Abstract
Dysregulation in total body copper causes severe complications and excess copper can be toxic. Divalent metal transporter 1, duodenal cytochrome B, and copper transporter ATPase7A are included in the many intestinal genes transactivated by HlF-α. On July X, 2022 an 80-year-old female patient on peritoneal dialysis was prescribed roxadustat 100 mg, because darbepoetin was unable to increase hemoglobin level effectively. On the same day, icodextrin 1 L was initiated to mitigate edema. Laboratory data showed hemoglobin 9.1 g/dL, transferrin saturation 77%, copper 123 μg/dL, and iron 170 μg/dL before changing to roxadustat. The patient visited us 6 days after the change because of the appetite loss. Transferrin saturation and serum copper and iron levels increased to 90%, 170 and 203 μg/dL, respectively, which were decreased or normalized after discontinuing roxadustat and icodextrin, suggesting that even short-term roxadustat administration can influence copper levels as well as iron levels. Excess copper and iron levels during roxadustat treatment do not immediately equate with toxicity, but indicate a physiological compensation or transient imbalance of metabolism especially in patients treated with ferric citrate. Further investigation for the hypoxia-inducible factor-prolyl hydroxylase inhibitors effects on iron and copper metabolisms is needed. Determining the short-term effect of roxadustat on serum copper and iron in only this case is impossible. Therefore, further accumulation of similar cases is necessary to clarify the short-term effects of roxadustat on serum copper and iron.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Copper is an indispensable trace metal element and total body copper is essentially dependent on the balance between intestinal absorption, cell uptake, and bile excretion [1]. Plasma total copper levels have been reported as increased in patients with Alzheimer's disease, although causative association is still controversial [2]. Deteriorated immune function, diabetes, coronary heart disease, and osteoporosis are associated with chronic copper excess which may be harmful to our health [3]. Hypoxia-inducible factor (HIF)-prolyl hydroxylase inhibitors (HIF-PHIs) have emerged as a novel approach for renal anemia management. Several clinical studies have demonstrated that HIF-PHIs effectively corrected and maintained target hemoglobin (Hb) levels in peritoneal dialysis (PD) patients [4, 5]. Real-world study on hemodialysis patients treated with roxadustat demonstrated the effectiveness in increasing hemoglobin levels [6]. Divalent metal transporter 1 (DMT1), duodenal cytochrome B (DCYTB), and copper transporter ATPase copper transporting alpha (ATP7A) related to iron absorption are included in the many intestinal genes transactivated by HlF-α. Iron and copper have similar physiochemical properties and points of interaction [7], and some studies have shown that DMT1 can transport copper [8]. Recently, possible relationship between copper excess and HIF-PHI treatments was reported [9]. In this study, we report a PD case that showed increased serum levels in both copper and iron after initiating roxadustat, which were decreased or normalized after discontinuing roxadustat, suggesting that even short-term roxadustat administration can influence serum copper as well as iron levels.
Case report
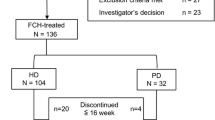
An 80-year-old female patient on continuous ambulatory PD for 2 years treated with a total of 4 L of 1.5 and 2.5% glucose-based solution. The patient had an aortic valve replacement history and reduced ejection fraction. The dialysate-to-creatinine ratio measured on May 2022 was 0.80. On July X, 2022, roxadustat 100 mg, before sleep, three times a week was prescribed, because 60 μg/month of darbepoetin alfa was unable to maintain the target Hb level. On the same day, icodextrin 1L was initiated to mitigate lower extremity edema. Her body weight was 40 kg and urine volume was 300 ml per day. Hyperphosphatemia has also been treated with ferric citrate 750 mg for more than 6 months. Laboratory data showed Hb 9.1 g/dL, albumin 2.7 g/dL, ferritin 629 ng/mL, transferrin saturation (TSAT) 77%, copper 123 μg/dL (normal range 66–130 μg/dL), and iron 170 μg/dL (normal range 40–188 μg/dL) shown in Table 1. She visited us because of appetite loss and chest discomfort 6 days after the change and Hb level increased to 10.0 g/gL. The TSAT and serum copper and iron levels increased to 90%, 170 μg/dL, and 203 μg/dL, respectively, on July X + 7, 2022. Therefore, she needed to be hospitalized to reconsider anemia and chronic heart failure management. After roxadustat, ferric citrate, and icodextrin discontinuation, her appetite gradually improved after initiation of polaprezinc 150 mg, a zinc-containing compound. The TSAT as well as copper and iron levels decreased to 34%, 123 μg/dL, and 69 μg/dL, respectively, on July X + 14, 2022 (Fig. 1). The copper concentration in the efferent solution after the overnight dwell showed 3.4 μg/dL on July X + 7, 2022. Quick Auto Neo Cu (SHINO-TEST Co., Sagamihara, Japan) was used to measure serum and efferent solution copper concentration described in detail in the previous paper [9].
Discussion
HIF-PHIs intervention effects on iron metabolism showed that ferritin, TSAT, and hepcidin decreased, and the total iron-binding capacity increased over a 24-week period according to several PD studies [5, 10]. However, the short-term serum changes in both iron and copper during HIF-PHI treatment are not well known. In the present case, the increase in ferritin, TSAT, copper, iron, and ceruloplasmin over 7 days after roxadustat initiation were noted. All these values decreased over 7 days after roxadustat and ferric citrate withdrawal, suggesting that even short-term treatment, two roxadustat oral administrations influence both iron and copper metabolism.
A short-term study [11] that investigates iron metabolism on hemodialysis demonstrated that roxadustat increased serum iron levels and TSAT 2 days after administration, which support our results seen on day X + 7. Then, serum iron and TSAT decreased on day 7.
In this case, the TSAT and ferritin level were already increased before initiating roxadustat, likely, due to ferric citrate treatment for more than 6 months and chronic heart failure exacerbation, and then, both values increased up to 90% and 1430 ng/mL, respectively, after initiating roxadustat. Although the patient had a tendency to overload iron, we speculated that roxadustat induced the imbalance between iron absorption and its use, which ended up in an increase in these iron-related parameters.
Hepcidin plays a pivotal role in the pathogenesis of inflammation-induced anemia. In contrast, hepcidin production increases in response to iron loading. Serum hepcidin levels are increased by inflammatory cytokines in hepatocytes. Erythropoietic action induction during ineffective erythropoiesis generates a preferential signal that results in hepcidin transcription suppression, even in the presence of excessive systemic iron [12]. Considering the data transition in this present case, the Hb level increased after roxadustat initiation, while iron and ferritin increased over 7 days, suggesting that hepcidin was decreased by roxadustat administration and iron absorption was induced at the intestine even in the short term. It is unclear whether the high serum iron levels will start to decrease by adjusting and improving iron metabolism if administration of roxadustat is continued.
The phase 2 study in Japan on patients undergoing hemodialysis reported that the treatment arm with roxadustat had the adverse events of nausea (5.2%) and vomiting (7.2%). In contrast, neither nausea nor vomiting was reported in the control arm with darbepoetin alpha. Increased iron and ferritin, in addition to appetite loss and rapid increase in hemoglobin (0.9 g/dL per 6 days), were reasons to discontinue roxadustat.
Ceruloplasmin is the main copper transport protein in the plasma and a known HIF-1 target. Both hypoxia and CuCl2 increased ceruloplasmin mRNA levels in hepatoma cells [13]. Ceruloplasmin is also a multicopper plasma protein containing ferroxidase activity necessary for converting Fe (II) to Fe (III) [14]. Close association between the change in ceruloplasmin level and roxadustat treatment was noted in this case. The aforementioned experimental results support our idea that roxadustat can increase serum copper and iron levels by raising the ceruloplasmin level.
A meta-analysis identified a significant association between high serum copper and heart failure (HF), and the authors speculated that the association between HF and high ceruloplasmin concentrations was caused by high serum copper levels [15]. In the present case, the short-term changes in serum copper and ceruloplasmin may be related to HF worsening or recovery in addition to roxadustat treatment.
The patient had spent her life at a public nursing home where she was provided every meal. Considering her meal management environment, the patient had less chance to have copper-rich food from July X to July X + 7.
This study has some limitations. Several clinical conditions, including renal failure [16] and anemia of inflammation [17], are known for reasons to increase serum copper due to elevated serum ceruloplasmin. Renal failure cannot be excluded and anemia of inflammation might be associated with copper excess.
Theoretically, PD could lead to greater depletion of elements than hemodialysis, because most elements are protein-bound, and significant peritoneal protein loss can occur [18]. It is unclear up to what extent serum copper level can be influenced by the amount of copper into efferent solution.
In conclusions, excess copper and iron levels during HIF-PHI treatment do not mean immediately toxicity, but indicate a physiological compensation or transient imbalance of copper and iron metabolism, especially in patients treated with ferric citrate. Determining the short-term effect of roxadustat on serum copper and iron in only this case is impossible. Therefore, further accumulation of similar cases is necessary to clarify the short-term effects of roxadustat on serum copper and iron.
References
Ferns GA, Lamb DJ, Taylor A. The possible role of copper ions in atherogenesis: the Blue Janus. Atherosclerosis. 1997;133:139–52. https://doi.org/10.1016/s0021-9150(97)00130-5.
Arnal N, Cristalli DO, de Alaniz MJ, Marra CA. Clinical utility of copper, ceruloplasmin, and metallothionein plasma determinations in human neurodegenerative patients and their first-degree relatives. Brain Res. 2010;1319:118–30. https://doi.org/10.1016/j.brainres.2009.11.085.
Harris ED. Basic and clinical aspects of copper. Crit Rev Clin Lab Sci. 2003;40:547–86.
Hou YP, Mao XY, Wang C, Xu ZH, Bu ZH, Xu M, Li B. Roxadustat treatment for anemia in peritoneal dialysis patients: a randomized controlled trial. J Formos Med Assoc. 2022;121:529–38. https://doi.org/10.1016/j.jfma.2021.06.004.
Akizawa T, Otsuka T, Reusch M, Ueno M. Intermittent oral dosing of roxadustat in peritoneal dialysis chronic kidney disease patients with anemia: a randomized, phase 3, multicenter, open-label study. Ther Apher Dial. 2020;24:115–25. https://doi.org/10.1111/1744-9987.12888.
Mima A, Horii Y. Treatment of Renal Anemia in Patients With Hemodialysis Using Hypoxia-inducible Factor (HIF) Stabilizer, Roxadustat: A Short-term Clinical Study. In Vivo. 2022;36:1785–9. https://doi.org/10.21873/invivo.12892.
Doguer C, Ha JH, Collins JF. Intersection of iron and copper metabolism in the mammalian intestine and liver. Compr Physiol. 2018;8:1433–61.
Wang X, Flores SR, Ha JH, Doguer C, Woloshun RR, Xiang P, Grosche A, Vidyasagar S, Collins JF. Intestinal DMT1 is essential for optimal assimilation of dietary copper in male and female mice with iron-deficiency anemia. J Nutr. 2018;148:1244–52.
Nakamura H, Kurihara S, Anayama M, Makino Y, Nagasawa M. Four cases of serum copper excess in patients with renal anemia receiving a hypoxia-inducible factor-prolyl hydroxylase inhibitor: a possible safety concern. Case Rep Nephrol Dial. 2022;12:124–31.
Nangaku M, Kondo K, Takabe S, Ueta K, Kaneko G, Otsuka M, Kawaguchi Y, Komatsu Y. Vadadustat for anemia in chronic kidney disease patients on peritoneal dialysis: A phase 3 open-label study in Japan. Ther Apher Dial. 2021;25:642–53. https://doi.org/10.1111/1744-9987.13611.
Ogawa C, Tsuchiya K, Tomosugi N, Maeda K. A hypoxia-inducible factor stabilizer improves hematopoiesis and iron metabolism early after administration to treat anemia in hemodialysis patients. Int J Mol Sci. 2020;28(21):7153. https://doi.org/10.3390/ijms21197153.
Mima A. Hypoxia-inducible factor-prolyl hydroxylase inhibitors for renal anemia in chronic kidney disease: Advantages and disadvantages. Eur J Pharmacol. 2021;912:174583. https://doi.org/10.1016/j.ejphar.2021.174583.
Martin F, Linden T, Katschinski DM, Oehme F, Flamme I, Mukhopadhyay CK, Eckhardt K, Tröger J, Barth S, Camenisch G, Wenger RH. Copper-dependent activation of hypoxia-inducible factor (HIF)-1: implications for ceruloplasmin regulation. Blood. 2005;105:4613–9. https://doi.org/10.1182/blood-2004-10-3980.
Osaki S, Johnson DA, Frieden E. The possible significance of the ferrous oxidase activity of ceruloplasmin in normal human serum. J Biol Chem. 1966;25(241):2746–51.
Huang L, Shen R, Huang L, Yu J, Rong H. Association between serum copper and heart failure: a meta-analysis. Asia Pac J Clin Nutr. 2019;28:761–9. https://doi.org/10.6133/apjcn.201912_28(4).0013.
Taylor JE, Belch JJ, Fleming LW, Mactier RA, Henderson IS, Stewart WK. Erythropoietin response and route of administration. Clin Nephrol. 1994;41:297–302.
Beaumier DL, Caldwell MA, Holbein BE. Inflammation triggers hypoferremia and de novo synthesis of serum transferrin and ceruloplasmin in mice. Infect Immun. 1984;46:489–94. https://doi.org/10.1128/iai.46.2.489-494.1984.
Thomson NM, Stevens BJ, Humphery TJ, Atkins RC. Comparison of trace elements in peritoneal dialysis, hemodialysis, and uremia. Kidney Int. 1983;23:9–14. https://doi.org/10.1038/ki.1983.3.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Nakamura has received the lecture fee from Astellas, Bayer Yakuhin, and Kyowa Kirin Co., Ltd.
Human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Patient consent confirmation statement
Consent to publish statement: Written informed consent was obtained from the patient for publication of this case report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Nakamura, H., Ueda, M., Anayama, M. et al. Short-term effects of roxadustat on serum copper and iron changes in a peritoneal dialysis patient. CEN Case Rep 12, 292–296 (2023). https://doi.org/10.1007/s13730-022-00765-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13730-022-00765-4