evening at least 1 h after the last daily dose of levodopa/DDC inhibitor (considered the bedtime dose). There should be no change to the patient’s levodopa/DDC inhibitor regimen throughout the double-blind period of the study, unless adjustment is necessary for patient safety. In the open-label period, levodopa/DDC inhibitor dose adjustments and new anti-PD drugs will be permitted, if necessary, for patient safety and/or to treat a worsening of the patient’s condition; adjustments for any other reason are discouraged.
Study Population
The study will be conducted in approximately 85 clinical sites in 13 countries (Belgium, Bulgaria, Czech Republic, France, Germany, Italy, Poland, Portugal, Serbia, Spain, Turkey, Ukraine, UK). Other countries and additional sites may be added, if required. Inclusion and exclusion criteria for the study population are outlined in Table 1.
Study Assessments
All endpoint assessments are outlined in Table 2 and the timing of these assessments is outlined in Fig. 2.
Timelines of study assessments. CGI-C Clinicians’ Global Impression of Change, C-SSRS Columbia-Suicide Severity Rating Scale, DDCi dopa decarboxylase inhibitor, EOS end-of-study, L-dopa levodopa, MDS-UPDRS Movement Disorder Society-Unified Parkinson’s Disease Rating Scale, mMIDI modified Minnesota Impulsive Disorders Interview, NMSS Non-Motor Symptoms Scale, PDQ-39 39-item Parkinson’s Disease Questionnaire, PDSS-2 Parkinson’s Disease Sleep Scale 2, PGI-C Patients’ Global Impression of Change, PSV post-study visit, V visit, WOQ-9 9-item Wearing-Off Questionnaire
Efficacy Assessments
The primary efficacy endpoint for the double-blind phase of the study is the change in MDS-UPDRS Part III total score from baseline (visit [V] 2) to the end of the double-blind period (V9). The change in MDS-UPDRS Part IV total score is included as a secondary endpoint to evaluate all patients with PD who develop motor complications during the study. For this reason, for the open-label phase of the study, the primary endpoint is the change in MDS-UPDRS Part IV total score from open-label baseline (V9) to the end of the open-label period (V15). Secondary efficacy assessments, using other measures of PD symptoms, will be evaluated in both phases of the study, as outlined in Table 2.
The MDS-UPDRS is a revised version of the UPDRS, evaluating various aspects of PD in four parts [25]. Parts IA and IB cover the non-motor aspects of experiences of daily living, Part II addresses the motor aspects of experiences of daily living, Part III involves an examination of the motor symptoms, and Part IV covers motor complications. The Hoehn and Yahr scale, which is used to classify symptom progression in PD, was originally described in 1967 to include stages 1–5 [26], but was subsequently modified to include stages 1.5 and 2.5, in order to account for the intermediate course of PD [27]. The Schwab and England Activities of Daily Living (ADL) Scale assesses the difficulties patients experience completing activities of daily living, and rates a patient’s functional ability on a scale from 0 (worst possible function) to 100 (no impairment) [28]. The PD Sleep Scale-2 (PDSS-2) is a visual analogue scale developed to assess nocturnal disturbances and sleep disorders in patients with PD [29, 30]. The scale has a maximum value of 60 points, with a higher score indicating greater sleep disturbance, and a cutoff value of ≥ 18 distinguishing poor sleep quality (≥ 18) from good sleep quality (< 18) [31]. The Non-Motor Symptoms Scale (NMSS) assesses 30 non-motor symptoms of PD across nine dimensions (cardiovascular, sleep/fatigue, mood/cognition, perceptual problems, attention/memory, gastrointestinal, urinary, sexual function, and miscellany [pain, smell, weight change, and hyperhidrosis]) [32]. The total score is quantified by multiplying severity (score 0–3) by frequency (score 1–4) for each question, giving a score range of 0–360. The PD Questionnaire-39 (PDQ-39) is a 39-item patient-reported outcome that assesses aspects of functioning and well-being that are usually adversely affected by PD across eight dimensions (mobility, activities of daily living, emotional well-being, stigma, social support, cognition, communication, and bodily discomfort) [33]. Each dimension score ranges from 0 (‘never have difficulty’) to 100 (‘always have difficulty’) and the overall score is the sum of the dimension scores divided by eight. The nine-item Wearing-Off Questionnaire (WOQ-9) is a screening tool for wearing-off symptoms in PD [34]. The Clinical Global Impression of Improvement (CGI-C) and Patient’s Global Impression of Improvement (PGI-C) are, respectively, physician and patient assessments of how much a patient’s overall status has improved or worsened since the start of the study, comprising a 7-point scale: (1, ‘very much improved’; 2, ‘much improved’; 3, ‘minimally improved’; 4, ‘no change’; 5, ‘minimally worse’; 6, ‘much worse’; 7, ‘very much worse’).
Safety Assessments
The safety and tolerability of OPC 50 mg as add-on therapy to levodopa/DDC inhibitor will be assessed as a secondary objective of the study. Assessments will include the incidence of treatment-emergent AEs (TEAEs), changes from baseline in vital signs, clinical and neurological examinations, 12-lead electrocardiogram readings, routine laboratory parameters, and the evaluation of suicidality (assessed using the Columbia-Suicide Severity Rating Scale [C-SSRS]) and impulse control disorders (assessed using the modified Minnesota Impulse control Disorders Interview [mMIDI]) (Table 2).
The C-SSRS was designed to distinguish domains of suicidal ideation and suicidal behaviour, measured using four constructs (severity of ideation, intensity of ideation, behaviour, and lethality) [35]. The mMIDI is an instrument developed to diagnose impulse control disorders, including compulsive buying, kleptomania, trichotillomania, intermittent explosive disorder, pyromania, pathological gambling, compulsive sexual behaviour, skin-picking, and binge-eating [36].
Sample Size Calculation
A minimum clinically relevant magnitude of effect in change from baseline of MDS-UPDRS Part III (primary endpoint) between treatment arms (OPC versus placebo) is expected to be at least 3 points. For the purpose of this evaluation, previous data were checked to understand the variability of an intended-to-treat population of patients with early PD. Results from the double-blind period of BIPARK-I and II studies [18, 19] showed a standard deviation (SD) for the change from baseline of UPDRS Part III equal to approximately 6.9 points for a group of patients with early fluctuations (< 1 year) and aged 80 years or younger (i.e. a population comparable as much as possible to patients with early PD). Following the conversion formula of Goetz et al. [25] to transform UPDRS Part III score to MDS-UPDRS Part III score, the SD for early PD subjects in change from baseline of MDS-UPDRS Part III is expected to be 8.3 points. Therefore, to determine the sample size, the following specifications and assumptions were applied: a two-sided 5% significance level; a power of 90%; a mean treatment effect (OPC versus placebo) of 3 points; and an SD of 8.3 points. It was also assumed that the primary endpoint would follow normal distribution and equal variance in both treatment groups. With these assumptions, a sample size of 162 patients in each treatment group is required. Approximately 382 patients will be screened to achieve a study population of approximately 324 patients (162 patients per treatment group), assuming a dropout rate of 15%. It was also considered that patients without end-of-dose motor fluctuations might have lower baseline MDS-UPDRS Part III scores; therefore, in order to see a magnitude of effect, only subjects with MDS-UPDRS Part III score of at least 20 will be allowed to enter the study as indicated in Table 1.
Blinding
Patients and study site personnel will remain blinded to individuals’ double-blind treatment until the end of the open-label phase. Masking of randomisation will be maintained by use of identical OPC 50 mg and placebo capsules. Unblinding of the double-blind period will be performed after database lock for the purpose of data analyses. In the case of an emergency, the investigator has the sole responsibility for determining if unblinding of a patient’s treatment assignment is warranted. Patient safety must always be the first consideration in making such a determination.
Statistical Methodology
The primary efficacy analysis will be performed after all patients have completed the double-blind period. Results of the open-label phase will be presented separately once the open-label period is completed. Unblinding of the double-blind period will be performed after database lock for the purpose of data analyses; however, patients and sites will remain blinded to their double-blind treatment until the end of the open-label phase. Efficacy assessments will be analysed for the full analysis set (FAS), defined as all patients who are randomised and who have at least one measurement of the primary efficacy assessment. Safety assessments will be analysed for the safety set, defined as all patients who take at least one dose of investigational product.
Primary Efficacy Analysis
The primary efficacy parameter, change from baseline (V2) in MDS-UPDRS Part III total score at the end of the double-blind period (V9), will be analysed for the double-blind FAS population, using a mixed model repeated measures (MMRM) approach, with fixed effects for baseline, centre, treatment, visit, treatment by visit interaction, and baseline by visit interaction, and patient as a random effect. Between-group differences (OPC versus placebo) will be estimated from the model.
Secondary Efficacy Analysis
An MMRM analysis will be used for relevant secondary efficacy endpoints in the double-blind period. The proportion of patients with an improvement from baseline in CGI-I and PGI-I scores, at 2 weeks after baseline and at the end of the double-blind period (V9), will be analysed using logistic regression, with treatment and baseline total score included in the model.
Sensitivity Analysis
A sensitivity analysis will be performed on the primary endpoint using an analysis of covariance (ANCOVA) approach, with fixed effects for baseline, centre and treatment. Missing data will be imputed using a multiple imputation method for the sensitivity analysis of the primary endpoint only.
Safety Analyses
TEAEs will be summarised with regard to the number and percentages of patients with TEAEs. Vital signs and laboratory parameters will be summarised using summary statistics of absolute values and changes from baseline. Summary statistics and shift tables will be presented for physical and neurological examinations. Demographic and baseline characteristics will be presented using descriptive statistics. C-SSRS and mMIDI results will be presented as incidence rates (overall and by visit) and shift tables.
Strengths and Limitations
In early tolcapone and entacapone studies, adding a COMT inhibitor to the levodopa regimen in subgroups of stable patients with PD improved UPDRS scores. However, these studies have not been viewed as unequivocally showing an effect in stable disease, and, as such, they have failed to make an impact on product labelling and use. The strengths of EPSILON are that it was designed as a pivotal study with a COMT inhibitor, OPC, to formally demonstrate an enhanced clinical benefit of levodopa therapy in patients in the early stages of PD, and that it will include a relatively large population of patients who will have the opportunity to be exposed to OPC 50 mg for an additional 1-year open-label extension.
Ethics and Dissemination
The study will be conducted in accordance with the Declaration of Helsinki on Ethical Principles for Medical Research Involving Human Patients adopted by the General Assembly of the World Medical Association (2013); the applicable regulatory requirements of the participating countries; the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH) Harmonised Guideline—integrated addendum to ICH E6(R1) Guideline for Good Clinical Practice E6(R2); and with the European Commission Directives 2001/20/EC and 2005/28/EC, and EU Regulation No. 536/2014. The protocol has been submitted to relevant institutional review boards (IRBs), namely National Regulatory Agencies and Central Ethics Committee, and when/if applicable to regional/local ethics committees; unconditional approval/favourable opinion must be obtained before the start of the study. All patients must provide written informed consent in order to participate in the study.
Protocol details are available at www.clinicaltrialsregister.eu (EudraCT number 2020-005011-52). In line with European Federation of Pharmaceutical Industries and Associations (EFPIA) and Pharmaceutical Research and Manufacturers of America (PhRMA) guiding principles, the sponsor (BIAL – Portela & Cª S.A.) undertakes to share, upon request, anonymised patient-level, study-level clinical trial data (analysable data sets), and other information (such as protocols) from clinical trials in patients for medicines and indications approved in the USA and the European Union, to qualified researchers as necessary for conducting legitimate research. Results of the study will be published when available.
Current Status
The study has received approval in Belgium, Bulgaria, Czech Republic, France, Germany, Italy, Poland, Portugal, Spain, Turkey, the UK and Ukraine; approval is pending in Serbia. To date, around 280 patients have been screened and over 215 patients randomised.
Discussion
Effective symptomatic treatment of PD is critical in order to offer relief from both motor and non-motor features of the disease and maintain patients’ quality of life. Degeneration of neurons in the nigrostriatal dopaminergic pathway and the resultant loss of dopamine is the primary cause of both the motor and non-motor features of PD; thus, maintenance of dopamine levels remains an important strategy to alleviate symptoms across the disease course [5, 37, 38]. Levodopa is the gold standard treatment for PD, but clinical response to levodopa decreases with time, as the duration of the benefits following a dose of levodopa shortens [39]. Use of adjunctive therapies to maximise levodopa bioavailability is a rational therapeutic approach [22].
Evidence supports the hypothesis that the development of motor complications is linked to the non-physiological, pulsatile stimulation of dopamine receptors [10, 11, 40]. However, studies have thus far failed to establish whether continuous dopamine stimulation in the early stages of PD, using either a controlled-release levodopa/DDI inhibitor or adjunctive therapy with entacapone, can prevent or delay the development of wearing-off motor complications over the longer term [15, 41]. Addition of OPC to levodopa therapy has been shown to be effective in reducing OFF-time in patients with PD and end-of-dose motor fluctuations, both in clinical trials [18, 19] and in the clinical practice setting [42]. Moreover, evidence has shown that OPC has enhanced efficacy in patients with end-of-dose motor fluctuations who are relatively early in their disease course and levodopa treatment pathway [24], and data suggest that the addition of OPC to levodopa in patients with PD without end-of-dose motor fluctuations might also be beneficial [10]. Initiating OPC in early PD might improve current symptoms in these patients and additionally prevent or delay the development of motor fluctuations (although not the primary objective of this study). The NMSS will allow us to gain a better understanding of the evolution of non-motor symptoms in relation to motor fluctuations by assessing which non-motor symptoms develop before the onset of motor fluctuations, which non-motor symptoms fluctuate in those patients who develop motor fluctuations and by evaluating the severity of non-motor fluctuations before and after the onset of motor fluctuations.
Despite having a relatively short plasma half-life, OPC has been shown to inhibit peripheral COMT activity long after its plasma clearance, resulting in sustained COMT inhibition that endures over 24 h, allowing once-daily dosing [7, 43].
Given the lack of unequivocal evidence for the use of COMT inhibitors during the early stages of PD, the EPSILON study will provide valuable information on whether the use of adjunctive OPC 50 mg treatment can improve symptoms in patients with early PD, before end-of-dose motor fluctuations become clinically manifest.
References
Greenland JC, Barker RA. Chapter 6: the differential diagnosis of Parkinson’s Disease. In: Stoker TB, Greenland JC, editors. Parkinson’s disease: pathogenesis and clinical aspects [Internet]. Brisbane: Codon; 2018.
Lebouvier T, Chaumette T, Paillusson S, et al. The second brain and Parkinson's disease. Eur J Neurosci. 2009;30(5):735–41. https://doi.org/10.1111/j.1460-9568.2009.06873.x.
GBD 2016 Parkinson's Disease Collaborators. Global, regional, and national burden of Parkinson's disease, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018;17(11):939–53. https://doi.org/10.1016/S1474-4422(18)30295-3.
van Uem JM, Marinus J, Canning C, et al. Health-related quality of life in patients with Parkinson’s disease—a systematic review based on the ICF model. Neurosci Biobehav Rev. 2016;61:26–34. https://doi.org/10.1016/j.neubiorev.2015.11.014
Müller T. Experimental dopamine reuptake inhibitors in Parkinson’s disease: a review of the evidence. J Exp Pharmacol. 2021;13:397–408. https://doi.org/10.2147/jep.s267032.
Poewe W, Antonini A, Zijlmans JC, Burkhard PR, Vingerhoets F. Levodopa in the treatment of Parkinson’s disease: an old drug still going strong. Clin Interv Aging. 2010;5:229–38. https://doi.org/10.2147/cia.s6456.
Almeida L, Rocha JF, Falcão A, et al. Pharmacokinetics, pharmacodynamics and tolerability of opicapone, a novel catechol-O-methyltransferase inhibitor, in healthy subjects: prediction of slow enzyme-inhibitor complex dissociation of a short-living and very long-acting inhibitor. Clin Pharmacokinet. 2013;52(2):139–51. https://doi.org/10.1007/s40262-012-0024-7.
Kiss LE, Ferreira HS, Torrão L, et al. Discovery of a long-acting, peripherally selective inhibitor of catechol-O-methyltransferase. J Med Chem. 2010;53(8):3396–411.
Antonini A, Martinez-Martin P, Chaudhuri RK, et al. Wearing-off scales in Parkinson’s disease: critique and recommendations. Mov Disord. 2011;26(12):2169–75. https://doi.org/10.1002/mds.23875.
Olanow CWCP, Obeso JA. Continuous dopaminergic stimulation as a treatment for Parkinson’s disease: current status and future opportunities. Mov Disord. 2020;35(10):1731–44.
Olanow CWOJ, Stocchi F. Continuous dopamine-receptor treatment of Parkinson’s disease: scientifi c rationale and clinical implications. Lancet Neurol. 2006;5:677–87.
Antonini A, Odin P, Pahwa R, et al. The long-term impact of levodopa/carbidopa intestinal gel on ’off’-time in patients with advanced parkinson’s disease: a systematic review. Adv Ther. 2021;38(6):2854–90. https://doi.org/10.1007/s12325-021-01747-1.
Stocchi F, Olanow CW. Continuous dopaminergic stimulation in early and advanced Parkinson’s disease. Neurology. 2004;62(1 Suppl 1):S56-63. https://doi.org/10.1212/wnl.62.1_suppl_1.s56.
Liao X, Wu N, Liu D, Shuai B, Li S, Li K. Levodopa/carbidopa/entacapone for the treatment of early Parkinson’s disease: a meta-analysis. Neurol Sci. 2020;41(8):2045–54. https://doi.org/10.1007/s10072-020-04303-x.
Stocchi F, Rascol O, Kieburtz K, et al. Initiating levodopa/carbidopa therapy with and without entacapone in early Parkinson disease: the STRIDE-PD study. Ann Neurol. 2010;68(1):18–27. https://doi.org/10.1002/ana.22060.
Stocchi F, Vacca L, Radicati FG. How to optimize the treatment of early stage Parkinson’s disease. Transl Neurodegener. 2015;4:4. https://doi.org/10.1186/2047-9158-4-4.
Azevedo Kauppila L, Pimenta Silva D, Ferreira JJ. Clinical utility of opicapone in the management of parkinson’s disease: a short review on emerging data and place in therapy. Degener Neurol Neuromuscul Dis. 2021;11:29–40. https://doi.org/10.2147/dnnd.s256722.
Ferreira JJ, Lees A, Rocha JF, Poewe W, Rascol O, Soares-da-Silva P. Opicapone as an adjunct to levodopa in patients with Parkinson’s disease and end-of-dose motor fluctuations: a randomised, double-blind, controlled trial. Lancet Neurol. 2016;15(2):154–65. https://doi.org/10.1016/s1474-4422(15)00336-1.
Lees AJ, Ferreira J, Rascol O, et al. Opicapone as adjunct to levodopa therapy in patients with parkinson disease and motor fluctuations: a randomized clinical trial. JAMA Neurol. 2017;74(2):197–206. https://doi.org/10.1001/jamaneurol.2016.4703.
European Medicines Agency. Ongentys® Summary of Product Characteristics, 2021. https://www.ema.europa.eu/en/documents/product-information/ongentys-epar-product-information_en.pdf. Accessed 20 Jan 2022.
Food and Drug Administration. Ongentys® Highlights of Prescribing Information, 2020. https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/212489s000lbl.pdf. Accessed 20 Jan 2022.
Fox SH, Katzenschlager R, Lim SY, et al. International Parkinson and Movement Disorder Society evidence-based medicine review: update on treatments for the motor symptoms of Parkinson’s disease. Mov Disord. 2018;33(8):1248–66. https://doi.org/10.1002/mds.27372.
Ferreira JJ, Lees A, Rocha JF, Poewe W, Rascol O, Soares-da-Silva P. Long-term efficacy of opicapone in fluctuating Parkinson’s disease patients: a pooled analysis of data from two phase 3 clinical trials and their open-label extensions. Eur J Neurol. 2019;26(7):953–60. https://doi.org/10.1111/ene.13914.
Rocha J-F, Ebersbach G, Lees A, et al. The added benefit of opicapone when used early in Parkinson’s disease patients with levodopa-induced motor fluctuations: a post-hoc analysis of BIPARK-I and -II. Front Neurol. 2021. https://doi.org/10.3389/fneur.2021.754016.
Goetz CG, Stebbins GT, Tilley BC. Calibration of unified Parkinson’s disease rating scale scores to Movement Disorder Society-unified Parkinson’s disease rating scale scores. Mov Disord. 2012;27(10):1239–42. https://doi.org/10.1002/mds.25122.
Hoehn MM, Yahr MD. Parkinsonism: onset, progression and mortality. Neurology. 1967;17(5):427–42. https://doi.org/10.1212/wnl.17.5.427.
Goetz CG, Poewe W, Rascol O, et al. Movement Disorder Society Task Force report on the Hoehn and Yahr staging scale: status and recommendations. Mov Disord. 2004;19(9):1020–8. https://doi.org/10.1002/mds.20213.
Schwab RS, England AC. Projection technique for evaluating surgery in Parkinson’s disease. In: Gilingham FH, Donaldson MC, editors. Edinburgh: Churchill Livingstone; 1969.
Chaudhuri KR, Pal S, DiMarco A, et al. The Parkinson’s disease sleep scale: a new instrument for assessing sleep and nocturnal disability in Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2002;73(6):629–35. https://doi.org/10.1136/jnnp.73.6.629.
Trenkwalder C, Kohnen R, Högl B, et al. Parkinson’s disease sleep scale–validation of the revised version PDSS-2. Mov Disord. 2011;26(4):644–52. https://doi.org/10.1002/mds.23476.
Muntean ML, Benes H, Sixel-Döring F, et al. Clinically relevant cut-off values for the Parkinson’s Disease Sleep Scale-2 (PDSS-2): a validation study. Sleep Med. 2016;24:87–92. https://doi.org/10.1016/j.sleep.2016.06.026.
Chaudhuri KR, Martinez-Martin P, Brown RG, et al. The metric properties of a novel non-motor symptoms scale for Parkinson’s disease: results from an international pilot study. Mov Disord. 2007;22(13):1901–11. https://doi.org/10.1002/mds.21596.
Peto V, Jenkinson C, Fitzpatrick R, Greenhall R. The development and validation of a short measure of functioning and well being for individuals with Parkinson’s disease. Qual Life Res. 1995;4(3):241–8. https://doi.org/10.1007/bf02260863.
Stacy M, Hauser R, Oertel W, et al. End-of-dose wearing off in Parkinson disease: a 9-question survey assessment. Clin Neuropharmacol. 2006;29(6):312–21. https://doi.org/10.1097/01.Wnf.0000232277.68501.08.
Posner K, Brown GK, Stanley B, et al. The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. 2011;168(12):1266–77. https://doi.org/10.1176/appi.ajp.2011.10111704.
Chamberlain SR, Grant JE. Minnesota Impulse Disorders Interview (MIDI): validation of a structured diagnostic clinical interview for impulse control disorders in an enriched community sample. Psychiatry Res. 2018;265:279–83. https://doi.org/10.1016/j.psychres.2018.05.006.
Zafar S, Yaddanapudi SS. Parkinson disease. Treasure Island: StatPearls; 2021.
Hirsch EC, Jenner P, Przedborski S. Pathogenesis of Parkinson’s disease. Mov Disord. 2013;28(1):24–30. https://doi.org/10.1002/mds.25032.
Fabbrini G, Mouradian MM, Juncos JL, Schlegel J, Mohr E, Chase TN. Motor fluctuations in Parkinson’s disease: central pathophysiological mechanisms. Part I. Ann Neurol. 1988;24(3):366–71. https://doi.org/10.1002/ana.410240303.
Chaudhuri KR, Jenner P, Antonini A. Should there be less emphasis on levodopa-induced dyskinesia in Parkinson’s disease? Mov Disord. 2019;34(6):816–9. https://doi.org/10.1002/mds.27691.
Block G, Liss C, Reines S, Irr J, Nibbelink D. Comparison of immediate-release and controlled release carbidopa/levodopa in Parkinson’s disease. A multicenter 5-year study. The CR first study group. Eur Neurol. 1997;37(1):23–7. https://doi.org/10.1159/000117399.
Reichmann H. Effectiveness and safety of opicapone in Parkinson’s disease patients with motor fluctuations: the OPTIPARK open-label study. Transl Neurodegen. 2020. https://doi.org/10.1186/s40035-020-00187-1.
Rocha JF, Falcão A, Santos A, et al. Effect of opicapone and entacapone upon levodopa pharmacokinetics during three daily levodopa administrations. Eur J Clin Pharmacol. 2014;70(9):1059–71. https://doi.org/10.1007/s00228-014-1701-2.
Acknowledgements
Funding
The study, data collection/analysis/interpretation, editorial assistance and the journal’s Rapid Service Fee are funded by Bial – Portela & Cª, S.A., Coronado, Portugal.
Editorial Assistance
Editorial assistance in the preparation of this article was provided by Eliana D’Araio and John Scopes of mXm Medical Communications. Support for this assistance was funded by Bial – Portela & Cª, S.A.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All authors contributed to the study conception and design. The first draft of the manuscript was written by José-Francisco Rocha and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Disclosures
Joaquim J. Ferreira has received grants from GlaxoSmithKline, Grunenthal, Fundação MSD (Portugal), TEVA, MSD, Allergan, Novartis, Medtronic. Received consultancy and speaker fees and participated in advisory boards for GlaxoSmithKline, Novartis, TEVA, Lundbeck, Solvay, BIAL, Merck-Serono, Merz, Ipsen, Biogen, Acadia, Allergan, Abbvie, Sunovion Pharmaceuticals, Zambon, Affiris and Angelini.
Werner Poewe has received lecture fees and honoraria for consultancy in relation to clinical drug development programmes from Alterity, AbbVie, Affiris, AstraZeneca, Axovant, BIAL, Biogen, Britannia, Lilly, Lundbeck, NeuroDerm, Neurocrine, Denali Pharmaceuticals, Orion Pharma, Roche, Stada, Sunovion, Takeda, UCB and Zambon, as well as grant support from the MJFF and the EU FP7 & Horizon 2020 programmes.
Olivier Rascol has participated in advisory boards and/or provided consultancy for AbbVie, Adamas, Acorda, Addex, AlzProtect, ApoPharma, AstraZeneca, Axovant, Bial, Biogen, Britannia, Buckwang, CereSpir, Clevexel, Denali, INC Research, IPMDS, Lundbeck, Lupin, Merck, MundiPharma, NeurATRIS, NeuroDerm, Novartis, ONO Pharma, Osmotica, Parexel, Pfizer, Prexton Therapeutics, Quintiles, Roche, Sanofi, Servier, Sunovion, Theranexus, Takeda, Teva, UCB, Vectura, Watermark Research, XenoPort, XO, Zambon; received grants from Agence Nationale de la Recherche (ANR), CHU de Toulouse, France-Parkinson, INSERM-DHOS Recherche Clinique Translationnelle, MJFox Foundation, Programme Hospitalier de Recherche Clinique, European Commission (FP7, H2020), Cure Parkinson UK; and received a grant to participate in a symposium and contribute to the review of an article by the International Parkinson and Movement Disorder Society.
Fabrizio Stocchi has received compensation for consultancy and speaker-related activities from Lundbeck, UCB, Chiesi, Zambon, Britannia, Cynapsus, Sunovion, Kyowa, Abbvie, Neuroderm, Biogen, Bial.
Angelo Antonini has received compensation for consultancy and speaker-related activities from UCB, Boehringer Ingelheim, Ever Pharma, General Electric, Britannia, AbbVie, Kyowa Kirin, Zambon, Bial, Theravance Biopharma, Jazz Pharmaceuticals, Roche, Medscape; he receives research support from Bial, Lundbeck, Roche, Angelini Pharmaceuticals, Horizon 2020—Grant 825785, Horizon2020 Grant 101016902, Ministry of Education University and Research (MIUR) Grant ARS01_01081, Cariparo Foundation, Movement Disorders Society for NMS Scale validation. He serves as consultant for Boehringer Ingelheim for legal cases on pathological gambling; owns Patent WO2015110261-A1; and owns shares in PD Neurotechnology Limited.
Joana Moreira, Ana Pereira, José-Francisco Rocha and Patrício Soares-da-Silva are current employees of Bial – Portela & Cª, S.A.
Compliance with Ethics Guidelines
The study will be conducted in accordance with the Declaration of Helsinki on Ethical Principles for Medical Research Involving Human Patients adopted by the General Assembly of the World Medical Association (2013); the applicable regulatory requirements of the participating countries; the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH) Harmonised Guideline—integrated addendum to ICH E6(R1) Guideline for Good Clinical Practice E6(R2); and with the European Commission Directives 2001/20/EC and 2005/28/EC, and EU Regulation No. 536/2014. The protocol will be submitted to national independent ethics committee(s) and competent authorities and unconditional approval/favourable opinion must be obtained before the start of the study. All patients must provide written informed consent in order to participate in the study.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ferreira, J.J., Poewe, W., Rascol, O. et al. Opicapone as an Add-on to Levodopa in Patients with Parkinson’s Disease Without Motor Fluctuations: Rationale and Design of the Phase III, Double-Blind, Randomised, Placebo-Controlled EPSILON Trial. Neurol Ther 11, 1409–1425 (2022). https://doi.org/10.1007/s40120-022-00371-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40120-022-00371-7