Abstract
Background
A considerable number of patients who contracted SARS-CoV-2 are affected by persistent multi-systemic symptoms, referred to as Post-COVID Condition (PCC). Post-exertional malaise (PEM) has been recognized as one of the most frequent manifestations of PCC and is a diagnostic criterion of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Yet, its underlying pathomechanisms remain poorly elucidated.
Purpose and methods
In this review, we describe current evidence indicating that key pathophysiological features of PCC and ME/CFS are involved in physical activity-induced PEM.
Results
Upon physical activity, affected patients exhibit a reduced systemic oxygen extraction and oxidative phosphorylation capacity. Accumulating evidence suggests that these are mediated by dysfunctions in mitochondrial capacities and microcirculation that are maintained by latent immune activation, conjointly impairing peripheral bioenergetics. Aggravating deficits in tissue perfusion and oxygen utilization during activities cause exertional intolerance that are frequently accompanied by tachycardia, dyspnea, early cessation of activity and elicit downstream metabolic effects. The accumulation of molecules such as lactate, reactive oxygen species or prostaglandins might trigger local and systemic immune activation. Subsequent intensification of bioenergetic inflexibilities, muscular ionic disturbances and modulation of central nervous system functions can lead to an exacerbation of existing pathologies and symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The persistence of long-term symptoms of COVID-19 is a common phenomenon among those who contracted a SARS-CoV-2 infection. A meta-analysis of 31 studies revealed that 43% experience lingering or newly appearing symptoms one month post-infection [1]. Symptoms that persist longer than three months post-infection are subsumed under the term Post-COVID Condition (PCC) [2]. Based on population-based studies from the United States, the number of people suffering from PCC is estimated to be around 6.9% [3]. In this context, it bears noting that acute disease severity has an impact on the risk of developing PCC [4]. Specifically, patients who have been hospitalized are more likely to experience residual symptoms compared to non-hospitalized individuals [5], with asymptomatic cases exhibiting the lowest risk of having PCC [6]. Yet, the mechanisms of PCC may differ following a severe versus mild infection. In addition to that, the risk of persistent symptoms is significantly lower in vaccinated compared to unvaccinated subjects [7, 8]. Whether the risk differs between variants and dependent on medication treatment during acute illness remains controversial [9,10,11,12,13].
The clinical spectrum of PCC comprises a variety of different symptoms affecting multiple organ systems, with fatigue, headache, shortness of breath, cognitive impairment, exercise intolerance and post-exertional malaise (PEM) being among the most commonly reported symptoms [14,15,16,17,18]. The latter refers to an inadequate exacerbation of symptoms and a prolonged recovery phase, most frequently triggered by physical exertion [15]. PEM is a debilitating clinical manifestation and it has been reported that at least 68% of individuals with PCC experience it [15, 19]. Moreover, it is considered a hallmark symptom for the diagnosis of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Although PEM can occur in other chronic diseases, the severity and length of PEM allows to distinguish ME/CFS from other diseases with similar clinical spectrums such as fibromyalgia or multiple sclerosis [20]. An overlapping clinical picture and the fact that more than one year post-infection 19–58% of PCC patients meet the diagnostic criteria for ME/CFS suggests a common etiology of both syndromes [21,22,23,24]. Beyond that, the onset of ME/CFS is most commonly described to be preceded by infection-like episodes [25]. However, the spectrum of PCC is more heterogenous compared to post-acute infection syndromes triggered by other pathogens. Specifically, the severity and duration of PEM in PCC varies, with a subset of PCC patients having episodes that last only for several hours or that are not severe enough to fulfill the Canadian or IOM criteria for ME/CFS [24]. Even though COVID-19 is not more likely to be associated with ME/CFS than other infections [26], this points towards potential virus-specific mechanisms underlying PEM in PCC.
However, there is still no unifying understanding of the pathophysiology of these conditions and the mechanisms that elicit episodes of PEM following acute and regular physical activities. In this review, we aim to conceptualize the evidence that has emerged on PCC and ME/CFS pathophysiology which has improved our understanding of the processes that lead to the development of PEM.
PEM symptom characterization across the post-acute infection syndrome spectrum
PEM is characterized by a disproportional clinical deterioration of one or multiple symptoms that can occur up to 72 h following exertional activities that were tolerated prior to the illness [27, 28]. This state can last for several days or weeks and is barely alleviated by rest or sleep [15]. The most common trigger of such “crashes” is physical exertion [27]. Other potential triggers include cognitive and emotional exertion, insufficient sleep, temperature extremes or orthostatic stress [29]. Reflecting its proposed pathophysiology and the fact that many patients experience a worsening of immune or nervous system related symptoms [30], PEM is also referred to as post-exertional neuroimmune exhaustion or simply post-exertional symptom exacerbation.
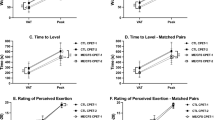
A characteristic decrease in function following physical exertion in patients with ME/CFS has been objectified by studies conducting two-day cardiopulmonary exercise testing (CPET). Patients with ME/CFS declined significantly in measures of aerobic capacity and workload on the second day of testing while controls improved in these performance instances [31]. In line with that, patients with ME/CFS showed greater declines in hand grip strength than healthy controls upon repeated testing, which correlated with higher PEM scores [32].
Importantly, PEM is clinically often accompanied by fatigue and profound exercise intolerance. Yet, while being pathogenically connected, they constitute separate entities of the post-infectious disease manifestations. In fact, exercise intolerance refers to the inability to uphold acute exercise due to lack of energy, or rapid development of palpitations, tachycardia, or breathlessness. On the other hand, PEM describes an inadequate delayed regulatory response that elicits the aggravation of symptoms such as fatigue, pain or cognitive impairment and a decrease in the physical capacity level. Importantly, this can occur after exercise as well as after moderate physical activity and activities of daily living [30]. [25]. In severe ME/CFS, already minor activities such as sitting up or brushing teeth can trigger PEM. For the context of this paper and in accordance with previous definitions, we refer to physical activity as any muscle-induced bodily movement that increases energy expenditure above resting conditions and to exercise as planned and structured forms of physical activity [33].
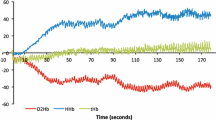
Hypoxic metabolic response profile to acute physical activity stimuli
The understanding of physical activity-induced symptom exacerbations requires consideration of the acute metabolic response to exercise stimuli and elicited regulatory processes in affected patients. Among others, findings established by studies conducting CPET using incremental cycle ergometry revealed a response pattern that suggests aberrant cell metabolism under hypoxic environments in PCC. Accordingly, patients with persistent symptoms exhibited a reduced aerobic capacity and attained their anaerobic threshold earlier compared to controls. Specifically, multiple studies reported a lower peak oxygen uptake (VO2peak) in PCC patients, regardless of acute disease severity [34,35,36,37]. In line with that, a meta-analysis of nine studies with 464 subjects showed that the mean difference in VO2peak of PCC subjects was 4.9 mL/kg/min lower than that of individuals that completely recovered from infection [38]. Correspondingly, an analysis of surrogates of mitochondrial function during exercise testing revealed that in addition to higher blood lactate concentrations, at peak exercise subjects with PCC showed significantly lower levels of β-oxidation of fatty acids compared with control subjects, which might serve as an indication for a premature switch to anaerobic glycolysis [35].
The mechanisms underlying reduced aerobic capacity are still lacking conclusive evidence, with some studies interpreting the observed limitations as muscular deconditioning [39]. Durstenfeld et al. concluded that 80% of studies that attributed deconditioning to diminished exercise capacity included subjects that were previously hospitalized with acute COVID-19 and thus potentially immobilized for extended periods of time [38]. Moreover, there exist studies that included non-hospitalized subjects that exhibited diminished aerobic capacity compared with healthy controls, while physical activity levels before infection and at examination did not differ significantly, which makes the contribution of deconditioning less likely [34]. In line with that, the functional limitations observed in PCC exceed the decline in oxygen uptake that would be expected from bed rest only [40, 41]. Beyond that, although it has to be noted that there is evidence that cardiovascular impairments exist among PCC patients [42, 43], cardiac and ventilatory limitations of exercise performance are rather uncommon [38].
In contrast, more profound analyses gave indications for loss of oxygen transport and metabolism pathway integrity [34, 44] (Fig. 1). Specifically, findings from invasive hemodynamic assessments combined with CPET revealed decreased systemic and peripheral oxygen extraction at peak exercise in PCC subjects which was attributed to reduced oxygen diffusion in the peripheral microcirculation [44,45,46]. This was particularly supported by findings from a study using near-infrared spectroscopy that revealed a reduced fractional oxygen extraction at the muscular level as well as a lower oxidative capacity [34].
Potential drivers of PEM include microvascular alterations and mitochondriopathy that can functionally culminate in reduced systemic oxygen extraction and oxidative phosphorylation capacity upon physical activities (a–b). Altered bioenergetics limit the patients’ ability to be physically active and induce the accumulation of lactate, reactive oxygen species and cations (c). Overexertion could manifest as delayed symptom exacerbation and systemic fatigue through subsequent immune activation that might aggravate bioenergetic inflexibilities and modulate CNS functions (d) (Figure created with biorender.com) ATP adenosine triphosphatem, CNS central nervous system, eNOS endothelial nitric oxide synthase, ETC electronic transport chain, FMD flow-mediated dilation, NO nitric oxide, ROS reactive oxygen species, TCA tricarboxylic acid
Thus, reduced oxygen extraction is found in both ME/CFS and PCC [47]. Evidence accumulates that mechanisms underlying impairments in peripheral oxygen consumption may include dysregulated microcirculation and mitochondrial dysfunction, as outlined below.
Muscular mitochondriopathy in PCC and ME/CFS
Evidence that mitochondrial function can be diverted in PCC comes from studies conducting histochemical analyses of muscle biopsy samples. Morphologically, histological staining of vastus lateralis samples revealed a significantly lower percentage of succinate dehydrogenase (SDH) positive and higher percentage of SDH-negative fibers in PCC patients compared to recovered controls [34]. With SDH being an essential enzyme of the tricarboxylic acid (TCA) cycle, these findings point towards decreased content of oxidative and increased content of glycolytic fibers [34], a finding that was also observed in patients specifically experiencing episodes of PEM [48]. Notably, muscle mitochondrial enzyme activity was shown to further decrease one day after the induction of PEM in PCC patients [48]. Further implications for a shift away from oxidative metabolism were provided by the observation that key metabolites of the TCA cycle (i.e. glutamate, α-ketoglutarate, citrate) and the citrate: lactate ratio are lower in skeletal muscle samples of PCC patients as compared to healthy subjects [48] (Fig. 1b).
In line with that, citrate synthase protein and mRNA levels were lower [34] and genetic pathways related to oxidative phosphorylation and cell respiration were downregulated in patients with persistent symptoms [49]. These findings are also reflected by impaired function of mitochondrial complexes. Specifically, high-resolution respirometry revealed a significantly reduced oxygen flux for mitochondrial complex II, and I and II together [34, 50]. Additionally, a loss of cytochrome c oxidase (complex IV) activity has been reported [51] (Fig. 1b). The significant increase of Wiskott-Aldrich Syndrome Protein Family Member 3 (WASF3) protein in muscle cells of ME/CFS patients has been implicated to be a molecular explanation for these functional mitochondrial disruptions [52]. Accordingly, the overexpression of WASF3 induced by stress to the endoplasmic reticulum has been demonstrated to lead to decreases in subunits of complex IV and thus to impair the assembly of supercomplex III2 + IV in mouse muscles. This disruption subsequently caused decreased muscular oxidative metabolism, a reduction in maximal running capacity and higher blood lactate levels. Conversely, knocking down WASF3 in myoblasts improved respiration capacity [52].
Beyond that, previously discussed indications for impaired fatty acid oxidation during CPET have been substantiated by a study finding higher levels of plasma carnitine-conjugated and free fatty acids in rest in PCC compared to control subjects [53]. On the other hand, a decrease in plasma acetylcarnitine may be associated with neurocognitive symptoms [54]. A virus-induced shift towards extra-mitochondrial metabolism has been suspected to inhibit antiviral signaling pathways and to promote viral particle formation for the purpose of replication enhancement [53, 55].
In summary, these findings point towards mitochondrial dysregulation with subsequent impairment of function, e.g. oxidative phosphorylation capacity and a switch towards glycolytic pathways (Fig. 1b). Consequently, alterations in mitochondrial structure and function could lead to lower oxygen pressure. This might also explain why PCC patients exhibit slower decline in tissue oxygenation upon occlusion-induced ischemia than subjects without persistent symptoms [56].
Hemodynamic and microvascular contribution to bioenergetic alterations
Dysfunctional microcirculation and organ perfusion disturbances are proposed to be key features of PCC. Pathogenically, they are supposed to be induced by several interdependent mechanisms that might further compromise a compensation of tissue oxygenation deficits emerging upon exertional activities.
Centrally involved in the development of COVID-19 complications is an endotheliopathy [57] that can outlast the acute illness and is associated with the persistence of symptoms [58]. Correspondingly, PCC patients exhibit elevated levels of circulating endothelial cells, endothelial colony-forming cells, and reduced ADAMTS-13: von Willebrand factor (vWF) ratio, implying ongoing cell damage [59, 60]. Beyond that, a lower flow-mediated dilation (FMD) in patients with PCC suggests a maladaptive capacity of the endothelium to adjust the vascular tone, which has been directly related to symptom persistence [58, 61]. Of note, both a reduced FMD and ADAMTS-13: vWF ratio are additionally associated with a lower exercise capacity, suggesting a potential contribution of endothelial dysfunction to peripheral oxygenation deficits [62, 63]. Of note, a recent MRI study showed that PCC patients exhibit widespread decreased brain oxygen levels in grey and white matter, indicating increased cerebral metabolism [64].
A major cause of compromised endothelial function is proposed to be an inadequate nitric oxide production of the endothelial isoform of nitric oxide synthase (eNOS) that is related to low bioavailability of essential substrates, such as arginine [65, 66]. Consistent with that, it has been shown that endothelial cells cultured in the plasma of ME/CFS patients produce less nitric oxide upon exposure to activating substances than in the presence of healthy control serum [67]. The fact that the supplementation of L-arginine improved FMD, physical performance and perception of effort and fatigue, proves that endothelial cell function might be a central disease pathway [66, 68, 69]. Moreover, potential disturbances in the regulation of molecule release by endothelial cells involved in NO availability and angiogenesis in PCC and ME/CFS compared to healthy donors could also impact the endothelial functionality [70]. Additional structural changes, such as a thickened capillary base membrane might further impair oxygen diffusion into peripheral tissues [51, 71] (Fig. 1a).
Secondly, PCC and ME/CFS are characterized by a thromboinflammatory state [59]. In particular, the discussed endothelial cell dysfunction and immune system activation likely trigger ongoing clotting activity [72]. Specifically, the formation of fibrinolysis-resistant microclots has been documented in PCC patients, which might be related to increased levels of antiplasmin [73] (Fig. 1a). Further analyses revealed that thrombogenicity is also a result of increase in platelet binding capacity that inversely correlated with ADAMTS-13 activity [74]. Of note, research on ME/CFS showed that the increase in clotting proteins (fibrinogen chain proteins FGA and FGB) 15 min after CPET until volitional exhaustion positively correlated with PEM that subjects were experiencing 24 h post-exercise [75]. A dysregulated hemostasis with microthrombi leading to small vessel occlusion could consequently lead to hypoperfusion and ischemia–reperfusion injury, for example to the mitochondrion through sodium and calcium overload [76, 77]. The pathogenic role of ischemia and reperfusion in the development of muscular mitochondriopathy is strengthened by the fact that patients with peripheral arterial occlusive disease present with similar morpho-functional changes like the previously discussed in PCC [78]. Yet, there is no evidence of overt microthrombosis formation from muscle histology studies [48, 50, 51, 71].
Lastly, evidence exists suggesting that perfusion and oxygenation deficits may be linked to altered erythrocyte functional morphology and oxygen affinity. Specifically, reduced MCV and MCH as well as structural membrane damages of erythrocytes that limit cell deformability have been demonstrated in COVID-19 convalescents and ME/CFS patients [79, 80]. Consequences of morpho-functional changes for peripheral oxygen homeostasis remain to be determined but diminished capillary trafficking properties and increased peripheral oxygen affinity are discussed [79, 81].
Further mechanisms underlying impairments in microcirculation may include autonomic dysfunction which may be mediated by sympathetic overactivity, autoantibodies or small fiber neuropathy [82]. Autoantibodies binding to adrenergic and muscarinic acetylcholine receptors were shown to correlate with symptoms of impaired peripheral microcirculation and cognitive impairment [83]. Also, a renin-angiotensin system dysfunction occurs as a consequence of COVID-19 and may result in a functional alteration of ACE2 favoring vasoconstriction [84].
Dysregulated immune activation imposes allostatic load
There is accumulating evidence suggesting that the etiology of microcirculatory and mitochondrial dysfunctions is, to a significant extent, induced by immunological dysregulation. Certain immune signatures indicating a dysregulated immune response to acute SARS-CoV-2 infection have been associated with the risk of developing PCC [85,86,87,88,89]. In this context, a subsequent persistence of viral antigen might be the pathophysiological link to an ongoing immune activation that distinguishes PCC patients from recovered subjects [86, 90]. Indeed, the persistence of spike protein components and viral RNA has been documented in the circulation and tissue reservoirs in a subset of PCC patients [91, 92] and directly attributed to ongoing antigen-specific cellular immune responses [86]. The latter is for instance indicated by a persistent IFN-γ secretion [87], higher levels of circulating SARS-CoV-2-specific antibodies and exhaustion of antigen-specific T cells [90]. Beyond that, high systemic levels of pro-inflammatory cytokines such as IL-1β, IL-6 and TNF-α relate to activation of coagulation pathways and metabolic disruptions [93]. Equally important, dysfunctional immune activity may also facilitate reactivation of harbored viruses that were previously checked by competent immune surveillance. Correspondingly, PCC patients demonstrate higher antibody responses against viruses such as Epstein-Barr virus [94, 95]. An explanation for a potential reduced capacity to respond to pathogens may be altered immunometabolism. Consistent with the discussed aberrant muscular energy metabolism, blood immune cells exhibit functional aberrations that may similarly alter effector functions. Specifically, compared to healthy controls, immortalized ME/CFS patient-derived lymphoblasts showed mitochondrial deficiency of ATP synthesis due to an isolated complex V inefficiency [96]. Lower ATP-linked respiration rates in PBMCs further underline this energy-generating deficiency [97]. Other studies provide evidence for a metabolic shift in favor of oxidation of fatty acids and protein degradation, as indicated by elevated levels of enzymes and transport proteins involved in these pathways [98, 99], as well as increased utilization of lipids upon activation [99].
In line with these findings, it has been proposed that constant immune activation and the fight against latent viral infections could induce a maladaptive behavioral response to limit energy allocation to processes less important to host survival, leaving no spare resources for e.g. activities of daily living [100].
Beyond that, direct pathogenic effects of the spike protein have been demonstrated. In particular, the induction of vWF, adhesion molecule and pro-inflammatory cytokine production by endothelial cells in an NF-κB and NLRP3 inflammasome-depended fashion promotes endotheliopathy and clotting pathology [101, 102]. Spike-mediated thrombogenicity is also caused by its interaction with fibrin(ogen) and prothrombin [103]. Moreover, a potential pathomechanistic role of spike persistence in a subset has been implied by a report of three PCC cases that experienced a rapid remission of symptoms after treatment with a monoclonal antibody cocktail (casirivimab/imdevimab) directed against the receptor binding domain [104].
Potential downstream effects of anaerobic metabolism
Under exercise conditions, patients with PCC and ME/CFS exhibit metabolic patterns that imply energy production through anaerobic pathways. The previously described microcirculatory impairments and mitochondrial dysfunction might be a mechanistic explanation for the disturbances in peripheral oxygen delivery and utilization.
Remarkably, the discussed metabolic alterations are characterized by elevated levels of lactate in rest and upon exercise [93, 105]. Additionally, anaerobic metabolism causes a deprivation of cellular energy sources, as pyruvate can no longer be oxidized in the TCA cycle and is thus converted to lactate at the expense of ATP that would otherwise be produced via mitochondrial respiration. As a result, local lactate acidosis and energy deprivation likely cause exercise intolerance and demand early cessation. Equally important, in conjunction with other accumulating products of mitochondrial dysfunction, lactate initiates a cascade of downstream effects. Evidence implying its significance in PEM comes for instance from an investigation that showed that ME/CFS patients with elevated lactate levels (≥ 2 mmol/L at rest) were more likely to experience severe PEM than those with normal levels [106].
Beyond that, cellular oxygen deprivation and mitochondrial dysfunction promotes the formation of reactive oxygen species (ROS) and vasodilatory tissue mediators (e.g., prostaglandins, bradykinin, adenosine) [76]. Mechanistically, this could be linked to PEM development by local and systemic immune activation, as the aforementioned substances possess diverse immunomodulatory effects. Specifically, there exists a vicious cycle between redox imbalance, inflammation, and mitochondrial dysfunction in which higher levels of ROS caused by mitochondria and eNOS induce cell damage and immune activation that in turn impair cell organelle function [107, 108]. Similarly, lactate can induce cytokine secretion, cell migration and nuclear translocation of NF-κB subunits [109]. In this context, it bears noting that physical exercise per se stimulates immunomodulation via metabolic and neuroendocrine pathways [110, 111]. From the described evidence it can be assumed that in PCC and ME/CFS, the threshold of activation is shifted in a way that activities of daily living are sufficient to trigger these pathways in some patients. Meanwhile, latent baseline immune activity and dysfunctional oxygenation reduce the regulatory window of homeostatic adaption.
The induction of PEM may include local and systemic mechanisms, reflecting that PEM has been proposed to be composed of muscle-specific fatigue and generalized systemic fatigue as two different experiences [112]. On the skeletal muscle level, the accumulation of immunoregulatory substances by the intensification of metabolic dyshomeostasis during physical activity may cause immune cell recruitment and local activation of inflammatory pathways that aggravate mitochondrial dysfunction [113]. For instance, NF-κB reduces muscle oxidative capacity [34], which may further decrease activity tolerance in the hours or days following activity. As a further consequence of hypoperfusion and mitochondrial dysfunction, the ionic homeostasis in muscles is severely impaired, leading to sodium and calcium overload and secondary muscle and mitochondrial damage [114, 115] (Fig. 1c). This mechanism can explain the development of delayed and prolonged symptom exacerbation and disease aggravation upon repeated PEM (detailed in [115]).
Neurological symptoms of PCC have been proposed to be associated with a blood–brain barrier (BBB) dysfunction that enables extravasation of blood components into the brain tissue [116]. In line with that, recent evidence demonstrated that brain fog is associated with increased BBB permeability, likely driven by systemic inflammation [117]. The spillover of cytokines and chemokines from tissues into the systemic circulation amid exertional activities may correspondingly contribute to the experience of generalized fatigue and aggravation of neurological symptoms due to a modulation of central nervous system (CNS) functions that resembles sickness behavior or overtraining syndrome [100, 118] (Fig. 1d). Accordingly, it has been reported in ME/CFS that the severity of symptom flare after moderate exercise is linked to cytokine activity [119]. Beyond that, it has been demonstrated that exosome-associated mitochondrial DNA that significantly increases after exercise in ME/CFS patients and potentially reaches the CNS by crossing a disrupted BBB stimulates cultured human microglia to secrete IL-1β [120].
Potential treatment options targeting PEM pathophysiology
Reflecting the still evolving understanding of their pathophysiology, the treatment of ME/CFS and PCC is currently limited to the management of individual symptoms. There is a paucity of causative treatment options for both conditions in general and for PEM specifically. In this context, pacing has been promoted to prevent the aggravation of bioenergetic capacities. This includes to avoid overexertion, allow adequate recovery periods, divide activities of daily living into smaller tasks that can be spread out over the day and to rest before symptoms arise [93, 121]. Beyond that, the discussed mechanisms may provide new starting points for therapeutic trials (Table 1). In particular, investigating options to improve microcirculation may prove to be pivotal to ensure adequate adaption of blood supply during physical activities. This could include the use of vasodilators and NO substrates to improve FMD as well as immunoadsorption to deplete vasoactive autoantibodies.
Just as important is the consideration of the bidirectional relationship between mitochondrial and immunometabolic alterations in pursuit of new therapeutic targets. Wang et al. demonstrated that alleviating stress to the endoplasmic reticulum decreased WASF3 and thus improved mitochondrial respiration [52]. Yet, they did not investigate how these molecular improvements related to clinical symptoms. It can be suspected that long-term improvements in oxidative capacity can only be achieved when immune activation and oxidative stress is concomitantly reduced. Hence, it may additionally be effective to look further into treatment options targeting viral reservoirs and inflammatory pathways. On the whole, several treatment candidates already proved to be effective in some regards (Table 1). However, more randomized controlled studies with clinically relevant endpoints are necessary, as case studies and case series have yielded contradictory results and do not provide sufficient evidence for individual use outside of studies.
Conclusions
In this literature review we discuss evidence that several homeostatic functions and regulatory mechanisms that are involved in physiological adaption to exercise are dysfunctional in patients experiencing PEM in PCC and ME/CFS. The accumulation of lactate, ROS, and the deprivation of cellular energy sources upon increased metabolic demand contributes significantly to lower exercise capacity. The complex dynamics of immunometabolic downstream effects may also lead to delayed and prolonged symptom exacerbations and dysregulated recovery. In particular, the disturbed metabolic homeostasis and consecutive ionic imbalance can lead to secondary muscle and mitochondrial damage and immune activation. Hence, exceeding their already reduced activity capacities enters affected patients into a recurrent and self-propagating loop. Considering the results of this review, it bears noting that we narratively synthesized and contextualized the results of multiple separate studies with different research focuses. There has not been a study that provided conclusive evidence for one disease etiology, which means that the described pathophysiological observations do not necessarily coexist. For that reason, future studies should look deeper into pathophysiological connections between herein highlighted systems, such as immunometabolic signatures that are associated with the development of PEM. Beyond that, activity prescriptions should take the pathophysiological mechanisms of PCC and ME/CFS into account to attenuate the risk of provoking PEM.
Data availability statement
No datasets were generated or analysed during the current study.
References
Chen C, Haupert SR, Zimmermann L, Shi X, Fritsche LG, Mukherjee B. Global prevalence of Post COVID-19 condition or long COVID: a meta-analysis and systematic review. J Infect Dis. 2022;6:100122.
Soriano JB, Murthy S, Marshall JC, Relan P, Diaz JV, Condition WCCDWG on P-C-19. A clinical case definition of post-COVID-19 condition by a delphi consensus. Lancet Infect Dis. 2021;S1473–3099:00703–9.
Adjaye-Gbewonyo D, Vahratian A, Perrine CG, Bertolli J. Long COVID in Adults: United States, 2022. NCHS Data Briefs No 480. 2023.
Appel KS, Nürnberger C, Bahmer T, Förster C, Polidori MC, Kohls M, et al. Definition of the Post-COVID syndrome using a symptom-based Post-COVID score in a prospective, multi-center, cross-sectoral cohort of the German National Pandemic Cohort Network (NAPKON). Infection. 2024;1–17.
Fernández-de-las-Peñas C, Palacios-Ceña D, Gómez-Mayordomo V, Florencio LL, Cuadrado ML, Plaza-Manzano G, et al. Prevalence of post-COVID-19 symptoms in hospitalized and non-hospitalized COVID-19 survivors: a systematic review and meta-analysis. Eur J Intern Med. 2021;92:55–70.
Ma Y, Deng J, Liu Q, Du M, Liu M, Liu J. Long-term consequences of asymptomatic SARS-CoV-2 infection: a systematic review and meta-analysis. Int J Environ Res Public Heal. 2023;20:1613.
Domènech-Montoliu S, Puig-Barberá J, Badenes-Marques G, Gil-Fortuño M, Orrico-Sánchez A, Pac-Sa MR, et al. Long COVID prevalence and the impact of the third SARS-CoV-2 vaccine dose: a cross-sectional analysis from the third follow-up of the Borriana Cohort, Valencia, Spain (2020–2022). 2023.
Al-Aly Z, Bowe B, Xie Y. Long COVID after breakthrough SARS-CoV-2 infection. Nat Med. 2022;28:1–7.
Jassat W, Mudara C, Vika C, Welch R, Arendse T, Dryden M, et al. A cohort study of post-COVID-19 condition across the Beta, Delta, and Omicron waves in South Africa: 6-month follow-up of hospitalized and nonhospitalized participants. Int J Infect Dis. 2023;128:102–11.
Liao X, Guan Y, Liao Q, Ma Z, Zhang L, Dong J, et al. Long-term sequelae of different COVID-19 variants: the original strain versus the Omicron variant. Global Heal Medicine. 2022;4:322–6.
Antonelli M, Pujol JC, Spector TD, Ourselin S, Steves CJ. Risk of long COVID associated with delta versus omicron variants of SARS-CoV-2. Lancet. 2022;399:2263–4.
Hopff SM, Appel KS, Miljukov O, Schneider J, Addo MM, Bals R, et al. Comparison of post-COVID-19 symptoms in patients infected with the SARS-CoV-2 variants delta and omicron—results of the Cross-Sectoral Platform of the German National Pandemic Cohort Network (NAPKON-SUEP). Infection. 2024. https://doi.org/10.1007/s15010-024-02270-5.
Fernández-de-las-Peñas C, Torres-Macho J, Catahay JA, Macasaet R, Velasco JV, Macapagal S, et al. Is antiviral treatment at the acute phase of COVID-19 effective for decreasing the risk of long-COVID? A systematic review. Infection. 2024;52:43–58.
Seeßle J, Waterboer T, Hippchen T, Simon J, Kirchner M, Lim A, et al. Persistent symptoms in adult patients 1 year after coronavirus disease 2019 (COVID-19): a prospective cohort study. Clin Infect Dis Official Publ Infect Dis Soc Am. 2021;74:1191–8.
Davis HE, Assaf GS, McCorkell L, Wei H, Low RJ, Re’em Y, et al. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. Eclinicalmedicine. 2021;38:101019.
Hartung TJ, Neumann C, Bahmer T, Chaplinskaya-Sobol I, Endres M, Geritz J, et al. Fatigue and cognitive impairment after COVID-19: a prospective multicentre study. eClinicalMedicine. 2022;53:101651.
Hartung TJ, Bahmer T, Chaplinskaya-Sobol I, Deckert J, Endres M, Franzpötter K, et al. Predictors of non-recovery from fatigue and cognitive deficits after COVID-19: a prospective, longitudinal, population-based study. eClinicalMedicine. 2024;69:102456.
Akbarialiabad H, Taghrir MH, Abdollahi A, Ghahramani N, Kumar M, Paydar S, et al. Long COVID, a comprehensive systematic scoping review. Infection. 2021;49:1–24.
Twomey R, DeMars J, Franklin K, Culos-Reed SN, Weatherald J, Wrightson JG. Chronic fatigue and postexertional malaise in people living with long COVID: an observational study. Phys Ther 2022.
Cotler J, Holtzman C, Dudun C, Jason LA. A brief questionnaire to assess post-exertional malaise. Diagnostics. 2018;8:66.
Jason LA, Dorri JA. ME/CFS and post-exertional malaise among patients with long COVID. Neurol Int. 2022;15:1–11.
Bonilla H, Quach TC, Tiwari A, Bonilla AE, Miglis M, Yang PC, et al. Myalgic encephalomyelitis/chronic fatigue syndrome is common in post-acute sequelae of SARS-CoV-2 infection (PASC): results from a post-COVID-19 multidisciplinary clinic. Front Neurol. 2023;14:1090747.
Reuken PA, Besteher B, Finke K, Fischer A, Holl A, Katzer K, et al. Longterm course of neuropsychological symptoms and ME/CFS after SARS-CoV-2-infection: a prospective registry study. Eur Arch Psychiatry Clin Neurosci. 2023. https://doi.org/10.1007/s00406-023-01661-3.
Kedor C, Freitag H, Meyer-Arndt L, Wittke K, Hanitsch LG, Zoller T, et al. A prospective observational study of post-COVID-19 chronic fatigue syndrome following the first pandemic wave in Germany and biomarkers associated with symptom severity. Nat Commun. 2022;13:5104.
Choutka J, Jansari V, Hornig M, Iwasaki A. Unexplained post-acute infection syndromes. Nat Med. 2022;28:911–23.
Unger ER, Lin J-MS, Wisk LE, Yu H, L’Hommedieu M, Lavretsky H, et al. Myalgic encephalomyelitis/chronic fatigue syndrome after SARS-CoV-2 infection. JAMA Netw Open. 2024;7:e2423555.
Hartle M, Bateman L, Vernon SD. Dissecting the nature of post-exertional malaise. Fatigue Biomed Heal Behav. 2021;9:1–12.
Holtzman CS, Bhatia S, Cotler J, Jason LA. Assessment of post-exertional malaise (PEM) in patients with myalgic encephalomyelitis (ME) and chronic fatigue syndrome (CFS): a patient-driven survey. Diagnostics. 2019;9:26.
Vernon SD, Hartle M, Sullivan K, Bell J, Abbaszadeh S, Unutmaz D, et al. Post-exertional malaise among people with long COVID compared to myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Work. 2023;74:1–8.
Chu L, Valencia IJ, Garvert DW, Montoya JG. Deconstructing post-exertional malaise in myalgic encephalomyelitis/ chronic fatigue syndrome: a patient-centered, cross-sectional survey. PLoS One. 2018;13: e0197811.
Lim E-J, Kang E-B, Jang E-S, Son C-G. The prospects of the two-day cardiopulmonary exercise test (CPET) in ME/CFS patients: a meta-analysis. J Clin Med. 2020;9:4040.
Jäkel B, Kedor C, Grabowski P, Wittke K, Thiel S, Scherbakov N, et al. Hand grip strength and fatigability: correlation with clinical parameters and diagnostic suitability in ME/CFS. J Transl Med. 2021;19:159.
Herold F, Müller P, Gronwald T, Müller NG. Dose-response matters! – a perspective on the exercise prescription in exercise-cognition research. Front Psychol. 2019;10:2338.
Colosio M, Brocca L, Gatti M, Neri M, Crea E, Cadile F, et al. Structural and functional impairments of skeletal muscle in patients with post-acute sequelae of SARS-CoV-2 infection. J Appl Physiol. 2023. https://doi.org/10.1152/japplphysiol.00158.2023.
de Boer E, Petrache I, Goldstein NM, Olin JT, Keith RC, Modena B, et al. Decreased fatty acid oxidation and altered lactate production during exercise in patients with post-acute COVID-19 syndrome. Am J Resp Crit Care. 2021;205:126–9.
Rinaldo RF, Mondoni M, Parazzini EM, Pitari F, Brambilla E, Luraschi S, et al. Deconditioning as main mechanism of impaired exercise response in COVID-19 survivors. Eur Respir J. 2021;58:2100870.
Skjørten I, Ankerstjerne OAW, Trebinjac D, Brønstad E, Rasch-Halvorsen Ø, Einvik G, et al. Cardiopulmonary exercise capacity and limitations 3 months after COVID-19 hospitalisation. Eur Respir J. 2021;58:2100996.
Durstenfeld MS, Sun K, Tahir P, Peluso MJ, Deeks SG, Aras MA, et al. Use of cardiopulmonary exercise testing to evaluate long COVID-19 symptoms in adults. Jama Netw Open. 2022;5: e2236057.
Naeije R, Caravita S. Phenotyping long COVID. Eur Respir J. 2021;58:2101763.
Joseph P, Singh I. Post-acute sequelae of SARS-CoV-2 more than deconditioning. Chest. 2023;164:583–4.
Baratto C, Caravita S, Faini A, Perego GB, Senni M, Badano LP, et al. Impact of COVID-19 on exercise pathophysiology: a combined cardiopulmonary and echocardiographic exercise study. J Appl Physiol. 2021;130:1470–8.
Raman B, Bluemke DA, Lüscher TF, Neubauer S. Long COVID: post-acute sequelae of COVID-19 with a cardiovascular focus. Eur Heart J. 2022;43:1157–72.
Gremme Y, Derlien S, Katzer K, Reuken PA, Stallmach A, Lewejohann J-C, et al. Visualizing exertional dyspnea in a post-COVID patient using electrical impedance tomography. Infection. 2023;51:1841–5.
Singh I, Joseph P, Heerdt PM, Cullinan M, Lutchmansingh DD, Gulati M, et al. Persistent exertional intolerance after COVID-19: Insights from invasive cardiopulmonary exercise testing. Chest. 2021;161:54–63.
Singh I, Leitner BP, Wang Y, Zhang H, Joseph P, Lutchmansingh DD, et al. Proteomic profiling demonstrates inflammatory and endotheliopathy signatures associated with impaired cardiopulmonary exercise hemodynamic profile in Post Acute Sequelae of SARS-CoV-2 infection (PASC) syndrome. Pulm Circ. 2023;13: e12220.
Kahn PA, Joseph P, Heerdt PM, Singh I. Differential cardiopulmonary haemodynamic phenotypes in PASC-related exercise intolerance. ERJ Open Res. 2024;10:00714–2023.
Joseph P, Singh I, Oliveira R, Capone CA, Mullen MP, Cook DB, et al. Exercise pathophysiology in myalgic encephalomyelitis/chronic fatigue syndrome and postacute sequelae of SARS-CoV-2 more in common than not? Chest. 2023;164:717–26.
Appelman B, Charlton BT, Goulding RP, Kerkhoff TJ, Breedveld EA, Noort W, et al. Muscle abnormalities worsen after post-exertional malaise in long COVID. Nat Commun. 2024;15:17.
Aschman T, Wyler E, Baum O, Hentschel A, Legler F, Preusse C, et al. Post-COVID syndrome is associated with capillary alterations, macrophage infiltration and distinct transcriptomic signatures in skeletal muscles. 2023;21:e68.
Bizjak DA, Ohmayer B, Buhl JL, Schneider EM, Walther P, Calzia E, et al. Functional and morphological differences of muscle mitochondria in chronic fatigue syndrome and Post-COVID syndrome. Int J Mol Sci. 2024;25:1675.
Hejbøl EK, Harbo T, Agergaard J, Madsen LB, Pedersen TH, Østergaard LJ, et al. Myopathy as a cause of fatigue in long-term post-COVID-19 symptoms: evidence of skeletal muscle histopathology. Eur J Neurol. 2022;29:2832–41.
Wang P, Ma J, Kim Y-C, Son AY, Syed AM, Liu C, et al. WASF3 disrupts mitochondrial respiration and may mediate exercise intolerance in myalgic encephalomyelitis/chronic fatigue syndrome. Proc Natl Acad Sci. 2023;120: e2302738120.
Guntur VP, Nemkov T, de Boer E, Mohning MP, Baraghoshi D, Cendali FI, et al. Signatures of mitochondrial dysfunction and impaired fatty acid metabolism in plasma of patients with post-acute sequelae of COVID-19 (PASC). Metabolites. 2022;12:1026.
Helbing DL, Dommaschk E-M, Danyeli LV, Liepinsh E, Refisch A, Sen ZD, et al. Conceptual foundations of acetylcarnitine supplementation in neuropsychiatric long COVID syndrome: a narrative review. Eur Arch Psychiatry Clin Neurosci. 2024. https://doi.org/10.1007/s00406-023-01734-3.
Burtscher J, Cappellano G, Omori A, Koshiba T, Millet GP. Mitochondria: In the cross fire of SARS-CoV-2 and immunity. Iscience. 2020;23: 101631.
Schäfer H, Teschler M, Mooren FC, Schmitz B. Altered tissue oxygenation in patients with post COVID-19 syndrome. Microvasc Res. 2023;148: 104551.
Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in COVID-19. New Engl J Med. 2020;383:120–8.
Charfeddine S, Amor HIH, Jdidi J, Torjmen S, Kraiem S, Hammami R, et al. Long COVID 19 syndrome: is it related to microcirculation and endothelial dysfunction? Insights from TUN-EndCOV study. Frontiers Cardiovasc Medicine. 2021;8: 745758.
Nicolai L, Kaiser R, Stark K. Thromboinflammation in long COVID—the elusive key to postinfection sequelae? J Thromb Haemost. 2023;21:2020–31.
Poyatos P, Luque N, Sabater G, Eizaguirre S, Bonnin M, Orriols R, et al. Endothelial dysfunction and cardiovascular risk in post-COVID-19 patients after 6- and 12-months SARS-CoV-2 infection. Infection. 2024;52:1269–85.
Ambrosino P, Calcaterra I, Molino A, Moretta P, Lupoli R, Spedicato GA, et al. Persistent endothelial dysfunction in post-acute COVID-19 syndrome: a case-control study. Biomed. 2021;9:957.
Ambrosino P, Parrella P, Formisano R, Perrotta G, D’Anna SE, Mosella M, et al. Cardiopulmonary exercise performance and endothelial function in convalescent COVID-19 patients. J Clin Medicine. 2022;11:1452.
Prasannan N, Heightman M, Hillman T, Wall E, Bell R, Kessler A, et al. Impaired exercise capacity in post–COVID-19 syndrome: the role of VWF-ADAMTS13 axis. Blood Adv. 2022;6:4041–8.
Chien C, Heine J, Khalil A, Schlenker L, Hartung TJ, Boesl F, et al. Altered brain perfusion and oxygen levels relate to sleepiness and attention in post-COVID syndrome. Ann Clin Transl Neurol. 2024. https://doi.org/10.1002/acn3.52121.
López-Hernández Y, Monárrez-Espino J, López DAG, Zheng J, Borrego JC, Torres-Calzada C, et al. The plasma metabolome of long COVID patients two years after infection. Sci Rep. 2023;13:12420.
Calvani R, Gervasoni J, Picca A, Ciciarello F, Galluzzo V, Coelho-Júnior HJ, et al. Effects of l-arginine plus Vitamin C supplementation on l-arginine metabolism in adults with long COVID: secondary analysis of a randomized clinical trial. Int J Mol Sci. 2023;24:5078.
Bertinat R, Villalobos-Labra R, Hofmann L, Blauensteiner J, Sepúlveda N, Westermeier F. Decreased no production in endothelial cells exposed to plasma from ME/CFS patients. Vasc Pharmacol. 2022;143: 106953.
Tosato M, Calvani R, Picca A, Ciciarello F, Galluzzo V, Coelho-Júnior HJ, et al. Effects of l-arginine plus Vitamin C supplementation on physical performance, endothelial function, and persistent fatigue in adults with Long COVID: a single-blind randomized controlled trial. Nutrients. 2022;14:4984.
Izzo R, Trimarco V, Mone P, Aloè T, Marzani MC, Diana A, et al. Combining L-arginine with vitamin C improves long-COVID symptoms: The LINCOLN survey. Pharmacol Res. 2022;183: 106360.
Flaskamp L, Roubal C, Uddin S, Sotzny F, Kedor C, Bauer S, et al. Serum of post-COVID-19 syndrome patients with or without ME/CFS differentially affects endothelial cell function in vitro. Cells. 2022;11:2376.
Aschman T, Wyler E, Baum O, Hentschel A, Rust R, Legler F, et al. Post-COVID exercise intolerance is associated with capillary alterations and immune dysregulations in skeletal muscles. Acta Neuropathol Commun. 2023;11:193.
Turner S, Khan MA, Putrino D, Woodcock A, Kell DB, Pretorius E. Long COVID: pathophysiological factors and abnormalities of coagulation. Trends Endocrinol Metab. 2023;34:321–44.
Pretorius E, Vlok M, Venter C, Bezuidenhout JA, Laubscher GJ, Steenkamp J, et al. Persistent clotting protein pathology in Long COVID/Post-Acute Sequelae of COVID-19 (PASC) is accompanied by increased levels of antiplasmin. Cardiovasc Diabetol. 2021;20:172.
Constantinescu-Bercu A, Kessler A, de Groot R, Dragunaite B, Heightman M, Hillman T, et al. Analysis of thrombogenicity under flow reveals new insights into the prothrombotic state of patients with post-COVID syndrome. J Thromb Haemost. 2023;21:94–100.
Giloteaux L, Glass KA, Germain A, Franconi CJ, Zhang S, Hanson MR. Dysregulation of extracellular vesicle protein cargo in female myalgic encephalomyelitis/chronic fatigue syndrome cases and sedentary controls in response to maximal exercise. J Extracell Vesicles. 2024;13:12403.
Wirth KJ, Löhn M. Microvascular capillary and precapillary cardiovascular disturbances strongly interact to severely affect tissue perfusion and mitochondrial function in myalgic encephalomyelitis/chronic fatigue syndrome evolving from the post COVID-19 syndrome. Medicina. 2024;60:194.
Kell DB, Pretorius E. The potential role of ischaemia–reperfusion injury in chronic, relapsing diseases such as rheumatoid arthritis, Long COVID, and ME/CFS: evidence, mechanisms, and therapeutic implications. Biochem J. 2022;479:1653–708.
Makris KI, Nella AA, Zhu Z, Swanson SA, Casale GP, Gutti TL, et al. Mitochondriopathy of peripheral arterial disease. Vascular. 2007;15:336–43.
Grau M, Ibershoff L, Zacher J, Bros J, Tomschi F, Diebold KF, et al. Even patients with mild COVID-19 symptoms after SARS-CoV-2 infection show prolonged altered red blood cell morphology and rheological parameters. J Cell Mol Med. 2022. https://doi.org/10.1111/jcmm.17320.
Nunes JM, Kell DB, Pretorius E. Cardiovascular and haematological pathology in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS): a role for viruses. Blood Rev. 2023;60: 101075.
Böning D, Kuebler WM, Vogel D, Bloch W. The oxygen dissociation curve of blood in COVID-19–an update. Front Med. 2023;10:1098547.
Joseph P, Arevalo C, Oliveira RKF, Faria-Urbina M, Felsenstein D, Oaklander AL, et al. Insights from invasive cardiopulmonary exercise testing of patients with myalgic encephalomyelitis/chronic fatigue syndrome. Chest. 2021;160:642–51.
Sotzny F, Blanco J, Capelli E, Castro-Marrero J, Steiner S, Murovska M, et al. Myalgic encephalomyelitis/chronic fatigue syndrome – evidence for an autoimmune disease. Autoimmun Rev. 2018;17:601–9.
Fajloun Z, Khattar ZA, Kovacic H, Legros C, Sabatier J-M. Why do athletes develop very severe or fatal forms of COVID after intense exercise following SARS-CoV-2 infection or anti-COVID vaccination? Infect Disord - Drug Targets. 2023;23:E110123212563.
Su Y, Yuan D, Chen DG, Ng RH, Wang K, Choi J, et al. Multiple early factors anticipate post-acute COVID-19 sequelae. Cell. 2022;185:881-895.e20.
Files JK, Sarkar S, Fram. TR, Boppana S, Sterrett S, Qin K, et al. Duration of post-COVID-19 symptoms are associated with sustained SARS-CoV-2 specific immune responses. JCI Insight. 2021.
Krishna BA, Lim EY, Metaxaki M, Jackson S, Mactavous L, BioResource N, et al. Spontaneous, persistent, T cell–dependent IFN-γ release in patients who progress to Long Covid. Sci Adv. 2024;10:eadie379.
Sbierski-Kind J, Schlickeiser S, Feldmann S, Ober V, Grüner E, Pleimelding C, et al. Persistent immune abnormalities discriminate post-COVID syndrome from convalescence. Infection. 2024;52:1087–97.
Pink I, Hennigs JK, Ruhl L, Sauer A, Boblitz L, Huwe M, et al. Blood T cell phenotypes correlate with fatigue severity in post-acute sequelae of COVID-19. Infection. 2024;52:513–24.
Yin K, Peluso MJ, Luo X, Thomas R, Shin M-G, Neidleman J, et al. Long COVID manifests with T cell dysregulation, inflammation and an uncoordinated adaptive immune response to SARS-CoV-2. Nat Immunol. 2024;25:218–25.
Swank Z, Senussi Y, Manickas-Hill Z, Yu XG, Li JZ, Alter G, et al. Persistent circulating severe acute respiratory syndrome coronavirus 2 spike is associated with post-acute coronavirus disease 2019 sequelae. Clin Infect Dis. 2022;76:e487–90.
Craddock V, Mahajan A, Spikes L, Krishnamachary B, Ram AK, Kumar A, et al. Persistent circulation of soluble and extracellular vesicle-linked Spike protein in individuals with postacute sequelae of COVID-19. J Méd Virol. 2023;95: e28568.
Haunhorst S, Bloch W, Wagner H, Ellert C, Krüger K, Vilser DC, et al. Long COVID: a narrative review of the clinical aftermaths of COVID-19 with a focus on the putative pathophysiology and aspects of physical activity. Oxf Open Immunol. 2022;3:iqac006.
Gyöngyösi M, Lukovic D, Mester-Tonczar J, Zlabinger K, Einzinger P, Spannbauer A, et al. Effect of monovalent COVID-19 vaccines on viral interference between SARS-CoV-2 and several DNA viruses in patients with long-COVID syndrome. NPJ Vaccines. 2023;8:145.
Klein J, Wood J, Jaycox JR, Dhodapkar RM, Lu P, Gehlhausen JR, et al. Distinguishing features of long COVID identified through immune profiling. Nature. 2023;623:139–48.
Missailidis D, Annesley SJ, Allan CY, Sanislav O, Lidbury BA, Lewis DP, et al. An isolated complex V inefficiency and dysregulated mitochondrial function in immortalized lymphocytes from ME/CFS patients. Int J Mol Sci. 2020;21:1074.
Tomas C, Elson JL, Strassheim V, Newton JL, Walker M. The effect of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) severity on cellular bioenergetic function. PLoS One. 2020;15: e0231136.
Missailidis D, Sanislav O, Allan CY, Smith PK, Annesley SJ, Fisher PR. Dysregulated provision of oxidisable substrates to the mitochondria in ME/CFS lymphoblasts. Int J Mol Sci. 2021;22:2046.
Maya J, Leddy SM, Gottschalk CG, Peterson DL, Hanson MR. Altered fatty acid oxidation in lymphocyte populations of myalgic encephalomyelitis/chronic fatigue syndrome. Int J Mol Sci. 2023;24:2010.
Raizen DM, Mullington J, Anaclet C, Clarke G, Critchley H, Dantzer R, et al. Beyond the symptom: the biology of fatigue. Sleep. 2023;46:1–13.
Villacampa A, Alfaro E, Morales C, Díaz-García E, López-Fernández C, Bartha JL, et al. SARS-CoV-2 S protein activates NLRP3 inflammasome and deregulates coagulation factors in endothelial and immune cells. Cell Commun Signal. 2024;22:38.
Montezano AC, Camargo LL, Mary S, Neves KB, Rios FJ, Stein R, et al. SARS-CoV-2 spike protein induces endothelial inflammation via ACE2 independently of viral replication. Sci Rep. 2023;13:14086.
Grobbelaar LM, Venter C, Vlok M, Ngoepe M, Laubscher GJ, Lourens PJ, et al. SARS-CoV-2 spike protein S1 induces fibrin(ogen) resistant to fibrinolysis: implications for microclot formation in COVID-19. 2021. Biosci Rep. https://doi.org/10.1042/BSR20210611.
Scheppke KA, Pepe PE, Jui J, Crowe RP, Scheppke EK, Klimas NG, et al. Remission of severe forms of long COVID following monoclonal antibody (MCA) infusions: a report of signal index cases and call for targeted research. Am J Emerg Med. 2024;75:122–7.
Berezhnoy G, Bissinger R, Liu A, Cannet C, Schäfer H, Kienzle K, et al. Maintained imbalance of triglycerides, apolipoproteins, energy metabolites and cytokines in long-term COVID-19 syndrome patients. Front Immunol. 2023;14:1144224.
Ghali A, Lacout C, Ghali M, Gury A, Beucher A-B, Lozac’h P, et al. Elevated blood lactate in resting conditions correlate with post-exertional malaise severity in patients with Myalgic encephalomyelitis/Chronic fatigue syndrome. Sci Rep. 2019;9:18817.
Paul BD, Lemle MD, Komaroff AL, Snyder SH. Redox imbalance links COVID-19 and myalgic encephalomyelitis/chronic fatigue syndrome. Proc National Acad Sci. 2021;118: e2024358118.
Walker M, Hall K, Peppercorn K, Tate W. The significance of oxidative stress in the pathophysiology of long COVID and myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Méd Res Arch. 2022;10.
McGarry T, Biniecka M, Veale DJ, Fearon U. Hypoxia, oxidative stress and inflammation. Free Radic Biol Med. 2018;125:15–24.
Haunhorst S, Bloch W, Ringleb M, Fennen L, Wagner H, Gabriel HHW, et al. Acute effects of heavy resistance exercise on biomarkers of neuroendocrine-immune regulation in healthy adults: a systematic review. Exerc Immunol Rev. 2022;28:36–52.
Ringleb M, Javelle F, Haunhorst S, Bloch W, Fennen L, Baumgart S, et al. Beyond muscles: Investigating immunoregulatory myokines in acute resistance exercise – a systematic review and meta-analysis. FASEB J. 2024;38: e23596.
McManimen SL, Sunnquist ML, Jason LA. Deconstructing post-exertional malaise: an exploratory factor analysis. J Heal Psychol. 2019;24:188–98.
Morris G, Maes M. Mitochondrial dysfunctions in myalgic encephalomyelitis/chronic fatigue syndrome explained by activated immuno-inflammatory, oxidative and nitrosative stress pathways. Metab Brain Dis. 2014;29:19–36.
Petter E, Scheibenbogen C, Linz P, Stehning C, Wirth K, Kuehne T, et al. Muscle sodium content in patients with myalgic encephalomyelitis/chronic fatigue syndrome. J Transl Med. 2022;20:580.
Wirth KJ, Scheibenbogen C. Pathophysiology of skeletal muscle disturbances in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). J Transl Med. 2021;19:162.
Monje M, Iwasaki A. The neurobiology of long COVID. Neuron. 2022;110:3484–96.
Greene C, Connolly R, Brennan D, Laffan A, O’Keeffe E, Zaporojan L, et al. Blood–brain barrier disruption and sustained systemic inflammation in individuals with long COVID-associated cognitive impairment. Nat Neurosci. 2024;27:421–32.
Low RN, Low RJ, Akrami A. A review of cytokine-based pathophysiology of Long COVID symptoms. Front Med. 2023;10:1011936.
White AT, Light AR, Hughen RW, Bateman L, Martins TB, Hill HR, et al. Severity of symptom flare after moderate exercise is linked to cytokine activity in chronic fatigue syndrome. Psychophysiology. 2010;47:615–24.
Tsilioni I, Natelson B, Theoharides TC. Exosome-associated mitochondrial DNA from patients with myalgic encephalomyelitis/chronic fatigue syndrome stimulates human microglia to release IL-1β. Eur J Neurosci. 2022;56:5784–94.
Décary S, Gaboury I, Poirier S, Garcia C, Simpson S, Bull M, et al. Humility and acceptance: Working within our limits with long COVID and myalgic encephalomyelitis/chronic fatigue syndrome. J Orthop Sport Phys. 2021;51:197–200.
Negro RWD, Turco P, Povero M. Nebivolol: an effective option against long-lasting dyspnoea following COVID-19 pneumonia - a pivotal double-blind, cross-over controlled study. Multidiscip Respir Med. 2022;17:886.
Pretorius E, Venter C, Laubscher GJ, Kotze MJ, Oladejo SO, Watson LR, et al. Prevalence of symptoms, comorbidities, fibrin amyloid microclots and platelet pathology in individuals with Long COVID/Post-Acute Sequelae of COVID-19 (PASC). Cardiovasc Diabetol. 2022;21:148.
Stein E, Heindrich C, Wittke K, Kedor C, Rust R, Freitag H, et al. Efficacy of repeat immunoadsorption in post-COVID ME/CFS patients with elevated Β2-adrenergic receptor autoantibodies: a prospective cohort study. 2024.
Giszas B, Reuken PA, Katzer K, Kiehntopf M, Schmerler D, Rummler S, et al. Immunoadsorption to treat patients with severe post‐COVID syndrome. Ther Apher Dial. 2023.
Rigo S, Urechie V, Diedrich A, Okamoto LE, Biaggioni I, Shibao CA. Impaired parasympathetic function in long-COVID postural orthostatic tachycardia syndrome – a case-control study. Bioelectron Med. 2023;9:19.
Glynne P, Tahmasebi N, Gant V, Gupta R. Long COVID following mild SARS-CoV-2 infection: characteristic T cell alterations and response to antihistamines. J Invest Med. 2022;70:61–7.
Strayer DR, Young D, Mitchell WM. Effect of disease duration in a randomized Phase III trial of rintatolimod, an immune modulator for myalgic encephalomyelitis/chronic fatigue syndrome. PLoS One. 2020;15: e0240403.
Abani O, Abbas A, Abbas F, Abbas J, Abbas K, Abbas M, et al. Baricitinib in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial and updated meta-analysis. Lancet. 2022;400:359–68.
Utrero-Rico A, Ruiz-Ruigómez M, Laguna-Goya R, Arrieta-Ortubay E, Chivite-Lacaba M, González-Cuadrado C, et al. A short corticosteroid course reduces symptoms and immunological alterations underlying long-COVID. Biomed. 2021;9:1540.
Castro-Marrero J, Domingo JC, Cordobilla B, Ferrer R, Giralt M, Sanmartín-Sentañes R, et al. Does coenzyme Q10 plus selenium supplementation ameliorate clinical outcomes by modulating oxidative stress and inflammation in individuals with myalgic encephalomyelitis/chronic fatigue syndrome? Antioxid Redox Signal. 2022;36:729–39.
Castro-Marrero J, Segundo MJ, Lacasa M, Martinez-Martinez A, Sentañes RS, Alegre-Martin J. Effect of dietary coenzyme Q10 plus NADH supplementation on fatigue perception and health-related quality of life in individuals with myalgic encephalomyelitis/chronic fatigue syndrome: a prospective, randomized, double-blind. Placebo-Controlled Trial Nutrients. 2021;13:2658.
Rostami S, Alavi SM, Daghagheleh R, Maraghi E, Hosseini SA. A randomized clinical trial investigating the impact of magnesium supplementation on clinical and biochemical measures in COVID-19 patients. Virol J. 2024;21:91.
Funding
Open Access funding enabled and organized by Projekt DEAL. No funding was received to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Simon Haunhorst and Christian Puta had the idea for the article and wrote the first draft of the manuscript. Carmen Scheibenbogen, Martina Seifert, Carsten Finke, Konrad Aden, Wilhelm Bloch, Phillipp Reuken, Diana Dudziak and Andreas Stallmach read and edited previous versions of the manuscript. All authors provided critical feedback and contributed to the final manuscript. Simon Haunhorst prepared the figure for publication.
Corresponding author
Ethics declarations
Competing interests
The authors have no competing interests to declare that are relevant to the content of this article.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Haunhorst, S., Dudziak, D., Scheibenbogen, C. et al. Towards an understanding of physical activity-induced post-exertional malaise: Insights into microvascular alterations and immunometabolic interactions in post-COVID condition and myalgic encephalomyelitis/chronic fatigue syndrome. Infection (2024). https://doi.org/10.1007/s15010-024-02386-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s15010-024-02386-8