Abstract
Purpose of Review
Skin cancers account for more than 40% of all cancers in the USA and continue to rise in incidence. It is prudent to understand the current burden and pathogenesis of photocarcinogenesis and preventive measures.
Recent Findings
Insights into recently discovered mechanisms have paved way for potential targets for prevention and therapeutics. Nicotinamide has shown promising results as an oral chemopreventive agent. UVB affects the DHODH pathway of pyrimidine synthesis via STAT 3. DHODH inhibition by leflunomide may be a potential targeted chemoprevention strategy. A photolyase containing sunscreen, which repairs UV-damaged DNA, effectively reduced new precancerous lesions. Several antioxidants and anti-inflammatory agents including many phytochemicals ameliorate the process of photocarcinogenesis in preclinical and clinical studies, e.g., green tea polyphenols, Polypodium leucotomos extract, and Timosaponin A III. Diet can potentially affect skin cancer risk by its ability to modify oxidative stress and cell signaling pathways.
Summary
Photocarcinogenesis is a multi-step process. An in-depth understanding is instrumental in development of novel agents for prevention and treatment of skin cancers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In an era in which the incidence of most forms of cancer has either stabilized or is decreasing, the incidence of basal cell and cutaneous squamous cell carcinoma, grouped together under the term keratinocyte carcinoma (KC), is increasing globally. Predictions are that, in the USA alone, over 5 million KCs are diagnosed each year [1]. This is greater than the incidence of cancers in all other organs combined. It is predicted that one in five Americans will develop at least one KC in their lifetime [2]. Although once considered to be a disease of seniors, BCCs and SCCs are being diagnosed with increasing frequency in younger and younger ages [3]. It is not unusual for people in their 20s and 30s to be treated for one or more KCs.
The mortality rate of KCs is small with an estimated age-adjusted mortality rate of 0.12 and 0.3 per 100,000 for BCC and SCC respectively [1, 4]. The risk of metastases in squamous cell carcinoma ranges from 0.5 to 3.3%. Basal cell carcinomas have significantly lower mortality and risk of generalized dissemination (< 0.1%); however, there have been occasional reports of metastases to the lymph nodes, lungs, liver, and bone. Although the mortality is low, these tumors can produce extensive local tissue damage and thereby cause considerable morbidity. KCs are located primarily on exposed areas of skin; treatment is mostly surgical and this often leads to significant scarring in cosmetically sensitive areas. In addition, UV-induced skin cancer and its precursors are an escalating economic burden [1]. The direct cost of medical care and indirect cost resulting from potential loss of productivity amount to a considerable financial burden. In the USA alone, the estimated annual medical expenditure on KC diagnosis and treatment exceeds $8 billion per year.
Solar ultraviolet radiation is the major environmental agent responsible for cutaneous squamous cell carcinomas, basal cell carcinomas, and pre-malignant actinic (solar) keratoses. It also is an important etiologic agent for melanomas and Merkel cell carcinoma Thus, because of the importance of the problem and because of the need for better methods for their prevention and treatment, there has been considerable interest in identifying the mechanisms by which UV-induced malignancies and pre-malignancies are produced.
Mechanisms of Photocarcinogenesis
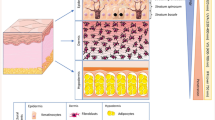
Studies over the past several decades have carefully defined the steps by which sunlight and artificial UV radiation sources cause KCs, a discipline called photocarcinogenesis. As a result of these studies, it is now known that cutaneous BCCs and SCCs develop through a systematic sequence of events in which molecular and biochemical changes accumulate in target keratinocytes over prolonged intervals. These phases have been termed initiation, promotion, and progression (see Fig. 1). The changes correlate exceedingly well with the progression of clinical and histological features from UV damage to invasive carcinomas. Although grouped together under a common term, it is important to note that BCCs and SCCs are individual neoplasms with their own clinical and histological features, different cells of origin, distinct mutations, and separate behaviors. For example, while intermittent and recreational sunlight exposure early in life is a risk factor for BCCs, chronic long-term solar damage is more strongly associated with SCC [5].
Spectrum of Wavelength and Sources of UV Exposure
For photocarcinogenesis to proceed, epidermal keratinocytes must be damaged by exposure to the appropriate wavelengths and doses of electromagnetic radiation. Blum was first to demonstrate that wavelengths within the UVB range (290–320 nm) were the most effective at the production of skin cancer [6]. He showed that interposition of plate glass, which filters out most UVB (but not UVA [320–400 nm]), between the artificial broadband UV light source and the mice being irradiated was sufficient to block the carcinogenic effect of the light source. In other studies, Setlow showed that wavelengths within the UVB range were 100–1000 times more mutagenic than UVA [7]. This was further confirmed by Freeman, who found that the same wavelengths that caused DNA damage also caused skin cancers in mice [8]. Although UVA in the absence of photosensitizers is capable of producing skin cancer in animal models, it requires a much higher dose and a longer duration of exposure [9]. Despite the fact that UVA is less potent than UVB, there is growing concern about the contribution of UVA to the development of skin cancers. First, although UVB wavelengths are primarily responsible for BCC and SCC, the wavelengths necessary for production of melanomas are not as well defined. Evidence from epidemiologic and preclinical studies suggests that UVA and even visible wavelengths may contribute in a significant way to melanoma development [10,11,12]. Second, tanning beds, popularly used to achieve an artificial tan, emit 10 times the amount of UVA compared with solar radiation. The odds ratio for developing melanoma in tanning bed users (highest tertile of use vs. never use) is 1.32 (95% confidence interval (CI): 1.08, 1.63) [13•]. The relative risk in tanning bed users (ever vs. never use) of developing BCC and SCC is 1.29 (95% CI = 1.08–1.53) and 1.67 (95% CI = 1.29–2.17) respectively [14]. Finally, chronic use of selected medications which absorb UVA wavelengths increases the risk of BCCs and SCCs. Stern et al. found an increased risk of SCCs (30×) and BCCs (5×) in those treated with PUVA (Psoralen and UVA), which was proportional to the total number of treatment sessions [15]. Voriconazole is another photosensitizing drug that has been associated with cutaneous squamous cell carcinomas [16]. Epidemiological studies on the use of other photosensitizing medications and an increased risk of cancer have been conflicting [17,18,19]. Diets rich in furocoumarins, naturally occurring chemicals in citrus products, can enhance UVA absorption [20]. Alcohol consumption also can increase the risk of BCCs by direct mutagenic and immunosuppressive mechanisms [21].
Initiation Stage of Photocarcinogenesis
UV-induced DNA mutations in keratinocytes are the most important event that occurs during the initiation stage of photocarcinogenesis. Although UV radiation alters the structure of many molecules within the cell, including proteins and lipids, it is photochemical changes in DNA that are the most important for initiation of photocarcinogenesis [22]. UV radiation produces distinctive mutations that distinguishes it from other forms of DNA damage. The UV signature mutations are characterized by C → T or CC → TT mutations. They are useful experimental markers for research. The photoproducts that result include cyclobutane pyrimidine dimers (CPDs), 6-4 pyrimidine-pyrimidone photoproducts (6-4PPs), and Dewar isomers. Of these, CPDs are the most important and the most abundant, comprising 80% of all photoproduct mutations. Their abundance is due in part to the fact that they are repaired more slowly than 6-4PPs. 6-4PPs can also photoisomerize to Dewar isomers which are less mutagenic. The UV signature mutations elude DNA repair enzymes as they resemble newly synthesized DNA, thereby making the initiation phase irreversible.
UVB has been shown to upregulate dihydroorotate dehydrogenase (DHODH), an enzyme located in the inner mitochondrial membrane which is important for synthesis of pyrimidine and its derivatives. Hosseini et al. showed that UVB irradiation results in DHODH upregulation via STAT3 signaling. Mice treated with the DHODH inhibitor leflunomide have reduced UVB-induced tumor formation, an effect which is reversed by pyrimidine supplementation. This could be a promising target for chemoprevention of skin cancers [23••].
For decades, CPDs were considered to be caused solely by UVB. CPDs are also the most important photoproduct of UVA radiation as well [24]. Even though UVA is significantly less effective than UVB in causing direct DNA damage, its relative abundance in sunlight and its use for therapeutic and recreational purposes make it an important offender. UVA is also responsible for oxidative damage by formation of reactive oxygen species which react with guanine. The result is formation of oxidation products (8-hydroxy-deoxyguanosine adducts) which cause transversion (G → T or T → G). However, these are less abundant than CPDs.
When DNA is damaged in keratinocytes, there is an active attempt to repair it by many different mechanisms. DNA repair processes are very efficient with only a small fraction going unrepaired. The repair process includes nucleotide excision repair (for bulky CPDs and 6-4PPs) and base excision repair (non-bulky oxidative DNA changes) [25]. A number of enzymes facilitate this process. A defect in any of these enzymes can result in an increased risk of skin cancers and/or photosensitivity. The importance of DNA repair processes in protection from skin cancer is exemplified by the disease xeroderma pigmentosum (XP). XP is an autosomal recessive genodermatosis in which individuals are predisposed to UV-induced photodamage and the development of early-onset BCC, SCC, and melanoma [26]. There are several complementation groups, XPA-XPG, each of which is caused by a defect in one of the enzymes in the global genome nucleotide excision repair pathway. A bypass mechanism for unrepaired photoproducts utilizes DNA polymerase η which is deficient in XP variant.
Although DNA repair processes work exceedingly well, they do not work perfectly. Mutations in p53 and the sonic hedgehog pathway (SHH) are most relevant with respect to photocarcinogenesis. PTCH1, suppressor of fused (SUFU), and smoothened (SMO) proteins are all protein participants in the SHH pathway [27]. During embryogenesis, this pathway regulates cell growth and differentiation but is not typically active after birth [28]. Postnatal activation causes BCCs in basal cell nevus syndrome and chronic UV radiation [29]. BCNS is caused by a mutation in the PTCH1 gene which results in unrestricted activation of the hedgehog pathway and, among other clinical manifestations, the development of large numbers of BCC [29]. Mutations in the SHH pathway are required for BCC, but do not contribute to SCCs.
The p53 protein is instrumental in directing repair of DNA damage or, if the damage is too severe, guiding the cell towards apoptosis. Mutations in p53 have been identified in 50% of BCCs and 90% of SCCs [30].
Promotion Stage of Photocarcinogenesis
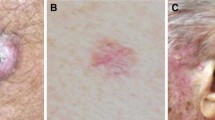
Upon repeated UV exposure, mutant keratinocytes that develop during the initiation stage have a selective proliferative advantage over normal keratinocytes. When chronically sun-damaged skin is examined with immunohistochemistry, mutant clones of cells are present [31]. Another characteristic of the promotion stage is the presence of inflammation. The end result of promotion is the presence of small foci of clinically apparent pre-malignant actinic keratoses.
The generation of reactive oxygen intermediates is involved in the process and efforts to inhibit their activity have proved to be helpful in preventing the development of UV-induced skin cancers in animal models [32, 33]. Another effect of UV radiation is activation of protein kinase C. PKC actually refers to a family of molecules [34]. Of particular interest to skin carcinogenesis are the PKCα and PKCε isoforms [35, 36]. PKCs have a number of biological effects on keratinocytes, including stimulation of the inflammatory response and augmentation of cell proliferation. This is particularly true of mutant keratinocytes, since they have a proliferative advantage.
Another biochemical feature that has been associated with the promotion stage is increased activity of the enzyme ornithine decarboxylase (ODC) [37]. ODC is the rate-limiting enzyme in the polyamine biosynthetic pathway. Polyamines increase keratinocyte proliferation. Eflornithine (also known as difluoromethylornithine [DFMO]) is an inhibitor of ODC, and when this compound is administered to animals receiving chronic UV exposure, fewer tumors develop [38].
Progression Stage of Photocarcinogenesis
During the progression stage, UV radiation produces additional genetic and biochemical changes which allow pre-malignant actinic keratoses to become invasive squamous cell carcinomas. Among the activities associated with the progression stage are epithelial-mesenchymal transition (EMT) [39] and activation of cyclooxygenase-2 (COX-2) [40,41,42, 43••]. EMT is the process by which cells in pre-malignant AKs and KCs lose expression of E-cadherin, a surface molecule necessary for cell-to-cell adhesion. As a result, there is an increase in the migratory activity and invasiveness of the mutant keratinocytes [44].
COX-2 is the rate-limiting enzyme in prostaglandin synthesis. Prostaglandins contribute to photocarcinogenesis through many actions, not only in the progression stage but also at other points in UV-induced skin cancer development. Among its actions are to promote EMT, augment the inflammatory response, inhibit immunity to tumor antigens, and stimulate angiogenesis [45].
The Immune System and Photocarcinogenesis
There is ample evidence that UV-induced photocarcinogenesis and immunosuppression are closely related. The experimental basis for this conclusion comes from observations made by Kripke in mice [46]. Mice that were chronically irradiated had their tumors excised. The tumors were then transplanted to genetically identical recipients. The tumors initially engrafted but within a few weeks were destroyed by the host’s immune response. However, when the same tumors were placed on mice that had been given subcarcinogenic UV doses, the tumors were not immunologically rejected, grew progressively, and ultimately killed their host. Thus, among the various actions of UV radiation is suppression of host immune responses that destroy mutant keratinocytes before they become invasive tumors.
Clinical observations also support the concept that UV-induced tumors are highly immunogenic and that evading the immune response is instrumental for their development. (1) KCs occur more frequently in people who receive immunosuppressive medications. Up to 70% of allogeneic kidney transplant recipients, who require immunosuppressive therapy to prevent organ rejection, will develop at least one non-melanoma skin cancer within 20 years [47]. Lymphoma and chronic lymphocytic leukemia patients, who, because of their disease, are immunosuppressed, also are at greater risk of being diagnosed with BCCs and SCCs [48]. (2) Skin cancer patients who have no underlying condition have been observed to have diminished reactions to skin test antigens and have a decreased likelihood of developing immunity to the contact allergen dinitrochlorobenzene (DNCB) [49]. (3) Microscopic examination reveals an increased number of regulatory T cells in the inflammatory infiltrate of BCCs [50]. (4) Patients treated with psoralen plus UVA photochemotherapy (PUVA) have reduced sensitization rates to contact allergens like mustine [51, 52].
Natural History of AKS and Non-melanoma Skin Cancers
A number of studies have investigated the natural history of pre-malignant actinic keratoses and their likelihood of developing into squamous cell carcinomas. The majority of AKs never progress to become invasiv+e squamous cell carcinoma. The relative risk of this occurrence increases proportionately with the burden of AKs, with the relative risk being < 1% for 5 or fewer lesions and 20% for > 20 AKs [53]. In studies in which AKs have been followed over several months, 30–40% of AKs regress and the same ones that have regressed can recur [54••]. Regression of AKs was associated with a loss of mutant p53 and an increase in E-cadherin expression. Conversely, progression from sun-exposed skin to AKs correlated with an increase in p53 and a loss of E-cadherin. These observations provide evidence that photocarcinogenesis is a dynamic process in which progression or regression can occur. This indicates that it is possible to intervene to prevent photocarcinogenesis from proceeding to the point of invasive malignancy.
Prevention and Treatment
One of the goals of a thorough investigation of the pathogenesis of UV-induced skin cancer is to devise better methods for its prevention and treatment. Based on the research into the various stages of photocarcinogenesis, several treatments have entered clinical trials and have been shown to be effective preventive agents in humans.
Agents that Target the Initiation Stage of Photocarcinogenesis
Several agents that target the DNA damage and its repair have been identified and show efficacy in human clinical trials. These include T4 endonuclease V (dimericine), photolyase, nicotinamide, and vismodegib.
T4 Endonuclease V (Dimericine)
T4 endonuclease V, also known as dimericine, is a bacterial enzyme that removes cyclobutane pyrimidine dimers from DNA by base excision repair. When incorporated into liposomes and applied to the skin, this DNA repair enzyme is readily absorbed by keratinocytes and Langerhans cells, quickly exerting its effect without any significant toxicities [55]. As was mentioned previously, xeroderma pigmentosum (XP) is a disease in which DNA repair is defective and this predisposes patients to large numbers of UV-induced skin cancers [56]. In XP patients treated with dimericine lotion, there was a 68% reduction in new AKs and a 30% reduction in BCCs compared with placebo [57].
Photolyase
In plants and algae, the enzyme photolyase is particularly important in the repairing of UV-induced damage. Preliminary clinical trials have shown that treatment with a photolyase containing sunscreen produced > 75% reduction in new AKs without any serious adverse effects [58•, 59].
Nicotinamide
Nicotinamide is a derivative of vitamin B3 (also known as niacin) in which an amide group has been added. Niacin is a component of nicotinamide adenine dinucleotide (NAD), which increases cellular ATP and enhances DNA repair [60, 61] while simultaneously reducing UV-induced immunosuppression [62]. A double-blind randomized clinical trial of nicotinamide 500 mg twice daily for 12 months in 386 participants with at least two non-melanoma skin cancers in the previous 5 years resulted in a 23% reduction in non-melanoma skin cancers compared with placebo (95% CI, 4–38; P = 0.02) [63••]. There were statistically significant reductions in SCC (30% reduction; 95% CI, 0–51; P = 0.05) and in AKs (P ≤ 0.01). There were no significant differences for BCC (20% reduction; 95% CI, − 6–39; P = 0.12). There were no serious toxicities [63••].
Vismodegib and Sonidegib
Vismodegib and sonidegib are competitive inhibitors of the smoothened protein (SMO), one of the major proteins in the SHH pathway. They, thus, inhibit the biological effects of the SHH pathway. Vismodegib and sonidegib are effective treatments for advanced and metastatic BCCs [64, 65, 66••]. In a multicenter, double-blind trial comparing two different doses of sonidegib, both 200 and 800 mg daily produced an objective response in over one-third of individuals with locally advanced or metastatic BCC [67]. Similarly, in a multinational, phase II trial in which patients with inoperable locally invasive or metastatic BCC received vismodegib 150 mg per day, objective response rate was 33.3% in patients with metastatic disease, and 47.6% in patients with the locally advanced form 12 months after primary analysis, demonstrating durability of response [68••]. Vismodegib has also been used to prevent new skin cancers in patients with basal cell nevus syndrome [69]. In a randomized, double-blind, controlled trial of 41 patients that received vismodegib for 8 months, subjects treated with vismodegib had > 90% reduction in new BCCs compared with controls (2 vs 29; P < 0.001). However, vismodegib and sonidegib have a number of side effects (loss of taste, muscle cramps, alopecia, and weight loss), which limit their widespread use as therapeutic and chemopreventive agents.
Agents that Target the Promotion Stage of Photocarcinogenesis
Low-Fat Diet
There is substantial evidence that a high-fat diet contributes to the development of several different types of cancer. Its role in NMSC was investigated in a randomized, controlled clinical trial in which dietary fat intake was restricted to 20% of total calories [70]. These individuals were compared with those on an unrestricted diet in which the fat content was estimated to be 37–40% of total calories. After 24 months, those on the low-fat diet developed significantly fewer AKs and NMSCs than those with an unrestricted diet. The mechanism by which a low-fat diet inhibits skin cancer development has been evaluated in animal models. Animals on a high-fat diet exhibited augmented levels of COX-2, prostaglandin E2, and NF-κB compared with controls [71].
Retinoids
Retinoids, chemical derivatives of vitamin A, limit cell growth and enhance differentiation. Preclinical studies which showed retinoid inhibition of skin cancer development were the impetus for clinical trials examining topical and systemic retinoids for skin cancer prevention. An 8-month trial of high-dose isotretinoin (average 3.1 mg/kg/day) markedly reduced new skin cancers in some patients while on treatment. Patients only benefitted while they were taking the oral retinoids, and there was a rebound once they discontinued them [72]. Treatment at this dose was associated with intolerable side effects, including mucocutaneous toxicity and hypertriglyceridemia. Lower doses of retinoids have not been effective at lowering skin cancer rates in otherwise healthy individuals [73]. On the other hand, oral retinoids, acitretin in particular, are effective at preventing skin cancer in selected patient populations. They reduce SCCs in psoriatic patients previously treated with PUVA, in organ transplant recipients, and in patients with xeroderma pigmentosum [74,75,76,77]. Retinoids do not significantly reduce BCC or melanomas, however.
Topical retinoids are not beneficial in preventing skin cancer. In a multi-institutional randomized, double-blind placebo-controlled trial in veterans treated with tretinoin cream 0.1% or placebo twice daily to the face and ears for 4 weeks, there was no reduction in skin cancers compared with controls [78].
Difluoromethylornithine
Difluoromethylornithine (DFMO) is an irreversible inhibitor of the enzyme ODC and thereby prevents activation of the polyamine biosynthetic pathway, an important step in tumor promotion. When given orally, it has excellent bioavailability. In a randomized, double-blind, placebo-controlled trial in nearly 200 patients who were followed for up to 4 years, there was a statistically significant 30% reduction in BCCs compared with control [79]. In another clinical trial with 209 subjects at risk for KCs, there was a decrease in new KCs, although it did not reach clinical significance. The reduction continued for more than 5 years after completion of treatment [80].
Agents that Target the Progression Stage of Photocarcinogenesis
Cyclooxygenase 2 Inhibitors
Because celecoxib is a selective COX-2 antagonist that has received FDA approval for rheumatoid arthritis, osteoarthritis, and familial adenomatous polyposis of the colon, and due to the knowledge that COX-2 is involved in UV-induced skin tumorigenesis, celecoxib was evaluated for its potential to prevent KCs in a multicenter, double-blind, placebo-controlled, randomized trial involving 240 participants. At a dose of 200 mg celecoxib twice daily for 9 months, there was a statistically significant 59% reduction in both BCCs and SCCs [81]. There was no effect on AKs. Although there was not an increased incidence of serious adverse effects in the study, long-term celecoxib treatment is associated with an increased incidence of cardiovascular side effects. These findings are supported by studies conducted in patients with the basal cell nevus syndrome [69]. In a double-blind, placebo-controlled trial, subjects with fewer than 15 BCCs at baseline developed significantly fewer new BCCs over a 2-year period when given celecoxib 200 mg twice daily than placebo-treated individuals.
Diclofenac is a COX-1 and COX-2 inhibitor. It is commercially available in a topical formulation [82]. A trial of the topical formulation in organ transplant patients applied topically over 16 weeks completely prevented invasive SCCs for 2 years [83].
Agents that Stimulate Immunity
Imiquimod
Imiquimod stimulates anti-tumor immune responses in the skin by binding to Toll-like receptor 7 (TLR7). This leads to increased production of proinflammatory cytokines such as IFN-α, IL-6, and TNF-α [84]. When applied topically, imiquimod activates Langerhans cells and adaptive immunity [85]. These effects have made imiquimod an effective treatment for AKs and in situ SCCs [86, 87]. A randomized double-blind study of 42 patients found that a 2-week treatment cycle resulted in nearly 100% reduction in the number of AKs with sustained clearance after 12 months [88•]. Imiquimod has also been used for the treatment of superficial BCCs [89].
5-Fluorouracil and Calcipotriol (Calcipotriene)
Topical 5-fluorouracil (5-FU) removes pre-malignant cells before they can develop into invasive KCs. Its mechanism of action is to inhibit the enzyme thymidylate synthase. This impedes DNA synthesis which limits the growth of rapidly dividing cells [90]. Calcipotriol is a vitamin D analog that increases the cytokine thymic stromal lymphopoietin (TSLP) [91••, 92, 93]. TSLP is produced by epidermal keratinocytes. It promotes immune responses by stimulating the release of chemokines, activating epidermal Langerhans cell maturation. When applied to sun-damaged skin for only 4 days, the combination of topical 5-FU and topical calcipotriol effectively causes regression of pre-malignant AKs [91••].
Other Agents for Skin Cancer Prevention and Treatment
A number of other agents show promise for the prevention or treatment of skin cancer. Many are in preclinical trials or are undergoing early testing in humans. Table 1 provides a list of chemopreventive agents.
Conclusions
Research into the mechanisms by which ultraviolet radiation causes skin cancer has generated new knowledge that is fundamental to our understanding of how environmental agents affect biological processes. These include DNA damage and repair, the role of oncogenes and tumor suppressor genes, tumor immunology, and prevention and treatment of cancer. These findings have implications not only for dermatological malignancies but also for cancer biology in general. The end result will be new molecules and pathways that can be targeted for prevention and treatment of cancer.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Rogers HW, Weinstock MA, Feldman SR, Coldiron BM. Incidence estimate of nonmelanoma skin cancer (keratinocyte carcinomas) in the US population, 2012. JAMA Dermatol. 2015;151:1081–6. https://doi.org/10.1001/jamadermatol.2015.1187.
Stern RS. Prevalence of a history of skin cancer in 2007: results of an incidence-based model. Arch Dermatol. 2010;146(3):279–82. https://doi.org/10.1001/archdermatol.2010.4.
Christenson LJ, Borrowman TA, Vachon CM, Tollefson MM, Otley CC, Weaver AL, et al. Incidence of basal cell and squamous cell carcinomas in a population younger than 40 years. JAMA. 2005;294:681–90.
Weinstock MA, Bogaars HA, Ashley M, Litle V, Bilodeau E, Kimmel S. Nonmelanoma skin cancer mortality. A population-based study. Arch Dermatol. 1991;127(8):1194–7.
Armstrong B, Kricker A. The epidemiology of UV-induced skin cancer. J Photochem Photobiol B: Biology. 2001;63:8–18.
Blum HF. Carcinogenesis by ultraviolet light. Princeton: Princeton University Press; 1959.
Setlow RB, Setlow JK. Evidence that ultraviolet-induced thymine dimers in DNA cause biological damage. Proc Natl Acad Sci U S A. 1962;48:1250–7.
Freeman RG. Action spectrum for ultraviolet carcinogenesis. Natl Cancer Inst Monogr. 1978;50:27–9.
Staberg B, Wulf HC, Klemp P, Poulsen T, Brodthagen H. The carcinogenic effect of UVA irradiation. J Invest Dermatol. 1983;81:517–9.
Setlow RB, Grist E, Thompson K, Woodhead AD. Wavelengths effective in induction of malignant melanoma. Proc Natl Acad Sci U S A. 1993;90:6666–70.
Noonan FP, Zaidi MR, Wolnicka-Glubisz A, Anver MR, Bahn J, Wielgus A, et al. Melanoma induction by ultraviolet A but not ultraviolet B radiation requires melanin pigment. Nat Commun. 2012;3:884. https://doi.org/10.1038/ncomms1893.
Lazovich D, Vogel RI, Berwick M, Weinstock MA, Anderson KE, Warshaw EM. Indoor tanning and risk of melanoma: a case-control study in a highly exposed population. Cancer Epidemiol Biomark Prev. 2010;19(6):1557–68. https://doi.org/10.1158/1055-9965.Epi-09-1249.
• Ghiasvand R, Rueegg CS, Weiderpass E, Green AC, Lund E, Veierod MB. Indoor tanning and melanoma risk: long-term evidence from a prospective population-based cohort study. Am J Epidemiol. 2017;185(3):147–56. https://doi.org/10.1093/aje/kww148. Data from a large prospective cohort study provides strong evidence of a dose-response association between indoor tanning and risk of melanoma and supports the hypothesis that vulnerability to the harmful effects of indoor tanning is greater at a younger age.
Wehner MR, Shive ML, Chren MM, Han J, Qureshi AA, Linos E. Indoor tanning and non-melanoma skin cancer: systematic review and meta-analysis. Bmj. 2012;345:e5909. https://doi.org/10.1136/bmj.e5909.
Stern RS. The risk of squamous cell and basal cell cancer associated with psoralen and ultraviolet A therapy: a 30-year prospective study. J Am Acad Dermatol. 2012;66(4):553–62. https://doi.org/10.1016/j.jaad.2011.04.004.
Cowen EW, Nguyen JC, Miller DD, McShane D, Arron ST, Prose NS, et al. Chronic phototoxicity and aggressive squamous cell carcinoma of the skin in children and adults during treatment with voriconazole. J Am Acad Dermatol. 2010;62(1):31–7. https://doi.org/10.1016/j.jaad.2009.09.033.
Vakharia PP, Nardone B, Schlosser BJ, Lee D, Serrano L, West DP. Chronic exposure to tetracyclines and subsequent diagnosis for non-melanoma skin cancer in a large Midwestern U.S. patient population. J Eur Acad Dermatol Venereol. 2017;31(12):e534–e6. https://doi.org/10.1111/jdv.14399.
Kaae J, Boyd HA, Hansen AV, Wulf HC, Wohlfahrt J, Melbye M. Photosensitizing medication use and risk of skin cancer. Cancer Epidemiol Biomark Prev. 2010;19(11):2942–9. https://doi.org/10.1158/1055-9965.EPI-10-0652.
Karagas MR, Stukel TA, Umland V, Tsoukas MM, Mott LA, Sorensen HT, et al. Reported use of photosensitizing medications and basal cell and squamous cell carcinoma of the skin: results of a population-based case-control study. J Invest Dermatol. 2007;127(12):2901–3. https://doi.org/10.1038/sj.jid.5700934.
Wu S, Cho E, Feskanich D, Li WQ, Sun Q, Han J, et al. Citrus consumption and risk of basal cell carcinoma and squamous cell carcinoma of the skin. Carcinogenesis. 2015;36(10):1162–8. https://doi.org/10.1093/carcin/bgv109.
Wu S, Li WQ, Qureshi AA, Cho E. Alcohol consumption and risk of cutaneous basal cell carcinoma in women and men: 3 prospective cohort studies. Am J Clin Nutr. 2015;102(5):1158–66. https://doi.org/10.3945/ajcn.115.115196.
Lee JW, Ratnakumar K, Hung KF, Rokunohe D, Kawasumi M. Deciphering UV-induced DNA Damage responses to prevent and treat skin cancer. Photochem Photobiol. 2020;96:478–99. https://doi.org/10.1111/php.13245.
•• Hosseini M, Dousset L, Michon P, Mahfouf W, Muzotte E, Bergeron V, et al. UVB-induced DHODH upregulation, which is driven by STAT3, is a promising target for chemoprevention and combination therapy of photocarcinogenesis. Oncogenesis. 2019;8(10):52. https://doi.org/10.1038/s41389-019-0161-z. The authors use a multistage model of UVB radiation-induced skin cancer, and show that UVB-induced DHODH upregulation is mainly regulated transcriptionally by STAT3. They found that chronic inhibition of DHODH by leflunomide (LFN) blocks UVB-induced tumor initiation making DHODH is a promising target for chemoprevention and combination therapy of UVB-induced cSCCs.
Mouret S, Baudouin C, Charveron M, Favier A, Cadet J, Douki T. Cyclobutane pyrimidine dimers are predominant DNA lesions in whole human skin exposed to UVA radiation. Proc Natl Acad Sci U S A. 2006;103(37):13765–70. https://doi.org/10.1073/pnas.0604213103.
de Gruijl FR. Skin cancer and solar UV radiation. Eur J Cancer. 1999;35(14):2003–9. https://doi.org/10.1016/s0959-8049(99)00283-x.
Cleaver JE, Lam ET, Revet I. Disorders of nucleotide excision repair: the genetic and molecular basis of heterogeneity. Nat Rev Genet. 2009;10(11):756–68. https://doi.org/10.1038/nrg2663.
Barroeta-Espar I, Weinstock LD, Perez-Nievas BG, Meltzer AC, Siao Tick Chong M, Amaral AC, et al. Distinct cytokine profiles in human brains resilient to Alzheimer’s pathology. Neurobiol Dis 2019;121:327–337. doi: https://doi.org/10.1016/j.nbd.2018.10.009.
Ingham PW, McMahon AP. Hedgehog signaling in animal development: paradigms and principles. Genes Dev. 2001;15(23):3059–87. https://doi.org/10.1101/gad.938601.
Tang JY, Epstein JEH, Oro AE. Basal cell carcinoma and basal cell nevus syndrome. In: Kang S, Amagai M, Bruckner AL, Enk AH, Margolis DJ, McMichael AJ, et al., editors. Fitzpatrick’s dermatology, 9e. New York: McGraw-Hill Education; 2019.
Ashton KJ, Weinstein SR, Maguire DJ, Griffiths LR. Molecular cytogenetic analysis of basal cell carcinoma DNA using comparative genomic hybridization. J Invest Dermatol. 2001;117(3):683–6. https://doi.org/10.1046/j.0022-202x.2001.01434.x.
Remenyik E, Wikonkal NM, Zhang W, Paliwal V, Brash DE. Antigen-specific immunity does not mediate acute regression of UVB-induced p53-mutant clones. Oncogene. 2003;22(41):6369–76. https://doi.org/10.1038/sj.onc.1206657.
Chen W, Barthelman M, Martinez J, Alberts D, Gensler HL. Inhibition of cyclobutane pyrimidine dimer formation in epidermal p53 gene of UV-irradiated mice by alpha-tocopherol. Nutr Cancer. 1997;29(3):205–11. https://doi.org/10.1080/01635589709514625.
Ahmad N, Katiyar SK, Mukhtar H. Antioxidants in chemoprevention of skin cancer. Curr Probl Dermatol. 2001;29:128–39.
Breitkreutz D, Braiman-Wiksman L, Daum N, Denning MF, Tennenbaum T. Protein kinase C family: on the crossroads of cell signaling in skin and tumor epithelium. J Cancer Res Clin Oncol. 2007;133(11):793–808. https://doi.org/10.1007/s00432-007-0280-3.
Wheeler DL, Martin KE, Ness KJ, Li Y, Dreckschmidt NE, Wartman M, et al. Protein kinase C epsilon is an endogenous photosensitizer that enhances ultraviolet radiation-induced cutaneous damage and development of squamous cell carcinomas. Cancer Res. 2004;64(21):7756–65. https://doi.org/10.1158/0008-5472.Can-04-1881.
Cataisson C, Joseloff E, Murillas R, Wang A, Atwell C, Torgerson S, et al. Activation of cutaneous protein kinase C alpha induces keratinocyte apoptosis and intraepidermal inflammation by independent signaling pathways. J Immunol. 2003;171(5):2703–13. https://doi.org/10.4049/jimmunol.171.5.2703.
Ahmad N, Gilliam AC, Katiyar SK, O’Brien TG, Mukhtar H. A definitive role of ornithine decarboxylase in photocarcinogenesis. Am J Pathol. 2001;159(3):885–92.
Raul F. Revival of 2-(difluoromethyl)ornithine (DFMO), an inhibitor of polyamine biosynthesis, as a cancer chemopreventive agent. Biochem Soc Trans. 2007;35(Pt 2):353–5. https://doi.org/10.1042/BST0350353.
Tjiu JW, Chen JS, Shun CT, Lin SJ, Liao YH, Chu CY, et al. Tumor-associated macrophage-induced invasion and angiogenesis of human basal cell carcinoma cells by cyclooxygenase-2 induction. J Invest Dermatol. 2009;129(4):1016–25. https://doi.org/10.1038/jid.2008.310.
Tjiu JW, Liao YH, Lin SJ, Huang YL, Tsai WL, Chu CY, et al. Cyclooxygenase-2 overexpression in human basal cell carcinoma cell line increases antiapoptosis, angiogenesis, and tumorigenesis. J Invest Dermatol. 2006;126(5):1143–51. https://doi.org/10.1038/sj.jid.5700191.
Pentland A, Schoggins J, Scott G, Khan K, Han R. Reduction of UV-induced skin tumors in hairless mice by selective COX-2 inhibition. Carcinogenesis. 1999;20:1939–44.
An KP, Athar M, Tang X, Katiyar SK, Russo J, Beech J, et al. Cyclooxygenase-2 expression in murine and human nonmelanoma skin cancers: implications for therapeutic approaches. Photochem Photobiol. 2002;76(1):73–80.
•• Elmets CA, J JL, Athar M. Cyclooxygenases: mediators of UV-induced skin cancer and potential targets for prevention. J Invest Dermatol. 2014. https://doi.org/10.1038/jid.2014.192. This review of preclinical, epidemiologic and translational studies provides proof of principal that agents which inhibit cyclooxygenase-2 have the potential to limit the development of new NMSCs.
Bakshi A, Shafi R, Nelson J, Cantrell WC, Subhadarshani S, Andea A, et al. The clinical course of actinic keratosis correlates with underlying molecular mechanisms. Br J Dermatol. 2020;182(4):995–1002. https://doi.org/10.1111/bjd.18338.
Dannenberg AJ, Subbaramaiah K. Targeting cyclooxygenase-2 in human neoplasia: rationale and promise. Cancer Cell. 2003;4(6):431–6. https://doi.org/10.1016/s1535-6108(03)00310-6.
Kripke ML. Antigenicity of murine skin tumors induced by ultraviolet light. J Natl Cancer Inst. 1974;53:1333–6.
Athar M, Walsh SB, Kopelovich L, Elmets CA. Pathogenesis of nonmelanoma skin cancers in organ transplant recipients. Arch Biochem Biophys. 2011;508(2):159–63. https://doi.org/10.1016/j.abb.2011.01.004.
Mellemgaard A, Geisler CH, Storm HH. Risk of kidney cancer and other second solid malignancies in patients with chronic lymphocytic leukemia. Eur J Haematol. 1994;53(4):218–22.
Weimar VM, Ceilley RI, Goeken JA. Cell-mediated immunity in patients with basal and squamous cell skin cancer. J Am Acad Dermatol. 1980;2:143–7.
Kaporis HG, Guttman-Yassky E, Lowes MA, Haider AS, Fuentes-Duculan J, Darabi K, et al. Human basal cell carcinoma is associated with Foxp3+ T cells in a Th2 dominant microenvironment. J Invest Dermatol. 2007;127(10):2391–8. https://doi.org/10.1038/sj.jid.5700884.
Moscicki RA, Morison WL, Parrish JA, Bloch KJ, Colvin RB. Reduction of the fraction of circulating helper-inducer T cells identified by monoclonal antibodies in psoriatic patients treated with long-term psoralen/ultraviolet-A radiation (PUVA). J Invest Dermatol. 1982;79:205–8.
Volden G, Molin L, Thomsen K. PUVA-induced suppression contact sensitivity to mustine hydrochloride in mycosis fungoides. Br Med J. 1978;2:865–6.
Criscione VD, Weinstock MA, Naylor MF, Luque C, Eide MJ, Bingham SF, et al. Actinic keratoses: natural history and risk of malignant transformation in the Veterans Affairs Topical tretinoin Chemoprevention Trial. Cancer. 2009;115(11):2523–30. https://doi.org/10.1002/cncr.24284.
•• Bakshi A, Shafi R, Nelson J, Cantrell WC, Subhadarshani S, Andea A, et al. Actinic keratosis clinical course correlates with underlying molecular mechanisms. Br J Dermatol. 2019;182:995–1002. https://doi.org/10.1111/bjd.18338. This observational study characterizes biomarkers associated with their persistence, progression and regression ofactinic keratoses. Decreased E-cadherin and increased p53, Snail, Slug and Twist (E-cadherin transcription factors) were associated with progression from AK to nonmelanoma skin cancer.These markers may be used to assess the efficacy of existing chemopreventive agents.
Kibitel J, Anderson C, Elmets C, Brash D, Yarosh D. Aberrant regulation of TNFa in the skin of p53 knockout mice before and after UV-B irradiation. Journal of Investigative Dermatology. 1999;112(4):549.
Gratchev A, Strein P, Utikal J, Sergij G. Molecular genetics of Xeroderma pigmentosum variant. Exp Dermatol. 2003;12(5):529–36.
Yarosh D, Klein J, O’Connor A, Hawk J, Rafal E, Wolf P. Effect of topically applied T4 endonuclease V in liposomes on skin cancer in xeroderma pigmentosum: a randomised study. Xeroderma Pigmentosum Study Group Lancet. 2001;357(9260):926–9.
• Navarrete-Dechent C, Molgo M. The use of a sunscreen containing DNA-photolyase in the treatment of patients with field cancerization and multiple actinic keratoses: a case-series. Dermatol Online J. 2017;23(1). In this prospective single arm case-series the authors propose a new concept called "active photoprotection" because of its dual mechanism involving therapy and protection.They concluded that patients with cutaneous field cancerization may benefit from addition of novel topical applications containing DNA-photolyase.
Carducci M, Pavone PS, De Marco G, Lovati S, Altabas V, Altabas K, et al. Comparative effects of sunscreens alone vs sunscreens plus DNA repair enzymes in patients with actinic keratosis: clinical and molecular findings from a 6-month, randomized. Clinical Study J Drugs Dermatol. 2015;14(9):986–90.
Thompson BC, Surjana D, Halliday GM, Damian DL. Nicotinamide enhances repair of ultraviolet radiation-induced DNA damage in primary melanocytes. Exp Dermatol. 2014;23(7):509–11. https://doi.org/10.1111/exd.12430.
Surjana D, Halliday GM, Damian DL. Nicotinamide enhances repair of ultraviolet radiation-induced DNA damage in human keratinocytes and ex vivo skin. Carcinogenesis. 2013;34(5):1144–9. https://doi.org/10.1093/carcin/bgt017.
Damian DL, Patterson CR, Stapelberg M, Park J, Barnetson RS, Halliday GM. UV radiation-induced immunosuppression is greater in men and prevented by topical nicotinamide. J Invest Dermatol. 2008;128(2):447–54. https://doi.org/10.1038/sj.jid.5701058.
•• Chen AC, Martin AJ, Choy B, Fernandez-Penas P, Dalziell RA, McKenzie CA, et al. A phase 3 randomized trial of nicotinamide for skin-cancer chemoprevention. N Engl J Med. 2015;373(17):1618–26. https://doi.org/10.1056/NEJMoa1506197. Oral nicotinamide wasfound to be safe and effective in reducing the rates of new nonmelanoma skin cancers and actinic keratoses in high-risk patients.
Von Hoff DD, LoRusso PM, Rudin CM, Reddy JC, Yauch RL, Tibes R, et al. Inhibition of the hedgehog pathway in advanced basal-cell carcinoma. N Engl J Med. 2009;361(12):1164–72. https://doi.org/10.1056/NEJMoa0905360.
Dummer R, Ascierto PA, Basset-Seguin N, Dreno B, Garbe C, Gutzmer R, et al. Sonidegib and vismodegib in the treatment of patients with locally advanced basal cell carcinoma: a joint expert opinion. J Eur Acad Dermatol Venereol. 2020. https://doi.org/10.1111/jdv.16230.
•• Dummer R, Guminksi A, Gutzmer R, Lear JT, Lewis KD, Chang ALS, et al. Long-term efficacy and safety of sonidegib in patients with advanced basal cell carcinoma: 42-month analysis of the phase II randomized, double-blind BOLT study. Br J Dermatol. 2019;182:1369–78. https://doi.org/10.1111/bjd.18552.
Migden MR, Guminski A, Gutzmer R, Dirix L, Lewis KD, Combemale P, et al. Treatment with two different doses of sonidegib in patients with locally advanced or metastatic basal cell carcinoma (BOLT): a multicentre, randomised, double-blind phase 2 trial. Lancet Oncol. 2015;16(6):716–28. https://doi.org/10.1016/S1470-2045(15)70100-2.
•• Sekulic A, Migden MR, Lewis K, Hainsworth JD, Solomon JA, Yoo S, Arron ST, Friedlander PA, Marmur E, Rudin CM, Chang AL, Dirix L, Hou J, Yue H, Hauschild A, ERIVANCE BCC investigators Pivotal ERIVANCE basal cell carcinoma (BCC) study: 12-month update of efficacy and safety of vismodegib in advanced BCC. J Am Acad Dermatol 2015;72(6):1021–1026 e8. https://doi.org/10.1016/j.jaad.2015.03.021. Primary analysis from the pivotal ERIVANCE BCC study resulted in approval of vismodegib for treatment of adults with metastatic or locally advanced basal cell carcinoma (BCC) that has recurred after surgery or for patients who are not candidates for surgery or radiation. The 12-month update of the study confirms the efficacy and safety of vismodegib in management of advanced BCC.
Tang JY, Aszterbaum M, Athar M, Barsanti F, Cappola C, Estevez N, et al. Basal cell carcinoma chemoprevention with nonsteroidal anti-inflammatory drugs in genetically predisposed PTCH1+/- humans and mice. Cancer Prev Res (Phila Pa). 2010;3(1):25–34. https://doi.org/10.1158/1940-6207.CAPR-09-0200.
Black HS, Herd JA, Goldberg LH, Wolf JE Jr, Thornby JI, Rosen T, et al. Effect of a low-fat diet on the incidence of actinic keratosis. N Engl J Med. 1994;330(18):1272–5.
Vaid M, Singh T, Prasad R, Katiyar SK. Intake of high-fat diet stimulates the risk of ultraviolet radiation-induced skin tumors and malignant progression of papillomas to carcinoma in SKH-1 hairless mice. Toxicol Appl Pharmacol. 2014;274(1):147–55. https://doi.org/10.1016/j.taap.2013.10.030.
Peck GL. Long-term retinoid therapy is needed for maintenance of cancer chemopreventive effect. Dermatologica. 1987;175(Suppl 1):138–44.
Kadakia KC, Barton DL, Loprinzi CL, Sloan JA, Otley CC, Diekmann BB, et al. Randomized controlled trial of acitretin versus placebo in patients at high-risk for basal cell or squamous cell carcinoma of the skin (North Central Cancer Treatment Group Study 969251). Cancer. 2012;118(8):2128–37. https://doi.org/10.1002/cncr.26374.
Kraemer KH, DiGiovanna JJ, Peck GL. Chemoprevention of skin cancer in xeroderma pigmentosum. J Dermatol. 1992;19(11):715–8.
Moon T, Levine N, Cartmel B, Bangert J, Rodney S, Dong Q, et al. Effect of retinol in preventing squamous cell skin cancer in moderate-risk subjects: a randomized, double-blind, controlled trial. Southwest kin Cancer Prevention Study Group. Cancer Epidemiol Biomark Prev. 1997;6(11):949–56.
Nijsten TE, Stern RS. Oral retinoid use reduces cutaneous squamous cell carcinoma risk in patients with psoriasis treated with psoralen-UVA: a nested cohort study. J Am Acad Dermatol. 2003;49(4):644–50.
Bavinck JN, Tieben LM, Van der Woude FJ, Tegzess AM, Hermans J, ter Schegget J, et al. Prevention of skin cancer and reduction of keratotic skin lesions during acitretin therapy in renal transplant recipients: a double-blind, placebo-controlled study. J Clin Oncol. 1995;13(8):1933–8.
Weinstock MA, Bingham SF, Lew RA, Hall R, Eilers D, Kirsner R, et al. Topical tretinoin therapy and all-cause mortality. Arch Dermatol. 2009;145(1):18–24. https://doi.org/10.1001/archdermatol.2008.542.
Bailey HH, Kim K, Verma AK, Sielaff K, Larson PO, Snow S, et al. A randomized, double-blind, placebo-controlled phase 3 skin cancer prevention study of a-difluoromethylornithine in subjects with previous history of skin cancer. Cancer Prev Res (Phila Pa). 2010;3(1):35–47. https://doi.org/10.1158/1940-6207.CAPR-09-0096.
Kreul SM, Havighurst T, Kim K, Mendonca EA, Wood GS, Snow S, et al. A phase III skin cancer chemoprevention study of DFMO: long-term follow-up of skin cancer events and toxicity. Cancer Prev Res (Phila). 2012;5(12):1368–74. https://doi.org/10.1158/1940-6207.CAPR-12-0233.
Elmets CA, Viner JL, Pentland AP, Cantrell W, Lin HY, Bailey H, et al. Chemoprevention of nonmelanoma skin cancer with celecoxib: a randomized, double-blind, placebo-controlled trial. J Natl Cancer Inst. 2010;102(24):1835–44. https://doi.org/10.1093/jnci/djq442.
Rivers JK, McLean DI. An open study to assess the efficacy and safety of topical 3% diclofenac in a 2.5% hyaluronic acid gel for the treatment of actinic keratoses. Arch Dermatol. 1997;133(10):1239–42.
Ulrich C, Johannsen A, Rowert-Huber J, Ulrich M, Sterry W, Stockfleth E. Results of a randomized, placebo-controlled safety and efficacy study of topical diclofenac 3% gel in organ transplant patients with multiple actinic keratoses. Eur J Dermatol. 2010;20(4):482–8. https://doi.org/10.1684/ejd.2010.1010.
Schon MP, Schon M. Imiquimod: mode of action. Br J Dermatol. 2007;157(Suppl 2):8–13. https://doi.org/10.1111/j.1365-2133.2007.08265.x.
Miller RL, Gerster JF, Owens ML, Slade HB, Tomai MA. Imiquimod applied topically: a novel immune response modifier and new class of drug. Int J Immunopharmacol. 1999;21(1):1–14.
Korman N, Moy R, Ling M, Matheson R, Smith S, McKane S, et al. Dosing with 5% imiquimod cream 3 times per week for the treatment of actinic keratosis: results of two phase 3, randomized, double-blind, parallel-group, vehicle-controlled trials. Arch Dermatol. 2005;141(4):467–73. https://doi.org/10.1001/archderm.141.4.467.
Patel GK, Goodwin R, Chawla M, Laidler P, Price PE, Finlay AY, et al. Imiquimod 5% cream monotherapy for cutaneous squamous cell carcinoma in situ (Bowen’s disease): a randomized, double-blind, placebo-controlled trial. J Am Acad Dermatol. 2006;54(6):1025–32. https://doi.org/10.1016/j.jaad.2006.01.055.
• Gupta G, Stockfleth E, Peris K, Aractingi S, Alomar A, Dakovic R, et al. Long-term sustained lesion clearance from Lmax with imiquimod 3.75%, a new field-directed treatment for actinic keratosis. J Eur Acad Dermatol Venereol. 2015;29(9):1840–2. https://doi.org/10.1111/jdv.12697. This randomized controlled study demonstrates the long-term efficacy of imiquimod 3.75% using the reduction in lesions from Lmax (maximum lesion count during treatment), which assesses the ability to clear subclinical and clinical lesions.
Kim JYS, Kozlow JH, Mittal B, Moyer J, Olencki T, Rodgers P. Guidelines of care for the management of basal cell carcinoma. J Am Acad Dermatol. 2018;78(3):540–59. https://doi.org/10.1016/j.jaad.2017.10.006.
Pinedo HM, Peters GF. Fluorouracil: biochemistry and pharmacology. J Clin Oncol. 1988;6(10):1653–64. https://doi.org/10.1200/JCO.1988.6.10.1653.
•• Cunningham TJ, Tabacchi M, Eliane JP, Tuchayi SM, Manivasagam S, Mirzaalian H, et al. Randomized trial of calcipotriol combined with 5-fluorouracil for skin cancer precursor immunotherapy. J Clin Invest. 2017;127(1):106–16. https://doi.org/10.1172/jci89820. This randomized controlled mouse model study demonstrates the synergistic effects of calcipotriol and 5-FU treatment in optimally activating a CD4+ T cell-mediated immunity against actinic keratoses.
Di Piazza M, Nowell CS, Koch U, Durham AD, Radtke F. Loss of cutaneous TSLP-dependent immune responses skews the balance of inflammation from tumor protective to tumor promoting. Cancer Cell. 2012;22(4):479–93. https://doi.org/10.1016/j.ccr.2012.08.016.
Demehri S, Turkoz A, Manivasagam S, Yockey LJ, Turkoz M, Kopan R. Elevated epidermal thymic stromal lymphopoietin levels establish an antitumor environment in the skin. Cancer Cell. 2012;22(4):494–505. https://doi.org/10.1016/j.ccr.2012.08.017.
Caini S, Cattaruzza S, Bendinelli B, Tosti G, Masala G, Gnagnarella P, et al. Coffee, tea and caffeine intake and the risk of non-melanoma skin cancer: a review of the literature and meta-analysis. Eur J Nutr. 2017;56(1):1–12. https://doi.org/10.1007/s00394-016-1253-6.
Willey A, Mehta S, Lee PK. Reduction in the incidence of squamous cell carcinoma in solid organ transplant recipients treated with cyclic photodynamic therapy. Dermatol Surg. 2010;36(5):652–8. https://doi.org/10.1111/j.1524-4725.2009.01384.x.
• Roozeboom MH, Arits AH, Mosterd K, Sommer A, Essers BA, de Rooij MJ, et al. Three-year follow-up results of photodynamic therapy vs. imiquimod vs. fluorouracil for treatment of superficial basal cell carcinoma: a single-blind, noninferiority, randomized controlled trial. J Invest Dermatol. 2016;136(8):1568–74. https://doi.org/10.1016/j.jid.2016.03.043. The study shows that imiquimod is superior and fluorouracil not inferior to MAL-PDT in treatment of superficial basal cell carcinoma.
• Zaar O, Fougelberg J, Hermansson A, Gillstedt M, Wennberg-Larkö A-M, Paoli J. Effectiveness of photodynamic therapy in Bowen’s disease: a retrospective observational study in 423 lesions. J Eur Acad Dermatol Venereol. 2017;31(8):1289–94. https://doi.org/10.1111/jdv.14164. The study shows that PDt is a relatively effective modality fpr treatment of Bowen's Disease(BD) with overall clearance rate of 63.4% for all BD lesions. Large lesion size (>2 cm) and a single PDT session were risk factors for unsuccessful treatment.
Wang H, Xu Y, Shi J, Gao X, Geng L. Photodynamic therapy in the treatment of basal cell carcinoma: a systematic review and meta-analysis. Photodermatol Photoimmunol Photomed. 2015;31(1):44–53. https://doi.org/10.1111/phpp.12148.
Singh CK, Mintie CA, Ndiaye MA, Chhabra G, Dakup PP, Ye T, et al. Chemoprotective effects of dietary grape powder on UVB radiation-mediated skin carcinogenesis in SKH-1 hairless mice. J Invest Dermatol. 2019;139(3):552–61. https://doi.org/10.1016/j.jid.2018.09.028.
Elmets C, Singh D, Tubesing K, Matsui M, Katiyar S, Mukhtar H. Prevention of cutaneous photodamage by polyphenols from green tea. J Amer Acad Dermatol. 2001;44:425–32.
Schwarz A, Maeda A, Gan D, Mammone T, Matsui MS, Schwarz T. Green tea phenol extracts reduce UVB-induced DNA damage in human cells via interleukin-12†. Photochem Photobiol. 2008;84(2):350–5. https://doi.org/10.1111/j.1751-1097.2007.00265.x.
Kim DJ, Kim J, Spaunhurst K, Montoya J, Khodosh R, Chandra K, et al. Open-label, exploratory phase II trial of oral itraconazole for the treatment of basal cell carcinoma. J Clin Oncol. 2014;32(8):745–51. https://doi.org/10.1200/jco.2013.49.9525.
Kim J, Tang JY, Gong R, Kim J, Lee JJ, Clemons KV, et al. Itraconazole, a commonly used antifungal that inhibits hedgehog pathway activity and cancer growth. Cancer Cell. 2010;17(4):388–99. https://doi.org/10.1016/j.ccr.2010.02.027.
Rizwan M, Rodriguez-Blanco I, Harbottle A, Birch-Machin MA, Watson RE, Rhodes LE. Tomato paste rich in lycopene protects against cutaneous photodamage in humans in vivo: a randomized controlled trial. Br J Dermatol. 2011;164(1):154–62. https://doi.org/10.1111/j.1365-2133.2010.10057.x.
• Delaitre L, Martins-Hericher J, Truchot E, Denis D, Prophette B, Maillard H, et al. Regression of cutaneous basal cell and squamous cell carcinoma under pembrolizumab. Ann Dermatol Venereol. 2019. https://doi.org/10.1016/j.annder.2019.10.031. The study shows that dietary grape powder mitigates UVB-mediated skin carcinogenesis in an SKH-1 hairless mouse model which could be attributable to antioxidant effect.
Mantel A, Carpenter-Mendini A, VanBuskirk J, Pentland AP. Aldo-keto reductase 1C3 is overexpressed in skin squamous cell carcinoma (SCC) and affects SCC growth via prostaglandin metabolism. Exp Dermatol. 2014;23(8):573–8. https://doi.org/10.1111/exd.12468.
• Kohli I, Shafi R, Isedeh P, Griffith JL, Al-Jamal MS, Silpa-Archa N, et al. The impact of oral Polypodium leucotomos extract on ultraviolet B response: a human clinical study. J Am Acad Dermatol. 2017;77(1):33–41.e1. https://doi.org/10.1016/j.jaad.2017.01.044. The study suggest that PLE can potentially be used as an adjunctive agent to lessen the negative photobiologic effects of UVB.
Rodriguez-Yanes E, Cuevas J, Gonzalez S, Mallol J. Oral administration of Polypodium leucotomos delays skin tumor development and increases epidermal p53 expression and the anti-oxidant status of UV-irradiated hairless mice. Exp Dermatol. 2014;23(7):526–8. https://doi.org/10.1111/exd.12454.
Funding
The author received NIH Grants P01CA210946, R01CA193885, P30 CA013148, N0135 CN2012-00033, and VA Grant 101BX003395.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Photodermatology
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Subhadarshani, S., Athar, M. & Elmets, C.A. Photocarcinogenesis. Curr Derm Rep 9, 189–199 (2020). https://doi.org/10.1007/s13671-020-00307-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13671-020-00307-0