Abstract
Purpose
The reduction in acquired infections (AI) due to methicillin-resistant Staphylococcus aureus (MRSA) with the mupirocin/chlorhexidine (M/C) decontamination regimen has not been well studied in intubated patients. We performed post hoc analysis of a prior trial to assess the impact of M/C on MRSA AI and colonization.
Methods
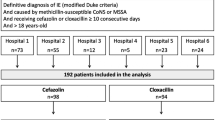
We conducted a multicenter, placebo-controlled, randomized, double-blind study with the primary aim to reduce all-cause AI. The two regimens used [topical polymyxin and tobramycin (P/T), nasal mupirocin with chlorhexidine body wash (M/C), or corresponding placebos for each regimen] were administered according to a 2 × 2 factorial design. Participants were intubated patients in the intensive care units of three French university hospitals. The patients enrolled in the study (n = 515) received either active P/T (n = 130), active M/C (n = 130), both active regimens (n = 129), or placebos only (n = 126) for the period of intubation and an additional 24 h. The incidence and incidence rates (per 1,000 study days) of MRSA AI were assessed. Due to the absence of a statistically significant interaction between the two regimens, analysis was performed at the margins by comparing all patient receiving M/C (n = 259) to all patients not receiving M/C (n = 256), and all patients receiving P/T (n = 259) to all patients not receiving P/T (n = 256).
Results
Incidence [odds ratio (OR) 0.39, 95 % confidence interval (CI) (0.16–0.96), P = 0.04] and incidence rates [incidence rate ratio (IRR) 0.41, 95 % CI 0.17–0.97, P = 0.05] of MRSA AI were significantly lower with the use of M/C. We also observed an increase in the incidence (OR 2.50, 95 % CI 1.01–6.15, P = 0.05) and the incidence rate (IRR 2.90, 95 % CI 1.20–8.03, P = 0.03) of MRSA AI with the use of P/T.
Conclusion
Among our study cohort of intubated patients, the use of M/C significantly reduced MRSA AI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Methicillin-resistant Staphylococcus aureus (MRSA) is considered to be the most prevalent nosocomial bacterium exhibiting multidrug-resistance [1]. MRSA accounted for 8.5 % of the pathogens responsible for healthcare-associated infections reported to the National Healthcare Safety Network during the period 2009–2010 [2]. In two studies, the routine screening of patients in intensive care units (ICUs) of large university hospitals revealed that 5–15 % of the patients had MRSA at admission [3] and up to 10 % had acquired MRSA during their stay in the ICU [4]. More recent estimates of MRSA incidence rates have varied from 2 to 14 per 1,000 patient-days, depending on whether infection or colonization is considered [5–7]. MRSA colonization increases considerably the risk of subsequent MRSA infection [8, 9]. The strategies to control MRSA infections in the ICU remain a controversial issue. Eradication of MRSA carriage with the use of nasal mupirocin and/or chlorhexidine body wash has been proposed and is widely recommended in some European countries. The mupirocin/chlorhexidine (M/C) regimen has been reported to reduce subsequent S. aureus infections in methicillin-susceptible S. aureus (MSSA) carriers [10], but a similar effect in MRSA carriers is uncertain. Recently, universal decolonization, but not MRSA carrier decolonization, has been shown to reduce the rate of MRSA clinical isolates [6].
Selective digestive decontamination (SDD), which primarily uses topical antibiotics (polymyxin and tobramycin), with or without systemic antibiotics, has been widely employed to prevent acquired infections (AI) in intubated patients in the ICU. SDD has been shown to reduce respiratory tract infections [11] and to improve survival [12, 13]. In a multicenter, placebo-controlled, randomized, double-blind study performed according to a 2 × 2 factorial design, we have shown that a double decontamination regimen using SDD plus a nasal mupirocin and chlorhexidine body wash substantially reduced all-cause ICU-AI in intubated patients, whereas each regimen administered alone was ineffective [14]. The objective of the present study was to examine whether the M/C regimen would be effective in preventing MRSA AI in intubated patients. For that purpose, we performed a post hoc analysis of the entire study population.
Patients and methods
Study design
The study was conducted at three multidisciplinary medical ICUs at three university-affiliated hospitals in France from April 1996 to June 1999. The protocol was approved by the regional committee on human investigation and has been reported elsewhere [14]. Patients aged >18 years who were intubated for <48 h and likely to require intubation and mechanical ventilation for >48 h were eligible for entry. Written consent had to be obtained from either the patient or their next of kin. The main exclusion criteria were a high probability of death, brain death, palliative treatments, neutropenia, ongoing trial, or prior decontamination therapy. Of the 4,444 patients who were recruited during the study period, 3,089 did not meet inclusion criteria (mostly due to lack of intubation or expected intubation for <2 days) and 655 had one or more defined exclusion criterion, leaving 516 eligible patients who were randomized among whom 515 were ultimately analyzed.
Decontamination regimens
The polymyxin/tobramycin regimen (P/T) did not use systemic antibiotics for the purpose of decontamination. Briefly, a solution containing polymyxin E (15 mg/ml) and tobramycin (10 mg/ml) or a gelatin solution (placebo) was administered to the nostrils (1 ml × 2), the oropharynx (3 ml), and the stomach (5 ml) every 6 h. The second regimen (M/C) was a nasal mupirocin 2 % ointment (Bactroban®; GlaxoSmithKline, Marly-le-Roi, France) and chlorhexidine 4 % soap (Hibiscrub®; Astra-Zeneca, Rueil-Malmaison, France) or petroleum jelly (placebo) and a non-antiseptic liquid soap mixed with the appropriate concentration of dye (cochineal red) and perfume (herbacol) to mimic the appearance of Hibiscrub® (placebo). Nurses’ aids washed each patient’s body twice daily with 15 ml of soap, followed by rinsing. Three times daily for 5 days, approximately 100 mg of nasal ointment was placed in both anterior nares. Following the initial course, additional 5-day courses of nasal ointment (up to two) were given to patients whose nasal swabs were positive for S. aureus (MSSA or MRSA) at follow-up. A nurse was independently in charge of the distribution of the nasal ointment treatment since the results of the colonization samples were not revealed to the clinicians during the study. Due to the 2 × 2 factorial design of the study, the 515 analyzed patients were allocated to one of the four following treatments: active P/T + placebo for M/C (P/T + 0, n = 130), placebo for P/T + active M/C (0 + M/C, n = 130), both active treatments (P/T + M/C, n = 129), or placebos only (0 + 0, n = 126) (Table 1). Active treatments or placebos were given during the intubation period plus an additional 24 h.
Report of S. aureus infection and colonization
All types of infections that were acquired between the randomization and the termination date of study treatments plus an additional 48 h, as defined by the Centers for Disease Control and Prevention [15], were recorded. Infections were characterized by site and a maximum of three microorganisms were identified. Only those infections involving S. aureus were considered for the purpose of the present study. S. aureus screening for colonization was performed by separately swabbing both nares and the groin area on admission into the ICU every week, then every 2 weeks from day 28 onwards, and then at the end of study or upon discharge from the ICU. Acquired MRSA or MSSA colonization was defined at the time of the first colonization sample (nose, groin) which was found positive for MRSA or MSSA among patients who were non-carriers at admission. Staphylococci were identified using standard methods (i.e., catalase, coagulase, and latex agglutination; Pastorex; Bio-Rad Laboratories, Marnes-la-Coquettte, France). The antibiotic susceptibility of S. aureus isolates was determined using the diffusion method only, with disks containing antibiotics (Bio-Rad) on Mueller–Hinton agar (Oxoid, Thermo Fisher Scientific, Waltham, MA). Susceptibility or resistance to methicillin was determined according to the recommendations of the French Society of Microbiology [16].
S. aureus colonization strains were tested for mupirocin resistance using 5-μg disks (Sanofi Diagnostics Pasteur, Marnes-La-Coquette, France) and E test assays (AB Nordisk, Solna, Sweden) [17]. Strains showing a zone diameter of ≥14 mm around 5-μg disks were considered to be mupirocin-susceptible, and those presenting diameters of ≤13 mm were considered to be mupirocin-resistant (either low-level or high-level resistance). High-level resistance was defined as a minimum inhibitory concentration of ≥512 μg/ml (E test). The mupirocin resistance rate was the proportion of all isolates tested that exhibited low- or high-level resistance.
Other prevention measures
Most ICU rooms were single. Standard precautions were applied, in accordance with the French recommendations for the surveillance and prevention of nosocomial infections (available at http://www.sante.gouv.fr/IMG/pdf/100_recommandations.pdf). Care bundles for the maintenance of arterial and central venous catheters, peripheral venous catheters, urinary catheters, the prevention of surgical site infection and the management of patients under mechanical ventilation were applied according to the institutional guidelines. Chlorhexidine was recommended for skin disinfection before the insertion of an intravascular device. Because the results of S. aureus screening were concealed, contact precautions for MRSA were taken based on the results of clinical cultures.
Endpoints
Rates of MRSA AI were the main endpoint of the present study. We calculated both the incidence (proportion of patients who acquired MRSA infection) and the incidence rate of MRSA AI expressed per 1,000 study days. As secondary endpoints, we examined MSSA and overall S. aureus AI and acquired colonization for MRSA and MSSA. The decolonization rate was calculated as the proportion of MRSA or MSSA carriers (either at admission to the ICU or during hospitalization in the ICU) in whom all subsequent screening tests (both nares and groin) were negative. This represents the analysis of data which had been collected prospectively at the time of the trial but not analyzed in the initial report [14].
Statistical analysis
Statistical analysis was performed using SAS statistical software ver. 9.3 (SAS Institute, Cary, NC). Differences in incidence were assessed using a logistic regression model and expressed with an odds ratio (OR) and 95 % confidence interval (CI). Incidence rates were tested using a Poisson regression model or a zero-inflated Poisson model, as appropriate, and expressed as an incidence rate ratio (IRR). A zero-inflated Poisson regression model was used when the data showed a higher incidence of zero counts than would be expected if the data were Poisson distributed [18]. We first used a complete regression model, which simultaneously tested the effect of each active regimen and their interaction. Because the interaction was not statistically significant (P value ≥0.30 for all comparisons), we finally performed analysis “at the margins”, rather than “inside the table”. The former analysis is appropriate to factorial trials when the two treatments are considered to act independently [19]. Based on a prior surveillance period, the sample size (125 patients per group) had been initially powered to detect a 50 % reduction of the number of AI per patient (α = 5 %; β = 10 %) under the assumption of no statistically significant interaction. In the final model, we compared the 259 patients who received active M/C treatment (all M/C) to the 256 patients who received the corresponding placebo (all no M/C). Comparisons between the patients who received active P/T treatment (all P/T, n = 259) and those who did not (all no P/T, n = 256) were also conducted, but these results did not represent the main objective of the study. A P value of ≤0.05 was considered to be statistically significant.
Results
Study patients
Among the 4,444 patients recruited during the study, 2,736 (61.6 %) were not included because they had an expected duration of intubation of <48 h and another 1,192 were not included due to the following reasons: age <18 years(1.0 %), intubation >48 h before admission (5.5 %), absence of consent or refusal (7.5 %), presence of one or more exclusion criteria (8.6 %), and/or clinical considerations or logistic problems (4.1 %). Baseline characteristics and primary diagnosis of the 515 analyzed patients were similar in the four groups (Table 1).
Effect of M/T treatment on MRSA-acquired infections
Compared to the corresponding placebo, the use of the M/C treatment regimen resulted in a statistically significant reduction in the incidence of MRSA infection [6.6 vs. 2.7 %, respectively; OR 0.39, 95 % CI 0.16–0.96, P = 0.04] (Table 2). The reduction was similar in the patients who received the P/T treatment regimen (comparison of P/T + M/C to P/T + 0: OR 0.40) and in those who did not receive P/T treatment (comparison of 0 + M/C to 0 + 0: OR 0.38). The incidence rates of MRSA AI were also reduced as well [2.0 ‰ vs. to 4.9 ‰; IRR 0.41, 95 % CI 0.17–0.97, P = 0.05]. The IRRs were also similar when P/T + M/C was compared to P/T + 0 (IRR 0.44) and when 0 + M/C was compared to 0 + 0 (IRR 0.39).
Effect of M/C treatment regimen on MSSA and overall S. aureus infections
With respect to MSSA AI, treatment with M/C alone did not result in a statistically significant reduction in the incidence (1.5 and 3.5 %; OR 0.43, 95 % CI 0.13–1.40; P = 0.16) or in the incidence rates (1.5 and 2.3 ‰; OR 0.65, 95 % CI 0.21–1.93, P = 0.76). With respect to overall S. aureus AI, treatment with M/C significantly reduced the incidence (all M/C vs. all no M/C: OR 0.41, 95 % CI 0.20–0.85, P = 0.02; P/T + M/C vs. P/T + 0: OR 0.48; 0 + M/C vs. 0 + 0: OR 0.33) and incidence rates [all M/C vs. all no M/C: IRR 0.49, 95 % CI 0.25–0.95, P = 0.05; P/T + M/C vs. P/T + 0: IRR 0.52; 0 + M/C vs. 0 + 0: OR 0.45] (Table 2).
Site of S. aureus-acquired infections
The sites of origin of the 45 S aureus AI are shown in Table 3. Twenty-nine AI were due to MRSA and 16 to MSSA. The most frequent site was pneumonia, which was ventilator-associated in all cases (MRSA n = 9; MSSA n = 9). There was a nonsignificant trend for a reduction in MRSA AI at any site with the use of M/C, except for catheter-related urinary tract infection. Due to the small number of infections, the decline in the rates of MSSA pneumonia with the use of M/C as compared to the corresponding placebos was not tested.
S. aureus colonization and impact of M/C regimen
Samples for colonization were not obtained for six of the 515 study patients. At the time of randomization, 121 patients (22.8 %) were found to be colonized with MSSA (nose n = 72; groin n = 22; nose and groin n = 27) and 54 (10.6 %) with MRSA (nose n = 20; groin n = 34; nose and groin n = 10). With the use of M/C, MRSA acquisition was nonsignificantly lower than the corresponding placebo (incidence: 7.9 vs. 12.9 %, respectively, P = 0.15; incidence rate: 5.8 vs. 9.0 ‰, respectively, P = 0.09) (Table 4). S. aureus colonization was not present prior to or at the time of diagnosis in 16 of the 45 S. aureus AIs (35.6 %; 5/16 MSSA AI; 11/29 MRSA AI). The decolonization rate for MRSA was significantly higher with the use of M/C (69.2 %) than without M/C (41.9 %; P = 0.04), but not with the use of P/T (60.0 %) versus no P/T (48.1 %; P = 0.36; P value for the interaction 0.89). The decolonization rate for MSSA was higher in the M/C (87 %, P = 0.004) and P/T + M/C (93.3 %, P = 0.003) groups than in the group not receiving either treatment regimen (48.1 %).
Impact of P/T treatment on S. aureus infection and colonization
Treatment with P/T compared with the placebo was associated with an increase in the incidence (6.6 vs. 2.7 %, respectively, OR 2.50, 95 % CI 1.01–6.15, P = 0.05) and the incidence rate [5.1 vs. 1.8 ‰, respectively, IRR 2.90, 95 % CI 1.20–8.03, P = 0.03) of MRSA AI. The reduction in MSSA AI was not statistically significant (incidence: OR 0.43, 95 % CI 0.13–1.40; incidence rate: IRR 0.31, 95 % CI 0.07–1.02). Overall S. aureus AI incidence (8.1 vs. 5.9 %, P = 0.33) and incidence rate (6.1 vs. 4.8 ‰, P = 0.61), MRSA- and MSSA-acquired colonization, and the MRSA decolonization rate (Table 4) were not significantly changed with the P/T treatment.
Mupirocin resistance
High-level mupirocin resistance was not detected. At randomization, 14 of the 509 screened patients (2.8 %) were colonized with low-level mupirocin-resistant S. aureus (P/T + M/C: 4/129; P/T + 0: 2/128; 0 + M/C: 4/129; 0 + 0: 4/123; P = 0.83). Following week 1, 15 of the 495 patients (3 %) who were initially non-carriers were diagnosed with low-level mupirocin-resistant S. aureus colonization (P/T + M/C: 1/125; P/T + 0: 2/126; 0 + M/C: 8/125; 0 + 0: 4/119; P = 0.06). Of a total of 2,230 screening samples that were collected at both sites on admission and during follow-up, 203 and 218 tested culture positive for MRSA and MSSA, respectively. The mupirocin resistance rate was 20.2 % for MRSA and 1.8 % for MSSA colonization isolates (P < 0.001), and there were 0/18 MRSA clinical isolates. Among the 29 patients colonized with mupirocin-resistant S. aureus, 27 did not acquire a S. aureus infection. Two patients colonized with mupirocin-resistant MSSA had MSSA AI (mupirocin sensitivity not tested on clinical isolates).
Adverse events
Treatment with the nasal ointment was discontinued due to discomfort in three patients who received the active mupirocin and in five who received the placebo. Skin allergy was reported in six patients receiving M/C and in six patients receiving the corresponding placebos. Body washing was discontinued due to allergy in five patients who received the active chlorhexidine, in three who received the liquid soap, and for other reasons in eight patients (P/T + M/C: 1; P/T + 0: 2; 0 + M/C: 3; 0 + 0: 3).
Discussion
The main result of this study was that the use of nasal mupirocin combined with chlorhexidine body wash in patients requiring intubation for >48 h was able to reduce MRSA ICU-acquired infections. Because this is a post hoc analysis of a previously published trial, the sample size was not calculated to specifically assess MRSA AI. This represents a limitation of the study which could result in inadequate power to detect a statistically significant interaction and thereby reduce the scope of the comparisons. Because the estimates of the risk for MRSA AI with the use of M/C were very similar in the “at the margins” analysis and in the two pairwise comparisons between groups, interaction was unlikely. This strengthens our conclusion on the reduction of MRSA AI with the use of M/C.
Although a decline in MRSA incidence rates [20] and in MRSA acquisition [21] has been reported in some European countries, great variations persist between countries and between types of hospital care, and MRSA is still considered a public health priority [22]. The methicillin resistance rate (proportion of MRSA among all S. aureus isolates) is >25 % in more than one-fourth of countries (available at http://www.ecdc.europa.eu/en/eaad/documents/eaad-2011-summary-antimicrobial-resistance-data.pdf) in the EU. This indicator is commonly used for the surveillance of MRSA because it correlates with MRSA incidence rates [23]. In France in 2010, the MRSA incidence rate in the ICU was approximately threefold higher (1.14 per 1,000 patient-days) than the overall incidence rate (0.40) [24]. S. aureus was involved in 12.2 % of AI (total AI incidence 13.2 %) and the methicillin resistance rate was 35.0 % (vs 48.7 % in 2004) (available at http://www.cclinparisnord.org/REACAT/REA2010/Rapport_REA2010.pdf). In the STAR*ICU trial, 6.2–24.3 % of patients, depending on centers, had surveillance cultures positive for MRSA within 2 days of ICU admission, On average, the incidence of MRSA colonization/infection was 13.9 per 1,000 patient-days at risk (range 3.8–49.0), highlighting a high variability between periods and ICUs in the USA (Supplementary Appendix [7]). Moreover, intubated patients have an approximately eightfold higher risk for MRSA acquisition [25] or infection [26] than those who are not intubated in the ICU.
In our study, there were high rates of MRSA colonization at admission and during the ICU stay as opposed to relatively low infection rates. Because the majority of S. aureus infections were associated with colonization, effective decolonization of MRSA-colonized patients was a likely explanation to the reduction in MRSA AI. The absence of molecular typing of MRSA isolates is a limitation of the study, and we could not be sure that colonization and clinical isolates were identical in all cases of infection. We previously reported that the clonal nature of epidemic MRSA stains recovered during a 9-year period at our institution could not be easily distinguished by pulsed-field gel electrophoresis [27, 28].
Decontamination with various topical agents has been attempted to prevent MRSA AI. The aim is to reduce both cross-transmission and the risk of subsequent infection among MRSA carriers. Nasal mupirocin decontamination alone may not be effective because of the persistence of MRSA carriage at other anatomic sites [29]. Skin decontamination with chlorhexidine body washing has been reported to significantly reduce MRSA acquisition, but not infection, in ICUs [30]. Ridenour et al. [31] reported a reduction in the incidence of acquired MRSA colonization and infection with the combined use of intranasal mupirocin with chlorhexidine body wash. Unlike the typical MRSA decolonization strategies targeting only MRSA carriers, in our study all patients immediately received nasal ointment (active mupirocin or placebo), and the results of S. aureus colonization samples were concealed to the clinicians. The absence of delay for decolonization of MRSA carriers could reduce the risk of cross-transmission. Moreover, whole-body washing with chlorhexidine may also notably reduce MRSA loads at extra-nasal sites, especially at the groin area [32]. Furthermore, we washed our intubated patients twice daily, which was twice more frequent than that usually reported for decolonization [5, 6]. Taken altogether, these factors could explain the level of prophylaxis achieved.
Although the study was performed more than one decade ago, due to the double-blind, placebo-controlled design, we believe the conclusion is still relevant to current practice in ICUs where MRSA prevalence rate remains substantial. The administration of M/C to patients intubated for an expected duration of >48 h targeted the patients at highest risk for MRSA AI. These patients represented 38 % of the 4,444 patients admitted to the three ICUs during the study period. This protocol could be more selective than universal decolonization applied to all ICU patients, which has been shown to significantly reduce the rates of MRSA clinical isolates, as well as reduce MRSA bloodstream infections, but not significantly [6]. Moreover, the combination of M/C with the P/T regimen achieved a substantial reduction in all-cause infections [14].
Our study also showed that the use of P/T was associated with a statistically significant increase in MRSA infection rates. Earlier studies reported an increase in MRSA isolates with the use of SDD [33–35], although the exact rates of MRSA AI were not calculated, and statistical significance not assessed. Due to the introduction of community-acquired MRSA (mostly susceptible to tobramycin) in the hospital setting and changing epidemiology in hospital-acquired MRSA, the impact of P/T on MRSA infection rates deserves re-assessment. MRSA-acquired colonization remained essentially unchanged with the use of P/T.
The M/C regimen was effective in decolonizing MSSA. No definite conclusion on MSSA AI could be drawn due to insufficient number of infections.
The mupirocin-resistant S. aureus prevalence rate on admission was considered to be moderate, similar to the acquisition rate in ICU. With the routine or widespread use of nasal mupirocin to control endemic S. aureus infection and transmission rates among general inpatient populations, the emergence of mupirocin resistance has been commonly observed, [36, 37], although it is not a universal trend [38, 39]. Resistance rates have varied from 7 to 65 % [40, 41]. The clinical significance of low-level resistance remains unclear, and the combined use of chlorhexidine with mupirocin might have limited the emergence of mupirocin resistance in our study. Genotypic chlorhexidine resistance, which may explain the failure of decolonization with M/C treatment in low-level mupirocin-resistant MRSA strains [42] was not tested.
In conclusion, the combined use of nasal mupirocin and chlorhexidine body wash significantly reduced the rates of MRSA AI in intubated patients. Surveillance of mupirocin resistance is mandatory with the use of mupirocin.
References
Grundmann H, Aires-de-Sousa M, Boyce J, Tiemersma E. Emergence and resurgence of meticillin-resistant Staphylococcus aureus as a public-health threat. Lancet. 2006;368:874–85.
Sievert DM, Ricks P, Edwards JR, Schneider A, Patel J, Srinivasan A, et al. Antimicrobial-resistant pathogens associated with healthcare-associated infections: summary of data reported to the national healthcare safety network at the centers for disease control and prevention, 2009–2010. Infect Control Hosp Epidemiol. 2013;34:1–14.
Lucet JC, Regnier B. Screening and decolonization: does methicillin-susceptible Staphylococcus aureus hold lessons for methicillin-resistant S. aureus? Clin Infect Dis. 2010;51:585–90.
Warren DK, Guth RM, Coopersmith CM, Merz LR, Zack JE, Fraser VJ. Epidemiology of methicillin-resistant Staphylococcus aureus colonization in a surgical intensive care unit. Infect Control Hosp Epidemiol. 2006;27:1032–40.
Climo MW, Yokoe DS, Warren DK, Perl TM, Bolon M, Herwaldt LA, et al. Effect of daily chlorhexidine bathing on hospital-acquired infection. N Engl J Med. 2013;368:533–42.
Huang SS, Septimus E, Kleinman K, Moody J, Hickok J, Avery TR, et al. Targeted versus universal decolonization to prevent ICU infection. N Engl J Med. 2013;68:2255–65.
Huskins WC, Huckabee CM, O’Grady NP, Murray P, Kopetskie H, Zimmer L, et al. Intervention to reduce transmission of resistant bacteria in intensive care. N Engl J Med. 2011;364:1407–18.
Davis KA, Stewart JJ, Crouch HK, Florez CE, Hospenthal DR. Methicillin-resistant Staphylococcus aureus (MRSA) nares colonization at hospital admission and its effect on subsequent MRSA infection. Clin Infect Dis. 2004;39:776–82.
Safdar N, Bradley EA. The risk of infection after nasal colonization with Staphylococcus aureus. Am J Med. 2008;121:310–5.
Bode LG, Kluytmans JA, Wertheim HF, Bogaers D, Vandenbroucke-Grauls CM, Roosendaal R, et al. Preventing surgical-site infections in nasal carriers of Staphylococcus aureus. N Engl J Med. 2010;362:9–17.
Liberati A, D’Amico R, Pifferi S, Torri V, Brazzi L, Parmelli E. Antibiotic prophylaxis to reduce respiratory tract infections and mortality in adults receiving intensive care. Cochrane Database Syst Rev. 2009; (4):CD000022. doi: 10.1002/14651858.CD000022.pub
de Jonge E, Schultz MJ, Spanjaard L, Bossuyt PM, Vroom MB, Dankert J, et al. Effects of selective decontamination of digestive tract on mortality and acquisition of resistant bacteria in intensive care: a randomised controlled trial. Lancet. 2003;362:1011–6.
de Smet AM, Kluytmans JA, Cooper BS, Mascini EM, Benus RF, van der Werf TS, et al. Decontamination of the digestive tract and oropharynx in ICU patients. N Engl J Med. 2009;360:20–31.
Camus C, Bellissant E, Sebille V, Perrotin D, Garo B, Legras A, et al. Prevention of acquired infections in intubated patients with the combination of two decontamination regimens. Crit Care Med. 2005;33:307–14.
Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM. CDC definitions for nosocomial infections, 1988. Am J Infect Control. 1988;16:128–40.
Courvalin P. Interpretive reading of in vitro antibiotic susceptibility tests (the antibiogramme). Clin Microbiol Infect. 1996;2:S26–34.
Finlay JE, Miller LA, Poupard JA. Interpretive criteria for testing susceptibility of staphylococci to mupirocin. Antimicrob Agents Chemother. 1997;41:1137–9.
Hall DB. Zero-inflated Poisson and binomial regression with random effects: a case study. Biometrics. 2000;56:1030–9.
McAlister FA, Straus SE, Sackett DL, Altman DG. Analysis and reporting of factorial trials: a systematic review. JAMA. 2003;289:2545–53.
Jarlier V, Trystram D, Brun-Buisson C, Fournier S, Carbonne A, Marty L, et al. Curbing methicillin-resistant Staphylococcus aureus in 38 French hospitals through a 15-year institutional control program. Arch Intern Med. 2010;170:552–9.
Edgeworth JD. Has decolonization played a central role in the decline in UK methicillin-resistant Staphylococcus aureus transmission? A focus on evidence from intensive care. J Antimicrob Chemother. 2011;66:ii41–7.
Johnson AP. Methicillin-resistant Staphylococcus aureus: the European landscape. J Antimicrob Chemother. 2011;66:iv43–8.
Lepelletier D, Richet H. Surveillance and control of methicillin-resistant Staphylococcus aureus infections in French hospitals. Infect Control Hosp Epidemiol. 2001;22:677–82.
Carbonne A, Arnaud I, Maugat S, Marty N, Dumartin C, Bertrand X, et al. National multidrug-resistant bacteria (MDRB) surveillance in France through the RAISIN network: a 9 years experience. J Antimicrob Chemother. 2013;68:954–9.
Matsushima A, Tasaki O, Tomono K, Ogura H, Kuwagata Y, Sugimoto H, et al. Pre-emptive contact precautions for intubated patients reduced healthcare-associated meticillin-resistant Staphylococcus aureus transmission and infection in an intensive care unit. J Hosp Infect. 2011;78:97–101.
Yamakawa K, Tasaki O, Fukuyama M, Kitayama J, Matsuda H, Nakamori Y, et al. Assessment of risk factors related to healthcare-associated methicillin-resistant Staphylococcus aureus infection at patient admission to an intensive care unit in Japan. BMC Infect Dis. 2011;11:303.
Donnio PY, Louvet L, Preney L, Nicolas D, Avril JL, Desbordes L. Nine-year surveillance of methicillin-resistant Staphylococcus aureus in a hospital suggests instability of mecA DNA region in an epidemic strain. J Clin Microbiol. 2002;40:1048–52.
Donnio PY, Preney L, Gautier-Lerestif AL, Avril JL, Lafforgue N. Changes in staphylococcal cassette chromosome type and antibiotic resistance profile in methicillin-resistant Staphylococcus aureus isolates from a French hospital over an 11 years period. J Antimicrob Chemother. 2004;53:808–13.
Harbarth S, Dharan S, Liassine N, Herrault P, Auckenthaler R, Pittet D. Randomized, placebo-controlled, double-blind trial to evaluate the efficacy of mupirocin for eradicating carriage of methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother. 1999;43:1412–6.
Climo MW, Sepkowitz KA, Zuccotti G, Fraser VJ, Warren DK, Perl TM, et al. The effect of daily bathing with chlorhexidine on the acquisition of methicillin-resistant Staphylococcus aureus, vancomycin-resistant Enterococcus, and healthcare-associated bloodstream infections: results of a quasi-experimental multicenter trial. Crit Care Med. 2009;37:1858–65.
Ridenour G, Lampen R, Federspiel J, Kritchevsky S, Wong E, Climo M. Selective use of intranasal mupirocin and chlorhexidine bathing and the incidence of methicillin-resistant Staphylococcus aureus colonization and infection among intensive care unit patients. Infect Control Hosp Epidemiol. 2007;28:1155–61.
Wendt C, Schinke S, Wurttemberger M, Oberdorfer K, Bock-Hensley O, von Baum H. Value of whole-body washing with chlorhexidine for the eradication of methicillin-resistant Staphylococcus aureus: a randomized, placebo-controlled, double-blind clinical trial. Infect Control Hosp Epidemiol. 2007;28:1036–43.
Kaufhold A, Behrendt W, Krauss T, van Saene H. Selective decontamination of the digestive tract and methicillin-resistant Staphylococcus aureus. Lancet. 1992;339:1411–2.
Nau R, Ruchel R, Mergerian H, Wegener U, Winkelmann T, Prange HW. Emergence of antibiotic-resistant bacteria during selective decontamination of the digestive tract. J Antimicrob Chemother. 1990;25:881–3.
Saunders GL, Hammond JM, Potgieter PD, Plumb HA, Forder AA. Microbiological surveillance during selective decontamination of the digestive tract (SDD). J Antimicrob Chemother. 1994;34:529–44.
Vasquez JE, Walker ES, Franzus BW, Overbay BK, Reagan DR, Sarubbi FA. The epidemiology of mupirocin resistance among methicillin-resistant Staphylococcus aureus at a Veterans’ Affairs hospital. Infect Control Hosp Epidemiol. 2000;21:459–64.
Perez-Roth E, Lopez-Aguilar C, Alcoba-Florez J, Mendez-Alvarez S. High-level mupirocin resistance within methicillin-resistant Staphylococcus aureus pandemic lineages. Antimicrob Agents Chemother. 2006;50:3207–11.
Raz R, Miron D, Colodner R, Staler Z, Samara Z, Keness Y. A 1-year trial of nasal mupirocin in the prevention of recurrent staphylococcal nasal colonization and skin infection. Arch Intern Med. 1996;156:1109–12.
Hudson IR. The efficacy of intranasal mupirocin in the prevention of staphylococcal infections: a review of recent experience. J Hosp Infect. 1994;27:81–98.
Fawley WN, Parnell P, Hall J, Wilcox MH. Surveillance for mupirocin resistance following introduction of routine peri-operative prophylaxis with nasal mupirocin. J Hosp Infect. 2006;62:327–32.
Vivoni AM, Santos KR, de-Oliveira MP, Giambiagi-deMarval M, Ferreira AL, Riley LW, et al. Mupirocin for controlling methicillin-resistant Staphylococcus aureus: lessons from a decade of use at a university hospital. Infect Control Hosp Epidemiol. 2005;26:662–7.
Lee AS, Macedo-Vinas M, Francois P, Renzi G, Schrenzel J, Vernaz N, et al. Impact of combined low-level mupirocin and genotypic chlorhexidine resistance on persistent methicillin-resistant Staphylococcus aureus carriage after decolonization therapy: a case-control study. Clin Infect Dis. 2011;52:1422–30.
Acknowledgments
This study was conducted with financial support from the French Ministry of Health (Clinical Research Hospital Program, PHRC 94, Direction des Hôpitaux, Paris, France) and from a grant from GlaxoSmithKline. The grant covered the additional costs of processing and culture of colonization samples and susceptibility testing of S. aureus isolates to mupirocin. GlaxoSmithKline had no role in the design, analysis or drafting of the manuscript.
Conflict of interest
All authors report no conflicts of interest relevant to this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Camus, C., Sebille, V., Legras, A. et al. Mupirocin/chlorexidine to prevent methicillin-resistant Staphylococcus aureus infections: post hoc analysis of a placebo-controlled, randomized trial using mupirocin/chlorhexidine and polymyxin/tobramycin for the prevention of acquired infections in intubated patients. Infection 42, 493–502 (2014). https://doi.org/10.1007/s15010-013-0581-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-013-0581-1