Abstract
Introduction
Considering the anticoagulant actions of vitamin D, we hypothesize that vitamin D status might affect the required dose of warfarin for maintaining the therapeutic international normalized ratio (INR).
Methods
In a retrospective single-center cohort study, serum levels of 25-hydroxyvitamin D were assessed for 89 subjects receiving a stable dose of warfarin for 3 months or longer and had a stable INR between 2 and 3.5 for at least three consecutive visits. A warfarin sensitivity index (WSI), defined as the steady-state INR divided by the mean daily warfarin dose, was used for measuring the warfarin dose response. The relation between the serum level of 25-hydroxyvitamin D and WSI value and the difference in the mean WSI value between the subjects with different vitamin D status categories (sufficient, insufficient, and deficient) were assessed.
Results
Twenty-one subjects had vitamin D deficiency, 43 had vitamin D insufficiency, and only 25 had normal levels of 25-hydroxyvitamin D. Based on the multiple linear regression analysis, there was a significant but weakly positive correlation between WSI and 25-hydroxyvitamin D serum levels, as the value of WSI increases by almost 0.0027434 for every unit increase in 25-hydroxyvitamin D serum level (p value = 0.041). Using one-way ANOVA analysis, there was a trend in a significant difference between the groups with different vitamin D status categories regarding the mean WSI value (F = 2.95, p value = 0.057), as subjects with sufficient vitamin D state compared to those with vitamin D deficiency had a higher WSI value.
Conclusions
Although the study’s limitations limit our ability to draw definite conclusions, the present data suggest that in addition to other traditional factors, vitamin D status might also affect warfarin sensitivity and maintenance dose requirement. However, to more clearly explain this link, further studies with high involvement subjects are required.
Similar content being viewed by others
A growing body of evidence has suggested that vitamin D, directly or indirectly, exerts anticoagulant effects. |
We hypothesize that the vitamin D status might affect the required dose of warfarin for maintaining the therapeutic international normalized ratio (INR). |
We found that compared to the patients with vitamin D deficiency, the patients with sufficient vitamin D state have a higher mean warfarin sensitivity index (WSI) value. |
These findings suggest that vitamin D status may also affect the sensitivity to warfarin and the maintenance dose requirements. |
Introduction
Although novel oral anticoagulants (NOACs) have become widely used in place of warfarin for chronic anticoagulation, in specific medical conditions such as patients with prosthetic valves, antiphospholipid syndrome, or a high risk of gastrointestinal bleeding, warfarin remains a preferred anticoagulant option [1]. However, despite the decades of clinical experience, high inter-individual variability in dose requirements, a narrow therapeutic range, and potential of several drug–disease, drug–food, and drug–drug interactions make warfarin a very challenging drug to use clinically, as under-dosing can lead to thromboembolism while overdosing may result in bleeding events or even death [2]. Numerous demographic, genetic, clinical, and environmental factors can influence warfarin maintenance dose requirements. Among them, genetic polymorphism of the vitamin K epoxide reductase complex 1 (VKORC1) and cytochrome p4502C9 (CYP2C9), which encode enzymes important in warfarin pharmacology, have the most significant influence [3]. Although algorithms based on a combination of demographic, clinical, and genetic factors have been developed for clinical use in predicting warfarin dose requirements [4, 5], they had limited success [6]. Thus, predicting an accurate maintenance dose of warfarin remains challenging in clinical practice [7].
Vitamin D is a fat-soluble vitamin that can be obtained from dietary sources, synthesized in the skin through exposure to sunlight, or dietary supplements [8]. The active form of vitamin D is 1,25-dihydroxyvitamin D that exerts most of its functions through a vitamin D receptor (VDR) distributed all over the body in diverse cells and tissues [9]. It has been well established that aside from its essential role in skeletal health and calcium and phosphorous homeostasis, vitamin D regulates diverse biological processes in numerous extra-skeletal systems [10]. However, vitamin D deficiency is now recognized as a pandemic, reportedly occurring in 30 to 60% of the general population worldwide [11, 12]. Accumulating epidemiological and laboratory evidence has documented that deficiency of vitamin D is associated with the onset and progression of many chronic diseases, such as cardiovascular disorders, neurodegenerative diseases, malignancies, and immune system disease [13]. Interestingly, more recently, a growing body of evidence has suggested that vitamin D, directly or indirectly, exerts anticoagulant effects, highlighting the potential role of vitamin D deficiency in the pathogenesis of thrombosis [14]. It has been shown that VDR ligands regulate the expression and activity of several pro- and anti-thrombotic proteins of the coagulation cascade [15,16,17]. According to this evidence, in some clinical studies, supplementation of vitamin D has been investigated as a potential therapeutic option for prophylaxis and treatment of thromboembolic events [18,19,20]. Moreover, recently, results of one pilot clinical trial showed that vitamin D supplementation enhances the anticoagulant effect of warfarin and thereby reduces warfarin maintenance dose requirement [21]. In light of this evidence, we hypothesize that vitamin D status might influence the dose of warfarin required to maintain a therapeutic international normalized ratio (INR), and compared to patients with vitamin D insufficiency and deficiency, patients with sufficient vitamin D state might require lower maintenance doses of warfarin to keep the INR within the therapeutic range.
Methods
Study Design
This single medical center retrospective cohort study was conducted at a cardiology outpatient clinic of a tertiary teaching hospital in the west of Iran between May 2021 and October 2021. The study was approved by the Ethics Committee of Hamadan University of Medical Sciences (license number: IR.UMSHA.REC.1400.620). Written informed consent was obtained from all participants after a thorough explanation of the study’s aims and protocol.
Recruited Patients
The study participants were recruited from the patients with medical records in the clinic. The inclusion criteria were as follows: ambulatory adult patients (18 years of age or older) who were receiving a stable dose of warfarin for 3 months or longer and had a stable INR between 2 and 3.5 for 3 months on at least three consecutive visits. To control for confounders, subjects with the following were excluded from the study: concurrent diseases which might influence warfarin requirements, including moderate to severe liver function impairment (serum aminotransferase levels at least twice the upper limit of normal), chronic kidney disease (eGFR < 60 ml/min/1.73 m2), advanced heart failure, hypothyroidism/hyperthyroidism, consumption of medication(s) known to have a major interaction with warfarin, smoking, heavy alcohol consumption (more than two drinks per day), obesity (body mass index (BMI) ≥ 30 kg/m2, history of vitamin D supplement therapy during recent 3 months, non-compliance, and pregnancy. Serum levels of 25-hydroxyvitamin D were assessed for 89 subjects who fulfilled inclusion and exclusion criteria. Finally, according to the vitamin D status, the subjects were divided into three groups: subjects with sufficient vitamin D, subjects with vitamin D insufficiency, and subjects with vitamin D deficiency.
Data Sampling
The following clinical and demographic information, including age (divided into “less than 65 years” and “more than 65 years”), gender, body weight, height, BMI, concomitant medications, and co-morbidities, indication for warfarin therapy, duration of warfarin therapy, INR, daily and weekly warfarin dose. The warfarin sensitivity index (WSI) was used for measuring the warfarin dose response. The WSI is a useful measure of a warfarin dose–response relationship as it incorporates the effect of warfarin dosage on resulting INRs [22,23,24]. The WSI value was calculated by dividing the steady-state INR value by the average daily warfarin dose calculated from the total weekly dose of warfarin.
25-hydroxyvitamin D Assay Method
Blood samples for assay of the serum concentration of 25-hydroxyvitamin D, which reflects total body vitamin D status, were taken at 08:30–9:30 a.m. after an overnight fast. Serum level of 25-hydroxyvitamin D was measured in duplicate using the enzyme-linked fluorescent assay (ELFA) technology (VIDAS system, Biomerieux, Paris, France). The results were reported in ng/ml. The limit of quantification (LOQ) is the lowest analyte concentration that can be quantitatively detected with a laboratory test, and for VIDAS Vit D kit LOQ is 8.1 ng/ml. The 25-hydroxyvitamin D levels lower than 20 ng/ml were considered as deficiency of vitamin D, concentrations between 21 and 29 ng/ml were considered as insufficient vitamin D, and concentrations between 30 and 100 ng/ml were considered as sufficient vitamin D [25].
Study Outcomes
The primary outcome was the relation between serum level of 25-hydroxyvitamin D and WSI value as well as the difference in the WSI value of the subjects with different vitamin D status categories (sufficient, insufficient, and deficient). Further, as a secondary outcome, it also examined whether there is a correlation or association between the WSI value and each of the other clinical/demographic variables of the study population, including age, BMI, gender, indication for warfarin therapy, as well as duration of warfarin therapy.
Statistical Analyses
All statistical analyses were performed using SPSS 21.0 (IBM Inc., Armonk, NY, USA). Descriptive statistics were used to assess baseline characteristics. The normal distribution of continuous data was examined using Shapiro–Wilk test. Continuous data were expressed as mean (standard deviation, SD). Categorical data were expressed as numbers with percentages. Differences among the mean WSI value of the groups were assessed using a one-way analysis of variance (ANOVA). A Tukey post hoc test was utilized to determine which vitamin D status classifications had a statistically significant difference on the mean WSI of the study patients. A Pearson correlation coefficient was calculated to assess the correlation between 25-hydroxyvitamin D serum levels and WSI values. Further, the multiple linear regression model was used to assess the correlation between WSI and demographic and clinical characteristics. All analyses were performed at a significant level of p value < 0.05.
Results
One hundred seventy-four ambulatory warfarin-treated patients were screened for enrollment. Of them, 85 were excluded. Eighty-nine patients who fulfilled the inclusion and exclusion criteria and gave informed consent to participate were enrolled in the study. The demographic and clinical characteristics of all study participants are presented in Table 1. All subjects participating in this study were Iranian. The mean age of the participants was 54.36 years (range, 19–79 years), and 51 (57.30%) were women. The mean WSI value for all subjects was 0.56 ± 0.21 (ranged, 0.31–1.12), and the mean of their INR value was 2.7 ± 0.38. The mean length of treatment with warfarin was 10.17 years (range, 1–28 years). The majority (41.6%) were treated for atrial fibrillation, while mechanical heart valve and venous thromboembolism were other indications for treatment with warfarin. The mean serum level of 25-hydroxyvitamin D for all subjects was 28.53 ng/ml (range, 8.10–76.30 ng/ml). Twenty-one subjects (23.6%) had vitamin D deficiency, 43 (48.3%) had vitamin D insufficiency, and only 25 (28.1%) had normal levels of 25-hydroxyvitamin D.
The correlation between WSI values and different clinical and demographic categorical variables of the study population is shown in Table 2. As shown, across the participants’ age category, subjects aged ≥ 65 years compared to those aged < 65 had a significantly higher mean WSI value (p value < 0.001). There was no significant correlation between WSI values and other clinical and demographic categorical variables.
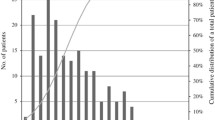
A depiction of the mean WSI value of the groups across vitamin D status categories has been shown in Fig. 1. The mean WSI value was 0.63 ± 0.21 in subjects with sufficient vitamin D state, 0.55 ± 0.19 in those with vitamin D insufficiency, and 0.49 ± 0.17 in those with vitamin D deficiency. Using one-way ANOVA analysis, there was a trend in a significant difference between the groups regarding the mean WSI value (Fig. 1, F = 2.95, p value = 0.057). Tukey’s post hoc test showed that the subjects with sufficient vitamin D state compared to those with vitamin D deficiency had a significantly higher WSI value (Fig. 1; p value = 0.047), demonstrating that subjects with sufficient vitamin D state compared to the deficient patients required lower warfarin dose to maintain their INR in the therapeutic range. The mean WSI value was also higher in subjects with sufficient vitamin D state than those with vitamin D insufficiency (0.63 ± 0.21 versus 0.55 ± 0.19), although the difference did not reach statistical significance (p value = 0.268).
Comparison of the mean warfarin sensitivity index (WSI) value between subjects with different vitamin D status. The results are expressed as means ± SD. One-way analysis of variance (ANOVA) was used for statistical analysis followed with Tukey’s post hoc test, at a significance level of 0.05. Results of one-way ANOVA analysis: F = 2.95, p value = 0.057. *p value < 0.05 compared with the sufficient vitamin D group
The relation between the serum level of 25-hydroxyvitamin D and WSI value is shown in Fig. 2. Based on the Pearson correlation analysis, we found that there was a possible weak but statistically significant positive correlation between the two variables (r = 0.199, p value = 0.003). This result suggested that the sensitivity to warfarin increased as the patients’ 25-hydroxyvitamin D concentration increased.
The correlation between the WSI value and demographic and clinical characteristics using multiple linear regression analysis is given in Table 3. Based on these results, there was a significant but weakly positive correlation between WSI and 25-hydroxyvitamin D serum levels and age. The value of WSI increases by almost 0.0027434 for every unit increase in 25-hydroxyvitamin D serum level adjusted for variables mentioned in the Table (p value = 0.041). In addition, the value of WSI increases by almost 0.0067841 for each year's increase in age (p value < 0.001). There was no significant correlation between the WSI value and other variables, including sex, BMI, and duration of warfarin treatment.
Discussion
To the best of our knowledge, our study is one of the first studies that addressed the influence of vitamin D status on warfarin maintenance dose requirements. Based on the results of our survey, there was a significant but weakly positive correlation between WSI and 25-hydroxyvitamin D serum levels. Our results showed that compared to the patients with vitamin D deficiency, the patients with sufficient vitamin D state had a higher mean WSI value, indicating that patients with sufficient vitamin D state require lower warfarin doses to maintain their INR in the therapeutic range. Our data suggests that, in addition to other traditional factors, vitamin D status may influence sensitivity to warfarin and maintenance dose requirements. This should be considered when determining warfarin dosing.
The exact molecular mechanism by which vitamin D exerts its anticoagulant effects has not been fully elucidated. Nevertheless, vitamin D, through regulatory effects on coagulation factors, endothelium homeostasis, and inflammatory pathways, exerts a protective role against the occurrence of thrombosis [26]. Both in vitro and in vivo experiments demonstrated that vitamin D and other VDR ligands up-regulate the expression of thrombomodulin, and down-regulate the expression of tissue factor (TF) [15, 17, 27,28,29]. TF is the high-affinity receptor and cofactor for factor VII/VIIa that plays a primary role in initiating the coagulation cascade [30]. On the other hand, thrombomodulin is an anticoagulant glycoprotein involved in promoting the activation of the anticoagulant protein C pathway [31]. Apart from this, vitamin D has been shown to reduce the production of pro-inflammatory cytokines that can induce a pro-thrombotic state by increasing the production of TF on the endothelium and suppressing the synthesis of the anticoagulant protein C [32,33,34]. The protective effect of VDR on endothelial cells has also been identified [35,36,37]. It has been observed that vitamin D therapy, through activation of VDR, improves endothelial function and thereby suppresses thrombogenicity in patients with vitamin D deficiency or insufficiency [38].
Accumulative data from the clinical reports are increasingly reporting a strong negative relationship between serum levels of 25-hydroxyvitamin D and the development of venous thromboembolism, suggesting inadequate vitamin D levels may increase the risk of venous thromboembolism [39,40,41,42]. Consistent with this evidence, several epidemiological studies have highlighted a seasonal pattern for the occurrence of thrombotic events, as the risk of thrombotic events is greater in the winter months compared to the summer months, which is thought to be related to the seasonal variation in vitamin D status [43,44,45]. In support of this hypothesis, the results of a prospective study on a cohort of 40,000 southern Swedish women after 11 years follow-up indicated that women with a habit of more active sun exposure were at a 30% lower risk of thromboembolism events than those who did not [46]. This evidence suggests that treating vitamin D deficiency or insufficiency can reduce the risk of venous thromboembolism events [14, 47]. Hejazi and colleagues in a pilot randomized control clinical trial on subjects with a diagnosis of deep vein thrombosis or pulmonary embolism who had vitamin D deficiency showed that compared to placebo treatment, subjects receiving oral vitamin D3 supplementation required significantly lower doses of warfarin to achieve a therapeutic INR. They concluded that treating vitamin D deficiency could enhance the anticoagulant effects of warfarin [21]. Consistent with these findings, in 2006, Beer and colleagues, in a randomized controlled clinical study on 250 men suffering from prostate cancer, showed that in comparison to the placebo, administration of a weekly high dose of calcitriol, as an active form of vitamin D3, could reduce thromboembolic events in such patients. They postulated that this benefit might be related to calcitriol’s antithrombotic effects [18]. Similarly, Moscarelli et al. also reported that combined therapy with calcitriol, angiotensin receptor blockers (ARBs), and angiotensin-converting enzyme inhibitors (ACEIs) could reduce the rate of venous thromboembolism in renal transplant recipients [48]. However, some inconsistent data have also been reported. Blondon and coworkers, in a randomized, double-blind, placebo-controlled trial where the participants were followed for an average period of 7 years, found that supplementation with calcium (1000 mg) plus vitamin D (400 IU) does not influence the overall risk of venous thrombotic events in postmenopausal women. The authors speculated that a higher dose of vitamin D might be required to see the antithrombotic effects of vitamin D supplementation in the general population [49]. However, in a supplemental analysis, they detected a modest thrombotic risk reduction for idiopathic thrombotic events among women with low 25-hydroxyvitamin D concentrations at baseline, which suggests subjects with severe vitamin D deficiency may benefit from vitamin D supplementation [49]. In support of this hypothesis, Blondon et al., in their recent study, showed that supplementation with a high dose of vitamin D for 3 months in subjects with severe vitamin D deficiency could decrease a prothrombotic profile [20]. However, some other studies evaluating the impact of vitamin D supplementation on coagulation and fibrinolysis parameters have generated conflicting data. A study conducted by Jorde et al. on obese or overweight subjects who had high serum vitamin D levels at baseline (a mean serum 25-hydroxyvitamin D level of 61.8 nmol/l), 1-year high-dose treatment of vitamin D (40,000 IU weekly) did not affect the fibrinolytic and thrombin generation parameters [50]. In a prospective cohort study of patients with vitamin D deficiency (25-hydroxyvitamin D serum levels of < 25 nmol/l) with and without hyperparathyroidism, the coagulation or fibrinolysis parameters did not change after 2 months of vitamin D treatment (900,000 IU in 2 months) [51]. Interestingly, in another study, Saliba and colleagues showed that vitamin D supplementation at a dose of 2000 IU daily for 90 days in healthy participants with serum 25-hydroxyvitamin D < 50 nmol/l levels could have prothrombotic effects [52]. Several factors, including the selected participants, having or not having comorbidities such as cardiovascular diseases and hyperparathyroidism, and methods of assaying fibrinolytic and thrombin generation parameters may be possible explanations for these conflicting data. However, the current data in the literature suggests that subjects with vitamin D deficiency might benefit more from the anticoagulant actions of vitamin D supplementation [14]. More studies are needed to elucidate which population may benefit from the anticoagulation actions of vitamin D supplementation.
Despite the novelty of our findings, there are some limitations in the present research. The main limitation of this study is that it was a retrospective single-center investigation with a relatively small number of participants. Further, unassessed confounding factors, such as diet and genotype that could affect the warfarin dose requirement, may affect the results in a way not anticipated. Additionally, due to financial constriction, we did not assess the relationship between vitamin D status and coagulation and fibrinolysis parameters. Thus, these findings should be interpreted with caution, and future studies are needed to better assess the relationship between vitamin D status and warfarin maintenance dose requirements.
Conclusions
Although the study’s limitations limit our ability to draw definite conclusions, our data provided preliminary evidence that, in addition to other traditional factors, vitamin D status might also affect sensitivity to warfarin and the maintenance dose requirements. We found that compared to patients with vitamin D deficiency, patients with sufficient vitamin D state had a trend to a higher sensitivity to warfarin and may require lower doses of warfarin for maintaining therapeutic INRs. Hence, it is relevant to treat vitamin D deficiency and insufficiency in patients requiring warfarin therapy. This may augment the anticoagulant effect of warfarin and reduce the required dose of warfarin to maintain INR values within the therapeutic range and thereby decrease the risk of hemorrhagic complications. However, additional studies with large, diverse patient cohorts are needed to clarify the link between vitamin D therapy and thromboembolic prevention with warfarin.
References
Wadsworth D, Sullivan E, Jacky T, Sprague T, Feinman H, Kim J. A review of indications and comorbidities in which warfarin may be the preferred oral anticoagulant. J Clin Pharm Ther. 2021;46(3):560–70.
Wen M-S, Lee MTM. Warfarin pharmacogenetics: new life for an old drug. Acta Cardiol Sin. 2013;29(3):235.
James A, Britt R, Raskino C, Thompson S. Factors affecting the maintenance dose of warfarin. J Clin Pathol. 1992;45(8):704–6.
Gage B, Eby C, Johnson J, Deych E, Rieder M, Ridker P, Milligan P, Grice G, Lenzini P, Rettie A. Use of pharmacogenetic and clinical factors to predict the therapeutic dose of warfarin. Clin Pharmacol Ther. 2008;84(3):326–31.
Shi C, Yan W, Wang G, Wang F, Li Q, Lin N. Pharmacogenetics-based versus conventional dosing of warfarin: a meta-analysis of randomized controlled trials. PLoS ONE. 2015;10(12): e0144511.
Kimmel SE. Warfarin therapy: in need of improvement after all these years. Expert Opin Pharmacother. 2008;9(5):677–86.
Nielsen PB, Lundbye-Christensen S, van der Male M, Larsen TB. Using a personalized decision support algorithm for dosing in warfarin treatment: a randomised controlled trial. Clin Trials Regul Sci Cardiol. 2017;25:1–6.
Stroud ML, Stilgoe S, Stott VE, Alhabian O, Salman K. Vitamin D: a review. Aust J General Pract. 2008;37(12):1002.
Issa L, Leong G, Eisman J. Molecular mechanism of vitamin D receptor action. Inflamm Res. 1998;47(12):451–75.
Pike JW, Christakos S. Biology and mechanisms of action of the vitamin D hormone. Endocrinol Metab Clin. 2017;46(4):815–43.
Thacher TD, Clarke BL. Vitamin D insufficiency. In: Mayo Clinic Proceedings: 2011: Elsevier; 2011, pp 50–60.
Adams J, Hewison M. Update in vitamin D. J Clin Endocrinol Metab. 2010;95:471–8.
Wang H, Chen W, Li D, Yin X, Zhang X, Olsen N, Zheng SG. Vitamin D and chronic diseases. Aging Dis. 2017;8(3):346.
Mohammad S, Mishra A, Ashraf MZ. Emerging role of vitamin D and its associated molecules in pathways related to pathogenesis of thrombosis. Biomolecules. 2019;9(11):649.
Ohsawa M, Koyama T, Yamamoto K, Hirosawa S, Kamei S, Kamiyama R. 1α, 25-dihydroxyvitamin D3 and its potent synthetic analogs downregulate tissue factor and upregulate thrombomodulin expression in monocytic cells, counteracting the effects of tumor necrosis factor and oxidized LDL. Circulation. 2000;102(23):2867–72.
Koyama T, Shibakura M, Ohsawa M, Kamiyama R, Hirosawa S. Anticoagulant effects of 1α, 25-dihydroxyvitamin D3 on human myelogenous leukemia cells and monocytes. Blood J Am Soc Hematol. 1998;92(1):160–7.
Maillard C, Berruyer M, Serre CM, Amiral J, Dechavanne M, Delmas PD. Thrombomodulin is synthesized by osteoblasts, stimulated by 1, 25-(OH) 2D3 and activates protein C at their cell membrane. Endocrinology. 1993;133(2):668–74.
Beer TM, Venner PM, Ryan CW, Petrylak DP, Chatta G, Dean Ruether J, Chi KN, Curd JG, DeLoughery TG. High dose calcitriol may reduce thrombosis in cancer patients. Br J Haematol. 2006;135(3):392–4.
Gholami K, Talasaz AH, Entezari-Maleki T, Salarifar M, Hadjibabaie M, Javadi MR, Dousti S, Hamishehkar H, Maleki S. The effect of high-dose vitamin D3 on soluble P-selectin and hs-CRP level in patients with venous thromboembolism: a randomized clinical trial. Clin Appl Thromb Hemost. 2016;22(5):483–9.
Blondon M, Biver E, Braillard O, Righini M, Fontana P, Casini A. Thrombin generation and fibrin clot structure after vitamin D supplementation. Endocr Connect. 2019;8(11):1447–54.
Hejazi ME, Modarresi-Ghazani F, Hamishehkar H, Mesgari-Abbasi M, Dousti S, Entezari-Maleki T. The effect of treatment of vitamin D deficiency on the level of P-selectin and hs-CRP in patients with thromboembolism: a pilot randomized clinical trial. J Clin Pharmacol. 2017;57(1):40–7.
Halkin H, Shapiro J, Kurnik D, Loebstein R, Shalev V, Kokia E. Increased warfarin doses and decreased international normalized ratio response after nationwide generic switching. Clin Pharmacol Ther. 2003;74(3):215–21.
Lubetsky A, Dekel-Stern E, Chetrit A, Lubin F, Halkin H. Vitamin K intake and sensitivity to warfarin in patients consuming regular diets. Thromb Haemost. 1999;81(03):396–9.
Rahman M, BinEsmael TM, Payne N, Butchart EG. Increased sensitivity to warfarin after heart valve replacement. Ann Pharmacother. 2006;40(3):397–401.
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, Murad MH, Weaver CM. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(7):1911–30.
Mohd S, Sharma S, Mishra A, Ashraf MZ. Vitamin D and its relationship with the pathways related to thrombosis and various diseases. London: IntechOpen; 2021.
Martinez-Moreno JM, Herencia C, Oca AM, Muñoz-Castañeda JR, Rodríguez-Ortiz ME, Díaz-Tocados JM, Peralbo-Santaella E, Camargo A, Canalejo A, Rodriguez M. Vitamin D modulates tissue factor and protease-activated receptor 2 expression in vascular smooth muscle cells. FASEB J. 2016;30(3):1367–76.
Toderici M, de la Morena-Barrio ME, Padilla J, Minano A, Antón AI, Iniesta JA, Herranz MT, Fernández N, Vicente V, Corral J. Identification of regulatory mutations in SERPINC1 affecting vitamin D response elements associated with antithrombin deficiency. PLoS ONE. 2016;11(3): e0152159.
Koyama T, Hirosawa S. Anticoagulant effects of synthetic retinoids and activated vitamin D3. In: Seminars in thrombosis and hemostasis: 1998: Copyright© 1998 by Thieme Medical Publishers, Inc.; 1998, pp 217–26.
Grover SP, Mackman N. Tissue factor: an essential mediator of hemostasis and trigger of thrombosis. Arterioscler Thromb Vasc Biol. 2018;38(4):709–25.
Weiler H, Isermann B. Thrombomodulin. J Thromb Haemost. 2003;1(7):1515–24.
Equils O, Naiki Y, Shapiro A, Michelsen K, Lu D, Adams J, Jordan S. 1, 25-Dihydroxyvitamin D3 inhibits lipopolysaccharide-induced immune activation in human endothelial cells. Clin Exp Immunol. 2006;143(1):58–64.
Veldman CM, Cantorna MT, DeLuca HF. Expression of 1, 25-dihydroxyvitamin D3 receptor in the immune system. Arch Biochem Biophys. 2000;374(2):334–8.
Timms P, Mannan N, Hitman G, Noonan K, Mills P, Syndercombe-Court D, Aganna E, Price C, Boucher B. Circulating MMP9, vitamin D and variation in the TIMP-1 response with VDR genotype: mechanisms for inflammatory damage in chronic disorders? QJM. 2002;95(12):787–96.
Xu W, Hu X, Qi X, Zhu R, Li C, Zhu Y, Yin S, Cheng L, Zhu R. Vitamin D ameliorates angiotensin II-induced human endothelial progenitor cell injury via the PPAR-γ/HO-1 pathway. J Vasc Res. 2019;56(1):17–27.
Kim D-H, Meza CA, Clarke H, Kim J-S, Hickner RC. Vitamin D and endothelial function. Nutrients. 2020;12(2):575.
Brewer CL, Michos DE, Reis PJ. Vitamin D in atherosclerosis, vascular disease, and endothelial function. Curr Drug Targets. 2011;12(1):54–60.
Hammer Y, Soudry A, Levi A, Talmor-Barkan Y, Leshem-Lev D, Singer J, Kornowski R, Lev EI. Effect of vitamin D on endothelial progenitor cells function. PLoS ONE. 2017;12(5): e0178057.
Wu W-X, He D-R. Low vitamin D levels are associated with the development of deep venous thromboembolic events in patients with ischemic stroke. Clin Appl Thrombosis Hemostasis. 2018;24(9_suppl):69S-75S.
Dehghani K, Nowrouzi A, Pourdavood AH, Rahmanian Z. Effect of Vitamin D deficiency in lower extremity and pulmonary venous thromboembolism. Biomed Res Therapy. 2019;6(4):3107–12.
Brøndum-Jacobsen P, Benn M, Tybjaerg-Hansen A, Nordestgaard B. 25-Hydroxyvitamin D concentrations and risk of venous thromboembolism in the general population with 18 791 participants. J Thromb Haemost. 2013;11(3):423–31.
Ehsanian R, Timmerman MA, Wright JM, McKenna S, Dirlikov B, Crew J. Venous thromboembolism is associated with lack of vitamin D supplementation in patients with spinal cord injury and low vitamin D levels. PM&R. 2019;11(2):125–34.
Gallerani M, Boari B, De Toma D, Salmi R, Manfredini R. Seasonal variation in the occurrence of deep vein thrombosis. Med Sci Monitor. 2004;10(5):CR191–6.
Clauss R, Mayes J, Hilton P, Lawrenson R. The influence of weather and environment on pulmonary embolism: pollutants and fossil fuels. Med Hypotheses. 2005;64(6):1198–201.
Ho J-D, Tsai C-Y, Liou S-W, Tsai RJ-F, Lin H-C. Seasonal variations in the occurrence of retinal vein occlusion: a five-year nationwide population-based study from Taiwan. Am J Ophthalmol. 2008;145(4):722-728.e723.
Lindqvist P, Epstein E, Olsson H. Does an active sun exposure habit lower the risk of venous thrombotic events? AD-lightful hypothesis. J Thromb Haemost. 2009;7(4):605–10.
Banerjee A, Khemka VK. Augmentation of anticoagulant effect with vitamin D: possible therapeutic target for venous thromboembolism. Int J Hematol Blo Dis. 2017;2(1):1–5.
Moscarelli L, Zanazzi M, Bertoni E, Caroti L, Rosso G, Farsetti S, Annunziata F, Paudice N, Salvadori M. Renin angiotensin system blockade and activated vitamin D as a means of preventing deep vein thrombosis in renal transplant recipients. Clin Nephrol. 2011;75(5):440–50.
Blondon M, Rodabough RJ, Budrys N, Johnson KC, Berger JS, Shikany JM, Raiesdana A, Heckbert SR, Manson JE, LaCroix AZ. The effect of calcium plus vitamin D supplementation on the risk of venous thromboembolism. Thromb Haemost. 2015;113(05):999–1009.
Jorde R, Sneve M, Torjesen P, Figenschau Y, Hansen J-B. Parameters of the thrombogram are associated with serum 25-hydroxyvitamin D levels at baseline, but not affected during supplementation with vitamin D. Thromb Res. 2010;125(5):e210–3.
Elbers LP, Wijnberge M, Meijers JC, Poland DC, Brandjes DP, Fliers E, Gerdes VE. Coagulation and fibrinolysis in hyperparathyroidism secondary to vitamin D deficiency. Endocr Connect. 2018;7(2):325–33.
Saliba W, Awad K, Ron G, Elias M. The effect of vitamin D supplementation on thrombin generation assessed by the calibrated automated thrombogram. Clin Appl Thromb Hemost. 2016;22(4):340–5.
Acknowledgements
We thank all patients and medical staff of the outpatient cardiology clinic of Farshchian Cardiovascular Hospital that contributed to this study.
Funding
This research was partially supported by funding from the vice-chancellor for research and technology, Hamadan University of Medical Sciences, Hamadan, Iran (Grant no: 140009097536). This grant was just for the provision of laboratory assessment of the study and was not assigned to the manuscript writing, editing, and publication fee.
Author contributions
Conceptualization: NK and MM. Methodology: NK, MM, and JP. Data acquisition: SH, NK, and MB. Statistical analysis: MM and JP. Writing—original draft preparation: MB. Writing—review and editing: SH and MM. All authors contributed to the interpretation of the results and read and approved the final manuscript.
Disclosures
Nakisa Khansari, Maryam Bagheri, Shahram Homayounfar, Jalal Poorolajal, and Maryam Mehrpooya all have nothing to disclose.
Compliance with ethics guidelines
The trial protocol was according to the Declaration of Helsinki as revised in 1989, and the study protocol was approved by the research and ethics committee at Hamadan University of Medical Sciences (IR.UMSHA.REC.1400.260). Written informed consent was obtained from all participants after a thorough explanation of the study’s aims and protocol.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request up to 2 years after publication.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Khansari, N., Bagheri, M., Homayounfar, S. et al. Influence of Vitamin D Status on the Maintenance Dose of Warfarin in Patients Receiving Chronic Warfarin Therapy. Cardiol Ther 11, 421–432 (2022). https://doi.org/10.1007/s40119-022-00268-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40119-022-00268-4