Abstract
Purpose
There is evidence that lower activity of the RAF/MEK/ERK network is associated with positive outcomes in mild and moderate courses of COVID-19. The effect of this cascade in COVID-19 sepsis is still undetermined. Therefore, we tested the hypothesis that activity of the RAF/MEK/ERK network in COVID-19-induced sepsis is associated with an impact on 30-day survival.
Methods
We used biomaterial from 81 prospectively recruited patients from the multicentric CovidDataNet.NRW-study cohort (German clinical trial registry: DRKS00026184) with their collected medical history, vital signs, laboratory parameters, microbiological findings and patient outcome. ERK activity was measured by evaluating ERK phosphorylation using a Proximity Ligation Assay.
Results
An increased ERK activity at 4 days after diagnosis of COVID-19-induced sepsis was associated with a more than threefold increased chance of survival in an adjusted Cox regression model. ERK activity was independent of other confounders such as Charlson Comorbidity Index or SOFA score (HR 0.28, 95% CI 0.10–0.84, p = 0.02).
Conclusion
High activity of the RAF/MEK/ERK network during the course of COVID-19 sepsis is a protective factor and may indicate recovery of the immune system. Further studies are needed to confirm these results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With the onset of the COVID-19 pandemic, a new disease pattern emerged [1]. While the majority of patients had asymptomatic to mild illness [2, 3], some patients experienced severe progressions associated with high mortality [4, 5]. The development of critical illness was characterized by an onset of acute respiratory distress syndrome (ARDS) and multiorgan failure [6] that fulfilled the criteria for sepsis [7]. Why some patients develop critical illness and succumb to COVID-19 induced sepsis and others present only mild symptoms is still not well understood and various signaling networks have been investigated to this end [8, 9]. A well-studied and frequently utilized approach by other viruses is the RAF/MEK/ERK network (rapidly accelerated fibrosarcoma/mitogen-activated protein kinase/extracellular signal-regulated kinase network) [10,11,12,13]. For COVID-19, exploitation of this specific pathway by the SARS-CoV-2 virus has also been identified for the early phase of infection, leading to increased viral replication [14]. Further studies showed that MEK inhibitors, such as those being tested against the influenza virus [15], can also alleviate viral replication of SARS-CoV-2 and subsequent cytokine release, which is considered to be a major driver of critical disease progression [16,17,18]. To date, it is unclear whether the suggested protective effects of a suppressed RAF/MEK/ERK activity are also applicable to the later phase of COVID-19-induced sepsis in humans [19, 20]. With the persistently poor prognosis of critically ill COVID-19 patients, this would provide an opportunity for a potential therapeutic approach. Therefore, we tested the hypothesis that activity of the RAF/MEK/ERK network in COVID-19-induced sepsis is associated with an impact on 30-day survival.
Methods
Study design
The multicentric CovidDataNet.NRW study (German Clinical Trial Registry No. DRKS00026184) prospectively enrolled patients with sepsis because of a COVID-19 infection, meeting the sepsis-3 criteria. These patients were recruited from the Intensive Care Units (ICUs) of three distinct university hospitals situated in the German state of North Rhine-Westphalia. Ethical approval for this study was granted by the Ethics Committee of the Medical Faculty of Ruhr-University Bochum (Registration No. 18–6606–BR) or the relevant ethics committee at each respective study center. Patients were recruited between March 1, 2020 and October 30, 2022.
This study encompassed adult patients diagnosed with COVID-19-induced sepsis within the preceding 36 h, in accordance with the current sepsis-3 definition, which requires a suspected or proven infection along with a Sequential Organ Failure Assessment (SOFA) score increase of at least two points. The patient cohort comprised a mix of surgical and medical cases admitted to the ICU. Exclusion criteria included: (1) age less than 18 years at the time of ICU admission, (2) withdrawal or withholding of consent, and (3) discontinuation of treatment. Patients with an unknown 30-day survival status were excluded from subsequent analysis.
Clinical data and patient characteristics
Electronic medical data, including vital signs, laboratory results, point-of-care diagnostics, demographic information, and the duration of ICU or hospital stays, were meticulously captured within a comprehensive database using CentraXX software, developed by Kairos GmbH in Bochum, Germany. This data collection process adhered to the pseudonymization procedures mandated by the ethics committee.
In cases of missing data, a qualified physician at each respective clinic conducted individual patient record investigations. Where deemed appropriate, data from ± 12 h of sepsis onset were included to ensure completeness. The SOFA scores were manually calculated by experienced physicians at each recruitment site. SARS-CoV-2 PCR Test were performed via nasopharyngeal swaps by the attending physicians and cycling time values (CT value) were reported. The number of cycles was limited to 40. If no viral RNA was detected by that time, the patient was considered negative. Throughout their ICU stay, each patient underwent comprehensive microbiological monitoring, which included surface swabs, tracheal secretions, urine cultures, and bronchial secretions or bronchoalveolar lavage where feasible. If a pathogen was detected and deemed in need of treatment by the attending physician (i.e., with no evidence of contamination or colonization), the patient was classified as superinfected. The findings were stratified according to the day of sample collection (during the overall ICU stay versus after day 4).
Extraction of peripheral blood mononuclear cells (PBMCs)
Blood was drawn from the patients at study inclusion and after 4, 8 and 14 days. Peripheral blood mononuclear cell (PBMCs) were isolated from EDTA stabilized blood samples using Ficoll density gradient centrifugation (GE Healthcare Europe, Freiburg, Germany). The phase containing PBMCs was collected and washed with PBS. Subsequent to erythrocyte lysis, and PBS (phosphate buffered saline) washing, the PBMCs were stored at – 196 °C until use. Upon thawing, cells were counted, spun onto microscopic slides using a cytospin (Cellspin II, Tharmac, Wiesbaden, Germany), and then fixed using 4% formaldehyde solution.
Proximity ligation assay for pERK
The Proximity Ligation Assay (PLA) to assess the phosphorylation level of ERK was performed as described previously [21]. Briefly, PBMCs were permeabilized using 1% Triton-X in PBS. Partial unfolding of the target proteins was done by incubating the slides with 1% SDS in PBS. After subsequent washing slides were blocked using the Duolink Block (Sigma). Primary antibodies against ERK (1:100, #4696, Cell Signaling Technology, Danvers, MA) and pERK (1:100, #4370, Cell Signaling Technology) were incubated at 4 °C over night. After another round of washing, we incubated the slides with secondary proximity probes (anti-mouse and anti-rabbit, NaveniFlex 100 MR, Navinci Diagnostics, Uppsala, Sweden) for 1h at 37 °C. The Unfold PLA reaction was conducted as per manufacturers recommendations (Navinci Diagnostics). After mounting the slides with slow fade antifade reagent (S36940, Thermo Fisher) and counterstaining the nuclei with DAPI we evaluated the pERK level using a IX51 Microscope (Zeiss, Germany).
Image analysis
Analysis of the images was undertaken using FIJI and the Cell Profiler software. First, maximal intensity projections were performed and channels were merged using FIJI. The images were then imported to Cell Profiler where the modules primary object identification, secondary object identification and relate object modules were used to quantify the PLA signals per cell. As we did no cytoplasmic counterstain, we estimated a cell to be of 30 pixel diameter around the nucleus. Only slides with at least 50 cells were evaluated.
Cytokine measurements
The following cytokines were measured on day 1 and day 4 by a customized human LegendPlex assay (BioLegend, San Dieago, CA): Inteleukin-1 beta (IL-1b), Interleukin-6 (IL-6), Interleukin-10 (IL-10), Interleukin-18 (IL-18), Interferon gamma (INF-γ), tumor necrosis factor alpha (TNF-α), Interferon alpha2 (INF-α2).
Plasma proteomics
The liquid chromatography-tandem mass spectrometry (LC–MS/MS) analyses were conducted as described before [22]. Briefly, plasma samples were prepared according to the SP3 protocol [23] and analyzed using an Ultimate 3000 RSLCnano HPLC coupled to an Orbitrap Exploris 240 mass spectrometer (both Thermo Scientific). The peptides were separated using a 37 min gradient from 4 to 28% acetonitrile in 0.1% formic acid and were measured using data independent acquisition. DIA-NN (v.1.8) was used for protein quantification with an in-house created spectral-library generated from plasma DDA measurements with FragPipe (v.17.1).
Statistics
Continuous variables are presented as means ± standard deviation in the case of normal distribution and as median and interquartile range (25th; 75th percentile) in the case of non-normally distributed variables. The statistical analyses were performed using the software R (R version 3.5.3; The R Foundation for Statistical Computing; http://www.R-project.org). A two-sided p-value < 0.05 was considered statistically significant. Confidence intervals (CIs) were calculated with 95% coverage.
Results
Cohort description
81 SARS-CoV-2 positive septic patients from three ICUs were included in our study (Fig. 1). The cohort consisted of 34 male patients (42%) and mean age was 58 (± 15) years. The median SOFA score at study inclusion was 9.5 (IQR: 5–12) and the Charlson Comorbidity Index (CCI) was 3 (IQR: 2–4). The 30d mortality rate of the cohort was 38%. For further base characteristics see Table 1.
Impact of ERK activity on 30-day survival
Looking at the Kaplan–Meier curve (Fig. 2), a significant difference in survival depending on the ERK activity on day 4 after sepsis diagnosis was observed. While only 20 of 41 patients with reduced pERK on day 4 were alive after 30 days (30d survival = 48.78%), 20 of 24 patients with increased pERK survived for 30 days (30d survival = 83.33%), which was statistically significant (p = 0.011). Regarding the rate of superinfections, there was no significant difference between groups (p = 0.17).
The Kaplan–Meier curve of 30-day survival as a function of ERK activity is plotted. Patients with increased ERK activity have a significantly lower mortality rate (p = 0.011). In the following Cox regression, the ERK activity was adjusted for CCI, gender and the SOFA score at the time of inclusion. Increased ERK activity was identified as the only significant, protective factor
The Cox regression analysis included the factors CCI, sex, and SOFA score at sepsis onset in addition to ERK activity at day 4 of sepsis (Fig. 2). Here, ERK activity was found to be a protective factor with respect to 30-day survival with a hazard ratio of 0.28 (95% CI 0.10–0.84) and remained the only statistically significant factor (p = 0.02).
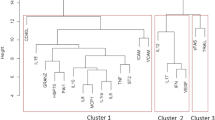
Regarding the trend of ERK activity in relation to survival, we observed that ERK activity decreases on average in the "non-survivors" while it remained almost constant in the "survivors". This resulted in a significant difference in ERK activity on day 4 between the survivors and the deceased (p = 0.011) (Fig. 3).
Classification of the cohort according to ERK activity
When the cohort was classified according to their ERK activity at day 4, no significant group differences except for mortality rate were observed. However, a trend towards a higher concentration of the pro-inflammatory cytokine IL-6 in association with high ERK activity was seen (p = 0.05). In contrast, patients with high ERK activity showed a decrease in CRP (p = 0.092). Of note, the SARS-CoV-2 PCR test CT value increased significantly from day 1 to day 4 in both cohorts. While the CT value increased from 26.13 to 28.87 (p = 0.018) within patients with high ERK activity, an increase from 24.17 to 28.79 (p < 0.001) in patients with low ERK was evident. However, there was no significant difference considering the mean increase from day 1 to day 4 between both groups (4.62 vs. 2.73, p = 0.23) Table 2.
Regarding plasma proteomics, no significant differences in abundant proteins was observed between patients with high and low ERK activity at day 1 or day 4 (Supplementary Fig. 1).
Discussion
The main finding of this study is: Increased ERK activity on day 4 of COVID-19 induced sepsis is associated with improved 30-day survival.
Despite extensive research, the precise pathophysiological mechanisms of (viral) sepsis remain incompletely elucidated. While pro- and anti-inflammatory cascades are simultaneously activated at the beginning of sepsis, hyperinflammation predominates during the early stages of sepsis, leading to a cytokine storm, vasodilation, oxygen deprivation and organ dysfunction [7]. In the later phase, sepsis can result in sepsis-associated immunosuppression or even immunoparalysis [24].
The RAF/MEK/ERK (also known as MAPK) network plays a crucial role in the inflammatory response as demonstrated by correlations with a range of cytokines [25]. The MAPK network is extensively studied in mammalian cells and also plays a critical role in various cellular functions besides the immune response such as cell proliferation or apoptosis. Hence, this network is often used as a proxy for the activation state of these cellular functions and the activation of ERK (or MAPK) is mostly used to evaluate the activation of this network.
Based on this, ERK activation on day 4 could be viewed as a restarting of the MAPK signaling, which in turn could be indicating a status of regaining immune balance of the patients. This, by preventing immune paralysis, could lead to a higher survival, hence explaining our results. The correlation between cytokines and ERK activation that we observed supports this hypothesis (see Supplementary Table 1).
However, an alternative perspective should be considered. Several articles have described the utilization of the RAF/MEK/ERK network by various viruses, including influenza [12, 26,27,28]. In case of the SARS-CoV-2 virus, MAPK signaling facilitates virus entry into the cell and promotes virus replication [16]. Therefore, the RAF/MEK/ERK network has been discussed as a valuable target in COVID-19 therapy [16,17,18]. Since MEK exclusively targets ERK, it serves as a significant pharmacological target for inhibiting the MAPK [25] network and many inhibitors of MEK have been developed [29]. Consequently, several authors have tested the hypothesis that applying MEK-inhibitors in COVID-19 infected cells could reduce viral replication and hyperinflammation [14, 16]. The authors showed that treatment with MEK antagonists inhibited inflammatory cytokines in vitro and an improved clinical severity score in vivo. These reports seem to contradict our main finding, namely that activation of ERK is beneficial for patients with severe COVID-19.
In order to discuss this, it is worth emphasizing that the previous studies on RAF/MEK/ERK were restricted to patients with moderate-to-severe COVID-19, i.e., without viral sepsis, and those receiving intensive care treatment or needing ventilator support were excluded. In these stages of COVID-19 it may be beneficial to block viral entry into the host cells and also curb a hyperinflammatory response in order to contribute to regaining immune balance of the patient, thus preventing a viral sepsis. During later stages of the disease, i.e. COVID-19 induced sepsis, activation of ERK, and hence increased pro-inflammation, may be beneficial in order to regain immune balance from the immunosuppressive state. In our work, high as well as low ERK activity patients showed an increase of the CT value. This indicates that there has already been a decrease in viral load in both cohorts. While effective antiviral therapy before and after the onset of viral sepsis is essential, modulation of the dysregulated immune response in COVID-19 sepsis is emerging as an area of major importance in improving patient outcomes [30] and may be more important for the survival of the patient at this stage. Therefore, while inhibiting ERK seems to be a promising therapeutic strategy in patients with moderate COVID-19, the same therapeutic strategy may be harmful for septic COVID-19 patients.
It is noteworthy that, upon stratifying the cohort based on their ERK activity in relation to the plasma proteome, no significant differences were observed. Despite detailed proteomic studies revealing characteristic changes in COVID-19 [31], we were unable to attribute these changes to the activity of the MAPK network in the late phase of infection. This lack of association may be explained by substantial interindividual heterogeneity in the proteome, compounded by the inherent critical condition of our cohort. While previous literature has underscored the value of proteomic analysis in categorizing COVID-19 courses into asymptomatic, mild, and severe [32], such categorization proved inherently unfeasible in our study, given that COVID-19 sepsis consistently accompanies a severe course.
As far as we know, the present study is the first to describe the impact of RAF/MEK/ERK network on outcome focusing on patients with COVID-19 sepsis. In summary, our findings contribute to the understanding of both the complexity and time sensitivity of the immune response in COVID-19 sepsis. Further research is required to obtain more nuanced perspectives and refine understanding COVID-19 sepsis and possible therapeutic targets.
Limitations
Although our study benefits from prospective enrollment and high-quality data, it is constrained by a relatively small sample size. Furthermore, the homogeneity of our cohort and the pronounced initial disease severity limit the generalizability of our findings. As a result, some established COVID-19 risk factors did not reach statistical significance in our analysis. Therefore, it is imperative to validate our results in a larger and more diverse population. This also applies to the rate of superinfections during COVID-19 sepsis. A strength of our study is the availability of comprehensive microbiological monitoring for the patients. The observed superinfection prevalence of 31% (21 out of 65 patients) aligns with findings reported in the literature [33]. We did not detect any significant differences between groups concerning MAPK network activity and superinfection rates, although there were hints for a more frequent occurrence in the cohort with lower ERK activity (high ERK activity 21% vs. low ERK activity 39%, p = 0.17). However, due to the small sample size, these results, as well, must be interpreted with caution and require validation in a larger cohort. In addition, it should be noted that the trajectory of ERK activity presented here represents only two snapshots. Both the activity at the onset of the disease and in the later stages are of interest to achieve a comprehensive understanding of the impact of the MAPK network throughout the course of the illness.
Conclusion
High activity of the MAPK network in the late phase of COVID-19 sepsis seems to be beneficial to the patient. Reestablishing balance of the immune system is a potential interpretation. Due to the variety of functions of ERK, further studies are needed to confirm these results.
Availability of data and materials
The dataset analyzed during the current study is available from the corresponding author on reasonable request.
Abbreviations
- CCI:
-
Charlson Comorbidity Index
- CI:
-
Confidence interval
- COVID-19:
-
Coronora virus disease 2019
- COPD:
-
Chronic obstructive pulmonary disease
- CRP:
-
C-reactive protein
- ERK:
-
Extracellular signal-regulated kinase
- ICU:
-
Intensive Care Unit
- IL-1b:
-
Inteleukin-1 beta
- IL-6:
-
Interleukin-6
- IL-10:
-
Interleukin-10
- IL-18:
-
Interleukin-18
- INF- α2:
-
Interferon alpha2
- INF- γ:
-
Interferon gamma
- IQR:
-
Interquatile range
- PBMC:
-
Peripheral blood mononuclear cells
- PBS:
-
Phosphate buffered saline
- pERK:
-
Phosphorylated extracellular signal-regulated kinase
- PLA:
-
Proximity Ligation Assay
- MAPK:
-
Mitogen-activated protein kinase
- MEK:
-
Mitogen-activated protein kinase
- RAF/MEK/ERK:
-
Rapidly accelerated fibrosarcoma/mitogen-activated protein kinase/extracellular signal-regulated kinase
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus type 2
- SOFA:
-
Sequential Organ Failure Assessment
- TNF-α:
-
Tumor necrosis factor alpha
References
Zhu N, et al. A Novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–33.
Ma Q, et al. Global percentage of asymptomatic SARS-CoV-2 Infections among the tested population and individuals with confirmed COVID-19 diagnosis: a systematic review and meta-analysis. JAMA Netw Open. 2021;4: e2137257.
Rodebaugh TL, et al. Acute symptoms of mild to moderate COVID-19 are highly heterogeneous across individuals and over time. Open Forum Infect Dis. 2021;8:ofab090.
Zhou F, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–62.
Collaborators C-EM. Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020–21. Lancet. 2022;399:1513–36.
Ramos-Casals M, Brito-Zeron P, Mariette X. Systemic and organ-specific immune-related manifestations of COVID-19. Nat Rev Rheumatol. 2021;17:315–32.
Seymour CW, et al. Assessment of clinical criteria for sepsis: for the third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016;315:762–74.
Rex DAB, et al. SARS-CoV-2 signaling pathway map: a functional landscape of molecular mechanisms in COVID-19. J Cell Commun Signal. 2021;15:601–8.
Schenz J, et al. Increased prevalence of clonal hematopoiesis of indeterminate potential in hospitalized patients with COVID-19. Front Immunol. 2022;13: 968778.
Preugschas HF, et al. Late activation of the Raf/MEK/ERK pathway is required for translocation of the respiratory syncytial virus F protein to the plasma membrane and efficient viral replication. Cell Microbiol. 2019;21: e12955.
Zhang Q, et al. Activation of the Ras/Raf/MEK pathway facilitates hepatitis C virus replication via attenuation of the interferon-JAK-STAT pathway. J Virol. 2012;86:1544–54.
Pleschka S, et al. Influenza virus propagation is impaired by inhibition of the Raf/MEK/ERK signalling cascade. Nat Cell Biol. 2001;3:301–5.
Bonjardim CA. Viral exploitation of the MEK/ERK pathway—a tale of vaccinia virus and other viruses. Virology. 2017;507:267–75.
Schreiber A, et al. The MEK1/2-inhibitor ATR-002 efficiently blocks SARS-CoV-2 propagation and alleviates pro-inflammatory cytokine/chemokine responses. Cell Mol Life Sci. 2022;79:65.
Haasbach E, et al. The MEK-inhibitor CI-1040 displays a broad anti-influenza virus activity in vitro and provides a prolonged treatment window compared to standard of care in vivo. Antiviral Res. 2017;142:178–84.
Ludwig S, Pleschka S, Planz O. MEK inhibitors as novel host-targeted antivirals with a dual-benefit mode of action against hyperinflammatory respiratory viral diseases. Curr Opin Virol. 2023;59: 101304.
Cusato J, et al. COVID-19: a possible contribution of the MAPK pathway. Biomedicines. 2023;11:1459.
Montazersaheb S, et al. COVID-19 infection: an overview on cytokine storm and related interventions. Virol J. 2022;19:92.
Xie J, et al. Inhibition of MEK signaling prevents SARS-CoV2-induced lung damage and improves the survival of infected mice. J Med Virol. 2022;94:6097–102.
Forsyth CB, et al. The SARS-CoV-2 S1 spike protein promotes MAPK and NF-kB activation in human lung cells and inflammatory cytokine production in human lung and intestinal epithelial cells. Microorganisms. 2022;10:1996.
Klaesson A, et al. Improved efficiency of in situ protein analysis by proximity ligation using UnFold probes. Sci Rep. 2018;8:5400.
Unterberg M, et al. Human cytomegalovirus seropositivity is associated with reduced patient survival during sepsis. Crit Care. 2023;27:417.
Hughes CS, et al. Single-pot, solid-phase-enhanced sample preparation for proteomics experiments. Nat Protoc. 2019;14:68–85.
Hotchkiss RS, et al. The sepsis seesaw: tilting toward immunosuppression. Nat Med. 2009;15:496–7.
Arthur JS, Ley SC. Mitogen-activated protein kinases in innate immunity. Nat Rev Immunol. 2013;13:679–92.
Marjuki H, et al. Membrane accumulation of influenza A virus hemagglutinin triggers nuclear export of the viral genome via protein kinase Calpha-mediated activation of ERK signaling. J Biol Chem. 2006;281:16707–15.
Wang C, et al. HA triggers the switch from MEK1 SUMOylation to phosphorylation of the ERK pathway in influenza a virus-infected cells and facilitates its infection. Front Cell Infect Microbiol. 2017;7:27.
Yewdell J, Garcia-Sastre A. Influenza virus still surprises. Curr Opin Microbiol. 2002;5:414–8.
Ascierto PA, Dummer R. Immunological effects of BRAF+MEK inhibition. Oncoimmunology. 2018;7: e1468955.
Li H, et al. SARS-CoV-2 and viral sepsis: observations and hypotheses. Lancet. 2020;395:1517–20.
Babačić H, et al. Comprehensive proteomics and meta-analysis of COVID-19 host response. Nat Commun. 2023;14:5921.
Pagani L, et al. Plasma proteomic variables related to COVID-19 severity: an untargeted nLC-MS/MS investigation. Int J Mol Sci. 2023;24:3570.
Musuuza JS, et al. Prevalence and outcomes of co-infection and superinfection with SARS-CoV-2 and other pathogens: a systematic review and meta-analysis. PLoS ONE. 2021;16: e0251170.
Acknowledgements
CovidDataNet.NRW research group (alphabetical order): Michael Adamzik1, Moritz Anft6, Nina Babel6, Malte Bayer1, Maha Bazzi1, Lars Bergmann1, Thilo Bracht1,2, Alexander von Busch1, Stefan F. Ehrentraut4, Martin Eisennacher2, Sai Spoorti Ramesh2, Helge Haberl1, Thilo von Groote3, Melanie Meersch-Dini3, Björn Koos1, Katrin Marcus2, Stephanie Pfänder5, Hartmuth Nowak1, Christian Putensen4, Lars Palmowski1, Tim Rahmel1, Katharina Rump1, Jens-Christian Schewe4, Jennifer Orlowski1, Barbara Sitek1, Andrea Witowski1, Britta Marco1, Matthias Unterberg1, Daniel Kühn5, Maike Weber2, Christina Weisheit4, Alexander Wolf1, Alexander Zarbock3, Dominik Ziehe1, Birgit Zuelch1
1Klinik für Anästhesiologie, Intensivmedizin und Schmerztherapie, Universitätsklinikum Knappschaftskrankenhaus Bochum, Bochum, Germany; 2Ruhr Universität Bochum, Medizinische Fakultät, Medizinisches Proteom-Center, Bochum, Germany; 3Klinik für Anästhesiologie, operative Intensivmedizin und Schmerztherapie, Universitätsklinikum Münster, Münster, Germany; 4Klinik für Anästhesiologie und operative Intensivmedizin, Universitätsklinikum Bonn, Bonn, Germany; 5Department for Molecular and Medical Virology, Ruhr-Universität Bochum, Bochum, Germany; 6Centrum für Translationale Medizin, Medizinische Klinik I, Marien Hospital Herne, Universitätsklinikum der Ruhr-Universität Bochum, Herne, Germany.
Funding
Open Access funding enabled and organized by Projekt DEAL. The project CovidDataNet.NRW was funded by the state of North Rhine-Westphalia, Germany.
Author information
Authors and Affiliations
Consortia
Contributions
Conceptualization: LP, AW, MA, BK, DZ. Writing the original draft: LP, AW. Revision of original draft: TR, MA, BK, DZ, TvG, MW. Data generation & patient recruitment: LP, AW, TR, HN, MA, SFE, CP, TvG, AZ, NB, MoA, BS, CW, SP, BK, DZ, KR. Data analysis: LP, AW, BK. Supervision: MA, BK, DZ.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of the Medical Faculty of the University of Bochum (Ruhr-University Bochum, registry number 18–6606-BR, German clinical trial registry: DRKS00026184). Informed consent forms were available for all included patients or their respective legal representatives, if patients were unable to provide informed consent at the time of study inclusion.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Witowski, A., Palmowski, L., Rahmel, T. et al. Activation of the MAPK network provides a survival advantage during the course of COVID-19-induced sepsis: a real-world evidence analysis of a multicenter COVID-19 Sepsis Cohort. Infection (2024). https://doi.org/10.1007/s15010-024-02325-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s15010-024-02325-7