Abstract
Purpose
Despite the need to generate valid and reliable estimates of protection levels against SARS-CoV-2 infection and severe course of COVID-19 for the German population in summer 2022, there was a lack of systematically collected population-based data allowing for the assessment of the protection level in real time.
Methods
In the IMMUNEBRIDGE project, we harmonised data and biosamples for nine population-/hospital-based studies (total number of participants n = 33,637) to provide estimates for protection levels against SARS-CoV-2 infection and severe COVID-19 between June and November 2022. Based on evidence synthesis, we formed a combined endpoint of protection levels based on the number of self-reported infections/vaccinations in combination with nucleocapsid/spike antibody responses (“confirmed exposures”). Four confirmed exposures represented the highest protection level, and no exposure represented the lowest.
Results
Most participants were seropositive against the spike antigen; 37% of the participants ≥ 79 years had less than four confirmed exposures (highest level of protection) and 5% less than three. In the subgroup of participants with comorbidities, 46–56% had less than four confirmed exposures. We found major heterogeneity across federal states, with 4–28% of participants having less than three confirmed exposures.
Conclusion
Using serological analyses, literature synthesis and infection dynamics during the survey period, we observed moderate to high levels of protection against severe COVID-19, whereas the protection against SARS-CoV-2 infection was low across all age groups. We found relevant protection gaps in the oldest age group and amongst individuals with comorbidities, indicating a need for additional protective measures in these groups.
Similar content being viewed by others
Introduction
During the SARS-CoV-2 pandemic, there was a lack of population-based panels in Germany capable of providing rapid and adaptable estimates of population immunity, vaccination coverage, infection dynamics, and underdetection of notified infections over time [1]. As a partial substitute, several individual studies tried to bridge this gap, e.g. by providing estimates of population immunity at defined time points early in the pandemic [2,3,4,5,6,7,8]. However, these studies were often cross-sectional and could not inform real-time infectious disease modelling rapidly and continuously enough to serve as a basic and pivotal information layer for what needed to be communicated to political decision makers [9].
The absence of centrally organised population panels resulted in a lack of data suited to provide evidence on population immunity in Germany after the summer of 2022. Additionally, there was relevant uncertainty regarding the choice of adequate endpoints for correlates of the levels of protection against infection or severe COVID-19 that would allow their use in real-time decision-making [9].
To derive estimates of protection levels against SARS CoV-2 infection and severe COVID-19 in the German general population, the IMMUNEBRIDGE project was established within the Network of University Medicine (NUM). It aimed to bring together established large population-based cohorts with newly designed cross-sectional studies by using central data linkage structures, targeted literature synthesis, and central laboratory infrastructure, to allow the preparation of action plans for winter 2022/23. The results of this study were made available rapidly to decision makers and the public; furthermore, rapid and continuous communication of the results to a newly established modelling network for severe infectious diseases (MONID) was essential to allow usage of results in the communication of harmonised scenario modelling from this network to decision makers and the public.
Here, we report estimates for the level of protection against SARS-CoV-2 infection and severe COVID-19 from nine epidemiological studies surveying 33,637 participants between June and November 2022 based on a combined endpoint developed for this study.
Methods
The IMMUNEBRIDGE project aimed to provide a comprehensive picture of the protection level within the German population against SARS-CoV-2 infection and severe COVID-19 from June to November 2022 using existing population-based cohort studies and newly set-up cross-sectional studies. Antibodies against the spike (S-) and nucleocapsid (N-) antigen of SARS-CoV-2 were measured within the participating studies, and seropositivity proportions for predefined subgroups (age, sex, and comorbidities) were derived. In addition, information on self-reported vaccination and infection history of the study participants were obtained. These data were harmonised across participating studies using a jointly developed minimal data set (MDS). The project was structured to enable early ad hoc feedback to consortia of a newly established modelling network for severe infectious diseases (MONID)[10] from early August 2022 onwards. For this, aggregated data were presented in a model-usable format in two interim reports in August [11] and October 2022 [12] to support the MONID modelling consortia. Within the framework of IMMUNEBRIDGE, a targeted literature synthesis was carried out to derive a categorisation of protection levels against infection and severe COVID-19 into a "combined endpoint" based on self-reported infections/vaccinations and immune correlates (Table 1 and Online Resource 2).
Participating studies
From June to the end of November 2022, new survey rounds on vaccination status and previous infections were performed, blood samples were collected, and antibodies against SARS-Cov-2 were measured in four existing population-based cohort studies: the ELISA-Study [7, 13], MuSPAD [4], the German National Cohort (NAKO) [8], and STAAB [5]. Four new cross-sectional studies were set up, one to provide regional depth (GUIDE Study; DRKS00029693 [6]) and three to provide relevant data on children (studies of the University Hospitals in Dresden (adolescents; DRKS00022549), Bochum (school children) [2], and Würzburg (pre-school children; Wü-Kita-CoV) [3, 14]). Studies were included if they were able to quickly survey and sample in the general population regionally or supra-regionally, and provide the MDS. For efficiency reasons, the GUIDE study used a self-sampling method in which capillary blood was collected by the participants themselves and put on dried blood cards. For all other studies, venous blood samples were collected on-site. The principle desirable characteristics of epidemic panels such as speed, adaptability, and linkage to other sources were realised differently in the participating studies. If some characteristics were not available in a particular study, the network format of the project ensured that these aims could be reached for the overall project. For example, not all studies were able to collect samples in June 2022, but this was compensated by the capacity of other studies or study sites to do this. Further, as not all studies were able to provide regional depth, other studies were built up for this purpose (Online Resource 1 Table S1).
In addition to the population-based studies, a prospective hospital-based study called IMMUNEBRIDGE_ED was conducted by the Central Emergency Department of the University Medical Center Göttingen to provide information on defined risk groups not covered in sufficient depth by the available population-based studies. Inclusion criteria for IMMUNEBRIDGE_ED comprised geriatric patients as well as patients with pre-existing immunodeficiency or severe pre-existing diseases. We followed STROBE as a reporting guideline for observational studies [15]. Further information on the participating studies, such as eligibility criteria, can be found in cohort profile publications of these studies [2,3,4,5,6,7, 16] (Online Resource 1 Table S1).
For all participating studies, local ethics committees` votes were obtained prior to the start of the IMMUNEBRIDGE project. Participants and patients were included only after written informed consent in each clinical study.
Laboratory analyses
The serum samples obtained in the STAAB, MuSPAD, ELISA, all children cohorts and IMMUNEBRIDGE_ED by on-site blood collection were analysed in the Institute of Clinical Chemistry and Laboratory Medicine in Oldenburg. Serum samples from NAKO were analysed in the Institute of Clinical Chemistry and Laboratory Medicine in Greifswald. The Elecsys® Anti-SARS-CoV-2 S and Elecsys® Anti-SARS-CoV-2 NC (both Roche Diagnostics, Mannheim, Germany) were used to determine the quantitative antibody response to the S- and qualitative antibody response to the N-antigen of SARS-CoV-2. All antibody measurements were provided as BAU/ml (BAU: Binding Antibody Units; S-antigen) or a ratio (N-antigen). Seropositivity to the S-antigen was defined as ≥ 0.80 BAU/ml, seropositivity to the N-antigen as being above the cut-off index of 1.0.
For GUIDE, capillary blood was collected by the participants themselves, put on dried blood cards (Ahlstrom-Munksjö TFN 460), and sent by mail to the laboratory MVZ Labor Krone GbR (Bad Salzuflen). To analyse the dried blood spot (DBS) samples, the Anti-SARS-CoV-2-QuantiVac ELISA (IgG) was used for the S-antigen and the Anti-SARS-CoV-2-NCP ELISA (IgG) for the N-antigen. Both assays have been validated for use with sample material from DBS cards by both the manufacturer and the performing laboratory. Seropositivity against the S-antigen was defined as ≥ 35.2 BAU/ml, against the N-antigen as a ratio of > 1.0. In the main analysis, DBS samples with borderline findings (ratio ≥ 0.8 to ≤ 1.0 for the N-antigen and ≥25.6 to <35.2 BAU/ml for the S-antigen) were defined as seropositive. This represents a conservative estimate of the waning function with the aim not to underestimate true protection in the population (as a positive antibody response served only as a confirmation of a self-reported infection in the main analysis).
Data collection and linkage
Data pooling took place using the Serohub (www.serohub.net) based on the MDS previously agreed on with the participating studies. The Serohub was designed during the SARS-CoV-2 pandemic as a digital tool able to link and collect individual participant data using common data sharing and MDS documents. In the MDS, variables regarding demographic, socioeconomic, and medical characteristics of participants were agreed on, and reporting categories of these variables were defined. Furthermore, variables regarding test characteristics, assay results, and reporting categories were fixed (Online Resource 1 Table S2).
Combined endpoint for protection levels against SARS-CoV-2 infection and severe course of disease and data analysis
As a proxy for protection levels against SARS-CoV-2 infection and severe course of disease, we formed four categories of protection levels based on a targeted literature review and associated them with graded levels of protection against (re-)infection and severe COVID-19 (Table 1). These four categories were based on a combination of the number of self-reported previous infections and vaccinations and the current antibody status against the N- and S-antigen; as the categories are based on a combination of infection, vaccination and antibody status, we will refer to this categorisation as the “combined endpoint” from here onwards. The number of previous self-reported infections and vaccinations will be denoted as “exposures” from hereafter. We defined a confirmed exposure as a self-reported infection or vaccination with a corresponding humoral immune correlate (antibody to N-antigen for infection, antibody to S-antigen for vaccination).
The four combined endpoint categories are as follows (highest to lowest protection levels): 3 + 1 confirmed exposures (with at least one confirmed exposure in 2022), corresponding to the highest level of protection; 3 confirmed exposures (regardless of the timing of the exposures); 1– < 3 confirmed exposures (regardless of the timing of the exposures); and 0 exposures, indicating no protection (Table 1).
The combined endpoint was reported stratified by age groups, self-reported comorbidities (hypertension, diabetes, lung diseases, cardiovascular diseases, cancers, diseases leading to immunosuppression), and self-reported sex. All estimates represent results that were age standardised according to the 2021 population status update of the 2011 German census of the Federal Statistical Office using the survey package in R [17, 18]. Results that were not age standardised can be found in Online Resource 1. In addition, the combined endpoint was presented stratified according to Nomenclature des Unités territoriales statistiques (NUTS) 2 regions as well as federal states (NUTS 1), using the R package eurostat [19]. NUTS divides areas of the European Union into three levels, allowing for cross-border comparisons [20].
In the analyses comparing vulnerable groups from the population-based studies with the IMMUNEBRIDGE_ED cohort, the results of the population-based cohorts were age standardised according to the age distribution in the IMMUNEBRIDGE_ED comorbidity groups.
Sensitivity analyses
In the sensitivity analyses, we assessed the combined endpoint if only self-reported information on infection and vaccination and no humoral immunity correlates for confirmation were included. Additionally, we evaluated the combined endpoint and seropositivity if DBS samples with borderline N-antigen findings (ratio ≥ 0.8 to ≤ 1.0) were treated as seronegative to provide a lower bound of protection levels compatible with the antibody analysis.
All analyses were carried out in R version 4.1 and 4.2 [21].
Results
General
A total of 33,637 participants from 9 studies surveyed between June and November 2022 were included. Online Resource 1, Table S1 describes the different participating studies, and Table 2 shows the baseline characteristics of the participants in these studies.
Combined endpoint for protection levels against SARS-CoV-2 infection and severe COVID-19
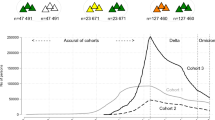
In the adult age groups, between 5% (of those over 79 years old) and 16% (of those 30–39 years old) of individuals had less than three confirmed exposures (Table 3, Fig. 1A). Among persons over 79 years of age, 37% had less than four antibody-confirmed exposures (Table 3, Fig. 1A). Among children and adolescents, 80% had less than three confirmed exposures, and 13% had neither a reported exposure nor an immunocorrelate. We found no relevant differences in the results when treating borderline antibody findings of the GUIDE study as seronegative (Online Resource 1 Figure S6).
A The combined endpoint on the proportion of exposures by infection or vaccination with corresponding humoral immune response, stratified by age; for definition of combined endpoint see Table 1; B the combined endpoint of the proportion of exposures by infection or vaccination regardless of a humoral immune response, stratified by age; C seropositivity against the S-antigen and D against the N-antigen by age, with 95% confidence intervals. Participants from IMMUNEBRIDGE_ED were excluded from this analysis. The combined endpoint could not be formed for 12,185 participants due to missing information from the participants from NAKO (n=10,595) and for additional 1,590 participants from the other cohorts. Vaccination recommendations for children differed from those for adults, recommendations of > 1 dose only currently exist for those > 11 years old
Among adults with self-reported comorbidities, 46–56% (depending on the pre-existing comorbidity) had less than four confirmed exposures and 5–10% had less than three confirmed exposures (Table 3).
When ignoring antibody results and building categories based on reported exposures only, the proportion of those with less than three exposures was lower in all age groups. However, the proportion of those with no reported exposure was higher, in particular in the age group under 18 years (Fig. 1B). While seropositivity against the N-antigen decreased with older age (Fig. 1D), this was not the case for seropositivity against the S-antigen, where a difference is only seen between children (80%) and adults (> 95%; Fig. 1C).
Figure 2A–F visualises the relative frequencies of the levels of the combined endpoint and seropositivity estimates on maps of Germany stratified by NUTS 2 units (usually German administrative districts). The combined endpoint is shown over time from June to September in Online Resource 1 Figure S1, over NUTS-2 regions in Online Resource 1 Figure S2, and over federal states in Online Resource 1 Figure S3. The combined endpoint could not be formed for 12,185 participants due to missing information from the participants from NAKO (n = 10,595) and for an additional 1,590 participants from the other cohorts. This was largely due to missing results from antibody tests due to difficulties in collecting blood for the DBS samples by the participants themselves and the resulting insufficient amount of sample material in the GUIDE study. Overall, between 0 and 12% of participants in all participating studies had missing laboratory results. In the GUIDE study, a higher proportion of missing lab results was seen among people in the older and very old age groups because of self-sampling. For between 0 and 13% of the study participants in the participating studies, information about vaccination and infection was missing.
Age-standardised maps stratified by NUTS 2 region displaying (A–D) the combined endpoint of A no exposures, B 1 to < 3 confirmed exposures, C 3 confirmed exposures, D 3 confirmed exposures and a confirmed exposure in 2022 and (E, F) seropositivity against E the S-antigen and F the N-antigen. Only data from the adult, population-based, cross-sectional studies and cohorts (GUIDE, MuSPAD, NAKO, STAAB) are included in this analysis
Seroprevalence against the S- and N-antigen of SARS-CoV-2
Across all age groups, 95% of the study participants had antibodies against the S-antigen. In the age group 1–17 years, this proportion was lowest with 80% (Fig. 1C; Table 3).
Across all age groups, 52% of the study participants had antibodies against the N-antigen. This proportion was highest in the age group 1–17 at 68% and lowest in people over 79 years of age at 28%; overall, there was a trend of decreasing proportions of antibodies against the N-antigen with increasing age (Fig. 1D; Table 3). A lower proportion of older people (over 64 years of age) and people with comorbidities had antibodies against the N-antigen (Table 3). An antibody response against the N-antigen was present in 71% of participants who reported a first infection in 2020, in 76% of those who reported a first infection in 2021, and in 84% of those with a first reported infection in 2022 (Table 3). 25% of participants who reported no infection showed antibodies against the N-antigen (Table 3).
In participants reporting the first infection after being vaccinated at least two times, seropositivity for antibodies against the N-antigen was 89% up to 5 months after infection and dropped to 68% in those with reported infections longer than 5 months ago. This was similar albeit slightly less pronounced in persons without vaccination (91% up to 5 months and 76% after 5 months). This corresponded to markedly lower titre levels against the N-antigen in those participants of the GUIDE study with infections after at least two vaccinations compared to those with infections without vaccination and a higher decrease in antibody titres after 5 months amongst vaccinated persons.
Regional heterogeneity
In relation to NUTS 2, the proportion of people with less than three confirmed exposures was highest in Dresden (28%) and lowest in Schleswig–Holstein (4%; Fig. 2, Online Resource 1 Figure S2). The proportion of people who had antibodies against the N-antigen ranged from 37% in Lüneburg to 60% in Leipzig (Fig. 2).
Comparison of data between population-based and hospital-based studies
In the hospital-based study IMMUNEBRIDGE_ED, the proportion of study participants who had less than three confirmed exposures (between 11 and 14%) was higher than that in the analogous strata in the population-based studies (between 4 and 7%; Fig. 3).
Comparison of (A) the combined endpoint and (B, C) seropositivity against the S- and N-antigen between the population-based studies and IMMUNEBRIDGE_ED in patients with cancer, cardiovascular disease (CVD), diabetes, hypertension, immunosuppression (IS), and lung disease. Post-stratification weights based on the age distribution in IMMUNEBRIDGE_ED comorbidity groups were applied to the population-based data
Compared to the population-based studies, there were lower or similar proportions of study participants with antibodies against the S-antigen and against the N-antigen in IMMUNEBRIDGE_ED in the higher age groups and defined comorbidity groups (Fig. 3).
Discussion
We showed within the IMMUNEBRIDGE project that a network of existing cohort studies and newly established cross-sectional studies were able to successfully provide model-usable estimates of levels of protection against infection and severe COVID-19 within 2 months of the start of sampling (first interim report in August 2022) and with high geographical resolution (up to NUTS-2). This was achieved by combining the advantages of established large population-based cohorts and newly designed cross-sectional studies, by using central data linkage structures and central laboratory infrastructures, and by collaboratively scaling up capacities for surveys and data analysis across various institutions in Germany. Continuous and rapid reporting of available results was achieved between August 2022 [11] and October 2022 [12] by direct communication to a newly established Modelling Network for Severe Infectious Diseases (MONID) [12]. Different modelling groups simulated possible further pandemic courses for the 2022/23 winter based on the provided data [10, 22].
By combining study results with the existing literature as well as the infection dynamics in the period of the survey, we noted that there was a moderate to high protection against severe COVID-19 (with the SARS-CoV-2 variant "Omicron BA.5" dominating in Germany at that time) in most age groups. Despite the high prevalence of antibodies against the S-antigen (95%) and N-antigen (52%) in the population, there was, however, low protection against infection, as confirmed by both the first BA.5 wave taking place when the surveys were performed as well as the second BA.5 wave in autumn 2022. Our results are in line with preliminary results from both the RKI-SOEP and the SeBluCo study based on data from February to March 2022 published in October and December 2022, and align with modelling results from the UK based on continuous population-based estimates available from large national population panels [9, 23, 24].
We identified gaps in protection against severe COVID-19 in people with pre-existing comorbidities as well as in certain population groups and in different regions of Germany. Among those with comorbidities, 49–56% had less than four confirmed exposures; 6–9% had less than three. The proportion of individuals with less than three confirmed exposures ranged from 4 to 28% across the NUTS2 regions.
Analyses for vulnerable populations with severe comorbidities in IMMUNEBRDIGE_ED indicated that relevant gaps still exist in risk groups. The proportion of study participants who had less than three confirmed exposures was considerably higher in IMMUNEBRIDGE_ED than in the analogous strata in the population-based studies. This is most likely due to a combination of two phenomena: an accumulation of those persons with less protection in the emergency department and the fact that studies in the emergency department reach participants of those groups that population-based studies may find difficult to recruit. The extent to which each of these two phenomena explain the gap found here between population- and hospital-based results could be estimated in future modelling studies and would support efforts to understand generalisability of results from population-based studies to the German population [27].
In our results, there were also relevant differences between children or adolescents compared to adults. The clearly lower proportion of children (80%) with antibodies against the S-antigen results probably from a high proportion of unvaccinated children (62%). This reflects the different vaccination recommendation of the Standing Commission on Vaccination (STIKO) in this age group, recommending COVID-19 vaccinations initially only for adolescents and children with comorbidities (Online Resource 1 Table S3). In contrast, the proportion of children with antibodies against the N-antigen following infection was 68%, i.e. the highest of all age groups (Table 3), although the proportion of children with self-reported infections (46%) was similar to the average of the adult age groups (Online Resource 1 Table S4). The reasons for this discrepancy could be a higher proportion of oligo- or asymptomatic courses of infection in this age group, a longer lasting measurable immune response after infection, or an increased proportion of children compared to adults with an infection in more recent waves of the pandemic, especially during the circulation of the Omicron BA.5 variant.
Even if the proportion of persons with low protection initially seemed small compared to the majority of people with high protection, the infection of no more than 4% to 8% of the total population by the Wuhan and the delta variant of SARS-CoV-2 in the second and fourth wave of the pandemic at the end of 2020 and 2021 already led to a significant burden in the outpatient and inpatient care sector [9]. This indicates that even small gaps of protection against severe COVID-19 may become relevant, in particular in light of waning immunity over the coming months and years [9, 25, 26].
Even though all included studies define a respective source population, they ultimately only provide a picture of the respective reference population with respect to predefined variables (e.g., age, sex, educational status). In addition, the under-recruitment of vaccination-averse groups across all studies may have led to an overestimation of protection. IMMUNEBRIDGE provides information on the presence of a humoral immune response against the S- and N-antigen of SARS-CoV-2, but not on the presence of neutralising activity or cellular immunity. However, such analyses were within the scope of some of the participating studies. There, an increasing activity of neutralising antibodies against the S-antigen for Wuhan and BA.5 variants could be detected with higher categories of the combined endpoint [22]. The extent to which an antibody response is actually associated with a protective effect against infection or a severe course after infection is strongly dependent on the SARS-CoV-2 variant circulating. Our analysis also does not fully take into account that the probability of developing seropositivity to the N-antigen potentially depends on the vaccination history of the infected persons [28]. Here, this may have led to an underestimation of the number of exposures in the group of vaccinated individuals.
In conclusion, we were able to quickly harmonise data collection, surveys, and data analysis across a network of nine existing and newly established population- and hospital-based studies to provide age-specific and regional estimates of protection levels against infection and severe COVID-19 in Germany. The combination of literature, data and infection dynamics during the survey period indicated moderate to high protection against severe COVID-19 with the BA.5 variant in most age groups, but low protection against infection in all age groups. The integration of this knowledge into current modelling studies that are required to reliably interpret the potential effects on infection dynamics was enabled by rapidly communicating preliminary results to a new modelling network for severe infectious diseases in Germany. Results of the IMMUNEBRIDGE project thus reflect the importance of networks covering a large number of scientific institutions in Germany when supported by relevant infrastructural and personnel resources.
References
Beermann S, Dörr M, Grill E, Karch A, Lange B, Zeeb H. Coronapandemie: Die Rolle epidemiologischer Forschung in Gesundheitskrisen. Dtsch Arztebl. 2022;119:753–6.
Brinkmann F, Diebner HH, Matenar C, Schlegtendal A, Spiecker J, Eitner L, et al. Longitudinal rise in seroprevalence of SARS-CoV-2 infections in children in western germany—a blind spot in epidemiology? Infect Dis Rep. 2021;13:957–64.
Engels G, Forster J, Streng A, Rücker V, Rudolph P, Pietsch F, et al. Acceptance of different self-sampling methods for semiweekly SARS-CoV-2 testing in asymptomatic children and childcare workers at german day care centers: a nonrandomized controlled trial. JAMA Netw Open. 2022;5:e2231798-e.
Gornyk D, Harries M, Glöckner S, Strengert M, Kerrinnes T, Heise J-K, et al. SARS-CoV-2 seroprevalence in germany: a population-based sequential study in seven regions. Dtsch Arztebl Int. 2021;118:824.
Eichner FA, Gelbrich G, Weißbrich B, Dölken L, Kurzai O, Deckert J, et al. Seroprävalenz von COVID-19 und psychosoziale Auswirkungen in der Allgemeinbevölkerung: Ergebnisse des STAAB-COVID-One Programms. Gesundheitswesen. 2021;83:965–75.
Schulze-Wundling K, Ottensmeyer PF, Meyer-Schlinkmann KM, et al. Immunity Against SARS-CoV-2 in the German Population [published online ahead of print, 2023 May 12]. Dtsch Arztebl Int. 2023;(Forthcoming):arztebl.m2023.0072. https://doi.org/10.3238/arztebl.m2023.0072.
Klein C, Borsche M, Balck A, Föh B, Rahmöller J, Peters E, et al. One-year surveillance of SARS-CoV-2 transmission of the ELISA cohort: a model for population-based monitoring of infection risk. Sci Adv. 2022;8:5016.
Peters AGK, Goettlicher S, Ahrens W, Albrecht M, Bamberg F, Baernighausen T, et al. Framework and baseline examination of the German National Cohort (NAKO). Eur J Epidemiol. 2022;37:1107.
Neuhauser H, Buttmann-Schweiger N, Ellert U, Fiebig J, Hövener C, Offergeld R, Prütz F, Sarganas G, Schaade L, Schaffrath Rosario A, Thamm R, Zimmermann M, Poethko-Müller C: Seroepidemiologische Studien zu SARS-CoV-2 in Stichproben der Allgemeinbevölkerung und bei Blut-spenderinnen und Blutspendern in Deutschland –Ergebnisse bis August 2021 Epid Bull 2021;37:3–12. https://doi.org/10.25646/8999.
Berndt JC, T, Hasenauer, J, Karch, A, Kheifetz, Y, Kirsten, H, Krueger,et al. A. Szenarien für den Verlauf der SARS-CoV-2-Pandemie im Winter 2022/23 - Ergebnisse eines Workshops des Modellierungsnetzes für schwere Infektionskrankheiten (Modellierungsnetz). Zenodo, 2022. https://doi.org/10.5281/zenodo.7126032.
Lange B, Jaeger V, Rücker V, Hassenstein MJ, Harries M, Berner R, et al. Interimsanalyse des IMMUNEBRIDGE-Projektes zur Kommunikation von vorläufigen Ergebnissen an die Modellierungskonsortien der BMBF-geförderten Modellierungsplattform. Zenodo. 2022. https://doi.org/10.5281/zenodo.6968574.
Lange B, Jäger, V, Rücker, V, Harries, M, Hassenstein, MJ, Dreier M, et al. 2. Interimsanalyse des IMMUNEBRIDGE-Projektes zur Kommunikation von vorläufigen Ergebnissen an das Modellierungsnetz für schwere Infektionskrankheiten. Zenodo, 2022. https://doi.org/10.5281/zenodo.7177592.
Balck A, Föh B, Borsche M, Rahmöller J, Vollstedt E-J, Waldeck F, et al. Protocol of the Luebeck longitudinal investigation of SARS-CoV-2 infection (ELISA) study–a prospective population-based cohort study. BMC Public Health. 2022;22:1–9.
Engels G, Oechsle AL, Schlegtendal A, et al. SARS-CoV-2 sero-immunity and quality of life in children and adolescents in relation to infections and vaccinations: the IMMUNEBRIDGE KIDS cross-sectional study. Infection. 2022;2023:1–9. https://doi.org/10.1007/s15010-023-02052-5.
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2014;12:1495–9.
German National Cohort (GNC) Consortium. The German National Cohort: aims, study design and organization. Eur J Epidemiol. 2014;29(5):371–82. https://doi.org/10.1007/s10654-014-9890-7.
Destatis - Statistisches Bundesamt. https://www-genesis.destatis.de/genesis/online?operation=previous&levelindex=0&step=0&titel=&levelid=1689661127749&acceptscookies=false
Lumley T (2004) Analysis of complex survey samples. J Stat Softw 9(1):1–19. R package verson 2.2.
Lahti L, Huovari J, Kainu M, Biecek P. Retrieval and analysis of eurostat open data with the eurostat package. The R Journal. 2017;9:385.
Commission E. Eurostat. TERCET Flat Files 2021 [Available from: https://gisco-services.ec.europa.eu/tercet/flat-files.
R Core Team R. R: A language and environment for statistical computing. R foundation for statistical computing Vienna, Austria; 2018.
Harries M, Jäger V, Rodiah I, Hassenstein MJ, Ortmann J, Dreier M, et al. Bridging the gap-estimation of 2022/2023 SARS-CoV-2 healthcare burden in Germany based on multidimensional data from a rapid epidemic panel. medRxiv. 2022;83:965. https://doi.org/10.1101/2022.12.30.22284061.
Barnard RC, Davies NG, Jit M, Edmunds WJJNC. Modelling the medium-term dynamics of SARS-CoV-2 transmission in England in the Omicron era. Nat Commun. 2022;13:1–15.
RKI. Corona-Monitoring bundesweit – Welle 2 (aktualisierte Version vom 14.12.2022). 2022; accessed at https://www.rki.de/DE/Content/Gesundheitsmonitoring/Studien/lid/Factsheet-CoMoBu-Welle-2.pdf?__blob=publicationFile.
Kleeblattprinzip: 93 Coronaintensivpatienten verlegt, das Konzept funktioniert: Deutsches Ärzteblatt; 2021 [Available from: https://www.aerzteblatt.de/nachrichten/129956/Kleeblattprinzip-93-Coronaintensivpatienten-verlegt-das-Konzept-funktioniert.
Faensen D, Claus H, Benzler J, Ammon A, Pfoch T, Breuer T, et al. SurvNet@ RKI–a multistate electronic reporting system for communicable diseases. Eurosurveillance. 2006;11:7–8.
Kuss O, Becher H, Wienke A, Ittermann T, Ostrzinski S, Schipf S, et al. Statistical Analysis in the German National Cohort (NAKO)–specific aspects and general recommendations. Eur J Epidemiol. 2022;37:429.
Follmann D, Janes HE, Buhule OD, Zhou H, Girard B, Marks K, et al. Antinucleocapsid antibodies after SARS-CoV-2 infection in the blinded phase of the randomized, placebo-controlled mRNA-1273 COVID-19 vaccine efficacy clinical trial. Ann Intern Med. 2022;175:1258–65.
Acknowledgements
The authors gratefully acknowledge all participants for their contribution, as well as the colleagues for data collection, in particular BOS112 and Heike Adam for the lab management, as well as Barbora Kessel for MuSPAD data management and Timo Ludwig for STAAB data management. We thank all participants who took part in the NAKO study and the staff of this research initiative. We thank the Federal State of Saxony for supporting the SchoolCoviDD19 (SchoolCoviDD19 (paedSAXCOVID) by a financial grant. We thank the Bavarian State Ministry of Health and Care/State Office for Health and Food Safety for supporting Wü-KiTa-CoV by a financial grant. We thank Josephine Schneider for her excellent organisation of the SchoolCoviDD19 (paedSAXCOVID) study.
Funding
Open Access funding enabled and organized by Projekt DEAL. IMMUNEBRIDGE is a research project funded by the Federal Ministry of Education and Research (BMBF) through the Network University Medicine (NUM) (FKZ 01KX1021). The central laboratory analysis in Oldenburg and Greifswald for the population-based cohort studies was financed via the IMMUNEBRIDGE project. Online Resource 1 Table S1 gives an overview of the basic funding for data collection for each study. The IMMUNEBRIDGE_ED study was conducted with a hospital-based approach at the Central Emergency Department of the University Medical Center Göttingen and funded by intramural funds. This project was conducted with data from the German National Cohort (NAKO) (www.nako.de). The NAKO is funded by the Federal Ministry of Education and Research (BMBF) [project funding reference numbers: 01ER1301A/B/C, 01ER1511D and 01ER1801A/B/C/D], federal states of Germany and the Helmholtz Association, the participating universities and the institutes of the Leibniz Association. The STAAB study received funding by the BMBF (01EO1004 and 01EO1504); the STAAB COVID program was funded by the Bavarian State Ministry for Science and Art (Aktenzeichen U.7-H4001.1.7/24/2). This work was performed as part of the project ‘Integrated Early Warning System for Local Recognition, Prevention, and Control for Epidemic Outbreaks’ (LOKI), which is funded by the Initiative and Networking Fund of the Helmholtz Association (grant agreement number KA1-Co-08). It was further supported by the Federal Ministry of Education and Research (BMBF) via the RESPINOW (grant number: MV2021-012) and OptimAgent (grant number: MV2021-014) projects.
Author information
Authors and Affiliations
Contributions
Conceptualisation: BL, AK, NT, AP, PH, HS, SB. Data quality: VKJ, MAK, MH, MJH, JO, VR. Formal analyses: VKJ, MJH, BL, AK, MH, AB, VR. Visualisation: VKJ, VR, AB. Project administration: BL, AK, CK, FB, NT, JL, SB, HS, PH. Laboratory analysis: AP, MN, GB, DR, KB, MF, TW, NT, FB, JL. Evidence synthesis: BL, MD, IvH, MB, OH. Writing—original draft: BL, VKJ, AK, Funding acquisition: HS, SB, BL, AK. Writing—review and editing: all. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
CK serves as a medical advisor to Centogene and Retromer Therapeutics and has received speaking honoraria from Desitin and Bial.
Ethical approval
The responsible ethics committees of individual studies approved all study-related analyses: GUIDE: 202/22 approved by the Ethics Committee of the Medical Faculty of the Rheinische Friedrich-Wilhelm-University Bonn. ELISA: University of Lübeck (Az. 20–150). NAKO: The study is continuously approved by the responsible local ethics committees of the German Federal States where all study centers are located in (original ethics approvals of the leading ethics committee of the Bayerische Landesärztekammer (protocol code 13023, Approval Date: 27 March 2013 and 14 February 2014 (rectification of documents, study protocol, consent form)). An external ethics advisory board has been established that accompanies NAKO over the full study period. A 'Code of Ethics' of NAKO (Ethikkodex) has been developed and the study is under steady surveillance by the ethics committees of the regional study centers [8]. STAAB: Ethics committee of the Medical Faculty of the University Würzburg (STAAB: #98/13). MuSPAD: Ethics committee of Hannover Medical School (9086_BO_S_2020 for MuSPAD), Dresden paedSAXCOVID: Ethics Committee of the Technische University (TU) Dresden (BO-EK-156042020). Bochum CorKID: Ethics Committee of the Ruhr University Bochum (Nr. 20-6927_7). Würzburg Wü-KITa-CoV: Würzburg, Kennzeichen 105/21. IMMUNEBRIDGE_ED: Ethics Committee of University Medical Center Göttingen (21/6/22).
Availability of data and materials
The aggregated data for this study will be made available to other academic researchers. The minimum dataset includes study site information, assay information, sample type, demographic information, self-administered diagnostic anamneses and lab results (NC, S Spike, IGRA and NAb). Institutions can apply for the data via serohub@helmholtz-hzi.de. Data were provided to the modelling network for severe infectious diseases in Germany (MONID [13]).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lange, B., Jaeger, V.K., Harries, M. et al. Estimates of protection levels against SARS-CoV-2 infection and severe COVID-19 in Germany before the 2022/2023 winter season: the IMMUNEBRIDGE project. Infection 52, 139–153 (2024). https://doi.org/10.1007/s15010-023-02071-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-023-02071-2