Abstract
The Edwards SAPIEN™ transcatheter heart valve (Edwards Lifesciences LLC, Irvine, CA, USA) is approved by the US Food and drug administration for use in the aortic position in patients with severe aortic stenosis who are not surgical candidates. This approval was backed by data from the Placement of AoRTic TraNscathetER Valve (PARTNER) I clinical trial, which showed the valve to be superior to standard medical therapy in high-risk nonoperative patients in cohort B of the trial. Although insertion of the valve is considered to be very safe, stroke, major vascular complications, and conduction abnormalities are the most frequent procedural complications. A dedicated team of physicians trained in structural cardiac interventions, including two interventional cardiologists, an echocardiographer, and a cardiac surgeon, are involved in every case. Improvements in valve design and streamlining of the delivery system, as well as favorable long-term outcomes, will hopefully pave the way for wider patient use in the future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
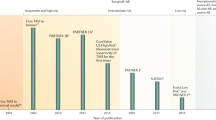
The concept of transcatheter insertion of heart valves as a treatment option for valvular heart disease has been around since the 1960s [1]. In the 1990s, transcatheter implantation of aortic valves in pig models was described [2], but it was not until 2000 that Bonhoeffer et al. [3] described the first implantation of a transcatheter pulmonic valve in a human being. The valve was comprised of a fresh bovine jugular vein, containing a native biological valve that was attached to a platinum stent. It was implanted in a 12-year-old boy with pulmonic stenosis and a degenerated right ventricle (RV) to pulmonary artery (PA) conduit with RV dysfunction. 2 years following this report, Cribier et al. [4] described the first percutaneous transcatheter implantation of an aortic valve prosthesis in a 57-year-old patient with calcific aortic stenosis. This valve consisted of three equine pericardial leaflets mounted within a tubular, slotted, stainless steel balloon-expandable stent, designed to achieve a diameter of 21–22 mm. This aortic valve model was the predecessor of the Edwards SAPIEN™ transcatheter heart valve (THV) (Edwards Lifesciences). Over the next decade, the field of transcatheter valve replacement skyrocketed with multiple large-scale randomized trials, which ultimately lead to the Edwards SAPIEN THV being the first percutaneous valve approved by the US food and drug administration (FDA) for inoperable patients with calcific aortic valve stenosis [5]. In this paper, the authors review the history and specifications of the valve, procedural steps for transfemoral insertion of the valve, and detailed results of the Placement of AoRTic TraNscathetER Valve (PARTNER) I trial.
Calcific Aortic Stenosis
Calcific aortic stenosis is a common disease process that is estimated to affect 8–12% of patients over the age of 75 years [6]. It is a progressive disease, and once symptoms develop, deterioration can be quite rapid with a high-level of morbidity and mortality. In symptomatic patients, if left untreated, the 2-year mortality approaches 50% [7, 8].
Fortunately, in the right patient, surgical aortic valve replacement (AVR) is an excellent option, which leads to symptom resolution and improved mortality [9, 10]. In patients with little or no comorbid conditions, surgery is quite safe and is associated with low operative mortality [11]. However, for a large proportion of patients with severe aortic stenosis (30%), due to multiple comorbid conditions, surgery is not an option [12, 13].
Transcatheter AVR
Transcatheter AVR (TAVR) was first introduced by Cribier et al. [4] in 2002 with the aim of offering an alternative treatment option for patients with severe symptomatic aortic stenosis who were at high-risk for surgical AVR [14]. Over the last 10 years since its conception, the technique and the devices available have rapidly evolved [15, 16]. Currently, over 50,000 patients have undergone TAVR worldwide [17], with at least 25,000 of those performed using the Edwards SAPIEN THV.
The Edwards SAPIEN THV
The Edwards SAPIEN THV is made up of three equal-sized bovine pericardial leaflets that are hand-sewn to a stainless steel, balloon-expandable stent (Fig. 1a1, a2). A polyethylene terephthalate (PET) fabric cuff covers the lower portion of the stent to enable a seal with the calcified valve, hoping to prevent paravalvular leak. The leaflet material has been designed to reduce leaflet stress and maximize coaptation. The pericardial tissue is processed with the ThermaFix® Process (Edwards Lifesciences LLC) anticalcification treatment that is utilized in the Carpentier-Edwards PERIMOUNT Magna™ (Edwards Lifesciences LLC) surgical valve. The Edwards SAPIEN THV is available in a diameter of 23 mm (for use in native valves with an annulus between 18 mm and 22 mm), 26 mm (for use in native valves with an annulus between 21 mm and 25 mm), and outside the US a 29 mm valve is available (for use in native valves with an annulus between 25 mm and 27 mm). The height of these valves varies between 14 mm and 19 mm. The 23 mm valve requires a 22 French (Fr.) sheath for delivery and the 26 mm valve requires a 24 Fr. sheath. The valve is manually compressed over the delivery balloon using a crimping tool to symmetrically reduce the valve diameter so it can be placed through the introducer sheath (Fig. 2).
The Edwards SAPIEN transcatheter heart valve and RetroFlex 3 transfemoral system. The valve (a1 and a2) is available in 23 mm or 26 mm diameter. It consists of three equal-sized bovine pericardial cusps mounted into a stainless-steel balloon expandable stent. The RetroFlex 3 delivery system has a tapered steerable tip (b), which facilitates valve crossing (white arrow indicates the location of the valve on the catheter). The handle of the RetroFlex 3 catheter (c) has a knob (white arrow) to steer the tip of the catheter during aortic arch crossing
The Edwards SAPIEN transcatheter heart valve being crimped on the balloon using a crimping tool. a Stent/valve on delivery balloon. The blue/green suture line on the valve (arrow) should be pointing towards the yellow tip for delivery in the aortic position. b The valve being crimped using the crimping tool (arrow). c Valve (arrow) crimped on the delivery balloon, and covered with the introducer/loader (d) to prevent damage to the valve when advancing it through the sheath
The Edwards SAPIEN THV was approved by the FDA in November 2011 for use in patients with severe symptomatic calcific aortic stenosis who are not surgical candidates [5].
The main competitor of the Edwards SAPIEN THV is the CoreValve® (Medtronic, Inc., Minneapolis, MN, USA). It consists of a self-expandable nitinol stent with porcine pericardial leaflets. The CoreValve is widely used internationally but is still undergoing clinical trials in the US and results are expected to be published in 2013. Table 1 outlines the main differences between the Edwards SAPIEN THV and the CoreValve [17].
There are multiple other valves that are under investigation domestically and internationally with the hope that clinical trials will start in the US and internationally in the near future.
In the US, the delivery system that is currently available for the Edwards SAPIEN THV through the transfemoral approach is the RetroFlex 3™ Transfemoral System (Edwards Lifesciences LLC; Fig. 1b, c). It has a distal cone tip, which helps in advancing the THV across tortuous vessels, reducing friction at the level of the aortic arch, and crossing the native calcified valve. The handle of the delivery system includes a rotating wheel for articulation of the flex catheter.
The newer model of the Edwards SAPIEN THV, the Edwards SAPIEN XT THV (Edwards Lifesciences LLC; Fig. 3a1, a2), is mounted on a cobalt-chromium alloy frame and has several advantages over its predecessors. Perhaps most importantly, it has a lower profile (16 Fr. for the 23 mm valve and 19 Fr. for the 26 mm valve), allowing for implantation in patients with smaller vessels and reducing the risk of vascular injury. This valve along with its newer delivery system, the NovaFlex+™ transfemoral system (Edwards Lifesciences LLC; Fig. 3b, c), is widely used internationally but is currently only available in the US through the PARTNER II clinical trial.
The Edwards SAPIEN XT transcatheter heart valve and NovaFlex + transfemoral system. The valve (a1 and a2) is available in 23 mm or 26 mm in the US, and 29 mm internationally. It consists of three bovine pericardial cusps mounted into a cobalt-chromium balloon expandable stent. b The NovaFlex delivery system has a much smaller tapered yellow tip (white arrow), which facilitates crossing the aortic valve; the black indicates valve position on the catheter when crimped. c1 The handle of the NovaFlex has a large front knob 1 to steer the tip of the catheter. The catheter is advanced inside the sheath where the tip of the catheter is at the crimped valve over the shaft. Once the catheter is in the thoracic/abdominal aorta the locking button 2 is pushed and the balloon catheter is retracted so that the valve straddles the markers on the balloon. Once it is close, then fine adjustments can be made using the back knob 3 until the valve is between the two markers on the balloon. c2 Prior to balloon inflation, one should push the button (arrow) and pull the catheter back off the balloon until it is completely away from the balloon
Patient Selection
Careful patient selection is critically important to ensure a successful procedure. The authors typically use the inclusion and exclusion criteria for the PARTNER I trial, as described in the clinical data section of this paper. As the Edwards SAPIEN THV is only approved for patients who are not surgical candidates, the authors make sure that each patient is thoroughly evaluated by a team of physicians, including a cardiac surgeon, an interventionalist, and a general cardiologist, prior to receiving a commercial TAVR. Two of the most important factors in deciding TAVR eligibility are the femoral vessel diameters and the aortic valve annulus by echocardiography or computed tomography (CT) angiography. Prior to TAVR, each patient has their femoral/iliac vessels evaluated by two methods: conventional angiography and CT angiography of the chest, thorax, abdomen, and pelvis. The minimal vessel diameter required for sheath insertion in the transfemoral approach is 7 mm for the 22 Fr. sheath and 8 mm for the 24 Fr. sheath in the absence of calcification. Vessel tortuosity should not be considered a contraindication for the transfemoral approach as long as the arteries straighten out during the insertion of a stiff guidewire. Patients with small, heavily calcified arteries should undergo placement of the valve through a transapical approach or via a surgical conduit (proximal to the narrowest diameter of the vessel or calcification) in order to prevent vascular complications. The aortic annulus diameter is measured by gated CT angiogram, and by transthoracic echocardiogram and transesophageal echocardiogram (TEE) during the procedure. Most interventionalists rely on TEE to choose the appropriately sized valve. Currently, in the US, patients with an annulus less than 18 mm or greater than 25 mm are not candidates for TAVR.
Procedural Steps
Patient Setup
The authors prefer to perform the procedures in the hybrid catheterization laboratory using monoplane fluoroscopy under general endotracheal anesthesia. However, it is also possible to perform TAVR under deep sedation if endotracheal intubation is contraindicated, such as in cases of severe end-stage lung disease. Given how sick these patients are, it is recommended that hemodynamic monitoring is performed throughout the procedure, including a dedicated arterial line for blood pressure monitoring and a triple lumen central venous catheter. The team performing the procedure consists of two interventional cardiologists, one cardiothoracic surgeon, and an echocardiographer. In addition, because of the potential risk of complications requiring emergent surgery, the patient’s chest is prepped in a surgical sterile-fashion (from supra sternal notch to the knees), and the authors have a surgical team of nurses and technicians, and cardiopulmonary bypass available in the room in case of emergency. Once the patient is intubated, the authors obtain an accurate aortic valve annulus measurement (Fig. 4a) to confirm that the annulus is appropriate for the available valves. In one instance, the authors encountered a patient where the TEE measurement in the lab was 27 mm, which was not appropriate for the largest available valve, 26 mm, and the procedure was abandoned.
Transesophageal views of the Edwards SAPIEN transcatheter heart valve being deployed. a Annulus measurement from leaflet insertion points. b Valve on delivery balloon across the valve in a 50:50 ratio (50% ventricular to 50% aortic). c Valve leaflets following deployment by transesophageal echocardiography. d Evidence of mild paravalvular leak by transesophageal echocardiography
Arterial Access
Because of the large caliber of the arterial sheaths, vascular access and closure are the most critical steps of the entire TAVR procedure. The femoral artery is the preferred site of insertion, and is the approved delivery method for the Edwards SAPIEN THV. Although a surgical cut-down was initially required to insert the large arterial sheaths, most centers are now performing percutaneous access. The device has also been inserted through various other routes, including through a transapical approach (as part of the PARTNER I trial), transaxillary, and an open surgical retroperitoneal approach in patients whose femoral vessels are too small to accommodate the large arterial sheath. Failure to obtain proper arterial access can lead to major bleeding complications. The authors always use a fluoroscopic-guided technique for arterial access. The authors first obtain arterial (6 Fr.) and venous (7 Fr.) access on the contralateral side. Once adequate arterial access is obtained on the contralateral side, abdominal aortography [at the bifurcation of the aorta to the common iliacs (Fig. 5a)] is performed in order to evaluate the location of the common femoral bifurcation. The authors then use fluoroscopic guidance to obtain arterial access on the side through which the authors plan to insert the valve. The authors typically start with an 8 Fr. sheath, and “preclose” the vessel with two Perclose® ProGlide™ 6F Suture-Medicated Closure System (Abbot Laboratories, Abbott Park, IL, USA), one at the 10 o’clock position and the other one at 2 o’clock position, that remain in place during the procedure and are used to achieve hemostasis at the end of the case. The authors reasoning for choosing the Perclose ProGlide instead of the Prostar® XL Percutaneous Vascular Surgical System (Abbott Vascular, Santa Clara, CA, USA) is the cost difference between these two devices and the ease of use.
Step-wise angiographic images of the Edwards SAPIEN transcatheter heart valve being deployed. a Abdominal aortogram with arrows pointing to the external iliac vessels. b Aortic root angiogram in left anterior oblique 10°/cranial 10° projection, demonstrating all three aortic cusps (white arrows). c Balloon aortic valvuloplasty prior to valve insertion. d Valve being positioned across the aortic annulus (arrow) in a 50:50 ratio (50% aortic to 50% ventricular). e Valve being deployed. f Valve in good position following deployment (arrow). g Aortic root angiography following valve deployment demonstrating no aortic insufficiency. h Flexor Ansell sheath cross-over from the contralateral side with balloon (10 mm × 2 cm; arrow) occluding anterograde flow down the vessel during hemostasis with two Perclose ProGlide sutures
Angiography
An aortic root angiogram is performed in order to have a reference view of the aortic valve and annulus (Fig. 5b). This is usually done in slight left anterior oblique (LAO) (10°) with cranial angulation (10°). It is critical to profile the aortic annular plane perpendicular to the screen with the three aortic cusps in a straight line. This line is used as a landmark for proper valve placement. On occasions, the calcification landmarks do not necessarily indicate the level of annulus. Careful attention must be paid to the location of the coronary ostia in relation to the calcium in the valve as there have been reports of coronary occlusion following valve delivery [18, 19].
Crossing the Valve
After the angiogram has been completed, the next step is to cross the valve. The authors use an AL-1 or AL-2 catheter with a straight soft tip Terumo Glidewire®. (Terumo Medical Corporation, Elkton, MD, USA) The authors have found this combination to work in most cases. The authors often create side holes in the AL catheter so that the authors can record pressure using this catheter. Once the catheter is inside the left ventricle (LV), simultaneous pressure recordings from the LV and ascending aorta are obtained to obtain the gradient across the valve.
The next step is to place a 5 Fr. pacing catheter to the RV apex and to test the pacing thresholds/rate. The authors usually choose a rate of 160–180 beats/min and observe the effect on blood pressure. The authors aim to have the mean aortic pressure drop to about 50 mmHg. Pacing is a crucial step and has to be perfected otherwise the untoward complication of valve migration may occur. The authors usually have one interventionalist in charge of deciding when to pace and when to terminate pacing. The pacing duration should be as brief as possible, but should be terminated upon complete balloon deflation. Some patients with poor LV function may not tolerate rapid pacing for a long period. Rapid RV pacing was first described with balloon aortic valvuloplasty (BAV) in 2001 [20] and has been an integral part of the TAVR procedure [21].
At this point, prior to BAV, the entire team takes a “timeout” to review all the necessary steps/equipment availability in the room in case of an emergency. A nurse who is in charge of the patient calls the timeout and goes over a few points (balloon size to be used, valve size to be used and the crimped orientation of the valve, pacemaker and the set-up, surgical backup, and the equipment required). The next step is the BAV (Fig. 5c). An Amplatz 0.035 inch extra stiff guidewire (Cook Medical, Bloomington, IN, USA) is exchanged and the sheath is also removed. The appropriately sized sheath necessary for valve deployment is now inserted for the valvuloplasty. Some teams may not insert this sheath until they are ready for valve deployment. The authors believe inserting the appropriate sheath at this point is better in case the patient develops severe aortic regurgitation (AR), requiring expedited valve deployment.
Aortic Valvuloplasty
BAV (Fig. 5c) is an important part of the TAVR procedure as it increases the effective orifice area of the aortic valve, and facilitates easier valve/stent passage through the calcified valve and precise placement. The authors prefer to use a Z-MED™ balloon (NuMED, Brooklyn, NY, USA) of the appropriate size, based on the size of the aortic annulus as measured by TEE. In general, for the 23 mm valve, the authors use a 20 mm × 5 cm Z-MED balloon and for the 26 mm valve, the authors use the 23 mm × 5 cm Z-MED balloon. Once valvuloplasty is complete, the balloon catheter is removed and the stiff wire is left in the ventricle in anticipation of valve placement.
Valve Delivery
The valve, which has been crimped on the delivery balloon (Fig. 2b) is covered with the loader before insertion into the arterial sheath (Fig. 2d); this prevents any damage to the stent. The valve is then advanced under fluoroscopic guidance. In the aortic arch, moderate flexion of the RetroFlex 3 system will decrease the friction against the wall and reduce the risk of plaque embolization. Once the stent is across the native valve, the RetroFlex 3 catheter is then withdrawn over the balloon catheter shaft without moving the bioprosthesis. This allows for full expansion of the balloon. At this point, the camera should be moved to the angle that was previously determined to profile the annulus best in order to orient the valve calcium perpendicular to the screen. TEE is helpful to determine whether the prosthesis is centered within the native valve (Fig. 4b), and angiography may be performed through a pigtail catheter from the contralateral artery sitting just above the sinuses (Fig. 5d). The authors aim to have the valve straddle the annulus in 50/50 (50% over the aortic side and 50% ventricular side) ratio. On occasions, the authors hold respiration and pace the ventricle during this crucial angiogram to determine valve position.
Valve Deployment
The valve is deployed with a manual inflation device that is provided with the valve set. The syringe is filled with 15:85 contrast medium to saline solution, the volume of which has been predetermined in order to obtain an optimal valve diameter. Valve deployment must be done with rapid RV pacing and cardiac standstill. The balloon should remain inflated for at least 3 s (Fig. 5e). RV pacing should be initiated before balloon inflation and should be terminated after the balloon is completely deflated. Appropriate valve position is quickly determined by TEE (Fig. 4c) and fluoroscopy (Fig. 5f, g). The presence of paravalvular leak is then evaluated by TEE (Fig. 4d) before the balloon catheter is removed. If there is significant paravalvular leak, re-expansion of the balloon with an additional 1 ml added to the volume in the syringe may reduce it. After the balloon is removed, valve function and position are further evaluated by angiography and TEE. For completeness, hemodynamics (including simultaneous LV and ascending aorta pressures, as well as right-sided pressures) may be recorded at the conclusion of the procedure.
Arterial Hemostasis
As mentioned previously, this is one of the most important steps of the entire procedure. The authors advocate the “preclose” technique where two Perclose ProGlide sutures are placed in the 10 o’clock and 2 o’clock positions at the beginning of the case, and the authors use the cross-over technique [22]. Once the procedure is finished (valve deployed and tested) and it is time for hemostasis, the authors insert an exchange length Terumo Glidewire through the contralateral artery, snare it with a 25 mm Amplatz GooseNeck Snare® (Covidien, Plymouth, MN, USA) and externalize it through the large sheath. The authors then remove the contralateral short sheath while leaving the wire, insert a 5–6 Fr. Flexor® Ansell sheath (Cook Medical) over this wire all the way to the large sheath, and insert the tip of the Ansell sheath into the distal end of the large sheath (Fig. 5h). Through the Ansell sheath, a peripheral balloon catheter (10–12 mm × 2 cm) is inserted over a 0.018 inch wire all the way to the external iliac artery and inflated to prevent distal blood flow. With no flow down the vessel, the previously placed Perclose ProGlide sutures can now be tightened without excessive bleeding. Once the sutures are secured, the balloon is deflated and an angiogram is performed through the Ansell sheath to ensure no dye extravasation. The contralateral artery is then usually closed with a closure device such as an Angio-Seal™ vascular closure device (St. Jude Medical, Saint Paul, MN, USA) or one Perclose ProGlide suture while the vein is either manually compressed, or a figure-eight suture is utilized to achieve hemostasis.
Follow-Up
The patients are generally observed in the coronary care unit for several days to ensure that no vascular complications occur and that the patient fully recovers prior to discharge. The patients are extubated in a timely manner, and early ambulation is encouraged. Three total doses of prophylactic antibiotics (first-generation cephalosporins) are administered, one during the procedure and two at 8-h intervals post-procedure. The patients are started on 81 mg acetylsalicyclic acid daily as well as clopidogrel 75 mg daily. In patients at higher risk for stroke (i.e., patients with atrial fibrillation), the authors administer warfarin with intravenous heparin bridging the day following the procedure if there are no contraindications. The typical hospital course following TAVR is 8 days. Most patients are discharged home and do not require a skilled nursing facility. Prior to discharge, an echocardiogram is performed to evaluate valve function and gradient. These patients are followed-up in the outpatient clinic at 1 month, 6 months, and 12 months, and yearly thereafter.
Clinical Data
The PARTNER I clinical trial was a randomized, multicenter clinical trial comparing TAVR with either medical therapy for those who are inoperable (cohort B) or to surgical AVR in patients who were at high-risk for surgery (cohort A) [23, 24]. The results were very favorable for TAVR and lead to the FDA approval for the Edwards SAPIEN THV in inoperable patients. Inclusion criteria in the PARTNER I trial included severe aortic stenosis (defined as aortic-valve area of less than 0.8 cm2, a mean aortic-valve gradient greater than or equal to 40 mmHg, or a peak aortic-jet velocity greater than or equal to 4 m/s). All patients were required to have New York Heart Association (NYHA) functional class II or greater. As mentioned above, the trial was divided into two cohorts. The first group (cohort A) were considered to be candidates for surgery, albeit at high-risk, which was defined by a Society of Thoracic Surgeons (STS) risk score of 10% or higher [25], or the presence of coexisting conditions that would be associated with a predicted risk of death of 15% or higher at 30 days [23]. The second group (cohort B) comprised of patients who were deemed to be inoperable due to coexisting conditions that would be associated with a predicted risk of 50% or more of death, or irreversible condition at 30 days following surgery. At least two surgeons had to agree that the patient was not a suitable candidate for surgery.
Exclusion criteria for the PARTNER I trial included bicuspid or noncalcific aortic stenosis, acute myocardial infarction, significant coronary artery disease requiring revascularization, LV ejection fraction of less than 20%, aortic valve annular diameter less than 18 mm or greater than 25 mm, severe (greater than 3+) mitral or AR, a transient ischemic attack or stroke in the previous 6 months, or renal insufficiency [23].
Between May 2007 to March 2009, a total of 358 patients with severe aortic stenosis who met the inclusion criteria and were not surgical candidates were enrolled in 21 sites (17 in the US) in PARTNER I cohort B. Patients were randomized to receive either standard medical therapy or TAVR with the Edwards SAPIEN THV (179 patients for each arm). The 1-year mortality in the TAVR group was 30.7% and 49.7% in the medical therapy arm (the 1-year cardiac mortality was 19.6% in the TAVR group and 41.9% in the medical therapy group). At 1 year, the risk of major bleeding, major vascular complications, or stroke were higher in the TAVR group (22.3%, 16.8%, and 7.8%, respectively, in the TAVR group as compared to 11.2%, 2.2%, and 3.9%, respectively, in the medical therapy arm). All values were statistically significant [23]. In the 2-year follow-up of the PARTNER I cohort B study, the mortality benefit continued with 43.3% mortality in the TAVR arm and 68.0% mortality in the medical therapy arm at 2 years [26].
During the same time period, 699 high-risk patients with severe aortic stenosis were randomized to undergo either TAVR or surgical AVR in the PARTNER I cohort A. TAVR was performed either via the transfemoral route using the RetroFlex 3 delivery system or transapically in patients whose femoral vessels were too small to accommodate the RetroFlex 3 system. The study showed that TAVR was noninferior to surgical AVR in this patient population. The rates of death from any cause were 3.4% in the TAVR group and 6.5% in the surgical group at 30 days (P = 0.07), and 24.2% and 26.8%, respectively, at 1 year (P = 0.44). The rates of major stroke were not statistically significant at 30 days but were higher in the TAVR group at 1 year, 5.1% as compared to 2.4% in the surgical group (P = 0.07). At 30 days, major vascular complications were significantly more frequent with transcatheter replacement (11.0% vs. 3.2%); adverse events that were more frequent after surgical replacement included major bleeding (9.3% vs. 19.5%) and new-onset atrial fibrillation (8.6% vs. 16.0%). All values were statistically significant. Although more patients had improvement in their symptoms at 30 days in the TAVR arm, the two groups were found to be comparable at 1 year [24]. The 2-year outcomes of the cohort B patients showed a continued similarity between the two treatment arms with respect to mortality, reduction in symptoms, and improved valve hemodynamics, but increased paravalvular regurgitation in the TAVR arm, which was associated with increased late mortality [27].
The health-related quality of life for the patients in the PARTNER I trial was evaluated at 1 month, 6 months, and 12 months using the Kansas City Cardiomyopathy Questionnaire (KCCQ) and the 12-item Short Form-12 General Health Survey (SF-12). In the cohort B patients, TAVR resulted in significant improvements in health-related quality of life that were maintained for at least 1 year when compared to standard therapy [28]. The same analysis was done on the cohort A patients and it was found that health-related quality of life improved substantially between baseline and 1 year after either TAVR or AVR. TAVR via the transfemoral, but not the transapical route, was associated with a short-term advantage compared with surgery [29].
In addition to the PARTNER I data from the US, there have been multiple reports of large registries from Europe and Canada using the Edwards SAPIEN valve [30–35]. Although these results are not randomized, they offer real-world experience for TAVR performed at high-volume centers using the Edwards SAPIEN valve. The results of some of the major registries, as well as a summary of the PARTNER I results are outlined in Table 2 [24, 26, 30–35].
A recent meta-analysis of 8,536 patients undergoing either surgical AVR or TAVR worldwide (including both Edwards SAPIEN THV and CoreValve) showed TAVR to be as safe as surgery [36]. However, the 30-day mortality for both surgery and TAVR were both higher (8–9%) than that observed in the PARTNER I trial (cohort A 30 day mortality was 3.4%). This may reflect the importance of the collaboration of the highly specialized team of interventional cardiologists, surgeons, and echocardiographers, which was a requirement for the PARTNER I trial. In many centers performing TAVR, especially in Europe, the procedure is performed without a surgeon present, under conscious sedation, and without the guidance of echocardiography, which may contribute to the higher 30-day mortality. This is one of the reasons the authors advocate the continued use of a multidisciplinary team, even when the Edwards SAPIEN valve is being performed commercially, not as part of the PARNTER I trial.
Complications
The TAVR procedure is surrounded by several potential complications, partially because of the high-risk nature of the patient population and partially because of the invasiveness of the procedure itself. Major vascular complications were the most common complication seen in the PARTNER I trial. The risk was 11.0% compared to 3.2% in the surgical AVR arm (PARTNER I cohort A) [24]. However, with increased familiarity with the preclose technique, vascular complications can be virtually eliminated. If the preclose technique is unsuccessful, the cross-over balloon tamponade of anterograde flow will prevent any major bleeding, whilst also having a surgeon available to perform a cut-down and repair the arteriotomy site will expedite hemostasis. Covered stents can also be used; however, when they are inserted at a point of flexion (as in the common femoral artery) they are more prone to fracture. It will be interesting to see the rate of vascular complications in the PARTNER II data now that operators are more familiar with vascular closure techniques.
Stroke is the second most common complication following TAVR. In the PARTNER I cohort A patient population, the risk of stroke in TAVR arm at 30 days was 3.8% compared to 2.1% in the surgical arm (P = 0.2). By 1 year, the risk of stroke in the TAVR arm had gone up to 5.1% compared to only 2.4% in the surgical arm (P = 0.07). Although these values were not found to be statistically significant, the increased rate of stroke in the TAVR group is concerning. In this elderly patient population, the aortic arch is filled with calcium and atherosclerosis, and delivery of the large caliber valve across the arch can easily cause embolization. This issue is currently being addressed by designing smaller devices and delivery sheaths. There are also carotid protection devices that are under development to prevent embolization of debris in the brain.
Paravalvular leak (Fig. 5d) is another important complication of the TAVR procedure. In the 2-year follow-up of the PARTNER I trial, it was seen in 6.9% of the TAVR patients, compared to only 0.9% of the surgical AVR patients (P < 0.001) and was associated with increased mortality [27]. To avoid paravalvular leak, it is important to position the valve centrally in the aortic annulus. The development of new THVs with better cuffs will hopefully improve this problem in the future. It has recently been shown that significant paravalvular leak following TAVR leads to increased morbidity and mortality. The AR index (diastolic blood pressure—LV end-diastolic pressure/systolic blood pressure) can be calculated and is predictive of 1-year mortality. Patients with an AR index <25 had a significantly increased 1-year mortality compared to patients with an AR index>25 (42.3% vs. 14.3%; P < 0.001) [37].
Other complications reported in the PARTNER I trial include endocarditis and need for a permanent pacemaker, which were similar in both the TAVR and surgical groups [24]. Coronary artery occlusion secondary to calcium embolization has been described and can usually be treated with emergent coronary artery stenting [18, 19]. Finally, valve embolization is a very rare but potentially devastating complication described in a few case reports [38]. When possible, the valve should be repositioned in the descending aorta and re-expanded there. If the valve embolizes into the LV, it needs to be removed surgically or transapically.
Current Use
The Edwards SAPIEN THV is currently only FDA-approved for use in patients who satisfy the PARTNER I cohort B criteria, and who are deemed to be inoperable by a cardiac surgeon. Currently in the US, there are strict guidelines enforced by Edwards Lifesciences as to who can implant the Edwards SAPIEN valve. Only centers that were involved in the PARTNER I trial or centers with a high-volume of structural interventions are authorized to perform commercial TAVR. Recently, the American College of Cardiology and the STS recommended restricting TAVR use to regional centers of excellence [39].
It is important to note that the Edwards SAPIEN valve is also being used successfully in the pulmonic position in patients with a history of congenital heart disease and an RV to PA conduit. In 2011, the Congenital Multicenter Trial of Pulmonic Valve Regurgitation Studying the SAPIEN Interventional THV (COMPASSION) demonstrated an effective reduction of RV outflow tract gradient with reduction in clinical symptoms and maintenance of pulmonary valve competence at 6-months follow-up [40].
Future Directions
The future for THV and the Edwards SAPIEN valve is very exciting. The PARTNER II trial is currently underway and, once those results are available, the authors hope that the lower-profile device will be available for commercial use. Also, multiple other aortic valves [Direct Flow Medical® percutaneous aortic valve (Direct Flow Medical Inc., Santa Rosa, CA, USA); Portico™ transcatheter aortic heart valve (St. Jude Medical, Saint Paul, MN, USA); Lotus™ Aortic Valve System (Boston Scientific Corporation, Natick, MA, USA); JenaValve™ (JenaValve Technology, Munich, Germany); Colibri® Heart Valves (Colibri Heart Valve, LLC, Broomfield, CO, USA) etc.,] are currently under development and will hopefully address some of the current difficulties with TAVR, including paravalvular leak and large sheath size. Currently, the Edwards SAPIEN3 valve is in the early stages of testing in Europe. It offers significant improvements on the SAPIEN and SAPIEN XT valves, primarily to reduce paravalvular leak. It is delivered through the 14-Fr. eSheath™ (Edwards Lifesciences LLC), which is Edwards’ expandable sheath. It is designed to reduce the time the access vessel is expanded; thereby, minimizing the risk of vascular trauma.
Another exciting area of potential development for TAVR and the Edwards SAPIEN valve is the possibility of a “valve-in-valve” procedure. Reoperation to replace degenerated surgical valves can be associated with a significant risk of morbidity and mortality. The frame of most bioprostheses can facilitate THV positioning. Smaller diameter valves (19 mm) will not facilitate the delivery of the currently available valves, but in patients with larger valves, a transcatheter valve-in-valve procedure may be a good option [41–43]. A registry is currently being conducted of all valve-in-valve cases and is sponsored by Edwards Lifesciences.
Conclusion
The Edwards SAPIEN TAVR procedure can be performed safely and effectively for treatment of patients with severe symptomatic aortic stenosis. It is currently indicated for use in patients who are considered to be inoperable; however, in the future these indications may be expanded.
References
Davies H. Catheter mounted valve for temporary relief of aortic insufficiency. Lancet. 1965;1:250.
Anderson HR, Knudsen LL, Hasemkam JM. Transluminal implantation of artificial heart valves: description of a new expandable aortic valve and initial result in implantation in closed chest pigs. Eur Heart J. 1992;13:704–8.
Bonhoeffer P, Boudjemline Y, Saliba Z, et al. Percutaneous replacement of pulmonary valve in a right-ventricle to pulmonary-artery prosthetic conduit with valve dysfunction. Lancet. 2000;356:1403–5.
Cribier A, Eltchaninoff H, Bash A, Borenstein N. Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis. Circulation. 2002;106:3006–8.
US Food and Drug Administration. News and Events: News Room: Press Announcement. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm278348.htm (2012). Accessed Oct 4, 2012.
Lindroos M, Kupari M, Heikkila J, Tilvis R. Prevalence of aortic valve abnormalities in the elderly: an echocardiographic study of a random population sample. J Am Coll Cardiol. 1993;21:1220–5.
Ross J Jr, Braunwald E. Aortic stenosis. Circulation. 1968;38:61–7.
Turina J, Hess O, Sepulcri F, Krayenbuehl HP. Spontaneous course of aortic valve disease. Eur Heart J. 1987;8:471–83.
Schwarz F, Baumann P, Manthey J, et al. The effect of aortic valve replacement on survival. Circulation. 1982;66:1105–10.
Lund O. Preoperative risk evaluation and stratification of long-term survival after valve replacement for aortic stenosis: reasons for earlier operative intervention. Circulation. 1990;82:124–39.
O’Brien SM, Shahian DM, Filardo G, et al. The Society of Thoracic Surgeons 2008 cardiac surgery risk models: part 2—isolated valve surgery. Ann Thorac Surg. 2009;88(Suppl. 1):S23–42.
Bouma BJ, van den Brink RBA, van der Meulen JHP, et al. To operate or not on elderly patients with aortic stenosis: the decision and its consequences. Heart. 1999;82:143–8.
Iung B, Cachier A, Baron G, et al. Decision-making in elderly patients with severe aortic stenosis: why are so many denied surgery? Eur Heart J. 2005;26:2714–20.
Cribier A, Litzler PY, Eltchaninoff H, et al. Technique of transcatheter aortic valve implantation with the Edwards-SAPIEN heart valve using the transfemoral approach. Herz. 2009;34:347–56.
Cribier A, Eltchaninoff H, Tron C, et al. Early experience with percutaneous transcatheter implantation of heart valve prosthesis for the treatment of end-stage inoperable patients with calcific aortic stenosis. J Am Coll Cardiol. 2004;43:698–703.
Cribier A, Eltchaninoff H, Tron C, et al. Treatment of calcific aortic stenosis with the percutaneous heart valve: midterm follow-up from the initial feasibility studies: the French experience. J Am Coll Cardiol. 2006;47:1214–23.
Webb JG, Wood DA. Current status of transcatheter aortic valve replacement. J Am Coll Cardiol. 2012;60:483–92.
Gogas BD, Zacharoulis AA, Antoniadis AG. Acute coronary occlusion following TAVI. Catheter Cardiovasc Interv. 2011;77:435–8.
Gurvitch R, Tay EL, Wijesinghe N, et al. Transcatheter aortic valve implantation: lessons from the learning curve of the first 270 high-risk patients. Catheter Cardiovasc Interv. 2011;78:977–84.
Agatiello C, Eltchaninoff H, Tron C, et al. Balloon aortic valvuloplasty in the adult. Immediate results and in-hospital complications in the latest series of 141 consecutive patients at the University Hospital of Rouen (2002–2005) [In French]. Arch Mal Coeur Vaiss. 2006;99:195–200.
Webb JG, Pasupati S, Achtem L, Thompson CR. Rapid pacing to facilitate transcatheter prosthetic heart valve implantation. Catheter Cardiovasc Interv. 2006;68:199–204.
Genereux P, Kodali S, Leon MB, et al. Clinical outcomes using a new crossover balloon occlusion technique for percutaneous closure after transfemoral aoritic valve implantation. Catheter Cardiovasc Interv. 2011;4:861–7.
Leon MD, Smith CR, Mack K, PARTNER trial investigators, et al. Transcatheter aortic valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med. 2010;363:1597–607.
Smith CR, Leon MD, Mack MJ, PARTNER Trial Investigators, et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med. 2011;364:2187.
Shroyer AL, Coombs LP, Peterson ED, Society of Thoracic Surgeons, et al. The Society of Thoracic Surgeons: 30-day operative mortality and morbidity risk models. Ann Thorac Surg. 2003;75:1856–64.
Makkar RR, Fontana GP, Hasan J, PARTNER Trial Investigators, et al. Transcatheter aortic-valve replacement in inoperable severe aortic stenosis. N Engl J Med. 2012;366:1696–704.
Kodali SS, Williams MR, Smith CR, PARTNER Trial Investigators, et al. Two years outcomes after transcatheter of surgical aortic-valve replacement. N Engl J Med. 2012;366:1686–95.
Reynolds MR, Magnuson AR, Lei Y, Placement of Aortic Transcatheter Valves (PARTNER) Investigators, et al. Health-related quality of life after transcatheter aortic valve replacement in inoperable patients with severe aortic stenosis. Circulation. 2011;124:1964–72.
Reynolds MR, Magnuson AR, Lei Y, Placement of Aortic Transcatheter Valves (PARTNER) Investigators, et al. Health-related quality of life after transcatheter or surgical aortic valve replacement in high-risk patients with severe aortic stenosis: results from the PARTNER (Placement of AoRTic TraNscathetER Valve) Trial (Cohort A). J Am Coll Cardiol. 2012;60:548–58.
Rodes-Cabau J, Webb JG, Cheung A, et al. Transcatheter aortic valve implantation for the treatment of severe symptomatic aortic stenosis in patients at very high or prohibitive surgical risk: acute and late outcomes of the multicenter Canadian experience. J Am Coll Cardiol. 2010;55:1080–90.
Thomas M, Schymik G, Walther T, et al. Thirty-day results of the SAPIEN aortic Bioprosthesis European Outcome (SOURCE) Registry: a European registry of transcatheter aortic valve implantation using the Edwards SAPIEN valve. Circulation. 2010;122:62–9.
Bosmans JM, Kefer J, De Bruyne B, Belgian TAVI Registry Participants, et al. Procedural, 30-day and one year outcome following CoreValve or Edwards transcatheter aortic valve implantation: results of the Belgian national registry. Interact Cardiovasc Thorac Surg. 2011;12:762–7.
Moat NE, Ludman P, de Belder MA, et al. Long-term outcomes after transcatheter aortic valve implantation in high-risk patients with severe aortic stenosis: the UK TAVI (United Kingdom Transcatheter Aortic Valve Implantation) Registry. J Am Coll Cardiol. 2011;58:2130–8.
Eltchaninoff H, Prat A, Gilard M, FRANCE Registry Investigators, et al. Transcatheter aortic valve implantation: early results of the FRANCE (FRench Aortic National CoreValve and Edwards) registry. Eur Heart J. 2011;32:191–7.
Gilard M, Eltchaninoff H, Iung B, et al. FRANCE 2 Investigators Registry of transcatheter aortic-valve implantation in high-risk patients. N Engl J Med. 2012;366:1705–15.
Jilaihawi H, Chakravarty T, Weiss RE, Fontana GP, Forrester J, Makkar RR. Meta-analysis of complications in aortic valve replacement: comparison of Medtronic-Corevalve, Edwards-Sapien and surgical aortic valve replacement in 8,536 patients. Catheter Cardiovasc Interv. 2012;80:128–38.
Vasa-Nicotera M, Sinning JM, Chin D, et al. Impact of paravalvular leakage on outcome in patients after transcatheter aortic valve implantation. J Am Coll Cardiol Interv. 2012;5:858–65.
Tay EL, Gurvitch R, Wijeysinghe N, et al. Outcomes of patients after transcatheter aortic valve embolization. JACC Cardiovasc Interv. 2011;4:228–34.
Holmes DR Jr, Mack MJ. Transcatheter valve therapy: a professional society overview from the American College of Cardiology Foundation and the Society of Thoracic Surgeons. J Am Coll Cardiol. 2011;58:445–55.
Kenny D, Hijazi ZM, Kar S, et al. Percutaneous implantation of the Edwards SAPIEN transcatheter heart valve for conduit failure in the pulmonary position: early phase 1 results from an international multicenter clinical trial. J Am Coll Cardiol. 2011;58:2248–56.
Gurvitch R, Cheung A, Ye J, et al. Transcatheter valve-in-valve implantation for failed surgical bioprosthetic valves. J Am Coll Cardiol. 2011;58:2196–209.
Webb JG, Wood DA, Ye J, et al. Transcatheter valve-in-valve implantation for failed bioprosthetic heart valves. Circulation. 2010;121:1848–57.
Piazza N, Bleiziffer S, Brockmann G, et al. Transcatheter aortic valve implantation for failing surgical aortic bioprosthetic valve: from concept to clinical application and evaluation (part 2). JACC Cardiovasc Interv. 2011;4:733–42.
Acknowledgments
The authors wish to thank Dr. Qi-Ling Cao for his help and for preparation of the figures. Also, the authors wish to thank the entire Hybrid laboratory staff at the Rush Center for Congenital & Structural Heart Disease and the entire valve team at Rush University Medical Center for their commitment to excellence. Dr. Hijazi is the guarantor for this article, and takes responsibility for the integrity of the work as a whole.
Conflict of interest
The authors have no conflict of interest to disclose related to the topic of this article.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Addendum
Since this manuscript was submitted, the US FDA approved the Edwards SAPIEN THV for use in patients who are considered to be at high risk for surgery.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Holoshitz, N., Kavinsky, C.J. & Hijazi, Z.M. The Edwards SAPIEN Transcatheter Heart Valve for Calcific Aortic Stenosis: A Review of the Valve, Procedure, and Current Literature. Cardiol Ther 1, 6 (2012). https://doi.org/10.1007/s40119-012-0006-8
Received:
Published:
DOI: https://doi.org/10.1007/s40119-012-0006-8