Abstract
Nonfunctional parathyroid carcinoma is a very rare malignant disease; only 25 cases have been reported over the last 85 years. We present a patient with a nonfunctional parathyroid carcinoma metastasis to the breast and a review of the pertinent literature. A 71-year-old woman was seen for a self-discovered mass in her left breast. She had undergone surgery 6 years previously for nonfunctional parathyroid cancer. Mammography and ultrasonography of the breast revealed an oval, circumscribed mass. Fine-needle aspiration findings were suspicious for metastasis of parathyroid carcinoma. Serum calcium and intact parathyroid hormone levels were within normal limits. We performed a partial mammary gland resection that included the tumor. Pathological analysis of the resected tumor disclosed findings consistent with parathyroid carcinoma. The nonsecretory state of the tumor was supported by negative immunoreactivity for parathyroid hormone in the tissue and lack of clinical evidence of hyperparathyroidism. To the best of our knowledge, this is the first reported case of parathyroid carcinoma metastasis to the breast. Breast metastasis of parathyroid carcinoma should be included in the differential diagnosis for a patient with a past history of parathyroid carcinoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parathyroid carcinoma accounts for 6% of patients with primary hyperparathyroidism in Japan [1]. The management of parathyroid carcinoma is primarily surgical, with en bloc resection of the tumor and involved adjacent structures. Cervical recurrences and lung metastases are most commonly encountered, and metastases to bone, liver, or pancreas have also been reported [2–6]. The overall 5- and 10-year survival rates have been reported as 85 and 49–77%, respectively [7, 8]. Most deaths are related to hypercalcemia.
While functional parathyroid carcinoma is an uncommon tumor, nonfunctional parathyroid carcinoma is exceedingly rare, with 25 reported cases in the world literature [9–12]. The presence of a neck mass is the common presenting symptom for nonfunctional parathyroid carcinoma, because the carcinoma is usually detected at an advanced stage because of the lack of hypercalcemia-associated symptoms. Operative resection is the only effective treatment modality, but more extensive surgery is often necessary, because of the higher frequency of local invasion or metastasis at diagnosis than seen for functional parathyroid carcinomas [12]. Presentation in the late stages and ineffective adjuvant therapies result in dismal outcomes. Patients dying from the disease eventually succumb to systemic tumor burden.
Previously, Nakamura et al. [10] reported this patient as a case of nonfunctional parathyroid carcinoma. In the present report, we describe a metastasis to her breast that was discovered 6 years after the initial surgery. To our knowledge, this is the first report in the world literature of parathyroid cancer that metastasized to the breast.
Case report
A 71-year-old woman presented with a mass in her left breast that she discovered herself. She had undergone initial surgery at our hospital in December 2004 performed by an otolaryngologist for a nonfunctional parathyroid cancer [10]. The surgical procedure consisted of resection of the tumor plus the left lobe of the thyroid gland, and lymph node dissections of the left neck and superior mediastinum. Histopathological examination of the primary tumor revealed dense fibrous band separating lobules of tumor cells, mitotic figures, necrosis, capsular invasion, and invasion of thyroid tissue (Fig. 1a, b). Immunoperoxidase staining of the primary tumor for carcinoembryonic antigen (CEA), thyroglobulin, S-100 protein, epithelial membrane antigen (EMA), calcitonin, carbohydrate antigen 19-9 (CA19-9), and parathyroid hormone (PTH) was negative, but strongly reactive for neuron-specific enolase (NSE) and chromogranin A (Fig. 1c). The Ki-67 labeling index of the primary tumor was 7.9% (Fig. 1d). Because there were 12 lymph nodes positive for metastases, postoperative radiotherapy (RT) (50 Gy in 25 treatments) was performed. The patient was then followed as an outpatient. Four years after her initial treatment, she had a recurrence in a superior mediastinal lymph node and underwent surgery consisting of resection of the superior mediastinal lymph node and dissection of the left supraclavicular lymph nodes. Six years after her initial surgery, she suddenly developed left hypoglossal nerve palsy caused by metastasis to the occipital bone around the left hypoglossal canal. She was to undergo RT of the affected area. Six years and 1 month after her initial surgery, she noticed the left breast mass and was referred to us.
Histological sections of the primary parathyroid carcinoma. a Fibrous bands and focal tumor cells stained with hematoxylin and eosin (H&E) (×40). b Tumor cells invading the thyroid (H&E stain ×40). c Tumor cell cytoplasm is clearly stained with chromogranin A (×100). d Ki-67 reactivity of primary tumor (×100)
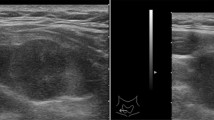
Physical examination revealed a 1.5-cm firm, circumscribed mass in the superior lateral region 3 cm from the nipple in the left breast. On mammography, mediolateral oblique and craniocaudal views revealed an oval, circumscribed mass of higher density than fibroglandular breast tissue (Fig. 2). Ultrasonography revealed an oval, circumscribed, homogenous hypoechoic mass with extreme posterior acoustic enhancement. Fine-needle aspiration of the mass was performed under ultrasonographic guidance. The diagnosis was malignant, with presumption of a metastasis of parathyroid carcinoma. Laboratory findings included: serum calcium 8.7 mg/dl (normal range, 8.7–10.3 mg/dl), intact parathyroid hormone (PTH-intact) 41 pg/ml (normal range, 10–65 pg/ml), thyroid-stimulating hormone 5.6 μU/ml (normal range, 0.27–4.2 μU/ml), and thyroxine 1.5 ng/dl (normal ranges, 1.0–1.8 ng/dl).
A partial resection of the mammary gland including the tumor with a 0.5-cm safety margin was performed under local anesthesia. Grossly, the sectioned specimen revealed a grayish-white, oval tumor measuring 1.1 cm in diameter, and the cut tumor surface displayed opalescence (Fig. 3). Histological examination of the tumor revealed tumor cells forming atypical solid nests with round to oval nuclei, granular chromatin with occasional small nucleoli, and scant cytoplasm (Fig. 4a, b). Immunohistochemical staining was negative for CEA, thyroglobulin, S-100 protein, EMA, calcitonin, CA19-9, E-cadherin, cytokeratin 34βE12 estrogen receptor, progesterone receptor, HER2, and parathyroid hormone (Fig. 4c); and was positive for NSE, synaptophysin (Fig. 5a), chromogranin A (Fig. 5b), and cytokeratin AE1/AE3. Ki-67 of the metastasis showed 10.2% positivity (Fig. 5c). Based on the light microscopy findings and the immunohistochemical staining profile, the breast tumor was diagnosed as a metastasis of parathyroid carcinoma.
Histological appearance of breast metastasis of nonfunctional parathyroid carcinoma: a Sheets or lobules of tumor cells are shown [hematoxylin and eosin (H&E) stain ×100]; b tumor cells showing atypical solid nests with round to oval nuclei, granular chromatin with occasional small nucleoli, and scant cytoplasm (H&E stain ×400); c the cytoplasm of tumor cells is negative for parathyroid hormone
The postoperative serum calcium was 8.8 mg/dl. The patient is now undergoing RT for metastasis to occipital bone around the left hypoglossal canal. She also continues to be followed in our hospital.
Discussion
Patients with nonfunctional parathyroid carcinomas are usually asymptomatic with normal calcium and PTH levels. Therefore, they are difficult to diagnose clinically, and most patients are diagnosed at an advanced stage of the disease with the initial symptoms being associated with the large size and invasiveness of these tumors. Our patient discovered the mass in her breast. This indicates that in cases with a past history of nonfunctional parathyroid carcinoma, regular self examination to detect metastases to external organs such as the breast is important. In addition, technetium-99m sestamibi and computed tomography (CT) scans and magnetic resonance imaging may be useful for detecting metastases to internal organs. Technetium-99m sestamibi imaging can locate endocrinologically inactive metastases [11]. Busaidy et al. presented a comparative summary of a few published institutional experiences covering 109 patients with parathyroid carcinoma from 1938 to 2002. Distant metastases to lungs, bones, liver, and brain were reported [13]. Distant metastasis from functioning parathyroid carcinomas is reported to occur with a frequency of 25%, mainly to the lungs. The cases of distant metastasis from nonfunctional parathyroid carcinomas are listed in Table 1 [9–12]. Metastasis occurred in 48% (12/25) of cases, and included the lungs (8/25, 32%), bone (4/25, 16%), liver (1/25, 4%), and skin (1/25, 4%) (Table 1). It appears that metastases from nonfunctional parathyroid carcinomas occur more frequently than metastases from functional parathyroid carcinomas.
We think that this breast tumor is one of the metastatic lesions. However, metastases to the breast from extramammary carcinomas are rare [14]. The frequency of nonprimary tumors of the breast has been reported to range from 0.5 to 1.3% of all breast malignancies [15]. The reason for the rare occurrence of metastases in the breast is not known. It may reflect the decreased blood flow to the breast in older patients. The most common metastatic lesions in the breast are widely disseminated malignant melanomas in advanced disease [14]. Other frequent sources of breast metastases are lung, prostate, ovarian, and stomach cancers [14]. A parathyroid carcinoma metastatic to the mammary gland has never been reported.
The characteristic mammographic and ultrasonographic findings of breast metastasis from parathyroid carcinomas have not been previously reported, although these imaging modalities are widely used to detect breast cancers. The breast mass of our patient appeared as a circumscribed mass on mammography and ultrasonography. The abundance of homogenous tumor cells resulted in homogenous hypoechoic tumor with extreme posterior acoustic enhancement. These findings suggest that metastasis of parathyroid carcinoma should be included in the differential diagnosis when a hypoechoic and homogenous tumor with enhanced posterior echo is seen in the breast of a patient with a past history of parathyroid carcinoma.
The differential diagnosis includes primary breast neuroendocrine carcinoma. Specific finding of primary breast neuroendocrine carcinoma, compared with metastatic breast neuroendocrine carcinoma, has not been reported. However, the primary lesion usually has intraductal component. Because the finding was not seen in our patient, primary neuroendocrine carcinoma of the breast is unlikely.
Knowledge of prognostic factors in parathyroid carcinoma is limited. Ki-67 is reported to be a valuable prognostic factor for patients with parathyroid carcinoma, and aggressive surgical resection at the initial surgery is reported to lead to better outcomes [16]. In our patient, the Ki-67 labeling index was slightly increased in the metastatic tumor (10.2%) compared with the primary (7.9%). This suggests that tumor cells with higher proliferative activity may be associated with recurrence and/or metastasis.
In conclusion, we have described the first case of a breast metastasis from parathyroid carcinoma. Physical examination, mammography, and ultrasonography were useful in detecting parathyroid carcinoma metastasis in the breast. Breast metastasis of parathyroid carcinoma should be included in the differential diagnosis for a patient with a past history of parathyroid carcinoma.
References
Fujita T (1983) Primary hyperparathyroidism. Nippon Rinsho 41(supplement):823–830
Schantz A, Castleman B (1973) Parathyroid carcinoma: a study of 70 cases. Cancer 31:600–605
Sandelin K, Auer G, Bondeson L et al (1992) Prognostic factors in parathyroid cancer: a review of 95 cases. World J Surg 16:724–731
Obara T, Fujimoto Y (1991) Diagnosis and treatment of patients with parathyroid carcinoma: an update and review. World J Surg 15:738–744
Sandelin K, Tullgren O, Farnebo LO (1994) Clinical course of metastatic parathyroid cancer. World J Surg 18:594–599
Cordeiro AC, Montenegro FL, Kulcsar MA et al (1998) Parathyroid carcinoma. Am J Surg 175:52–55
Hundahl SA, Fleming ID, Fremgen AM et al (1999) Two hundred eighty-six cases of parathyroid carcinoma treated in the U.S. between 1985–1995: a National Cancer Data Base Report. The American College of Surgeons Commission on Cancer and the American Cancer Society. Cancer 86:538–544
Busaidy NL, Jimenez C, Habra MA et al (2004) Parathyroid carcinoma: a 22-year experience. Head Neck 26:716–726
Wilkins BJ, Lewis JS Jr (2009) Non-functional parathyroid carcinoma: a review of the literature and report of a case requiring extensive surgery. Head Neck Pathol 3:140–149
Nakamura Y, Kataoka H, Sakoda T et al (2010) Nonfunctional parathyroid carcinoma. Int J Clin Oncol 15:500–503
Ashkenazi D, Elmalah I, Rakover Y (2006) Concurrent nonfunctioning parathyroid carcinoma and parathyroid adenoma. Am J Otolaryngol 27:204–206
Gao WC, Ruan CP, Zhang JC et al (2010) Nonfunctional parathyroid carcinoma. J Cancer Res Clin Oncol 136:969–974
Busaidy NL, Jimenez C, Habra MA et al (2004) Parathyroid carcinoma: a 22-year experience. Head Neck 26:716–726
Nielsen M, Andersen JA, Henriksen FW et al (1981) Metastases to the breast from extramammary carcinomas. Acta Pathol Microbiol Scand A 89:251–256
Toombs BD, Kalisher L (1977) Metastatic disease to the breast: clinical, pathologic, and radiographic features. AJR Am J Roentgenol 129:673–676
Iihara M, Okamoto T, Suzuki R et al (2007) Functional parathyroid carcinoma: long-term treatment outcome and risk factor analysis. Surgery 142:936–943
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Uchida, N., Ishiguro, K., Suda, T. et al. Metastatic breast tumor due to nonfunctional parathyroid carcinoma. Int Canc Conf J 1, 47–52 (2012). https://doi.org/10.1007/s13691-011-0008-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13691-011-0008-8