Abstract
Purpose
To assess the therapeutic effect and toxicity of intravenous colistin in the treatment of multidrug-resistant (MDR) Gram-negative bacteria in patients with severe burns.
Methods
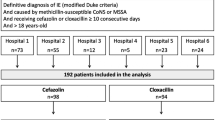
The medical records of 930 patients admitted to the Burn Intensive Care Unit (ICU) at Hallym University Hangang Sacred Heart Hospital, Seoul, South Korea between April 2007 and December 2009 were retrospectively reviewed. Of these, the 104 patients who had received intravenous colistin treatments (104 courses) during this period were enrolled in the study. Changes in creatinine level were analyzed in three groups: all patients receiving colistin (n = 104), patients with undergoing continuous renal replacement therapy (CRRT group; n = 38), and patients not undergoing CRRT (non-CRRT group; n = 66).
Results
Among these patients, the burnt body surface area ranged from 5 to 96% (mean 49.7%). Thirty-five patients (33.7%) suffered inhalation injury, and CRRT was administered to 38 patients. The mean duration of colistin treatment was 14.7 (range 4–71) days. The total dose of colistin was 3,045.7 mg (range 100–13,800). The length of ICU stay was 48.9 (range 7–154) days. Forty patients (38.5%) died. The mean pre-colistin creatinine level of all patients was 1.04 mg/dL, and the mean post-colistin level was 1.34 mg/dL. The mean pre-colistin creatinine level of the CRRT group and non-CRRT group was 1.68 and 0.66 mg/dL, and the mean post-colistin level was 1.68 and 1.14 mg/dL, respectively.
Conclusions
Colistin appears to be a relatively safe and effective treatment for major burn patients with infections caused by MDR Gram-negative bacteria when no other drug is available. Additionally, we found no statistically significant impairment of creatinine levels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introductions
Among hospitalized patients, those with severe burns are especially exposed to infection due to immune compromise and loss of the skin barrier. Despite advances in burn treatments, complications due to infection have a significant effect on mortality and morbidity. In recent years, the emergence of resistant pathogens has forced burn treatment providers to search for alternative treatments [1]. Nevertheless, multidrug-resistant (MDR) Gram-negative organisms, including Pseudomonas aeruginosa and Acinetobacter baumannii, remain the major microbial agents contributing to the increase in morbidity and mortality. Outbreaks of P. aeruginosa resistant to most available β-lactams, aminoglycosides, and fluoroquinolones have been reported in burn units [2]. Additionally, A. baumannii strains susceptible only to polymyxins have become a common problem, especially in intensive care units (ICUs) [3]. Thus, colistin has re-emerged as a highly effective treatment against MDR Pseudomonas and Acinetobacter infections.
There are five types of polymyxins (A–E), but only polymyxin B and E have been used in humans [4]. Colistin, also known as polymyxin E, is a relatively old antibiotic with significant in vitro activity against a number of MDR Gram-negative pathogens, including P. aeruginosa, A. baumannii, and Klebsiella pneumonia. It is one of the polymyxin antibiotics produced by Bacillus colistinus [5]. Polymyxins were discovered in 1947 [5] and have been available since 1959 for the treatment of infections caused by Gram-negative bacteria [6]. However, early clinical reports suggested a high incidence of toxicity, and their use was reduced when the potentially less toxic aminoglycosides and other anti-pseudomonal agents became available [7, 8]. Thus, the emergence of Gram-negative bacteria resistant to most available antibiotics has revived interest in the therapeutic use of colistin for treating infections in critically ill patients.
Nephrotoxicity is a commonly observed adverse effect following intravenous (IV) administration of sodium colistin methanesulfonate [9]. However, few reports are available on nephrotoxicity following colistin therapy in major burn patients. Nephrotoxicity usually occurs within the first 4 days of therapy, with signs continuing for 1–2 weeks after cessation of the therapy. However, renal function usually returns to normal within 3–9 weeks [9]. Severe burns also lead to a hypermetabolic response that is far in excess of anything seen in any other disease state, with different antibiotic pharmacokinetics and pharmacodynamics compared with those in patients in other critical conditions. Consequently, optimal colistin dosing strategies for major burn patients, including total daily dose, mode of administration, and dosing intervals, are also different. The aim of this study was to evaluate the use of colistin in our burn center for the treatment of MDR Gram-negative organisms and to evaluate the nephrotoxicity of this drug in major burn patients.
Methods
Patient identification
The medical records of 930 patients who were admitted to the Burn ICU at Hallym University Hangang Sacred Heart Hospital, Seoul, South Korea between April 2007 and December 2009 were retrospectively reviewed. Among these patients, 104 courses of IV colistin treatments had been administered to 104 patients during the study period; these 104 patients were enrolled in the study. Our burn center, with seven general surgeons and five plastic surgeons, is the largest burn unit and only tertiary burn center in South Korea. It offers 21 ICU beds dedicated to the primary care of burn victims, and there are more than 2,000 registered admissions per year. There are eight isolation rooms and ten silicone beds (air-floating beds) in the Burn ICU. This study was approved by the ethics committee of the Hangang Sacred Heart Hospital and informed consent was obtained from the lineal relatives. Patients were excluded if they received ≤2 days of colistin therapy because ≤2 days of colistin administration is not considered therapeutic failure [10]. Continuous renal replacement therapy (CRRT) was administered to 38 patients who met at least two of following criteria: non-obstructive oliguria; severe academia; azotemia; hyperkalemia; suspected uremic organ involvement; progressive severe dysnatremia; hyperthermia; clinically significant organ edema [11].
Route of colistin administration and dosage
Colistin (colistin sulfomethate sodium) was administered IV at a dosage of 2.5–5.0 mg/kg/day, and the daily dose was adjusted when patients presented with renal failure (baseline creatinine level ≥1.2 mg/dL).
Diagnosis
A survey program was routinely implemented. A blood culture was performed if the patient’s core temperature was >38.5°C, and burn wounds, the urinary tract, and sputum were cultured two times per week for bacterial and fungal identification. Urinary and central venous catheters were changed every 5 days and cultured. Blood cultures were ordered at the discretion of the primary physician when signs and symptoms of possible bloodstream infection were present. MDR Gram-negative organisms were defined as isolates resistant to at least three drugs in the following classes: β-lactams, carbapenems, aminoglycosides, and fluoroquinolones. Due to domestic legal regulations, nebulized colistin could not be used. Patients with MDR Gram-negative organisms were given IV colistin sulfomethate sodium only. Response to colistin was based on the presence of two of the following four criteria: an improvement in clinical symptoms; a change in the properties of secretions; a reduction in the need for organ support; a reduction in temperature; a decrease in white blood cell and inflammatory markers; negative culture. The presence of pandrug-resistant Gram-negative bacteria was also assessed.
Renal function was monitored by serial measurements of the serum creatinine level. Serum creatinine levels were measured at the initiation of therapy and at weekly intervals thereafter until the colistin treatment was completed. In patients with normal renal function (serum creatinine level <1.2 mg/dL), renal failure was defined as a serum creatinine value of >2.0 mg/dL. In patients with preexisting renal dysfunction, renal failure was defined as an increase of ≥50% of the baseline creatinine or as a decline in renal function that resulted in the need for renal replacement therapy.
Treatment
All patients received proper fluid and electrolyte resuscitation, pain management, nutritional support, wound care, and surgical debridement of dead tissue by a burn surgeon. The wound dressings of all ICU patients were changed every day. The dressing methods varied in accordance with the wound condition and were applied by specialized burn therapists. Fluid resuscitation was based on the Parkland or Warden formula. Antibiotics were used only to treat systemic infections, according to the wound, urine, sputum, and blood cultures.
Statistical analysis
All data were analyzed using SPSS ver. 17.0 software (SPSS, Chicago, IL) and presented as frequency and percentage for categorical variables and as mean and range for continuous variables. Continuous variables were analyzed with the Student’s t test or one-way analysis of variance (ANOVA) test when appropriate. Categorical variables were analyzed with Pearson’s chi-square test or with the chi-square test with Yate’s correction.
Results
During the study period, 930 patients were cared for in our Burn ICU. Of these, the 104 patients (11.1%) who had received colistin treatment were enrolled in the study. The mean age of these 104 patients was 48.4 (range 12–88) years and 78 (75%) were male. The burnt body surface area varied between 5 and 96% (mean 49.7%), with full-thickness burns present in 36.0% of patients (range 0–96%). Thirty-five patients (33.7%) had suffered inhalation injury, and the mean length of ICU stay was 48.9 (range 7–154) days. The patients received an average dose of 3,045.7 mg colistin, and the mean duration of colistin treatment was 14.7 (range 4–71) days. Forty patients (38.5%) died (Table 1).
Among these 104 patients, 38 patients were given CRRT. The mean age of the CRRT group was 52.7 (range 24–88) years. Among these patients, the burnt body surface area varied between 5 and 93% (mean 50.3%), and full-thickness burns were present in 38.5% of then (range 0–90%). Ten patients (26.3%) had suffered inhalation injury, and the mean length of ICU stay was 43.2 (range 10–154) days. The patients received an average dose of 2,817.3 mg colistin, and the mean duration of colistin treatment was 15.6 (range 4–71) days. Twenty-six patients (64.8%) died (Table 1).
The non-CRRT group comprised 66 patients. The mean age of patients in this group was 45.9 (range 12–88) years. The burnt body surface area varied between 6 and 96% (mean 49.4%), and full-thickness burns were present in 34.6% of them (range 0–96%). Twenty-five patients (37.9%) had suffered inhalation injury, and the mean length of ICU stay was 52.2 (range 7–133) days. The patients received an average dose of 3,177.2 mg colistin, and the mean duration of colistin treatment was 14.2 (range 4–35) days. Fourteen patients (21.2%) died (Table 1).
The patients received a minimum and maximum of 100 and 13,800 mg of colistin, respectively, during their respective treatment (Table 2). All patients had previously received antibiotics other than colistin because of other infections, and all had previously received antibiotics concomitant with colistin because of copathogens. The most common combination was colistin, teicoplanin, and meropenem (Table 3). Forty-three patients underwent simultaneous antifungal treatment. Most of the samples collected from these patients cultured positive for Pseudomonas and Acinetobacter. We performed culture at the wound, sputum, urine, whole blood, bronchial washing, and catheters. In the case of Pseudomonas, five cases presented multi-antibiotic resistance, including to colistin, at the wound, and there were 16 cases of multi-antibiotic resistance at the sputum (Fig. 1). Multi-antibiotic resistant Acinetobacter, also to colistin, was also found at the wound, sputum, and urine (one case at each site) (Fig. 2).
The serum creatinine levels were measured at admission (admission), prior to initiating colistin therapy (pre-colistin), and after cessation of colistin administration (post-colistin). Three groups of patients were analyzed: all those receiving colistin (entire patient cohort), patients receiving colistin but not CRRT (CRRT group), and patients receiving both colistin and CRRT (CRRT group). Among the entire patient cohort, the mean admission creatinine level, pre-colistin creatinine level, and post-colistin level was 1.33, 1.04, and 1.34 mg/dL, respectively (P = 0.320); among the CRRT group, these mean values were 2.07, 1.68, and 1.68 mg/dL (P = 0.739), respectively; among the non-CRRT group, these mean values were 0.91, 0.66, and 1.14 mg/dL, respectively (P = 0.000). All estimates were made using one-way ANOVA (Fig. 3). In the CRRT group, although serum creatinine levels increased significantly, the elevated level of serum creatinine following colistin administration was within the normal range.
Discussion
Patients who suffer severe burns are at a higher risk for local and systemic infections. “Innovations in fluid management, ventilator support, surgical care, and antimicrobial therapy have contributed to a significant reduction in morbidity and mortality rates in burn patients” [1]. Nevertheless, serious life-threatening infections remain a leading cause of death in seriously ill burn patients.
The emergence of MDR Gram-negative organisms causing nosocomial infections is a growing problem for clinicians. Indiscriminate use of empiric antibiotic therapy can lead to the development of MDR bacteria [12], an example of which is the growth of MDR P. aeruginosa and A. baumannii in patients receiving prolonged antibiotic therapy [13]. These species are noted for their intrinsic resistance to antibiotics and for their ability to acquire genes encoding further resistance determinants. Foremost among the mechanisms of resistance in both of these pathogens is the production of β-lactamases and aminoglycoside-modifying enzymes. The diminished expression of outer membrane proteins, mutations in topoisomerases, and upregulation of efflux pumps also play an important part in antibiotic resistance. Unfortunately, the accumulation of multiple mechanisms of resistance leads to the development of MDR or even panresistant strains [14]. Although acquired resistance is rare, among our 104 patients, we observed panresistant strains in 21 cases of P. aeruginosa infection and three cases of A. baumannii infection. Trottier et al. [15] reported that the majority of A. baumannii isolates were MDR, and a significant proportion was sensitive only to colistin.
The current expansion of MDR bacteria, including A. baumannii and P. aeruginosa, has led to renewed interest in older antibiotics, such as the polymyxins [16], because the decreased use of these agents during recent years has preserved their activity against MDR pathogens [17]. Montero et al. [18] reported colistin to be a safe agent for treating MDR P. aeruginosa, which is the most common pathogen found in burn patients. Improvements in pharmaceutical formulations and new dosage strategies have considerably reduced the toxicity previously attributed to these drugs, thereby enabling their reintroduction into clinical situations [19]. Even so, most of the available information about the pharmacokinetics, safety, and clinical value of polymyxins is derived from studies performed during the 1970s; consequently, it is difficult to apply this information to the formulations and dosage regimens currently used [17, 19]. Additionally, a considerable proportion of pharmacokinetic and pharmacodynamic studies were performed in patients with cystic fibrosis, and few studies of colistin use in adult major burn patients have been reported.
Two forms of colistin have been commercialized: colistin sulfate and colistimethate sodium (also known as colistin methanesulfonate sodium, colistin sulfomethate sodium, pentasodium colistimethanesulfate, or methanesulfate) [20]. Colistin sulfate has greater antimicrobial activity, but is also more toxic and, therefore, restricted to topical use. Colistimethate presents better tolerability and is administered parenterally or by nebulization. Colistimethate is actually a nonactive prodrug of colistin, but in aqueous solutions (such as human plasma), it is hydrolyzed to colistin, which has antimicrobial activity [19]. The target of the antimicrobial activity of colistin is the bacterial cell membrane. Its cationic (polypeptide) portion binds to the anionic portion of the lipopolysaccharide (LPS), a major component in the Gram-negative bacterial membrane. Colistin displaces magnesium and calcium, which normally stabilize the LPS molecule, from the negatively charged LPS, leading to a local disturbance of the outer membrane. This union generates a major disruption in the bacterial membrane, increasing its permeability and ultimately leading to cellular lysis [21].
Toxicity, particularly nephrotoxicity, is an important concern with colistin. In the 1980s, colistin was abandoned because of renal and neurological toxicity. Renal toxicity primarily includes acute tubular necrosis, which is characterized by decreased creatinine clearance and increased serum urea and creatinine levels. In the study conducted by Koch-Weser et al. [8], impairment in renal function, usually reversible with the termination of treatment, was observed in 20.2% of 288 patients. Levin et al. [22] also reported a high incidence of nephrotoxicity (37%), especially in patients who already had compromised renal function. Doses for patients with renal insufficiency must be adjusted because colistin is primarily excreted by the kidneys, and elevated blood levels of the drug may further impair renal function. However, renal function impairment should not be attributed solely to colistin toxicity because other factors, such as the development of septic shock and multiorgan failure, may also make a significant contribution [23].
In a study of 14 pediatric patients, Goverman et al. [24] reported a significant increase in urea and creatinine levels in two patients (14.3%), but none of the children required renal replacement therapy and none developed neurological complications. Additionally, in a study by Rosanova et al. involving 45 children [24], none of the children developed increases in serum creatinine concentrations or neurological complications during treatment with colistin. However, in adult patients, the reported nephrotoxicity rates are variable, ranging from 0 to 37% [25]. Most studies have involved critically ill patients. However, reported experience with the use of colistin in adult burn patients is scarce.
The main finding of our study is that there was no significant deterioration of renal function in our patients with normal baseline serum creatinine levels during administration of intravenous colistin. However, a few patients undergoing colistin treatment showed increased serum creatinine levels, and care with the use of colistin was therefore required.
Our study has a number of limitations. First, it was a retrospective study. Secondly, there was no control group. Thirdly, in most patients, colistin was used in combination with other antimicrobials. The use of concomitant drugs does not allow us to draw any definitive conclusions on the clinical effectiveness of colistin. Despite these limitations, our study involved a relatively large number of patients, and all were major burn victims.
Conclusions
Colistin appears to be a relatively safe and effective therapeutic agent for treating major burn patients with infections caused by MDR Gram-negative bacteria when no other drug is available. Thus, the reasonable application of colistin is a good option. Further studies with larger numbers of patients and control groups are necessary to confirm these results. In addition, studies to define the optimum dosing strategies in burn patients, including total daily dose, mode of administration, and dosing intervals, are needed.
References
Branski LK, Al-Mousawi A, Rivero H, Jeschke MG, Sanford AP, Herndon DN. Emerging infections in burns. Surg Infect. 2009;10:389–97. doi:10.1089/sur.2009.024.
Hsueh PR, Teng LJ, Yang PC, Chen YC, Ho SW, Luh KT. Persistence of a multidrug-resistant Pseudomonas aeruginosa clone in an intensive care burn unit. J Clin Microbiol. 1998;36:1347–51.
Tankovic J, Legrand P, De Gatines G, Chemineau V, Brun-Buisson C, Duval J. Characterization of a hospital outbreak of imipenem-resistant Acinetobacter baumannii by phenotypic and genotypic typing methods. J Clin Microbiol. 1994;32:2677–81.
Molina J, Cordero E, Pachon J. New information about the polymyxin/colistin class of antibiotics. Expert Opin Pharmacother. 2009;10:2811–28. doi:10.1517/14656560903334185.
Benedict RG, Langlykke AF. Antibiotic activity of Bacillus polymyxa. J Bacteriol. 1947;54:24.
Reed MD, Stern RC, O’Riordan MA, Blumer JL. The pharmacokinetics of colistin in patients with cystic fibrosis. J Clin Pharmacol. 2001;41:645–54.
Ryan KJ, Schainuck LI, Hickman RO, Striker GE. Colistimethate toxicity. Report of a fatal case in a previously healthy child. J Am Med Assoc. 1969;207:2099–101.
Koch-Weser J, Sidel VW, Federman EB, Kanarek P, Finer DC, Eaton AE. Adverse effects of sodium colistimethate. Manifestations and specific reaction rates during 317 courses of therapy. Ann Intern Med. 1970;72:857–68.
Evans ME, Feola DJ, Rapp RP. Polymyxin B sulfate and colistin: old antibiotics for emerging multiresistant gram-negative bacteria. Ann Pharmacother. 1999;33:960–7.
Markou N, Apostolakos H, Koumoudiou C, Athanasiou M, Koutsoukou A, Alamanos I, et al. Intravenous colistin in the treatment of sepsis from multiresistant Gram-negative bacilli in critically ill patients. Crit Care. 2003;7:78–83. doi:10.1186/cc2358.
Bellomo R, Ronco C. Continuous haemofiltration in the intensive care unit. Crit Care. 2000;4:339–45.
Hand WL. Current challenges in antibiotic resistance. Adolescent Med. 2000;11:427–38.
Kollef MH. The prevention of ventilator-associated pneumonia. New Engl J Med. 1999;340:627–34. doi:10.1056/NEJM199902253400807.
Bonomo RA, Szabo D. Mechanisms of multidrug resistance in Acinetobacter species and Pseudomonas aeruginosa. Clin Infect Dis. 2006;43:49–56. doi:10.1086/504477.
Trottier V, Namias N, Pust DG, Nuwayhid Z, Manning R, Marttos AC Jr, et al. Outcomes of Acinetobacter baumannii infection in critically ill surgical patients. Surg Infect (Larchmt). 2007;8:437–43. doi:10.1089/sur.2006.029.
Falagas ME, Kasiakou SK. Colistin: the revival of polymyxins for the management of multidrug-resistant Gram-negative bacterial infections. Clin Infect Dis. 2005;40:1333–41. doi:10.1086/429323.
Falagas ME, Kasiakou SK. Toxicity of polymyxins: a systematic review of the evidence from old and recent studies. Crit Care. 2006;10:27. doi:10.1186/cc3995.
Montero M, Horcajada JP, Sorli L, Alvarez-Lerma F, Grau S, Riu M, et al. Effectiveness and safety of colistin for the treatment of multidrug-resistant Pseudomonas aeruginosa infections. Infection. 2009;37:461–5.
Landman D, Georgescu C, Martin DA, Quale J. Polymyxins revisited. Clin Microbiol Rev. 2008;21:449–65. doi:10.1128/CMR.00006-08.
Michalopoulos A, Papadakis E. Inhaled anti-infective agents: emphasis on colistin. Infection. 2010;38:81–8. doi:10.1007/s15010-009-9148-6.
Kaye KM, Kaye D. Polymyxins (polymyxin B and colistin). In: Mandell GL, Bennett JE, Dolin R, editors. Mandell, Douglas, and Bennett’s principles and practice of infectious diseases. 6th edn. Philadelphia: Churchill Livingstone; 2005. p. 435–6.
Levin AS, Barone AA, Penco J, Santos MV, Marinho IS, Arruda EA, et al. Intravenous colistin as therapy for nosocomial infections caused by multidrug-resistant Pseudomonas aeruginosa and Acinetobacter baumannii. Clin Infect Dis. 1999;28:1008–11. doi:10.1086/514732.
Ganapathy H, Pal SK, Teare L, Dziewulski P. Use of colistin in treating multi-resistant Gram-negative organisms in a specialised burns unit. Burns. 2010;36:522–7. doi:10.1016/j.burns.2009.07.010.
Goverman J, Weber JM, Keaney TJ, Sheridan RL. Intravenous colistin for the treatment of multi-drug resistant, Gram-negative infection in the pediatric burn population. J Burn Care Res. 2007;28:421–6. doi:10.1097/BCR.0B013E318053D346.
Rosanova M, Epelbaum C, Noman A, Villasboas M, Alvarez V, Berberian G, et al. Use of colistin in a pediatric burn unit in Argentina. J Burn Care Res. 2009;30:612–5. doi:10.1097/BCR.0b013e3181abffb6.
Acknowledgments
We would like to thank all physicians of the Burn Therapeutic Unit and Burn Intensive Care Unit who participated in this study as well as pharmacist J. Yim for expert advice.
Conflict of interest
The authors have nothing to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s15010-011-0209-2.
Rights and permissions
About this article
Cite this article
Cho, Y.S., Yim, H., Yang, H.T. et al. Use of parenteral colistin for the treatment of multiresistant Gram-negative organisms in major burn patients in South Korea. Infection 40, 27–33 (2012). https://doi.org/10.1007/s15010-011-0192-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-011-0192-7