Abstract
Amid COVID-19, world has gone under environmental reformation in terms of clean rivers and blue skies, whereas, generation of biomedical waste management has emerged as a big threat for the whole world, especially in the developing nations. Appropriate biomedical waste management has become a prime concern worldwide in the pandemic era of COVID-19 as it may affect environment and living organisms up to a great extent. The problem has been increased many folds because of unexpected generations of hazardous biomedical waste which needs extraordinary attentions. In this paper, the impacts and future challenges of solid waste management especially the biomedical waste management on environment and human beings have been discussed amid COVID-19 pandemic. The paper also recommends some guidelines to manage the bulk of medical wastes for the protection of human health and environment. The paper summarizes better management practices for the wastes including optimizing the decision process, infrastructure, upgrading treatment methods and other activities related with the biological disasters like COVID-19. As achieved in the past for viral disinfection, use of UV- rays with proper precautions can also be explored for COVID-19 disinfection. For biomedical waste management, thermal treatment of waste can be an alternative, as it can generate energy along with reducing waste volume by 80–95%. The Asian Development Bank observed that additional biomedical waste was generated ranged from 154 to 280 tons/day during the peak of COVID-19 pandemic in Asian megacities such as Manila, Jakarta, Wuhan, Bangkok, Hanoi, Kuala Lumpur.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
COVID-19 (or Coronavirus disease 2019) originated from the animals (meat/fisheries market of the Wuhan city, China) can cause severe infections to the human respiration system (Cascella et al. 2020; Roujian et al. 2020; Zhu et al. 2020; Xu et al. 2020). Firstly, it was diagnosed in the end of December, 2019 in Wuhan city of China when like pneumonia symptoms were observed in the local residents of Wuhan (WHO 2020a; Lokhandwala and Gautam 2020; Sohrabi et al. 2020). Other health problems were also got detected because of CIVID-19 infections including breath shortness, fever, pain in muscles and head (Huang et al. 2020). WHO declared worldwide human health emergency (pandemic) due to fast rate of COVID-19 infections as it took around 3 months durations only to reach in 100 nations. Moreover, 10 million people of the world got infected with COVID-19 till the last of May, 2020, whereas up to last week of June, 2020, COVID-19 infections reached in 216 countries (WHO 2020b). Even top economic nations of the world (USA, Germany, France, Spain, Japan, Singapore, Italy etc.) were stuck in the raising COVID-19 infections among the community people (Amanat and Krammer 2020). However, USA was and still on the top in terms of highest numbers of both infections and deaths due this pandemic (CDC 2020). In Asia, India is on the top position reading deaths as well infections due to corona virus (MoHFW 2020). In the absence of vaccine, testing of COVID-19 has become very important to prevent its further infections and reverse-transcription polymerase chain reaction, medical imaging and computed tomography are the recommended methods of detection (Ardakani et al. 2020). Despite of infecting huge population, the fatality rate of COVID-19in India is less than Middle East respiratory syndrome (MERS, year 2012) and severe acute respiratory syndrome (SARS CoV-1 year 2003) and more than the Spanish flu (year 1918) as shown in Fig. 1.
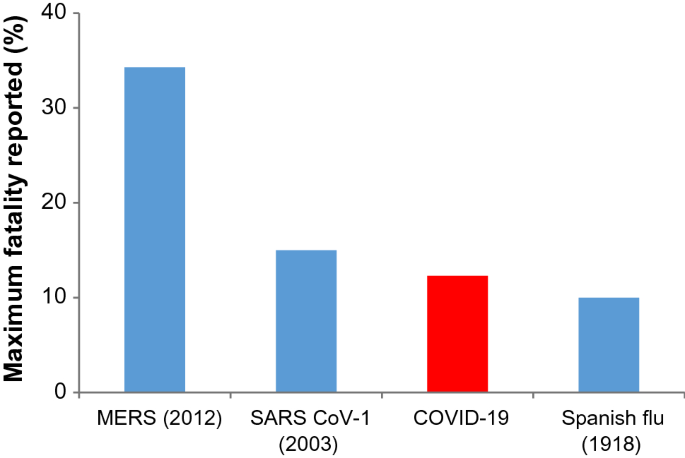
Source: Modified from Goel et al. 2020)
Human fatality rates of different viral infections (
From Fig. 1, it was observed that in year 2012, MERS had affected people of 27 countries of the world with maximum fatality rate of 34.3% followed by SARS CoV-1 in year 2003 with 15%. In 1918, the fatality rate of Spanish flu was rescored as 10% which is less than COVID-19 (12.3%) (Callaway et al. 2020; Goel et al. 2020). However, according to Gates (2020), it can kill only 1% of total infected persons including old aged people as well as adults, if they were already suffering with some serious health disorders. However, it can spread easily among the humans as compared to other illness (Goel et al. 2020). Because of this reason, initially, rate of infection was slow and later through community transmission; it has reached in every part of the world (Anderson et al. 2020; Shammi et al. 2020).
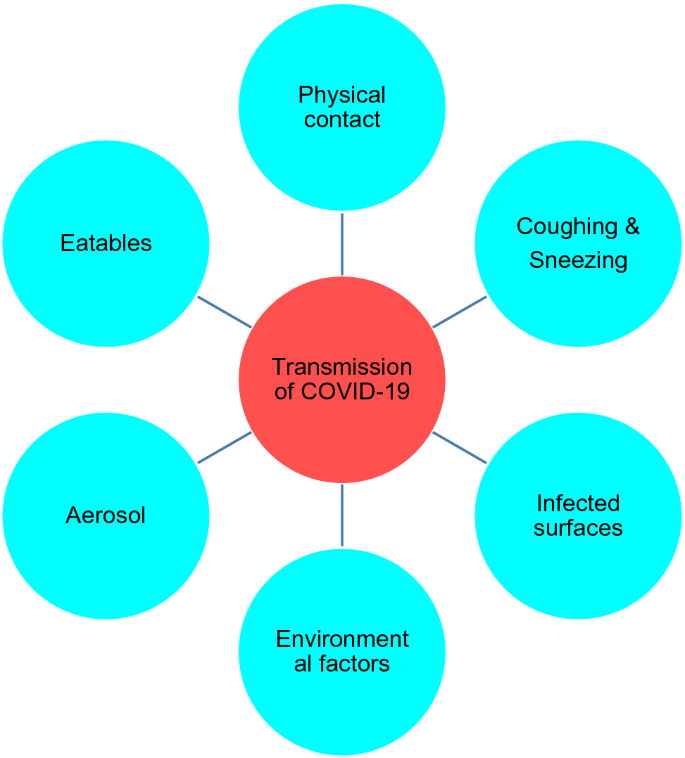
Factors responsible for the transmission of COVID-19
As per the studies, it has been found that several days are required for complete inactivation of COVID-19 virus (Casanova et al. 2009; Qu et al. 2020). It is quite evident corona virus is mostly spreading through physical contacts between the individuals knowingly or unknowingly. However, it can also infect the healthy people through the skin, mouth, nose and eyes of any COVID-19 patient after direct or indirect interactions. The virus can survive on the various types of surfaces (medical wastes, plastic etc.) or environment for a specific time (Weber et al. 2016; Qu et al. 2020). Further, the chances of viral infection may be governed by several factors including stability of virus containing aerosols in the air (usually 3 h is reported), active periods of the virus on the surfaces like steel (7 days), glasses and currency papers (4 days). Even after applying soap on the hands, additional five minutes are required to inactivate the virus. Hence, it is advisable that one should avoid touching any part of the face within 5 min of hand wash (Goel et al. 2020).Other factors of COVID-19 transmission may also be considered as sneezing, coughing, and talking with any infected person. In many studies, presence of COVID-19 virus has been diagnosed in the excreta, tear, urine and other body secretions of the infected people (Zhang et al. 2020; Xia et al. 2020; Peng et al. 2020). In Japan, a study has shown that COVID-19 transmission is also possible through the lighter water droplets containing virus. As lighter water droplets (or aerosols) when come in the contact of any COVID-19 infected person and thereafter it can transmit into healthy people. However, this type of airborne infection depends upon the local weather conditions (wet or dry) (Chin and Poon 2020; Wölfel et al. 2020). Moreover, a theory of asymptomatic or oligosymptomatic infections are also reported in the literatures (Wölfel et al. 2020). There are different types of which can trigger in the transmission of the COVID-19 (Fig. 2).
Most importantly, poor people (may be due to insanitary practices), elderly persons, workers of waste management authorities are in high risk zone of COVID-19 infection. However, their restricted movement can reduce the chance of pandemic outbreak (United Nations 2020). Because of this reason, in USA and Singapore, recycling of waste materials has been discontinued or carried out with less frequency to reduce the risk of further transmission of COVID-19 among the sanitary workers (Zambrano-Monserrate et al. 2020; National Environmental Agency, Singapore 2020). In developing world, situation has become very critical during this pandemic because of unemployment during lockdown and panic of infection among waste management people, and ultimately, it may affect the economy of the nations too (World Bank 2020). According to Nghiem et al. (2020) and Kulkarni and Anantharama (2020) it can be managed by adopting best practices of waste management to safeguard the health of these workers during handling of contagious wastes. Major objective of the present research paper is to explore the practices which can be helpful in the management of biomedical wastes during pandemic like COVID-19. Moreover, alternatives options and challenges of future have also been discussed.
Impacts of COVID-19 pandemic
(i) Impact on the human health
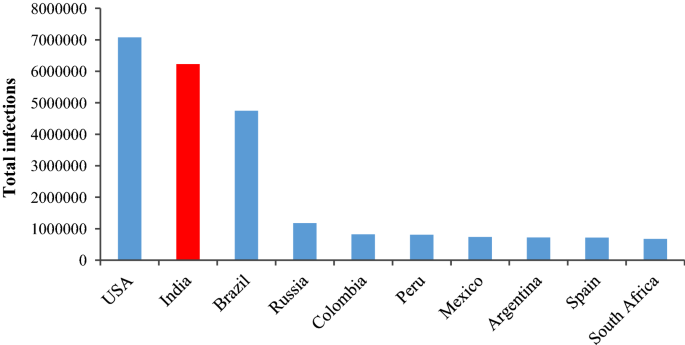
Human respiration system is the main target of this COVID-19 virus. Moreover, this has become more dangerous for the elderly people or the people who are suffering with sever diseases related with cardiac system, diabetes, cancer, or else (Dhama et al. 2020; Rodriguez-Morales et al. 2020; Mahajan and Kaushal 2020). However, it has also found that children are not a common victim of the COVID-19 virus (Huang et al. 2020) because usually they do not go outside the home as well as less travelling exercise (Lee et al. 2020). Chen et al. (2020) reported that only in China health recovery of the citizens was so better due to an improvement in air quality amid COVID-19 lockdown periods. Therefore, due to lockdown, the pollution load of environmental systems (atmosphere, hydrosphere and lithosphere) has decreased worldwide and this may be helpful for the protection of public health. Figure 3 shows the confirmed infections of COVID-19 in top ten countries as on Sept. 30, 2020.
Total COVID-19 infections in top 10 mostly affected countries (WHO 2020b) (assessed on the 30.09.2020)
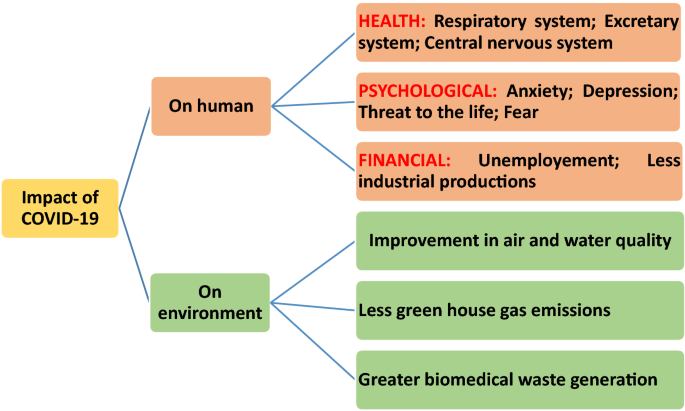
From Fig. 3, it appears that till Sept. 30, most affected countries with COVID-19 infections are USA, Indian, Brazil, Russia and Columbia. Similar problems have been observed in the Bangladesh during lockdown periods amid COVID-19 pandemic (Hopman et al. 2020). Transmission of corona virus through air is also reported (Bourouiba 2020) and can be prevented by using face mask at crowded places (Klemeš et al. 2020). Moreover, during the crisis maintaining employment opportunities along with public health protection has become top priorities of the government authorities. For public health protection, there are many issues should be handles with due care like advancement of medical standards, easy availability of testing facility, revisions of policies for local public etc. (WHO 2020b; Sharma et al. 2020). In addition to these, many psychological disorders have been observed especially among patients due to this pandemic as studied in United Kingdom (Ford et al. 2020; Holmes et al. 2020). Figure 4 summarises the diverse types of impacts observed during the COVID-19 outbreak.
Elderly people are found at the larger risks of COVID-19 and during quarantine period, there is a great chance of developing mental disorders (for example, anxiety, guiltiness, dementia, depression etc.) because of loneliness (Armitage and Nellums 2020; Holmes et al. 2020; Ahorsu et al. 2020; Shammi et al. 2020).These mental problems may be responsible for the increase in number of suicide cases in the society (Duan and Zhu 2020). However, few medicines are recommended in case of emergency situation for COVID-19 patients (Singh et al. 2020). Recently, Goel et al. (2020) reported that silver coated grapheme oxide sheets and chiral gold nanohybrids for the inhibition as well as detection of the different types of viruses including corona virus. According to Chan (2020) application of different types of nano-materials should also be explored against the coronavirus. Because of unavailability of proper medication, “social lockdown” or “social distancing” has been imposed to stop the transmission of COVID-19 virus across the world (Paital et al. 2020; Zambrano-Monserrate et al. 2020; Lokhandwala and Gautam 2020; Somani et al. 2020). During lockdown, restrictions were imposed on every type of public meetings, industries and automobiles to maintain social distancing. Due to shutdown of factories and vehicles many positive changes have been observed in the cosmopolitan environment.
(ii) Impact on the environmental systems
In twenty-first century, there are many challenges for whole world including severe environmental quality diminution (Chakraborty and Maity 2020) due to over industrialization as well as unorganized fast urbanization as it requires huge demand of natural resources. Because of overexploitation of resources, ecological systems have been deteriorated which includes air pollution, water quality degradation, soil contamination, global warming, threat to the biodiversity, human health problems etc. (Bremer et al. 2019). Amid COVID-19 pandemic, world has gone into complete lockdown except essential commodities which imposed ban on the opening of industries as well as movement of the vehicles. Hence, during lockdown periods emission of harmful gases and wastewater discharges were decreased significantly and considerable environmental healing was observed across the world (Australia, China, France, Germany, India, Italy, Iran, Spain, South Korea, Taiwan, Turkey, United Kingdom and USA) since March 2020 (Chakraborty and Maity 2020; Elavarasan and Pugazhendhi 2020; Atalan 2020). As it has been observed that air pollution is responsible for > 7 million human deaths in whole world and out of it, 1.2 million deaths were reported in only in India (WHO 2018; Polk 2019). Significant reduction in the concentration of air pollutants (particulate matters and greenhouse gases) was reported from the various parts of the world like Kazakhstan (Kerimray et al. 2020), India (Mahato et al. 2020) and Brazil (Dantas et al. 2020). Besides, industries and automobiles, operations of aeroplanes were also affected during lockdown and it was also helped in the reduction of greenhouse gases in the atmosphere (Corletta et al. 2020). However, level of indoor air pollutants (including black carbon of smoke) was increased amid lockdown as most of the people were got stuck inside their homes (NASA 2020). Availability of adequate natural ventilation (not any artificial systems like air conditioner etc.) inside the homes could dilute the concentrations of indoor air pollutants (Bhatia and Bhaskar 2020; Somani et al. 2020). Moreover, concentrations of greenhouse gases were also remarkably decreased during lockdown periods, for example 2600 metric tons of carbon dioxide was decreased across the global amid COVID-19 pandemic (Global Climate Report 2019) due to less energy demand as around 64% of total electrical energy is getting produced from the natural gas and coals (Somani et al. 2020). In India, the carbon dioxide emission was decreased in between 15 and 30% during March to April, 2020 (Myllavirta and Dahiya 2020). Similarly, due to closure of machines and restricted vehicle movements, level of noise also got decreased as reported in many countries such as China (19%), USA (36%) and United Kingdom (54%) (Somani et al. 2020). Moreover, decrease in oceanic noise levels were also observed during lockdown due to limited waterways traffic and it could have provided a better environment for aquatic lives (Ian Randall 2020). In India, around 40–75% noise level reductions were reported from the various states or cities (for example, Karnataka, Delhi, Bengaluru, Kolkata) due to non-movements of the trains (Somani et al. 2020) as trains and other vehicles are the principal causes of noise pollution in megacities of India (Mishra et al. 2010). Furthermore, biodiversity conservation via revival of natural shelters for marine organisms (turtles), other aquatic lives, birds, wild life animals were found to be very rapid due to less movement of human beings (Corletta et al. 2020; Zambrano-Monserrate et al. 2020) as the reports were published in the countries like Mexico, Spain, India as well as Ecuador (Zambrano-Monserrate et al. 2020; Somani et al. 2020). Self-purification capacities of many rivers/lakes increased amid lockdown because of less wastewater discharge as most of the pollution in surface water reservoirs is due to the raw sewage mixing into them (Sinha et al. 2016; CPCB 2020a; Corletta et al. 2020; Zambrano-Monserrate et al. 2020). In India, amid lockdown, water quality of rivers Ganga and Yamuna were improved for bathing and aquaculture purpose as observed by the Central Pollution Control Board (CPCB) than previous years (CPCB 2020a). Most importantly, Uttarakhand Pollution Control Board of India stated that Ganga river water at Haridwar (location: Har-ki-Pauri) was improved for drinking purpose after more than 30 years (Katariya 2020). Similarly, (Yunus et al. 2020) reported ~ 15.6% water pollution reduction in the Venbanad Lake of Kerala province of India. These improvements were observed in many Indian states (Uttrakhand, UttarPradesh, West Bengal, Karnataka, Tamilnadu) because of very less number of visitors, drastic decrease in the volume of the untreated effluents (~ 500%) during lockdown periods (Somani et al. 2020).
Challenges of biomedical waste generation and its proper management amid COVID-19 pandemic
Apart from some environmental benefits, great negative impacts will be observed across the globe due to COVID-19 pandemic including public health crisis (WHO 2020a) including hurdles in the recycling of the wastes (Calma 2020), economical emergency and unemployment (Atalan 2020), proper management and disposal of hospital wastes and need of extra disinfectants (Zambrano-Monserrate et al. 2020). Certainly, COVID-19 pandemic is one of the greatest challenges for everyone such as the scientists, industrialists, doctors, paramedical staffs, police, municipal authorities, government authorities as well as local public of the world. Since its beginning in 2019 from China, researchers of the world are working 24 h a day to develop effective medication/or vaccine against it. However, no any solution is reported till now against this virus (Vellingiri et al. 2020). Because of high mutagenic characters and continuous morphological changes in the COVID-19, development of its vaccine is facing difficulties (American Society of Microbiology 2020). Therefore, governments of most of the nations have imposed compulsory national lockdowns to keep safe their citizens except essential supplies of the goods and medicines. Apart from it, individual physical distancing and self-quarantine were also recommended for each person to ensure wellbeing (Balachandar et al. 2020). On the other hand, because of the lockdown, worldwide huge economical loss is expected in near future (Somani et al. 2020) due to closure of industries and manufacturing units (United Nations Industrial Development Organization 2020). Because of shutting industries, product supply chain of goods has been ruined (Kahlert and Bening 2020; Kulkarni and Anantharama 2020). In addition to huge economical loss, health workers and hospitals of the world (both developed and developing countries) are under tremendous pressure due to exponential rate of COVID-19 infections. Moreover, critical patients are not getting proper care due to unavailability of intensive care units in most of the hospitals. Health workers are using personal protective equipments (for example, face mask, transparent face shield, gloves etc.) to protect themselves from this virus and providing these safety devices are also a challenge for the authorities (Dargaville et al. 2020). Some misconceptions have been spread into the society that intake of lemon beverages, wine etc. can be used as medications against Coronavirus (Shammi et al. 2020). Moreover, in most of the countries, numbers of unemployed personas have been increased due to the pandemic (Kulkarni and Anantharama 2020). In order to handle these challenges, many governments are planning effective strategies for the sustainable development of the world after COVID-19 era (Rosenbloom and Markard 2020).
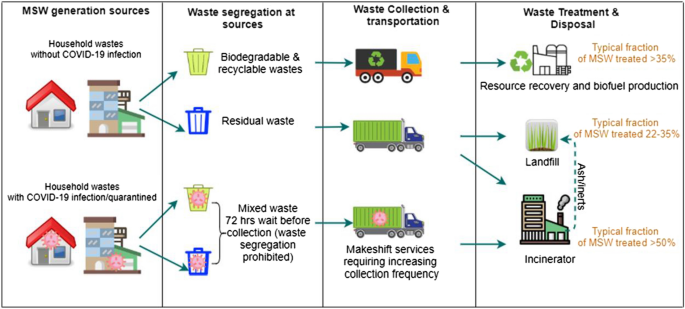
Owing to lockdown amid COVID-19 pandemic, world has gone under environmental reformation in terms of clean rivers and blue skies, whereas, this pandemic has created lots of problems in the management of solid waste (Gardiner 2020). Appropriate solid waste management has been a big challenge for the world especially to the developing nations. COVID-19 pandemic has boosted this problem many folds because of unexpected generations of waste materials (especially biomedical waste: a type of hazardous waste). It needs to be given extraordinary attentions by the waste management authorities and governments (Ferronato and Torretta 2019; Kaufman and Chasan 2020) as the compositions and volumes of the waste materials has been changed (Mallapur 2020). Moreover, Fan et al. (2021) reported that during COVID-19 pandemic many challenges have been emerged while managing waste materials because of changes observed in the volume, types, composition, disposal rate, frequency of collection, availability of treatment options, funds availability etc. as shown in Fig. 5.

modified from Fan et al. 2021)
Common challenges of infected waste management during pandemic (
In order to prevent transmission of COVID-19, lockdown was imposed in many countries which increased online shopping for the household products especially in developed countries. This panic situation has created a big concern of proper waste management in terms of collection, recycle, treatment as well as disposal (Zambrano-Monserrate et al. 2020; Nghiem et al. 2020). Moreover, Rahman et al. (2020) observed that hospital waste can cause severe environmental as well as public health problems as 5.2 million people of the world are dying annually due to mismanagement of hospital waste materials. During the pandemic, the composition of medical waste has changed drastically as it contains huge quantities of discarded masks, gloves, PPE kits etc. (UNEP 2020; Somani et al. 2020) and it could be dangerous for the society (especially workers of waste management authorities) in terms of increasing transmission due to mishandling of such types of infected wastes (Sharma et al. 2020). Similar, concern was also expressed by Occupational Safety and Health Administration (OSHA) regarding further infections among the workers of waste management authorities (OSHA 2020). Further, wastage of plastic waste also got increased across the world which is being used by pharmaceutical industries for packaging purpose (WHO 2020d). Therefore, World Health Organization, Central Pollution Control Board (India), OSHA and other prestigious international organizations have developed new guidelines to manage the waste materials (especially hospital wastes) during COVID-19 (Somani et al. 2020; Kulkarni and Anantharama 2020). According to WHO, > 80% wastes of the hospitals were found in the category of noncontiguous wastes which can be treated and managed similar as municipal waste materials (WHO 2020d). Normally, biomedical wastes are waste generated from the hospitals and veterinary medical premises including syringe, pathological materials, pharmaceutics etc. (Sharma et al. 2020; Somani et al. 2020). Due to COVID-19 pandemic, huge mass of plastic wastes has been increased across the world as it is being used in personal protection kits (for example, gloves, masks, face shield, ventilator etc.) (Klemeš et al. 2020). In India, waste management authorities are in more trouble due to fear of infection as safety measures are not good in the comparison of developed countries. During, lockdown in India, the bulk of biomedical waste was found to be greater than the municipal solid wastes (Somani et al. 2020). Significant reduction in municipal solid waste quantity was attributed to the shutdown of markets, shops, hotels, commercial premises, offices, transport etc. (Somani et al. 2020), whereas, huge amount of biomedical waste was generated probably because of high numbers of the COVID-19 infected persons admitted in the hospitals. In USA, huge quantities of food waste were generated during lockdown as most of the commercial institutes (like hotels, restaurants, mess etc.) had already purchased the raw materials (Kulkarni and Anantharama 2020). During lockdown, similar observations of change in the quantity and composition of waste materials have been reported from North America (SWANA 2020) and China (Klemeš et al. 2020). According to Klemeš et al. (2020), only in Hubei (China), around 370% increase in biomedical waste after COVID-19 infections. However, the quantity of municipal solid waste was generated less than 30% during pandemic. Nghiem et al. (2020) and Zambrano-Monserrate et al. (2020) have also studied the change in the waste composition (and quantity) along with their negative impacts of change in waste generation on the environment and health workers. They found that transmission of virus in community has significantly affected waste recycling facilities around the world. For instance, in United Kingdom, 46% material recovery process was stopped due to lockdown amid COVID-19 pandemic and similarly 31% recycling units of USA were also closed in the similar situations (Somani et al. 2020).
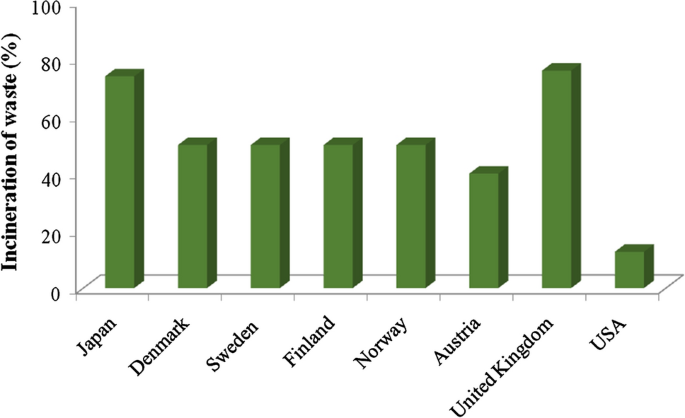
Contagious biomedical wastes can spread disease in living organisms and their mishandling may also be responsible for soil contamination, water pollution (both groundwater and surface water), injuries and death of ecofriendly microbes (Datta et al. 2018). Incineration is one of the preferred options for the waste management especially biomedical (or infectious) wastes in developed countries as shown in Fig. 6.
From the above figure, it is visible that Japan used to treat municipal solid waste through 74% incineration, 17% recycling and only 3% as landfill disposal before the pandemic (Mollica and Balestieri 2020). In Wuhan (China), normally 40 tons of biomedical waste was generated every day and after COVID-19 infections, it was reached up to 240 tons/day. Therefore, the increase in infectious wastes was around 6 times more as compared to normal days. This huge bulk of medical waste created big challenge to the management authorities as Wuhan administration could incinerate only 49 tons (maximum) of waste every day. Moreover, this will not be economical for any country as the costs of incineration for hazardous and municipal solid wastes in China were calculated as 281.7–422.6 USD/tons and 14.1 USD/tons, respectively (Tang 2020; Klemeš et al. 2020). According to WHO (2017), usually, 85% biomedical wastes are not hazardous in nature, rest 10% may be infectious along with 5% radioactive wastes. Before pandemic, except USA (12.7% only) (United States Environmental Protection Agency 2017), many developed countries incinerate their waste materials to recover energy such as 50% municipal waste incinerated in Denmark, Finland, Norway and Sweden (Istrate et al. 2020); 40% in Austria (Kyriakis et al. 2019); 76% in United Kingdom (DEFRA Government of UK 2020). However, recycling of the waste reported 32% in Austria (including composting) (Kyriakis et al. 2019); 45% in United Kingdom (DEFRA Government of UK 2020), and 35.2% in USA (both recycling and composting) (United States Environmental Protection Agency 2017). Therefore, it can be seen from the above results that collection and recycling of waste materials has been disturbed due COVID-19 pandemic. Moreover, pandemic has caused huge economical losses by many ways to the affected countries along with an unseen fear of its infections. Datta et al. (2018) studied that in India by the year 2017, 500 MT/day biomedical wastes were generated and infrastructure of managing biomedical waste is not good. Hence, based on the data of biomedical waste generated in Wuhan (> 6 times) during pandemic, India this situation is expected. However, till now biomedical waste generation data is not available for whole India (Somani et al. 2020). Further, according to one Indian leading newspaper in Gurugram (India), only in 2 months of pandemic, the quantity of biomedical wastes has increased around 40 times as compared to normal months. Similarly, before pandemic 550–600 kg biomedical waste was generated every day in Ahmadabad. Now, it has already increased up to 1000 kg/day during pandemic with an expectation of reaching up to 3000 kg/day especially in the red zones (COVID-19 containment zones (TOI 2020; Somani et al. 2020). Tables 1 and 2 shows the biomedical waste generation in some Asian cities and Indian cities/states.
From Table 1, it can be seen that around every Asian city, the quantity of biomedical wastes has been increased many folds during the outbreak of COVID-19 in the community. In terms of maximum additional biomedical waste was generated in the capital of Philippines, i.e., Manila followed by Jakarta (Indonesia). In, Wuhan (China) and Bangkok (Thailand), 210 tons of additional biomedical waste was generated amid COVID-19 pandemic (ADB 2020). Improper medical waste handling may increase the number of COVID-19 infections in the community (Peng et al. 2020) due to presence of pathogenic microbes (Windfeld and Brooks 2015). Due to airborne infections of the COVID-19 virus in healthy people, use of masks, gloves, face cover etc. has been also increased up to dangerous levels in the world (Bourouiba 2020). At global level, 89 million masks and 76 million gloves are required against the protection from COVID-19 infection (WHO 2020c). According to UNEP (2020), appropriate management of extra waste materials generated during COVID-19 pandemic has become a major concern for the countries. Therefore, medical wastes from the COVID-19 affected zones/hospitals need to be disinfected with careful handling. Treatment of medical waste can be carried out by using thermal techniques such as autoclaving, incineration, microwave and plasma method. However, selection above processes of waste treatment will be governed by many factors like economic feasibility, easy and safe handling, eco-friendly nature as well as harmless to the society (Liu et al. 2015). In order to reduce the chance of infection in the community, effective medical waste (or infectious waste) management should be adapted. Apart from collection and transport, trained manpower should be involved in this activity and disinfection of infectious waste should be compulsory (Klemeš et al. 2020).
The waste management as well as waste recycling process of the developed nations has been disturbed due to this COVID-19 outbreak. Figure 7 shows the waste management practices adapted by developed countries.
From Fig. 7, it can be seen that in developed countries waste management practice involves segregation of the waste at the source of generation followed by their effective collection, transpiration, treatment and disposal. However, during COVID-19 outbreak, the waste collection guidelines were changed as segregation and collection of the wastes from the infected area is carried out after a waiting period of 72 h (ACRPlus 2020; Nghiem et al. 2020). In most of the Asian countries like Bangladesh, India, Indonesia, Malaysia, Myanmar and Thailand, municipal solid wastes are getting managed by land-filling (Yadav and Samadder 2018). Integrated solid waste management system can be a good alternative for the recycling of wastes and also producing energy from the waste materials (Ramachandra et al. 2018). Lack of scientific designing of land-fill sites for waste disposal may lead several environmental problems such as air pollution, water pollution, soil pollution, marine pollution and vector borne-diseases among humans (Pujara et al. 2019). Therefore, mishandling of the biomedical wastes will be more dangerous as it may cause infections in the living organisms.
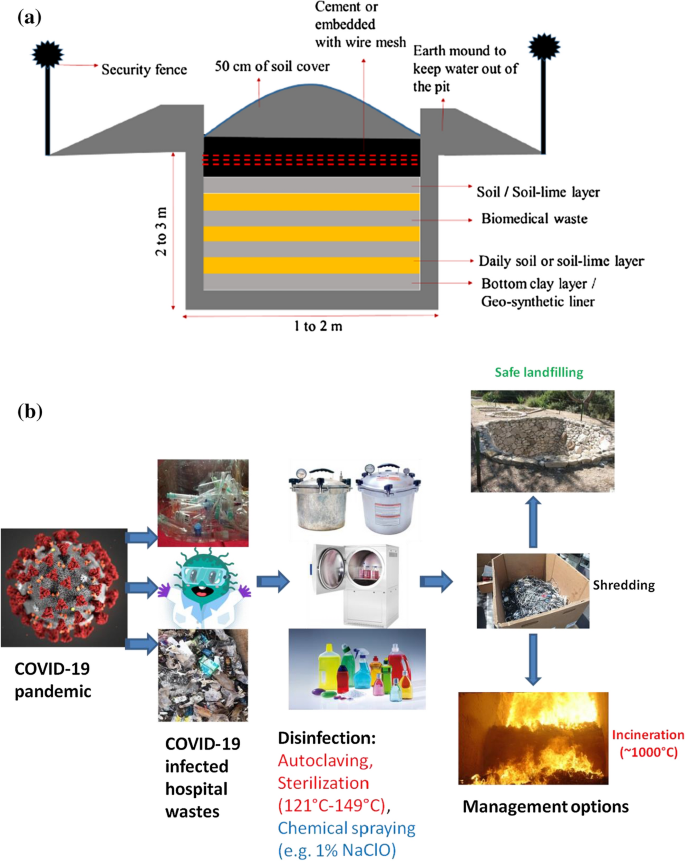
Biomedical waste management is a big challenge for every country especially during this pandemic time. According to the WHO, most of the developing countries do not have advanced systems for the management of biomedical wastes (Chartier et al. 2014). Chartier et al. (2014) proposed a close pit (as shown in Fig. 8a) which should have a dimension of 2 m and 3 m and can be made by clay or geo-synthetic materials used at the base. This arrangement can be used for the safe management of biomedical wastes in emergency situations such as COVId-19 pandemic.
a Layout of a pit for onsite disposal of biomedical wastes in low-income countries during COVID-19 like emergency situation (Chartier et al. 2014; Sharma et al. 2020). (Reprinted from Sharma et al. 2020 with permission from Elsevier). b COVID-19 infected waste handling procedure for low income countries
Figure 8a gives a temporary arrangement for the effective and safe disposal of biomedical wastes in low-income countries (Chartier et al. 2014; Sharma et al. 2020). Further, Fig. 8b can be adopted during the handling infected hospital wastes.
Figure 8b gives a detail outline for the management of infected wastes generated during the pandemic like COVID-19. In this diagram, it can be seen that disinfection of hospital waste has become very important as recommended by many government authorities of the world. For disinfection, autoclaving and sterilization of the tools can be carried out at the temperature ranged between 121 and 149 °C or with the spraying of 0.1% of NaClO. After, disinfection processes, the medical wastes can be shredded and incinerated (~ 1000 °C temperature) followed by ultimate disposal in landfills. Further, incineration has been considered as the best method for the treatment of hazardous wastes (e.g. medical wastes) as it will condense the weight along with volume of the wastes (Rajor et al. 2012). Even, US Environmental Protection Agency (USEPA 2020) issued special guidelines for managing food wastes of residential colonies and other commercial buildings during pandemic. Similarly, Government of India issued guidelines for the management of waste products generated during sudden lockdown. These wastes included perishable agricultural products as well (FAO 2020). According to Klemeš et al. (2020), environment and human health can be protected well after appropriate waste management. Hospital or infectious wastes can be managed effectively through proper collection, transport, treatment and final disposal. It also requires trained health workers who should be aware about the proper disinfection process along with self-protection too. Wasted PPE kits volume can also be decreased, if these materials (like antiviral masks, face shields etc.) can be reused after disinfections (Goel et al. 2020).Previously, viral disinfection was achieved by using UV-C rays (at 254 nm) in 40 min (Darnell et al. 2004), but in case of COVID-19, it is a matter of exploration. Moreover, it was also reported that UV-C rays can lead skin and eye disorders. Therefore, it must be examined before suggesting the application of UV-C rays as a disinfectant (Goel et al. 2020).Thermal treatment of waste can be an alternative for their management as it will generate energy along with reducing waste volume by 80–95%, and mineralization etc. (Singh et al. 2011; Brunner and Rechberger 2015; World Bank 2018). Implementation of these technologies were successful in some developed and developing countries and land-filling has become a rare practice in the developed nations because of land scarcity or/and environmental pollutions. Further, due to high investments, in developing countries it is still inaccessible (Mayer et al. 2019). Apart from the above advantages, incineration generates the ash residues which may contain toxic metals etc. Similarly, groundwater contamination may happen due to the disposal of such residues in the landfills (Rajor et al. 2012). Dargaville et al. (2020) recommended some steps to reduce the wastage of PPE kits which includes:
-
To explore the possibility of recycling of PPE kits (gloves, mask, face shield etc.);
-
Disinfection should be ensured before recycling
-
One of the best disinfection methods should be shared with everyone (especially medical workers)
-
Material’s properties should be examined before recycling
-
Fix the guidelines for their number of recycling
-
Exchange of recycled materials should not be allowed
-
Time to time expert’s (material science, clinical doctors, virologist etc.) guidelines should be shared.
These are the general guidelines to be followed everywhere to reduce the quantity of medical wastes along with the human health and environmental protections (Dargaville et al. 2020).According to WHO, thermal treatment and/or application of conventional biocidal materials can be integrated with waste treatment systems for inactivating Coronavirus before the disposal of biomedical wastes (Kampf et al. 2020). Apart from these options of biomedical waste management; some extra efforts are needed to upgrade the existing waste management systems so that it can deal with emergency situations like this pandemic (COVID-19).
Some challenges observed as wastes are also generated from the mildly infected or asymptomatic people that may have viral infections. COVID-19 virus can be present in active form for different time periods (few hours to days) on the cardboards, plastic materials and metallic objects (Kampf et al. 2020; Doremalen et al. 2020; Nghiem et al. 2020). Somani et al. (2020) observed other waste materials which may be considered as infectious in nature, if not treated properly. These wastes are syringe, needles, masks, gloves, medicines, discarded materials from the home quarantine patients etc. Mishandling of these wastes may trigger the chance of more infections in public as well as health workers (Sharma et al. 2020; Kulkarni and Anantharama 2020).Further studies have shown that in between 21 and 23 °C temperature in presence of 40% relative humidity, the survival time of Coronavirus was 7 days. However, in atmosphere, with 65% relative humidity the activation time was drastically reduced up to 3 h with same temperature range (Doremalen et al. 2020). Kampf et al. (2020) reported 9 days active period of Coronavirus on the metal, glass or plastic. Further, Chin et al. (2020) found that at 70 °C, COVID-19 virus did not survive more than 5 min. National Biodefense Analysis and Countermeasures Centre, USA found in the initial studies that direct sunlight can be very effective to inactivate the Coronavirus within minutes from the many surfaces (Goel et al. 2020). Better management of the wastes can be carried out by optimizing the decision process, infrastructure, upgrading treatment methods and other activities related with the biological disasters like COVID-19 (Klemeš et al. 2020).
Provisions for biomedical waste management in India amid COVID-19
According to Bio-Medical Waste Management Rules, 2016 passed by Indian parliament data of biomedical waste generation should be updated on daily basis by the health care service providers and also, they must expose monthly information on their website (BMWM 2016). These rules were amended at time to time as per the need of the hour to make the effective biomedical waste management in the country. Amid COVID-19 pandemic, like other countries, Indian government has also taken many initiations for the purpose of quarantine, isolation, sampling, laboratory works etc. These initiatives were in agreement with the guidelines of various international (WHO, CDC etc.) and national agencies (MoH&FW, ICMR, CPCB etc.) such as application of separate colour storage basket or double layered bags with proper labelling, separate collection for biomedical wastes etc. During COVID-19 pandemic, some activities were recommended for the rapid and effective waste management by the Indian government to reduce the chance of further infections such as use PPE kits especially by the health workers/waste management people, providing training for their safety, record maintenance, extra working times for treatment facilities etc. (Soni 2020). CPCB has developed a mobile app, i.e., ‘COVID19BWM’ for the daily updation of the generation of biomedical wastes from COVID-19 related places. Moreover, 0.5% chlorine solution was recommended for the disinfection purpose where the patients wards. However, COVID-19 waste and their storage places should be disinfected with 1% sodium hypochlorite solution on daily basis (CPCB 2020b). These guidelines were revised again (on July 17, 2020) and some significant amendments were carried out to fight with the COVID-19 virus such as rail coaches can also be used as isolation wards the materials used by COVID-19 patients included in the category of biomedical waste and their treatment should be mandatory as per the guidelines provided by CPCB and yellow bags can be used for their collection. It was mandatory that do not mix the municipal solid wastes with the waste generated from the COVID-19 infected places/homes (CPCB 2020c). There, it can be said that despite of being a developing nation, Indian authorities are also doing lots of efforts to reduce the numbers of COVID-19 infections in the community.
Conclusion
Amid COVID-19, world has gone under environmental reformation in terms of clean rivers and blue skies, whereas, this pandemic has hurdled the appropriate solid waste management process and the same has emerged as a big threat for the world especially to the developing nations. Researchers have suggested some steps to reduce the wastage of biomedical waste and explored the mechanisms of safe and hygienic recycling. As advised by the WHO, developing countries, who are deficient of advanced systems for the management of biomedical wastes should follow the temporary solution of a close pit with a dimension of 2 m and 3 m and can be made by clay or geo-synthetic materials used at the base and the same arrangement can be used for the safe management of biomedical wastes in emergency situations such as COVId-19 pandemic wastes in emergency situations. The paper summarizes that better management of the wastes can be carried out by optimizing the decision process, infrastructure, upgrading treatment methods and other activities related with the biological disasters like COVID-19. National Biodefense Analysis and Countermeasures Centre, USA found in the initial studies that direct sunlight can be very effective to inactivate the Coronavirus within minutes from the many surfaces. Hospital or infectious wastes can be managed effectively through proper collection, transport, treatment and final disposal. The health workers must be trained enough and should be aware about the proper disinfection process along with self-protection too. Wasted PPE kits volume can also be decreased by reusing the same after disinfections. As achieved in the past for viral disinfection, the use of UV-C rays with proper precautions can also be explored for COVID-19 disinfection. Waste management especially for biomedical waste management, thermal treatment of waste can be an alternative, as it can generate energy along with reducing waste volume by 80–95%.
References
ACRPlus-Association of Cities and Regions for Sustainable Resource Management (2020) Municipal waste management and COVID-19. https://www.acrplus.org/en/municipal-waste-management-covid-19. Accessed 4 May 2020
ADB (2020) Asian Development Bank. Managing infectious medical waste during the COVID-19 pandemic. https://www.adb.org/sites/default/files/publication/578771/managingmedical-waste-covid19.pdf. accessed 4 May 2020
Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH (2020) The fear of COVID-19 scale: development and initial validation. Int J Ment Health Addict. https://doi.org/10.1007/s11469-020-00270-8
Amanat F, Krammer F (2020) SARS-CoV-2 vaccines: status report. Immunity 52(4):83–589. https://doi.org/10.1016/j.immuni.2020.03.007
American Society of Microbiology (2020). https://asm.org/PressReleases/2020/COVID-19. Accessed Aug 10 2021
Anderson RM, Heesterbeek H, Klinkenberg D, Hollingsworth TD (2020) How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet 395(10228):931–934
Ardakani AA, Kanafi AR, Acharya UR, Khadem N, Mohammadi A (2020) Application of deep learning technique to manage COVID-19 in routine clinical practice using CT images: results of 10 convolutional neural networks. Comput Biol Med 30:103795
Armitage R, Nellums LB (2020) COVID-19 and the consequences of isolating the elderly. Lancet Public Health 5(5):e256. https://doi.org/10.1016/S2468-2667(20)30061-X
Atalan A (2020) Perspective—Is the lockdown important to prevent the COVID-19 pandemic? Effects on psychology, environment and economy-perspective. Ann Med Surg 56:38–42
Balachandar V, Kaavya J, Mahalaxmi I, Arul N, Vivekanandhan G, Bupesh G, Singaravelu G, Anila V, Dhivya V, Harsha G, Kamarajan R (2020) COVID-19: a promising cure for the global panic. Sci Total Environ 725:138277
Bhatia A, Bhaskar S (2020) Coronavirus outbreak explained: are air conditioners safe to use during the COVID-19 pandemic. NDTV. https://swachhindia.ndtv.com
BMWM (2016) Bio-medical waste management rules, 2016. Ministry of Environment, Forest & Climate Change, Delhi – 110032, India. Dated 19 Feb 2020
Bourouiba L (2020) Turbulent gas clouds and respiratory pathogen emissions. Potential implications for reducing transmission of COVID-19. J Am Med Assoc. https://doi.org/10.1001/jama.2020.4756
Bremer S, Schneider P, Glavovic B (2019) Climate change and amplified representations of natural hazards in institutional cultures. Oxf Res Encycl Nat Hazard Sci. https://doi.org/10.1093/acrefore/9780199389407.013.354
Brunner PH, Rechberger H (2015) Waste to energy—key element for sustainable waste management. Waste Manag 37:3–12. https://doi.org/10.1016/j.wasman.2014.02.003
Callaway E, Cyranoski D, Mallapaty S, Stoye E, Tollefson J (2020) Coronavirus by the numbers. Nature 579:482
Calma J (2020) https://www.theverge.com/2020/3/26/21194647/the-covid-19-pandemic-is-generating-tons-of-medical-waste
Casanova L, Rutala WA, Weber DJ, Sobsey MD (2009) Survival of surrogate coronaviruses in water. Water Res 43(7):1893–1898
Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Napoli RD (2020) Features, evaluation and treatment Corona Virus (COVID-19), NCBI Bookshelf. StatPearls Publishing, Treasure Island, FL
CDC (2020) https://www.ecdc.europa.eu/sites/default/files/documents/RRA-sixth-updateOutbreak-of-novel-coronavirus-disease-2019-COVID-19.pdf. Accessed 5 July 2020
Chakraborty I, Maity P (2020) COVID-19 outbreak: migration, effects on society, global environment and prevention. Sci Total Environ 728:138882
Chan WC (2020) Nano research for COVID-19. ACS Nano 14(4):3719–3720. https://doi.org/10.1021/acsnano.0c02540
Chartier Y, Emmanuel J, Pieper Ute PA, Philip R, Ruth S, William T, Wilburn S, Zghondi R (2014) Safe management of wastes from health-care activities. WHO, Geneva
Chen K, Wang M, Huang C, Kinney PL, Anastas PT (2020) Air pollution reduction and mortality benefit during the COVID-19 outbreak in China. Lancet Planet Health 4(6):e210–e212
Chin AW, Chu JT, Perera MR, Hui KP, Yen HL, Chan MC, Peiris M, Poon LL (2020) Stability of SARS-CoV-2 in different environmental conditions. Lancet Microbe 1(1):10
Corletta RT, Primack RB, Devictor V, Maasd B, Goswami VR, Bates AE, Koh LP, Regani TJ, Loyolaj R, Pakemanl RJ, Cummingm GS, Pidgeon A, Johns D, Roth R (2020) Impacts of the coronavirus pandemic on biodiversity conservation. Biol Conserv 246:108571
CPCB (2020a) Report on assessment of impact of lock down on water quality of river Yamuna- Delhi stretch. Central Pollution Control Board, Ministry of Environment, Forests and Climate Change, Delhi – 110032
CPCB (2020b) Guidelines for handling, treatment, and disposal of waste generated during treatment/diagnosis/quarantine of COVID-19 patients—Rev. 3, dated 10 June 2020b. Central Pollution Control Board, (Ministry of Environment, Forest & Climate Change), Delhi – 110032, India
CPCB (2020c) Guidelines for handling, treatment and disposal of waste generated during treatment/diagnosis/quarantine of COVID-19 patients—Rev. 4, dated 17 July 2020c. Central Pollution Control Board, (Ministry of Environment, Forest & Climate Change), Delhi – 110032, India
Dantas G, Siciliano B, França BB, da Silva CM, Arbilla G (2020) The impact of COVID-19 partial lockdown on the air quality of the city of Rio de Janeiro, Brazil. Sci Total Environ. https://doi.org/10.1016/j.scitotenv.2020.139085
Dargaville T, Spann K, Celina M (2020) Opinion to address a potential personal protective equipment shortage in the global community during the COVID-19 outbreak. Polymer Degrad Stab 176:109162
Darnell ME, Subbarao K, Feinstone SM, Taylor DR (2004) Inactivation of the coronavirus that induces severe acute respiratory syndrome, SARS-CoV. J Virol Methods 121(1):85–91
Datta P, Mohi GK, Chander J (2018) Biomedical waste management in India: critical appraisal. J Lab Physicians 10(1):6–14
DEFRA-Department for Environment Food & Rural Affairs, Government of UK (2020) UK statistics on waste. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/874265/UK_Statistics_on_Waste_statistical_notice_March_2020_accessible_FINAL_rev_v0.5.pdf
Dhama K, Sharun K, Tiwari R et al (2020) Coronavirus disease 2019—COVID-19. Preprints. https://doi.org/10.20944/preprints202003.0001.v1
Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, Tamin A, Harcourt JL, Thornburg NJ, Gerber SI, Lloyd-Smith JO, Wit E, Munster VJ (2020) Aerosol and surface stability of HCoV-19 (SARS-CoV-2) compared to SARS-CoV-1. N Engl J Med. https://doi.org/10.1101/2020.03.09.20033217
Duan L, Zhu G (2020) Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychol 7(4):300–302
Elavarasan RM, Pugazhendhi R (2020) Restructured society and environment: a review on potential technological strategies to control the COVID-19 pandemic. Sci Total Environ 725:138858
EPCA (2020) The Environment Pollution (Prevention and Control) Authority (EPCA).https://www.epca.org.in/EPCA-Reports1999-1917/EPCA-reportno-112.pdf. Accessed on 17 Dec 2020
Fan VY, Jiang P, Hemzal M, Klemeš JJ (2021) An update of COVID-19 influence on waste management. Sci Total Environ 754:142014
FAO (2020) Food and Agriculture Organization of the United Nations. Local food systems and COVID-19; a glimpse on India's responses. http://www.fao.org/in-action/foodfor-cities-programme/news/detail/en/c/1272232/
Ferronato N, Torretta V (2019) Waste mismanagement in developing countries: a review of global issues. Int J Environ Res Public Health 16(6):1060
Ford T, Vizard T, Sadler K et al (2020) Data resource profile: the mental health of children and young people surveys (MHCYP). Int J Epidemiol. https://doi.org/10.1093/ije/dyz259
Gardiner B (2020) Pollution made COVID-19 worse. Now, lockdowns are clearing the air. National Geographic. https://www.nationalgeographic.com/science/2020/04/pollution-made-the-pandemic-worse-but-lockdowns-clean-the-sky/. Accessed 15 May 2020
Gates B (2020) Responding to Covid-19—a once-in-a-century pandemic? N Engl J Med 382(18):1677–1679
Global Climate report (2019) https://www.ncdc.noaa.gov/sotc/global/201913
Goel S, Hawi S, Goel G, Thakur VK, Agrawal A, Hoskins C, Pearce O, Hussain T, Upadhyaya HM, Cross G, Barber AH (2020) Resilient and agile engineering solutions to address societal challenges such as coronavirus pandemic. Mater Today Chem 17:100300
Holmes EA, O’Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, Ballard C, Christensen H, Silver RC, Everall I, Ford T (2020) Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry 7:547–560. https://doi.org/10.1016/S2215-0366(20)30168-1
Hopman J, Allegranzi B, Mehtar S (2020) Managing COVID-19 in low-and middle-income countries. JAMA 323(16):1549–1550
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet 395(10223):497–506
Istrate I-R, Iribarren D, Galvez-Martos J-L, Dufour J (2020) Review of life-cycle environmental consequences of waste-to-energy solutions on the municipal solid waste management system. Resour Conser Recov 157:104778. https://doi.org/10.1016/j.resconrec.2020.104778
Kahlert S, Bening CR (2020) Plastic recycling after the global pandemic: resurgence or regression? Resour Conserv Recycl 160:104948. https://doi.org/10.1016/j.resconrec.2020.104948
Kampf G, Todt D, Pfaender S, Steinmann E (2020) Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect 104:246–251. https://doi.org/10.1016/j.jhin.2020.01.022
Katariya M (2020) 10 Things that have happened for the first time in years during the coronavirus lockdown. Scoopwhoop, https://www.scoopwhoop.com/news/things-that-have-happened-for-the-first-time-inyearsduring-coronavirus-lockdown/
Kaufman L, Chasan E (2020) Cities wonder whether recycling counts as essential during the virus. Bloomberg Green. https://www.bloomberg.com/news/articles/2020-03-27/cities-wonder-whether-recycling-counts-as-essential-during-the-virus. Accessed 26 April 2020
Kerimray A, Baimatova N, Ibragimova OP, Bukenov B, Kenessov B, Plotitsyn P, Karaca F (2020) Assessing air quality changes in large cities during COVID-19 lockdowns: the impacts of traffic-free urban conditions in Almaty, Kazakhstan. Sci Total Environ 730:139179. https://doi.org/10.1016/j.scitotenv.2020.139179
Klemeš JJ, Van Fan Y, Tan RR, Jiang P (2020) Minimising the present and future plastic waste, energy and environmental footprints related to COVID-19. Renew Sustain Energy Rev 127:109883
Kulkarni BN, Anantharama V (2020) Repercussions of COVID-19 pandemic on municipal solid waste management: challenges and opportunities. Sci Total Environ 743:140693
Kyriakis E, Psomopoulos C, Kalkanis K (2019) Investigating the correlation of purchase power parity with the adopted waste management method in EU28. J Soc Sci 8:162. https://doi.org/10.3390/socsci8050162
Lee PI, Hu YL, Chen PY, Huang YC, Hsueh PR (2020) Are children less susceptible to COVID-19? J Microbiol Immunol Infect. https://doi.org/10.1016/j.jmii.2020.02.011
Liu HC, You JX, Lu C, Chen YZ (2015) Evaluating health-care waste treatment technologies using a hybrid multi-criteria decision making model. Renew Sustain Energy Rev 41:932–942
Lokhandwala S, Gautam P (2020) Indirect impact of COVID-19 on environment: a brief study in Indian context. Environ Res 188:109807
Mahajan P, Kaushal J (2020) Epidemic trend of COVID-19 transmission in India during lockdown-1 phase. J Commun Health. https://doi.org/10.1007/s10900-020-00863-3
Mahato S, Pal S, Ghosh KG (2020) Effect of lockdown amid COVID-19 pandemic on air quality of the megacity Delhi, India. Sci Total Environ 730:139086. https://doi.org/10.1016/j.scitotenv.2020.139086
Mallapur C (2020) Sanitation workers at risk from discarded medical waste related to COVID-19. IndiaSpend. https://www.indiaspend.com/sanitation-workersat-risk-from-discarded-medical-waste-related-tocovid-19/
Mayer F, Bhandari R, Gath S (2019) Critical review on life cycle assessment of conventional and innovative waste-to-energy technologies. Sci Total Environ 672:708–721. https://doi.org/10.1016/j.scitotenv.2019.03.449
Ministry of Health and Family Welfares (MoHFW), Government of India (2020) COVID-19 INDIA. https://www.mohfw.gov.in/
Mishra RK, Parida M, Rangnekar S (2010) Evaluation and analysis of traffic noise along bus rapid transit system corridor. Int J Environ Sci Technol 7(4):737–750. https://doi.org/10.1007/BF03326183
Mollica GJG, Balestieri JAP (2020) Is it worth generating energy with garbage? Defining a carbon tax to encourage waste-to-energy cycles. Appl Therm Eng 173:115195. https://doi.org/10.1016/j.applthermaleng.2020.115195
Myllavirta L, Dahiya S (2020) Analysis: India's CO2 emissions fall for first time in four decades amid coronavirus. Carbon Brief, https://www.carbonbrief.org/analysis-indias-co2-emissions-fall-for-first-time-in-four-decades-amidcoronavirus#
National Aeronautics and Space Administration (NASA) (2020) Airborne particle levels plummet in Northern India. Retrieved on 11 May 2020 from https://earthobservatory.nasa.gov/images/146596/airborne-particle-levels-plummet-innorthern-india
National Environment Agency Singapore (2020)Waste management-public waste collection services during circuit breaker. https://www.nea.gov.sg/our-services/wastemanagement/overview.
Nghiem LD, Morgan B, Donner E, Short MD (2020) The COVID-19 pandemic: considerations for the waste and wastewater services sector. Case Stud Chem Environ Eng. https://doi.org/10.1016/j.cscee.2020.100006
Occupational Safety and Health Administration (OSHA) (2020) Guidance on Preparing Workplaces for COVID-19
Paital B, Das K, Parida SK (2020) Review-Inter nation social lockdown versus medical care against COVID-19, a mild environmental insight with special reference to India. Sci Total Environ 728:138914
Peng L, Liu J, Xu W, Luo Q, Chen D, Lei Z, Huang Z, Li X, Deng K, Lin B, Gao Z (2020) SARS-CoV-2 can be detected in urine, blood, anal swabs, and oropharyngeal swabs specimens. J Med Virol. https://doi.org/10.1002/jmv.25936
Polk HS (2019) State of global air 2019: a special report on global exposure to air pollution and its disease burden. Health Effects Institute, Boston, MA
Pujara Y, Pathak P, Sharma A, Govani J (2019) Review on Indian Municipal Solid Waste Management practices for reduction of environmental impacts to achieve sustainable development goals. J Environ Manage 248:109238
Qu G, Li X, Hu L, Jiang G (2020) An imperative need for research on the role of environmental factors in transmission of novel coronavirus (COVID-19). Environ Sci Technol 54:3730–3732
Rahman MM, Bodrud-Doza M, Griffiths MD, Mamun MA (2020) Biomedical waste amid COVID-19: perspectives from Bangladesh. Lancet Glob Health 8(10):e1262
Rajor A, Xaxa M, Mehta R (2012) An overview on characterization, utilization and leachate analysis of biomedical waste incinerator ash. J Environ Manage 108:36–41
Ramachandra TV, Bharath HA, Kulkarni G, Han SS (2018) Municipal solid waste: generation, composition and GHG emissions in Bangalore, India. Renew Sustain Energy Rev 82:1122–1136. https://doi.org/10.1016/j.rser.2017.09.085
Randall I (2020) Sound of the sea: underwater noise pollution from ships plummets during the coronavirus lockdown offering respite for 'stressed' whales and other marine life. The Daily Mail. https://mol.im/a/8262147
Rodriguez-Morales A, Tiwari R, Sah R, Dhama K (2020) COVID-19, an emerging coronavirus infection: current scenario and recent developments—an overview. J Pure Appl Microbiol 14:6150
Rosenbloom D, Markard J (2020) A COVID-19 recovery for climate. Science 368(6490):447. https://doi.org/10.1126/science.abc4887
Roujian L, Xian Z, Juan L et al (2020) Genomic characterization and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet 395:565–574
Shammi M, Bodrud-Doza M, Islam ARMT, Rahman MM (2020) COVID-19 pandemic, socioeconomic crisis and human stress in resource-limited settings: a case from Bangladesh. Heliyon 6:e04063
Sharma HB, Vanapalli KR, Cheela VS, Ranjan VP, Jaglan AK, Dubey B, Goel S, Bhattacharya J (2020) Challenges, opportunities, and innovations for effective solid waste management during and post COVID-19 pandemic. Resour Conser Recycl 162:105052
Singh RP, Tyagi VV, Allen T, Ibrahim M, Kothari R (2011) An overview of exploring the possibilities of energy generation from municipal solid waste (MSW) in Indian scenario. Renew Sustain Energy Rev 15:4797–4808. https://doi.org/10.1016/j.rser.2011.07.071
Singh AK, Singh A, Shaikh A, Singh R, Misra A (2020) Chloroquine and hydroxychloroquine in the treatment of COVID-19 with or without diabetes: a systematic search and a narrative review with a special reference to India and other developing countries. Diab Metab Syndr Clin Res Rev 14:241–246
Sinha SN, Paul D, Biswas K (2016) Effects of Moringaoleifera Lam. and Azadirachtaindica A. Juss. leaf extract in treatment of tannery effluent. Our Nat 14:47–53
Sohrabi C, Alsafi Z, O’Neill N, Khan M, Kerwan A, Al-Jabir A, Iosifidis C, Agha R (2020) Review- World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19). Int J Surg 76:71–76
Somani M, Srivastava AN, Gummadivalli SK, Sharma A (2020) Indirect implications of COVID-19 towards sustainable environment: an investigation in Indian context. Bioresour Technol Rep 11:100491
Soni DK (2020) Regulatory interventions in Covid-19 waste management in India. Natl J Life Sci 17(1):5–7
SWANA - Solid Waste Association of North America article (2020) SWANA reminds all state and local governments that solid waste management is an essential public service. https://swana.org/news/swana-news/article/2020/03/19/swana-reminds-allstate-and-localgovernments-that-solid-waste-management-is-an-essential-publicservice
Tang W (2020) The medical waste related to COVID-2019 is cleaned up every day—the medical waste treatment market needs to be standardised. 21st Century Business Herald; 2020. www.21jingji.com/2020/3-12/xNMDEzODFfMTU0MjIxNQ.html
Times of India (TOI) (2020) 350 Tonnes of trash disappear from streets of Ahmedabad. http://timesofindia.indiatimes.com/articleshow/75039037.cms?utm_source=contentofinterest&utm_medium=text&utm_campaign=cppst
UNEP (2020) BASEL: waste management an essential public service in the fight to beat COVID-19. The United Nations Environment Programme (UNEP) and The Basel Convention. http://www.basel.int/Implementation/PublicAwareness/PressReleases/WastemanagementandCOVID19/tabid/8376/Default.aspx
United Nations Industrial Development Organization (UNIDO) (2020) India's manufacturing reels from the impact of COVID-19. https://www.unido.org/stories/indias-manufacturingreelsimpact-covid-19
United Nations (2020) The Social Impact of COVID-19. Department of Economics and Social Affairs. https://www.un.org/development/desa/dspd/2020/04/social-impact-ofcovid-19
United States Environmental Protection Agency (2020) Recycling and sustainable management of food during COVID-19 public health emergency. https://www.epa.gov/coronavirus/recycling-and-sustainable-management-food-duringcoronaviruscovid-19-public-health
United States Environmental Protection Agency (2017) National overview: facts and figures on materials, wastes and recycling. https://www.epa.gov/facts-and-figuresabout-materials-waste-and-recycling/national-overview-facts-and-figures-materials. Accessed 10 May 2020.
Vellingiri B, Jayaramayya K, Iyer M, Narayanasamy A, Govindasamy V, Giridharan B, Ganesan S, Venugopal A, Venkatesan D, Ganesan H, Rajagopalan K (2020) COVID-19: a promising cure for the global panic. Sci Total Environ 725:138277
Weber DJ, Rutala WA, Fischer WA, Kanamori H, Sickbert-Bennett EE (2016) Emerging infectious diseases: focus on infection control issues for novel coronaviruses (Severe Acute Respiratory Syndrome-CoV and Middle East Respiratory Syndrome-CoV), hemorrhagic fever viruses (Lassa and Ebola), and highly pathogenic avian influenza viruses, A(H5N1) and A(H7N9). Am J Infect Control 44(5):E91–E100
WHO (2017) Report on health-care waste management (HCWM) status in Countries of the South-East Asia Region (SEA-EH-593). The World Health Organization. https://apps.who.int/iris/handle/10665/258761.
WHO (2018) World Health Organization. Global status report on alcohol and health. https://www.who.int/substance_abuse/publications/global_alcohol_report/en/.
WHO, 2020a. Pneumonia of unknown cause- China. World Health Organization.
WHO (2020b) Coronavirus Disease (COVID-2019) Situation Reports-67. World Health Organization
WHO (2020c) World Health Organization. WHO-Director-general-s-opening-remarks-at-the-media briefing-on-covid-19. www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19
WHO (2020d) Water, sanitation, hygiene, and Waste Management For the COVID-19 virus: interim guidance, 23 April 2020d (No. WHO/2019-nCoV/IPC_WASH/2020.3).WorldHealth Organization URL. https://apps.who.int/iris/bitstream/handle/10665/331846/WHO-2019-nCoV-IPC_WASH-2020.3-eng.pdf. Accessed 30 April 2020.
Windfeld ES, Brooks MS-L (2015) Medical waste management—a review. J Environ Manag 163:98–108
Wölfel R, Corman VM, Guggemos W, Seilmaier M, Zange S, Müller MA, Niemeyer D, Jones TC, Vollmar P, Rothe C, Hoelscher M (2020) Virological assessment of hospitalized patients with COVID-2019. Nature 581(7809):465–469
World Bank Urban Development Series (2018) Decision Maker’s Guides for Solid Waste Management Technologies.
World Bank (2020) Waste workers are protecting our communities during COVID-19. https://blogs.worldbank.org/sustainablecities/waste-workers-are-protecting-ourcommunitiesduring-covid-19. Accessed 11 May 2020.
Xia J, Tong J, Liu M, Shen Y, Guo D (2020) Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection. J Med Virol 92(6):589–594
Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, Liu S, Zhao P, Liu H, Zhu L (2020) Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Resp Med 8(4):420–422
Yadav P, Samadder SR (2018) A critical review of the life cycle assessment studies on solid waste management in Asian countries. J Clean Prod 185:492–515. https://doi.org/10.1016/j.jclepro.2018.02.298
Yunus AP, Masago Y, Hijioka Y (2020) COVID-19 and surface water quality: improved lake water quality during the lockdown. Sci Total Environ 731:139012. https://doi.org/10.1016/j.scitotenv.2020.139012
Zambrano-Monserrate MA, Ruano MA, Sanchez-Alcalde L (2020) Indirect effects of COVID-19 on the environment. Sci Total Environ 728:138813. https://doi.org/10.1016/j.scitotenv.2020.138813
Zhang W, Du RH, Li B, Zheng XS, Yang XL, Hu B, Wang YY, Xiao GF, Yan B, Shi ZL, Zhou P (2020) Molecular and serological investigation of 2019-nCoV infected patients: implication of multiple shedding routes. Emerg Microbes Infect 9(1):386–389
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P (2020) A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 382:727–733
Acknowledgements
The authors wish to thank all who assisted in conducting this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they do not have any personal or financial conflict of interests.
Additional information
Editorial responsibility: Samareh Mirkia.
Rights and permissions
About this article
Cite this article
Kanwar, V.S., Sharma, A., Rinku et al. An overview for biomedical waste management during pandemic like COVID-19. Int. J. Environ. Sci. Technol. 20, 8025–8040 (2023). https://doi.org/10.1007/s13762-022-04287-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13762-022-04287-5