Abstract
Breast cancer is the most commonly diagnosed cancer globally among women and is the leading cause of cancer death. Breast cancer prevention trials have shown up to 50% reduction in breast cancer incidence among women at increased risk for breast cancer with the use of chemopreventive agents. Despite such a large potential reduction in breast cancer risk, the uptake of these agents has been poor as compared with the use of preventive agents for other health outcomes. This review provides an update of the trials evaluating chemoprevention agents for breast cancer and highlights the populations likely to benefit from them. Healthcare providers need to be comfortable with the use of chemopreventive agents for breast cancer, as they are a real option for women at increased risk, particularly those with early precursor lesions. Work is ongoing to identify agents for estrogen receptor–negative cancer and agents with minimal toxicity for more general use.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
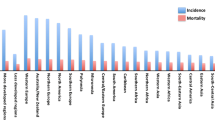
The cancer burden continues to increase around the globe because of increasing age and an expanding population. Among women, breast cancer is now the most commonly diagnosed cancer globally, accounting for 23% of the total cancer cases, and the leading cause of cancer death, with 14% of all cancer deaths attributed to it [1]. Agents have been identified that prevent estrogen receptor–positive breast cancer in both premenopausal and postmenopausal women at increased risk, with observed reductions in breast cancer incidence of up to 50%. Despite such a large potential reduction in breast cancer risk, the uptake of these agents has been poor when compared with the use of preventive agents for other health outcomes [2]. The poor uptake has been attributed to a combination of factors including both the adverse effect profile of these agents and the lack of knowledge and comfort of physicians (particularly gynecologists and primary care providers who deal with women’s health issues) concerning the prescribing of chemoprevention [3]. This review provides an update on chemoprevention agents for breast cancer and highlights the populations that are most likely to benefit.
Prevention of Estrogen Receptor–Positive Breast Cancer
Tamoxifen
Breast Cancer Effects
Tamoxifen belongs to the group of selective estrogen receptor modulators (SERMs) and behaves both as an estrogen antagonist in breast tissue and an agonist in the uterus, vagina, and liver [4]. The agonistic effects in the uterus and liver are associated with enhanced risk for uterine cancer and thromboembolic events. It also acts as a partial agonist on bone by inhibiting osteoclast activity [5], and on lipids by reducing low-density lipoprotein (LDL) [6]. The American Society of Clinical Oncology (ASCO), National Cancer Institute (NCI), National Comprehensive Cancer Network (NCCN), United States Preventive Services Task Force (USPSTF), and Canadian Task Force on Preventive Health Care (CTFPHC) currently recommend that tamoxifen (20 mg/day for 5 years) be considered as a preventive option for both premenopausal and postmenopausal women at increased risk of breast cancer, to reduce the risk of invasive ER-positive breast cancer (Table 1).
Contraindications for tamoxifen use include a prior history of deep venous thrombosis, pulmonary embolus, stroke, or transient ischemic attack. Further, a gynecologic examination at baseline before the initiation of tamoxifen and annually thereafter is recommended in the United States, along with a timely workup of abnormal vaginal bleeding.
The evidence demonstrating the clinical effectiveness of tamoxifen for reducing the risk of primary breast cancer comes from four large randomized controlled trials comparing tamoxifen (20 mg daily for 5 years) with placebo [7••]. The majority of study participants in all these trials were white, and outcomes by race or ethnic group were not reported. None of these trials were powered to evaluate breast cancer mortality or survival advantage. A meta-analysis of the four major tamoxifen prevention trials conducted predominantly in women at increased risk reported a 48% (95% CI, 36–58%; P < 0.0001) reduction in ER-positive breast cancer and no effect on the incidence of ER-negative breast cancer (HR, 1.22; 95% CI, 0.89–1.67) [8]. Below, we briefly discuss the composition and results pertaining to breast cancer risk for each of the trials, as their study populations varied, and later we summarize the adverse events in these trials.
The Breast Cancer Prevention Trial (P-1) initiated by the National Surgical Adjuvant Breast and Bowel Project (NSABP) was conducted between 1992 and 1997 [9]. Participants were 13,388 women who were at increased risk of breast cancer (defined as 35–59 years of age with 5-year breast cancer risk ≥ 1.66 using a modified Gail model, ≥ 60 years old, or with prior lobular carcinoma in situ). The women were randomly assigned to placebo or tamoxifen (20 mg/day orally) for 5 years. After a median follow-up of 4.6 years, tamoxifen use was associated with a 49% risk reduction in overall invasive breast cancers (RR, 0.51; 95% CI, 0.39–0.66) [9]. There was a 69% reduction in the risk of ER-positive breast cancer (RR, 0.31; 95% CI, 0.22–0.45) and no difference in ER-negative breast cancer. A similar risk reduction in ER-positive cancer among the tamoxifen group was observed across all age groups and all 5-year predicted risk strata for breast cancer. An even greater benefit was noted in women with atypical hyperplasia or a history of lobular carcinoma in situ. Tamoxifen use was also associated with a 50% reduction in the risk of noninvasive breast cancers (RR, 0.50; 95% CI, 0.33–0.77). Based on these results, the trial was unblinded and tamoxifen was approved for breast cancer prevention by the US Food and Drug Administration (FDA) in 1998. A persistent reduction in both invasive breast cancer (RR, 0.57; 95% CI, 0.46–0.70) and noninvasive breast cancer (RR, 0.63; 95% CI, 0.45–0.89) was observed at a median follow-up of 7 years [10]. The reduction in ER-positive breast cancer among the tamoxifen group was 62% (RR, 0.38; 95% CI, 0.28–0.50).The updated results should be interpreted with some caution, however, given that there was some crossover in treatment after unblinding.
Between 1992 to 2001, as part of the International Breast Intervention Study-1 (IBIS-1), 7,145 women aged 35 to 70 years at increased breast cancer risk were randomly assigned to tamoxifen (20 mg/day orally) or placebo for 5 years. Increased risk was defined as twofold, fourfold, and tenfold relative risk of breast cancer for women between the ages of 45–70, 40–44, and 35–39 years respectively. The primary outcome was the incidence of invasive and noninvasive breast cancer. Initial data for the IBIS-1 trial after a median follow-up of 50 months showed that tamoxifen use reduced overall risk of breast cancer (primarily ER-positive cancers) by 32% (OR, 0.68; 95% CI, 0.50–0.92) [11]. Unlike in the NSABP-1, most (89.1%) of the IBIS-1 participants opted to remain blinded after the primary results were reported, enabling prolonged follow-up. After a median follow-up of 96 months after randomization, an updated analysis showed a 27% risk reduction in overall breast cancer with tamoxifen use versus placebo (RR, 0.73; 95% CI, 0.58–0.91; P = 0.004); the reduction was 34% for ER-positive breast cancer (RR, 0.66; 95% CI, 0.50–0.87) [12]. Although slightly less, the benefit of tamoxifen continues to be observed for up to 10 years after randomization.
The Royal Marsden Tamoxifen Prevention Trial was a double-blinded tamoxifen/placebo breast cancer prevention trial that randomly assigned 2,494 healthy women to tamoxifen (20 mg/day orally) or placebo for 8 years between 1986 and 1996 [13]. The study population consisted of healthy women between 30 and 70 years of age without clinical or screening evidence of breast cancer, but with an increased risk due to a family history of breast cancer. Early results of the Royal Marsden trial did not observe a reduction in breast cancer [13], but a 20-year follow-up analysis showed a decrease in the breast cancer risk. The primary outcome of this trial was occurrence of invasive breast cancer, and at a median follow-up of 13 years, a 39% risk reduction for ER-positive invasive breast cancer was noted (HR, 0.61; 95% CI, 0.43–0.86; P = 0.005). This benefit was observed only during posttreatment follow-up (HR, 0.48; 95% CI, 0.29–0.79; P = 0.004) [14].
Lastly, the Italian Randomized Tamoxifen Prevention Trial [15], another randomized, double-blind, placebo-controlled trial, evaluated the chemopreventive efficacy of tamoxifen from 1992 to 1997 in 5,408 women between ages 35 and 70 years. These women had undergone a total hysterectomy, and 53% of participants also had bilateral oophorectomy, which reduces breast cancer risk in premenopausal women. They were assigned to tamoxifen (20 mg/day orally) or placebo for 5 years. After 11 years of follow-up, there was no statistically significant risk reduction in overall breast cancer risk (RR, 0.84; 95% CI, 0.60–1.17; P = 0.30). In the subgroup analysis, a risk reduction for ER-positive breast cancer was noted with tamoxifen use among women at high risk for breast cancer (RR, 0.24; 95% CI, 0.10–0.59). Only 13% of the participants in this trial were considered high-risk women, defined as being taller than 160 cm, having at least one intact ovary, being younger than age 14 years at menarche, and having no full-term pregnancy before age 24 years.
Adverse Events
In a meta-analysis of the tamoxifen prevention trials, Cuzick et al. [8] reported an increase in the risk of endometrial cancer with tamoxifen use (RR, 2.4; 95% CI, 1.5–4.0; P = 0.0005). Braithwaite et al. reported a similar risk in a meta-analysis that included 32 randomized trials in which tamoxifen was used for prevention and treatment (RR, 2.70; 95% CI, 1.94–3.75) [16]. Gail et al. performed a risk/benefit analysis based on participants in the NSABP P-1 trial at 7 years of followup. These data can be used to determine potential risk or benefit for patients of different ages [17]. Overall, women less than 50 years of age had the best risk/benefit profile. In the NSABP P-1 trial, the risk of endometrial cancer was not increased in women younger than age 50 (RR, 1.42; 95% CI, 0.55–3.81), but was enhanced fivefold (RR, 5.33; 95% CI, 2.47–13.17) in women at least 50 years of age [10]. Most cases of endometrial cancer in this trial were stage 1. A similar trend was also observed in the IBIS-I trial.
An enhanced risk of venous thromboembolic events was also reported in the meta-analysis of the chemoprevention trials (RR, 1.9; 95% CI, 1.4–2.6; P < 0.0001); the most frequent event was pulmonary embolism, followed by deep venous thrombosis and retinal vein thrombosis [8]. Interestingly in the IBIS trial, the increased risk of thromboembolic events with tamoxifen use was noted only during the active treatment (RR, 2.26; 95% Cl, 1.36–3.87), and this enhanced risk disappeared after tamoxifen was stopped (RR, 1.14; 95% CI, 0.52–2.53) [12]. An enhanced risk of ischemic stroke, particularly among women age 50 years or older, has also been reported in another meta-analysis (OR, 1.82; 95% CI, 1.41–2.36) [18]. An increased risk of stroke was observed in all of the cancer prevention trials except for the Royal Marsden trial, in which the participants were relatively young women. Hence tamoxifen is contraindicated in women with prior history of stroke or transient ischemic attack.
In the NSABP P-1 trial, there were significant increases in the incidence of cataracts (RR, 1.21; 95% CI, 1.10–1.34) and cataract surgery (RR, 1.39; 95% CI, 1.19–1.63) [10]. A similar but statistically nonsignificant trend for cataract with tamoxifen use was also noted in the Royal Marsden trial [14]. During the posttreatment period of the IBIS trial, the women on tamoxifen had a higher risk of cataracts (RR, 1.92; 95% CI, 1.12–3.29), although no difference was seen during the active phase [15].
Vaginal discharge (55%) and hot flashes (78%) were the main gynecologic and vasomotor symptoms reported during active treatment in the NSABP P-1 trial [9]. Similar effects were reported during active treatment in the IBIS-I and Royal Marsden trials [12, 14].
Reduction in fractures was a potential benefit. A 32% risk reduction in hip, spine, and radius fracture (RR, 0.68; 95% CI, 0.51–0.92) was reported in NSABP P-1 trial, with 90% of the fractures reported among women age 50 years and older. No such reduction was noted in the IBIS-I and Royal Marsden trials, both of which on average had younger women.
In the meta-analysis by Cuzick et al. [8], there was no overall effect of tamoxifen on all-cause mortality (HR, 0.90; 95% CI, 0.70–1.17; P = 0.44). However, it is important to understand that none of the chemoprevention trials were powered to determine survival. Nevertheless, a reduction in incidence, even if it does not translate into an improvement in survival but rather delays the development of cancer, is an important end point in itself. In addition, a cost-effectiveness meta-analysis of tamoxifen chemoprevention [19] reported that benefits of tamoxifen chemoprevention can compensate sufficiently for its side-effect profile in a postmenopausal population less than 55 years of age with a 5-year risk ≥1.66%. Tamoxifen use in this population was projected to save 85 quality-adjusted life years (QALYs) per 1,000 postmenopausal women less than 55 years of age, with cost savings of $47,580 compared with no treatment over lifetime follow-up.
Tamoxifen and Hormone Therapy
The use of hormone therapy along with tamoxifen has been evaluated in menopausal women in some of the prevention trials described above [12, 14, 15] with mixed results. The IBIS-1 trial reported no reduction in breast cancer incidence among women using combined therapy compared with placebo [12], whereas the Royal Marsden and Italian trials showed significant breast cancer risk reduction even among women receiving both tamoxifen and hormone therapy. An ongoing trial, Hormone replacement therapy Opposed by low dose Tamoxifen (HOT), is currently evaluating breast cancer risk in women taking low-dose tamoxifen (5 mg/d) with hormone therapy alone; we hope that it will help us to better understand the interaction of tamoxifen and hormone therapy [20]. Given the inconsistencies of existing data, combining tamoxifen and hormone is currently not recommended.
Raloxifene
Raloxifene, another SERM, was approved by the FDA in September, 2007, for the prevention of breast cancer only in high-risk postmenopausal women. The American Society of Clinical Oncology [7••] recommends that raloxifene (60 mg/d for 5 years) may be offered to reduce the risk of ER-positive invasive breast cancer in postmenopausal women with a 5-year projected breast cancer risk ≥1.66% or with lobular carcinoma in situ (LCIS). It may be used longer than 5 years in women with osteoporosis, in whom breast cancer risk reduction is a secondary benefit. Raloxifene should not be used for breast cancer prevention in premenopausal women and is not recommended for women with a prior medical history of deep venous thrombosis, pulmonary embolism, stroke, or transient ischemic attack. The impact on breast cancer mortality remains unknown.
Raloxifene is even better known for its use in the prevention and treatment of osteoporosis. Three of four randomized prospective trials have evaluated whether treatment with raloxifene affects breast cancer incidence. These four trials are the Multiple Outcomes of Raloxifene Evaluation (MORE) [21], Continuing Outcomes Relevant to Evista (CORE) [22], Raloxifene Use for The Heart (RUTH) [23], and the Study of Tamoxifen and Raloxifene (STAR) [24]. Only the STAR trial was designed specifically to study breast cancer incidence, based on the results from the other trials. The CORE study was conducted in women with osteoporosis and the RUTH Trial was in women with elevated coronary risk.
The NSABP, with support from the National Cancer Institute (NCI) initiated STAR in 1999 in postmenopausal women, with the primary end point being breast cancer incidence [24]. The STAR trial randomly assigned 19,747 postmenopausal women with high risk (based on a Gail model 5-year breast cancer risk of 1.66% or higher) to tamoxifen (20 mg/d) or raloxifene (60 mg/d) for 5 years. The 5-year projected breast cancer risk was higher in the STAR trial participants (58.7% with Gail-based 5-year breast cancer risk >3%) than in the NSABP P-1 trial participants (44% with a 5-year projected risk >3%). The mean age of the participants was 58.5 years; women receiving hormone therapy were excluded from the STAR trial, as were women with uncontrolled diabetes mellitus, hypertension, or a past history of stroke. About 51% of women had a prior hysterectomy, 9% had a history of breast LCIS, and 23% had a history of breast atypical hyperplasia (AH), compared with the NSABP P-1 trial, in which 37.1% had a history of hysterectomy, 6.3% of LCIS, and 9.1% of AH. The incidence of invasive breast cancer in the tamoxifen and raloxifene groups over a mean follow-up of 3.9 years did not differ significantly overall (RR, 1.02; 95% CI, 0.82–1.28). The estimates were similar for ER-positive tumors (RR, 0.94; 95% CI, 0.72–1.24). There were more noninvasive breast cancers in the raloxifene group (n = 80) than in the tamoxifen group (n = 57) (RR, 1.40; 95% CI, 0.98–2.00), but the difference was not statistically significant. Raloxifene also resulted in lower risk of endometrial cancer (RR, 0.62; 95% CI, 0.35–1.08), thromboembolic events (RR, 0.70; 95% CI, 0.54–0.91), osteoporotic fractures (RR, 0.79; 95% CI, 0.68–0.92), and cataracts (RR, 0.82; 95% CI, 0.68–0.99) than tamoxifen. Interestingly, in an updated analysis after a mean follow-up of 81 months, there was no significant difference between the raloxifene and tamoxifen groups in the incidence of invasive breast cancer (RR, 1.24; 95% CI, 1.05–1.47) or noninvasive breast cancer (RR, 1.22; 95% CI, 0.95–1.59) [25]. The risk of endometrial cancer was significantly lower with raloxifene than with tamoxifen, however (RR, 0.55; 95% CI, 0.36–0.83; P = 0.003) [25].
Risk-benefit analyses based on the results of the STAR trial suggest that for postmenopausal women at increased risk for breast cancer who have an intact uterus, the risk of using raloxifene as chemoprevention would be favored over tamoxifen because of the decreased endometrial cancer risk, whereas in postmenopausal women without a uterus, either agent could be considered. However, one must also consider the potentially higher age-related risks of side effects with tamoxifen. In postmenopausal women with osteoporosis, raloxifene would be the preferred option [26••].
Other SERMS
Lasofoxifene is another SERM that blocks the effects of estrogen in breast tissue. Its effects on breast cancer incidence were evaluated in the Postmenopausal Evaluation and Risk-Reduction with Lasofoxifene (PEARL) trial among women with osteoporosis. Breast cancer was one of the primary end points. At 5 years follow-up, a 48% risk reduction in ER-positive breast cancer was reported with low-dose lasofoxifene (0.25 mg) (RR, 0.52; 95% CI, 0.25–1.08) and an 81% reduction with high-dose lasofoxifene (0.50 mg) (RR, 0.19; 95% CI, 0.07–0.56) [27]. Lasofoxifene is more than 100 times more potent than raloxifene [28] and is currently approved in the European Union for the prevention and treatment of osteoporosis but not for breast cancer prevention.
Arzoxifene, a third-generation SERM, and Acolbifene, a fourth-generation SERM, have shown promising higher potency in preclinical models, as compared with tamoxifen and raloxifene, for inhibiting the growth of tamoxifen-sensitive tumors [29]. The results from a pivotal phase 3 study in 2011 (the GENERATIONS trial) showed that arzoxifene significantly reduced the risk of vertebral fractures and invasive breast cancer in postmenopausal women [30]. These new-generation SERMs are still under investigation.
Aromatase Inhibitors
Role of aromatase inhibitors (AIs) in the primary prevention of breast cancer is supported by adjuvant studies comparing AIs and tamoxifen in preventing the incidence of a second primary breast cancer (contralateral breast cancer). The ExCEL trial (Exemestane in Preventing Cancer in Post-menopausal Women at Increased Risk of Developing Breast Cancer) [31] compared exemestane (25 mg daily) with placebo in 4,560 postmenopausal women at increased risk for breast cancer (Gail risk score >1.66%, age >60 years, prior atypical ductal or lobular hyperplasia, or ductal carcinoma in situ [DCIS] treated with mastectomy). This trial was recently unblinded and the results were published. It was initially planned to randomly assign women to 3 years of treatment with exemestane, exemestane plus celecoxib, or placebo. However, because of the increase in cardiovascular events reported with the use of rofecoxib and celecoxib in the colon cancer prevention trial [32], the celecoxib arm of ExCEL was stopped. The others arms were continued until a median follow-up of 35 months, when the trial was unblinded because the reduction in the incidence of invasive breast cancer was greater than expected in the exemestane group. Compared with placebo, a 65% risk reduction in breast cancer (HR, 0.35; 95% CI, 0.18–0.70; P = 0.002) was observed in the exemestane group. This decrease was significant only for ER-positive breast cancer (HR, 0.27; 95% CI, 0.12–0.60). There was no risk reduction in the women with DCIS. Adverse effects among women taking exemestane included hot flashes in 40% (P < 0.001), fatigue in 23% (P = 0.03), insomnia in 10% (P = 0.04), arthritis in 11% (P = 0.01), arthralgia in 30% (P = 0.04), and myalgia in 7% (P = 0.01). Differences in effects such as fractures, incidence of other cancers, and hypercholesterolemia were not statistically significant between the two groups. As a result of the short follow-up, we will need to depend on data in the treatment setting to help inform long-term effects of exemestane, a key factor when considering any preventive agent. Factors such as arthritis are concerning; bone loss appears to be a transient effect, based on one study. Although it has not been FDA-approved, it is a potential option for postmenopausal women, including women in whom the other agents are contraindicated. Guidelines are now being updated.
The International Breast Cancer Intervention IBIS-II trial is comparing anastrozole to placebo in postmenopausal women at increased risk of breast cancer. Entry criteria are similar to those for IBIS-I, except that women with mammographic density covering at least 50% of the breast are also eligible [33]. All these trials are accompanied by substudies looking at quality of life and effects on other important issues such as bone metabolism. The results of these ongoing trials are awaited with much interest and will help to clarify the role of AIs as breast cancer preventive therapy.
Prevention of Estrogen Receptor–Negative Breast Cancer
ER-negative breast cancer accounts for almost 30% of all breast cancer in Caucasian populations and 40% or higher in African Americans. All breast cancer risk reduction trials evaluating SERMs and AIs have reported risk reduction in only in ER-positive breast cancer, so ER-negative breast cancer remains a challenge for prevention strategies. Several agents are being investigated.
Tyrosine Kinase Inhibitors
Lapatinib is a tyrosine kinase inhibitor that targets both human epidermal growth factor receptor 2 (HER-2) and epidermal growth factor receptor (EGFR) tyrosine kinases. It is currently approved in combination with letrozole for the treatment of postmenopausal women with HER-2–positive metastatic breast cancer. Initial reports from the LAPIS trial (Lapatinib in Treating Women With Ductal Carcinoma In Situ of the Breast) evaluating its effect in women with HER-2–positive or EGFR-positive DCIS [34] have shown that short-term lapatinib decreases cell proliferation in ductal intraepithelial neoplasia, ductal hypertrophy, and invasive HER-2–positive (especially ER-negative) breast cancer. Thus this trial provides a possible rationale for future evaluation of lapatinib as preventive therapy for HER-2–positive breast cancer.
3-Hydroxy-3-Methylglutaryl Coenzyme A (HMG-CoA) Inhibitors (Statins)
Support for lipophilic statins as preventive therapy comes from Women’s Health Initiative study analysis showing a reduced risk of breast cancer with lipophilic statins only [35]. Additional evidence to support this hypothesis comes from retrospective cohort analysis that showed a lower frequency of ER-negative breast cancer in women taking statins for more than a year [36]. Recently published results of a pilot study also suggest that statins have some biologic effects, with reduced tumor proliferation in the high-grade subset of early breast cancer [37]. Several phase 2 prevention trials are ongoing at the NCI, evaluating the role of lipophilic statins in breast cancer prevention (JHOC-J0485, V0407, BRSNSTU0010). Further evidence is therefore needed to establish statins as preventive therapy for breast cancer.
Metformin
Metformin is an oral hypoglycemic agent used for type 2 diabetes and polycystic ovary syndrome. Metformin primarily inhibits hepatic glucose production, but it also increases the sensitivity of peripheral tissue to insulin, therefore reducing both hyperglycemia and hyperinsulinemia. Metformin is thought to have an antiproliferative effects through mechanism of reducing hyperinsulinemia and activation of the adenosine monophosphate-activated protein kinase (AMPK) pathway, which may result in inhibition of cellular protein synthesis and growth of tumor cells [38]. Moreover, metformin has been shown to inhibit the growth of breast cancer cells in vitro and of tumors in vivo [39]. The European Institute of Oncology in Milan is currently conducting a two-arm phase 2 clinical trial testing metformin against placebo in women with early breast cancer.
Bisphosphonates
Bisphosphonates, used for the prevention and treatment of osteoporosis, reduce bone metastasis-related bone fractures and may have a role in prevention. Rennert et al. [40] reported a 28% breast cancer risk reduction among bisphosphonate users in a population-based case–control study in Northern Israel, and Chlebowski et al. [41] reported a 30% breast cancer risk reduction in a prospective study of the Women's Health Initiative (WHI) among bisphosphonate users. This reduction in breast cancer incidence was statistically significant only for ER-positive breast cancer. Based on preclinical studies, it has been hypothesized that bisphosphonates can affect angiogenesis by reducing vascular endothelial growth factor (VEGF), therefore inducing apoptosis, in addition to reducing proliferation and preventing invasion of the extracellular matrix [42]. Additional evidence is therefore needed to establish bisphosphonates as preventive therapy.
Retinoids
The ability of retinoids to prevent cancer has been demonstrated in various animal models. Fenretinide, a derivative of retinoic acid, was studied as a preventive agent for second primary breast cancers and showed no overall reduction in risk, but it did demonstrate a significant risk reduction (38%) for second breast cancers among premenopausal women [43]. Retinoids are currently not recommended as breast cancer preventive therapy.
Poly ADP-Ribose Polymerase (PARP) Inhibitors
Poly ADP-ribose polymerases (PARPs) are a family of enzymes that are involved in DNA repair, maintaining the genomic integrity of the cell and in turn influencing cell survival [44]. In tumor cells, PARP inhibitors generate unrepaired DNA single-strand breaks, causing DNA double-strand breaks and collapsed replication forks that otherwise would be repaired by PARP enzymes [45]. Their ability to selectively kill tumor cells while posing no threat to normal cells and their good tolerability profile make PARP inhibitors potential candidates for breast cancer preventive therapy. Currently there is insufficient evidence to recommend the use of PARP inhibitors as preventive therapy for breast cancer.
Implementation of Breast Cancer Preventive Therapy
Risk Assessment and Risk Models
Several mathematical models are available for use in clinical practice (Table 2) to estimate the risk of developing breast cancer on the basis of a combination of family history, reproductive history, age, hormonal factors, benign breast disease, and race or ethnicity [46]. These models have only moderate discriminatory accuracy, so they are not yet optimal for determining an individual’s breast cancer risk, but they are useful to determine an individual’s eligibility for chemoprevention [47]. The most widely used risk assessment tool is the Breast Cancer Risk Assessment Tool (BCRAT) [48]. This is a modified version of the Gail models and was used to determine eligibility for the NSABP P-1 and P-2 trials and the STAR trial, based on a 5-year risk of 1.66% or greater. It was initially validated in a screening population known as the Breast Cancer Detection Demonstration Project (BCDDP) and the Contraceptive and Reproductive Experiences (CARE) Trial. There is also now a modified version of this tool for African Americans, based on the CARE study [49]. Other risk assessment models include the Claus [50] or the TyrerCuzick [51] models, which also incorporate detailed family history. The Tyrer-Cuzick model predicts 10-year breast cancer development by including a family history of breast and ovarian cancer along with nongenetic risk factors; it was used for breast cancer risk assessment in the UK International Breast Cancer Intervention Study (IBIS). It appears to have improved discriminant accuracy in women with a strong family history [47].
Barriers to Prescribing Chemoprevention
Despite the potential benefit, the use of preventive agents to reduce breast cancer incidence has been extremely low. Armstrong and colleagues conducted a random survey of US primary care practices including internal medicine, obstetrics and gynecology, and family medicine and reported that very few primary care physicians are prescribing tamoxifen for chemoprevention because of lack of experience in determining patient eligibility, lack of patient demand, and lack of personal experience with breast cancer patients [4]. Other reasons from studies include poor physician-patient communication, inadequate time for counseling, self-perceived low risk for breast cancer, lack of belief that tamoxifen prevents breast cancer, unfavorable risk-benefit ratio, and concerns about potentially fatal effects such as pulmonary embolism, deep venous thrombosis, and endometrial cancer [52–56]. Using the Gail model criteria (women at least 35 years of age with a 5-year risk of breast cancer of at least 1.67%), more than 15% of women in the general population are eligible for chemoprevention [57]. A 2010 systematic review evaluating rates of breast cancer chemoprevention using tamoxifen or raloxifene reported the use of breast cancer preventive therapy to be 14.7%, but this use dropped to less than 5% after exclusion of patients participating in clinical trials [58].
Conclusions
Despite the advances in chemoprevention for ER-positive breast cancer in women at high risk and the demonstration that it can be cost-effective, agents such as tamoxifen and raloxifene are not being widely used even when the benefits may outweigh the risk (and raloxifene has additional benefits). Therefore in addition to identifying less toxic agents and agents that are effective in preventing ER-negative cancer, we need to develop more effective means of educating and updating healthcare providers about the use of these agents and the incorporation of breast cancer risk assessment more easily into clinical practice.
References
Recently published papers of interest have been highlighted as: •• Of major importance
Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90.
Waters EA, Cronin KA, Graubard BI, et al. Prevalence of tamoxifen use for breast cancer chemoprevention among U.S. women. Cancer Epidemiol Biomarkers Prev. 2010;19:443–6.
Armstrong K, Quistberg DA, Micco E, et al. Prescription of tamoxifen for breast cancer prevention by primary care physicians. Arch Intern Med. 2006;166:2260–5.
Fabian CJ, Kimler BF. Selective estrogen-receptor modulators for primary prevention of breast cancer. J Clin Oncol. 2005;23:1644–55.
Love RR, Mazess RB, Barden HS, et al. Effects of tamoxifen on bone mineral density in postmenopausal women with breast cancer. N Engl J Med. 1992;326:852–6.
Love RR, Wiebe DA, Newcomb PA, et al. Effects of tamoxifen on cardiovascular risk factors in postmenopausal women. Ann Intern Med. 1991;115:860–4.
•• Visvanathan K, Chlebowski RT, Hurley P, et al.: American Society of Clinical Oncology clinical practice guideline update on the use of pharmacologic interventions including tamoxifen, raloxifene, and aromatase inhibition for breast cancer risk reduction. J Clin Oncol 2009, 27:3235-58. This article provides recommendations for chemoprevention of breast cancer from the American Society of Clinical Oncology, includes a discussion of the chemoprevention trials in detail, and also touches on implementation strategies.
Cusick J, Powles T, Veronesi U, et al. Overview of the main outcomes in breast-cancer prevention trials. Lancet. 2003;361:296–300.
Fisher B, Costantino JP, Wickerham DL, et al. Tamoxifen for prevention of breast cancer: report of the national surgical adjuvant breast and bowel project P-1 study. J Natl Cancer Inst. 1998;90:1371–88.
Fisher B, Costantino JP, Wickerham DL, et al. Tamoxifen for the prevention of breast cancer: current status of the National Surgical Adjuvant Breast and Bowel Project P-1 study. J Natl Cancer Inst. 2005;97:1652–62.
Cuzick J, Forbes J, Edwards R, IBIS investigators, et al. First results from the International Breast Cancer Intervention Study (IBIS-I): a randomised prevention trial. Lancet. 2002;360:817–24.
Cuzick J, Forbes JF, Sestak I, et al. Long-term results of tamoxifen prophylaxis for breast cancer—96-month follow-up of the randomized IBIS-I trial. J Natl Cancer Inst. 2007;99:272–82.
Powles T, Eeles R, Ashley S, et al. Interim analysis of the incidence of breast cancer in the Royal Marsden hospital tamoxifen randomized chemoprevention trial. Lancet. 1998;352:98–101.
Powles TJ, Ashley S, Tidy A, et al. Twenty-year follow-up of the Royal Marsden randomized, double-blinded tamoxifen breast cancer prevention trial. J Natl Cancer Inst. 2007;99:283–90.
Veronesi U, Maisonneuve P, Rotmensz N, et al. Tamoxifen for the prevention of breast cancer: late results of the Italian Randomized Tamoxifen Prevention Trial among women with hysterectomy. J Natl Cancer Inst. 2007;99:727–37.
Braithwaite RS, Chlebowski RT, Lau J, et al. Meta-analysis of vascular and neoplastic events associated with tamoxifen. J Gen Intern Med. 2003;18:937–47.
Gail MH, Costantino JP, Bryant J, et al. Weighing the risks and benefits of tamoxifen treatment for preventing breast cancer. J Natl Cancer Inst. 1999;91:1829–46.
Bushnell CD, Goldstein LB. Risk of ischemic stroke with tamoxifen treatment for breast cancer: a meta-analysis. Neurology. 2004;12:1230–3.
Noah-Vanhoucke J, Green LE, Dinh TA, et al. Cost-effectiveness of chemoprevention of breast cancer using tamoxifen in a postmenopausal US population. Cancer. 2011;117:3322–31.
Bonanni B, Maisonneuve P, Serrano D, et al.: Safety and efficacy of HRT and low-dose tamoxifen in a phase II trial (HOT): Analysis of mammographic density and endometrial thickness. J Clin Oncol 29: 2011 (suppl; abstr 1527).
Cummings SR, Eckert S, Krueger KA, et al. The effect of raloxifene on risk of breast cancer in postmenopausal women: results from the MORE randomized trial. Multiple Outcomes of Raloxifene Evaluation. JAMA. 1999;281:2189–97.
Martino S, Cauley JA, Barrett-Connor E, et al. Continuing outcomes relevant to Evista: breast cancer incidence in postmenopausal osteoporotic women in a randomized trial of raloxifene. J Natl Cancer Inst. 2004;96:1751–61.
Barrett-Connor E, Mosca L, Collins P, et al. Effects of raloxifene on cardiovascular events and breast cancer in postmenopausal women. N Engl J Med. 2006;355:125–37.
Land SR, Wickerham DL, Costantino JP, et al. Patient-reported symptoms and quality of life during treatment with tamoxifen or raloxifene for breast cancer prevention: the NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 trial. JAMA. 2006;295:2742–51.
Vogel VG, Costantino JP, Wickerham DL, et al. Update of the national surgical adjuvant breast and bowel project Study of Tamoxifen and Raloxifene (STAR) P-2 trial: preventing breast cancer. Cancer Prev Res (Phila). 2010;3:696–706.
•• Freedman AN, Yu B, Gail MH, et al.: Benefit/risk assessment for breast cancer chemoprevention with raloxifene or tamoxifen for women age 50 years or older. J Clin Oncol 2011, 29:2327-33. This article provides the most recent risk/benefit analyses for tamoxifen and raloxifene in women age 50 or above and can be used to inform clinical practice.
Cummings SR, Ensrud K, Delmas PD, et al. Lasofoxifene in postmenopausal women with osteoporosis. N Engl J Med. 2010;362:686–96.
Lerner LJ, Jordan VC. Development of antiestrogens and their use in breast cancer: eighth Cain memorial award lecture. Cancer Res. 1990;50:4177–89.
Roy J, Couillard S, Gutman M, et al. A novel pure SERM achieves complete regression of the majority of human breast cancer tumors in nude mice. Breast Cancer Res Treat. 2003;81:223–9.
Cummings SR, McClung M, Reginster JY, et al. Arzoxifene for prevention of fractures and invasive breast cancer in postmenopausal women. J Bone Miner Res. 2011;26:397–404.
Goss PE, Ingle JN, Ales-Martinez JE, et al. Exemestane for breast-cancer prevention in postmenopausal women. N Engl J Med. 2011;364:2381–91.
Solomon SD, McMurray JJ, Pfeffer MA, et al. Cardiovascular risk associated with celecoxib in a clinical trial for colorectal adenoma prevention. N Engl J Med. 2005;352:1071–80.
Anastrozole in Preventing Breast Cancer in Postmenopausal Women at Increased Risk of Breast Cancer. ClinicalTrials.gov Identifier: NCT00078832.
Decensi A, Puntoni M, Pruneri G, et al. Lapatinib activity in premalignant lesions and HER-2-positive cancer of the breast in a randomized, placebo-controlled presurgical trial. Cancer Prev Res (Phila). 2011;4:1181–9.
Cauley JA, McTiernan A, Rodabough RJ, et al. Statin use and breast cancer: prospective results from the Women’s Health Initiative. Natl Cancer Inst J. 2006;98:700–7.
Kumar AS, Benz CC, Shim V, et al. Estrogen receptor-negative breast cancer is less likely to arise among lipophilic statin users. Cancer Epidemiol Biomarkers Prev. 2008;17:1028–33.
Garwood ER, Kumar AS, Baehner FL, et al. Fluvastatin reduces proliferation and increases apoptosis in women with high grade breast cancer. Breast Cancer Res Treat. 2010;119:137–44.
Shaw RJ, Lamia KA, Vasquez D, et al. The kinase LKB1 mediates glucose homeostasis in liver and therapeutic effects of metformin. Science. 2005;310:1642–6.
Pollak M. Metformin and other biguanides in oncology: advancing the research agenda. Cancer Prev Res (Phila). 2010;3:1060–5.
Rennert G, Pinchev M, Rennert HS. Use of bisphosphonates and risk of postmenopausal breast cancer. Clin Oncol J. 2010;28:3577–81.
Chlebowski RT, Chen Z, Cauley JA, et al. Oral bisphosphonate use and breast cancer incidence in postmenopausal women. J Clin Oncol. 2010;28:3582–90.
Lipton A. Emerging role of bisphosphonates in the clinic–antitumor activity and prevention of metastasis to bone. Cancer Treat Rev. 2008;34 Suppl 1:S25–30.
Veronesi U, Mariani L, Decensi A, et al. Fifteen-year results of a randomized phase III trial of fenretinide to prevent second breast cancer. Ann Oncol. 2006;17:1065–71.
Amé JC, Spenlehauer C, de Murcia G. The PARP superfamily. Bioessays. 2004;26:882–93.
Sandhu SK, Yap TA, de Bono JS. Poly (ADP-ribose) polymerase inhibitors in cancer treatment: a clinical perspective. Eur J Cancer. 2010;46:9–20.
Bozovic-Spasojevic I, Azambuja E, McCaskill-Stevens W, et al.: Chemoprevention for breast cancer. Cancer Treat Rev 2011 Aug 17 (Epub ahead of print).
Amir E, Freedman OC, Seruga B, et al. Assessing women at high risk of breast cancer: a review of risk assessment models. J Natl Cancer Inst. 2010;102:680–91.
Gail MH, Brinton LA, Byar DP, et al. Projecting individualized probabilities of developing breast cancer for white females who are being examined annually. J Natl Cancer Inst. 1989;81:1879–86.
Gail MH, Costantino JP, Pee D, et al. Projecting individualized absolute invasive breast cancer risk in African American women. J Natl Cancer Inst. 2007;99:1782–92.
Claus EB, Risch N, Thompson WD. Autosomal dominant inheritance of early-onset breast cancer: implications for risk prediction. Cancer. 1994;73:643–51.
Tyrer J, Duffy SW, Cuzick J. A breast cancer prediction model incorporating familial and personal risk factors. Stat Med. 2004;23:1111–30.
Bober SL, Hoke LA, Duda RB, et al. Decision-making about tamoxifen in women at high risk for breast cancer: clinical and psychological factors. J Clin Oncol. 2004;22:4951–7.
Melnikow J, Paterniti D, Azari R, et al. Preferences of Women Evaluating Risks of Tamoxifen (POWER) study of preferences for tamoxifen for breast cancer risk reduction. Cancer. 2005;103:1996–2005.
Taylor R, Taguchi K. Tamoxifen for breast cancer chemoprevention: low uptake by high-risk women after evaluation of a breast lump. Ann Fam Med. 2005;3:242–7.
Fagerlin A, Zikmund-Fisher BJ, Nair V, et al. Women’s decisions regarding tamoxifen for breast cancer prevention: responses to a tailored decision aid. Breast Cancer Res Treat. 2010;119:613–20.
Ravdin PM. The lack, need, and opportunities for decision-making and informational tools to educate primary-care physicians and women about breast cancer chemoprevention. Cancer Prev Res (Phila). 2010;3:686–8.
Freedman AN, Graubard BI, Rao SR, et al. Estimates of the number of US women who could benefit from tamoxifen for breast cancer chemoprevention. J Natl Cancer Inst. 2003;95:526–32.
Ropka ME, Keim J, Philbrick JT. Patient decisions about breast cancer chemoprevention: a systematic review and meta-analysis. J Clin Oncol. 2010;28:3090–5.
Disclosure
No potential conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Khaliq, W., Visvanathan, K. Breast Cancer Chemoprevention: Current Approachesand Future Directions. Curr Obstet Gynecol Rep 1, 33–41 (2012). https://doi.org/10.1007/s13669-011-0005-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13669-011-0005-0