Abstract
Purpose
To examine patterns of outpatient and community antibiotic use among adults in five European countries.
Methods
We used healthcare data of 28.8 million adults from six population-based ARITMO project databases to ascertain information on systemic antibiotic use in Denmark (2000–2008), the Netherlands (1999–2010), Italy (2000–2010), the UK (1996–2009), and Germany (2004–2008). We estimated overall, and age-group and sex specific antibiotic use as defined daily doses (DDD) per 1000 inhabitants per day. We computed annual age- and sex-standardized population prevalence of antibiotic use per 1000 persons-years (p-y) and the mean duration (in days) of antibiotic use.
Results
The overall antibiotic use varied from 8.7 DDD per 1000 inhabitants per day in the UK to 18.1 DDD in Denmark, representing a 2.1-fold geographical variation. In all countries, prescribing was relatively high among individuals aged 15–19 years; lower in those aged 20–50 years; and then increased steadily reaching 41.8 DDD per 1000 inhabitants per day in individuals ≥85 years in Denmark. After age- and sex-standardization, prevalence of antibiotic use varied threefold from 160.2/1000 p-y in the UK to 421.1/1000 p-y in Italy. The ratio of broad- to narrow-spectrum penicillin, cephalosporin, and macrolide use varied from 0.6 in Denmark to 120.2 in Italy. Women used more antibiotics than men did in all countries. Across countries, the mean duration of antibiotic use varied 1.3 to 21.1-fold for different antibiotics.
Conclusions
Antibiotic use is high in women and the elderly. Prescribing patterns vary substantially across European countries, both according to overall consumption, user prevalence, duration, and narrow- versus broad-spectrum antibiotics.






Similar content being viewed by others
References
The European Centre for Disease Prevention and Control (ECDC). Antimicrobial resistance surveillance in Europe: annual report of the European Antimicrobial Resistance Surveillance Network (EARS-Net). 2013. http://www.ecdc.europa.eu/en/publications/Publications/antimicrobial-resistance-surveillance-europe-2012.pdf. Accessed 21 Nov 2014.
World Health Organization 2014. Antimicrobial resistance: global report on surveillance. 2014. http://apps.who.int/iris/bitstream/10665/112642/1/9789241564748_eng.pdf?ua=1. Accessed 23 June 2014.
European Centre for Disease Prevention and Control. European Medicines Agency. The bacterial challenge: time to react. 2009. http://www.ecdc.europa.eu/en/publications/Publications/0909_TER_The_Bacterial_Challenge_Time_to_React.pdf. Accessed 20 Jan 2014.
European Centre for Disease Prevention and Control. Surveillance of antimicrobial consumption in Europe 2011. Stockholm: ECDC; 2014. http://www.ecdc.europa.eu/en/publications/Publications/antimicrobial-consumption-europe-surveillance-2011.pdf. Accessed 21 Nov 2014.
Versporten A, Coenen S, Adriaenssens N, Muller A, Minalu G, Faes C, et al. European Surveillance of Antimicrobial Consumption (ESAC): outpatient cephalosporin use in Europe (1997–2009). J Antimicrob Chemother. 2011;66:vi25–35.
Coenen S, Adriaenssens N, Versporten A, Muller A, Minalu G, Faes C, et al. European Surveillance of Antimicrobial Consumption (ESAC): outpatient use of tetracyclines, sulphonamides and trimethoprim, and other antibacterials in Europe (1997–2009). J Antimicrob Chemother. 2011;66:vi57–70.
Sacchetti E, Trifiro G, Caputi A, Turrina C, Spina E, Cricelli C, et al. Risk of stroke with typical and atypical anti-psychotics: a retrospective cohort study including unexposed subjects. J Psychopharmacol. 2008;22:39–46.
Mazzaglia G, Mantovani LG, Sturkenboom MC, Filippi A, Trifiro G, Cricelli C, et al. Patterns of persistence with antihypertensive medications in newly diagnosed hypertensive patients in Italy: a retrospective cohort study in primary care. J Hypertens. 2005;23:2093–100.
Bourke A, Dattani H, Robinson M. Feasibility study and methodology to create a quality-evaluated database of primary care data. Inform Prim Care. 2004;12:171–7.
Grant RL, Drennan VM, Rait G, Petersen I, Iliffe S. First diagnosis and management of incontinence in older people with and without dementia in primary care: a cohort study using the health improvement network primary care database. PLoS Med. 2013;10(8):e1001505.
Coloma PM, Schuemie MJ, Trifiro G, Gini R, Herings R, Hippisley-Cox J, et al. Combining electronic healthcare databases in Europe to allow for large-scale drug safety monitoring: the EU-ADR Project. Pharmacoepidemiol Drug Saf. 2011;20(1):1–11.
Trifiro G, Coloma PM, Rijnbeek PR, Romio S, Mosseveld B, Weibel D, et al. Combining multiple healthcare databases for postmarketing drug and vaccine safety surveillance: why and how? J Intern Med. 2014;275(6):551–61.
WHO Collaborating Centre for Drug Statistics Methodology. Anatomical Therapeutic Chemical (ATC) Classification System: Guidelines for ATC Classification and DDD Assignment 2011. http://www.whocc.no/filearchive/publications/2011guidelines.pdf. Accessed 14 Oct 2013.
Weist K, ESAC-Net participants and the Antimicrobial Resistance and Healthcare-associated Infections (ARHAI) programme at ECDC. ECDC publishes its first data on antimicrobial consumption in Europe. Euro Surveill. 2013;7:20419.
Vaccheri A, Bjerrum L, Resi D, Bergman U, Montanaro N. Antibiotic prescribing in general practice: striking differences between Italy (Ravenna) and Denmark (Funen). J Antimicrob Chemother. 2002;50:989–97.
Ternhag A, Hellman J. More on U.S. outpatient antibiotic prescribing, 2010. N Engl J Med. 2013;369:1175.
Huttner B, Harbarth S. Variations in outpatient antimicrobial use between and within countries: an ongoing mystery. Infection. 2010;38:1–2.
Veninga CC, Lundborg CS, Lagerlov P, Hummers-Pradier E, Denig P, Haaijer-Ruskamp FM. Treatment of uncomplicated urinary tract infections: exploring differences in adherence to guidelines between three European countries. Drug Education Project Group. Ann Pharmacother. 2000;34:19–26.
Cadieux G, Tamblyn R, Dauphinee D, Libman M. Predictors of inappropriate antibiotic prescribing among primary care physicians. CMAJ. 2007;177:877–83.
Wang KY, Seed P, Schofield P, Ibrahim S, Ashworth M. Which practices are high antibiotic prescribers? A cross-sectional analysis. Br J Gen Pract. 2009;59:e315–20.
Habib G, Hoen B, Tornos P, Thuny F, Prendergast B, Vilacosta I, et al. Guidelines on the prevention, diagnosis, and treatment of infective endocarditis (new version 2009): the Task Force on the Prevention, Diagnosis, and Treatment of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and the International Society of Chemotherapy (ISC) for Infection and Cancer. Eur Heart J. 2009;30(19):2369–413.
Hulscher ME, van der Meer JW, Grol RP. Antibiotic use: how to improve it? Int J Med Microbiol. 2010;300(6):351–6.
Zhang Y, Steinman MA, Kaplan CM. Geographic variation in outpatient antibiotic prescribing among older adults. Arch Intern Med. 2012;172(19):1465–71.
Harbarth S, Albrich W, Brun-Buisson C. Outpatient antibiotic use and prevalence of antibiotic-resistant pneumococci in France and Germany: a sociocultural perspective. Emerg Infect Dis. 2002;8(12):1460–7.
Butler CC, Hood K, Verheij T, Little P, Melbye H, Nuttall J, et al. Variation in antibiotic prescribing and its impact on recovery in patients with acute cough in primary care: prospective study in 13 countries. BMJ. 2009;338:b2242.
Boggon R, Hubbard R, Smeeth L, Gulliford M, Cassell J, Eaton S, et al. Variability of antibiotic prescribing in patients with chronic obstructive pulmonary disease exacerbations: a cohort study. BMC Pulm Med. 2013;13:32.
Molstad S, Erntell M, Hanberger H, Melander E, Norman C, Skoog G, et al. Sustained reduction of antibiotic use and low bacterial resistance: 10-year follow-up of the Swedish Strama programme. Lancet Infect Dis. 2008;8(2):125–32.
Monnet DL, Molstad S, Cars O. Defined daily doses of antimicrobials reflect antimicrobial prescriptions in ambulatory care. J Antimicrob Chemother. 2004;53(6):1109–11.
Safrany N, Monnet DL. Antibiotics obtained without a prescription in Europe. Lancet Infect Dis. 2012;12(3):182–3.
Napolitano F, Izzo MT, Di Giuseppe G, Angelillo IF. Public knowledge, attitudes, and experience regarding the use of antibiotics in Italy. PLoS One. 2013;8(12):e84177.
Acknowledgments
The current study is part of the EU-funded ARITMO study which aims to assess the utilisation and arrhythmogenic potential of antiinfectives, antihistamines and antipsychotics. ARITMO is a Research and Development project funded by the Health Area of the European Commission under the VII Framework Program (FP7/2007–2013) under Grant agreement no. 241679-the ARITMO project.
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
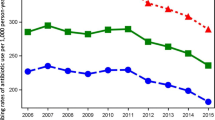
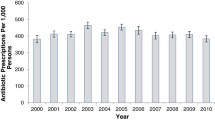
See Tables 4, 5, 6, 7 and Figs. 5, 6, 7.
Overall volume of antibiotics as DDDs per 1000 inhabitants per day by country and sex. DDDs defined daily doses, DID DDD per 1000 inhabitants per day, AUH Aarhus University Hospital, ERD Emilia-Romagnia regional database, GePaRD German Pharmacoepidemiological Research Database, THIN The Health improvement network
Rights and permissions
About this article
Cite this article
Mor, A., Frøslev, T., Thomsen, R.W. et al. Antibiotic use varies substantially among adults: a cross-national study from five European Countries in the ARITMO project. Infection 43, 453–472 (2015). https://doi.org/10.1007/s15010-015-0768-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-015-0768-8