Abstract
Purpose of Review
Sexual function and satisfaction in the transgender community is a nascent field with a paucity of data due to the fast paced nature of improving upon surgical technique and variety of patient experiences. The authors aim to review the current literature for areas of success as well as areas of improvement in order to better the sexual health of the transgender community.
Recent Findings
Gender dysphoria is a feeling of distress experienced by those whose gender assigned at birth is not in line with their gender identity. While social transition to the desired gender can suffice for some, medical and surgical interventions are often sought out to achieve gender euphoria, the decrease or absence of gender dysphoria. Often, issues with sexual function and satisfaction can trigger gender dysphoria, especially prior to social, medical, or surgical transition.
Summary
Surgical genital gender affirmation has been the most studied in terms of sexual function and improvement of gender dysphoria. Surgical complications, hormonal changes, and other organic causes of sexual dysfunction can still interfere with one’s overall sexual satisfaction. A validated measure of sexual function for trans men and trans women is needed to better assess outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sexual health is multifactorial and is heavily intertwined with other aspects of one’s health status as well as quality of life [1]. Sexual dysfunction is multifactorial and can be attributed to both external and internal factors, both of which can be distressing and at times debilitating to the individual experiencing it [2]. In current literature, sexual dysfunction is often discussed in four categories: lack of desire, orgasm/ejaculatory dysfunction, arousal dysfunction, and sexually related pain and further categorized by ICD and DSM-5 diagnoses [3, 4].
In a meta-analysis assessing sexual dysfunction, the prevalence was 31% in cisgender men and 41% in cisgender women [5]. Notably, the results of the studies in this meta analysis vary due to the different forms of measuring sexual function as there is no current gold standard for either sex. In determining the prevalence of sexual dysfunction in the transgender and gender diverse population, the data is much more limited and methods of assessment sparse. Transgender and gender diverse individuals (TGDI) are people whose gender identity is not in line with their sex [6]. TGDI is an umbrella term and can include several groups of people including transmasculine, transfeminine, and non-binary individuals [7]. Transitioning is not a requirement for being transgender, and can be social, medical and/or surgical. 1.3 million people in the United States identify as transgender [8]. Nevertheless, disparities are stark and sexual health is not an exception. In a large survey study assessing 27,715 transgender persons in 2015, both transgender men and women frequently reported delaying health care utilization due to the fear of discrimination and past experiences of discrimination [6]. To further analyze these disparities, the European Network for the Investigation of Gender Incongruence (ENIGI) came together as a multicenter establishment to study gender incongruence prospectively [9]. One study from this network demonstrated a decrease in sexual aversion with trans affirming care, both medical and surgical.
The goal of trans-affirming care is to reduce gender dysphoria and affirm TGDI in who they are via medically necessary interventions. Gender dysphoria is a feeling of distress experienced by those whose gender assigned at birth is not in line with their gender identity [7]. While social transition to the desired gender can suffice for some, medical and surgical interventions are often sought out to achieve gender euphoria, the decrease or absence of gender dysphoria [3]. Often, issues with sexual function and satisfaction can trigger gender dysphoria, especially prior to social, medical, or surgical transition. Nevertheless, this is not to say that issues surrounding sexual function and satisfaction cannot occur post-transition of any kind for the TGDI community.
Many validated sexual satisfaction and function surveys exist for cisgender individuals. These include the Sexual Health Inventory for Men (SHIM), the Index of Male Genital Self Image (IMGSI), Female Sexual Function Index (FSFI), the Female Sexual Distress Scale, and the Female Genital Self-Image Scale (FGSIS) [10,11,12,13,14]. Due to the differences in anatomy and life experience between cisgender and transgender individuals, these surveys cannot capture several aspects of function and experience for TGDI. For example, satisfaction with vaginal width and depth as well as genital self image of the vulva is not addressed in any of the available surveys [15•]. Therefore, surveys are needed to be created and validated among TGDI, not only for assessment, but also for progression of surgical techniques, establishment of longitudinal post-operative care, and betterment of overall sexual health.
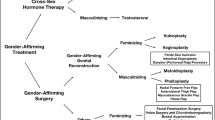
In this chapter we will discuss sexual function and dysfunction for TGDI. This will include the current evidence based research surrounding the topic, anatomic and hormonal considerations, pre and post-operative considerations, and future directions. Throughout the text, the authors will refer to trans men and trans women within the binary, albeit known that gender exists on a spectrum.
Prior to Medical and/or Surgical Affirming Treatments
Several factors, both mental and physical, must be considered when assessing for sexual dysfunction in TGDI prior to medical or surgical intervention as these factors contribute to one’s gender dysphoria. A systematic review of 44 studies analyzed data on sexual satisfaction, desire, arousal, orgasm, and pain [16•]. Generally, studies found that a healthy and positive relationship can have a positive impact on general sexual function, orgasm frequency and associated pleasure [17].
Trans Men
In a survey study of 170 trans men prior to medical or surgical intervention, 42.9% experienced low sexual desire and 28.6% experienced sexual aversion [9]. Distress surrounding sexual activity or one’s own sexual health, which may or may not include individual anatomy, may impact general sexual satisfaction [17, 18]. Thus, those experiencing high levels of gender dysphoria may have lower levels of sexual satisfaction. Dissatisfaction with one’s body, or body dysmorphia can heavily contribute to sexual dysfunction and plays a large role in gender dysphoria [3]. Specifically, one study of 141 trans men demonstrated a connection between body dysmorphia and difficulty with sexual arousal in 91% of participants [18].
Orgasm, or climax, differs per the individual and can be affected by a multitude of factors, sometimes resulting in differing intensities or its absence. While in some cases dysfunction of the orgasm is psychological in nature, in other cases it can be iatrogenic with antidepressants as a common culprit [6]. Gender dysphoria, which is often tied to depression, is often implicated in dysfunction of orgasm in trans men. One study including 211 trans men prior to medical or surgical intervention showed a 42.9% rate of difficulty with orgasm that affected their daily life [9].
The experience of pain in association with sexual activity can be extremely detrimental to one’s view of intimacy and overall sexual health. While there is not much data on sexual pain in trans men, one study found that 12% of 211 participants reported pain at the same frequency before and after genital reconstruction surgery [9]. Multiple studies found that pelvic pain was the most prevalent pain experienced prior to testosterone use [19, 20]. In one study of 351 participants, 98.3% experienced some amount of pelvic pain prior to testosterone. Of note, another study found that history of pain with orgasm prior to testosterone initiation and persistent menstruation with testosterone were both predictors of pelvic pain after testosterone initiation [20]. Pelvic floor dysfunction remains a possibility that has not been well studied and may contribute to pelvic pain.
Trans Women
Gender affirming care is known to alleviate general distress including, but not limited to distress associated with sexual dysfunction. One study surveyed multiple treatment groups of transgender women including those with no history of hormone therapy or genital reconstruction, those who had initiated hormone therapy, and those who had undergone vaginoplasty. Those who had not undergone medical or surgical treatment had more difficulty initiating and seeking sexual contacts (40%), fear of sexual contacts (33.3%), difficulty with arousal (33.3%), and pain during sexual intercourse (28.6%) compared to those who had initiated hormone therapy (34.1%, 18.8%, 32.6%, 11.4%) and those who had undergone vaginoplasty (23%, 20.8%, 15.9%, 27.1%), respectively [9].
In investigating the ability to achieve orgasm prior to initiation of hormonal or surgical treatment, dysfunction occurred in 46.7% of 29 participants [9]. Dysfunction in this setting may be attributable to distress surrounding orgasm with natal anatomy as well as difficulty achieving orgasm. In the same study, 12% of participants expressed distress associated with ejaculation. Another study of 208 trans women who had not initiated hormone therapy reported that 18.3% of participants had never experienced a pleasant orgasm [21].
Post Medical and/or Surgical Affirming Treatments
Although gender affirming medical therapy and surgery have been shown to dramatically reduce gender dysphoria and many associated sexual dysfunctions, TGDI continue to experience both positive and sometimes negative sexual experiences with specific correlation to their transition [3].
Trans Men
Satisfaction
General sexual satisfaction has been shown to improve after initiation of gender affirming care, both medical and surgical. Several studies have shown a decrease in sexual distress after a combination of hormone therapy and gender affirming surgery [17, 18, 22]. Interestingly some studies discussed a difference in sexual satisfaction based on the type of genital reconstruction that was performed, with one study showing an increase in sexual satisfaction for those who received a metoidioplasty compared to those who received a phalloplasty [23]. Gender affirming surgery has shown to increase sexual satisfaction, even when solely analyzing body self-image as demonstrated in several studies despite surgical complications [23, 24].
Desire
After hormonal or surgical transition, one study of 138 individuals demonstrated a 5% rate of hypoactive sexual desire disorder with 85% of these participants having completed surgery [25]. Testosterone increases sexual desire in both cisgender and transgender individuals [16•]. Several studies demonstrate an increase in sexual desire in up to 60% of trans male individuals starting within months and lasting for greater than a year after initiation of testosterone [25, 26]. Nevertheless, enhanced sexual desire is not always desirable, especially when it exceeds expectations. 3.6% of individuals in one study expressed distress from this elevation in sexual desire [25]. In examining surgical effects on sexual desire, results from studies were inconsistent and most studies determined no effects on its prevalence [25, 26].
Some studies also investigated sexual orientation after medical and surgical affirming therapy with mixed results. One study reported 22% of 59 trans men changed their sexual orientation after medical or surgical management while another study of 50 participants found no change [27, 28].
Arousal
While body dysmorphia has a negative effect on sexual arousal, testosterone and affirming surgery via mastectomy or genital reconstruction, have demonstrated improvement in sexual arousal. One study reported a 65% improvement in sexual arousal and another study demonstrated a 18.9% decrease in arousal dysfunction after mastectomy and hysterectomy and 23.2% decrease after phalloplasty [9, 17]. Of note, there is variability in how genital reconstruction surgeries are performed, with phalloplasties often being performed in multiple stages, thus affecting sensation and arousal perceptions depending on the stage of the procedure and techniques used.
Orgasm
While an orgasm has the potential to be impacted iatrogenically via certain medications, studies investigating testosterone use without gender affirming surgery did not demonstrate a significant change in intensity or ability of orgasm [28]. Of note, serum testosterone levels did not impact these findings. Most survey studies demonstrated an increase in ability to attain orgasm and an increase in intensity of the orgasm after medical and surgical transition [9, 17, 22]. Data from these studies showed a 30% increase in ability to orgasm during sexual intercourse or masturbation after genital reconstruction surgery, not differentiating between metoidioplasty and phalloplasty.
Pain
Trans men who had undergone phalloplasty were four times more likely to experience pain during sexual intercourse compared to those who underwent metoidioplasty [9]. A recent publication also documented complications of penile and testicular prosthesis following gender-affirming phalloplasty. Three of 45 patients experienced pelvic or pubic pain with prosthesis [29]. Individuals undergoing penile prosthetic implantation may experience acute or chronic post-operative pain. This could be due to prosthesis malpositioning, alterations in proprioceptive nerves particularly with ilioinguinal nerve coaptation, excessive pressure from the prosthesis on the skin of the free flap, or irritation of the pubic bone at the fixation point [30].
Trans Women
Satisfaction
General satisfaction may be related to genital self image and its impact on gender dysphoria as well as general function. One systematic review determined that satisfaction is correlated to neovaginal function and depth, clitoral sensation, appearance of the vulva and labia minora, and natural lubrication [31]. They found that 80% of patients are satisfied with their sexual function post-vaginoplasty regardless of surgical technique and 60–80% report their neovagina is deep enough for penetration.
Desire
Several studies demonstrate a decrease in sexual desire after initiation of estrogen and antiandrogen medications [26, 32]. Prevalence of low sexual desire ranged from 32% to 73%, but the percentage of those experiencing distress from low sexual desire or hypoactive sexual desire disorder (HSDD) was 22% in a study of 214 trans women after medical and surgical affirmation [9, 25]. This distress associated with low sexual desire is a key marker for HSDD, a diagnosis often paired with depression [33].
Time since initiation of hormone therapy, regardless of regimen or dosage, impacts the level of sexual desire with most experiencing the decrease within the first year after initiation [26, 32]. One study of 205 trans women demonstrated the lowest point of sexual desire occuring at three months after initiation and then returning to baseline, defined as sexual desire prior to initiation of hormone therapy, at 12 months [32]. Another study of 401 trans women found a decrease in desire occurring within the first year after initiation and returning to baseline at three years after initiation [26]. Interestingly, this study differentiated between sexual desire with and without a partner, demonstrating increased sexual desire with a partner relative to their baseline prior to initiation of hormone therapy.
With regards to gender affirming surgery and its effect on sexual desire, most studies demonstrated an overall increase in desire compared to preoperative levels. One study of 307 trans women measured sexual desire pre and post-operatively with 32.7% experiencing low sexual desire preoperatively and 18.3% experiencing low sexual desire post-operatively [9]. Decrease in desire may also occur post-operatively, especially post-orchiectomy [3]. However, patients report an enhanced degree of spontaneous sexual desire after gender affirming surgery, likely due to reduced dysphoria [22]. Add-back testosterone, phosphodiesterase type 5 (PDE5) inhibitors, and bremelanotide may be indicated in these scenarios to improve sexual desire, but data are lacking on medical treatment for transwomen after surgery [31].
Arousal
Sexual arousal is defined as a positive sensory physiologic response to sexual stimuli [34]. When exploring the effects of hormone therapy in trans women on sexual arousal, most studies found no impact. One study looking at the prevalence of arousal difficulties in trans women with and without use of hormone therapy found a 32.6% and 33.3% respectively [9].
Effects of vaginoplasty on sexual arousal have also been studied. In a survey study of 119 trans women after penile inversion vaginoplasty, results showed a 71.5% ease associated with sexual arousal post-operatively as well as a correlation between ease of sexual arousal with ability to orgasm [34]. Anatomically speaking, the sensitivity of the neoclitoris was more associated with sexual arousal than was depth of the neovagina. Multiple studies have compared sexual arousal levels of trans women post-operatively with sexual arousal in cisgender women. In these studies, 90–100% of trans women reported experiencing sexual arousal post-operatively, but when level of sexual arousal was assessed using the Female Sexual Function Index (FSFI), sexual arousal scores were overall lower in trans women than in their cisgender counterparts [35,36,37]. The FSFI is a validated 19 question tool that measures sexual function in cisgender women, assessing desire, arousal, lubrication, orgasm, satisfaction, and pain [38].
Lubrication as a measure of arousal has also been assessed. While lubrication is not directly associated with neovaginal function, it can be more prevalent in certain vaginoplasty types. FSFI scores assessing lubrication for cisgender women and trans women were obtained with subgroup analyses differentiating between penile inversion vaginoplasties and intestinal vaginoplasties [35,36,37]. Lubrication scores out of 6 were on average 5.7 for cisgender women, 2.8 for trans women who received a penile inversion and 4.0 for trans women who received an intestinal vagina. One study was also done to investigate the association of lubrication with arousal in trans women and demonstrated a 64.3% rate of lubrication during sexual arousal and 76% rate of lubrication during orgasm [22].
Orgasm
In trans women who have initiated hormone therapy, but who have not undergone genital reconstruction surgery, difficulty in achieving orgasm was seen to decrease. In one study, the prevalence of orgasmic dysfunction decreased to 29.2% from 46.7% after the initiation of hormone therapy [9]. Whether this finding can be attributed to the simultaneous decrease in gender dysphoria and body dysmorphia associated with the initiation of hormone therapy still needs to be investigated.
Ability to orgasm in trans women post-vaginoplasty has also been studied. Due to the unique anatomy of trans women post-operatively, it must be noted that orgasms can occur at multiple locations including the clitoris and prostate via masturbation or vaginal penetration, for example. There is variability in the rates of orgasm post-operatively with studies citing percentages between 40–100% [35,36,37]. These studies used the FSFI to assess orgasmic scores and demonstrated ranges of 2.82 to 4.0 out of 6 in comparison to cisgender women without sexual dysfunction who scored an average of 5.1. When analyzing the correlation between sexual activity and achieving orgasm, one study found that direct stimulation of the clitoris had a higher frequency of orgasm when compared to intercourse [34]. In assessing frequency and quality of orgasms post-operatively, studies are inconsistent. While one study reported an increase in orgasm frequency with sexual activity post-operatively, another study of 91 trans women post-operatively found orgasms to occur less frequently in 52.6% of participants and more frequently in 20.5% of participants [22, 34]. Quality of orgasms, when investigated, was found to be more pleasurable postoperatively in 51% of a 218 person study and with no changes in 62.5% of a 31 person study [37, 39].
Pain
Experiencing pain during sex is associated with reduced overall sexual health [40]. Sexual pain can be further specified by timing as well as anatomic location with some experiencing pain on insertion or after sexual intercourse and some experiencing either clitoral, vulvar, or vaginal pain during sexual activity. In one survey study delineating between those who had initiated hormone therapy and those who had also undergone vaginoplasty, pain during sexual intercourse occurred at a rate of 11.4% and 27.1% respectively and pain after sexual intercourse occurred at a rate of 9.1% and 16.7% respectively demonstrating a relative increase in sexual pain post-operatively [9]. Dyspareunia, or pain during sexual activity, can have multiple causes dependant on anatomic location including hair in the vaginal canal, small or stenosed vaginal canal, vaginal dryness, and painful clitoral sensation, sometimes due to spongiosum remnants during arousal [41].
Anatomic and Surgical Considerations
Trans Men
When it comes to phalloplasty, surgical technique, staging processes, flaps utilized and donor nerves selected have been markedly variable. Radial forearm phalloplasty, utilizing the radial forearm flap for phallic construction, has been the most common. Although the cutaneous sensibility of the radial flap is less than that of a male phallus, its thinness and the high density of cutaneous innervation from the medial and lateral antebrachial cutaneous nerves give it a sensory advantage over other flaps. The anterolateral thigh flap for example, is the second most commonly utilized flap, in which the lateral femoral cutaneous nerve allows for sensation. However, this flap has a lower density of innervation, and possesses considerable thickness which necessitates thinning, a procedure that risks sensation. Lastly, the latissimus dorsi flap is considered insensate because the intercostal nerves which provide cutaneous sensation to this flap are not coapted [42].
Four regional nerves can be utilized as donor nerves for the neophallus: the left or right dorsal nerves of the clitoris which are branches of the pudendal nerve, the ilioinguinal nerve, and the genital branch of the genitofemoral nerve. Transecting one for donor use while maintaining innervation of the clitoris with another can preserve erogenous sensation. About 100% of transgender people who have undergone phalloplasty reported maintained erogenous sensation, and that is due to preservation of innervation to their buried clitoris. Consequently, it is advised against using both branches of the dorsal nerve to innervate the neophallus, suggesting that erogenous sensation post-phalloplasty is more related to preserving sensation in the buried clitoris, rather than creating a phallus with erogenous capacity [42]. Testing for sensation in the neophallus is complicated by the fact that movement of the neophallus may inadvertently result in pulling on the innervated mons pubis or stimulating the buried clitoris, meaning new sensory testing methods that isolate the phallus must be adapted [42].
A systematic review and meta-analysis found the overall complication rate of phalloplasty to be 76.5% [43], with higher rates of complication in two-stage phalloplasty compared to single-stage phalloplasty [44]. Following the initial surgery, some patients choose to have a secondary procedure to improve aesthetic and functional outcomes. One study found secondary phalloplasty following primary metoidioplasty was done for the following reasons: to have a larger phallus (38.6%), to allow for penetrative sex (30.1%), and to void while standing (18.1%), while 20.5% of patients had a metoidioplasty done as the first step toward a phalloplasty [45]. In one study, 17% of 69 Trans masculine people who de-transitioned cited medical complications as the main reason [30].
Aside from sexual function outcomes, 93.9% of patients report tactile sensation and 92.2% of patients report an ability to void while standing following phalloplasty [43]. Across metoidioplasty techniques, an ability to void while standing was reported in most patients, with the lowest rate (67%) reported with the labial ring flap technique [46].
Trans Women
The optimal surgical techniques for sexual function have not been determined. One study stated that the goal is to create a canal that is “moist, elastic, hairless, at least 11 cm deep and at least 3 cm wide to allow for receptive intercourse” [35]. The neoclitoris is made from the glans penis, preserving the neuro-vascular bundle. The neurovascular bundle of the penis extends from 11 and 1 o’clock to the urethral spongiosum [47]. To surgically elevate the neurovascular bundle, the dissection needs to remain directly on top of the tunica albuginea to prevent neuronal injury. Therefore, as long as the surgical planes are respected, injury to the nerves should be avoided and sensation should be intact after surgery. However, up to 18% report uncomfortable or painful clitoral sensation after surgery [48]. Specifically, recession of the clitoral hood causes high risk of hypersensitivity. Fortunately, most individuals (70%) can achieve orgasm after revision of the clitoris and/or hood.
In a large cohort study of 869 patients undergoing vaginoplasty, 220 (25.3%) suffered at least one complication, with 97 developing a complication that required surgical intervention. The most common complications reported were bleeding (5.8%), stricture (3.2%), fistula (0.7%) and surgical site bleeding, breakdown or infection (5.7%) [49].
A more recent systematic review reported the incidence of vaginal stenosis following vaginoplasty to be 5.83% (range of 0%-34.2%) with the rate of vaginal stenosis greater in the penile inversion vaginoplasty subgroup compared to the primary intestinal vaginoplasty subgroup, 5.7% and 0.2% respectively [50].
Of those affected with vaginal stenosis, 73.5% of patients experienced difficulty with vaginal dilation in the post-operative period, indicating that stenosis of the neovagina is often related to discontinuation of dilation due to pain [51]. Vaginal dilation is required for all types of vaginoplasty that incorporate a canal. While surgeons differ on post-operative instructions, many recommend 3 times daily dilation for the first month, followed by twice daily for several months until only once daily is sufficient to keep the vaginal canal patent before regular penetrative sexual activity, if desired. This highly demanding schedule often leads to non-adherence and vaginal stenosis, most commonly in the first year post-operatively.
Revision surgery may include procedures to address complications, aesthetics, or functional issues. One study found that 40 out of 354 patients that underwent trans feminizing vaginoplasty required cosmetic revision surgery with no difference in revision prevalence between vaginoplasty techniques. The most frequent revisions are labiaplasty, clitoroplasty, mons venus, and urethral meatoplasty [52]. Another study found that up to 80% of patients undergo secondary procedures to optimize function or improve vulvar aesthetics [1].
Conclusion
Both medical and surgical affirmation care is improving with the overall goal of reducing gender dysphoria. Nevertheless, there are multiple areas for growth. Trans men and women undergo medical and surgical transitions in ways that affect sexual function and satisfaction. These sexual experiences can be directly correlated to gender affirming medical and surgical interventions. Overall, despite medical and specifically surgical complications, satisfaction with transition and sexual health is high. To better assess sexual health in this community, the authors stress the importance of tools to evaluate all aspects of sexual function and satisfaction that are unique to the TGDI population.
Data Availability
No datasets were generated or analysed during the current study.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Ramlachan P, Naidoo K. Enhancing sexual health in primary care: Guidance for Practitioners. South African Family Practice. 2024. https://doi.org/10.4102/safp.v66i1.5822.
Koops TU, Klein V, Bei der Kellen R, Hoyer J, Löwe B, Briken P. Association of sexual dysfunction according to dsm-5 diagnostic criteria with avoidance of and discomfort during sex in a population-based sample. Sex Med. 2023. https://doi.org/10.1093/sexmed/qfad037.
Holmberg M, Arver S, Dhejne C. Supporting sexuality and improving sexual function in transgender persons. Nat Rev Urol. 2018;16:121–39.
McCabe MP, Sharlip ID, Atalla E, Balon R, Fisher AD, Laumann E, Lee SW, Lewis R, Segraves RT. Definitions of sexual dysfunctions in women and men: A consensus statement from the Fourth International Consultation on Sexual Medicine 2015. J Sex Med. 2016;13:135–43.
Ramírez-Santos J, Cristóbal-Cañadas D, Parron-Carreño T, Lozano-Paniagua D, Nievas-Soriano BJ. The problem of calculating the prevalence of sexual dysfunction: A meta-analysis attending gender. Sex Med Rev. 2024. https://doi.org/10.1093/sxmrev/qead058.
Kachen A, Pharr JR. Health Care Access and utilization by transgender populations: A united states transgender survey study. Transgend Health. 2020;5:141–8.
Sahmoud A, Hamilton D, Pope R. A trauma-informed and gender-inclusive medical nomenclature. Obstet Gynecol. 2022;140:115–20.
Herman JL (2022) How many adults and youth identify as transgender in the United States?In:WilliamsInstitute.https://williamsinstitute.law.ucla.edu/publications/trans-adults-united-states/. Accessed 13 Mar 2024.
Kerckhof ME, Kreukels BPC, Nieder TO, Becker-Hébly I, van de Grift TC, Staphorsius AS, Köhler A, Heylens G, Elaut E. Prevalence of sexual dysfunctions in transgender persons: Results from the ENIGI follow-up study. J Sex Med. 2019;16:2018–29.
DeRogatis L, Clayton A, Lewis-D’Agostino D, Wunderlich G, Fu Y. Validation of the female sexual distress scale-revised for assessing distress in women with hypoactive sexual desire disorder. J Sex Med. 2008;5:357–64.
Alwaal A, Awad M, Boggs N, Kuzbel J, Snoad B. Sexual health inventory for men questionnaire as a screening method for erectile dysfunction in a General Urology Clinic. Sex Med. 2020;8:660–3.
Wiegel M, Meston C, Rosen R. The Female Sexual Function Index (FSFI): Cross-validation and development of Clinical Cutoff scores. J Sex Marital Ther. 2005;31:1–20.
Morrison TG, Bearden A, Ellis SR, Harriman R. Correlates of Genital Perceptions among Canadian Post-Secondary Students. Electron J Hum Sex. 2005;8:1–22.
Davis SNP, Binik YM, Amsel R, Carrier S. The index of Male Genital Image: A new scale to assess male genital satisfaction. J Urol. 2013;190:1335–9.
• Fraiman E, Goldblatt C, Loria M, Mishra K, Pope R. One survey fits all? evaluating the relevance of sexual function measures designed for CIS women in trans women post vaginoplasty. J Sex Med. 2023;20:1133–8. This study evaluated surveys used to assess sexual function in cis women. It found that all the surveys had questions irrelevant to transgender women’s experiences. Moreover, it highlighted the importance of creating surveys specific for the transgender population for an accurate assessment of sexual function and satisfaction.
• Mattawanon N, Charoenkwan K, Tangpricha V. Sexual dysfunction in transgender people. Urol Clin North Am. 2021;48:437–60. This systematic review analyzed data in the literature concerning sexual desire, arousal, orgasm, pain, and satisfaction in transmen and transwomen before, during and after transitioning.
Wierckx K, Van Caenegem E, Elaut E, et al. Quality of life and sexual health after sex reassignment surgery in transsexual men. J Sex Med. 2011;8:3379–88.
Ristori J, Cocchetti C, Castellini G, et al. Hormonal treatment effect on sexual distress in transgender persons: 2-year follow-up data. J Sex Med. 2019;17:142–51.
Grimstad FW, Boskey ER, Clark RS, Ferrando CA (2023) Prevalence of pelvic pain in transgender individuals on testosterone. In: OUP Academic. https://doi.org/10.1093/jsxmed/qdad135. Accessed 13 Mar 2024.
Zwickl S, Burchill L, Wong AF, et al. Pelvic pain in transgender people using testosterone therapy. LGBT Health. 2023;10:179–90.
Cerwenka S, Nieder TO, Cohen-Kettenis P, De Cuypere G, Haraldsen IR, Kreukels BP, Richter-Appelt H. Sexual behavior of gender-dysphoric individuals before gender-confirming interventions: A european multicenter study. J Sex Marital Ther. 2014;40:457–71.
De Cuypere G, TSjoen G, Beerten R, Selvaggi G, De Sutter P, Hoebeke P, Monstrey S, Vansteenwegen A, Rubens R. Sexual and physical health after sex reassignment surgery. Arch Sex Behav. 2005;34:679–90.
van de Grift TC, Pigot GLS, Boudhan S, et al. A longitudinal study of motivations before and psychosexual outcomes after genital gender-confirming surgery in transmen. J Sex Med. 2017;14:1621–8.
Becker I, Auer M, Barkmann C, Fuss J, Möller B, Nieder TO, Fahrenkrug S, Hildebrandt T, Richter-Appelt H. A cross-sectional multicenter study of Multidimensional body image in adolescents and adults with gender dysphoria before and after transition-related medical interventions. Arch Sex Behav. 2018;47:2335–47.
Wierckx K, Elaut E, Van Hoorde B, Heylens G, De Cuypere G, Monstrey S, Weyers S, Hoebeke P, T’Sjoen G. Sexual desire in trans persons: Associations with sex reassignment treatment. J Sex Med. 2014;11:107–18.
Defreyne J, Elaut E, Kreukels B, Fisher AD, Castellini G, Staphorsius A, Den Heijer M, Heylens G, T’Sjoen G. Sexual desire changes in transgender individuals upon initiation of hormone treatment: Results from the longitudinal European Network for the investigation of gender incongruence. J Sex Med. 2020;17:812–25.
Fein LA, Salgado CJ, Sputova K, Estes CM, Medina CA. Sexual preferences and partnerships of transgender persons mid- or post-transition. J Homosex. 2017;65:659–71.
Costantino A, Cerpolini S, Alvisi S, Morselli PG, Venturoli S, Meriggiola MC. A prospective study on sexual function and mood in female-to-male transsexuals during testosterone administration and after sex reassignment surgery. J Sex Marital Ther. 2013;39:321–35.
Fascelli M, Hennig F, Dy GW. Penile and testicular prosthesis following gender-affirming phalloplasty and scrotoplasty: A narrative review and technical insights. Transl Androl Urol. 2023;12:1568–80.
Marinelli L, Cagnina S, Bichiri A, Magistri D, Crespi C, Motta G. Sexual function of transgender assigned female at birth seeking gender affirming care: A narrative review. Int J Impot Res. 2023. https://doi.org/10.1038/s41443-023-00711-7.
Schardein JN, Nikolavsky D. Sexual functioning of transgender females post-vaginoplasty: Evaluation, outcomes and treatment strategies for sexual dysfunction. Sex Med Rev. 2022;10:77–90.
van Dijk D, Dekker MJHJ, Conemans EB, Wiepjes CM, de Goeij EGM, Overbeek KA, Fisher AD, den Heijer M, T’Sjoen G. Explorative prospective evaluation of short-term subjective effects of hormonal treatment in trans people—results from the European Network for the investigation of gender incongruence. J Sex Med. 2019;16:1297–309.
Cocchetti C, Ristori J, Mazzoli F, Vignozzi L, Maggi M, Fisher AD. Management of hypoactive sexual desire disorder in transgender women: A guide for clinicians. Int J Impot Res. 2021;33:703–9.
Hess J, Henkel A, Bohr J, Rehme C, Panic A, Panic L, Rossi Neto R, Hadaschik B, Hess Y. Sexuality after male-to-female gender affirmation surgery. Biomed Res Int. 2018;2018:1–7.
Buncamper ME, Honselaar JS, Bouman MB, Özer M, Kreukels BPC, Mullender MG. Aesthetic and functional outcomes of neovaginoplasty using penile skin in male to female transsexuals. J Sex Med. 2015;12:1626–34.
Weyers S, Elaut E, De Sutter P, Gerris J, T’Sjoen G, Heylens G, De Cuypere G, Verstraelen H. Long-term assessment of the physical, mental, and sexual health among transsexual women. J Sex Med. 2009;6:752–60.
Bouman M-B, van der Sluis WB, van Woudenberg Hamstra LE, Buncamper ME, Kreukels BPC, Meijerink WJHJ, Mullender MG. Patient-reported esthetic and functional outcomes of primary total laparoscopic intestinal vaginoplasty in transgender women with penoscrotal hypoplasia. J Sex Med. 2016;13:1438–44.
Rosen C, Brown J, Heiman S, Leib R. The Female Sexual Function Index (FSFI): A multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26:191–208.
Lawrence AA. Sexuality before and after male-to-female sex reassignment surgery. Arch Sex Behav. 2005;34:147–66.
Gil-Llario MD, Gil-Juliá B, Giménez-García C, Bergero-Miguel T, Ballester-Arnal R. Sexual behavior and sexual health of transgender women and men before treatment: Similarities and differences. Int J Transgend Health. 2020;22:304–15.
Kloer C, Parker A, Blasdel G, Kaplan S, Zhao L, Bluebond-Langner R. Sexual health after vaginoplasty: A systematic review. Andrology. 2021;9:1744–64.
Calotta NA, Coon D. Reply: Sensibility, sensation, and nerve regeneration after reconstructive genital surgery: Evolving Concepts in Neurobiology. Plast Reconstr Surg. 2022. https://doi.org/10.1097/prs.0000000000009279.
Wang AMQ, Tsang V, Mankowski P, Demsey D, Kavanagh A, Genoway K. Outcomes following gender affirming phalloplasty: A systematic review and meta-analysis. Sex Med Rev. 2022;10:499–512.
Huayllani MT, Boczar D, Saleem HY, Cinotto G, Avila FR, Manrique OJ, Ciudad P, Rinker BD, Forte AJ. Single versus two-stage phalloplasty for transgender female-to-male patients: A systematic review of the literature. Ann Transl Med. 2021;9:608–608.
Al-Tamimi M, Pigot GL, van der Sluis WB, et al. The surgical techniques and outcomes of secondary phalloplasty after Metoidioplasty in transgender men: An international, multi-center case series. J Sex Med. 2019;16:1849–59.
Jolly D, Wu CA, Boskey ER, Taghinia AH, Diamond DA, Ganor O. Is clitoral release another term for Metoidioplasty? A systematic review and meta-analysis of metoidioplasty surgical technique and outcomes. Sex Med. 2021;9:100294–100294.
Baskin LS, Erol A, Li YW, Liu WH. Anatomy of the neurovascular bundle: Is safe mobilization possible? J Urol. 2000;3:977–80.
Boas SR, Ascha M, Morrison SD, Massie JP, Nolan IT, Shen JK, Vyas KS, Satterwhite T. Outcomes and predictors of revision labiaplasty and clitoroplasty after gender-affirming genital surgery. Plast Reconstr Surg. 2019;144:1451–61.
Dallas K, Kuhlmann P, Zhao H, Scott V, Eilber K, Reyblat P, Anger J. PD31-08 complications after gender affirming vaginoplasty in a large population-based cohort. J Urol. 2021. https://doi.org/10.1097/ju.0000000000002032.08.
De Rosa P, Kent M, Regan M, Purohit RS. Vaginal stenosis after gender-affirming vaginoplasty: A systematic review. Urology. 2024. https://doi.org/10.1016/j.urology.2024.02.005.
Kozato A, Karim S, Chennareddy S, et al. Vaginal stenosis of the neovagina in transfeminine patients after gender-affirming vaginoplasty surgery. Plast Reconstr Surg Glob Open. 2021;9:75–75.
Mañero I, Arno AI, Herrero R, Labanca T. Cosmetic revision surgeries after transfeminine vaginoplasty. Aesthetic Plast Surg. 2022;47:430–41.
Author information
Authors and Affiliations
Contributions
RP and AS conceptualized the manuscript. RP, AS and AC drafted the manuscript. RP, AS AC and JA all contributed to editing, formatting and preparing the manuscript for publication.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sahmoud, A., Castellanos, A.R., Zeki, J.A. et al. Sexual Function After Gender Affirming Surgery. Curr Obstet Gynecol Rep 13, 128–135 (2024). https://doi.org/10.1007/s13669-024-00390-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13669-024-00390-1