Abstract
Introduction
The effectiveness of telmisartan has been reported in Indian clinical trials; however, real-world data are limited. We aimed to provide real-world evidence regarding the effectiveness of telmisartan as monotherapy or in combination with other antihypertensive drugs (AHDs) in Indian patients with essential hypertension.
Methods
Electronic medical record data of adult patients diagnosed with essential hypertension (≥ 140/90 mmHg) and who were prescribed telmisartan as mono- or add-on therapy were retrospectively analyzed. Patients were classified according to the number of AHD classes prescribed on initiating telmisartan. Change in systolic and diastolic blood pressure (SBP and DBP) after a month of treatment and the proportion of patients who achieved treatment goals according to the 2018 European Society of Cardiology/European Society of Hypertension guidelines were evaluated.
Results
A majority (90.6%) of the 1304 patients included in the study were on telmisartan monotherapy or telmisartan + 1 AHD. The mean (95% confidence interval [CI]) change in the telmisartan monotherapy group was SBP (−13.3 [−14.6, −12.0] mmHg) and DBP (−7.2 [−7.9, −6.5] mmHg), and the mean (95% CI) change in the telmisartan + 1 AHD group was SBP (−10.8 [−13.1, −8.5] mmHg) and DBP (−6.5 [−7.7, −5.3] mmHg) (P < 0.001 for all). SBP and DBP goals were achieved by 35.9% and 47.3% of patients on telmisartan monotherapy and by 35.9% and 46.8% of patients on telmisartan + 1 AHD. Among patients with comorbid diabetes, the mean (95% CI) change in the telmisartan monotherapy group was SBP (−13.3 [−15.0, −11.6] mmHg) and DBP (−7.3 [-8.2, −6.5] mmHg), and the mean (95% CI) change in the telmisartan + 1 AHD group was SBP (−13.0 [−16.5, −9.5] mmHg) and DBP (−6.9 [−8.7, −5.1] mmHg) (P < 0.001 for all). SBP and DBP goals were achieved by 31.7% and 39.7% of patients on telmisartan monotherapy and by 31.9% and 41.8% of patients on telmisartan + 1 AHD.
Conclusion
Telmisartan may be a good candidate for blood pressure control in Indian patients with essential hypertension and comorbidities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
We evaluated the effectiveness of telmisartan prescribed to Indian patients with hypertension during routine clinical practice in India. |
Telmisartan was found to be effective in reducing blood pressure in patients with mild to moderate hypertension and comorbid diabetes or dyslipidemia during routine clinical practice in India. |
Digital Features
This article is published with digital features, including a summary slide, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.14199011.
Introduction
Hypertension, a major risk factor for cardiovascular diseases such as arrhythmia, stroke, and valvular heart disease [1] is on the rise globally. In India, the Great India Blood Pressure survey reported 234 million adults with hypertension [2], with around 98,912 deaths and over 2.5 million disability-adjusted life-years attributed to hypertensive heart disease in 2017 [3]. Poor control of hypertension also results in higher healthcare resource utilization and costs [4]. In spite of the negative outcomes of hypertension, overall awareness, treatment, and control of hypertension in India remains poor [5, 6].
A plethora of guidelines, including the 2014 Eighth Joint National Committee evidence-based guidelines [7], 2017 American College of Cardiology guidelines [8], 2018 European Society of Cardiology/European Society of Hypertension (ESC/ESH) guidelines [9], and 2019 Indian Guidelines on Hypertension–IV (IGH-IV) [10], describe the definition, evaluation, classification, and management of hypertension. Angiotensin receptor II blockers (ARBs) are one of the first-line drug classes recommended by the aforementioned guidelines [7,8,9,10]. In line with these guidelines, multiple observational studies have reported the use of ARBs as first-line therapy both as monotherapy and in combination with other antihypertensive drugs (AHDs) for the management of essential hypertension in India [11,12,13,14,15,16]. Among ARBs, telmisartan was reported to be preferred by almost 73% of physicians in India as a first-line agent for managing essential hypertension [11].
Telmisartan has been proven to be effective in reducing blood pressure in Indian patients with hypertension in clinical trials [17, 18] as well as a few real-world studies [19, 20]. However, the real-world data currently available are either more than a decade old or localized to a single center. Moreover, these studies evaluated telmisartan either as monotherapy or in a single combination. We conducted the present study to provide updated evidence regarding the effectiveness of telmisartan as mono- or add-on therapy among Indian patients with essential hypertension in a real-world setting.
Methods
Data Source(s)
Analysis was performed with an Indian electronic software owned and administered by HealthPlix Technologies PRV. This software has been in operation since 2016 and fulfills the day-to-day operational needs of 12 medical specialties across 150+ cities in 20 states. Information including demographics, diagnoses, medications, cardiac risk factors, tests and procedures conducted, functional status, and other data elements obtained from the software were used to conduct the analysis.
The study was conducted according to the applicable national regulatory laws and guidelines. The study protocol was approved by an independent ethics committee (Suraksha—Ethics Committee, Asian Institute of Medical Sciences [AIIMS], Dombivli, Maharashtra, India) on 03 December, 2019. Patient confidentiality was maintained at all times, as the study was performed using anonymized information only.
Study Design and Sample Selection
This retrospective observational study assessed the electronic medical record (EMR) data of Indian patients diagnosed with essential hypertension between January 2018 and September 2019. HealthPlix Technologies PRV identified the AHDs that were prescribed to the patients by mapping the brand name on the prescriptions with the generic name. Adult patients (≥ 18 years old) who were diagnosed with essential hypertension by their physicians according to the 2018 ESC/ESH [9] and 2019 IGH-IV guidelines [10] (≥ 140/90 mmHg) at baseline, were prescribed telmisartan either as monotherapy or add-on therapy, and had data available for at least two visits with a minimum gap of 1 month after initiation of telmisartan were included in the study. Patients diagnosed with secondary hypertension and those on other ARBs at visit 1 (baseline) were excluded from the study.
Each patient was required to have two valid blood pressure (BP) readings in the EMR. Visit 1 (baseline) reading was the BP measurement taken on the day of telmisartan initiation, and visit 2 reading was the first available BP reading after ≥ 30 days of telmisartan initiation. The gap of ≥ 30 days was observed because a smaller gap between visits might result in inaccurate analyses. This reading was required to be obtained before the earliest event among telmisartan discontinuation, initiation of any other AHD, or end of study period. Further readings available until telmisartan discontinuation, addition of new therapy, or up to end of study were collected.
Study Endpoints
The primary endpoint was the mean change in systolic BP (SBP) and diastolic BP (DBP) from baseline to post-index (composite of telmisartan discontinuation, addition of new therapy, or up to end of study) in patients prescribed telmisartan. The secondary endpoint was the proportion of patients with essential hypertension on telmisartan who achieved individualized BP goals (SBP and DBP) according to ESC/ESH 2018 guidelines from baseline to post-index (telmisartan discontinuation, addition of new therapy, or up to end of study). These endpoints were also assessed according to subgroups (age; gender; and comorbid diabetes, chronic kidney disease [CKD], coronary artery disease [CAD], stroke, or dyslipidemia).
Assessments
Demographic characteristics including age, gender, personal and family history, and clinical characteristics such as grade of hypertension according to ESC/ESH 2018 guidelines, BP readings, comorbidities as diagnosed by the physician, medications used within the previous 30 days (identified based on prescriptions), and laboratory data and electrocardiogram in the last 6 months (if available) were collected at baseline. Data regarding BP, medications in use, and laboratory data were collected from the next visit.
Prior antihypertensive therapy was defined as the use of any AHDs before initiation of telmisartan that were not discontinued on or before the start of telmisartan therapy. Prior AHDs were classified into the following groups: angiotensin-converting enzyme inhibitors/angiotensin II receptor blockers, β-blockers, diuretics, calcium channel blockers, and others (α-blockers, vasodilators, methyldopa, clonidine, and mineralocorticoid receptor antagonists). Patients using fixed-dose combination products were classified as receiving AHDs in each of the classes. Patients were also classified into one of the following groups depending on the number of AHD classes they received at the start of telmisartan therapy: no other AHD (telmisartan monotherapy), telmisartan + 1 AHD, telmisartan + 2 AHDs, and telmisartan + 3 AHDs.
Statistical Analysis
All study variables were summarized using descriptive statistics. Frequency and percentages were reported for categorical variables, while means and standard deviations were reported for continuous variables. Changes in continuous variables were reported as mean change with 95% confidence intervals (CI). P values were calculated using the Altman and Bland method [21], and P < 0.05 was considered statistically significant.
Results
Baseline characteristics
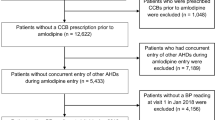
Among the 1304 patients who met the inclusion criteria and were included in the study (Fig. 1), 1181 (90.6%) were prescribed telmisartan as monotherapy or along with one other AHD. Patients on telmisartan monotherapy were the youngest (mean ± SD age 53.2 ± 12.0 years), while those on telmisartan + 3 AHDs were the oldest (mean ± SD age 62.9 ± 10.9 years). The latter group also had the highest proportion of women (56.0%). The highest proportion of diabetes mellitus was reported by patients on telmisartan monotherapy (61.6%). On the other hand, patients on telmisartan + 3 AHDs reported the highest proportion of cardiovascular events (28.6%) and CKD (14.3%). The majority of patients on telmisartan monotherapy were treatment-naïve (92.6%). Grade 1 hypertension was usually more common than other grades across the groups. A majority of the patients in each group were prescribed a 40 mg dose of telmisartan (56.0–67.3%). The average duration between visits 1 and 2 was 99.8 days, 102.0 days, 103.9 days, and 69.2 days for patients on telmisartan monotherapy, telmisartan + 1 AHD, telmisartan + 2 AHDs, and telmisartan + 3 AHDs, respectively (Table 1).
Primary endpoint
All the treatment regimens reduced SBP and DBP in the overall cohort (Table 2). The greatest change in SBP and DBP was observed in patients on telmisartan monotherapy (mean [95% CI] −13.3 [−14.6, −12.0] mmHg; P < 0.001) and telmisartan + 3 AHDs (−8.8 [−12.5, −5.1] mmHg; P < 0.01), respectively (Fig. 2).
Telmisartan-induced change in blood pressure. Mean (95% confidence interval) change in blood pressure from visit 1 to visit 2 is shown. The error bars represent the 95% confidence interval. Visit 2 readings were statistically compared against visit 1 readings. **P < 0.01 and ***P < 0.001. AHD antihypertensive drug, DBP diastolic blood pressure, SBP systolic blood pressure, TELM telmisartan
Among patients with essential hypertension and comorbid diabetes, the greatest change in SBP (mean [95% CI] −13.3 [−15.0, −11.6] mmHg; P < 0.001) and DBP (−7.3 [−8.2, −6.5] mmHg; P < 0.001) was observed in patients on telmisartan monotherapy. Among patients with essential hypertension and comorbid dyslipidemia, the greatest change in SBP (mean [95% CI] −12.5 [−14.9, −10.1] mmHg; P < 0.001) and DBP (−8.8 [−11.3, −6.3] mmHg; P < 0.001) was observed in patients on telmisartan monotherapy and telmisartan + 2 AHDs, respectively. As only a few patients with comorbid CKD or CAD were present in each therapeutic group, we have presented the overall results instead of group-wise data. Among patients with essential hypertension and CKD (n = 15), telmisartan initiation reduced mean (SD) SBP from 158.8 (12.6) to 156.2 (21.1) mmHg (mean [95% CI] change in SBP −2.6 [– 13.0, 7.8] mmHg) and mean (SD) DBP from 94.0 (5.9) to 90.3 (7.6) mmHg (mean [95% CI] change in DBP −3.6 [– 8.7, 1.5] mmHg). Among patients with essential hypertension and CAD (n = 55), telmisartan initiation reduced mean (SD) SBP from 163.3 (15.5) to 143.3 (19.1) mmHg (mean [95% CI] change in SBP −20.0 [– 25.5, −14.5] mmHg) and mean (SD) DBP from 94.5 (6.0) to 84.1 (9.9) mmHg (mean [95% CI] change in DBP −10.4 [−13.1, −7.7] mmHg) (Table 3). Data for patients with stroke were minimal and hence are not presented.
Patients were classified according to age into three subgroups: ≤ 45 years, < 65 years, and ≥ 65 years. In the ≤ 45 years subgroup, the greatest statistically significant change in SBP (mean [95% CI] −12.7 [−15.1, −10.3] mmHg; P < 0.001) and DBP (−7.0 [−8.5, −5.5] mmHg) was observed in patients on telmisartan monotherapy. In the < 65 years subgroup, the greatest change in SBP (mean [95% CI] −12.7 [−17.6, −7.8] mmHg; P < 0.001) and DBP (−8.4 [−11.1, −5.7] mmHg; P < 0.001) was observed in patients on telmisartan + 2 AHDs. In the ≥ 65 years subgroup, the greatest change in SBP (mean [95% CI] −16.2 [−19.4, −13.0] mmHg; P < 0.001) and DBP (−12.2 [−16.9, −7.5] mmHg; P < 0.001) was observed in patients on telmisartan monotherapy and telmisartan + 3 AHDs, respectively (Online Resource 1).
Among male patients with essential hypertension, the greatest change in SBP (mean [95% CI] −12.5 [−14.3, −10.7] mmHg; P < 0.001) and DBP (−7.4 [−10.2, −4.6] mmHg; P < 0.001) was observed in patients on telmisartan monotherapy and telmisartan + 2 AHDs, respectively. Similarly, among female patients with essential hypertension, the greatest statistically significant change in SBP (mean [95% CI] −14.2 [−16.2, −12.2] mmHg; P < 0.001) and DBP (−7.4 [−10.8, −4.0] mmHg; P < 0.05) was observed in patients on telmisartan monotherapy and telmisartan + 2 AHDs, respectively (Online Resource 1).
Secondary Endpoint
Overall, 35.5% and 47.8% of the patients achieved their SBP and DBP goals, respectively, according to the ESC/ESH 2018 guidelines. Group-wise, the highest proportion of patients who achieved their SBP goals were on telmisartan monotherapy and telmisartan + 1 AHD (both 35.9%) and the highest proportion of DBP goal achievers were on telmisartan + 3 AHDs (56.0%), respectively (Fig. 3).
Proportion of patients with essential hypertension who achieved individualized blood pressure goals after therapy with telmisartan according to ESC/ESH 2018 guidelines. SBP target was < 140 mmHg and DBP target was < 90 mmHg. AHD antihypertensive drug, DBP diastolic blood pressure, ESC/ESH European Society of Cardiology/European Society of Hypertension, SBP systolic blood pressure
Among patients with comorbid diabetes, 30.5% achieved their SBP goal and 40.4% achieved their DBP goal according to the ESC/ESH 2018 guidelines. Group-wise, patients on telmisartan + 1 AHD were most successful in achieving the SBP goal (31.9%), and patients on telmisartan + 2 AHDs were most successful in achieving the DBP goal (50.0%) (Fig. 4). Among patients with comorbid dyslipidemia, 35.2% achieved their SBP goal and 53.5% achieved their DBP goal. Group-wise, patients on telmisartan + 1 AHD were most successful in achieving the SBP goal (39.7%), and patients on telmisartan + 2 AHDs were most successful in achieving the DBP goal (59.2%) (Fig. 5). As only a few patients with comorbid CKD or CAD were present in each therapeutic group, we have presented the overall results instead of group-wise data. Among patients with comorbid CKD, 13.3% of the patients achieved the SBP goal and 40.0% of the patients achieved the DBP goal; among patients with comorbid CAD, 43.6% of the patients achieved the SBP goal and 61.8% of the patients achieved the DBP goal according to the ESC/ESH 2018 guidelines. Data for patients with comorbid stroke were minimal and hence are not presented.
Proportion of patients with essential hypertension and diabetes who achieved individualized blood pressure goals after therapy with telmisartan according to ESC/ESH 2018 guidelines. SBP target was ≤ 130 mmHg and DBP target was ≤ 80 mmHg. AHD antihypertensive drug, DBP diastolic blood pressure, ESC/ESH European Society of Cardiology/European Society of Hypertension, SBP systolic blood pressure
In patients aged ≤ 45 years, patients on telmisartan + 3 AHDs were most successful in achieving the SBP goal (50.0%), while patients on telmisartan + 2 AHDs and telmisartan + 3 AHDs were most successful in achieving the DBP goal (both 50.0%). In patients aged ≥ 65 years, the highest proportion of patients achieving SBP goals was observed in the telmisartan + 1 AHD group (36.9%), and the highest proportion of DBP goal achievers was observed in the telmisartan + 3 AHDs group (27.3%) (Online Resource 2).
Discussion
Telmisartan has been reported to have high affinity for angiotensin II type 1 receptor [22], high lipophilicity and tissue distribution [22], and a long half-life (24 h) [23], thus providing long-lasting antihypertensive effects. Commonly observed side effects include headache, dizziness, malaise/fatigue, cough, musculoskeletal pain, nausea, bronchitis, tachycardia, and sleep disorders [24, 25].
The current study is one of the first in India to evaluate the effectiveness of an AHD using EMR data. The study provides updated evidence regarding the effectiveness of telmisartan among Indian patients with essential hypertension in a real-world setting. The major advantages of the current study compared with previous studies within India are its large sample size and coverage of physicians throughout the nation, thus increasing generalizability. In the current study, the majority of patients with hypertension (90.6%) were prescribed telmisartan as monotherapy or in combination with one additional AHD. However, the current study did not analyze specific AHDs or classes that were prescribed in combination with telmisartan. Usage of telmisartan as mono- or add-on therapy decreased overall mean SBP and DBP by 11.6 mmHg and 7.5 mmHg, respectively. As the availability of studies that used electronic medical records or databases to evaluate the effectiveness of telmisartan in patients with hypertension were limited, we could not compare the current study’s results with others.
The 2019 IGH-IV guidelines recommend telmisartan as one of the drugs of choice to treat hypertension in patients with comorbid diabetes and metabolic syndrome [10]. This recommendation is supported by previous evidence of the efficacy and safety of telmisartan in these populations. Multiple studies have reported that telmisartan monotherapy or in combination with other AHDs significantly reduces and normalizes BP in adults with hypertension and comorbid diabetes and/or metabolic syndrome [26,27,28,29]. Moreover, a recent meta-analysis reported that telmisartan was superior to other ARBs in improving insulin resistance and reducing fasting blood glucose and insulin levels [30], probably due to the pleiotropic effects of telmisartan on the peroxisome proliferator-activated receptor γ [31]. Other benefits of usage of telmisartan as mono- or combination therapy include improvement of lipid levels [27, 29], visceral fat reduction [32], and improvement in proteinuria/albuminuria or prevention of progression of proteinuria/albuminuria [33]. The aforementioned studies suggest that telmisartan is a good candidate for managing hypertension in patients with comorbid conditions such as diabetes, metabolic syndrome, dyslipidemia, or renal disease.
Limitations
The retrospective design of the study is a major limitation. Second, the sample size in a few subgroups was quite small due to the stringent inclusion criteria. However, larger sample sizes can be incorporated in future studies to validate the findings obtained in the current study. BP was measured at various centers using different methods instead of a uniform protocol, which may have caused variation in the measurements. Unlike clinical trials, wherein drug administration is conducted under medical supervision, patients were responsible for administering the prescribed medication themselves at the specified time. Therefore, it is possible that a few patients may have not adhered to the given prescription, resulting in a low therapeutic effect. Also, it is possible that the effect of telmisartan on some parameters were not evident due to the short duration between visits 1 and 2 (≥ 30 days). In the combination groups (i.e. telmisartan + other AHDs), the use of different AHDs may have differing effects on BP reduction. However, we did not perform matching across these groups to adjust for this effect. Finally, as the objective was to evaluate only the effectiveness of telmisartan, we did not assess the safety and tolerability of telmisartan in the study. Also, the EMR database does not capture adverse events or clinical outcomes such as mortality, hospitalization, and cardiovascular outcomes.
Conclusion
This study is one of the first EMR-based studies conducted in India that reports the effectiveness of telmisartan, either as monotherapy or in combination with other AHDs, in reducing SBP and DBP in Indian patients with essential hypertension. We observed that telmisartan prescribed as mono- or add-on therapy during routine clinical practice significantly reduced blood pressure in Indian patients with mild to moderate hypertension and comorbid diabetes or dyslipidemia as well. These results suggest that telmisartan may be a good candidate for controlling BP in Indian patients with essential hypertension and comorbidities.
References
Kjeldsen SE. Hypertension and cardiovascular risk: general aspects. Pharmacol Res. 2018;129:95–9.
Ramakrishnan S, Zachariah G, Gupta K, Shivkumar Rao J, Mohanan PP, Venugopal K, et al. Prevalence of hypertension among Indian adults: results from the great India blood pressure survey. Indian Heart J. 2019;71:309–13.
Gheorghe A, Griffiths U, Murphy A, Legido-Quigley H, Lamptey P, Perel P. The economic burden of cardiovascular disease and hypertension in low- and middle-income countries: a systematic review. BMC Public Health. 2018;18:975.
Paramore LC, Halpern MT, Lapuerta P, Hurley JS, Frost FJ, Fairchild DG, et al. Impact of poorly controlled hypertension on healthcare resource utilization and cost. Am J Manag Care. 2001;7:389–98.
Anchala R, Kannuri NK, Pant H, Khan H, Franco OH, Di Angelantonio E, et al. Hypertension in India: a systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hypertens. 2014;32:1170–7.
Prenissl J, Manne-Goehler J, Jaacks LM, Prabhakaran D, Awasthi A, Bischops AC, et al. Hypertension screening, awareness, treatment, and control in India: A nationally representative cross-sectional study among individuals aged 15 to 49 years. PLoS Med. 2019;16:e1002801.
James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507–20.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:1269–324.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104.
AoPo I. Indian guidelines on hypertension-IV 2019. J Assoc Physicians India. 2019;67:8–46.
Ramakrishnan S, Ingole S, Dey A, Jain R. Management of hypertension: Insights into prescribing behavior with focus on angiotensin receptor blockers. J Pract Cardiovasc Sci. 2017;3:22–7.
Gupta R, Malhotra A, Malhotra P. Study of prescribing pattern of drugs used in the treatment of hypertension in a tertiary care teaching hospital in North India: an observational study Int J Res. Med Sci. 2018;6:2380–4.
Cidda M, Mateti UV, Batchu MK, Martha S. Study of prescribing patterns of antihypertensives in South Indian population. Int J Basic Clin Pharmacol. 2014;3:303–7.
Beg MA, Dutta S, Varma A, Kant R, Bawa S, Anjoom M, et al. A study on drug prescribing pattern in hypertensive patients in a tertiary care teaching hospital at Dehradun. Uttarakhand Int J Med Sci Public Health. 2014;3:922–6.
Romday R, Gupta AK, Bhambani P. An assessment of antihypertensive drug prescription patterns and adherence to joint national committee-8 hypertension treatment guidelines among hypertensive patients attending a tertiary care teaching hospital. Int J Res Med Sci. 2016;4:5125–33.
Patta S. Drug utilization pattern of antihypertensives in geriatric and non-geriatric population in a tertiary care Government Hospital Srikakulum, A.P. J Evol Med Dental Sci. 2015;4:2101–6.
Kalikar M, Nivangune KS, Dakhale GN, Bajait CS, Sontakke SD, Motghare VM, et al. Efficacy and tolerability of olmesartan, telmisartan, and losartan in patients of stage i hypertension: a randomized. Open-label Study J Pharmacol Pharmacother. 2017;8:106–11.
Gore PN, Badar VA, Hardas MM, Bansode VJ. Comparative effect of telmisartan vs lisinopril on blood pressure in patients of metabolic syndrome. Endocr Metab Immune Disord Drug Targets. 2015;15:64–70.
Gadge P, Gadge R, Paralkar N, Jain P, Tanna V. Effect of telmisartan on blood pressure in patients of type 2 diabetes with or without complications. Perspect Clin Res. 2018;9:155–60.
Arif AF, Kadam GG, Joshi C. Treatment of hypertension: postmarketing surveillance study results of telmisartan monotherapy, fixed dose combination of telmisartan + hydrochlorothiazide/amlodipine. J Indian Med Assoc. 2009;107:730–3.
Altman DG, Bland JM. How to obtain the P value from a confidence interval. BMJ. 2011;343:d2304.
Burnier M. Telmisartan: a different angiotensin II receptor blocker protecting a different population? J Int Med Res. 2009;37:1662–79.
Abraham HM, White CM, White WB. The comparative efficacy and safety of the angiotensin receptor blockers in the management of hypertension and other cardiovascular diseases. Drug Saf. 2015;38:33–54.
Ingino C, Farsang C, Laucevicius A, Bergovec M. An open-label study investigating the efficacy and safety of 12–96 weeks of telmisartan treatment in patients with hypertension. J Int Med Res. 2003;31:561–74.
Michel MC, Bohner H, Koster J, Schafers R, Heemann U. Safety of telmisartan in patients with arterial hypertension: an open-label observational study. Drug Saf. 2004;27:335–44.
Farsky S, Striskova A, Borcin M. Hypertension treatment in patients with metabolic syndrome and/or type 2 diabetes mellitus: analysis of the therapy effectivity and the therapeutic inertia in outpatient study. Cardiol Res Pract. 2018;2018:8387613.
Derosa G, Cicero AF, Bertone G, Piccinni MN, Fogari E, Ciccarelli L, et al. Comparison of the effects of telmisartan and nifedipine gastrointestinal therapeutic system on blood pressure control, glucose metabolism, and the lipid profile in patients with type 2 diabetes mellitus and mild hypertension: a 12-month, randomized, double-blind study. Clin Ther. 2004;26:1228–36.
Faruqui AA. Evaluation of safety and efficacy of telmisartan-amlodipine combination in treating hypertension. J Indian Med Assoc. 2008;106(612–4):624.
Oh GC, Han JK, Han KH, Hyon MS, Doh JH, Kim MH, et al. Efficacy and safety of fixed-dose combination therapy with telmisartan and rosuvastatin in korean patients with hypertension and dyslipidemia: TELSTA-YU (TELmisartan-rosuvaSTAtin from YUhan), a Multicenter, Randomized, 4-arm, Double-blind, Placebo-controlled, Phase III Study. Clin Ther. 2018;40(676–691):e1.
Wang Y, Qiao S, Han DW, Rong XR, Wang YX, Xue JJ, et al. Telmisartan improves insulin resistance: a meta-analysis. Am J Ther. 2018;25:e642–51.
Benson SC, Pershadsingh HA, Ho CI, Chittiboyina A, Desai P, Pravenec M, et al. Identification of telmisartan as a unique angiotensin II receptor antagonist with selective PPARgamma-modulating activity. Hypertension. 2004;43:993–1002.
Choi GJ, Kim HM, Kang H, Kim J. Effects of telmisartan on fat distribution: a meta-analysis of randomized controlled trials. Curr Med Res Opin. 2016;32:1303–9.
Takagi H, Yamamoto H, Iwata K, Goto SN, Umemoto T, Group A. Effects of telmisartan on proteinuria or albuminuria: a meta-analysis of randomized trials. Int J Cardiol. 2013;167:1443–9.
Acknowledgments
Funding
Conductance of this study and the journal’s Rapid Service Fee was funded by Dr. Reddy’s Laboratories.
Medical Writing Assistance
The authors thank Leo J. Philip Tharappel (SIRO Clinpharm Pvt Ltd.) for providing medical writing assistance. This assistance was funded by Dr. Reddy’s Laboratories.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
Mohammed Yunus Khan, Sucheta Pandit, Amey Mane, and Snehal Shah developed the concept and performed the study. Snehal Shah performed data analysis. Mohammed Yunus Khan and Sucheta Pandit drafted the manuscript. Mohammed Yunus Khan, Sucheta Pandit, Jabir Abdulkutty, Girish Navasundi, Prakash Kumar Hazra, Uday Phadke, Amey Mane, Suyog Mehta, and Snehal Shah reviewed the manuscript and gave final approval.
Disclosures
Mohammed Yunus Khan, Sucheta Pandit, Amey Mane, and Suyog Mehta are employees of Dr. Reddy’s Laboratories and may own stock. Snehal Shah is an employee of Healthplix Ltd, which received consultancy fees from Dr. Reddy’s Laboratories to perform the study. Jabir Abdulkutty, Girish Navasundi, Prakash Kumar Hazra, and Uday Phadke are members of the advisory board for Dr. Reddy’s Laboratories.
Compliance with Ethics Guidelines
The study protocol was approved by an independent ethics committee (Suraksha – Ethics Committee, Asian Institute of Medical Sciences [AIIMS], Dombivli, Maharashtra, India) on 03 December, 2019. Patient confidentiality was maintained at all times, as the study was performed using anonymized information only.
Data Availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Suyog Mehta was an employee of Dr. Reddy’s Laboratories when the study was conducted
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Khan, M.Y., Pandit, S., Abdulkutty, J. et al. Effectiveness of Telmisartan on Blood Pressure Control in Hypertensive Patients in India: A Real-World Retrospective Study from Electronic Medical Records. Cardiol Ther 10, 255–269 (2021). https://doi.org/10.1007/s40119-021-00217-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40119-021-00217-7