Abstract
Background:
Therapeutic strategies that can promote platelet production are in demand to enhance clinical outcomes of bone marrow transplantation (BMT). Our research group has studied human tonsil-derived mesenchymal stem cells (T-MSCs) and their effectiveness in promoting bone marrow (BM) engraftment. Here, we analyzed the effects of T-MSCs on platelet production and hemostasis.
Methods:
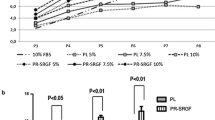
Donor BM cells (BMCs) were isolated from C57BL/6 mice and transplanted with or without T-MSCs to BALB/c recipient mice. Mice were sacrificed and blood cells were counted using an Auto Hematology Analyzer. Femur sections were stained with CD41 antibody to analyze megakaryocytes in the BM. Growth factor secretion from MSCs was analyzed using the Quantibody Array. Effects of T-MSC conditioned medium (CM) on megakaryopoiesis were investigated using the MegaCult assay. In a mouse model of BMT, T-MSC CM was injected with or without anti-placental growth factor (α-PlGF) blocking antibody, and blood cell numbers and coagulation were analyzed.
Results:
T-MSC co-transplantation increased percent survival of BMT mice. Platelet numbers were significantly lower in the BMC-only group, whereas T-MSC co-transplantation restored circulating platelets to levels similar to those of the control group. Significantly reduced numbers of CD41 + megakaryocytes in Bu-Cy and BMC groups were increased by T-MSC co-transplantation. PlGF secretion from T-MSCs were detected and enhanced megakaryopoiesis, platelet production, and coagulation by T-MCS CM were disrupted in the presence of the α-PlGF blocking antibody.
Conclusion:
We demonstrated the effectiveness of T-MSC co-transplantation in promoting platelet production and coagulation after BMT. These findings highlight the potential therapeutic relevance of T-MSCs for preventing thrombocytopenia after BMT.



Similar content being viewed by others
References
Ara T, Tokoyoda K, Sugiyama T, Egawa T, Kawabata K, Nagasawa T. Long-term hematopoietic stem cells require stromal cell-derived factor-1 for colonizing bone marrow during ontogeny. Immunity. 2003;19:257–67.
Juarez JG, Harun N, Thien M, Welschinger R, Baraz R, Pena AD, et al. Sphingosine-1-phosphate facilitates trafficking of hematopoietic stem cells and their mobilization by CXCR4 antagonists in mice. Blood. 2012;119:707–16.
Walasek MA, van Os R, de Haan G. Hematopoietic stem cell expansion: challenges and opportunities. Ann N Y Acad Sci. 2012;1266:138–50.
Ratajczak MZ, Suszynska M. Emerging strategies to enhance homing and engraftment of hematopoietic stem cells. Stem Cell Rev Rep. 2016;12:121–8.
Noort WA, Kruisselbrink AB, Anker PS, Kruger M, van Bezooijen RL, de Paus RA, et al. Mesenchymal stem cells promote engraftment of human umbilical cord blood-derived CD34(+) cells in NOD/SCID mice. Exp Hematol. 2002;30:870–8.
Koç ON, Gerson SL, Cooper BW, Dyhouse SM, Haynesworth SE, Caplan AI, et al. Rapid hematopoietic recovery after coinfusion of autologous-blood stem cells and culture-expanded marrow mesenchymal stem cells in advanced breast cancer patients receiving high-dose chemotherapy. J Clin Oncol. 2000;18:307–16.
Li T, Luo C, Zhang J, Wei L, Sun W, Xie Q, et al. Efficacy and safety of mesenchymal stem cells co-infusion in allogeneic hematopoietic stem cell transplantation: a systematic review and meta-analysis. Stem Cell Res Ther. 2021;12:246.
Tay J, Allan D, Beattie S, Bredeson C, Fergusson D, Maze D, et al. Rationale and design of platelet transfusions in haematopoietic stem cell transplantation: the PATH pilot study. BMJ Open. 2016;6:e013483.
Christou G, Kekre N, Petrcich W, Tokessy M, Neurath D, Giulivi A, et al. Impact of platelet transfusion on toxicity and mortality after hematopoietic progenitor cell transplantation. Transfusion. 2015;55:253–8.
Kumar A, Mhaskar R, Grossman BJ, Kaufman RM, Tobian AA, Kleinman S, et al. Platelet transfusion: a systematic review of the clinical evidence. Transfusion. 2015;55:1116–27; quiz 1115.
Deutsch VR, Tomer A. Megakaryocyte development and platelet production. Br J Haematol. 2006;134:453–66.
Ghanima W, Cooper N, Rodeghiero F, Godeau B, Bussel JB. Thrombopoietin receptor agonists: ten years later. Haematologica. 2019;104:1112–23.
Kuter DJ. Romiplostim. Cancer Treat Res. 2011;157:267–88.
Carpenedo M, Cantoni S, Coccini V, Pogliani EM, Cairoli R. Response loss and development of neutralizing antibodies during long-term treatment with romiplostim in patients with immune thrombocytopenia: a case series. Eur J Haematol. 2016;97:101–3.
Ryu JH, Park M, Kim BK, Kim YH, Woo SY, Ryu KH. Human tonsilderived mesenchymal stromal cells enhanced myelopoiesis in a mouse model of allogeneic bone marrow transplantation. Mol Med Rep. 2016;14:3045–51.
Kim YH, Cho KA, Lee HJ, Park M, Shin SJ, Park JW, et al. Conditioned medium from human tonsil-derived mesenchymal stem cells enhances bone marrow engraftment via endothelial cell restoration by pleiotrophin. Cells. 2020;9:221.
Lee HJ, Kim YH, Choi DW, Cho KA, Park JW, Shin SJ, et al. Tonsil-derived mesenchymal stem cells enhance allogeneic bone marrow engraftment via collagen IV degradation. Stem Cell Res Ther. 2021;12:329.
Ryu KH, Cho KA, Park HS, Kim JY, Woo SY, Jo I, et al. Tonsil-derived mesenchymal stromal cells: evaluation of biologic, immunologic and genetic factors for successful banking. Cytotherapy. 2012;14:1193–202.
Kim YH, Cho KA, Lee HJ, Park M, Kim HS, Park JW, et al. Identification of WNT16 as a predictable biomarker for accelerated osteogenic differentiation of tonsil-derived mesenchymal stem cells in vitro. Stem Cells Int. 2019;2019:8503148.
Choi DW, Cho KA, Lee HJ, Kim YH, Woo KJ, Park JW, et al. Cotransplantation of tonsilderived mesenchymal stromal cells in bone marrow transplantation promotes thymus regeneration and T cell diversity following cytotoxic conditioning. Int J Mol Med. 2020;46:1166–74.
Wang X, Zhang M, He P. Pre-infusion single-dose mesenchymal stem cells promote platelet engraftment and decrease severe acute graft versus host disease without relapse in haploidentical peripheral blood stem cell transplantation. J Int Med Res. 2020;48:300060520920438.
Schiffer CA, Bohlke K, Delaney M, Hume H, Magdalinski AJ, McCullough JJ, et al. Platelet transfusion for patients with cancer: American society of clinical oncology clinical practice guideline update. J Clin Oncol. 2018;36:283–99.
Friedmann AM, Sengul H, Lehmann H, Schwartz C, Goodman S. Do basic laboratory tests or clinical observations predict bleeding in thrombocytopenic oncology patients? A reevaluation of prophylactic platelet transfusions. Transfus Med Rev. 2002;16:34–45.
Wandt H, Schaefer-Eckart K, Wendelin K, Pilz B, Wilhelm M, Thalheimer M, et al. Therapeutic platelet transfusion versus routine prophylactic transfusion in patients with haematological malignancies: an open-label, multicentre, randomised study. Lancet. 2012;380:1309–16.
Desborough M, Estcourt LJ, Doree C, Trivella M, Hopewell S, Stanworth SJ, et al. Alternatives, and adjuncts, to prophylactic platelet transfusion for people with haematological malignancies undergoing intensive chemotherapy or stem cell transplantation. Cochrane Database Syst Rev. 2016;8:CD010982.
Mirghafourvand M, Mohammad-Alizadeh S, Abbasalizadeh F, Shirdel M. The effect of prophylactic intravenous tranexamic acid on blood loss after vaginal delivery in women at low risk of postpartum haemorrhage: a double-blind randomised controlled trial. Aust N Z J Obstet Gynaecol. 2015;55:53–8.
Estcourt LJ, Desborough M, Brunskill SJ, Doree C, Hopewell S, Murphy MF, et al. Antifibrinolytics (lysine analogues) for the prevention of bleeding in people with haematological disorders. Cochrane Database Syst Rev. 2016;3:CD009733.
Carlo-Stella C, Di Nicola M, Longoni P, Cleris L, Lavazza C, Milani R, et al. Placental growth factor-1 potentiates hematopoietic progenitor cell mobilization induced by granulocyte colony-stimulating factor in mice and nonhuman primates. Stem Cells. 2007;25:252–61.
Hattori K, Heissig B, Wu Y, Dias S, Tejada R, Ferris B, et al. Placental growth factor reconstitutes hematopoiesis by recruiting VEGFR1(+) stem cells from bone-marrow microenvironment. Nat Med. 2002;8:841–9.
Pitchford SC, Lodie T, Rankin SM. VEGFR1 stimulates a CXCR4-dependent translocation of megakaryocytes to the vascular niche, enhancing platelet production in mice. Blood. 2012;120:2787–95.
Repetto O, De Re V. Coagulation and fibrinolysis in gastric cancer. Ann N Y Acad Sci. 2017;1404:27–48.
Kim YH, Park M, Cho KA, Kim BK, Ryu JH, Woo SY, et al. Tonsil-derived mesenchymal stem cells promote bone mineralization and reduce marrow and visceral adiposity in a mouse model of senile osteoporosis. Stem Cells Dev. 2016;25:1161–71.
Acknowledgements
This work was supported by the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health and Welfare, Republic of Korea (Grant Number: HI18C2392), the National Research Foundation of Korea funded by the Ministry of Science and ICT (2020R1C1C1014665) and RP-Grant 2020 of Ewha Womans University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no actual or potential conflict of interest.
Ethical statement
The animal studies were performed after receiving approval of the Institutional Animal Care and Use Committee (IACUC) in Ewha Womans University College of Medicine (IACUC approval No. EUM 20–014).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kim, YH., Lee, HJ., Cho, KA. et al. Promotion of Platelet Production by Co-Transplantation of Mesenchymal Stem Cells in Bone Marrow Transplantation. Tissue Eng Regen Med 19, 131–139 (2022). https://doi.org/10.1007/s13770-021-00401-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13770-021-00401-9