Abstract
Introduction
The aim of this study was to investigate how long hospitalized patients stayed positive to the nasopharyngeal swab, and what demographic and clinical factors influence the time-to-negative swab.
Methods
We enrolled in a multicenter, observational, retrospective study involving 17 COVID-19 units in eight cities of the Campania, southern Italy all patients hospitalized from March 2020 to May 2021 diagnosed with Severe Acute Respiratory Distress Syndrome-Coronavirus-2 (SARS-CoV-2) infection for whom time-to-negative swab was available.
Results
963 patients were enrolled. We defined three groups considering time-to-negative swab: the first including patients with time-to-negative swab before the 26th day, the second including patients with time-to-negative swab from day 26 to day 39, and the third including patients with time-to-negative swab > 39 days. 721 (74.9%) patients belonged to the first group, 194 (20.1%) to the second, and 52 (5.4%) belonged to the third group. Belonging to group 2 and 3 seemed to be influenced by age (p value < 0.001), Charlson comorbidity index (p = 0.009), arterial hypertension (p = 0.02), cardiovascular disease (p = 0.017), or chronic kidney disease (CKD) (p = 0.001). The multivariable analysis confers a leading role to CKD, with an odds ratio of 2.3 as factor influencing belonging to the groups showing a longer time-to-negative swab. Patients with CKD and diabetes were more frequently in the third group.
Discussion
Our analysis showed that CKD is a factor related to longer time-to-negative swab, probably because of immunosuppression related to this condition.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
To date, COronaVirus Disease-2019 (COVID-19) pandemic, caused by Severe Acute Respiratory Distress Syndrome-Coronavirus-2 (SARS-CoV-2) infection, has interested more than 700 hundred million cases and almost 7 million deaths worldwide [1].
Real-Time Polymerase Chain Reaction (RT-PCR) on nasopharyngeal swabs is considered the gold standard for the diagnosis of SARS-CoV-2 infection. Especially, during the first phases of the pandemic, it played a role in helping to end social isolation [2]. Soon afterward, antigenic swabs became central in controlling shelter-in-place isolation [3], with RT-PCR keeping a role where a certainty of non-contagiousness was required, e.g., in outpatient services for in-hospital admission.
In the literature, a few studies have focused on the issue of time-to-negative swab; nonetheless, some data on the positivity time span were possible to deduce from studies with different endpoints: this time ranged from 17 to 32 days in patients under 18 years old [4, 5], and from 14 to 27 days in adult patients [6,7,8]. Moreover, according to the recent studies conducted in the Omicron era, a prolonged time-to-negative swab, indicator of prolonged viral shedding, may be an element considered able to increase the risk of developing viral mutations [9]. The worry of the development of vaccine and therapy escape mutations has created the impulse to develop studies including time-to-negative swab or time-to-low viral load, still measured according to the high Ct levels in RT-PCR. Promising data show how early antiviral therapies can shorten the time-to-negative swab, potentially reducing mutation odds [10, 11]. From this point of view, identifying potential patients with longer than average time-to-negative swab may be an independent element in assessing who should receive early antiviral treatment; moreover, a prolonged time-to-negative swab was often a problem in the management of other co-pathologies where the paths dedicated to COronaVIrus Disease-2019 (COVID-19) were not identified.
The aims of the present study was to investigate positivity time spans in a large cohort of hospitalized patients with COVID-19 and the demographic and clinical factors influenced this time span, to determine which patients have a higher risk of long viral shedding.
Materials and methods
Study design and setting
We performed a multicenter, observational, retrospective study involving seventeen COVID-19 units in eight cities in the Campania region in southern Italy: Naples, Caserta, Salerno, Benevento, Avellino, Pozzuoli, Eboli, and Vallo della Lucania. All adult (≥ 18 years) patients, hospitalized with a diagnosis of SARS-CoV-2 infection confirmed by RT-PCR on a naso-oropharyngeal swab, from February 28th, 2020 to May 31st, 2021 at one of the centers participating in the study, were enrolled in the CoviCamp cohort [12,13,14,15]. No study protocol or guidelines regarding the criteria of hospitalization were shared among the centers involved in the study and the patients were hospitalized following the decision of the physicians of each center.
From the CoviCamp cohort, we included all patients for whom a time-to-negative swab was available. Exclusion criteria included minority age, lack of the data on the time-to-negative swab, and lack of informed consent; also, the patients who died during hospitalization were excluded.
The study was approved by the Ethics Committee of the University of Campania L. Vanvitelli, Naples (n°10877/2020). All procedures performed in this study were in accordance with the ethics standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethics standards. Informed consent was obtained from all participants included in the study.
This study was reported following the STROBE recommendations for an observational study (Supplementary Table 1).
Variables and definitions
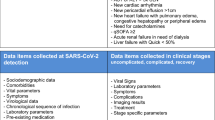
All demographic and clinical data of patients with SARS-CoV2 infection enrolled in the cohort were collected in an electronic database. From this database, we extrapolated the data for the present study.
The microbiological diagnosis of SARS-CoV-2 infection was defined as a positive RT-PCR test on a naso-oropharyngeal swab. All the units included used the same RT-PCR kit, Bosphore V3 (Anatolia Genework, Turkey, https://covid-19-diagnostics.jrc.ec.europa.eu/devices/detail/31). We considered the time-to-negative swab as the days from the first positive RT-PCR for SARS-CoV-2 to the first negative RT-PCR: the data were extrapolated from the regional database (https://sinfonia.regione.campania.it/preview/ecovid). Where available, we included the time from the last positive nasopharyngeal swab to the first negative nasopharyngeal swab for SARS-CoV-2.
We divided the patients enrolled according to the clinical outcome of COVID-19: patients with a mild outcome were those who did not require oxygen therapy, or performed oxygen therapy with a nasal cannula or venturi mask, hemodynamically stable patients, patients with a Glasgow Coma Scale greater than 9; patients with severe outcome were those who underwent oxygen therapy with high flow nasal cannula or non-invasive or invasive ventilation; non-hemodynamically stable patients, patients with a Glasgow Coma Scale less than 9.
Statistical analysis
For the descriptive analysis, categorical variables were presented as absolute numbers and their relative frequencies. Continuous variables were summarized as mean and standard deviation or as median and interquartile range (Q1–Q3). We performed a comparison of patients with different time-to-negative swab (days) using Pearson chi-square or Fisher’s exact test for categorical variables and Student’s t test or Mann–Whitney test for continuous variables. Odds ratios were calculated using binomial logistic regression; these analyses were performed only for parameters clinically relevant and for those who resulted statistically significant at univariate analysis. We used the Benjamini–Hochberg (BH) procedure for controlling the false discovery rate (FDR) which entailed the correction of p values in the context of multiple comparisons. Analyses were performed by STATA [16].
Results
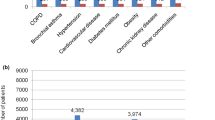
During the study period, 2,054 patients with a diagnosis of SARS-CoV-2 infection, confirmed by a positive RT-PCR on a naso-oropharyngeal swab, were hospitalized in one of the centers participating in the study. We excluded 1,091 patients with insufficient data on swabs or those who died during hospitalization and, thus, 963 patients were enrolled for the present study (Fig. 1). The demographic and clinical characteristics of the 963 patients included in the study were similar to the 1,091 excluded (data not shown). Table 1 shows the demographic and clinical characteristics at admission and the clinical outcome of the 963 patients enrolled. Six hundred and eighteen (64.2%) subjects were male; median age was 61 years (Q1–Q3: 51–71 years). Overall, 60 patients (6.3%) had active cancer, and of these only 5 had a hematological malignancy. A severe outcome of COVID-19 was observed in 225 (23.5%) of the patients enrolled.
The median time from the first positive to the first negative swab was 19 days (Q1–Q3: 13–26 days) (Table 1). To identify patients with an abnormally longer time-to-negative swab, representing long viral shedding, the patients who had the first negative swab before the 26th day (the 75th percentile) were included in Group A, those with a time to-negative-swab from 26 to 39 days (the 95th percentile) in Group B, and those with a time-to-negative swab > 39 days in Group C: the groups included 721, 194 and 52 patients, respectively. Since how often an SARS-CoV 2 positive patient would undergo a nasopharyngeal swab was an independent decision by the physician in care, we analyzed how long before the first negative swab the patients had had the previous swab: the median time was 5 (2–8) days in the first group, 6 (4–10) days in the second group, and 7 (4–13) days in the third group.
Table 2 shows the demographic, biochemical, and clinical data according to the three groups of patients. Median age was higher in groups B [64 years (55–72)] and C [67 years (57–77)] compared to Group A [60 years (50–70)] (p < 0.0001). The Median Charlson Comorbidity Index was higher in group C [3 (2–5)] than in groups A and B (p = 0.009). Compared to the patients in group A, those in Groups B and C more frequently had arterial hypertension, cardiovascular diseases, and chronic kidney disease, differences all significant to the statistical analysis (Table 2). Linear-by-linear association was non-significant for arterial hypertension (p = 0.121), while it was significant for cardiovascular diseases and Chronic Kidney Diseases (CKD) (p = 0.002 and p = 0.003). Considering the clinical outcome of COVID-19, the prevalence of severe patients was higher with the increase in time-to-negative swab [(22% in group A, 26% in group B and 30.7% in group C) with a linear-by-linear association of 0.046].
To identify independent factors associated with more prolonged viral shedding, we performed a multiple logistic regression on variables associated with belonging to groups with longer time-to-negative swab (Table 3 and Fig. 2): age and the presence of a history of CKD were the only independent factors associated with prolonged viral shedding: odds ratio (OR) 1.01 (95% Confidence Interval CI 1.00–1.03, p = 0.003) for age and OR 2.3 (95% CI 1.33–3.9, p = 0.025) for CKD. To control false discovery rate, we adjust p value with Benjamini–Hochberg method in multiple comparison test, after adjust p value was significant only for CKD in multivariable analysis (Table 2). To evaluate in the patients with CKD the role of diabetes in the prolonged time-to-negative swab, we defined two groups: the first including patients with diabetes and CKD, the second with CKD and no associated diabetes. Although between the two groups of patients, there was no statistical difference in time-to-negative swab [median 24 days (Q1–Q3: 17–33) vs 20 days (13–33) (p = 0.338)], 5 (16.7%) of the 30 patients with diabetes and CKD had a time-to-negative swab longer than 39 days compared to none of the 33 patients with CKD without diabetes (p = 0.045).
Discussion
In this multicenter observational retrospective study, our aim was to find demographic and clinical factors that may predict persistency of positive nasopharyngeal specimen to SARS-CoV-2. In our population of 963 patients, we identified a median time-to-negative swab of 19 days (Q1–Q3: 13–26 days) and in about 5% of the population very prolonged SARS-CoV-2 shedding (more than 39 days after the first positive swab). Moreover, the prevalence of patients with severe COVID-19 increased with the increase in time-to-negative swab.
Persistence of SARS-CoV-2 is a current issue considering its impact and the poor scientific evidence on the management of this condition. Studies have underlined the impact of persistent viral shedding, especially in immunocompromised populations: prolonged viral shedding was associated with higher infectivity, the accumulation of mutations, immune escape, and poor prognosis because of the consequent impossibility to give treatments for the ongoing disease [9, 17]; furthermore, it was associated with in-hospital delirium (OR 2.43; 95% CI 1.42, 4.29) [18]. The scientific community is aware of this issue and is currently trying to improve the management of patients with prolonged viral shedding. For example, case reports and studies have highlighted how the combination of different antiviral drugs commonly used in early treatment could be effective in inducing virus clearance, especially in patients with a hematological malignancy [19,20,21,22]
Previous studies have evaluated the predictive factors for prolonged viral persistence. The factors highlighted as prognostic were both demographic factors such as age and sex, but also clinical factors such as the presence of hypertension and pharmacological treatments [23,24,25]. Differently from our study, these studies included patients who were asymptomatic or had mild symptoms [24, 25] and one included only 113 patients in early 2020 [23]. Mostly prolonged viral shedding was observed in immunocompromised populations [26] especially in hematological malignancies, with an average negativization time of about 4 weeks [27].
In the present study on 963 hospitalized COVID-19 patients, the variable independently associated with a longer viral shedding was the presence of CKD (OR 2.3, 1.33–3.9). Moreover, the patients with CKD and diabetes were more likely to have a longer time-to-negative swab, frequently more than 39 days.
The association of CKD as a factor that can increase time-to-negative swab, to our knowledge, is a new and relevant factor. In fact, previously, several studies showed that patients with CKD had higher mortality and worse outcome compared with patients without [28,29,30], but, to our knowledge, no studies showed the impact of CKD on the time-to-negative swab. The persistence of SARS-CoV-2 in patients with CKD observed in the present study could be related to an alteration in the immune system due to renal impairment [31]. In fact, in patients with CKD, the increase in pro-inflammatory cytokines, the increase in acute phase protein, and the dysfunction of phagocytes B- and T-cells can lead to systemic inflammation and acquired immunodepression, which accounts for infectious complications [31], including a prolonged SARS-CoV-2 shedding. In addition, our data showed that patients with diabetes and CKD were more likely to have a time-to-negative swab longer than 39 days compared to patients without diabetes with CKD. These data may be due to the impact of diabetes on inflammatory pathways [32]: diabetes leads to a dysregulation of immune pathways such as an alteration in signaling mediated by Toll-like receptors, an alteration in NLR family Pyrin domain containing 3 (NLRP3) inflammasome with the activation of a pro-inflammatory cascade of Il-1β and IL-18 [32], probably increasing immune alteration.
Our study shows several limitations. First, its retrospective design. Second, we had very low prevalence of patients with a hematological malignancy and given the small number may not have shown the correlation with the time-to-negative swab. Third, swabs were performed without a pre-fixed timing, so each test result depicted a result from a random sample at a random point in time [33]; furthermore, there was a small but significant difference between the groups considering the time from last positive test and the first negative; however, it is usual in clinical practice to delay the SARS-CoV-2 nasopharyngeal test in patients who are positive for longer. Fourth, due to the historical period of our study, our cohort of patients did not include subjects who were vaccinated against SARS-CoV-2 and/or early treatments (antivirals or monoclonal antibodies), nor the impact of different variants. Fifth, we excluded patients who died during hospitalization. Sixth, it has to be taken into account a certain degree if false positive test risk in patients with long viral shedding, as for example, due to the detection of inactive viral particles [34]. Seventh, because of the absence of data, no longitudinal survival model was be performed in our study. On the other hand, the strengths of our study are the multicenter design, the sample size of the population, and the heterogeneity of age and multi-co-morbidities, which may be considered representative in the setting of hospitalized COVID-19 patients.
Conclusion
In conclusions, our study estimated that about 5% of hospitalized COVID-19 patients were SARS-CoV-2 positive at nasopharyngeal swab for at least 39 days after the first positive. Moreover, the patients with CKD and diabetes were more likely to have a time-to-negative swab of more than 39 days, probably due to immune system alterations related to this condition.
Data availability
The data that support the findings of this study are available from the corresponding author, Coppola Nicola, upon reasonable request.
References
WHO. WHO coronavirus (COVID-19) dashboard. Geneva: World Health Organization; 2021.
Centre for Disease Prevention E. Guidance for discharge and ending isolation in the context of widespread community transmission of COVID-19-first update Scope of this document. 2020.
Test diagnostici, contact tracing, isolamento e autosorveglianza. 2023. https://www.salute.gov.it/portale/nuovocoronavirus/dettaglioFaqNuovoCoronavirus.jsp?lingua=italiano&id=244#18. Accessed 08 May 2023.
Tagarro A, Sanz-Santaeufemia FJ, Grasa C, Cobos E, Yebra J, Alonso-Cadenas JA, Baquero-Artigao F, Mesa-Guzmán JM, Pérez-Seoane B, Calvo C, Herreros ML, Epalza C, Melendo S, Dominguez-Rodriguez S, Vidal P, Pacheco M, Ballesteros A, Bernardino M, Villanueva-Medina S, Rodríguez-Molino P, Miragaya Castro S, Rivière J, Garcés R, Santiago B, Fumadó V, Urretavizcaya-Martínez M, García-García ML, Penín M, Cava F, Sáez E, Iglesias-Bouzas MI, Herrero B, de Reinoso T, J, Moraleda C,. Dynamics of reverse transcription-polymerase chain reaction and serologic test results in children with SARS-CoV-2 infection. J Pediatr. 2022;241:126-132.e3. https://doi.org/10.1016/J.JPEDS.2021.09.029.
Bahar B, Jacquot C, Mo YD, De Biasi RL, Campos J, Delaney M. Kinetics of viral clearance and antibody production across age groups in children with severe acute respiratory syndrome coronavirus 2 infection. J Pediatr. 2020;227:31-37.e1. https://doi.org/10.1016/J.JPEDS.2020.08.078.
Cento V, Colagrossi L, Nava A, Lamberti A, Senatore S, Travi G, Rossotti R, Vecchi M, Casati O, Matarazzo E, Bielli A, Casalicchio G, Antonello M, Renica S, Costabile V, Scaglione F, Fumagalli R, Ughi N, Epis OM, Puoti M, Vismara C, Faccini M, Fanti D, Alteri C, Perno CF. Persistent positivity and fluctuations of SARS-CoV-2 RNA in clinically-recovered COVID-19 patients. J Infect. 2020;81:e90–2. https://doi.org/10.1016/J.JINF.2020.06.024].
Morone G, Palomba A, Iosa M, Caporaso T, de Angelis D, Venturiero V, Savo A, Coiro P, Carbone D, Gimigliano F, Iolascon G, Paolucci S. Incidence and persistence of viral shedding in COVID-19 Post-acute patients with negativized pharyngeal swab: a systematic review. Front Med (Lausanne). 2020. https://doi.org/10.3389/FMED.2020.00562].
Bragazzi NL, Motoc NS, Ruta V-M, Man MA, Ungur RA, Ciortea VM, Irsay L, Nicola A, Valean D, Usatiuc LO, Matei IR, Borda IM. Factors associated with prolonged RT-PCR SARS-CoV-2 positive testing in patients with mild and moderate forms of COVID-19: a retrospective study. Medicina. 2022. https://doi.org/10.3390/medicina.
Gliga S, Lübke N, Killer A, Gruell H, Walker A, Dilthey AT, Thielen A, Lohr C, Flaßhove C, Krieg S, Pereira JV, Seraphin TP, Zaufel A, Däumer M, Orth H-M, Feldt T, Bode JG, Klein F, Timm J, Luedde T, Jensen B-EO. Rapid selection of sotrovimab escape variants in severe acute respiratory syndrome coronavirus 2 omicron-infected immunocompromised patients. Clin Infect Dis. 2023;76:408–15. https://doi.org/10.1093/CID/CIAC802].
Wong CKH, Au ICH, Lau KTK, Lau EHY, Cowling BJ, Leung GM. Real-world effectiveness of early molnupiravir or nirmatrelvir–ritonavir in hospitalised patients with COVID-19 without supplemental oxygen requirement on admission during Hong Kong’s omicron BA.2 wave: a retrospective cohort study. Lancet Infect Dis. 2022;22:1681–93. https://doi.org/10.1016/S1473-3099(22)00507-2].
Martin-Blondel G, Marcelin AG, Soulié C, Kaisaridi S, Lusivika-Nzinga C, Zafilaza K, Dorival C, Nailler L, Boston A, Ronchetti AM, Melenotte C, Cabié A, Choquet C, Trinh-Duc A, Lacombe K, Gaube G, Coustillères F, Pourcher V, Martellosio JP, Peiffer-Smadja N, Chauveau M, Housset P, Piroth L, Devaux M, Pialoux G, Martin A, Dubee V, Frey J, Le Bot A, Cazanave C, Petua P, Liblau R, Carrat F, Yordanov Y. Time to negative PCR conversion amongst high-risk patients with mild-to-moderate Omicron BA.1 and BA.2 COVID-19 treated with sotrovimab or nirmatrelvir. Clin Microbiol Infect. 2023. https://doi.org/10.1016/j.cmi.2022.12.016).
Pisaturo M, Russo A, Pattapola V, Astorri R, Maggi P, Numis FG, Gentile I, Sangiovanni V, Rossomando A, Gentile V, Calabria G, Pisapia R, Codella AV, Masullo A, Iodice V, Giolitto G, Parrella R, Dell’Aquila G, Gambardella M, Di Perna F, Coppola N, CoviCam Group. clinical characterization of the three waves of COVID-19 occurring in Southern Italy: results of a multicenter cohort study. Int J Environ Res Public Health. 2022;19:16003. https://doi.org/10.3390/ijerph192316003.
Macera M, De Angelis G, Sagnelli C, Coppola N, VanvitelliCovid-Group. Clinical presentation of COVID-19: case series and review of the literature. Int J Environ Res Public Health. 2020;17:5062. https://doi.org/10.3390/ijerph17145062.
Russo A, Pisaturo M, Palladino R, Maggi P, Numis FG, Gentile I, Sangiovanni V, Esposito V, Punzi R, Calabria G, Rescigno C, SalomoneMegna A, Masullo A, Manzillo E, Russo G, Parrella R, Dell’Aquila G, Gambardella M, Ponticiello A, Coppola N, On Behalf Of CoviCam Group. Prognostic value of transaminases and bilirubin levels at admission to hospital on disease progression and mortality in patients with COVID-19-an observational retrospective study. Pathogens. 2022;11:652. https://doi.org/10.3390/pathogens11060652.
Pisaturo M, Calò F, Russo A, Camaioni C, Giaccone A, Pinchera B, Gentile I, Simeone F, Iodice A, Maggi P, Coppola N. Dementia as risk factor for severe coronavirus disease 2019: a case-control study. Front Aging Neurosci. 2021;13:698184. https://doi.org/10.3389/fnagi.2021.698184.
StataCorp. Stata statistical software: release 16. College Station: StataCorp LLC; 2019.
Truong TT, Ryutov A, Pandey U, Yee R, Goldberg L, Bhojwani D, Aguayo-Hiraldo P, Pinsky BA, Pekosz A, Shen L, Boyd SD, Wirz OF, Röltgen K, Bootwalla M, Maglinte DT, Ostrow D, Ruble D, Han JH, Biegel JA, Li M, Huang C, Sahoo MK, Pannaraj PS, O’Gorman M, Judkins AR, Gai X, Dien BJ. Increased viral variants in children and young adults with impaired humoral immunity and persistent SARS-CoV-2 infection: a consecutive case series. EBioMedicine. 2021;67:1355. https://doi.org/10.1016/j.ebiom.2021.103355.
Batra A, Clark JR, Kang AK, Ali S, Patel TR, Shlobin NA, Hoffman SC, Lim PH, Orban ZS, Visvabharathy L, Graham EL, Sullivan DP, Muller WA, Chou SH, Ungvári Z, Koralnik IJ, Liotta EM. Persistent viral RNA shedding of SARS-CoV-2 is associated with delirium incidence and six-month mortality in hospitalized COVID-19 patients. Geroscience. 2022;44:1241–54. https://doi.org/10.1007/s11357-022-00561-z.
Trottier CA, Wong B, Kohli R, Boomsma C, Magro F, Kher S, Anderlind C, Golan Y. Dual antiviral therapy for persistent coronavirus disease 2019 and associated organizing pneumonia in an immunocompromised host. Clin Infect Dis. 2023;76:923–5. https://doi.org/10.1093/cid/ciac847.
Baldi F, Dentone C, Mikulska M, Fenoglio D, Mirabella M, Magnè F, Portunato F, Altosole T, Sepulcri C, Giacobbe DR, Uras C, Scavone G, Taramasso L, Orsi A, Cittadini G, Filaci G, Bassetti M. Case report: Sotrovimab, remdesivir and nirmatrelvir/ritonavir combination as salvage treatment option in two immunocompromised patients hospitalized for COVID-19. Front Med (Lausanne). 2023;9:1062450. https://doi.org/10.3389/fmed.2022.1062450.
Ford ES, Simmons W, Karmarkar EN, Yoke LH, Braimah AB, Orozco JJ, Ghiuzeli CM, Barnhill S, Sack CL, Benditt JO, Roychoudhury P, Greninger AL, Shapiro AE, Hammond JL, Rusnak JM, Dolsten M, Boeckh M, Liu C, Cheng GS, Corey L. Successful treatment of prolonged, severe coronavirus disease 2019 lower respiratory tract disease in a b cell acute lymphoblastic leukemia patient with an extended course of remdesivir and nirmatrelvir/ritonavir. Clin Infect Dis. 2023;76:926–9. https://doi.org/10.1093/cid/ciac868.
Mikulska M, Sepulcri C, Dentone C, Magne F, Balletto E, Baldi F, Labate L, Russo C, Mirabella M, Magnasco L, Di Grazia C, Ghiggi C, Raiola AM, Giacobbe DR, Vena A, Beltramini S, Bruzzone B, Lemoli RM, Angelucci E, Bassetti M. Triple combination therapy with two antivirals and monoclonal antibodies for persistent or relapsed SARS-CoV-2 infection in immunocompromised patients. Clin Infect Dis. 2023. https://doi.org/10.1093/cid/ciad181.
Xu K, Chen Y, Yuan J, Yi P, Ding C, Wu W, Li Y, Ni Q, Zou R, Li X, Xu M, Zhang Y, Zhao H, Zhang X, Yu L, Su J, Lang G, Liu J, Wu X, Guo Y, Tao J, Shi D, Yu L, Cao Q, Ruan B, Liu L, Wang Z, Xu Y, Liu Y, Sheng J, Li L. Factors associated with prolonged viral RNA shedding in patients with coronavirus disease 2019 (COVID-19). Clin Infect Dis. 2020;71:799–806. https://doi.org/10.1093/cid/ciaa351.
Gui H, Zhang Z, Chen B, Chen Y, Wang Y, Long Z, Zhu C, Wang Y, Cao Z, Xie Q. Development and validation of a nomogram to predict failure of 14-day negative nucleic acid conversion in adults with non-severe COVID-19 during the Omicron surge: a retrospective multicenter study. Infect Dis Poverty. 2023;12:7. https://doi.org/10.1186/s40249-023-01057-4.
Li R, Jin C, Zhang L, Kong D, Hu K, Xuan M, Liu Q, Li S, Zhang K, Xue Y. Clinical characteristics and risk factors analysis of viral shedding time in mildly symptomatic and asymptomatic patients with SARS-CoV-2 Omicron variant infection in Shanghai. Front Public Health. 2023;4:1073387. https://doi.org/10.3389/fpubh.2022.1073387.
Kang SW, Kim JW, Kim JY, Lim SY, Jang CY, Chang E, Yang JS, Kim KC, Jang HC, Kim D, Shin Y, Lee JY, Kim SH. Characteristics and risk factors of prolonged viable virus shedding in immunocompromised patients with COVID-19: a prospective cohort study. J Infect. 2023;86:412–4. https://doi.org/10.1016/j.jinf.2023.01.024.
Garmendia JV, García AH, De Sanctis CV, Hajdúch M, De Sanctis JB. Autoimmunity and immunodeficiency in severe SARS-CoV-2 infection and prolonged COVID-19. Curr Issues Mol Biol. 2022;45:33–50. https://doi.org/10.3390/cimb45010003.
Moeinzadeh F, Raeisi V, Babahajiani M, Mortazavi M, Pourajam S, Seirafian S, Shirzadi M, Taheri S, Salahi M, Mansourian M, Toghyani A, Zamani Z. Is chronic kidney disease, a predictor of in-hospital mortality in coronavirus disease 2019 (COVID-19) patients? Adv Biomed Res. 2023;25:39. https://doi.org/10.4103/abr.abr_352_21.
Flythe JE, Assimon MM, Tugman MJ, Chang EH, Gupta S, Shah J, Sosa MA, Renaghan AD, Melamed ML, Wilson FP, Neyra JA, Rashidi A, Boyle SM, Anand S, Christov M, Thomas LF, Edmonston D, Leaf DE, STOP-COVID Investigators. Characteristics and outcomes of individuals with pre-existing kidney disease and COVID-19 admitted to intensive care units in the United States. Am J Kidney Dis. 2021;77:190-203.e1. https://doi.org/10.1053/j.ajkd.2020.09.003.
Tan TT, Ng HJ, Young B, Khan BA, Shetty V, Azmi N, Clissold S. Effectiveness of vaccination against SARS-CoV-2 and the need for alternative preventative approaches in immunocompromised individuals: a narrative review of systematic reviews. Expert Rev Vaccines. 2023;22:341–65. https://doi.org/10.1080/14760584.2023.2191716.
Kurts C, Panzer U, Anders HJ, Rees AJ. The immune system and kidney disease: basic concepts and clinical implications. Nat Rev Immunol. 2013;13:738–53. https://doi.org/10.1038/nri3523.
Tang SCW, Yiu WH. Innate immunity in diabetic kidney disease. Nat Rev Nephrol. 2020;16:206–22. https://doi.org/10.1038/s41581-019-0234-4.
Mouliou DS, Pantazopoulos I, Gourgoulianis K. COVID-19 diagnosis in the emergency department: seeing the tree but losing the forest. Emerg Med J. 2022;39:563. https://doi.org/10.1136/emermed-2021-212219.
Mouliou DS, Gourgoulianis KI. False-positive and false-negative COVID-19 cases: respiratory prevention and management strategies, vaccination, and further perspectives. Expert Rev Respir Med. 2021;15:993–1002. https://doi.org/10.1080/17476348.2021.1917389.
Acknowledgements
Campania COVID-19 (CoviCamp) network: Nicola Coppola, Caterina Monari, Caterina Sagnelli, Paolo Maggi, Vincenzo Sangiovanni, Fabio Giuliano Numis, Ivan Gentile, Alfonso Masullo, Carolina Rescigno, Giosuele Calabria, Angelo Salomone Megna, Michele Gambardella, Elio Manzillo, Grazia Russo, Vincenzo Esposito, Giuseppina Dell’Aquila, Roberto Parrella, Rodolfo Punzi, Antonio Ponticiello, Mariantonietta Pisaturo, Enrico Allegorico, Raffaella Pisapia, Francesco Maria Fusco, Giovanni Porta, Margherita Macera, Federica Calò, Angela Cascone, Gianfranca Stornaiuolo, Maria Stanzione, Lorenzo Onorato, Paola Medusa, Carro Nicola, Andrea Dell’aquila, Simona Imbriani, Ricozzi Carmen, Klodian Gjeloshi, Roberta Astorri, Anna Maria Rossomando, Mariana Di Lorenzo, Antonio Russo, Giorgio Bosso, Claudia Serra, Ferdinando Dello Vicario, Valentina Minerva, Giulia De Angelis, Stefania De Pascalis, Salvatore Martini, Giovanni Di Caprio, Addolorata Masiello, Domenica Di Costanzo, Mariano Mazza, Vincenzo Bianco, Valeria Gentile, Antonio Riccardo Buonomo, Biagio Pinchera, Riccardo Scotto. The authors would like to thank Dr. Carlo Garofalo, Unit of Nephrology, Department of Advanced Medical and Surgical Sciences, University of Campania "Luigi Vanvitelli", Naples, Italy, for critical review of the manuscript.
Funding
Open access funding provided by Università degli Studi della Campania Luigi Vanvitelli within the CRUI-CARE Agreement. POR Campania FESR 2014-2020-Avviso per l’acquisizione di manifestazioni di interesse per la realizzazione di servizi di ricerca e sviluppo per la lotta contro il Covid-19 (DGR n. 140 del 17 marzo 2020), Regione Campania, Italy, Project: IDENTIFICAZIONE DEI FATTORI DEMOGRAFICI, CLINICI, VIROLOGICI, GENETICI, IMMUNOLOGICI E SIEROLOGICI ASSOCIATI AD OUTCOME SFAVOREVOLE NEI SOGGETTI CON COVID-19, and POR FESR Campania 2014-2020-Avviso per l’acquisizione di manifestazioni di interesse da parte degli Organismi di Ricerca per la realizzazione di servizi di ricerca, sviluppo e innovazione per la lotta contro il COVID-19 (DGR n. 504 del 10.11.2021)–Regione Campania, Italy; Project: IMPATTO DELLE NUOVE VARIANTI, L’USO DI TERAPIE ANTIVIRALI PRECOCI E STATO VACCINALE SULLA PRESENTAZIONE CLINICA DEL COVID-19: STUDIO RESTROSPETTIVO/PROSPETTICO MULTICENTRICO.
Author information
Authors and Affiliations
Consortia
Contributions
NC, AR, PG, and MP were involved in study concept and design, drafting of the manuscript: NC, AR, MP, PM, IG, PG, EA, VS, RP, RaPi, AnRo, RoPa, GC, EM, AM, CC, GDA, GR, MC, AP, and LO were involved in critical revision of the manuscript for important intellectual content; AR and PG were involved in the analysis of data; NC, AR, MP, PM, IG, PG, EA, VS, RP, RaPi, AnRo, RoPa, GC, EM, AM, CC, GDA, GR, MC, AP, and LO were involved in acquisition of data, interpretation of data, and critical revision of the manuscript; CoviCamp (Campania COVID-19 group) was involved in the enrollment of the patients. All authors contributed to data analysis, drafting, or revising the article, and have agreed on the journal to which the article will be submitted, have given final approval of the version to be published, and have agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Institutional review board statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of the University of Campania L. Vanvitelli, Naples (n°10877/2020, May 11, 2020).
Informed consent statement
Informed consent was obtained from all subjects involved in the study.
Additional information
The members of the CoviCam group are listed in “Acknowledgments” section.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Grimaldi, P., Russo, A., Pisaturo, M. et al. Clinical and epidemiological factors causing longer SARS-CoV 2 viral shedding: the results from the CoviCamp cohort. Infection 52, 439–446 (2024). https://doi.org/10.1007/s15010-023-02095-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-023-02095-8