Abstract
Introduction
Regular physical activity is recommended to patients with chronic coronary syndrome (CCS). However, vigorous physical exercise occurs as a risk factor of sudden cardiac death (SCD). The effect of short-term and irregular exercise is controversial. The aim of this research is to assess the role of regular training in the incidence of SCD and to identify risk factors among patients with CCS participating in a long-term training program.
Methods
Data of risk factors, therapy, and participation were collected retrospectively for a 10-year period, assessing the length and regularity of participation. The incidence of SCD and related mortality was registered. ANOVA, χ2 test, and multinominal logistic regression and stepwise analysis were performed.
Results
The Incidence of chronic kidney disease (CKD) was higher (p < 0.01) and taking beta-blockers (BBs) was lower (p = 0.04) in the SCD group. Irregular training, lack of BBs, smoking, and CKD increased the risk of SCD, while female sex, angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers (ACEI/ARBs), and BBs decreased the risk of SCD.
Conclusions
Taking ACEI/ARBs and BBs proved to be a protective factor, emphasizing the use of optimal medical therapy. Assessment of cardiac risk factors and control of comorbidities also proved to be important. The occurrence of SCD was connected to irregular physical activity, probably relating to the adverse effects of ad hoc exercising.
Similar content being viewed by others
Why carry out this study? |
Proper use of cardiac rehabilitation as secondary prevention can lessen the burden on other parts of healthcare, providing benefits for patients. |
The aim of this study was to assess the role of regular and irregular physical exercise and appropriate management of cardiovascular risk factors in preventing sudden cardiac death in patients with chronic coronary syndrome. |
What was learned from the study? |
Beta-blocker medication should be used according to the guidelines, since it can decrease the mortality of post-infarct patients, including mortality caused by sudden cardiac death. |
Chronic kidney disease can increase the occurrence of sudden cardiac death when combined with chronic coronary syndrome, therefore adequate management of chronic kidney disease is required. |
Physical activity is a crucial component of cardiovascular prevention and all patients with chronic coronary syndrome meeting the requirements should be taking part of a physical training program, in a regular and controlled manner. |
Introduction
At the close of the last century, global cardiovascular mortality surged to over 17 million deaths per year. According to the latest OECD data, there was a slight decrease in cardiovascular mortality in Hungary between 2000 and 2017, showing a 16% reduction. However, the figures remain more than twice the average of the EU-28 countries, with 286 deaths in Hungary per 100,000 compared to 115 in the EU-28. Additionally, the 30-day mortality following an acute coronary event is significantly higher in Hungary compared to other EU member states and the 32 OECD countries, standing at 15.2 in Hungary per 100 admissions, in contrast to 9.5 in the EU [1]. Although the primary care of acute myocardial infarction (AMI) (i.e., catheter labs, professionals) improved in the last 20 years, only 10–15% of eligible patients were referred to cardiac rehabilitation programs, which according to the National Myocardial Infarction Registry of Hungary could be among others a reason of the above-mentioned unchanged 30-day mortality in Hungary [2, 3].
AMI is associated with acute myocardial injury with clinical evidence of acute myocardial ischemia. The term AMI should be used when a rise and/or fall of cardiac troponin is detected accompanying with at least of the following: symptoms of myocardial ischemia, new ischemic electrocardiographic (ECG) changes, development of pathological Q waves, imaging evidence, and identification of a coronary thrombus [4].
Cardiac rehabilitation programs are professional and complex tools for effective secondary prevention, and have I/A recommendations by the European Society of Cardiology (ESC) and American Heart Association/American College of Cardiology (AHA/ACC) guidelines. The objective of these programs is to reduce cardiovascular mortality by lifestyle modification (i.e., dietary changes, smoking cessation, psychological intervention techniques, and optimization of medical therapy) [5,6,7,8]. Most guidelines recommend exercise-based cardiac rehabilitation, since medically supervised physical activity is an effective prevention action for all-cause and cardiovascular mortality, especially in patients with chronic coronary syndrome (CCS) [9, 10]. Several studies have described and verified the importance of this type of long-lasting, out-patient or home-based physiotherapy after a coronary event [11,12,13].
Sudden cardiac death (SCD) is an unexpected and nontraumatic form of death, which occurs within 1 h after the onset or the worsening of the symptoms [14,15,16]. Sudden cardiac arrest (SCA) shares similar underlying causes with sudden cardiac death (SCD). However, in contrast, SCA is a non-fatal event, as the patient does not progress to clinical death [15, 16]. SCD is one of the leading causes of cardiovascular death and has a significant contribution to high lost life-years statistical data among young people [16]. The occurrence clearly increases after the age of 35 but slightly decreases after 75 [17]. Below the age of 65, the incidence in men is four–sevenfold higher than in women [16,17,18,19]. Although physical inactivity is a risk factor for cardiovascular events, vigorous training could increase temporarily the risk for SCD [20] and AMI [21]. Approximately 6–17% of SCD cases occur during high-intensity physical exercise [22, 23] both in non-regularly and regularly exercising groups, but less frequently in the latter [23]. During vigorous exercise, the more rapidly elevating heart-rate could be associated with higher incidence of SCD, which, together with the recovery heart-rate profile could be also a predictor of SCD [24]. However, the overall risk in a habitually exercising population is not elevated; furthermore, the incidence of cardiovascular events is lower [20]. Generally, the benefits of performing regular physical exercise are beyond the SCD/SCA risk both in healthy and CCS populations; however, only few data are available regarding the incidence of SCD in verified CCS populations performing regular physical activity.
Our working group aimed to assess retrospectively the 11-year incidence of SCD/SCA in a cohort of long-standing patients with CCS attending a physical training program as part of their outpatient cardiac rehabilitation. The investigation intended to validate the hypothesis, whether irregular physical training sessions, even as part of a long-term physical training program could increase the occurrence of SCD/SCA. Our research intended to reveal eventual interventional options considering traditional cardiovascular risk factors, comorbidities, and medication as well.
Methods
Patients and the Compounds of the Physical Training
A group of 135 patients with CCS were involved in this retrospective cohort study. Inclusion criteria were prior ACS treated by percutaneous coronary intervention (PCI) and/or acute coronary artery bypass graft surgery (CABG) or having a primary CABG surgery on the basis of CCS. All the patients have been treated immediately after the indexed cardiovascular event in an inpatient cardiac rehabilitation unit at the University of Pecs, Medical Centre, 1st Department of Medicine, Division of Preventive Cardiology and Rehabilitation. According to the guidelines [25], 3 months after the index event every patient has an extensive physical examination, echocardiography, and treadmill stress test performed by Bruce protocol. After checking the test results by a cardiologist, patients with no residual symptoms, normal clinical chemistry (normal potassium level, liver function, blood count, inflammation parameters, troponin), EF > 50%, MET > 5, no significant arrhythmia or ischemic sign on baseline ECG or during the treadmill test and in the recovery could enter the outpatient training program. Patients with an indication for implantable cardioverter defibrillator (ICD) implantation are excluded from the program; therefore, no patients with ICD were included and no ICD discharge occurred during the study. These inclusion criteria are responsible for the relatively good health of the patient group involved in the study. Subsequently, our recruited subjects participated in an outpatient cardiac rehabilitation program for a minimum of 1 month. This program involved 1-h sessions of physical training, held three times a week, and was designed and conducted by a physiotherapist under the supervision of a cardiologist. Patients were not obligatory to attend all training sessions through the entire observational period. Due to personal or working issues, other than health problems (i.e., new-onset of arrhythmia, heart failure, acute coronary event, etc.), our patients may left transitionally or permanently the training program.
The present aerobic exercise training program used in our cohort study was preceded and ended with blood pressure and pulse measurements. The patients began with warm-up exercises (breathing exercises, and stretching of the large joints) for 5–10 min. In the second phase, they participated in a moderate-intensity training. Intensity was defined as 50–70% of peak VO2 (starting at 50% and gradually increasing to 70% of VO2max). The intensity was assessed by the Borg scale (13–15/20) [26] and pulse measurements. The training involved static (exercises with medicine ball, half-squats, toe raises, body flexions) and dynamic (walking, jogging, ball games e.g., basketball, football) exercise elements. The aerobic phase lasted for 35–40 min. Finally, relaxation exercises were performed (stretching and breathing exercises) for 10 min.
Data Collection
Our cohort was created retrospectively by 135 patients on March 1, 2010, and was followed up until March 1, 2021. The morbidity and mortality data of the participants were collected with retrospective data mining using the e-MedSolution program, an integrated information system of the patient care at the University of Pecs.
We obtained the following demographical and morbidity data from our patients: age, sex, length of attending training and/or being absent from training, cardiovascular risk factors as smoking habits, baseline and output (at the time patients left the training program) body mass index (BMI), left ventricular ejection fraction (LVEF) and metabolic equivalent (MET). The ∆ values of BMI, LVEF and MET were calculated from baseline and output data (when patient left program permanently) [baseline-output/baseline] and used for further analyses. Based on the total number of training sessions within the observational period, patients with higher than 90% attendance at training sessions were considered as regular participants. In case of more than 10% absence, the participation was considered irregular. From a cardiovascular aspect, important comorbidities, i.e., hypertension, diabetes, chronic kidney disease (CKD), peripheral arterial disease (PAD), and the currently used CCS guideline recommended medications, meaning angiotensin-converting-enzyme inhibitors (ACEI) and angiotensin II receptor blockers (ARB), beta-blockers (BBs), statins, platelet aggregation inhibitors (PAI) were also obtained.
The endpoint of the study was specified as SCD or SCA, where SCD was defined as mentioned above as a clinical death and SCA as an aborted case of SCD. The group that did not experience any SCD or SCA events was defined as the control group. The control study's endpoint was either the end of the observational period or death from a cause other than SCD/SCA. Patients in the SCA group received appropriate treatment and ICD implantation after the event. However, since these patients were unable to continue attending the program, the SCA event marked the endpoint of the study for them, and we did not collect further data for these patients.
The study was approved by the Regional Ethics Committee of the University of Pecs (9274 – PTE 2022.). The study was conducted according to the guidelines of the Declaration of Helsinki. Informed consent was obtained from all subjects involved in the study. We would like to thank the participants of the study.
Statistical Analysis
Differences were evaluated by IBM SPSS Statistics® 20.0. Significance level was defined as p < 0.05.
In case of continuous variables (age, training length of participation and absence, BMI, LVEF, MET) differences between SCD and SCA group and between SCD/SCA and control group were evaluated by a one-way repeated ANOVA statistical test after using the Kolmogorov–Smirnov test to check on the normality of the data distribution. Data are shown as mean ± SEM.
In case of categorical variables (sex, smoking, comorbidities, medication), associations between SCD and SCA group and between SCD/SCA and control group were determined by using chi-square test analyses. Data are shown as percentage and incidence (absolute number compared to total number).
Multinominal logistic regression and stepwise analysis of the data were performed considering the principle of multicollinearity (all independent variables have a variance inflation factor under 1,2) [27] to reveal occurrence of SCD/SCA using age, absent training months, ΔBMI, ΔLVEF, ΔMET, diabetes, CKD, smoking, taking ACEIs, ARBs, BBs, and statins as independent variables.
Cox regression models were created as time-to-event analyses regarding SCD/SCA event as dichotomous categorical outcome to compare independent variables age, sex, irregular training participation, CKD, BB, ΔLVEF, and smoking. Estimated hazard ratios and related 95% confidence intervals (CI) are shown.
Multinominal logistic regression and stepwise analysis of the data were performed considering the principle of multicollinearity (all independent variables have a variance inflation factor under 1,35) [27] to reveal occurrence of death between SCD and SCA subgroups using sex, attending and absent training months, taking ACEIs, ARBs, PAIs and statins as independent variables.
Cox regression models were created as time-to-event analyses regarding SCD and SCA uncensored event among SCD and SCA subgroups as dichotomous categorical outcome to compare independent variables sex, number of training months, and irregular training participation, taking BBs. Estimated hazard ratios and related 95% confidence intervals (CI) are shown.
Results
Population Characteristics
The mean age in our sample (n = 135) was 74 ± 0.58 years, 37.8% of the participants were female, 62.2% male. The mean observational period was 104 ± 24 months. We registered 17 (12.59%) deaths during the observational period: five patients died because of oncological reasons, three of infection, one of hemorrhagic stroke, one of gastrointestinal bleeding, one of postoperative bleeding, two of heart failure, and four SCD.
SCD/SCA was observed in eight patients (5.93%) during the 11-year observational period; these patients formed the SCD/SCA group. This group included two female (25%) and six male (75%) patients with a mean age of 75.25 ± 2.55 years. Patients with SCD/SCA spent 70.1 ± 15.7 months in the training program on average and 4.9 ± 3.9 months in absence. SCD could be reported in four cases (2.96%), likewise SCA in four cases (2.96%).
The patients did not suffer SCD/SCA formed the control group, which involved 127 cases (94.07%). In the group we found 78 (61.42%) male and 49 (38.58%) female patients with an average age of 73.93 ± 3.65 years. These patients have 70.61 ± 3.65 attending training months, and 3.54 ± 0.71 absent months (Table 1).
One-way ANOVA of the continuous variables revealed no significant differences between SCD/SCA and the control group regarding age (p = 0.81), attending (p = 0.975), and absent (p = 0.654) training months or in the baseline BMI (29 ± 0.35 vs. 29.5 ± 0.53; p = 684), MET (8.14 ± 0.92 vs. 8.6 ± 0.21; p = 0.632) and LVEF (55.4 ± 1.9 vs. 56.1 ± 0.72; p = 0.874) parameters.
Likewise, one-way ANOVA analysis was performed to describe differences between SCD and SCA subgroups, and it showed no significant differences in any of the variables: age (p = 0.756), months attending (p = 0.601) and absent (p = 0.361), baseline BMI (29.5 ± 8.5 vs. 28 ± 8.01; p = 0.578), MET (7.25 ± 1.03 vs. 9.33 ± 1.9; p = 0.34), and LVEF (56 ± 2.8 vs. 54.75 ± 3.1; p = 0.812).
Comparison of the Categorical Variables
Results of the chi-square test showed no significant differences between the SCD/SCA and the control group concerning sex, smoking, PAD, diabetes, hypertension, taking ACEI/ARB, statin, PAI. In contrast, data indicated a significantly higher number of patients with CKD and being an irregular trainer and significantly lower number of patients taking BBs in the SCD/SCA group compared to the controls (Table 2).
Regression
Multinominal logistic regression and stepwise analyses of the data were performed to predict SCD/SCA occurrence concerning age, absent training months, ΔBMI, ΔLVEF, ΔMET, diabetes, CKD, smoking, taking ACEIs, ARBs, BBs, statins, and PAIs as independent variables. The full model statistically significantly predicts the dependent variable better than the intercept-only model alone (Pearson χ2 = 0.011, p = 1.000; df = 13, p = 0.001). Each of these variables added statistically significantly (p < 0.001) to the prediction, df = 13, p = 0.001.
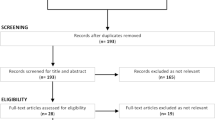
The variance analyses and regression test findings were further verified with Cox regression proportional hazards model time-to-event analyses with the uncensored event SCD or SCA. Based on the findings of the statistical analyses and the principle of multicollinearity age, sex, irregular training participation, CKD, BB, ΔLVEF, and smoking were included in a multivariable prediction model. CKD, irregular training, and BB were the strongest predictors, but only CKD and BB reached a level of significance. The presence of CKD increases the risk for SCD/SCA; however, taking BBs is protective against it. Irregular training (p = 0.093) could be considered a risk factor for SCD or SCA. On the basis of the results, CKD and BB are true predictors for SCD or SCA, and irregular training participation could presumably mean higher risk (more, than four times higher, than among not irregular trainers) (Fig. 1). Data are shown as HR, 95% CI, and significance in Table 3.
Multinominal logistic regression and stepwise analyses of the data were performed to predict death in front of aborted SCD (i.e., SCA) concerning sex, attending and absent training months, taking ACEI/ARB, PAI, and statin as independent variables. The full model statistically significantly predicts the dependent variable better than the intercept-only model alone (Pearson χ2 < 0.001, p = 1.000; df = 5, p = 0.05). Sex (p = 0.02), attending (p = 0.05) and absent training months (p = 0.02), taking ACEI/ARB (p = 0.01) added statistically significantly (p < 0.001) to the prediction, df = 2, p = 0.05. The Cox regression showed no further significance: female sex (p = 0.903; HR < 0.001; CI 0.000–1.38E + 48), higher number of training months (p = 0.965; HR = 0.957; CI 0.134–6.85), taking BBs (p = 0.932; HR = 0.001; CI 0.000–3.95E + 62), irregular training participation (p = 0.986; HR 5.069; CI 0.000–1.4E + 80).
Discussion
SCD is not just a medical condition but a very important economic parameter, as even in the industrialized countries only 50% of SCD victims survive. In recent decades, sudden cardiac death (SCD) has garnered significant attention, particularly because young athletes unexpectedly died from cardiac causes during physical activities. While physical training becomes an important part of everyday life, its safety should be considered as crucial. The currently published ESC guidelines recommend moderate physical activity for apparently healthy people even above the age of 65 [28]. By prescribing physical exercise, the guideline defines the FITT discipline, which describes the frequency, intensity, time, and type of physical activity. In elderly people who are fit and have no health conditions that limit their mobility, the guidelines recommend moderate training 150 min weekly [28].
In case of patients with long-standing CCS, cardiac rehabilitation programs could offer safe and very effective physical training possibilities. This form of activity has a significantly positive effect on the cardiovascular outcomes (reduced rehospitalization and cardiovascular mortality) (IA recommendations) [25, 29]. Although these patients should also be encouraged to perform physical activity, there are several factors such as critical coronary stenosis, LVEF < 50% with wall motion abnormalities, inducible myocardial ischemia on exercise testing, non-sustained ventricular tachycardia, or ACS with PCI within 12 months, which could contribute to an exercise-induced adverse cardiac event (e.g., SCD or SCA) [28]. Therefore, patients with long-standing CCS should always undergo risk stratification before starting an exercise program [28]. Thereafter, physical training is recommended for all patients with long-standing CCS at low risk for exercise-induced adverse event (IIaC recommendation) [28]. Patients at high cardiovascular and/or exercise-induced adverse event risk or with residual ischemia should not perform any kind of competitive sports (IIIC recommendation) [28].
The present investigation was based on an 11-year follow-up, observational cohort with 135 patients with long-standing CCS. Our study aimed to evaluate the role of irregular participation as a risk factor for SCD/SCA in an outpatient training program for patients with long-standing CCS.
Significance of Effective Treatment of Comorbidities and Medication
Findings of the population characteristics determined a homogenous group of patients regarding age, left ventricular ejection fraction, BMI, and MET. The analyses of the nominal variables comparing control and patients with SCD/SCA revealed higher incidence of CKD and lower number of patients on BBs in the SCD/SCA group. However, BBs are one of the four recommended medications in case of post-myocardial infarction patients with IA level of evidence; only 50% of the patients in the SCD/SCA group regularly take BBs, while the amount was 80.6% in the control group [29]. However, during the examined period, there were significant changes in the related guidelines affecting medical therapies (i.e., recommendations about the length of dual antiplatelet therapy), the importance and positive effect of BBs on mortality and recurrent cardiovascular events are widely described and proven by several randomized, multicenter clinical trials in the last 20 years [30,31,32,33,34]. BBs have even more significant mortality-reducing effect in patients after CABG surgery [29]. Recent studies addressing the uncertainty regarding the ideal length of BB therapy after MI may suggest that beyond the first year, the BB therapy is not associated with improved cardiovascular outcomes in case of patients without heart failure or LVSD [35]. All of our patients were treated in accordance with the current long-standing-CCS guideline recommendations, including the BB therapy [29]. The main effect is the oxygen demand decreasing (therefore antianginal) effect and vasodilatation in case of carvedilol and nebivolol. The connections between BBs and reduced risk of SCD/SCA are also well described in previous clinical trials [36], although differences were observed between the lyophilic and hydrophilic types [37]. In concordance with the mentioned studies, our multinominal logistic regression analyses and Cox regression have proved that the underuse of BBs significantly added to the prediction of SCD/SCA. According to the latest ESC guidelines on cardiovascular disease prevention published in 2021, BBs are effective in the secondary prevention of STEMI. They are underused by clinicians because of their potential side effects (e.g., fatigue, depression, bradycardia, heart block, bronchospasm, peripheral vasoconstriction, postural hypotension and impotence), especially in the case of elderly patients [38, 39]. The underuse of BBs in our patients underlines the importance of regular recheck of the optimal medical treatment. The slow doses up-titration of BBs or even ACEIs/ARBs or statins is the key element in avoiding side effects (e.g., hypotension, fatigue, dizziness, muscle weakness) and in securing better medication adherence.
Patients suffering from CKD were more presented in the SCD/SCA group. CKD was defined as a glomerular filtration rate of 60 ml/min or less for at least 3 months. Since dialysis patients were excluded from the training program, such patients did not participate in the study. CKD is a major cardiovascular risk factor for CCS, but cardiovascular complications also frequently occur as major fatal events in patients with CKD [40, 41]. There is a linear connection between increasing cardiovascular risk and decreasing glomerular filtration rate (GFR). According to our results of the multinominal logistic regression and Cox regression analyses, CKD is a very important risk factor of SCD/SCA. The proportional hazards model was used to validate these findings, and the results suggest that the presence of CKD increases the incidence of SCD/SCA by nearly 14 times. Taking BBs is also a significant predictor, and decreases the occurrence of SCD/SCA. Previous studies have also observed a lower occurrence of SCD and lower overall mortality in patients with CKD who were treated by regular hemodialysis and were on BBs, compared to similar group of patients but without BB treatment [42].
The other investigated traditional comorbidities, risk factors, and medication of our CCS population as hypertension, diabetes, smoking, PAD, ACEI/ARBs or statins, were not statistically significantly different in the control and SCD/SCA group. Still in our multinominal logistic regression analysis model we have verified that proper medication (RAAS inhibitor, BBs, statins), smoking, and diabetes have all together a significant role in the prediction of SCD/SCA. As atherosclerosis is the most important risk factor for SCD/SCA, the lipid target levels are very important [43]. Taking ACEI/ARBs and reduced risk for SCD/SCA could play an important role, since every patient in the SCD/SCA group had hypertension, which itself increases the risk for SCD/SCA. Based on the 2020 ESC guideline, ACEI/ARB treatment is a I/A recommendation in patients with previous myocardial infarction and/or revascularization [29], since RAAS inhibitors have a proven, reducing effect on cardiovascular mortality in this group. This may underline that well-treated hypertension has a positive effect on survival, presumably via the known anti-remodeling effect of RAAS inhibitors. Even the calculated ∆BMI, ∆MET, and ∆LVEF parameters were significant in our regression model. As already discussed, reduced LVEF is the most important predictive factor of SCD [18, 44, 45]. Therefore, the detection of impaired LVEF and presumably MET (by regular exercise testing and echocardiographic controls) can help to identify high-risk patients by whom regular physical activity has to be stopped (at least until the required therapies/solutions for the underlying causes are settled) and/or even prophylactic ICD implantation is needed [46].
Significance of Irregular Training
Our study showed no differences in training and absent training months between control and SCD/SCA group. However, the absolute numbers of training months could be confusing because the participants perform training not with the same length. Therefore, we considered patients with more than 10% absent training months (calculated: total training months/absent training months) irregular trainers. If we analyzed irregularity, our results revealed a higher number of irregular trainees among the SCD/SCA group compared to the control. According to other studies assessing habitual physical activities among patients with CCS, we can declare that any kind of regular habitual exercising is associated with lower all-cause and cardiovascular mortality compared to sedentary patients [47]. Habitual exercise caused even greater risk reduction in high-risk CCS patients. Furthermore, among physically active patients, exercising more was associated with lower cardiovascular mortality [47]. Our results are in concordance with those previous findings verifying the cardioprotective effect of regular physical activity [9, 10]. On the other hand, they raise a question about the role of irregular physical activity. Based on our Cox regression results, irregular training could be associated with higher risk for overall occurrence of SCD/SCA. This result may suggest that the frequency of physical exercise affects not just the incidence but even the survival of a SCD/SCA event in patients with CCS, which makes the adherence to the life-style changes as important as the adherence to OMT is. Further multicenter research is certainly needed to univocally prove this assumption.
Strength and Limitations
The strength of our study lies in the homogeneity of the enrolled patient group and the high-quality, reliable data stored in our medical information system. This is further enhanced by the close contact with patients during their participation in the training program.
The number of patients who could have been involved is limited by the generally low participation in cardiac rehabilitation [2] and the specific requirements of the training program (e.g., regular availability during working hours). In spite of the number of patients with CCS participating in our study, the quality of our results is limited by the low incidence of SCD/SCA events during the 11-year observational period, although the low occurrence validates the safety of our training program. In the study, we only included patients with previous coronary revascularization.
Some of our variables show only a weak connection to the investigated SCD and SCA. However, they should still be considered noteworthy and warrant confirmation through further randomized, multicenter clinical trials.
Conclusions
All of the above discussed findings of our study highlight the strong connection between complex but adequate treatment of CCS risk factors and comorbidities (especially CKD) as well as the guidelines recommended optimal medical treatment (especially BBs). Our results demonstrate that physical activity is a crucial component of cardiovascular prevention. Therefore, all patients with CCS who meet the requirements should participate in a physical training program, preferably in an organized, regular, and controlled manner. Properly secured and professionally supervised programs should be available within the framework of cardiac rehabilitation departments. Physical activity programs should run in conjunction with patient education, which has a particularly important role regarding better compliance, medication adherence and lifestyle management, and should cover the management of symptoms and acute events possibly occurring during exercising. Before participation in exercise-based cardiac rehabilitation programs, a proper risk stratification should be assessed regarding exercise-induced adverse cardiac events, and after starting physical activity an irregular and short-term attendance should be avoided. Both healthcare facilities and patients should strive to form and maintain good quality and regular frequency of the training programs as a complex system of safe cardiac prevention and rehabilitation.
Data Availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
OECD. Health at a Glance 2019: OECD Indicators. Paris: OECD Publishing; 2019. https://doi.org/10.1787/4dd50c09-en.
Jánosi A. A szívinfarktus miatt kezelt betegek ellátásának és prognózisának fontosabb adatai. Nemzeti Szívinfarktus Regiszter 2018. Card. Hung. 49, 2019; 119–123 https://doi.org/10.26430/CHUNGARICA.2021.51.4.254
Állami Egészségügyi Ellátó Központ, Egészségügyi Rendszer Teljesítményértékelési Munkacsoportja. Fókuszterület: Szívinfarktus-ellátás. Magyar Egészségügyi Rendszer Teljesítményértékelési Jelentése 2013–15. (mérték). 2016; 1011–1060.
Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction. Circulation. 2018;138(20): e652. https://doi.org/10.1161/CIR.0000000000000617. (13; 10.1016/j.jacc.2018.08.1038).
Lindsey Anderson L, Thompson DR, Oldridge N, et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2016. https://doi.org/10.1002/14651858.CD001800.pub3.
Salzwedel A, Jensen K, Rauch B, et al. Effectiveness of comprehensive cardiac rehabilitation in coronary artery disease patients treated according to contemporary evidence based medicine: update of the Cardiac Rehabilitation Outcome Study (CROS-II). Eur J Prev Cardiol. 2020;27:17561774. https://doi.org/10.1177/2047487320905719.
Santiago CAP, Marzolini S, Pakosh M, Grace SL. Effect of cardiac rehabilitation dose on mortality and morbidity: a systematic review and meta-regression analysis. Mayo Clin Proc. 2017;92:16441659. https://doi.org/10.1016/j.mayocp.2017.07.019.
van Halewijn G, Deckers J, Tay HY, van Domburg R, Kotseva K, Wood D. Lessons from contemporary trials of cardiovascular prevention and rehabilitation: a systematic review and meta-analysis. Int J Cardiol. 2017;232: 294303. https://doi.org/10.1016/j.ijcard.2016.12.125.
Paffenbarger RS Jr, Hyde RT, Wing AL, Lee IM, Jung DL, Kampert JB. The association of changes in physical-activity level and other lifestyle characteristics with mortality among men. N Engl J Med. 1993;328(8):538–45. https://doi.org/10.1056/nejm199302253280804.
Kushi LH, Fee RM, Folsom AR, Mink PJ, Anderson KE, Sellers TA. Physical activity and mortality in postmenopausal women. JAMA. 1997;277(16):1287–92.
Benzer W, Rauch B, Schmid JP, et al. Exercise-based cardiac rehabilitation in twelve European countries results of the European cardiac rehabilitation registry. Int J Cardiol. 2017;228:5867. https://doi.org/10.1016/j.ijcard.2016.11.059.
Abell B, Glasziou P, Hoffmann T. The contribution of individual exercise training components to clinical outcomes in randomised controlled trials of cardiac rehabilitation: a systematic review and meta-regression. Sports Med Open. 2017;3:19. https://doi.org/10.1186/s40798-017-0086-z.
Kotseva K, De Backer G, De Bacquer D, et al. Lifestyle and impact on cardiovascular risk factor control in coronary patients across 27 countries: results from the European Society of Cardiology ESC-EORP EUROASPIRE V registry. Eur J Prev Cardiol. 2019;26: 824835. https://doi.org/10.1177/2047487318825350.
Al-Khatib SM, Stevenson WG, Ackerman MJ, et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Circulation. 2018;138:272–391. https://doi.org/10.1016/j.jacc.2017.10.054.
Buxton AE, Calkins H, Callans DJ, et al. ACC/AHA/HRS 2006 key data elements and definitions for electrophysiological studies and procedures: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Data Standards (ACC/AHA/HRS Writing Committee to Develop Data Standards on Electrophysiology). J Am Coll Cardiol. 2006;48(11):2360–96. https://doi.org/10.1016/j.jacc.2006.09.020.
Kuriachan VP, Sumner GL, Mitchell LB. Sudden cardiac death. Curr Probl Cardiol. 2015;40(4):133–200. https://doi.org/10.1016/j.cpcardiol.2015.01.002.
Bogle BM, Ning H, Mehrotra S, Goldberger JJ, Lloyd-Jones DM. Lifetime risk for sudden cardiac death in the community. J Am Heart Assoc. 2016;5(7): e002398. https://doi.org/10.1161/jaha.115.002398.
Myerburg RJ, Goldberger JJ. Cardiac Arrest and Sudden Cardiac Death. In: Mann DL, Zipes DP, Libby P, editors. Braunwald’s Heart disease: a textbook of cardiovascular medicine. 11th ed. Philadelphia: Elsevier; 2019. p. 807–47.
Koch CG. Statin therapy. Curr Pharm Des. 2012;18(38):6284–90. https://doi.org/10.2174/138161212803832335.
Albert CM, Mittleman MA, Chae CU, Lee M, Hennekens CH, Manson JE. Triggering of sudden death from cardiac causes by vigorous exertion. N Engl J Med. 2000;343(19):1355–61.
Mittleman MA, Maclure M, Tofler GH, Sherwood JB, Goldberg RJ, Muller JE. Triggering of acute myocardial infarction by heavy physical exertion. Protection against triggering by regular exertion. Determinants of Myocardial Infarction Onset Study Investigators. N Engl J Med. 1993;329(23):1677–83. https://doi.org/10.1056/nejm200011093431902.
Cobb LA, Weaver WD. Exercise: a risk for sudden death in patients with coronary heart disease. J Am Coll Cardiol. 1986;7(1):215–9. https://doi.org/10.1016/s0735-1097(86)80284-4.
Siscovick DS, Weiss NS, Fletcher RH, Lasky T. The incidence of primary cardiac arrest during vigorous exercise. N Engl J Med. 1984;311(14):874–7. https://doi.org/10.1056/nejm198410043111402.
Jouven X, Empana JP, Schwartz PJ, Desnos M, Courbon D, Ducimetière P. Heart-rate profile during exercise as a predictor of sudden death. N Engl J Med. 2005;352(19):1951–8. https://doi.org/10.1056/nejmoa043012.
Visseren FLJ, Mach F, Smulders YM, et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2021;42(34):3227–337. https://doi.org/10.1093/eurheartj/ehab484.
Brun JF, Khaled S, Raynaud E, Bouix D, Micallef JP, Orsetti A. The triphasic effects of exercise on blood rheology: which relevance to physiology and pathophysiology? Clin Hemorheol Microcirc. 1998;19(2):89–104.
Everitt BS, Skrondal A. The Cambridge dictionary of statistics. 4th ed. Cambridge: Cambridge University Press; 2010. (ISBN 978-0-521-76699-9).
Pelliccia A, Sharma S, Gati S, et al. 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur Heart J. 2021;42(1):17–96. https://doi.org/10.1093/eurheartj/ehaa605.
Knuuti J, Wijns W, Saraste A, et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41(3):407–77. https://doi.org/10.1093/eurheartj/ehz425.
Bangalore S, Bhatt DL, Steg PG, et al. β-blockers and cardiovascular events in patients with and without myocardial infarction: post hoc analysis from the CHARISMA trial. Circ Cardiovasc Qual Outcomes. 2014;7(6):872–81. https://doi.org/10.1161/circoutcomes.114.001073.
Freemantle N, Cleland J, Young P, Mason J, Harrison J. Beta blockade after myocardial infarction: systematic review and meta regression analysis. BMJ. 1999;318(7200):1730–7. https://doi.org/10.1136/bmj.318.7200.1730.
Andersson C, Shilane D, Go AS, et al. β-blocker therapy and cardiac events among patients with newly diagnosed coronary heart disease. J Am Coll Cardiol. 2014;64(3):247–52. https://doi.org/10.1016/j.jacc.2014.04.042.
Leizorovicz A, Lechat P, Cucherat M, Bugnard F. Bisoprolol for the treatment of chronic heart failure: a meta-analysis on individual data of two placebo-controlled studies-CIBIS and CIBIS II. Cardiac Insufficiency Bisoprolol Study. Am Heart J. 2002;143(2):301–7. https://doi.org/10.1067/mhj.2002.120768.
Hwang D, Lee JM, Kim HK, et al. KAMIR Investigators. Prognostic impact of betablocker dose after acute myocardial infarction. Circ J. 2019;83: 410417. https://doi.org/10.1253/circj.CJ-18-0662.
Ishak D, Suleman Aktaa S, Lindhagen L. Association of beta-blockers beyond 1 year after myocardial infarction and cardiovascular outcomes. Heart. 2023;109(15):1159–65. https://doi.org/10.1136/heartjnl-2022-322115.
Zhang H, Yuan X, Zhang H, et al. Efficacy of long-term beta-blocker therapy for secondary prevention of long-term outcomes after coronary artery bypass grafting surgery. Circulation. 2015;131:21942201. https://doi.org/10.1161/CIRCULATIONAHA.114.014209.
Hjalmarson A. Prevention of sudden cardiac death with beta blockers. Clin Cardiol. 1999;22(Suppl 5):V11–5.
Everly MJ, Heaton PC, Cluxton RJ Jr. Beta-blocker underuse in secondary prevention of myocardial infarction. Ann Pharmacother. 2004;38(2):286–93. https://doi.org/10.1345/aph.1c472.
Kelly J, Kelleher K. Beta-blocker use in elderly patients with coronary heart disease. Age Ageing. 2000;29(1):17–21. https://doi.org/10.1093/ageing/29.1.17.
Fujii H, Kono K, Nishi S. Characteristics of coronary artery disease in chronic kidney disease. Clin Exp Nephrol. 2019;23(6):725–32. https://doi.org/10.1007/s10157-019-01718-5.
Sarnak MJ, Amann K, Bangalore S, et al. Chronic kidney disease and coronary artery disease: JACC state-of-the-art review. J Am Coll Cardiol. 2019;74(14):1823–38. https://doi.org/10.1016/j.jacc.2019.08.1017.
Matsue Y, Suzuki M, Nagahori W, Ohno M, Matsumura A, Hashimoto Y. β-blocker prevents sudden cardiac death in patients with hemodialysis. Int J Cardiol. 2013;165(3):519–22. https://doi.org/10.1016/j.ijcard.2011.09.037.
Lamb YN. Rosuvastatin/Ezetimibe: a review in hypercholesterolemia. Am J Cardiovasc Drugs. 2020;20(4):381–92. https://doi.org/10.1007/s40256-020-00421-1.
Priori SG, Blomström-Lundqvist C, Mazzanti A, et al. ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC). Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Eur Heart J. 2015;36(41):2793–867. https://doi.org/10.1093/europace/euv319.
Goldberger JJ, Cain ME, Hohnloser SH, et al. American Heart Association/American College of Cardiology Foundation/Heart Rhythm Society Scientific Statement on Noninvasive Risk Stratification Techniques for Identifying Patients at Risk for Sudden Cardiac Death. A scientific statement from the American Heart Association Council on Clinical Cardiology Committee on Electrocardiography and Arrhythmias and Council on Epidemiology and Prevention. J Am Coll Cardiol. 2008;52(14):1179–99. https://doi.org/10.1016/j.hrthm.2008.05.031.
Santangeli P, Dello Russo A, Casella M, Pelargonio G, Di Biase L, Natale A. Left ventricular ejection fraction for the risk stratification of sudden cardiac death: friend or foe? Intern Med J. 2011;41(1):55–60. https://doi.org/10.1111/j.1445-5994.2010.02371.x.
Stewart RAH, Held C, Hadziosmanovic N, et al. Physical activity and mortality in patients with stable coronary heart disease. J Am Coll Cardiol. 2017;70(14):1689–700. https://doi.org/10.1016/j.jacc.2017.08.017.
Medical Writing and Editorial Assistance
We declare that no medical writing or editorial assistance was received during the writing of this article (including AI).
Funding
The research was carried out within the framework of the Higher Education Institutional Excellence Program (TKP-2021-EGA-17). The Rapid Service Fee was funded by author Dr. Barbara Sandor.
Author information
Authors and Affiliations
Contributions
Barbara Sandor conceived the study. Gergely Galos, Eszter Szabados, Miklos Rabai, Rita Szalai, Luca Anna Ferkai, Ildiko Papp, Kalman Toth and Barbara Sandor contributed to the study design. Material preparation and data collection were performed by Gergely Galos and Ildiko Papp and analysis were performed by Barbara Sandor. The first draft of the manuscript was written by Gergely Galos and Barbara Sandor. Eszter Szabados, Miklos Rabai, Rita Szalai, Luca Anna Ferkai, Ildiko Papp and Kalman Toth commented on previous versions and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors Gergely Galos, Eszter Szabados, Miklos Rabai, Rita Szalai, Luca Anna Ferkai, Ildiko Papp, Kalman Toth and Barbara Sandor declare no conflicts of interest.
Ethical Approval
The study was approved by the Regional Ethics Committee of the University of Pecs (9274 – PTE 2022.). The study was conducted according to the guidelines of the Declaration of Helsinki. Informed consent was obtained from all subjects involved in the study.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Galos, G., Szabados, E., Rabai, M. et al. Evaluation of Incidence and Risk Factors of Sudden Cardiac Death in Patients with Chronic Coronary Syndrome Attending Physical Training. Cardiol Ther 12, 689–701 (2023). https://doi.org/10.1007/s40119-023-00331-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40119-023-00331-8