Abstract
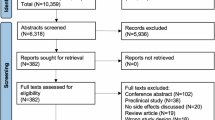
Purpose of Review
In recent years, drug repurposing has gained traction as a method to accelerate the availability of effective treatments. This review focuses on timolol, originally a topical non-selective β-adrenergic antagonist used for increased intraocular pressure and glaucoma, and its emerging role in the wound healing landscape—a field that has been lacking in effective treatments for decades.
Recent Findings
Preclinical and clinical studies have highlighted timolol’s promise as a therapeutic option in wound healing. Its benefits are attributed to various mechanisms including improved re-epithelialization, modulation of inflammation, and wound maturation, in addition to its impacts microbial quorum sensing and virulence. However, existing research also points to the need for larger, more comprehensive clinical trials to determine optimal dosing, efficacy, and safety. Some such trials are presently underway.
Summary
Timolol presents a new avenue for wound healing therapies, overcoming limitations seen in current treatment options. This review outlines timolol’s historical context in wound care, elaborates on its pharmacological mechanisms, and assesses ongoing research to validate its therapeutic potential. Future studies are needed for more conclusive data on its efficacy and safety in wound management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intractability of Chronic Wounds and the Lack of New Therapies
Chronic wounds affect over 3% of the US population aged 65 and older [1]. Over the past 50 years, non-healing wounds have become a significant global health burden, exacerbated by an aging population and rising incidence of chronic comorbidities such as diabetes [1,2,3]. Often overlooked, is the substantial impact that chronic wounds can have on patients' economic well-being in addition to their general quality of life (QOL). This impact is comparable to that seen with other common chronic conditions such as chronic obstructive pulmonary disease (COPD) and cardiovascular disease [2]. However, the burden of chronic wounds does not stop at the patient, extending to the healthcare systems as well; for instance, in 2014, US Medicare expenditures related to wounds upwards of 95 billion US dollars annually. This makes chronic wounds an important area for advancement, not only for patients but also for the healthcare systems that serve them [4].
Within the overarching term of chronic wounds there are several common categories including diabetic foot ulcers (DFUs), venous leg ulcers (VLUs), pressure injuries (PIs). DFUs in particular have a significant impact on patients and healthcare systems, estimating to cost the US healthcare system $9–13 billion annually [4]. Additionally, they have been associated with a shocking 5-year mortality rate close to 50% [5•]. To put this in perspective, a 50% mortality rate surpasses that of colon cancer (48%), Hodgkin’s disease (47%), breast cancer (15%), and prostate cancer (15%) [6, 7]. Other chronic wounds have similarly been found to have high mortality rates with VLUs reported as having a 2-year mortality rate around 28%, and PIs associated with a 124% increased risk of death [8].
There are over 500 million people in the world with diabetes, and it is estimated that a staggering 25% of them will go on to develop a DFU during their lifetime, with around 15% of them requiring an amputation [9]. Though estimates suggest that targeted interventions may reduce amputation rates to around 5% [10], accessible and effective therapies are notably lacking despite significant advancements in wound management technology [9, 11,12,13,14]. The large financial burdens, high mortality rates, and lack of currently available therapies highlight the urgent need for innovative and effective wound care strategies [1, 10, 15, 16]. For this reason, it is important to provide an overview on the use of topical timolol as a novel therapeutic option in wound healing and the pre-clinical and clinical [17] advancements that have been reported around its use.
Background
Topical Medications in Wound Healing
The global wound care market was valued at over $20.6 billion US dollars in 2022 and is projected to reach $30 billion by 2030 [18], however despite the financial incentive, many therapies have yet to display consistent therapeutic efficacy. A 2007 meta-analysis of 42 randomized controlled trials (RTCs) encompassing over 1000 patients found no significant advantage among various dressing types, such as hydrocolloid, hydrogel foams, pastes, silver-impregnated dressings, and simple nonadherent dressings [19]. An updated meta-analysis covering an additional 43 RCTs from 2014 to 2021 similarly revealed no further compelling evidence regarding these often commonly prescribed topical treatments [20]. When the size of the wound care market is evaluated against the lack of proven effective therapies, it is easy to see that these vulnerable patients deserve better.
When topical wound treatments were first beginning to be evaluated in the mid 1950s, efforts were made to evaluate strong topical antibiotics to reduce microbial burden and promote wound healing, however they were quickly abandoned due to frequent adverse events (AEs) including skin hypersensitivity and allergic contact dermatitis [21]. As a result, there was a pivot towards other topicals such as growth factor-based therapies, such as those utilizing platelet-derived growth factor (PDGF), fibroblast growth factor, and epidermal growth factor. Although pre-clinical findings were encouraging, only PDGF progressed beyond phase 2/3 clinical trials and became a clinically available topical therapeutic in 1997 sold under the brand name Regranex (becaplermin) [7, 22]. Many of the other growth factor based therapies had their trials cut short due to poor absorption, short half-lives, and even potential carcinogenicity [21, 23]. Notably, in May 2023, the FDA approved a gene-based novel therapy, Vyjuvek, making it the first approved FDA therapy for wound healing since Regranex 26 years prior. However, Vyjuvek is indicated solely for the use in dystrophic epidermolysis bullosa and has not been tested for efficacy in other more general wounds [24].
With the recognized challenges in the development of wound healing therapeutics, there have been recent efforts to repurpose already approved medications, such as topical timolol. Given its supportive pre-clinical evidence and long history of safe use in its topical ophthalmologic application, timolol has shown to be a new therapeutic candidate with excellent tolerance and accessibility. In this context drug repurposing presents multiple benefits as expediting the wound therapy pipeline, facilitating regulatory clearance, reducing failure incidences, and significantly diminishing developmental costs [25].
Timolol
Timolol (TM), a β-adrenergic receptor (βAR)-antagonist, was first approved for topical use in the USA in 1978 for the treatment of increased intraocular pressure [26]. By 2020, it had continued to be a standard therapeutic option in the treatment of increased intraocular pressure and glaucoma, with an estimated 4 million prescriptions in the USA alone [27]. There are currently two FDA-labeled uses of topical TM, including open-angle glaucoma and ocular hypertension, and one off-label use in the treatment of infantile hemangiomas [28]. Though generally well tolerated, TM is contraindicated in patients with a history of asthma, COPD, and other pre-existing pulmonary conditions [29], in addition to underlying cardiovascular conditions such as bradycardia, heart block, or syncope [28, 30]. However, the risks may far outweigh the benefits regarding the potential applications in wound healing and are further evaluated below. This review aims to help provide a better understanding into TM's potential role in wound healing by providing a broad overview of the historical and mechanistic contexts as they are currently understood.
Early Studies of Timolol and Beta-Adrenergic Receptors in Wound Healing: 1970–1980s
The presence of adrenergic receptors (ARs) in the skin has been recognized since 1972 [31]. However, it was not until 12 years later that Donaldson and Mahan began to investigate the influence of ARs on wound healing [32]. Their work demonstrated the inhibitory effect catecholamines can have on epithelial cell migration, primarily via βAR activation. Subsequent research by, other investigators revealed the varied roles of β2-ARs on several wound-resident cells, including endothelial cells, keratinocytes, and fibroblasts [33,34,35]. ARs were found to impact important cellular processes such as melanogenesis, vascular dilation, fibroblast proliferation, wound matrix deposition, and re-epithelialization. However the extent and mechanism of these effects remained poorly understood [33].
During the early 1980s, studies began to highlight the potential benefits of βAR-antagonism in enhancing corneal wound healing and reducing ophthalmic bacterial wound burden [36, 37]. However reports emerged suggesting that TM might slow corneal epithelium healing [33, 38,39,40]. This led to a slowing in the evaluation of TM for wound healing until the 1990s. It was then discovered that the impaired corneal healing previously reported was not due to TM, but rather to the preservative benzalkonium chloride, which was commonly used for ophthalmic compounding [41].
Developments from the Turn of the Century: 1990s–2000s
In the early 1990s, there was a notable increase in interest in transcutaneous glaucoma treatments, leading to a new wave of studies investigating TM’s transcutaneous absorption profiles and side effects. This research laid the groundwork for its future dermatologic applications [42,43,44,45]. Beyond profiling TM's transcutaneous pharmacokinetics, the rising interest contributed to a deeper understanding of the cutaneous adrenergic system. For instance, it was discovered that keratinocytes synthesize both epinephrine (EPI) and norepinephrine (NE). This built on earlier findings of the presence of βARs on keratinocyte cell membranes, marking significant step in recognizing the skin as a self-sustaining catecholamine network [46, 47]. At the turn of the century, the previous discoveries in βAR and TM led to a broadening of TM's potential as as therapeutic option, with various studies highlighting its capabilities for retinal neuroprotection [48,49,50] in addition to its anti-inflammatory properties [41, 51, 52].
Additionally, during the same period of time, there was an increase in research focusing on the micro and molecular environment of chronic wounds. This research helped show how βAR-antagonism significantly impacts on key pathways, such as the ERK/cAMP signaling pathways [53,54,55]. It also demonstrated that βAR activation is involved in unchecked inflammation, impaired keratinocyte migration, and irregular angiogenesis [56,57,58,59,60,61,62,63,64,65]. The utility of beta blockers such as TM in wound healing garnered more attention, with numerous in-vitro and in-vivo studies showing its potential therapeutic potential. For example, some studies showed that βAR-antagonism could enhance murine keratinocyte single-cell migration by up to 33% [66]. By the end of the early 2000s, the understanding of the role βARs in wound healing had expanded substantially, including areas such as wound contraction and remodeling [67], modulation of mesenchymal stem cells, fibrocytes and inflammation [60, 68], improvement in wound angiogenesis [60, 69, 70], and re-epithelialization [61, 71, 72].
From Bench to Bedside: 2010s–2023
It was in the past decade, since, since 2010, that TM began to be clinically evaluated for its dermatologic applications in patients, starting with the general adoption of its use in the treatment of infantile hemangiomas [73, 74]. Then, after over three decades of bench research evaluating βARs, wound healing, and TM, the first cases showcasing TM's clinical therapeutic potential were published in the early 2010s [75, 76]. These early case reports were then followed by a surge in clinical research on the topic, including more case reports, observational studies, and clinical trials. These studies evaluated TM for the use in various indications such as vascular lesions [77,78,79], thermal wounds [80, 81], chronic wounds [82, 83], surgical wounds [84, 85], and other soft tissue disorders including pyoderma gangrenosum [86, 87] and epidermolysis bullosa [7, 14]. With this mounting evidence, TM appears well-positioned as a promising therapeutic option for wound healing in the coming decade [7, 14].
Physiology and Pathophysiology of Timolol in Wound Healing
Wound healing is a multifaceted process composed of four phases: hemostasis, inflammation, proliferation, and maturation. Disruption or prolongation of these phases often results in dysregulated wound healing [53,54,55,56,57, 60, 88]. TM can have various impacts on all of these phases, however the most clinically relevant for this review include inflammation, proliferation, and maturation. Within these phases of healing TM has been found to antagonize the β1- and β2-ARs receptors expressed on keratinocytes [63, 89, 90], fibroblasts, and macrophages [59, 91,92,93,94, 95•, 96•, 97]. Notably, keratinocytes have been found to not only be sensitive to adrenergic signaling via ARs, but to also synthesize their own EPI [98], making the skin a self-contained catecholaminergic system [46, 61, 95•, 99]. EPI has a unique biphasic relationship within wound healing, with supra-physiological levels hindering healing, and physiological levels potentially promoting it. For this reason the adrenergic pathway is a unique option for potential therapeutic intervention through adrenergic system modulators such as TM [62, 90, 100, 101].
Jia et al. recently published a comprehensive review that discusses the mechanism of βARs and their effect on wound healing [95•]. This review will instead provide only an overview of the topic.
Effect on the Inflammatory Phase
Upon injury and subsequent achievement of hemostasis inflammatory cascades are activated in the local injured tissue, marking the initiation of the inflammatory phase. The inflammatory phase begins with the degranulation of local platelets, which lead to the release of chemokines such as IL-8, TGF-β1, and PDGFs thereby intensifying the inflammatory cascade [102]. Within the first 24 hours, polymorphonuclear neutrophils (PMNs) are recruited and become the predominant cell type found within the wound, constituting of up to 50% of the cellular composition [103]. PMNs play a crucial role in debris and microbial defense as they secrete inflammatory mediators such as IL-8, TNF-α, and IL-1β, further upregulating the inflammatory response and drawing even more neutrophils to the site of injury [102, 104, 105]. As the inflammatory phase progresses, there is a notable shift in the cytokine profile. Initially, increased levels of chemokines such as CCL2 attract monocytes which subsequently replace PMNs as the predominant cell type within the wound [106]. As the concentration of monocytes within the wound bed increases, another shift occurs in the cytokine profile, marked by significant rise in IL-6. This enhances the migration of mast cells and lymphocytes to the healing site [102]. Influenced by these incoming cells, the monocytes differentiate into specific macrophage subtypes, mainly M1 (pro-inflammatory) and M2 (anti-inflammatory) [107]. Once differentiated, these various macrophages add to the cytokine-rich environment [108], facilitating various processes, from cellular apoptosis and microbial clearance (via M1) to resolution of inflammation and aiding in the transition from the inflammatory to the proliferative phase (via M2) [102, 108].
Catecholamines, have been proposed to play a significant role in the communication pathways involved during the inflammatory phase, particularly by β2-ARs [95•, 99, 109, 110]. Persistent catecholamine presence within wounds has been associated with significantly dysregulated and delayed wound healing [111] by prolonged activation of β2-ARs leading to decreased neutrophil functionality, hindered Langerhans cell migration, skewed differentiation of CD4+ cells towards a pro-inflammatory Th2 profile, and metabolic disruption in CD8 + cells [97, 112,113,114,115,116].
TM has been shown to be effective in actively countering the increased inflammatory response seen in unopposed EPI-mediated healing dysregulation [81]. Though TM’s impact on the inflammatory phase has improved significantly over the years, its full mechanism of action has been yet to be fully been understood and appears to be quite multifaceted [45, 95•, 97, 102, 117,118,119] That being said, TM's effect on the inflammatory phase is notably associated with improved regulation of pro-inflammatory neutrophils and macrophages [106, 120]. Furthermore, TM has also shown potential in driving cellular differentiation in an anti-inflammatory direction, favoring M2 macrophages and Th1 CD4+ cell polarization [113, 115, 121].
Effect on the Proliferative Phase
Re-Epithelialization
A few days after wounding, and the inflammatory phase reaches its peak, the proliferative phase gradually start. This phase typically lasts for approximately four to twenty-four days, reaching its peak around two weeks post-injury. During this phase, new tissue is generated to repair and replace the damaged tissue. Re-epithelialization is the process by which basal keratinocytes reestablish the skin's barrier, a defining feature of a healed wound. Multiple cytokine and growth factor pathways converge to mediate this process, as reviewed by Pastar et al. [122]. Relevant to this review, one cytochemical pathway is via modulation of the ARs expressed by keratinocytes, predominantly β2-ARs [63, 99, 123]. When activated, the β2-AR pathway inhibits keratinocyte migration through the elevation of cAMP and the phosphorylation of ERK, AMPK, and p38 mitogen-activated protein kinase (MAPK), alongside the downregulation of the PI3/AKT pathways, all of which lead to decreased activation of pro-migratory pathways [58, 90, 111, 124,125,126,127]. Additionally, β2-AR activation downregulates keratinocyte proliferation, primarily through nitric oxide (NO) generation, facilitated through the same cAMP-PKA pathway [99, 123, 126]. By blocking these pathways, TM promotes keratinocyte proliferation and migration. By the improved keratinocyte migration seen within the context of TM has been extensively studied, and has been found to be primarily due to modulation of pro-migratory cytoskeletal remodeling [124], and prevention of ERK and AKT dephosphorylation. This leads to reduced expression of tyrosine hydroxylase (TH) and PNMT, consequently diminishing endogenous catecholamine synthesis in keratinocytes [64, 95•, 128, 129]. In this way TM has demonstrated the ability to increase keratinocyte migratory speeds by around 28% and ERK phosphorylation by 2.5-fold [64], improving the rate of wound re-epithelialization [61, 63].
Granulation Tissue Formation
Fibroblast Proliferation and Migration
The production of granulation tissue, occurring approximately 3–4 days post-injury, is characterized primarily by the activation and migration of fibroblasts. Proliferating fibroblasts migrate to the wound bed attracted in a similar fashion as keratinocytes (as described above) [130].
The proliferation, migration, and activation of fibroblasts have all similarly been found to involve βAR regulation [107, 131,132,133]. However, contrasting to the inhibition of keratinoctye proliferation and migration, studies have demonstrated that, in fibroblasts, β2-AR activation can lead to an up-regulation, rather than a reduction, in both the migration and proliferation of fibroblasts [59, 134]. Although this upregulation may seem beneficial, it has been associated with undesirable consequences, including excessive fibrosis, scarring, and ultimately compromised contraction capability [67, 71]. Mechanistically, the enhanced fibroblast migration attributed to βAR activation is believed to be orchestrated through src-mediated transactivation of the epidermal growth factor receptor (EGFR) [59]. TM however has been found to help modulate fibroblast migration and proliferation by blocking βARs and dampening ERK 1/2 phosphorylation [59, 134]. Notably β3-ARs are the most abundantly found ARs on fibroblasts, which is another possible explanation for the unique responses seen in fibroblasts compared to other cell types, with an increase in proliferation and migration rather than being being inhibited when in an EPI rich environment [135,136,137,138].
ECM Deposition
After fibroblasts have migrated to the wound bed, they begin to form the extracellular matrix (ECM), synthesizing collagen fibers, and other essential ECM materials such as fibronectin, glycosaminoglycans, proteoglycans, and hyaluronic acid [139]. During the early phase of granulation tissue development, there is a marked increase of immature blood vessel formation, accompanied by a rich cellular framework and fibers [130]. As this phase progresses, a subset of fibroblasts, under the influence of TGF signaling, undergo further differentiation becoming myofibroblasts, the main cells responsible for wound contraction [140, 141].
ARs have been found to regulate development of the ECM and ultimately, the scarring process [131, 142]. In this way, TM and other βAR-antagonists have been reported to improve scarring cosmesis, through more effective wound contraction, and a downregulation of pro-fibrotic mRNA [80, 131, 142]. The effect has been hypothesized to be in part due to modulation of multiple pathways including: PNMT, ERK, and phosphoprotein phosphatases (PP2A) [95•, 143]. Paradoxically, it has been demonstrated that decreased expression of βARs, rather than an increase, has been related with hypertrophic scarring, though it is possible this is due to unregulated fibroblast proliferation as mentioned above [131, 144]. Furthermore, fibroblasts derived from hypertrophic scars were noted to have a lower βAR-stimulated cAMP concentration compared to typical fibroblasts [131], further implicating that the adrenergic system may be involved, however to what to degree or how remains still an area of investigation.
Angiogenesis
Angiogenesis is another important step in granulation tissue formation, playing a vital role in supplying nutrients and removing waste from the wound environment [140]. After injury, vascular endothelial cells are stimulated by growth factors such as vascular endothelial growth factor (VEGF) and PDGF [130, 145]. Notably, these endothelial cells express a range of receptors, including β1-, β2-, and β3-ARs [90, 95•, 100, 110]. The roles of ARs in angiogenesis have been extensively reviewed [146], and here, we note only that the relationship between βAR-antagonists and angiogenesis is intricate, with multiple overlapping facets [99, 130, 147, 148]. TM is reported to enhance vascular permeability and amplify VEGF secretion [144, 145, 148]. However, despite the wealth of data on angiogenesis, the exact mechanism of action of TM, and other βAR-antagonists, in optimizing wound healing via angiogenesis regulation has yet to be fully understood [95•, 149].
Effect on the Maturation Phase
The maturation phase is the final phase of wound healing and can vary greatly in duration, depending on patient and wound-related factors, typically lasting anywhere from weeks to years. The influence of TM during the maturation phase has been primarily associated with controlling scar formation through 8-hydroxy-2’-deoxyguanosine (8OHdG) [101] and its effect on the modulation of matrix metalloproteinases (MMPs). As tissues move into the maturation phase, approximately 3 weeks post injury, the provisional fibrin-rich matrix matures into a robust collagen-dominated matrix [140, 150]. MMPs play an integral role in refining the collagen structure, continuously degrading, and reshaping it. Notably, several MMPs have distinct targets within the wound bed leading modulation of each MMP have various long term remodeling consequences [150, 151]. A deviation from balanced collagen construction and destruction can result in significant wound healing dysregulation and delay [151].
TM has been shown to modify MMP-mediated outcomes by inhibiting the activation of MMP-9 and MMP-2 [95•, 150, 152]. Studies have shown that the effect appears to be linked to complex dynamic between MMPs, ARs, PP2A, and their common β-Arrestin/NF-κB-dependent pathway [111, 153]. Additionally, there has also been recent new data showing that βAR-antagonists might promote the expression of beneficial MMPs, such as MMP-1, -3, and -13, especially in the presence of IL-1β [153]. However, the relevance of these findings to wounds and its therapeutic potential remains to be fully explored [105].
Bacterial Modulation
Modulation of Bacterial Activity and Quorum Sensing
Beyond it's immediate impact on the wound healing phases, there has been a growing body of literature evaluating the potential anti-virulence effect of TM, primarily through its interactions with bacterial quorum sensing (QS) systems. QS systems are a unique chemical language intrinsic to bacteria, enabling them to gauge adrenergic signals within their environment [154] permitting bacteria to dynamically adjust their motility, biofilm formation, and gene expression based on external stimuli [155]. In a recent study, when Pseudomonas aeruginosa, a common pathogen that has been linked to wound healing dysregulation, was exposed to TM, the pathogens demonstrated significantly decreased biofilm formation when compared to those not exposed to TM [96•]. This is particularly consequential as catecholamines have been identified to increase wound bacterial burden, especially after antibiotic use [156]. By inhibiting QS, TM and other βAR-antagonists essentially blind bacteria, undermining their adaptive responses, thereby potentially reducing infections and improving wound recovery [155].
Trace Amine Interactions and Microbiota Adaptation
Many skin microbiota phyla are equipped with the sadA gene, which catalyzes the conversion of aromatic amino acids such as tryptamine, phenethylamine, and tyramine into trace amines (TAs) [157, 158•]. These TAs can have both agonist and antagonist properties, activating α2-AR receptors [159] inhibiting βARs and α1-ARs [160,161,162]. In light of recent investigative efforts highlighting the positive effect on βAR-antagonism on wound healing, it is unsurprising that these pathways have been leveraged organically by various bacteria. For instance, strains of Staphylococcus epidermidis that produce TA, have been shown to improve wound healing compared to non-TA-producing strains. Furthermore, QS systems are known to exhibit binding affinities for TAs, which can counteract the effects of local catecholamines, leading to the various dysregulated wound healing impacts previously described in environments with up-regulated EPI [162].
Effect on Biofilm
Biofilm formation in wounds has been associated with worse wound healing outcomes and chronic wounds and burns [163,164,165] making it an important area of wound healing research. Recently studies have shown that catecholamine-rich environments can upregulate the production of biofilms [166,167,168]. Notably, it has been demonstrated that this catecholamine-induced biofilm growth can be directly inhibited by βAR-antagonists like TM [96•] with biofilms grown on physiological collagen substrates, showing marked reductions in their growth triggered by either EPI or NE when in the presence of TM [96•].
Clinical Studies
The clinical studies of TM and wound healing are listed in Table 1, 2, 3, and 4 and briefly summarized below.
Chronic Wounds
Clinical Trials
TM demonstrated improved wound healing in VLUs compared to standard of care (SOC) in two RTCs, with an average difference in absolute area reduction (ARR) between the TM and SOC groups of 39.2% (TM ARR 69.35% n=31, SOC ARR 30.15% n=29) [82, 83].
Observational Studies
A total of six observational studies have evaluated the use of TM in chronic wounds, with two being retrospective in nature [85, 181,182,183,184, 186]. One study focused on evaluating plasma concentration and side effects [184], whereas the remaining five assessed wound healing efficacy. Among these efficacy studies, 271 patients were enrolled, and all reported improved wound healing in subjects treated with TM compared to those in the comparison group [202].
Descriptive Studies
Four case reports have been published highlighting TMs efficacy in improving healing in chronic wounds. These reports document seven separate patients with VLUs being the most common condition, observed five of the patients [75, 76, 183, 187, 188].
Current Studies
A 5-year randomized double-blinded control study is currently underway evaluating 0.5% TM against placebo in the treatment of DFUs [177•].
Radiation Dermatitis
Patients pre-treated with TM displayed reduced severity of acute radiation dermatitis (ARD) in a RCT including 64 women who received radiation for breast cancer. When evaluated using the RTOG/EORTC toxicity criteria, the ARD experience by the women in the TM group was markedly diminished (31.3% grade II ARD) compared to those in the placebo group (75.0 % grade II ARD) consisting of only glycerin [171].
Split-Thickness Skin Graft Donor Sites
Clinical Trials
TM application led to a significantly faster re-epithelialization (11.5 ± 2.3 days, n=32) than a placebo (14.5 ± 3.2 days, n=32, p < 0.001) in a RCT. While there were reduced pain scores and improved scar appearance in the TM group after 3 months were significantly improved as measured by the Vancouver Scar Score (VSS) [185].
Observational Studies
In a case-control study of 42 patients, TM showed a significant decrease in the average days required to heal in split-thickness skin graft donor sites with an average of 6.4 days in the TM group and 12.7 days in the control group [185].
Acute Surgical Wound
TM has been demonstrated to be effective in the treatment of acute surgical wounds, as evidenced by both a small RCT (n=6) and a retrospective review (n=86). These studies have shown faster healing rates and improved Visual Analog Scale (VAS) scores when compared to SOC [85, 175, 191]. The retrospective review specifically evaluated the use of topical TM following Mohs micrographic surgery on the lower extremities in patients with high comorbidities for delayed wound healing. Results indicated that patients in the TM group healed as quickly as healthy control patients (7.9 weeks compared to 7.7 weeks), and more effectively than similar patients with comorbidities who did not receive TM (10.8 weeks) [85].
Current Studies
Currently, there are two ongoing clinical trials evaluating the effect of 0.25% TM versus the standard of care in post-resection of malignancy wounds and open surgical wounds [178, 179].
Nail Lesions
TM has been shown to be effective in the treatment of endothelial growth factor receptor inhibitor (EGFRi)-induced paronychia when evaluated by the physician Global Assessment Score (pGAS) [169] in a small RCT of 8 patients. There have also been various case reports providing evidence for the use of TM in healing other nail lesions refractory healing like ingrown nail post-avulsion wounds and pyogenic granulomas associated with paronychia [198,199,200]
Ablative Fractional CO2 Laser (AFCO2)
TM-treated patients after AFCO2 procedures have also showcased superior skin hydration levels, reduced transepidermal water loss (TEWL), and better cosmetic scores in 3 separate RCTs, evaluating a total of 56 patients (though of note, one of the studies showed an improvement which was not statistically significant) [172,173,174].
Acne Scar Revision
In a blinded RTC, when used afterTCA-CROSS, injected normal saline (NS) and topical TM not only improved scar appearances but notably reduced scar hyperpigmentation when compared to injected NS alone, though the difference was not found to be significant [176].
Current Studies
A current trial is assessing the utility of 0.5% TM when combined with micro-needling for the treatment of atrophic acne scars [180].
Vascular Lesions
Previous clinical trials have demonstrated a significant lesion reduction in pyogenic granulomas with the use of 0.5% TM [170]. Other vascular lesions have been extensively studied; all of which have demonstrated promising effectivity regarding the use of TM in the treatment of vasculitic ulcers, angioendotheliomatoses, Kaposi sarcomas, and ulcerated hemangiomas [17, 189, 192, 194, 203,204,205,206,207,208,209].
Other Descriptive Studies
Refractory Hypergranulation Tissue (RHT)
Two case studies exhibited complete resolution within two weeks of start 0.5% topical TM treatment for refractory hypergranulation tissue (RHT) [190].
Hidradenitis Suppurativa
A reported case of a patient showing and 80% area reduction with the use of 0.5% topical TM [201].
Junctional Epidermolysis Bullosa
A case report including two infants treated with 0.5% topical TM for lesions associated with junctional epidermolysis bullosa showed a signficant improvement with a 100% area reduction in one infant, and 80% in the other after 8 weeks of treatment [193].
Hydroxyurea-Induced Ulcers
A case report documented complete resolution of hydroxyrea-induced ulcers after using 0.5% topical TM for 17 weeks [195].
Recalcitrant Fissures
Two separate reports of 0.5% topical TM use in in deep non-healing fissures of the heels and hands were reported with complete resolution after 4 weeks for the heel fissures and only 1 week for the hands [196, 197].
Pyoderma Gangranosum (PG)
Two case reports documented the successful treatment of idiopathic PG in two female patients after 5 months of 0.5% topical TM therapy [86, 87].
Considerations for Use
TM is currently widely used as a topically applied ophthalmologic treatment for wide-angle glaucoma, and generally considered to be well tolerated. With the growing repurpose of TM for topical applications, understanding its potential for systemic effects and adverse events (AEs) is critical. Given that a recent prospective study revealed no significant difference in plasma levels of TM 1 hour post-ophthalmic application compared to the topical application chronic wounds, it is assumed that the safety profile for both applications can be considered equivalent [184]. Yoon et al. [210•] provided clinical guidelines that offer valuable considerations accompanied by a proposed prescribing algorithm for dermatologic applications. This section further underscores the importance of these guidelines, aiming to equip clinicians with the tools need to make informed decisions regarding the use of TM in wound healing for their patients.
Current Clinical Data and Guidelines
Contraindications
The use of TM for wound healing is contraindicated in patients with preexisting heart block, syncope, bradycardia, asthma, or COPD [211].
Adverse Events (AEs)
AEs are most often reported from ophthalmic TM solution use due to the significant prevalence of use over the past 4 decades. With the absorption of ophthalmic and topical TM applications being comparable [184], it is reasonable to assume similar potential for systemic AEs which have been listed as the following: arrhythmia, tachycardia, palpitations, heart failure, angina, respiratory arrest, respiratory failure, respiratory distress, dyspnea, apnea, asthma, bronchitis, contracted lung function, apneic spell, syncope, headache, cerebrovascular accident, depression, gastrointestinal distress, and sexual impotence [212].
Patient Monitoring
Yoon et al. recommend observing heart rate, blood pressure, and lung function prior to and 20 min after TM application. An ambulatory ECG may be necessary for high-risk candidates [210•, 212].
Dosage and Application
Lower concentration formulations (0.1% of TM solution) have exhibited fewer cardiac side effects in glaucoma patients [213]. However, both 0.25% and 0.5% formulations have shown good tolerability in previous studies as well [184]. Notably, the most common formulation provided in the literature for topical use in wound healing is 0.5% TM between once and twice a day (Tables 1, 3, and 4). Regarding application, the current standard is that the TM drops should be applied directly to the wound edges to promote keratinocyte migration [212]. Given the comparable AEs and absorption profiles between the two types of applications, stringent patient monitoring, pre-screening, and dosing continue to be essential.
Safety Concerns from Historical Data
Bradycardia stands out as the most common significant AE, with other major concerns being cardiac and respiratory dysfunctions. Historical data highlights 20 reported deaths linked to TM use since 2013, primarily from cardiac and respiratory causes [214]. This further underscores the need for rigorous safety evaluations, especially as 4.29% of AEs reported since 1978 relate to bradycardia in topical TM use [214]. Current clinical studies focusing on dermatological applications tend to prioritize drug efficacy and often overshadowing the importance of monitoring for potential AEs [210•], however as with all medications, the potential benefits and risks must be weighed for each patient independently.
Pharmacodynamics, Metabolism, and Potential Genetic Considerations
Systemic effects of TM, even if not considered as significant AEs, should be evaluated cautiously, especially given the potential for unique individual predispositions. Genetic variances, such as polymorphisms in genes like CYP2D6 or the β1-AR, can affect TM response, creating suggested metabolization categories for patients which have been defined as: ultra-rapid metabolizers, extensive metabolizers, intermediate metabolizers, and poor metabolizers [215,216,217]. Genotyping for these polymorphisms may offer an added safety layer for those susceptible to AEs, as suggested by Yoon et al. [210•, 212], especially given the ambiguous correlation between TM’s plasma concentration and its bioactivity [210•].
Drug-Drug Interactions
Recent discoveries highlight potential drug interactions between TM and other drugs such as selective serotonin reuptake inhibitors (SSRIs), cyclo-oxygenase-2 (COX-2) inhibitors, and histamine receptor antagonists [218,219,220,221]. These interactions might amplify the systemic absorption of TM and potentially exacerbate AEs, especially in elderly patients within the setting of potential polypharmacy, and should be considered prior to prescribing to patients [210•].
Conclusion
Since its initial use for glaucoma, the application of timolol has evolved considerably over the years, now presenting a novel opportunity for therapeutic discovery in wound healing. Significant efforts have been invested in both pre-clinical and clinical studies, revealing not only its mechanism of action but its positive impact on inflammation, proliferation, and maturation of wounds through interactions with both endogenous and microbial adrenergic signaling. As the use of timolol for wound healing expands, it is vital to ensure sound research to further understand its efficacy and safety. This is particularly important considering the years of stagnation in finding significant improvement in potential wound healing therapies. Timolol appears to be a promising therapeutic option that is low-cost, globally accessible, and a high incidence of reported effectiveness, making it a viable treatment choice for wounds in the appropriate circumstance.
Abbreviations
- QOL:
-
Quality of life
- COPD:
-
Chronic obstructive pulmonary disease
- DFU:
-
Diabetic foot ulcer
- VLU:
-
Venous leg ulcer
- RTC:
-
Randomized controlled trial
- AE:
-
Adverse event
- PDGF:
-
Platelet-derived growth factor
- TM:
-
Timolol
- AR:
-
Adrenergic receptor
- EPI:
-
Epinephrine
- NE:
-
Norepinephrine
- ERK:
-
Extracellular signal-regulated kinases
- cAMP:
-
Cyclic adenosine monophosphate
- IL:
-
Interleukin
- TGF:
-
Transforming growth factor
- PMN:
-
Polymorphonuclear neutrophil
- TNF-α:
-
Tumor necrosis factor-alpha
- CCL2:
-
Monocyte chemoattractant protein-1
- AMPK:
-
Adenosine monophosphate-activated protein kinase
- MAPK:
-
Mitogen-activated protein kinase
- PI3K:
-
Phosphoinositide 3-kinase
- NO:
-
Nitric oxide
- PKA:
-
Protein kinase A
- TH:
-
Tyrosine hydroxylase
- PNMT:
-
Phenylethanolamine N-methyltransferase
- EGFR:
-
Endothelial growth factor receptor
- ECM:
-
Extracellular matrix
- PP2A:
-
Protein phosphatase 2A
- VEGF:
-
Vascular endothelial growth factor
- 8OHdG:
-
-Hydroxy-2’-deoxyguanosine
- MMP:
-
Matrix metalloproteinase
- NF-κB:
-
Nuclear factor-kappa light chain of activated B cells
- QS:
-
Quorum sensing
- TA:
-
Trace amine
- SOC:
-
Standard of care
- RTOG:
-
Radiation Therapy Oncology Group
- EORTC:
-
European Organization for Research and Treatment of Cancer
- EGFRi:
-
Epithelial growth factor receptor inhibitor
- AFCO2:
-
Ablative fractional CO2 laser
- TEWL:
-
Transepidermal water loss
- TCA:
-
Trichloroacetic acid
- CROSS:
-
Chemical reconstruction of skin scars
- SSRI:
-
Selective serotonin reuptake inhibitor
- COX-2:
-
Cyclo-oxygenase-2 inhibitor
- UNS:
-
Unspecified
- LE:
-
Lower extremity
- NS:
-
Normal saline
- Exp:
-
Experimental/study group
- AAR:
-
Average area reduction
- Ctr:
-
Control group
- ♀:
-
Female
- ♂:
-
Male
- GAS:
-
Physician global assessment scores
- ARD:
-
Acute radiation dermatitis
- Post-Op:
-
Post-operative
- VSS:
-
Vancouver Scar Scale Assessment
- Gt(t):
-
Drop(s)
- Sig.:
-
Statistically significant
- MMS:
-
Mohs micrographic surgery
- AMSC:
-
Adipose mesenchymal stem cell
- HDL:
-
High density lipoaspirate
- VAS:
-
Visual assessment score
- Inj.:
-
Injection
- PIH:
-
Post-inflammatory hyperpigmentation
- SD:
-
Standard deviation
- (R/L)LE:
-
(Right/left) lower extremity
- OU:
-
Ophthalmic
- ED&C:
-
Electrodessication and curettage
- (R/L)UE:
-
(Right/left) upper extremity
- HSCT:
-
Hematopoietic stem cell transplant
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Sen CK. Human wounds and its burden: an updated compendium of estimates. Adv Wound Care. 2019;8(2):39–48.
Olsson M, et al. The humanistic and economic burden of chronic wounds: a systematic review. Wound Repair Regen. 2019;27(1):114–25.
Phillips CJ, et al. Estimating the costs associated with the management of patients with chronic wounds using linked routine data. Int Wound J. 2016;13(6):1193–7.
Nussbaum SR, et al. An economic evaluation of the impact, cost, and medicare policy implications of chronic nonhealing wounds. Value in Health. 2018;21(1):27–32.
• Chen L, Sun S, Gao Y, Ran X. Global mortality of diabetic foot ulcer: a systematic review and meta-analysis of observational studies. Diabetes Obes Metab. 2023;25(1):36–45. Large global systematic review evaluating the global mortality of DFUs demonstrating a 5-year mortality of 50.9%.
Armstrong DG, Wrobel J, Robbins JM. Guest Editorial: are diabetes-related wounds and amputations worse than cancer? Int Wound J. 2007;4(4):286–7.
Eaglstein WH, Kirsner RS, Robson MC. Food and Drug Administration (FDA) drug approval end points for chronic cutaneous ulcer studies. Wound Repair Regen. 2012;20(6):793–6.
Maida V, Ennis M, Kuziemsky C, Corban J. Wounds and survival in noncancer patients. J Palliat Med. 2010;13(4):453–9.
Freedman BR. Breakthrough treatments for accelerated wound healing. Sci Adv. 2023;9(20):eade7007–eade7007.
Driver VR, Fabbi M, Lavery LA, Gibbons G. The costs of diabetic foot: the economic case for the limb salvage team. J Vasc Surg. 2010;52(3 Suppl):17S-22S.
Broderick C, Pagnamenta F, Forster R. Dressings and topical agents for arterial leg ulcers. Cochrane Database Syst Rev. 2020;2020(1).
Dalisson B, Barralet J. Bioinorganics and wound healing. Adv Healthcare Mater. 2019;8(18):1900764–1900764.
Monika P, et al. Challenges in healing wound: Role of complementary and alternative medicine. Front Nutr. 2021;8:791899–791899.
Verma KD, et al. Food and Drug Administration perspective: advancing product development for non-healing chronic wounds. Wound repair and regeneration: official publication of the Wound Healing Society [and] the European Tissue Repair Society. Wound Repair Regen. 2022;30(3):299–302. https://doi.org/10.1111/wrr.13008.
Ma H, O’Donnell TF, Rosen NA, Iafrati MD. The real cost of treating venous ulcers in a contemporary vascular practice. J Vasc Surg Venous Lymphat Disord. 2014;2(4):355–61.
Raghav A, et al. Financial burden of diabetic foot ulcers to world: a progressive topic to discuss always. Ther Adv Endocrinol Metab. 2017;9(1):29–31. https://doi.org/10.1177/2042018817744513.
Cahn BA, et al. Use of topical timolol maleate as re-epithelialization agent for treatment of recalcitrant wounds of varying etiologies. J Drugs Dermatol. 2020;19(12):1252–6.
Facts & Factors. Global wound care market share is expected to grow at a CAGR of 5.6% by 2030. Published May 16, 2023. Accessed August 10, 2023. https://www.fnfresearch.com/news/global-wound-care-market.
Palfreyman S, Nelson EA, Michaels JA. Dressings for venous leg ulcers: systematic review and meta-analysis. BMJ. 2007;335(7613):244.
Shaydakov ME, et al. Review of the current evidence for topical treatment for venous leg ulcers. J Vasc Surg Venous Lymphat Disord. 2022;10(1):241-247.e15.
Frykberg RG, Banks J. Challenges in the treatment of chronic wounds. Adv Wound Care. 2015;4(9):560–82.
Öhnstedt E, Lofton Tomenius H, Vågesjö E, Phillipson M. The discovery and development of topical medicines for wound healing. Expert Opin Drug Discov. 2019;14(5):485–97. https://doi.org/10.1080/17460441.2019.1588879.
Tottoli EM, Dorati R, Genta I, Chiesa E, Pisani S, Conti B. Skin wound healing process and new emerging technologies for skin wound care and regeneration. Pharmaceutics. 2020;12(8):735.
Kempler C. FDA Approves first topical gene therapy for treatment of wounds in patients with dystrophic epidermolysis bullosa. Editor: FN Release; 2023.
Begley CG, et al. Drug repurposing: misconceptions, challenges, and opportunities for academic researchers. Sci Trans Med. 2021;13(612).
Katz IM, Hubbard WA, Getson AJ, Gould AL. Intraocular pressure decrease in normal volunteers following timolol ophthalmic solution. Invest Ophthalmol. 1976;15(6):489–92.
Timolol - Drug Usage Statistics. 2020. Available from: https://clincalc.com/DrugStats/Drugs/Timolol.
Barnes J, Timolol MM. StatPearls. Florida: Treasure Island; 2023.
Negri L, Ferreras A, Iester M. Timolol 0.1% in glaucomatous patients: efficacy, tolerance, and quality of life. J Ophthalmol. 2019;2019:4146124.
Taniguchi T, Kitazawa Y. The potential systemic effect of topically applied beta-blockers in glaucoma therapy. Curr Opin Ophthalmol. 1997;8(2):55–8.
Tseraidis GS, Bavykina EA. Adrenergic innervation of normal human skin. Vestn Dermatol Venerol. 1972;46(7):40–5.
Donaldson DJ, Mahan JT. Influence of catecholamines on epidermal cell migration during wound closure in adult newts. Comp Biochem Physiol C Toxicol Pharmacol. 1984;78(2):267–70.
O’Brien WJ, DeCarlo JD, Stern M, Hyndiuk RA. Effects of timoptic on corneal reepithelialization. Arch Ophthalmol. 1982;100(8):1331–3.
Sheppard JR, et al. The adrenergic responsiveness of Down syndrome cells. Prog Clin Biol Res. 1982;97:307–25.
Szabó K. Clinical experiences with beta adrenergic blocking therapy on burned patients. Scand J Plast Reconstr Surg. 1979;13(1):211–5.
Takahashi N, Murota H, Sutoh I. Antimicrobial activity of topical beta-adrenergic blocking agents. Ophthalmic Res. 1983;15(6):277–9.
Reidy JJ, Zarzour J, Thompson HW, Beuerman RW. Effect of topical beta blockers on corneal epithelial wound healing in the rabbit. Br J Ophthalmol. 1994;78(5):377–80.
Liu GS, Trope GE, Basu PK. Beta adrenoceptors and regenerating corneal epithelium. J Ocul Pharmacol. 1990;6(2):101–12.
Nork TM, et al. Timolol inhibits corneal epithelial wound healing in rabbits and monkeys. Arch Ophthalmol. 1984;102(8):1224–8.
Trope GE, Liu GS, Basu PK. Toxic effects of topically administered Betagan, Betoptic, and Timoptic on regenerating corneal epithelium. J Ocul Pharmacol. 1988;4(4):359–66.
Ishibashi T, Yokoi N, Kinoshita S. Comparison of the short-term effects on the human corneal surface of topical timolol maleate with and without benzalkonium chloride. J Glaucoma. 2003;12(6):486–90.
Kubota K, Koyama E, Twizell EH. Dual sorption model for the nonlinear percutaneous permeation kinetics of timolol. J Pharm Sci. 1993;82(12):1205–8.
Kubota K, Koyama E, Yasuda K. A random walk method for percutaneous drug absorption pharmacokinetics: application to repeated administration of a therapeutic timolol patch. J Pharm Sci. 1991;80(8):752–6.
Kubota K, Koyama E, Yasuda K. Skin irritation induced by topically applied timolol. Br J Clin Pharmacol. 1991;31(4):471–5.
Kubota K, et al. Pharmacokinetics and beta-blocking effects of transdermal timolol. Eur J Clin Pharmacol. 1993;44(5):493–5.
Schallreuter KU. Epidermal adrenergic signal transduction as part of the neuronal network in the human epidermis. J Investig Dermatol Symp Proc. 1997;2(1):37–40.
Schallreuter KU, et al. Catecholamines in human keratinocyte differentiation. J Invest Dermatol. 1995;104(6):953–7.
Goto W, et al. Protective effects of timolol against the neuronal damage induced by glutamate and ischemia in the rat retina. Brain Res. 2002;958(1):10–9.
Baptiste DC, et al. Comparison of the neuroprotective effects of adrenoceptor drugs in retinal cell culture and intact retina. Invest Ophthalmol Vis Sci. 2002;43(8):2666–76.
Wood JP, et al. The beta-adrenoceptor antagonists metipranolol and timolol are retinal neuroprotectants: comparison with betaxolol. Exp Eye Res. 2003;76(4):505–16.
Ostwald J, Graumuller S, Dommerich S, Hoff M. Influence of rhinologic usual and unusual drugs on fibroblasts from nasal polyps in cell culture. Laryngorhinootologie. 2003;82(6):408–15.
Baudouin C, et al. Conjunctival epithelial cell expression of interleukins and inflammatory markers in glaucoma patients treated over the long term. Ophthalmology. 2004;111(12):2186–92.
Bucalo B, Eaglstein WH, Falanga V. Inhibition of cell proliferation by chronic wound fluid. Wound Repair Regen. 1993;1(3):181–6.
Falanga V. Growth factors and wound healing. J Dermatol Surg Oncol. 1993;19(8):711–4.
Falanga V. Chronic wounds: pathophysiologic and experimental considerations. J Invest Dermatol. 1993;100(5):721–5.
Singer AJ, Clark RA. Cutaneous wound healing. N Engl J Med. 1999;341(10):738–46.
Steed DL, et al. Guidelines for the treatment of diabetic ulcers. Wound Repair Regen. 2006;14(6):680–92.
Pullar CE, Chen J, Isseroff RR. PP2A activation by beta2-adrenergic receptor agonists: novel regulatory mechanism of keratinocyte migration. J Biol Chem. 2003;278(25):22555–62.
Pullar CE, Isseroff RR. The beta 2-adrenergic receptor activates pro-migratory and pro-proliferative pathways in dermal fibroblasts via divergent mechanisms. J Cell Sci. 2006;119(Pt 3):592–602.
Pullar CE, Manabat-Hidalgo CG, Bolaji RS, Isseroff RR. β-Adrenergic receptor modulation of wound repair. Pharmacol Res. 2008;58(2):158–64.
Pullar CE, Rizzo A, Isseroff RR. β-adrenergic receptor antagonists accelerate skin wound healing: evidence for a catecholamine synthesis network in the epidermis. J Biol Chem. 2006;281(30):21225–35.
Sivamani RK, et al. Stress-mediated increases in systemic and local epinephrine impair skin wound healing: potential new indication for beta blockers. PLoS Med. 2009;6(1):0105–15.
Sivamani RK, Lam ST, Isseroff RR. Beta adrenergic receptors in keratinocytes. Dermatol Clin. 2007;25(4):643–53.
Pullar CE, et al. β2AR antagonists and β2AR gene deletion both promote skin wound repair processes. J Invest Dermatol. 2012;132(8):2076–2076.
Mohammadi AA, et al. Efficacy of propranolol in wound healing for hospitalized burn patients. J Burn Care Res. 2009;30(6):1013–7.
Ghoghawala SY, et al. Beta2-adrenergic receptor signaling mediates corneal epithelial wound repair. Invest Ophthalmol Vis Sci. 2008;49(5):1857–63.
Pullar CE, Isseroff RR. ß2-adrenergic receptor activation delays dermal fibroblast-mediated contraction of collagen gels via a cAMP-dependent mechanism. Wound Repair Regen. 2005;13(4):405–11.
Flierl MA, et al. Catecholamines - crafty weapons in the inflammatory arsenal of immune/inflammatory cells or opening Pandora’s box§? Mol Med. 2008;14(3–4):195–204.
Souza BR, Santos JS, Costa AM. Blockade of beta1- and beta2-adrenoceptors delays wound contraction and re-epithelialization in rats. Clin Exp Pharmacol Physiol. 2006;33(5–6):421–30.
Gosain A, et al. Norepinephrine modulates the inflammatory and proliferative phases of wound healing. J Trauma Acute Care Surg. 2006;60(4):736–44.
Pullar CE, Grahn JC, Liu W, Isseroff RR. β2-Adrenergic receptor activation delays wound healing. FASEB J. 2006;20(1):76–86.
Aarabi S, et al. Mechanical load initiates hypertrophic scar formation through decreased cellular apoptosis. FASEB J. 2007;21(12):3250–61.
Guo S, Ni N. Topical treatment for capillary hemangioma of the eyelid using beta-blocker solution. Arch Ophthalmol. 2010;128(2):255–6.
Pope E, Chakkittakandiyil A. Topical timolol gel for infantile hemangiomas: a pilot study. Arch Dermatol. 2010;146(5):564–5.
Tang JC, Dosal J, Kirsner RS. Topical timolol for a refractory wound. Dermatol Surg. 2012;38(1):135–8.
Lev-Tov H, Dahle S, Moss J, Isseroff RR. Successful treatment of a chronic venous leg ulcer using a topical beta-blocker. J Am Acad Dermatol. 2013;69(4).
Fernández Faith E, et al. Clinical features, prognostic factors, and treatment interventions for ulceration in patients with infantile hemangioma. JAMA Dermatol. 2021;157(5):566.
Sebaratnam DF, Rodríguez Bandera Al, Wong LCF, Wargon O. Infantile hemangioma, Part 2: Management. J Am Acad Dermatol. 2021;85(6):1395–404.
Monteiro RC, et al. Letter to the editor regarding Effectiveness and safety of 0.5% timolol solution in the treatment of pyogenic granuloma: a randomised, double-blind and placebo-controlled study. Indian J Dermatol Venereol Leprol. 2023;89(1):76–100.
Freiha M, et al. In vivo study of the effects of propranolol, timolol, and minoxidil on burn wound healing in wistar rats. J Burn Care Res. 2023;
Albrecht H, et al. The beta 2 adrenergic receptor antagonist timolol improves healing of combined burn and radiation wounds. Radiat Res. 2018;189(4):441–5.
Baltazard T, et al. Evaluation of timolol maleate gel for management of hard-to-heal chronic venous leg ulcers. Phase II randomised-controlled study. Ann Dermatol Venereol. 2021;148(4):228–32.
Rai A, Janani K, Rai R. Efficacy of topical timolol versus saline in chronic venous ulcers: a randomized controlled trial. J Cutan Aesthet Surg. 2020;13(1):18–23.
Ghanbarzamani A, et al. Efficacy and safety of 0.25% timolol gel in healing split-thickness skin graft site. Iran J Pharm Res. 2021;20(3):178–178.
Manci R, Nazir ZH, Dusza SW, Chen CSJ. Topical timolol enhances surgical wound healing in the lower portion of the leg in older patients with comorbidities: a retrospective review. J Am Acad Dermatol. 2022;87(3):661–3.
Liu DY, Fischer R, Fraga G, Aires DJ. Collagenase ointment and topical timolol gel for treating idiopathic pyoderma gangrenosum. J Am Acad Dermatol. 2014;71(5):e225–6.
Moreira C, Lopes S, Cruz MJ, Azevedo F. Topical timolol for the treatment of pyoderma gangrenosum. BMJ Case Rep. 2017;2017.
Kirsner RS, et al. Spray-applied cell therapy with human allogeneic fibroblasts and keratinocytes for the treatment of chronic venous leg ulcers: a phase 2, multicentre, double-blind, randomised, placebo-controlled trial. Lancet. 2012;380(9846):977–85.
Harper RA, Flaxman BA. Effect of pharmacological agents on human keratinocyte mitosis in vitro. II. Inhibition by catecholamines. J Cell Physiol. 1975;86(2):293–9.
Yang HY, et al. Alpha and beta adrenergic receptors modulate keratinocyte migration. PLoS ONE. 2021;16(7):e0253139–e0253139.
Schallreuter KU, et al. The induction of the alpha-1-adrenoceptor signal transduction system on human melanocytes. Exp Dermatol. 1996;5(1):20–3.
Schallreuter KU, et al. Increased in vitro expression of beta2-adrenoceptors in differentiating lesional keratinocytes of vitiligo patients. Arch Dermatol Res. 1993;285(4):216–20.
Steinkraus V, et al. Autoradiographic mapping of beta-adrenoceptors in human skin. Arch Dermatol Res. 1996;288(9):549–53.
Gupta D, Kaushik D, Mohan V. Role of neurotransmitters in the regulation of cutaneous wound healing. Exp Brain Res. 2022;240(6):1649–59.
• Jia S, Wang X, Wang G, Wang X. Mechanism and application of β-adrenoceptor blockers in soft tissue wound healing. Medicinal Research Reviews. 2023. In depth literature review, evaluating the mechanism of βARs in wound healing and our current understanding.
• Medina Lopez AI, et al. Beta adrenergic receptor antagonist can modify Pseudomonas aeruginosa biofilm formation in vitro: implications for chronic wounds. FASEB J. 2022;36. Pre-clinical data supporting the evidence that βAR-antagonism can lead to decreased biofilm production.
Kim MH, et al. Catecholamine stress alters neutrophil trafficking and impairs wound healing by β2-adrenergic receptor-mediated upregulation of IL-6. J Invest Dermatol. 2014;134(3):809–17.
Gillbro JM, Marles LK, Hibberts NA, Schallreuter KU. Autocrine catecholamine biosynthesis and the beta-adrenoceptor signal promote pigmentation in human epidermal melanocytes. J Invest Dermatol. 2004;123(2):346–53.
Ivanov E, Akhmetshina M, Erdiakov A, Gavrilova S. Sympathetic system in wound healing: multistage control in normal and diabetic skin. Int J Mol Sci. 2023;24(3):2045.
Chakroborty D, Goswami S, Basu S, Sarkar C. Catecholamines in the regulation of angiogenesis in cutaneous wound healing. FASEB J. 2020;34(11):14093–102.
Valente VB, et al. Stress hormones promote DNA damage in human oral keratinocytes. Sci Rep. 2021;11(1):19701.
Strang H, et al. Chapter 11 - Role ofcytokines and chemokines in wound healing. In: Bagchi D, Das A, Roy S, et al., editors. Wound healing, tissue repair, and regeneration in diabetes. Academic Press; 2020. p. 197–235.
Engelhardt E, et al. Chemokines IL-8, GROα, MCP-1, IP-10, and Mig are sequentially and differentially expressed during phase-specific infiltration of leukocyte subsets in human wound healing. Am J Pathol. 1998;153(6):1849–60.
Nwomeh BC, Yager DR, Cohen IK. Physiology of the chronic wound. Clin Plast Surg. 1998;25(3):341–56.
Hwang HS, Lee MH, Go DJ, Kim HA. Norepinephrine modulates IL-1β-induced catabolic response of human chondrocytes. BMC Musculoskelet Disord. 2021;22(1):724.
Kanashiro A, et al. The role of neutrophils in neuro-immune modulation. Pharmacol Res. 2020;151:104580.
Barrientos S, et al. Growth factors and cytokines in wound healing. Wound Repair Regen: official publication of the Wound Healing Society [and] the European Tissue Repair Society. Wound Repair Regen. 2008;16(5):585–601.
Boniakowski AE, et al. Macrophage-mediated inflammation in normal and diabetic wound healing. J Immunol. 2017;199(1):17–24.
Bellinger DL, Lorton D. Autonomic regulation of cellular immune function. Auton Neurosci. 2014;182:15–41.
Fahy EJ, et al. The adrenergic system in plastic and reconstructive surgery: physiology and clinical considerations. Ann Plast Surg. 2021;87(4):e62–70.
Romana-Souza B, Porto LC, Monte-Alto-Costa A. Cutaneous wound healing of chronically stressed mice is improved through catecholamines blockade. Exp Dermatol. 2010;19(9):821–9.
Nicholls AJ, et al. Activation of the sympathetic nervous system modulates neutrophil function. J Leukoc Biol. 2017;103(2):295–309.
Panina-Bordignon P, et al. Beta2-agonists prevent Th1 development by selective inhibition of interleukin 12. J Clin Investig. 1997;100(6):1513–9.
Swanson MA, Lee WT, Sanders VM. IFN-gamma production by Th1 cells generated from naive CD4+ T cells exposed to norepinephrine. J Immunol. 2001;166(1):232–40.
Qiao G, et al. β-Adrenergic signaling blocks murine CD8(+) T-cell metabolic reprogramming during activation: a mechanism for immunosuppression by adrenergic stress. Cancer Immunol Immunother. 2019;68(1):11–22.
McAlees JW, et al. Epigenetic regulation of beta2-adrenergic receptor expression in T(H)1 and T(H)2 cells. Brain Behav Immun. 2011;25(3):408–15.
Oliver E, Mayor F Jr, D’Ocon P. Beta-blockers: historical perspective and mechanisms of action. Revista Española de Cardiología (English Edition). 2019;72(10):853–62.
Drummond PD, et al. Up-regulation of cutaneous α1-adrenoceptors after a burn. Burns. 2015;41(6):1227–34.
Wijaya LK, Stumbles PA, Drummond PD. A positive feedback loop between alpha1-adrenoceptors and inflammatory cytokines in keratinocytes. Exp Cell Res. 2020;391(2).
Rough J, et al. Beta2 adrenoreceptor blockade attenuates the hyperinflammatory response induced by traumatic injury. Surgery. 2009;145(2):235–42.
Elenkov IJ, Wilder RL, Chrousos GP, Vizi ES. The sympathetic nerve–an integrative interface between two supersystems: the brain and the immune system. Pharmacol Rev. 2000;52(4):595–638.
Pastar I, et al. Epithelialization in wound healing: a comprehensive review. Adv Wound Care (New Rochelle). 2014;3(7):445–64.
Wu CS, Tsao DA, Chang HR. Beta2-adrenergic receptor agonist inhibits keratinocyte proliferation by mechanisms involving nitric oxide. Advances in Dermatology and Allergology/Postȩpy Dermatologii i Alergologii. 2021;38(3):396–396.
Chen J, Hoffman BB, Isseroff RR. Beta-adrenergic receptor activation inhibits keratinocyte migration via a cyclic adenosine monophosphate-independent mechanism. J Invest Dermatol. 2002;119(6):1261–8.
Sivamani RK, Porter SM, Isseroff RR. An epinephrine-dependent mechanism for the control of UV-induced pigmentation. J Invest Dermatol. 2009;129(3):784–7.
Fitsialos G, et al. Transcriptional signature of epidermal keratinocytes subjected to in vitro scratch wounding reveals selective roles for ERK1/2, p38, and phosphatidylinositol 3-kinase signaling pathways. J Biol Chem. 2007;282(20):15090–102.
Luqman A, Götz F. The ambivalent role of skin microbiota and adrenaline in wound healing and the interplay between them. Int J Mol Sci. 2021;22(9):4996.
Sivamani RK, et al. Acute wounding alters the beta2-adrenergic signaling and catecholamine synthetic pathways in keratinocytes. J Invest Dermatol. 2014;134(8):2258–66.
Berg T. β1-Blockers lower norepinephrine release by inhibiting presynaptic, facilitating β1-adrenoceptors in normotensive and hypertensive rats. Front Neurol. 2014;5:51.
Basu P, Martins-Green M. Signaling pathways associated with chronic wound progression: a systems biology approach. Antioxidants (Basel, Switzerland). 2022;11(8):1506.
El Ayadi A, et al. Beta-adrenergic receptor trafficking, degradation, and cell surface expression are altered in dermal fibroblasts from hypertrophic scars. J Invest Dermatol. 2018;138(7):1645–55.
Au K, Ehrlich HP. When the Smad signaling pathway is impaired, fibroblasts advance open wound contraction. Exp Mol Pathol. 2010;89(3):236–40.
Liao MH, et al. The stimulatory effects of alpha1-adrenergic receptors on TGF-beta1, IGF-1 and hyaluronan production in human skin fibroblasts. Cell Tissue Res. 2014;357(3):681–93.
Romana-Souza B, et al. Stress-induced epinephrine levels compromise murine dermal fibroblast activity through β-adrenoceptors. Exp Dermatol. 2011;20(5):413–9.
Fahy EJ, et al. Effects of β3 adrenergic receptor agonist treatment in murine full thickness dorsal cutaneous wounds. J Am Coll Surg. 2021;233(5):S197–8.
Slominski AT, et al. Sensing the environment: regulation of local and global homeostasis by the skin’s neuroendocrine system. Adv Anat Embryol Cell Biol. 2012;212:v, vii, 1-115.
Anesini C, Borda E. Modulatory effect of the adrenergic system upon fibroblast proliferation: participation of beta 3-adrenoceptors. Auton Autacoid Pharmacol. 2002;22(3):177–86.
Schena G, Caplan MJ. Everything you always wanted to know about β3-AR * (* but were afraid to ask). Cells. 2019;8(4):357.
Landén NX, Li D, Ståhle M. Transition from inflammation to proliferation: a critical step during wound healing. Cell Mol Life Sci. 2016;73(20):3861–85.
Gushiken LFS, et al. Cutaneous wound healing: an update from physiopathology to current therapies. Life. 2021;11(7):665–665.
Hinz B. Formation and function of the myofibroblast during tissue repair. J Investig Dermatol. 2007;127(3):526–37.
Le Provost GS, Pullar CE. β2-Adrenoceptor activation modulates skin wound healing processes to reduce scarring. J Investig Dermatol. 2015;135(1):279–88.
Chay A, et al. Control of βAR- and N-methyl-D-aspartate (NMDA) receptor-dependent cAMP dynamics in hippocampal neurons. PLoS Comput Biol. 2016;12(2):123–45.
Herndon D, et al. Reduced postburn hypertrophic scarring and improved physical recovery with yearlong administration of oxandrolone and propranolol. Ann Surg. 2018;268(3):431–41.
O’Leary AP, Fox JM, Pullar CE. Beta-adrenoceptor activation reduces both dermal microvascular endothelial cell migration via a cAMP-dependent mechanism and wound angiogenesis. J Cell Physiol. 2015;230(2):356–65.
Xanthopoulos A, Daskalopoulou I, Frountzi S, Papadimitriou E. A systematic review on the role of adrenergic receptors in angiogenesis regulation in health and disease. International Journal of Translational Medicine. 2021;1(3):353–65.
Droho S, Cuda CM, Perlman H, Lavine JA. Monocyte-derived macrophages are necessary for beta-adrenergic receptor-driven choroidal neovascularization inhibition. Invest Ophthalmol Vis Sci. 2019;60(15):5059–69.
Ciccarelli M, et al. Impaired neoangiogenesis in β2–adrenoceptor gene-deficient mice: restoration by intravascular human β2–adrenoceptor gene transfer and role of NFκB and CREB transcription factors. Br J Pharmacol. 2011;162(3):712–712.
Eming SA, Brachvogel B, Odorisio T, Koch M. Regulation of angiogenesis: wound healing as a model. Prog Histochem Cytochem. 2007;42(3):115–70.
López-López N, et al. Expression and vitamin D-mediated regulation of matrix metalloproteinases (MMPs) and tissue inhibitors of metalloproteinases (TIMPs) in healthy skin and in diabetic foot ulcers. Arch Dermatol Res. 2014;306(9):809–21.
Caley MP, Martins VL, O’Toole EA. Metalloproteinases and wound healing. Adv Wound Care (New Rochelle). 2015;4(4):225–34.
Uzunlar O, et al. Effects of repeated propranolol administration in a rat model of surgically induced endometriosis. Eur J Obstet Gynecol Reprod Biol. 2014;182:167–71.
Rietz A, Spiers J. The relationship between the MMP system, adrenoceptors and phosphoprotein phosphatases. Br J Pharmacol. 2012;166(4):1225–43.
Abisado RG, et al. Bacterial quorum sensing and microbial community interactions. 2018;3(10):128. https://doi.org/10.1128/mbio.02331-17.
Almalki AJ, et al. Computational and biological evaluation of beta-adrenoreceptor blockers as promising bacterial anti-virulence agents. Pharmaceuticals. 2022;15(2):110. https://doi.org/10.3390/ph15020110.
Freestone PP, et al. Pseudomonas aeruginosa-catecholamine inotrope interactions: a contributory factor in the development of ventilator-associated pneumonia? Chest. 2012;142(5):1200–10.
Luqman A, et al. SadA-expressing staphylococci in the human gut show increased cell adherence and internalization. Cell Rep. 2018;22(2):535–45.
• Luqman A, et al. The neuromodulator-encoding sadA gene is widely distributed in the human skin microbiome. Front Microbiol. 2020;11:573679. Pre-clinical study demonstrating the distribution of sadA gene in the cutaneous microbiome, the role of TAs, catecholamines, and the potential opportunity to use this pathway as in wound healing therapeutics.
Luqman A, et al. A new host cell internalisation pathway for SadA-expressing staphylococci triggered by excreted neurochemicals. Cell Microbiol. 2019;21(9):e13044.
Luqman A, et al. Trace amines produced by skin bacteria accelerate wound healing in mice. Commun Biol. 2020;3(1):277.
Kleinau G, et al. Differential modulation of beta-adrenergic receptor signaling by trace amine-associated receptor 1 agonists. PLoS ONE. 2011;6(10):e27073.
Luqman A, Kharisma VD, Ruiz RA, Götz F. In silico and in vitro study of trace amines (TA) and dopamine (DOP) interaction with human alpha 1-adrenergic receptor and the bacterial adrenergic receptor QseC. Cell Physiol Biochem. 2020;54(5):888–98.
Diban F, et al. Biofilms in chronic wound infections: innovative antimicrobial approaches using the in vitro Lubbock chronic wound biofilm model. Int J Mol Sci. 2023;24(2):1004.
Versey Z, et al. Biofilm-innate immune interface: contribution to chronic wound formation. Front Immunol. 2021;12:648554.
Gajula B, Munnamgi S, Basu S. How bacterial biofilms affect chronic wound healing: a narrative review. IJS Global Health. 2020;3(2):e16.
Cambronel M, et al. Epinephrine affects motility, and increases adhesion, biofilm and virulence of Pseudomonas aeruginosa H103. Sci Rep. 2019;9(1):20203.
Scardaci R, et al. Norepinephrine and serotonin can modulate the behavior of the probiotic Enterococcus faecium NCIMB10415 towards the host: is a putative surface sensor involved? Microorganisms. 2022;10(3):487.
Cambronel M, et al. Influence of catecholamines (epinephrine/norepinephrine) on biofilm formation and adhesion in pathogenic and probiotic strains of Enterococcus faecalis. Front Microbiol. 2020;11:1501.
Hsiao YW, Huang YC. Is the combination of cryotherapy and topical timolol solution superior to cryotherapy alone in the treatment of epidermal growth factor receptor inhibitor-induced paronychia? A double-blinded, left-to-right comparison, randomized controlled trial. J Am Acad Dermatol. 2023;89(5):1049–50. https://doi.org/10.1016/j.jaad.2023.06.040.
Patra AC, et al. Effectiveness and safety of 0.5% timolol solution in the treatment of pyogenic granuloma: a randomized, double-blind and placebo-controlled study. Indian J Dermatol Venereol Leprol. 2022;88(4):500–8.
Nabi-Meybodi M, et al. Effects of topical timolol for the prevention of radiation-induced dermatitis in breast cancer: a pilot triple-blind, placebo-controlled trial. BMC Cancer. 2022;22(1):1079.
Kimwattananukul K, Noppakun N, Asawanonda P, Kumtornrut C. Topical 0.5% timolol maleate significantly enhances skin-barrier restoration after fractional carbon dioxide laser treatment for acne scars. Lasers Surg Med. 2021;53(5):610–5.
Joo JS, Isseroff RR. Application of topical timolol after CO2 laser resurfacing expedites healing. Dermatol Surg. 2021;47(3):429–31.
Hawwas ARM, Mohamed HAK, Sayedahmed OME, Elsaie ML. Topical timolol maleate 0.5% after fractional carbon dioxide laser versus fractional carbon dioxide laser alone in treatment of acne scars: split face comparative study. Sci Rep. 2023;13(1):9402.
Dabiri G, et al. Topical timolol may improve overall scar cosmesis in acute surgical wounds. Cutis. 2017;100(1):E27-e28.
Ghassemi M, et al. Efficacy and safety of topical timolol 0.5% plus saline 0.9% versus each one alone in acne scar trichloroacetic acid-CROSS therapy: a blinded randomized controlled trial. Dermatol Therapy. 2022;35(4):e15341.
• Kaur R, et al. Beta-adrenergic antagonist for the healing of chronic diabetic foot ulcers: study protocol for a prospective, randomized, double-blinded, controlled and parallel-group study. Trials. 2020;21(1). Five-year long clinical trial evaluating the efficacy of topical TM vs SOC in DFUs.
Schmults CD, Brigham and Women's Hospital. Efficacy and safety of 0.25% timolol gel in healing surgical open wounds: a randomized controlled trial. Interventional (Phase 2/Phase 3). Identifier NCT03452072. Accessed August 26, 2023. https://www.medifind.com/articles/clinical-trial/6604520.
LeBlanc KG, Dickerson TG. Topical timolol: a comparison of surgical outcomes. 2021. Identifier NCT05114239. Accessed August 20, 2023. https://clinicaltrials.gov/ct2/show/NCT05114239.
Anees N, Zagazig University. The role of topical timolol 0.5% in wound healing and scar improvement following atrophic acne scar microneedling. ClinicalTrials.gov Identifier: NCT05597813. Not yet recruiting. Estimated study start date: March 1, 2023; Estimated primary completion date: October 1, 2023; Estimated study completion date: November 1, 2023. Accessed August 26, 2023. https://classic.clinicaltrials.gov/ct2/show/NCT05597813.
Thomas B, et al. Topical timolol promotes healing of chronic leg ulcer. J Vasc Surg Venous Lymphat Disord. 2017;5(6):844–50.
Hwang AS, Yang YW, Mangold AR. 28228 Effects of timolol on wound healing: a single-center retrospective study. J Am Acad Dermatol. 2021;85(3):AB42.
Larsen L, et al. Combination therapy of autologous adipose mesenchymal stem cell-enriched, high-density lipoaspirate and topical timolol for healing chronic wounds. J Tissue Eng Regen Med. 2018;12(1):186–90.
Gallegos AC, et al. Absorption and safety of topically applied timolol for treatment of chronic cutaneous wounds. Adv Wound Care (New Rochelle). 2019;8(11):538–45.
Vestita M, et al. Abstract: efficacy, safety and costs of 0.1% timolol gel in healing. Plast Reconstr Surg Glob Open. 2017;5(9 Suppl):139–40.
Vestita M, Filoni A, Bonamonte D, Annoscia P, Giudice G. Topical 0.5% timolol for chronic refractory wounds: an observational prospective study. Plast Reconstr Surg Glob Open. 2017;5(9S):21. https://doi.org/10.1097/01.GOX.0000526190.20003.08.
Manahan MN, et al. Topical timolol for a chronic ulcer — a case with its own control. Med J Aust. 2014;200(1):49–50.
Braun LR, Lamel SA, Richmond NA, Kirsner RS. Topical timolol for recalcitrant wounds. JAMA Dermatol. 2013;149(12):1400–2.
Bhatia R, et al. Treatment of posttraumatic reactive angioendotheliomatosis with topical timolol maleate. JAMA Dermatol. 2021;157(8):1002–4.
Waldman RA, Lin G, Sloan B. Clinical pearl: topical timolol for refractory hypergranulation. Cutis. 2019;104(2):118–9.
Beroukhim K, Rotunda AM. Topical 0.5% timolol heals a recalcitrant irradiated surgical scalp wound. Dermatol Surg. 2014;40(8):924–6.
Alsaidan MS, Aljarbou OZ, Alajroush W. Kaposi sarcoma in a child after fanconi anemia-induced haploidentical hematopoietic stem cell transplant: a case report. Children (Basel, Switzerland). 2023;10(2):188.
Chiaverini C, Passeron T, Lacour JP. Topical timolol for chronic wounds in patients with junctional epidermolysis bullosa. J Am Acad Dermatol. 2016;75(6):e223–4.
Alsaad AMS, Alsaad SM, Fathaddin A, Al-Khenaizan S. Topical timolol for vasculitis ulcer: a potential healing approach. JAAD Case Rep. 2019;5(9):812–4.
Yang Y, Hoss E, Pittelkow M. Treatment of hydroxyurea-induced ulcers with topical timolol. J Am Acad Dermatol. 2018;79(3):AB301.
Pawar MK. Treatment of painful and deep fissures of the heel with topical timolol. J Am Acad Dermatol. 2021;85(1):e3–4.
Pawar M. Topical timolol in chronic, recalcitrant fissures and erosions of hand eczema. J Am Acad Dermatol. 2021;84(3):e125–6.
Dave DD, et al. Topical Timolol for ingrown nail post-avulsion refractory wound. Dermatol Ther. 2022;35(6):e15493–e15493.
Sollena P, et al. Efficacy of topical beta-blockers in the management of EGFR-inhibitor induced paronychia and pyogenic granuloma-like lesions: case series and review of the literature. Drugs Context. 2019;8:212613.
Cubiró X, Planas-Ciudad S, Garcia-Muret MP, Puig L. Topical timolol for paronychia and pseudopyogenic granuloma in patients treated with epidermal growth factor receptor inhibitors and capecitabine. JAMA Dermatol. 2018;154(1):99–100.
Chen X, Guffey DJ. Topical timolol for treatment of persistent granulation tissue in the setting of severe hidradenitis suppurativa. Dermatol Online J. 2019;25(11).
Hwang AS, Yang YW, Mangold AR. Effects of timolol on wound healing: A single-center retrospective study. J Am Acad Dermatol. 2021;85(3, Suppl):AB42. doi:10.1016/j.jaad.2021.06.193.
Poulose D, Lote S, Mahajan A, Gogineni JM. Nonselective beta-blockers for the efficacious healing of ulcerated infantile hemangiomas in unusual locations of two female infants. Cureus. 2021;13(7):e16683.
Provvidenziale L, Russo F, Taddeucci P, Rubegni P. Treatment of childhood pyogenic granuloma of the nail bed with topical timolol. Dermatol Ther. 2020;33(4):e13710.
Ebrahimi Z, et al. Oral propranolol and topical timolol in the treatment of post-burn pyogenic granuloma: two cases and a review of the literature. Clin Case Rep. 2022;10(11):e6538.
Guedes Neto HJ, et al. What do Cochrane systematic reviews say about congenital vascular anomalies and hemangiomas? A narrative review. Sao Paulo Med J. 2022;140(2):320–7.
Goodarzi A, et al. The role of topical timolol in wound healing and the treatment of vascular lesions: a narrative review. Dermatol Ther. 2021;34(2):e14847–e14847.
Lin Z, Zhang B, Yu Z, Li H. The effectiveness and safety of topical β-receptor blocker in treating superficial infantile haemangiomas: a meta-analysis including 20 studies. Br J Clin Pharmacol. 2020;86(2):199–209.
Huang H, et al. Comparison of the efficacy and safety of lasers, topical timolol, and combination therapy for the treatment of infantile hemangioma: a meta-analysis of 10 studies. Dermatol Ther. 2022;35(12):e15907.
• Yoon DJ, et al. Repurposing ophthalmologic timolol for dermatologic use: caveats and historical review of adverse events. Am J Clin Dermatol. 2021;22(1):89–99. A narrative review that also provides a clinical algorithm for the use of topical TM in dermatology and stratification of potential risk for AEs.
Jain N, Ganjoo S. A few drops may go a long way: topical timolol in pediatric dermatology. Indian J Pediatr. 2022;23(3):260–4.
Yoon DJ, et al. Adverse effects of topical timolol: safety concerns and implications for dermatologic use. J Am Acad Dermatol. 2021;84(1):199–200.
Uusitalo H, et al. Improved systemic safety and risk-benefit ratio of topical 0.1% timolol hydrogel compared with 0.5% timolol aqueous solution in the treatment of glaucoma. Graefes Arch Clin Exp Ophthalmol. 2006;244(11):1491–6.
Administration UFaD. (2023). FDA Adverse Event Reporting System (FAERS) public dashboard. Available from: https://www.fda.gov/drugs/questions-and-answers-fdas-adverse-event-reporting-system-faers/fda-adverse-event-reporting-system-faers-public-dashboard.
Sidjanin DJ, et al. Pharmacogenetics of ophthalmic topical beta-blockers. Per Med. 2008;5(4):377–85.
Zhou SF. Polymorphism of human cytochrome P450 2D6 and its clinical significance: Part I. Clin Pharmacokinet. 2009;48(11):689–723.
Edeki TI, He H, Wood AJ. Pharmacogenetic explanation for excessive beta-blockade following timolol eye drops. Potential for oral-ophthalmic drug interaction Jama. 1995;274(20):1611–3.
Noble SL, King DS, Olutade JI. Cyclooxygenase-2 enzyme inhibitors: place in therapy. Am Fam Physician. 2000;61(12):3669–76.
Ishii Y, et al. Drug interaction between cimetidine and timolol ophthalmic solution: effect on heart rate and intraocular pressure in healthy Japanese volunteers. J Clin Pharmacol. 2000;40(2):193–9.
Mäenpää J, et al. Paroxetine markedly increases plasma concentrations of ophthalmic timolol; CYP2D6 inhibitors may increase the risk of cardiovascular adverse effects of 0.5% timolol eye drops. Drug Metab Dispos. 2014;42(12):2068–76.
Volotinen M, et al. Effects of selective serotonin reuptake inhibitors on timolol metabolism in human liver microsomes and cryo-preserved hepatocytes. Basic Clin Pharmacol Toxicol. 2010;106(4):302–9.
Author information
Authors and Affiliations
Contributions
Rawlings E. Lyle: Rawlings drafted, edited and revised the article, developed Tables 1–4, and aided in approving the final version for publication. Anuj Budhiraja: Contributed to Tables 1–4. Alisha Mehta: Contributed to Tables 1–4. Dr. Sara E. Dahle, DPM.: Revised the article, oversaw the review process, and approved the final version for publication. Dr. R. Rivkah Isseroff, MD: Edited and revised the article, provided oversight for the project, directed the research, and approved the final version for publication.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any primary study material with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lyle, R.E., Budhiraja, A., Mehta, A. et al. The Use of Timolol for Wound Healing—A Review. Curr Derm Rep 13, 8–27 (2024). https://doi.org/10.1007/s13671-024-00421-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13671-024-00421-3