Abstract
Purpose of Review
The Environmental Justice Movement centers on addressing inequitable distribution of environmental harms in marginalized communities. It has been commonly understood as the disproportionate concentration of environmental pollutants or hazards. As such, much of the work on environmental harms and maternal pregnancy complications have focused on environmental toxins. This scoping review surveyed the literature exploring the built and social environment factors and maternal pregnancy complications among racially marginalized women and highlights how an environmental justice framework can inform policy interventions for maternal health inequities caused by structural racism in built and social environments.
Recent Findings
The literature examining the association between neighborhood level built and social environment factors and maternal pregnancy complications in the last five years is sparse. When excluding environmental toxins, we identified 16 studies that fit our criteria of neighborhood-level environmental exposure, with the majority focused on built environment factors, specifically proximity to greenspace and food environment.
Summary
We identified a few important gaps and opportunities for future research in this area. First is a need to explore additional built environment elements. Secondly, extensive research is needed on the social environment. Third is a critical understanding to incorporate structural racism and cultural perspectives to better understand these relationships in minoritized populations and highlight the intersection between environmental hazards concentration and their structural causes. Finally, an environmental justice framework is critically needed in the interpretation and translation of this literature to inform policy solutions that can counteract the harms in racially marginalized communities and improve health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Across the USA, large and persistent racial inequities in maternal morbidity and mortality have been well documented, with maternal pregnancy complications contributing largely to both [1–3]. Much of this research examines individual level risk, as well as disparities in access to adequate health services and racial bias in healthcare settings [4, 5]. Increasingly, however, there is greater understanding of how structural racism harms health [6], and how broader social and structural factors shape reproductive health inequities in particular [7••, 8, 9•].
Due to historic and ongoing structural racism, manifest in residential segregation and the resulting concentration of poverty and underinvestment in racially and ethnically minoritized communities, health-harming exposures are often concentrated at the neighborhood level for racially marginalized groups [6, 10–16]. In this sense, environmental racism is a core pillar of structural racism, yet environmental epidemiology has too often failed to interrogate and integrate the role of racism as a driver of poor health and health inequities [17]. An environmental justice lens offers an opportunity to examine how neighborhood-level environments can create the conditions for improved maternal health and could contribute to narrowing racial inequities in maternal pregnancy complications [18, 19].
Environmental justice is defined by the Environmental Protection Agency (EPA) and other government agencies as “the fair treatment and meaningful involvement of all people regardless of race, color, national origin, or income with respect to the development, implementation and enforcement of environmental laws, regulations and policies” [20]. They further define that fair treatment means “no group of people should bear a disproportionate share of the negative environmental consequences resulting from industrial, governmental and commercial operations or policies” [20].
Most research exploring environmental factors and maternal pregnancy complications has centered on environmental pollutants, from air pollution to toxic waste and environmental chemicals [21,22,23,24,25], with environmental racism commonly understood as the disproportionate concentration of environmental pollutants or hazards in or near communities of color. However, a broader understanding of environmental racism to include the lack of access to beneficial built and social environmental resources such as greenspace, safe and affordable housing, quality education, nutrient-rich food, quality public transportation, treated water, and nature is needed to comprehensively address seemingly intractable inequities. The negative social and built environment consequences resulting from industrial, governmental, and commercial operations or policies are rarely explored in the literature or included in population level environmental justice interventions.
We conducted this scoping review with two primary objectives: (1) to survey the state of the literature exploring the association between neighborhood-level built and social environment factors and maternal pregnancy complications among racially marginalized women in the USA and (2) briefly highlight how an environmental justice framework can be used to offer policy and clinical interventions for maternal health inequities caused by structural racism in built and social environments.
Methods
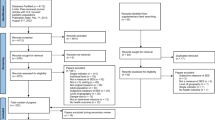
We searched peer-reviewed literature from January 2017 to January 2022 in databases known to index scholarship on neighborhood context, environmental factors, and maternal pregnancy complications from various sources and fields. These included PubMed, Academic Search Premier, and Environment Index. We also searched the reference lists of related articles to find additional relevant studies when applicable.
We developed a list of broad exposure terms after reviewing the structural racism and neighborhood literature. The broad terms included housing, policing, parks and greenspace, neighborhood segregation, schools, food environment, and public transportation. These broader terms were then broken down to reflect related concepts and cultural adaptions in the literature (i.e., ethnic enclaves vs segregation). Our outcome search terms included gestational diabetes, all maternal hypertension outcomes (gestational hypertension, preeclampsia, eclampsia, and HELLP), and gestational weight gain. We intentionally limited our search to maternal specific complications during pregnancy to center the experiences of birthing people rather than on the infant outcomes. Additionally, maternal specific complications are among the leading causes of severe maternal morbidity and mortality, but many can be intervened upon. Evidence suggests that inequitable distribution in these conditions drive many of the racial disparities we see for acute and chronic conditions that lead to increased mortality and morbidity like maternal hemorrhage and postpartum hypertension [2]. Corresponding MESH terms were identified for each exposure and outcome search term in PubMed, and this was used to develop the search strategy for Academic Search Premier and Environment Index.
To be included in the study, articles had to meet five criteria and be published within the last five years: (1) written in the English language, (2) based in the United States, (3) quantitative (qualitative studies, if any, will be included in discussion for future recommendations) (4) exposure: contextual factor measured at the neighborhood level, beyond environmental pollutants (5) outcome: defined maternal pregnancy complication (individual or at the neighborhood level).
The first and second authors (BB and AG) reviewed abstracts, read all full text articles, and extracted relevant data. Team meetings were used to adjudicate any inclusion discrepancies. Reference review and data extraction were conducted using Covidence web-based software.
Results
Our search returned 1,215 unique abstracts for screening after removal of duplicates. Authors discussed conflicts and agreed on which articles warranted further review. After screening all abstracts and removing duplicates, we reviewed 43 full-text articles. We excluded studies that were outside of the USA [3], not empirical [2], and did not measure social or built environment variables at the neighborhood level [14]. We also excluded studies that did not meet our outcome criteria [5], were intervention-based [1], review papers [1], and full text not available [1]. A total of 16 studies met our full eligibility criteria for inclusion in this review (see Table 1).
Retrospective cohort/observational study was the design most used to assess the association between neighborhood contextual factors and pregnancy complications [6]. Other studies used cross-sectional [4], prospective cohort [1], case–control [2], exposome-wide association [1], or time-series [1] study designs. One study employed an unclear design.
Six of the eligible studies included some measure of neighborhood food access/environment as a primary exposure, and five assessed neighborhood-level exposures of greenspace. Other studies used neighborhood-level residential segregation [2], crime [3], local expenditures [1], physical disorder [1], and proximity to roadways [1] as primary exposures. Studies assessed a variety of pregnancy complications. Outcomes included gestational diabetes, preeclampsia, eclampsia, gestational weight gain, and maternal morbidity. Among included studies, hypertensive disorders of pregnancy (HDP) were the most frequently studied outcome.
Three of the six studies that focused on the food environment examined living in neighborhoods classified by the USDA as “food deserts.” Pedersen et al. found that living in a food desert, characterized by the USDA as a low-income census tract that also has low access to food outlets, was associated with higher odds of experiencing a pregnancy morbidity and when examined separately the same association was also seen for preeclampsia [25]. Using the same measure but differing distances, neither Rammah et al. nor Tipton et al. found the same association when examining hypertensive disorders. However, Banner et al. did find that living in a food desert was associated with lower odds for gestational diabetes [22, 26]. Banner et al. developed a neighborhood asset index and found that pregnant individuals living in neighborhoods with low assets (high poverty/low retail) had higher BMI and C-reactive protein concentrations-cardiometabolic factors closely related to maternal pregnancy complications [27]. While Black women reported lower levels of assets compared to white women in the study, these relationships were not modified by race or ethnicity [27]. Two studies examined food access and gestational weight gain. Assibey-Mensah found that a higher number of grocery stores within 3 km was associated with lower odds of having excessive or inadequate gestational weight gain [28]. Grobman et al. found that living within a half-mile of culturally specific foods, specifically a Mexican restaurant, was associated with lower odds of excessive weight gain [29].
The studies focused on greenspace, walkability, and access to recreational facilities also showed varying results. Most studies found an inverse association with pregnancy related complications, while others found no association. Of those examining hypertensive disorders, Giuntella and Weber et al. conducted two studies that found that living in a neighborhood with higher percentages or higher density of greenspace (within a 100 or 500 m buffer) was associated with reduction in odds of maternal hypertension, specifically super imposed preeclampsia and severe preeclampsia [30, 31]. In one study, Weber et al. also found that these associations differed by neighborhood-level socioeconomic status [31]. Using the same measure of higher density of greenspace, but variable distances, Weber and Choe et al. found no association [32, 33]. Despite Weber et. al finding no association between greenspace and hypertension, they did show that living within 500 m of a recreational facility (parks, playgrounds, fishing, etc.) was associated with lower odds of gestational hypertension [32]. Hu et al. used a different measure of greenspace and found that living in neighborhoods with less available greenspace per person, less accessible greenspace within a 10-min walk, and less total available greenspace were associated with higher odds of gestational diabetes and preeclampsia [34].
When comparing ability to access greenspace within a 10-min walk, women in neighborhoods comprised predominantly of low-income Black residents were more likely to develop preeclampsia or gestational diabetes than neighborhoods comprised predominantly of high-income white residents [34]. When examining general walkability and proximity to parks in relation to gestational weight gain, Grobman et al. found an inverse association, where increases in walkability score and number of parks were associated with reduced odds in both excessive and inadequate weight gain [28]. Weber et al. also explored proximity to highways and found that living within close proximity of a major roadway was associated with higher odds of gestational diabetes, but no association for hypertensive disorders [32].
Of the studies that explored neighborhood contextual factors of the social environment, four explored crime, violence, or physical disorder, and two studies examined residential segregation. Galin et al. focused on crime, finding that living in neighborhoods with higher rates of violence and crime is associated with increased risk of excessive gestational weight gain [35]; among Asian and Pacific Islander women, they found that high exposure of neighborhood violence was associated with reduced risk of inadequate weight gain as well as increased risk of excessive weight gain [35].
Two studies examined neighborhood-level crime and maternal hypertension. Choe et al. found a positive association between increasing neighborhood crime and maternal hypertension, specifically when examining burglary and forcible sex offenses [33]. Galin et al. found a similar positive association between living in a neighborhood with high crime rates and odds of hypertensive disorders of pregnancy, particularly assaults and incivilities [36]. Another study done by Mayne et al. examined neighborhood physical disorder which was also shown to be associated with an increased prevalence for hypertensive disorders of pregnancy [37]. Both studies on segregation examined maternal hypertension and found positive associations. One study done by Mayne et al. found that residential segregation was associated with a higher prevalence ratio of hypertensive disorders of pregnancy among Black women living in the high poverty neighborhoods [38]. The other study, by Mayne et al. examined segregation through the practice of “redlining” and found that living in neighborhoods that were previously deemed “hazardous” was associated with higher odds of maternal hypertension compared to neighborhoods that were deemed “best” [39].
Expenditures on various neighborhood assets like policing, education, and greenspace was examined by Hollenbach et al. They documented that increases in spending on policing in a locality were associated with higher odds of severe maternal morbidity, while increases in spending on transportation and housing resulted in reduction of odds of severe morbidity [40].
Discussion
Our scoping review of the literature found that the research examining the association between neighborhood-level built and social environment factors and maternal pregnancy complications is sparse, especially in relation to structural racism for racially marginalized groups. When excluding environmental pollution and toxins, we identified only 16 studies in the last five years that fit our criteria of neighborhood-level environmental exposure, with the majority focused on built environment factors, and in particular proximity to greenspace and food access. Fewer papers were identified that focused on contextual neighborhood-level social environmental factors—with crime and physical disorder most examined. Collectively, these studies provide important information on the association between built and social environmental features and maternal pregnancy complications. These connections should be further explored in the literature, to complement studies exclusively focused on environmental hazards and pollutants.
In our exploration and synthesis of the literature, we identified a few important gaps. First, there has been limited exploration of other factors in the built environment that disproportionately impact racially marginalized communities such as access to safe and treated water, housing quality and access, transportation, and highway construction [41••, 42–44]. We do acknowledge however that this gap may primarily reflect our exclusion criteria (the fact that exposure had to be a contextual factor measured at the neighborhood level, beyond environmental pollutants).
Secondly, considerable research is still needed to examine the social environment, especially in relation to structural racism. There are many adverse social environmental factors that disproportionately impact racially marginalized neighborhoods over the life course. These conditions result from industrial, governmental, and commercial operations or policies such as over policing and hyper surveillance, poor school quality and inadequate educational access, unaffordable housing, mortgage discrimination, and acculturation. Such factors are not currently explored and likely interact and intersect with other forms of environmental racism to impact maternal pregnancy complications [45–51].
Understanding the social environment can help us move away from the narrative that “biological race” is a meaningful risk factor that increases risk of maternal pregnancy complications [9•, 52], but rather towards an understanding that the social environment plays a large role in access and exposure to key determinants of health, thus shaping health behaviors [9•]. Exploring some of these factors may also help elucidate why we see disparities for racially marginalized groups and inform policy solutions to combat them. Finally, these associations need to be explored critically in various racially marginalized groups and through a structural racism lens. Most of the studies included racially diverse samples but did not stratify analyses, examine interactions, or explicitly engage with an intersectional analysis. This specific examination is necessary given the historical and continued context of divestment at the neighborhood level for racially marginalized communities and that these associations may not behave the same in white populations or neighborhoods.
The available literature also points to a critical need to apply an environmental justice lens to guide future research on built and social environment factors and maternal pregnancy complications. Utilizing an environmental justice framework will help elucidate the numerous practices, policies, and environmental consequences at the neighborhood level that disproportionately burden racially marginalized groups and shape maternal health outcomes [53]. It will also point to why we see aggregation of social determinants of health at the neighborhood level and inform population health and clinical interventions. Additionally, as the environmental justice framework hinges on identifying solutions and tools to advance equity for the groups most impacted by the environmental racism [18], examining practices in the social and built environment and their harms on maternal pregnancy complications directly can be a useful way to inform policy solutions for equity. For example, Muchomba et al.’s study on municipal spending highlights that where and how we invest funding at the local level has lasting impacts for health outcomes [40]. As racially marginalized, over surveilled, and harassed communities call for diversion of funding away from policing into neighborhood level infrastructure and resources [54], examining these studies on the built and social environment through a structural racism and environmental justice framework shows how spending practices at the neighborhood level, specifically reallocation of funds from policing and into community infrastructure like greenspace, grocery stores, schools. and affordable housing, can be potentially meaningful environmental justice interventions for maternal morbidity and counteract the health impacts of over policing, discriminatory housing practices, and inequitable investment in education in racially minoritized communities [55–58].
Conclusion
We have witnessed a galvanization around sustainability and environmental health from industrial, government, and commercial agencies over the last decade in response to climate change and depleting natural resources. This shift has been critical in thinking about a sustainable planet and future. As we continue to invest in understanding the impacts of our environments on pregnancy and inter-generational wellbeing, it is necessary to examine the built and social environments that create racially disparate incidence in maternal pregnancy complications. A narrow definition of the environment, which does not consider the overlapping ways in which the built and social environment intersect with the more traditional understanding of environmental pollution and harm to shape reproductive health outcomes, is likely to result in interventions that are similarly narrow in scope and impact. To address injustices and disparities in maternal morbidity caused by inequitable environments, clinical interventions and policies should incorporate the Environmental Justice Principles outlined at the First National People of Color Environmental Leadership Summit in 1991 [18]. While all principles should be considered, particular attention should be given to the following: Principle 2, which requires public policy be based on mutual respect and justice, free from discrimination and bias; Principle 7, which requires equal participation in decision-making by impacted communities; and Principle 13, which underscores informed consent and the end to experimental reproductive or medical procedures on people of color. In addition, Principle 3 and Principle 12, which focus on the responsible uses of land and renewable resources, and the need for integrated urban and rural ecological policies, respectively, are foundational for any work that protects the health of our planet for humans and other living beings. More actionable research that bridges the literature on structural racism and environmental justice is needed as a first step to fundamentally address the stark racial inequities in maternal health outcomes and pregnancy complications.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Somer SJH, Sinkey RG, Bryant AS, editors. Epidemiology of racial/ethnic disparities in severe maternal morbidity and mortality. Seminars in perinatology; 2017: Elsevier.
Howell EA. Reducing disparities in severe maternal morbidity and mortality. Clin Obstet Gynecol. 2018;61(2):387.
Division of Reproductive Health NCfCDPaHP. Data on Selected Pregnancy Complications in the United States 2017 [Available from: https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pregnancy-complications-data.htm.
Lu MC. Reducing maternal mortality in the United States. JAMA. 2018;320(12):1237–8.
Petersen EE, Davis NL, Goodman D, Cox S, Syverson C, Seed K, et al. Racial/ethnic disparities in pregnancy-related deaths—United States, 2007–2016. Morb Mortal Wkly Rep. 2019;68(35):762.
Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. The Lancet. 2017;389(10077):1453–63.
Alson JG, Robinson WR, Pittman L, Doll KM. Incorporating measures of structural racism into population studies of reproductive health in the United States: A narrative review. Health Equity. 2021;5(1):49–58. This paper reviews existing measures of structural racism being explored in the reproductive literature and provides recommendations on future directions for research in this area.
Sutton MY, Anachebe NF, Lee R, Skanes H. Racial and ethnic disparities in reproductive health services and outcomes, 2020. Obstet Gynecol. 2021;137(2):225.
Crear-Perry J, Correa-de-Araujo R, Lewis Johnson T, McLemore MR, Neilson E, Wallace M. Social and structural determinants of health inequities in maternal health. Journal of Women's Health. 2021;30(2):230–5. This paper outlines how many of the social and structural inequities that shape maternal health in the U.S. are shaped by the social and political structures and policies in the U.S.
Riley AR. Neighborhood disadvantage, residential segregation, and beyond—lessons for studying structural racism and health. J Racial Ethn Health Disparities. 2018;5(2):357–65.
Sewell AA. The racism-race reification process: a mesolevel political economic framework for understanding racial health disparities. Sociology of Race and Ethnicity. 2016;2(4):402–32.
Krieger N, Van Wye G, Huynh M, Waterman PD, Maduro G, Li W, et al. Structural racism, historical redlining, and risk of preterm birth in New York City, 2013–2017. Am J Pub Health. 2020(0):e1-e8.
Acevedo-Garcia D, Lochner KA, Osypuk TL, Subramanian SV. Future directions in residential segregation and health research: a multilevel approach. Am J Public Health. 2003;93(2):215–21.
Kramer MR, Hogue CR. Is segregation bad for your health? Epidemiol Rev. 2009;31(1):178–94.
Diez Roux AV, Mair C. Neighborhoods and health. Ann N Y Acad Sci. 2010;1186(1):125–45.
Henderson S, Wells R. Environmental racism and the contamination of Black lives: a literature review. J Afr Am Stud. 2021;25(1):134–51.
Perry MJ, Arrington S, Freisthler MS, Ibe IN, McCray NL, Neumann LM, et al. Pervasive structural racism in environmental epidemiology. Environ Health. 2021;20(1):1–13.
The first national people of color environmental leadership summit: principles of environmental justice. Race, Poverty & the Environment. 1991;2(3/4):32–1.
Wilson SM. An ecologic framework to study and address environmental justice and community health issues. Environmental Justice. 2009;2(1):15–24.
Institute of Medicine Committee on Environmental J. The National Academies Collection: reports funded by National Institutes of Health. Toward Environmental Justice: Research, Education, and Health Policy Needs. Washington (DC): National Academies Press (US). Copyright © National Academy of Sciences.; 1999.
Varshavsky J, Smith A, Wang A, Hom E, Izano M, Huang H, et al. Heightened susceptibility: A review of how pregnancy and chemical exposures influence maternal health. Reprod Toxicol. 2020;92:14–56.
Rammah A, Whitworth KW, Symanski E. Particle air pollution and gestational diabetes mellitus in Houston. Texas Environmental Research. 2020;190:109988
Hu H, Ha S, Roth J, Kearney G, Talbott EO, Xu X. Ambient air pollution and hypertensive disorders of pregnancy: a systematic review and meta-analysis. Atmos Environ. 2014;97:336–45.
Bai W, Li Y, Niu Y, Ding Y, Yu X, Zhu B, et al. Association between ambient air pollution and pregnancy complications: a systematic review and meta-analysis of cohort studies. Environ Res. 2020;185:109471.
Pedersen M, Stayner L, Slama R, Sørensen M, Figueras F, Nieuwenhuijsen MJ, et al. Ambient air pollution and pregnancy-induced hypertensive disorders: a systematic review and meta-analysis. Hypertension. 2014;64(3):494–500.
Tipton MJ, Wagner SA, Dixon A, Westbay L, Darji H, Graziano S. Association of living in a food desert with pregnancy morbidity. Obstet Gynecol. 2020;136(1):140–5.
Banner GC, Weaver KN, Rushovich T, York SL, Yee LM. Association between food deserts and gestational diabetes mellitus in a large metropolitan area. Am J Perinatol. 2021;38(S 01):e39-e45.
Assibey-Mensah V, Fabio A, Mendez DD, Lee PC, Roberts JM, Catov JM. Neighbourhood assets and early pregnancy cardiometabolic risk factors. Paediatr Perinat Epidemiol. 2019;33(1):79–87.
Grobman WA, Crenshaw EG, Marsh DJ, McNeil RB, Pemberton VL, Haas DM, et al. Associations of the neighborhood built environment with gestational weight gain. Am J Perinatol 2021.
Giuntella O. Has the growth in “fast casual” Mexican restaurants impacted weight gain? Econ Hum Biol. 2018;31:115–24.
Weber KA, Lyons E, Yang W, Stevenson C, Stevenson DK, Shaw GM. Residential proximity to green space and preeclampsia in California. Environmental Epidemiology (Philadelphia, Pa). 2020;4(6).
Weber KA, Yang W, Lyons E, Stevenson DK, Padula AM, Shaw GM. Greenspace, air pollution, neighborhood factors, and preeclampsia in a population-based case-control study in California. Int J Environ Res Public Health. 2021;18(10):5127.
Choe S-A, Kauderer S, Eliot MN, Glazer KB, Kingsley SL, Carlson L, et al. Air pollution, land use, and complications of pregnancy. Sci Total Environ. 2018;645:1057–64.
Hu H, Zhao J, Savitz DA, Prosperi M, Zheng Y, Pearson TA. An external exposome-wide association study of hypertensive disorders of pregnancy. Environ Int. 2020;141:105797.
Runkle JD, Matthews JL, Sparks L, McNicholas L, Sugg MM. Racial and ethnic disparities in pregnancy complications and the protective role of greenspace: a retrospective birth cohort study. Sci Total Environ. 2022;808:152145.
Galin J, Abrams B, Leonard SA, Matthay EC, Goin DE, Ahern J. Living in violent neighbourhoods is associated with gestational weight gain outside the recommended range. Paediatr Perinat Epidemiol. 2017;31(1):37–46.
Mayne SL, Pool LR, Grobman WA, Kershaw KN. Associations of neighbourhood crime with adverse pregnancy outcomes among women in Chicago: analysis of electronic health records from 2009 to 2013. J Epidemiol Community Health. 2018;72(3):230–6.
Mayne SL, Pellissier BF, Kershaw KN. Neighborhood physical disorder and adverse pregnancy outcomes among women in Chicago: a cross-sectional analysis of electronic health record data. J Urban Health. 2019;96(6):823–34.
Mayne SL, Yellayi D, Pool LR, Grobman WA, Kershaw KN. Racial residential segregation and hypertensive disorder of pregnancy among women in Chicago: analysis of electronic health record data. Am J Hypertens. 2018;31(11):1221–7.
Hollenbach SJ, Thornburg LL, Glantz JC, Hill E. Associations between historically redlined districts and racial disparities in current obstetric outcomes. JAMA network open. 2021;4(9):e2126707-e.
Muchomba FM, Teitler J, Kruse L, Reichman NE. Municipality-level variation in severe maternal morbidity and association with municipal expenditures in New Jersey. JAMA network open. 2021;4(11):e2135161-e. This paper documents the associations between municipal spending practices and maternal morbidity, highlighting the importance of investment community level infastrastructure in improving health.
Tanana H, Combs J, Hoss A (2021) Water is life: law, systemic racism, and water security in Indian country. Health Security. 2021;19(S1):S-78-S-82.
Swope CB, Hernández D. Housing as a determinant of health equity: a conceptual model. Soc Sci Med. 2019;243:112571
Sanchez TW, Stolz R, Ma JS. Inequitable effects of transportation policies on minorities. Transp Res Rec. 2004;1885(1):104–10.
Karas D. The disparate impact of the interstate highway system on poor and minority communities in American Cities. New Visions for Public Affairs. 2015;7.
Perry A, Rothwell J, Harshbarger D. The devaluation of assets in Black neighborhoods: the case of residential property. Metropolitan Policy Program at Brookings. 2018.
Massey DS. Still the Linchpin: segregation and stratification in the USA. Race Soc Probl. 2020;12(1):1–12.
Retzlaff R. Connecting public school segregation with urban renewal and interstate highway planning: the case of Birmingham. Alabama J Plan History. 2020;19(4):256–80.
McArdle N, Acevedo-Garcia D. Consequences of segregation for children’s opportunity and wellbeing. 2017.
Ellen IG, Glied S. Housing, neighborhoods, and children’s health. Future Child. 2015;25(1):135–53.
Bower KM, Thorpe RJ Jr, Rohde C, Gaskin DJ. The intersection of neighborhood racial segregation, poverty, and urbanicity and its impact on food store availability in the United States. Prev Med. 2014;58:33–9.
Abraído-Lanza AF, Echeverría SE, Flórez KR. Latino immigrants, acculturation, and health: promising new directions in research. Annu Rev Public Health. 2016;37(1):219–36.
Johnson JD, Louis JM. Does race or ethnicity play a role in the origin, pathophysiology, and outcomes of preeclampsia? An expert review of the literature. Am J Obstet Gynec. 2020.
Corburn J. Concepts for studying urban environmental justice. Curr Environ Health Rep. 2017;4(1):61–7.
Cobbina-Dungy JE, Jones-Brown D. Too much policing: why calls are made to defund the police. Punishment & Society.0(0):14624745211045652.
DeVylder JE, Anglin DM, Bowleg L, Fedina L, Link BG. Police violence and public health. Annu Rev Clin Psychol. 2021.
Taylor WC, Floyd MF, Whitt-Glover MC, Brooks J. Environmental justice: a framework for collaboration between the public health and parks and recreation fields to study disparities in physical activity. J Phys Act Health. 2007;4(Suppl 1):S50-63.
Solomon D, Maxwell C, Castro A. Systemic inequality: displacement, exclusion, and segregation. Center for American Progress. 2019;7.
Smedley B, Stith A, Colburn L, Evans C, editors. Inequality in teaching and schooling: How opportunity is rationed to students of color in America. the right thing to do, the smart thing to do: enhancing diversity in the health professions: summary of the symposium on diversity in health professions in honor of Herbert W Nickens, MD Washington (DC): National Academies Press[Google Scholar]; 2001.
Funding
This project was done with the support by The JPB Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of Topical Collection on Environmental Exposures and Pregnancy Outcomes
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Butler, B., Gripper, A. & Linos, N. Built and Social Environments, Environmental Justice, and Maternal Pregnancy Complications. Curr Obstet Gynecol Rep 11, 169–179 (2022). https://doi.org/10.1007/s13669-022-00339-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13669-022-00339-2