Abstract
Asthma is a disease of the airways that is characterized by chronic inflammation and disordered airway function. The purpose of writing the current review paper is to review the history, current situation, control history, challenges, and ongoing management programs of asthma. Some official websites of known respiratory professional bodies were consulted for asthma guidelines, and information from Google Scholar® and PubMed® was also consulted. We reviewed around two hundred eight papers, and then, inclusion and exclusion criteria were applied to prepare this manuscript. Out of these papers, thirty papers, factsheets, and some official websites were used to prepare this manuscript. Physicians should follow already existing asthma guidelines in order to manage asthma. All prescribed medications should be continued. The government should make and adopt more strategies to promote the rational use of anti-asthmatic drugs and healthcare facilities and also make plans to disseminate more awareness among people about the schemes and programs made for safeguarding people against this life-threatening disease. We have done so much advancement to fight against this deadly disease, and we still need time to make the globe asthma-free. The number of people suffering from asthma is more than the number of people suffering from HIV infection and tuberculosis. Understanding the recommendations of professional bodies will assist in medical decision-making in asthma management. The individual needs of patients should be considered by healthcare professionals.
Graphical Abstract
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
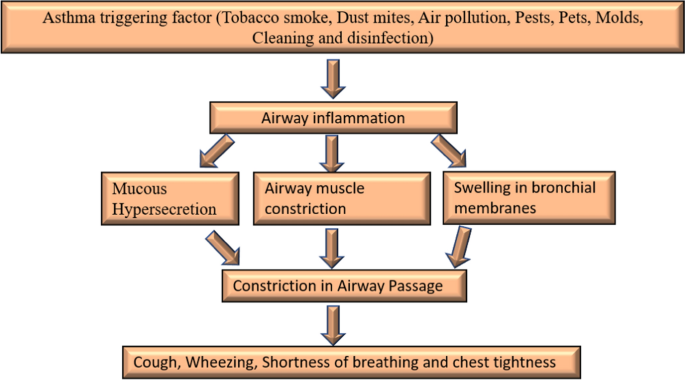
Asthma is one of the most ancient diseases of the airways, characterized by chronic inflammation and disordered airway function [1]. Despite numerous advancements in the treatment and diagnosis of asthma, unfortunately, a large population is still suffering, and worldwide it becomes one of the top infectious diseases. Approximately 10% of children and 5% of adults are suffering from this disease. A WHO key facts dated May 3, 2021, on asthma stated that approximately 262 million people are affected by this life-threatening disease in 2019 and the number will be expected to hike in the future. It is also characterized by some other symptoms like epithelial rupture, hypertrophy of airway smooth muscles, hypersecretion of mucous in lungs bronchial walls, wheezing, coughing, and dyspnea (Fig. 1). Although there is no proper treatment available for asthma, it can be controlled with proper management and help asthmatics to live in a better way [2]. The primary preventive measure taken by WHO (world health organization) for asthma and disease management is reducing tobacco smoke exposure, and the initiative MPOWER and Mtobacco cessation is enabling progress in this area of tobacco control.
The use of bronchodilators is the principal therapy used in asthma but a greater understanding of the chief role of inflammation in asthma has led to the conclusion of the use of anti-allergic or anti-inflammatory agents for the management of asthma and is an internationally recognized strategy for its cure. The ICS (Inhaled corticosteroids) can provide ideal disease control but not as monotherapy. They need additional therapies such as SABA (Short-acting β2 agonists), LABA (Long-acting β2 agonists), LTRA (Leukotriene receptor antagonist therapy), and theophylline to achieve adequate control [3]. The primary aim of writing this review paper is to provide a brief understanding of asthma by critically assessing articles related to asthma.
Material and Methods
We performed an electronic search to find out the existing literature on asthma. Initially, the search was conducted on search engines like Google Scholar® and PubMed® to gather updated information about asthma. In addition, the search was conducted on the official websites of professional organizations such as GINA (Global initiative for asthma), WHO, MOHFW (Government of India-ministry of health and family welfare), and CDC (Centers for disease control and prevention) to get relevant guidelines for asthma control, anti-asthmatic drugs, challenges, prevention, and control management programs. Approximately 10 months were completely used to compile data for this manuscript. The key terms used during the search were “Asthma,” “history of asthma” “current situation of asthma,” “asthma control history,” “challenges in asthma,” and “ongoing asthma management programs.” Two hundred eight papers were screened, and then, inclusion and exclusion criteria were applied to prepare this manuscript. Out of these papers, thirty papers were used to prepare this manuscript. The last search was conducted on October 30, 2021.
Inclusion and Exclusion Criteria
Resources that were targeted at healthcare professionals and articles with a thorough understanding of asthma were included. All those papers which do not have original data and studies targeting the general public and patients were excluded.
History
Ancient History
For the very first-time, respiratory distress was recorded in China in 2600BC. The evidence was found in the form of “noisy breathing.” Shen nong in 2700BC was the first person to taste ephedra which was popularly known as anti-asthmatic herbal medicine around 5000 years ago [2, 3]. The ancient Egyptians in 3000–1200BC believed respiration was one of the most crucial functions of the human body. Greco-roman (1000BC–200AD), both believe that asthma was produced due to demonic possession. Hippocrates was the first person who found that people suffering from asthma may have a hunch back. He also tried to understand the correlation between environment and respiratory problems. He also recommended ephedra along with red wine for the treatment of asthma [4].
Modern History
In the modern period, the understanding of the root cause of asthma began. In Europe 1500s, tobacco was introduced for the treatment of asthma, expectorate mucus and induce coughing. In 1579–1644, one of the chemists and physicians from Belgium Jean Baptiste Van Helmont said, “asthma was developed in the pipes of the lungs.” In (1633–1714), Bernardino Ramazzini found for the first-time exercise-induced asthma. He also acknowledged the correlation between organic dust and asthma. In the year 1873, Charles Blackley discovered the main cause of “hay asthma” and found that pollen was related to it. He rubbed pollen on different body parts to reproduce the symptoms [5]. In the 1900s, selective beta-2 adrenoceptors agonists were used for asthma treatment. In 1916, a physician and allergist named Francis Minot Rackemann reported that not all asthma is related to allergies. In 1920s, the deaths from asthma were related to airway structural changes and extensive inflammation but the information on why this happened and how it is responsible for bronchospasm was not known. For some decades, the treatment of asthma was done as episodic exacerbations [6]. Kustner and Prausnitz in the year 1921 noticed that asthmatics suffer from allergy symptoms due to indoor and outdoor irritants. In 1960s–1970s, technological advancements led to the use of peak flow meters to measure obstruction in airways and arterial blood gasses [7]. After the 1970s, inhaled corticosteroids were used for asthma cure. In 1980s, a depth understanding of how an allergen exposure, affect the release of a chemical mediator from mast cell which results in allergic asthmatic response [8].
Global Scenario
According to WHO information, asthma is included among (NCD) non-communicable diseases which is prevalent in children and adults. Generally, the deaths related to this disease mostly occur in countries with the economy in creeping and walking stage. The top fifteen countries with the largest asthmatic patients are Myanmar, Kiribati, Laos, Sri Lanka, New Guinea, Mali, Nepal, Fiji, Lesotho, Indonesia, Solomon Island, Sierra Leone, Timor-Leste, Philippines, and Vanuatu (https://www.worldlifeexpectancy.com/cause-of-death/asthma/by-country/). In 2010, according to the data provided by National Hospital Ambulatory Medical Care Survey, approximately 1.3 million patients hospital visits were due to asthma [9]. In 2011–2012, the national survey for children’s health reported that around 3.4% of children have used emergency hospital visits due to this life-threatening disease [5, 8]. Around 10.1 million physician office visits were reported for the year 2015. In 2017, around 43.12 million asthma cases were recorded whereas 272.68 asthma prevalence (prevalence 3.57%) and 0.49 million deaths (mortality rate 0.006%). More than 1.6 million asthmatic patient emergency visits were reported for the year 2018. According to the 2019 data by WHO, this disease is considered one of the top ten deadliest diseases. It cannot be completely cured but proper management with inhaled medications can help to control the disease and thereby help people to lead normal life [10]. Around 262 million people were affected by this deadly disease in 2019 which caused 461,000 deaths. Globally, this disease is ranked 16th among the leading causes of years lived with a disability as well as 28th among the leading causes of burden of disease as calculated by DALY (disability-adjusted life years). It is estimated that around 300 million people were suffering from asthma worldwide and by 2025 around 100 million people were affected. There is a huge geographical variation in asthma severity, prevalence, and mortality. The prevalence is extremely high in high-income countries whereas the mortality rate is high in low-middle-income countries. As per the Lancet, the asthma statistics worldwide for 2020 reported that more than 339 million people were suffering from asthma and globally approx. four million children develop asthma each year. In North America, approx. 8% population has been diagnosed with asthma. The estimated prevalence of severe asthma is 5–10% of the global asthma population. It is more common in Puerto Rican Hispanic (13.3%) and Black (8.7%) than in white people (7.6%). The mortality rate is higher in black 25.4 than in whites 8.8 per million annually. The treatment options available for asthma are discussed as follows:
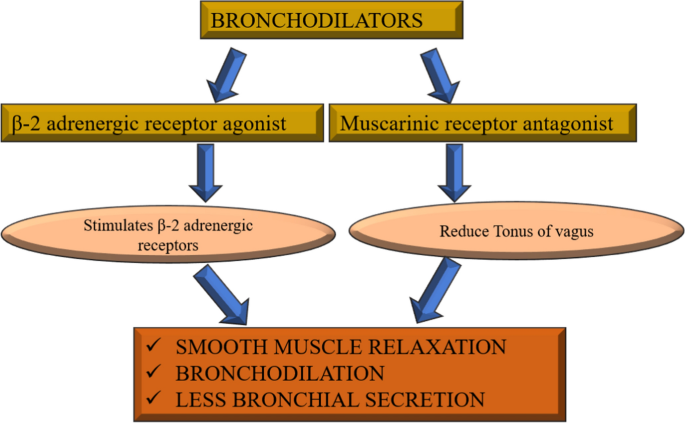
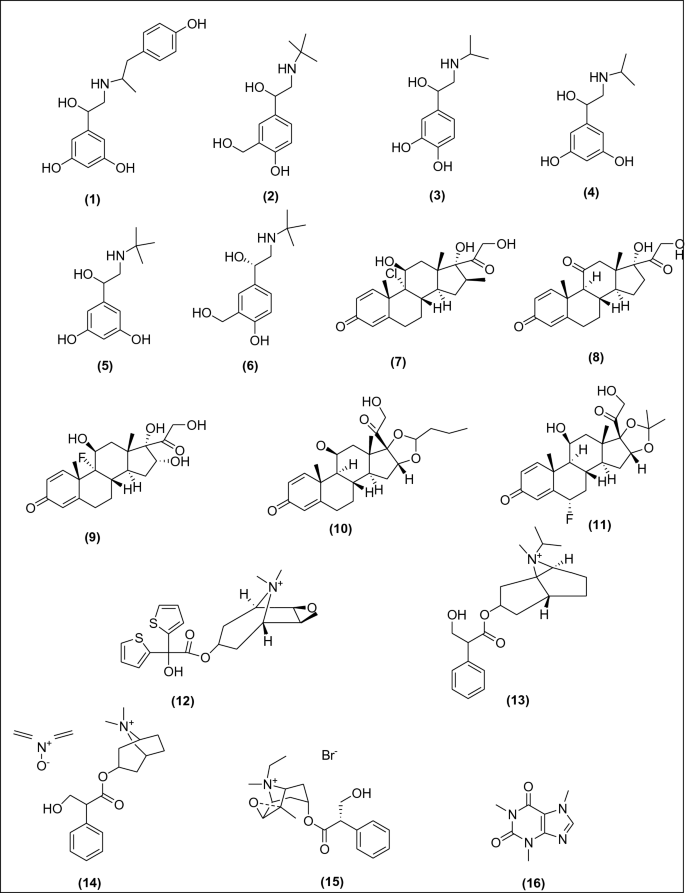
Bronchodilators or relievers act by quickly opening the airways and improving the rate of breathing. They also remove mucous from the lungs. As the airways get dilated, the mucous can be coughed with more ease. These act by targeting the β-2 adrenergic receptors in the airways. Activation of this receptor may relax the airway smooth muscles, thereby ensuring better airflow in the lungs [11]. Furthermore, they also help in inhibiting the parasympathetic nervous system receptors from functioning. As the parasympathetic nervous system increases the bronchial secretions and constriction in airways, inhibiting the nervous system should result in bronchodilation and lesser bronchial secretion [12] (Fig. 2). Bronchodilators are subdivided into the following parts (Fig. 3), Inhaled rapid-acting β-2 agonists: Fenoterol (1), Salbutamol (2), Isoproterenol (3), Metaproterenol (4), Terbutaline (5), Albuterol (6), Glucocorticoids (systemic): Beclomethasone (7), Prednisone (8), Triamcinolone (9), Budesonide (10), Flunisonide (11), Anticholinergics: Tiotropium bromide (12), Ipratropium bromide (13), Atropine methonitrate (14), Oxitropium bromide (15), Xanthine derivatives: Caffeine (16), Theobromine (17), Theophylline (18), Aminophylline (19), Hydroxyethyl theophylline (20), Choline theophyllinate (21), Doxophylline (22), Deriphylline (23), Diprophylline (24), Theophylline ethanolate of piperazine (25), Oral SABA: Salbutamol (2), Terbutaline (5), Bitolterol (26), Fenoterol (27), Rimiterol (28), Levalbuterol (29), and Pirbuterol (30).
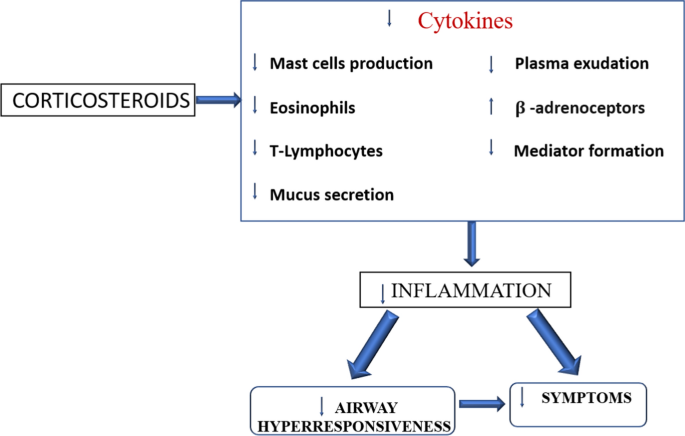
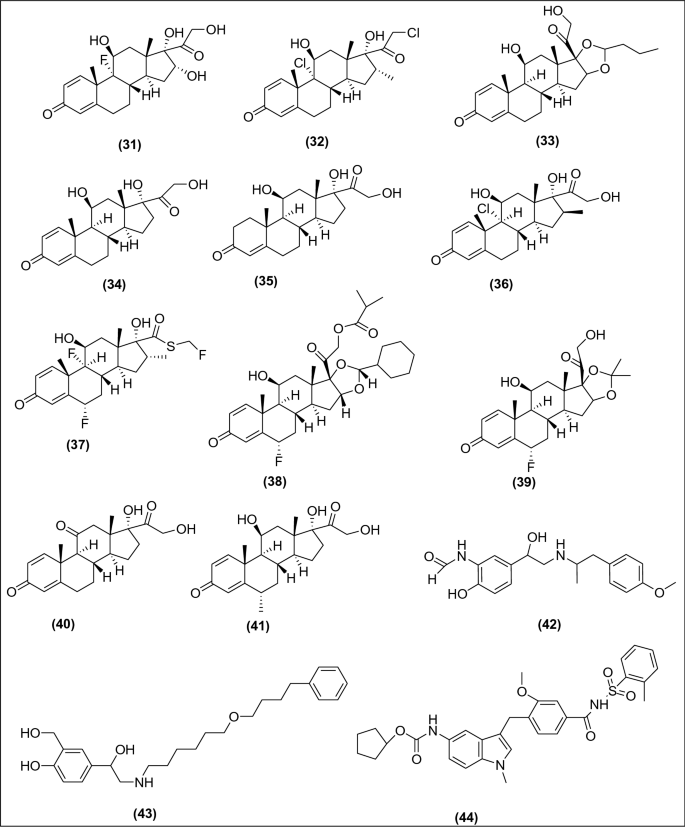
Anti-inflammatory agents reduce inflammation, swelling, and mucus production in the airways. The most important anti-inflammatory treatments are given by inhalation. Their mode of action is not completely understood, but they are likely to act in several different ways to produce an anti-inflammatory effect. The glucocorticoids act by inhibiting transcription factors that help in the regulation of pro-inflammatory mediators such as eosinophils, macrophages, dendritic cells, mast cells, and lymphocytes [13]. The steroids also act on mast cells and exert their anti-allergic action by inhibiting the signaling pathways in mast cells [14]. Furthermore, they also reduce plasma exudation in the airways and inhibit mucus glycoprotein secretion (Fig. 4). Anti-inflammatory agents are further classified into (Fig. 5), Inhaled or systemic corticosteroids: Triamcinolone (31), Mometasone (32), Budesonide (33), Prednisolone (34), Hydrocortisone (35), Beclomethasone (36), Fluticasone (37), Ciclesonide (38), Flunisolide (39), prednisone (40), Methylprednisolone (41), LABA: Formoterol (42), Salmeterol (43), Anti-IgE: Omalizumab, Leukotriene antagonist: Zafirlukast (44), Montelukast (45), Pranlukast (46), Iralukast (47), Oral anti-allergic compounds: Tranilast (48), Mast cell stabilizer: Sodium cromoglycate (49), Nedocromil Sodium (50), and Ketotifen (51).
Indian Scenario
The Indians ayurveda believe that asthma results due to the imbalance between three doshas: (a) pitta (bile), (b) Kapha (phlegm), and (c) vata (wind). A person stays healthy if these three humors were balanced. The first book Ayurveda Materia medica from India ‘Charaka Samhita’ has a good clinical description of this life-threatening disease. A recent study on respiratory symptoms and chronic bronchitis performed on 85,105 men and 84,470 women from eleven rural and twelve urban areas in India estimated the prevalence rate of asthma is 2.05% among those aged above 15 years with an estimated national burden causing 18 million asthmatics [15]. Despite enormous advancements in the treatment and management of this disease, it becomes a major public health issue in India.
Asthma Control History
The Early Period of Asthma Control
In 1500BC, the inhalation of the smoke of herbs is recommended for use as the treatment therapy for asthmatic patients in Egypt. In ancient China around 5000 years ago, the treatment was done by using ma-huang (Ephedra sinica), a type of Chinese herb which was later examined to have ephedrine (muscle relaxant), and these agents work as bronchodilators [6, 13]. For a prolonged period, bronchodilators were used as the first-line drugs for the management of asthma which indicates contraction of airways as the chief pathology involved in the treatment. In 1900, the avoidance of allergens was used as the foremost therapy for asthma [5]. The use of a pressurized metered-dose inhaler in the mid-1950 has been developed for the administration of adrenaline and isoproterenol and was later used as a β2-adrenergic agonist. Later salbutamol and terbutaline were introduced as SABA. Recently, LABA is used as the principal drug incorporated into the inhaled corticosteroids in Japanese guidelines for asthma. Furthermore, LTRA and theophylline were used as the first-line drugs along with LABA and inhaled corticosteroids. The American thoracic society in the year 1962 describes asthma as a disease identified by the presence of airway hyper-responsiveness as well as reversible airway constriction [12]. Moreover, chronic airway inflammation was finally found as the clinical etiology involved in the pathogenesis of asthma and inhaled corticosteroids and the use of anti-inflammatory drugs became the first-line therapy for asthmatic patients [16]. In the early twentieth century, inhalation and intravenous administration of anticholinergic drugs were regarded as the principal therapy for asthma [2].
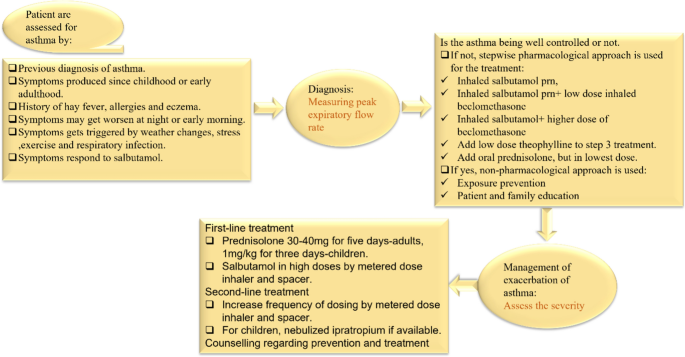
Current WHO-Aided Asthma Control Program
For the prevention and control of asthma, this disease has been incorporated in the WHO global action plan as well as the UN (United Nations) 2030 agenda for the sustainable development. WHO has taken several actions to extend the diagnosis and treatment of this disease. The PEN (package of essential non-communicable) disease intervention was developed by WHO to support people with non-communicable diseases with the help of UHC (universal health coverage) [17]. The PEN includes rules for assessment, diagnosis, and management of asthma and (COPD) chronic obstructive pulmonary disease and includes modules on healthy lifestyles (Fig. 6) [18]. The primary preventive measure taken for asthma and disease management is reducing tobacco smoke exposure, and the initiative MPOWER and Mtobacco cessation is enabling progress in this area of tobacco control. MPOWER is the WHO framework convention on tobacco control, and its guidelines were meant for countries working toward tobacco control. These guidelines were introduced in the year 2008 to manage tobacco control at the country level.
WHO Global Action Plan 2013–2020
The goal of this action plan is to reduce the number of morbidities, mortality, and disability due to NCD by using multisectoral cooperation and collaboration at distinct levels (national, regional, and global), so that the population will remain at the highest standard of health and productivity at all ages as well as those diseases will no longer act as a barrier to well-being. As per the WHO, the total number of deaths due to NCD may increase to 55 million by 2030. The scientific knowledge demonstrates that the prevalence of non-communicable diseases is greatly decreased if cost-effective preventive and curative action, as well as interventions for prevention and control of NCD which are already available, are implemented in a balanced and effective manner [19].
GINA Global Strategy for Asthma 2021
On Nov 1, 2021, the GINA published an executive summary of an updated evidence-based summary for the treatment and prevention of asthma. On Oct 18, 2021, the summary was published online. The GINA science committee was developed in the year 2002 to review published research on asthma. This GINA report is updated every year and approx. 500,000 copies of GINA reports were downloaded each year by one hundred countries [20]. GINA report has been updated in the year 2020 with some modifications such as interim guidance about asthma and Covid-19, additional information for the new as well as existing therapies; additional documents have been added in supporting the use of ICS (Inhaled corticosteroid)—formoterol in mild asthma; assessment of symptom control and new data have been incorporated for the initial treatment of newly diagnosed asthma; information related to a maximum daily dose of ICS-Formoterol has been added; additional documents for the support of the use of ICS and addition of minimum and maximum doses of ICS have been incorporated in the treatment recommendation for asthma, and new additional information about the management of asthma in children has also been added [21].
India Asthma Report
As per demographics, around 6% of children and 2% of adults were suffering from this disease. A maximum number of people in India have no health insurance, and there is a big gap in healthcare facilities for the poor and the rich people. Most of the medications available in India (inhaled corticosteroids, combination inhalers, and β-2 agonists) are too expensive compared to oral formulations [22]. According to the data compiled from 1990 to 2005, the mortality rate in India decreased mainly in areas where healthcare facilities were better (urban areas and prosperous states). It was documented that Rajasthan and Uttar Pradesh have the highest mortality rate. The Rajasthan government had provided free access to medicines to all the asthmatic patients of the state at government hospitals since 2011 and around 15,000 pharmacies had been opened by the state government across the state along with a free supply of metered-dose inhalers, nebulizer solutions, and dry powder inhaler capsules to asthmatic patients. In 2018, the Indian government planned to provide health insurance at no cost to 100 million low-income families, to cover their treatment costs [23].
Ongoing Challenges in Asthma Therapy
The problem of asthma is a global burden affecting more than 300 million people and causing around 2,50,000 deaths per year. Despite several effective treatments available, the control of this disease in the population remains inadequate. The advancement in treatments for children is lesser as compared to the adults due to the varying immunopathology, respiratory pathology, need for a child, parent education, and communication barrier. As most of the asthma research work was performed on adult asthma, thus this seems to be one of the principal barriers to managing the therapy childhood asthma [16]. The data on LABA use for the treatment of asthma in adults are widely available while the data available for LABA use in children are limited. Since then, several studies have been conducted to complete the gap for LABA use in children and adolescents resulting in several regulatory approvals for LABA inhalers, and inhaled corticosteroids such as fluticasone + salmeterol, budesonide + formoterol have been approved as maintenance treatment for children and adolescents in the USA and Europe [24, 25]. Asthma management in children is a complex process due to variability in asthma severity, control, and difficulty in measuring lung function as well as airway inflammation. The primary challenge in the management of pediatric asthma is treating the symptoms of asthma rather than treating the root cause, i.e., inflammation, and switching to controller therapy when the problem worsens. The prevalence of childhood asthma increased in the 1980s–1990s, and the rate kept on increasing over the past decade; it seems to be one of the greatest global economic burdens in terms of direct and indirect costs.
Furthermore, the healthcare providers, as well as patients, are dealing with several types of challenges such as challenges in diagnosis, treatment, and follow-up challenges. As poor healthcare facilities are provided in rural areas, poverty, lack of awareness, and the high price of anti-asthmatic drugs are some of the routinely faced challenges of patients [26]. The diagnosis of asthma seems to be challenging work, both in terms of underdiagnosis and overdiagnosis. The underdiagnosis of asthma is familiar and was documented in epidemiological as well as clinical studies while the data on overdiagnosis are new [27]. Physicians are entirely dependent on asthma guidelines for the diagnosis and management of this disease. The NIH (National Institute of health) released latest updates to the national guidelines meant for the diagnosis, management, and treatment of asthma. The guidelines were made to upgrade patient care and to support decision-making about asthma management in a clinical setting.
In India, the national rural health mission (NRHM) was implemented to improve primary healthcare facilities in rural areas, to improve the health status and quality of life of people living in rural areas, and to prevent and control communicable and non-communicable diseases. The diagnosis of asthma is a difficult process because for some reasons: (a) The signs and symptoms might not show during routine analysis, (b) unavailability of the standard diagnostic test—in clinical practice, spirometry and peak expiratory flow assessment are done to check the signs and symptoms, and (c) The guideline recommendation is not always compatible with the working systems in primary care. Some of the other treatment options which might help in improving asthma management and control are switching from relievers SABA to LABA along with a combination of inhaled corticosteroids as per the recommendation of GINA to make sure that the person with asthma receives an inhaled corticosteroid to get symptomatic relief whenever possible.
Ongoing Asthma Management Programs
The problem of asthma is prevalent among children and elderly people. In UK 1 in 14 adults are affected by this alarming condition. The national public health agency of the USA, i.e., CDC has made a self-management education (SME) program “Breathe well, live well” that helps those people with prevailing health conditions to feel better. The SME program helps people to strategize and develop the skills and confidence to tackle ongoing health conditions efficiently and help in dealing with the following conditions: cope with symptoms, communicate with doctors, manage fatigue, handle stress, manage medication, eat healthy, reduce depression, and be active. These strategies can help the patients to make good decisions about health and makes them feel better [28].
The 2020 focused updates to the asthma management guidelines were published for the diagnosis and management of asthma. These guidelines help the clinician integrate the new recommendation into clinical care. These are meant for individual patient management [29]. The Alameda County public health department (ACPHD) enabled community health services asthma start programs that help families of children with asthma by providing in-home case management studies. They provide education, support, and assistance in developing an action plan to address the needs of families where the child has asthma thereby helping in regulating it. The services provided by them is as follows: (a) education to families about the disease, several types of triggers, prevention of attacks, treatments, etc., (b) collaborating with daycare providers and schools to make sure asthma medication is accessible to every child, and moreover, supplying asthma-related education to all the school staff as well as daycare providers, (c) assistance with health insurance, housing, and employment, and (d) remote home inspections to find the triggers and causes of asthma [30].
Results and Discussion
Generally, the recommendations from different professional bodies suggest that physicians should follow the already existing guidelines for the proper management of this disease. The key points are as follows: bronchodilators were considered a principal therapy for the treatment of asthma in early times, but after the advent of inhaled corticosteroids, the therapeutic history gets drastically changed. The use of bronchodilators is the principal therapy used in asthma but a greater understanding of the chief role of inflammation in the pathogenesis of asthma has led to the conclusion of the use of anti-allergic or anti-inflammatory agents for the management of asthma. The ICS can provide ideal disease control but not as monotherapy. They need additional therapies such as SABA, LABA, LTRA, and theophylline to achieve adequate control.
It is very much clear from the above discussion that we have done so much advancement to fight against this deadly disease and we still need time to make the globe asthma-free. The number of people suffering from asthma is more than the number of people suffering from HIV infection and tuberculosis.
Conclusion
Understanding the recommendations of professional bodies will assist in medical decision-making in asthma management. Healthcare professionals should consider the individual needs of patients. In conclusion, the main problem in the management of this disease is improper use of healthcare facilities, lack of knowledge about anti-asthmatic drugs, poverty, and the cost of drugs. The government should make and adopt more strategies to promote the rational use of anti-asthmatic drugs and make plans to spread more awareness among people about the schemes and programs made for safeguarding people against this life-threatening disease.
References
Löwhagen O (2015) Diagnosis of asthma–new theories. J Asthma 67(6):713–717. https://doi.org/10.3109/02770903.2014.991971
Stein SW, Thiel CG (2017) The history of therapeutic aerosols: a chronological review. J Aerosol Med Pulm Drug Deliv 30(1):20–41. https://doi.org/10.1089/jamp.2016.1297
Bergmann KC (2014) Asthma. Chem Immunol Allergy 100:69–80. https://doi.org/10.1159/000358575
Rothe TA (2018) Century of “intrinsic asthma.” Allergo J 27:19–23. https://doi.org/10.1007/s15007-018-1719-3
Sanders MJ (2017) Guiding inspiratory flow: development of the in-check DIAL G16, a tool for improving inhaler technique. Pulm Med. https://doi.org/10.1155/2017/1495867
Beasley R, Harper J, Bird G et al (2019) Inhaled corticosteroid therapy in adult asthma: time for a new therapeutic dose terminology. Am J Respir Crit Care Med 199(12):1471–1477. https://doi.org/10.1164/rccm.201810-1868ci
Silverman RA, Hasegawa K, Egan DJ et al (2017) Multicenter study of cigarette smoking among adults with asthma exacerbations in the emergency department, 2011–2012. Respir Med 125:89–91. https://doi.org/10.1016/j.rmed.2017.02.004
Quirt J, Hildebrand KJ, Mazza J et al (2018) Asthma. Allergy Asthma Clin Immunol 14:15–30. https://doi.org/10.1186/s13223-018-0279-0
Centers for Disease Control and Prevention (2018) Usual place for medical care among children, pp 13–17. https://www.cdc.gov/nchs/data/nhis/earlyrelease/EarlyRelease201803_02.pdf. Accessed 8 April 2021
GBD 2019 Diseases and Injuries Collaborators (2020) Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396(10258):1204–1222. Erratum in: Lancet. 2020; 396(10262):1562. https://doi.org/10.1016/s0140-6736(20)30925-9
Matera MG, Page CP, Calzetta L et al (2020) Pharmacology and therapeutics of bronchodilators revisited. Pharmacol Rev 72(1):218–252. https://doi.org/10.1124/pr.119.018150
Harma S, Hashmi MF, Chakraborty RK (2021) Asthma medications. StatPearls Publishing, Treasure Island
Williams DM (2018) Clinical pharmacology of corticosteroids. Respir Care 63(6):655–670. https://doi.org/10.4187/respcare.06314
Oppong E, Flink N, Cato ACB (2013) Molecular mechanisms of glucocorticoid action in mast cells. Mol Cell Endocrinol 380(1–2):119–126. https://doi.org/10.1016/j.mce.2013.05.014
Joshi KS, Nesari TM, Dedge AP et al (2016) Dosha phenotype specific Ayurveda intervention improves asthma symptoms through cytokine modulations: results of whole system clinical trial. J Ethnopharmacol 197:110–117. https://doi.org/10.1016/j.jep.2016.07.071
Barcik W, Boutin RCT, Sokolowska M, Finlay BB (2020) The role of lung and gut microbiota in the pathology of asthma. Immunity 52(2):241–255. https://doi.org/10.1016/j.immuni.2020.01.007
World Health Organization (2021) factsheet: Asthma. https://www.who.int/news-room/fact-sheets/detail/asthma. Accessed 17 April 2021
World Health Organization (2020) package of essential non communicable (PEN) disease interventions for primary healthcare. https://www.who.int/publications/i/item/who-package-of-essential-noncommunicable-(pen)-disease-interventions-for-primary-health-care. Accessed 24 April 2021
World Health Organization (2013) Global action plan for the prevention and control of non-communicable diseases 2013–2020. https://apps.who.int/iris/bitstream/handle/10665/94384/9789241506236_eng.pdf?sequence=1. Accessed 2 May 2021
Global Initiative for Asthma (GINA) (2021) Global strategy for asthma management and prevention. https://ginasthma.org/wp-content/uploads/2021/07/GINA-2021_Methodology_20210523.pdf. Accessed 12 May 2021
Global Initiative for Asthma (GINA) (2020) Pocket guide for asthma management and prevention for adults and children (updated 2020). https://ginasthma.org/wp-content/uploads/2020/04/Main-pocket-guide_2020_04_03-final-wms.pdf. Accessed 17 June 2021
The Global Asthma Report (2018) http://globalasthmareport.org/management/india.php. Accessed 22 June 2021
Centers for Disease Control and Prevention (2019) Most recent national asthma data. https://www.cdc.gov/asthma/most_recent_national_asthma_data.htm. Accessed 8 Aug 2021
Szefler SJ, Chipps B (2018) Challenges in the treatment of asthma in children and adolescents. Ann Allergy Asthma Immunol 120(4):382–388. https://doi.org/10.1016/j.anai.2018.01.003
Pearlman DS, Eckerwall G, McLaren J et al (2017) Efficacy and safety of budesonide/formoterol pMDI vs budesonide pMDI in asthmatic children (6–<12years). Ann Allergy Asthma Immunol 118:489–499. https://doi.org/10.1016/j.anai.2017.01.020
Bakirtas A (2017) Diagnostic challenges of childhood asthma. Curr Opin Pulm Med 23(1):27–33. https://doi.org/10.1097/MCP.0000000000000338
Aaron SD, Boulet LP, Reddel HK, Gershon A (2018) Under-diagnosis and over-diagnosis of asthma. Am J Respir Crit Care Med 198(8):1–25. https://doi.org/10.1164/rccm.201804-0682ci
Centers for Disease Control and Prevention. Managing asthma. https://www.cdc.gov/learnmorefeelbetter/programs/asthma.htm. Accessed 15 Aug 2021
2020 Focused updates to the asthma management guidelines (2020) Briefly guide. https://www.nhlbi.nih.gov/sites/default/files/publications/AsthmaClinicians-At-a-Glance-508.pdf. Accessed 10 Sept 2021
Alameda County Public Health Department. Asthma Start program. https://acphd.org/asthma/. Accessed 30 Oct 2021
Acknowledgements
The authors are thankful to the Honorable Vice-Chancellor, Banasthali Vidyapith, Banasthali, Rajasthan, for providing essential facilities.
Funding
There was no funding provided for the preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Nitin Gupta contributed to Conception and design of study, Swati Pant contributed to literature collection and Anandi Kapri contributed to Drafting the manuscript and Sumitra Nain & Sarvesh Paliwal contributed to Overall supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Significance Statement: This review paper aims to spread awareness among the general public about the scenario of Asthma. The physicians should prescribe bronchodilators and anti-inflammatory agents to manage asthma symptoms.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kapri, A., Pant, S., Gupta, N. et al. Asthma History, Current Situation, an Overview of Its Control History, Challenges, and Ongoing Management Programs: An Updated Review. Proc. Natl. Acad. Sci., India, Sect. B Biol. Sci. 93, 539–551 (2023). https://doi.org/10.1007/s40011-022-01428-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40011-022-01428-1