Abstract
Objective
The aim of our study was to build a predictive model able to stratify the risk of bacterial co-infection at hospitalization in patients with COVID-19.
Methods
Multicenter observational study of adult patients hospitalized from February to December 2020 with confirmed COVID-19 diagnosis. Endpoint was microbiologically documented bacterial co-infection diagnosed within 72 h from hospitalization. The cohort was randomly split into derivation and validation cohort. To investigate risk factors for co-infection univariable and multivariable logistic regression analyses were performed. Predictive risk score was obtained assigning a point value corresponding to β-coefficients to the variables in the multivariable model. ROC analysis in the validation cohort was used to estimate prediction accuracy.
Results
Overall, 1733 patients were analyzed: 61.4% males, median age 69 years (IQR 57–80), median Charlson 3 (IQR 2–6). Co-infection was diagnosed in 110 (6.3%) patients. Empirical antibiotics were started in 64.2 and 59.5% of patients with and without co-infection (p = 0.35). At multivariable analysis in the derivation cohort: WBC ≥ 7.7/mm3, PCT ≥ 0.2 ng/mL, and Charlson index ≥ 5 were risk factors for bacterial co-infection. A point was assigned to each variable obtaining a predictive score ranging from 0 to 5. In the validation cohort, ROC analysis showed AUC of 0.83 (95%CI 0.75–0.90). The optimal cut-point was ≥2 with sensitivity 70.0%, specificity 75.9%, positive predictive value 16.0% and negative predictive value 97.5%. According to individual risk score, patients were classified at low (point 0), intermediate (point 1), and high risk (point ≥ 2). CURB-65 ≥ 2 was further proposed to identify patients at intermediate risk who would benefit from early antibiotic coverage.
Conclusions
Our score may be useful in stratifying bacterial co-infection risk in COVID-19 hospitalized patients, optimizing diagnostic testing and antibiotic use.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bacterial co-infections have been associated with a huge increase in patient morbidity and mortality during influenza pandemics [1]. Such experience has prompted physicians to start empiric antibiotic coverage in patients hospitalized with COVID-19 [2]. In addition, several guidelines have recommended to initiate antibiotics within 1–4 h from hospital admission in patients with COVID-19 suspected of having bacterial co-infection and/or with criteria of sepsis or septic shock [3]; https://www.who.int/publications/i/item/clinical-management-of-covid-19; https://www.nice.org.uk/guidance/ng173).
Current literature shows that the rate of bacterial co-infection at hospital admission in patients with COVID-19 ranged from 3.5 to 11.6%, increasing to 14% among those with severe/critical disease who required intensive care [4,5,6]. However, more than two third of hospitalized patients were started on antibiotics [5,6,7]. Indeed, pre–post cross-sectional studies have revealed significant increase in antibiotic use during the first wave of COVID-19 pandemic compared with prior periods in their hospitals [8, 9]. In some cases, this finding has been associated with a concerning decrease in antibiotic susceptibility to several antibiotic classes among nosocomial pathogens such as Klebsiella pneumoniae [8]. Other reports have underlined an increased isolation of Enterococcus spp. from hospitalized patients with complicated COVID-19 course, probably because of antibiotic selective pressure [10].
Experts have exhorted physicians to not neglect antimicrobial stewardship principles during COVID-19 pandemic to avoid a worsening of the healthcare crisis related to antimicrobial resistance [11]. Thus, physicians are challenged to differentiate COVID-19 patients who may benefit from a prompt antibiotic therapy from those at low risk for co-infection where antibiotic pressure should be avoided. Studies performed to date have underlined a potential role in such discrimination process of biomarkers such as C-reactive protein (CRP), procalcitonin (PCT) and whole blood counts [12,13,14,15]. However, for all of them, low specificity with limited positive predictive value has been reported. Few authors have addressed the predictive role of clinical factors suggesting a role for steroid use, but in such studies also, superinfections were considered [15, 16].
Therefore, the objective of our study was to investigate the risk factors for bacterial co-infection at hospital admission for COVID-19 to create a predictive model able to stratify patients according to their probability of having a community-onset bacterial co-infection useful to guide microbiological work up and antibiotic use.
Methods
Study design
Multicenter observational study of patients hospitalized from February 22 through December 31, 2020, and diagnosed with COVID-19.
Diagnostic testing for COVID-19 and for bacterial co-infection were dictated by local policies and clinical judgement, and were not encompassed by a general protocol.
Clinical charts and hospital electronic records were used as data sources. Pseudo-anonymous data were prospectively collected and managed using REDCap electronic data capture tool, hosted by Alma Mater University of Bologna [17, 18].
The study was approved by the Ethic Committee of the promoting center (Comitato Etico Indipendente di Area Vasta Emilia Centro, n. 283/2020/Oss/AOUBo). Informed consent was obtained contacting patients via email or phone call. In case of deceased or unreachable patients, the informed consent was waived considering the observational nature of the study.
Setting
The study was carried out at the three main hospitals of the metropolitan area of Bologna: (i) S. Orsola-Malpighi Hospital (1420-bed tertiary teaching hospital); (ii) Bellaria Hospital (320-bed tertiary center); and (iii) Maggiore Hospital (870-bed tertiary hospital). A unique infectious disease unit as well as a unique microbiology laboratory serve all the hospitals of the metropolitan area of Bologna.
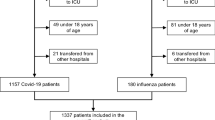
Participants
All consecutive adult (≥18 years) patients hospitalized with confirmed COVID-19 diagnosis by real-time reverse transcription polymerase chain reaction (RT-PCR) on nasopharyngeal swabs (NPS) were included. Patients on palliative care and/or discharged within 72 h from hospital admission were excluded as well as patients who acquired COVID-19 during hospital admission. Patients were followed-up to hospital discharge; those with multiple hospitalizations were included only once.
Variables and definitions
The endpoint variable was a microbiologically documented bacterial co-infection diagnosed within 72 h from hospital admission defined according to clinical guidelines [19,20,21]. All positive microbiological assays were independently revised by two investigators (MR, CC) to confirm the diagnosis of bacterial co-infection against such criteria; any disagreement was resolved by a third senior investigator (MG).
The exposure variables were assessed at hospital admission and included: age, sex, body mass index, underlying conditions such as hypertension, immunosuppression and those included in the Charlson comorbidity index [22]. COVID-19 variables included: (i) date and symptoms at onset; (ii) date and symptoms at hospitalization; (iii) vital signs, laboratory tests and radiological findings. Clinical severity at hospitalization was recorded according to SOFA and CURB-65 scores. The attempt to diagnose bacterial co-infection defined as one or more samples collected for this purpose, the type of samples collected, the assays performed and their results were also recorded.
Sample size
Based on literature data, bacterial co-infection rate among hospitalized patients with COVID-19 was estimated to be on average 8% [4, 5]. According to this, we planned to enroll at least 1600 patients to obtain 100 events with α = 0.10 and power of 90% (two-tailed hypothesis test) [23].
Statistical analysis
The overall cohort of COVID-19 patients was randomly split into 70% of the cohort (derivation) and 30% of the cohort (internal validation) [24]. Descriptive statistics were calculated for the overall cohort as well as for the derivation and validation cohort. Continuous variables were expressed as median and interquartile range (IQR) and compared using Mann–Whitney U test. The assumption of normality of the variables was tested through the skewness and kurtosis test for normality as well as visual inspections. Categorical variables were reported as counts and percentages and compared with Pearson’s chi-squared test or Fisher’s exact test, as appropriate.
To develop the risk score, the analyses were initially performed in the derivation cohort, while the validation cohort was used to validate the predictive model.
Complete case analysis was performed. To investigate risk factors for bacterial co-infection univariable and multivariable logistic regression analyses were performed (i.e. derivation cohort). Odds ratios (ORs) and their corresponding 95% confidence intervals (95% CIs) were estimated. The covariates to be included in the multivariable logistic regression models were selected through a backward stepwise selection strategy (P value for inclusion ≤ 0.1, P value for exclusion > 0.2). Variables were primarily entered according to clinically relevance and lack of collinearity. The full model included the following variables: Charlson index, white blood cells (WBC), procalcitonin (PCT), C-reactive protein (CRP), and hypertension. The reduced model finally retained: Charlson index, WBC, and PCT. WBC was entered as a binary variable on the basis of the median value of coinfected patients, while the cut-offs for the other variables were assigned according to Youden's criterion [25]. Overall goodness of fit was evaluated by Nagelkerke's R2 and Hosmer and Lemeshow goodness of fit. Discrimination of the model was assessed by receiver-operator characteristics (ROC) curve of the predicted probability and Somers' D.
To develop the predictive risk score, variables in the final multivariable logistic regression model (i.e. derivation cohort) were assigned a point value corresponding to β coefficients rounded up to the nearest whole number [26]. The risk score was then calculated by adding individual points and categorized into three classes of risk (i.e. low, intermediate, and high) according to tertiles distribution. To better discriminate the risk for bacterial co-infection at intermediate level, a value of CURB-65 ≥ 2 was applied [27]. An optimized cut-point was then assigned using the Youden's J statistic and performance characteristics at cut-point (i.e. sensitivity, specificity, positive and negative predictive values) were calculated. For internal validation, these findings were then applied to the validation cohort. Discrimination measures were calculated to assess the model’s performance on the validation dataset.
To take into account other applications in clinical setting (e.g. cancer patients) an alternative predictive risk score was developed considering age, COPD, diabetes, renal diseases, and immunosuppression in place of Charlson index along with WBC and PCT (see supplementary Tables 1–3 and supplementary Fig. 1). We performed statistical analyses using Stata 16.1 (Stata Corp., College Station, TX, USA). All statistical tests were two-sided and an alpha error of 0.05 was accepted.
Results
The study cohort consisted of 1811 patients hospitalized during the study period and diagnosed with COVID-19; 78 patients were excluded because they were treated with palliative care (n = 12), died or were discharged within 72 h from hospital admission (n = 43), or COVID-19 was diagnosed after 72 h from hospital admission (n = 23). Thus, 1733 patients were analyzed: 61.4% were males, with median age of 69 years (IQR 57–80), and median Charlson index of 3 (IQR 2–6) (Table 1).
Bacterial co-infection was diagnosed in 110 (6.3%) patients. The most common types of bacterial co-infections were community acquired pneumonia and urinary tract infection that were diagnosed in 46 and 43 patients, respectively. Bloodstream infection at hospital admission was diagnosed in 26 patients, in 13 cases were deemed as primary, in 7 as device-related and in 6 as secondary. The most common causative agents were Streptococcus pneumoniae (n = 32) and Escherichia coli (n = 31) (Table 2).
Patients were randomly divided into derivation (n = 1213) and validation cohort (n = 520). The comparison between derivation and validation cohort in terms of clinical and demographic characteristics is reported in Table 1. The rate of co-infections is 6.0% (73/1213) and 7.1% (37/520) in the derivation and validation cohort, respectively.
Descriptive characteristics of COVID-19 patients with and without bacterial co-infection along with univariable analysis of risk factors are reported in Tables 3 and 4 for derivation and validation cohort, respectively.
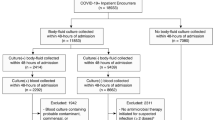
At multivariable analysis in the derivation cohort: WBC ≥ 7.7/mm3, PCT ≥ 0.2 ng/mL, and Charlson index ≥ 5 were risk factors for bacterial co-infection and used for the predictive score (Table 5). For each variable a point was assigned according to the β coefficient rounded up to the nearest whole number. The predictive score resulted from the sum of the individual points and ranged from 0 to 5. In the ROC analysis, AUC was 0.83 (95%CI 0.78–0.88) (Fig. 1a) with Somers' D 0.67 (95%CI 0.57–0.77). Optimal cut-point was identified at risk score ≥ 2 with a sensitivity of 79.4% (95%CI 67.3–88.5%), specificity of 76.4% (95%CI 73.7–79.0%), positive predictive value of 17.2% (95%CI 13.0–22.0%) and negative predictive value of 98.4% (95%CI 97.2–99.1%).
In the validation cohort, the ROC analysis showed an AUC of 0.83 (95%CI 0.75–0.90) (Fig. 1b) with Somers’ D 0.65 (95%CI 0.51–0.80). At optimal cut-point of risk score ≥ 2, we found sensitivity of 70.0% (95%CI 50.6–85.3%), specificity of 75.9% (95%CI 71.7–79.7%), positive predictive value of 16.0% (95%CI 10.2–23.5%) and negative predictive value of 97.5% (95%CI 95.2–98.8%).
According to the suggested risk score, we classified patients at low, intermediate and high risk for bacterial co-infection, considering the value of CURB-65 ≥ 2 as a further element to discriminate patients at intermediate risk who would benefit from early antibiotic coverage (Table 6). The score applicability in terms of performance characteristics in the validation cohort is reported in Table 7. Using the score, 8 patients would be treated for each co-infection as compared to 16 that were treated without any score application.
Considering that the Charlson index could not be applicable in all settings (e.g. cancer patients), an alternative multivariable logistic regression model was developed using age and immunosuppression (in place of the Charlson index) along with WBC and PCT values. Data are shown in supplementary Tables 1–3 and supplementary Fig. 1.
Discussion
We have investigated the rate of and the risk factors for bacterial co-infection, diagnosed within 72 h from hospital admission, in a large cohort of patients hospitalized for confirmed COVID-19 diagnosis. We developed a predictive risk score with few and easily accessible data (i.e. Charlson index, WBC and PCT) to stratify patients at low, intermediate and high risk of bacterial co-infection. For patients at intermediate risk, we propose to use CURB-65 severity score to further discriminate patients who may need early antibiotic coverage. The proposed score could be useful to standardize the approach to the microbiological work-up and to the therapeutic treatment of patients hospitalized for COVID-19 and suspected of having a bacterial co-infection.
As previously reported, we have shown a rate of bacterial co-infection lower than 10%, while the use of antibiotic therapy since the hospital admission was as high as 60% [4, 5]. It is worth mentioning that this rate was similar among patients with and without eventually confirmed bacterial co-infection to stress the difficulties in identifying among patients hospitalized with COVID-19 those with a concomitant bacterial co-infection as several symptoms and signs overlap between the SARS-COV2 infection and its complicated course and the bacterial disease [2, 28, 29]. For this reason, our risk score may be useful to standardize the approach to both the microbiological work-up, that could be avoid in patients at low risk at least in the most critical periods (i.e. pandemic waves, winter periods), and the therapeutic management reserving early antibiotic coverage only for patients at high risk. In addition, to optimize antibiotic use in patients at intermediate risk we propose to use the CURB-65, a well-known and largely used score for the management of patients with community-acquired pneumonia (CAP) [27, 30]. This allowed us to increase in the validation cohort the sensitivity of 13.3% points, and decrease the specificity of 13.6% points, as compared to baseline risk score (i.e. 70.0 and 75.9%, respectively).
Our study has several limitations. First, we limited our analysis only to microbiologically documented bacterial co-infection. Generally, in more than half of CAP the causative pathogens remain unknown despite an appropriate microbiological work-up. Thus, the prevalence of co-infection of the present study, mainly involving the respiratory tract, is likely to be underestimated, and consequently the PPV and NPV of our model may be biased. However, as the approach to clinical diagnosis and therapeutic management of bacterial (co-)infections is varying according to patient setting, clinical severity and physician specialty we have preferred to include only documented episodes to avoid the influence of several confounding factors in the definition of our events. Second, the approach to microbiological diagnosis of bacterial co-infection was not standardized during the study period, as it happened to the vast majority of centers during normal life [31] and even more during COVID-19 pandemic. Indeed, the overwhelmed emergency rooms, the overloading of microbiology laboratories, and the concerns for the safety of healthcare staff may have played a role in the performance and turnaround time of diagnostic testing for bacterial co-infections. However, we observed similar rates and types of bacterial co-infections described in literature suggesting a similar approach across centers dealing with high volume of COVID-19 hospitalizations to the microbiological diagnosis of bacterial co-infection in real life. Finally, the major drawback of randomly splitting the dataset into two parts (i.e. derivation and validation cohort) is that the precision of the fitted parameters will be reduced as only a part of the dataset is used for model derivation; this will also tend to give optimistic estimates of model performance [24]. To obtain reliable estimates, models should be externally validated as well.
To conclude, our study underlines that although the overall rate of bacterial co-infection among patients hospitalized with COVID-19 was lower than 10%, almost 60% of patients were started on antibiotics, and that the rate of antibiotic use was similar among patients with and without co-infection. Thus, our risk stratification in low, intermediate and high risk using a score based on Charlson index (alternatively on age and immunosuppression), WBC and PCT may be useful to guide diagnostic testing and to optimize antibiotic use. To improve its sensitivity in patients at intermediate risk, we also proposed to consider clinical severity using CURB-65, reserving antibiotic coverage only in patients with CURB-65 ≥ 2. External validation is needed to confirm the good performance of our score, and its impact on diagnostic and therapeutic management of hospitalized COVID-19 patients should be investigated.
Change history
25 July 2022
Missing Open Access funding information has been added in the Funding Note.
References
Chertow DS, Memoli MJ. Bacterial coinfection in influenza: a grand rounds review. JAMA. 2013;309:275–82.
Vaughn VM, Gandhi TN, Petty LA, Patel PK, Prescott HC, Malani AN, et al. Empiric antibacterial therapy and community-onset bacterial coinfection in patients hospitalized with coronavirus disease 2019 (COVID-19): a multi-hospital cohort study. Clin Infect Dis. 2021;72:e533–41.
Alhazzani W, Møller MH, Arabi YM, Loeb M, Gong MN, Fan E, et al. Surviving sepsis campaign: guidelines on the management of critically Ill adults with coronavirus disease 2019 (COVID-19). Crit Care Med. 2020;48:e440–69.
Lansbury L, Lim B, Baskaran V, Lim WS. Co-infections in people with COVID-19: a systematic review and meta-analysis. J Infect. 2020;81:266–75.
Rawson TM, Moore LSP, Zhu N, Ranganathan N, Skolimowska K, Gilchrist M, et al. Bacterial and fungal coinfection in individuals with coronavirus: a rapid review to support COVID-19 antimicrobial prescribing. Clin Infect Dis. 2020;71:2459–68.
Langford BJ, So M, Raybardhan S, Leung V, Westwood D, MacFadden DR, et al. Bacterial co-infection and secondary infection in patients with COVID-19: a living rapid review and meta-analysis. Clin Microbiol Infect. 2020;26:1622–9.
Langford BJ, So M, Raybardhan S, Leung V, Soucy JR, Westwood D, et al. Antibiotic prescribing in patients with COVID-19: rapid review and meta-analysis. Clin Microbiol Infect. 2021;27:520–31.
Nori P, Cowman K, Chen V, Bartash R, Szymczak W, Madaline T, et al. Bacterial and fungal coinfections in COVID-19 patients hospitalized during the New York City pandemic surge. Infect Control Hosp Epidemiol. 2021;42:84–8.
Abelenda-Alonso G, Padullés A, Rombauts A, Gudiol C, Pujol M, Alvarez-Pouso C, et al. Antibiotic prescription during the COVID-19 pandemic: A biphasic pattern. Infect Control Hosp Epidemiol. 2020;41:1371–2.
Gaibani P, D’Amico F, Bartoletti M, Lombardo D, Rampelli S, Fornaro G, et al. The gut microbiota of critically ill patients with COVID-19. Front Cell Infect Microbiol. 2021;11:670424.
Huttner BD, Catho G, Pano-Pardo JR, Pulcini C, Schouten J. COVID-19: don’t neglect antimicrobial stewardship principles! Clin Microbiol Infect. 2020;26:808–10.
Mason CY, Kanitkar T, Richardson CJ, Lanzman M, Stone Z, Mahungu T, et al. Exclusion of bacterial co-infection in COVID-19 using baseline inflammatory markers and their response to antibiotics. J Antimicrob Chemother. 2021;76:1323–31.
Wang L, Amin AK, Khanna P, Aali A, McGregor A, Bassett P, et al. An observational cohort study of bacterial co-infection and implications for empirical antibiotic therapy in patients presenting with COVID-19 to hospitals in North West London. J Antimicrob Chemother. 2021;76:796–803.
Pink I, Raupach D, Fuge J, Vonberg RP, Hoeper MM, Welte T, et al. C-reactive protein and procalcitonin for antimicrobial stewardship in COVID-19. Infection. 2021;49:935–43.
He S, Liu W, Jiang M, Huang P, Xiang Z, Deng D, et al. Clinical characteristics of COVID-19 patients with clinically diagnosed bacterial co-infection: a multi-center study. PLoS One. 2021;16:e0249668.
Nasir N, Rehman F, Omair SF. Risk factors for bacterial infections in patients with moderate to severe COVID-19: a case-control study. J Med Virol. 2021;93:4564–9.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81.
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208.
Metlay JP, Waterer GW, Long AC, Anzueto A, Brozek J, Crothers K, et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American thoracic society and infectious diseases Society of America. Am J Respir Crit Care Med. 2019;200(7):e45–67.
Mermel LA, Allon M, Bouza E, Craven DE, Flynn P, O’Grady NP, et al. Clinical practice guidelines for the diagnosis and management of intravascular catheter-related infection: 2009 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2009;49:1–45.
Bonkat G, Cai T, Veeratterapillay R, Bruyère F, Bartoletti R, Pilatz A, et al. Management of urosepsis in 2018. Eur Urol Focus. 2019;5:5–9.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Rosner B, Glynn RJ. Power and sample size estimation for the clustered wilcoxon test. Biometrics. 2011;67:646–53.
Altman DG, Vergouwe Y, Royston P, Moons KG. Prognosis and prognostic research: validating a prognostic model. BMJ. 2009;338:b605.
Fluss R, Faraggi D, Reiser B. Estimation of the Youden Index and its associated cutoff point. Biom J. 2005;47:458–72.
Mehta HB, Mehta V, Girman CJ, Adhikari D, Johnson ML. Regression coefficient-based scoring system should be used to assign weights to the risk index. J Clin Epidemiol. 2016;79:22–8.
Lim WS, van der Eerden MM, Laing R, Boersma WG, Karalus N, Town GI, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax. 2003;58:377–82.
Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents. 2020;55:105924.
Shafran N, Shafran I, Ben-Zvi H, Sofer S, Sheena L, Krause I, et al. Secondary bacterial infection in COVID-19 patients is a stronger predictor for death compared to influenza patients. Sci Rep. 2021;11:12703.
Sharp AL, Jones JP, Wu I, Huynh D, Kocher KE, Shah NR, et al. CURB-65 performance among admitted and discharged emergency department patients with community-acquired pneumonia. Acad Emerg Med. 2016;23:400–5.
Giannella M, Pinilla B, Capdevila JA, Martínez Alarcón J, Muñoz P, López Álvarez J, et al. Pneumonia treated in the internal medicine department: focus on healthcare-associated pneumonia. Clin Microbiol Infect. 2012;18:786–94.
Funding
Open access funding provided by Alma Mater Studiorum - Università di Bologna within the CRUI-CARE Agreement. No external funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest related to the content of this manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visithttp://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Giannella, M., Rinaldi, M., Tesini, G. et al. Predictive model for bacterial co-infection in patients hospitalized for COVID-19: a multicenter observational cohort study. Infection 50, 1243–1253 (2022). https://doi.org/10.1007/s15010-022-01801-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-022-01801-2