Abstract
Purpose of Review
Time-restricted eating (TRE), a form of intermittent fasting, restricts feeding time across the day, imposing a daily ‘eating window’. The time of day when the eating window occurs could result in differential metabolic effects. Here, we describe recent intervention studies in humans assessing the metabolic consequences of an early- (i.e., eating window starting in the early morning) vs. late (i.e., eating window starting after midday)-TRE protocol.
Recent Findings
Well-controlled studies indicate that both TRE protocols effectively reduce body weight and improve altered glucose metabolism, lipid profile, inflammation, or blood pressure levels. An early-TRE (e-TRE) might have a further positive impact on improving blood glucose, insulin levels, and insulin resistance. However, the studies directly assessing the metabolic consequences of an early- vs. late-TRE have shown dissimilar findings, and more well-controlled clinical trials are needed on the metabolic benefits of these two types of TRE.
Summary
Evidence suggests that an e-TRE might have enhanced metabolic results, particularly regarding glucose homeostasis. More long-term studies, including larger sample sizes, are needed to assess the metabolic, circadian, and adherence benefits, together with socio-cultural acceptance of both TRE approaches.

Similar content being viewed by others
Data Availability
No datasets were generated or analysed during the current study.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Abarca-Gómez L, Abdeen ZA, Hamid ZA, Abu-Rmeileh NM, Acosta-Cazares B, Acuin C, et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. The Lancet. 2017;390:2627–42.
World Health Organization (W.H.O.). Obesity and overweight. (updated 2024 March 1). Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
Saklayen MG. The global epidemic of the metabolic syndrome. Curr Hypertens Rep. 2018;20:12.
Kelly T, Yang W, Chen CS, Reynolds K, He J. Global burden of obesity in 2005 and projections to 2030. Int J Obes. 2008;32:1431–7.
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet. 2014;384:766–81.
WHO Consultation on Obesity (1999: Geneva, Switzerland) & World Health Organization. Obesity: preventing and managing the global epidemic: report of a WHO consultation. 2000. World Health Organization. https://iris.who.int/handle/10665/42330
Zhang Q, Liu S, Liu R, Xue H, Wang Y. Food policy approaches to obesity prevention: an international perspective. Curr Obes Rep. 2014;3:171–82.
Kheniser K, Saxon DR, Kashyap SR. Long-term weight loss strategies for obesity. J Clin Endocrinol Metab. 2021;106:1854–66.
Heilbronn LK, Ravussin E. Calorie restriction and aging: review of the literature and implications for studies in humans. Am J Clin Nutr. 2003;78:361–9.
Middleton KR, Anton SD, Perri MG. Long-term adherence to health behavior change. Am J Lifestyle Med. 2013;7:395–404.
Mann T, Tomiyama AJ, Westling E, Lew AM, Samuels B, Chatman J. Medicare’s search for effective obesity treatments: diets are not the answer. Am Psychol. 2007;62:220–33.
Dandanell S, Skovborg C, Præst CB, Kristensen KB, Nielsen MG, Lionett S, et al. Maintaining a clinical weight loss after intensive lifestyle intervention is the key to cardiometabolic health. Obes Res Clin Pract. 2017;11:489–98.
MacLean PS, Wing RR, Davidson T, Epstein L, Goodpaster B, Hall KD, et al. NIH working group report: innovative research to improve maintenance of weight loss. Obesity. 2015;23:7–15.
Hutchison AT, Heilbronn LK. Metabolic impacts of altering meal frequency and timing - Does when we eat matter? Biochimie. 2016;124:187–97.
Mattson MP, Allison DB, Fontana L, Harvie M, Longo VD, Malaisse WJ, et al. Meal frequency and timing in health and disease. Proc Natl Acad Sci. 2014;111:16647–53.
Dashti HS, Scheer FAJL, Saxena R, Garaulet M. Timing of food intake: identifying contributing factors to design effective interventions. Adv Nutr. 2019;10:606–20.
de Cabo R, Mattson MP. Effects of intermittent fasting on health, aging, and disease. N Engl J Med. 2019;381:2541–51.
Trepanowski JF, Kroeger CM, Barnosky A, Klempel MC, Bhutani S, Hoddy KK, et al. Effect of alternate-day fasting on weight loss, weight maintenance, and cardioprotection among metabolically healthy obese adults: a randomized clinical trial. JAMA Intern Med. 2017;177:930–8.
• Varady KA, Cienfuegos S, Ezpeleta M, Gabel K. Cardiometabolic benefits of intermittent fasting. Annu Rev Nutr. 2021;41:333–61. This article thoroughly reviews body weight and cardiometabolic changes under three main forms of intermittent fasting: alternated day fasting, modified alternated day fasting (the 5:2 diet), and time-restricted eating.
Gabel K, Varady KA. Feasibility of time-restricted eating. Obesity. 2020;28:860–860.
Anton SD, Lee SA, Donahoo WT, McLaren C, Manini T, Leeuwenburgh C, et al. The effects of time restricted feeding on overweight, older adults: a pilot study. Nutrients. 2019;11:1500.
Melkani GC, Panda S. Time-restricted feeding for prevention and treatment of cardiometabolic disorders. J Physiol. 2017;595:3691–700.
Rothschild J, Hoddy KK, Jambazian P, Varady KA. Time-restricted feeding and risk of metabolic disease: a review of human and animal studies. Nutr Rev. 2014;72:308–18.
Gabel K, Hoddy KK, Varady KA. Safety of 8-h time restricted feeding in adults with obesity. Appl Physiol Nutr Metab. 2019;44:107–9.
Moon S, Kang J, Kim SH, Chung HS, Kim YJ, Yu JM, et al. Beneficial effects of time-restricted eating on metabolic diseases: a systemic review and meta- analysis. Nutrients. 2020;12:1267.
• Ezpeleta M, Cienfuegos S, Lin S, Pavlou V, Gabel K, Tussing-Humphreys L, et al. Time-restricted eating: watching the clock to treat obesity. Cell Metab. 2024. This review article gives an in-depth review of the effect of TRE without caloric counting on metabolic risk factors from RCT.
Chaix A, Zarrinpar A, Miu P, Panda S. Time-restricted feeding is a preventative and therapeutic intervention against diverse nutritional challenges. Cell Metab. 2014;20:991–1005.
de Goede P, Foppen E, Ritsema WIGR, Korpel NL, Yi CX, Kalsbeek A. Time-restricted feeding improves glucose tolerance in rats, but only when in line with the circadian timing system. Front Endocrinol. 2019;10:554.
García-Gaytán AC, Miranda-Anaya M, Turrubiate I, López-De Portugal L, Bocanegra-Botello GN, López-Islas A, et al. Synchronization of the circadian clock by time-restricted feeding with progressive increasing calorie intake. Resemblances and differences regarding a sustained hypocaloric restriction. Sci Rep. 2020;10:10036.
Sutton EF, Beyl R, Early KS, Cefalu WT, Ravussin E, Peterson CM. Early time-restricted feeding improves insulin sensitivity, blood pressure, and oxidative stress even without weight loss in men with prediabetes. Cell Metab. 2018;27:1212–21.
Chamorro R, Jouffe C, Oster H, Uhlenhaut NH, Meyhöfer SM. When should I eat: a circadian view on food intake and metabolic regulation. Acta Physiol. 2023;237:e13936.
Jamshed H, Beyl RA, Manna DLD, Yang ES, Ravussin E, Peterson CM. Early time-restricted feeding improves 24-hour glucose levels and affects markers of the circadian clock, aging, and autophagy in humans. Nutrients. 2019;11:1234.
Roenneberg T. Having trouble typing? What on earth is chronotype? J Biol Rhythms. 2015;30:487–91.
Mongrain V, Lavoie S, Selmaoui B, Paquet J, Dumont M. Phase relationships between sleep-wake cycle and underlying circadian rhythms in morningness-eveningness. J Biol Rhythms. 2004;19:248–57.
Ekiz Erim S, Sert H. The relationship between chronotype and obesity: a systematic review. Chronobiol Int. 2023;40:529–41.
Muscogiuri G, Barrea L, Aprano S, Framondi L, Di Matteo R, Altieri B, et al. Chronotype and cardio metabolic health in obesity: does nutrition matter? Int J Food Sci Nutr. 2021;72:892–900.
Klerman EB, Kramer A, Zee PC. From bench to bedside and back again: translating circadian science to medicine. J Biol Rhythms. 2023;38:125–30.
Ravussin E, Beyl RA, Poggiogalle E, Hsia DS, Peterson CM. Early time-restricted feeding reduces appetite and increases fat oxidation but does not affect energy expenditure in humans. Obesity. 2019;27:1244–54.
Mayra ST, Chondropoulos K, De Leon A, Kravat N, Johnston CS. The feasibility and preliminary efficacy of early time-restricted eating on diet quality in college students: a randomized study. Obes Res Clin Pract. 2022;16:413–20.
LeCheminant JD, Christenson E, Bailey BW, Tucker LA. Restricting night-time eating reduces daily energy intake in healthy young men: a short-term cross-over study. Br J Nutr. 2013;110:2108–13.
Kahleova H, Belinova L, Malinska H, Oliyarnyk O, Trnovska J, Skop V, et al. Eating two larger meals a day (breakfast and lunch) is more effective than six smaller meals in a reduced-energy regimen for patients with type 2 diabetes: a randomised crossover study. Diabetologia. 2014;57:1552–60.
Jones R, Pabla P, Mallinson J, Nixon A, Taylor T, Bennett A, et al. Two weeks of early time-restricted feeding (eTRF) improves skeletal muscle insulin and anabolic sensitivity in healthy men. Am J Clin Nutr. 2020;112:1015–28.
Phillips NE, Mareschal J, Schwab N, Manoogian ENC, Borloz S, Ostinelli G, et al. The effects of time-restricted eating versus standard dietary advice on weight, metabolic health and the consumption of processed food: a pragmatic randomised controlled trial in community-based adults. Nutrients. 2021;13(3):1042.
Wilkinson MJ, Manoogian ENC, Zadourian A, Lo H, Fakhouri S, Shoghi A, et al. Ten-hour time-restricted eating reduces weight, blood pressure, and atherogenic lipids in patients with metabolic syndrome. Cell Metab. 2020;31:92-104.e5.
Li C, Xing C, Zhang J, Zhao H, Shi W, He B. Eight-hour time-restricted feeding improves endocrine and metabolic profiles in women with anovulatory polycystic ovary syndrome. J Transl Med. 2021;19:148.
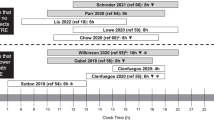
•• Jamshed H, Steger FL, Bryan DR, Richman JS, Warriner AH, Hanick CJ, et al. Effectiveness of early time-restricted eating for weight loss, fat loss, and cardiometabolic health in adults with obesity: a randomized clinical trial. JAMA Intern Med. 2022;182:953–62. This RCT evaluated weight loss and metabolic impact of an 8-hour e-TRE (eating window, 0700 h to 1500 h) vs a control group (self-selected ≥12-hour window) in patients with obesity, both groups under a hypocaloric diet (-500 kcal/d) and exercised 75-150 minutes/week. After 14 weeks, e-TRE further reduced body weight and diastolic blood pressure without differences in body composition.
Turner-McGrievy GM, Wirth MD, Bernhart JA, Aydin H. The fasting and shifted timing (FAST) of eating study: a pilot feasibility randomized crossover intervention assessing the acceptability of three different fasting diet approaches. Appetite. 2022;176:106135.
•• Liu D, Huang Y, Huang C, Yang S, Wei X, Zhang P, et al. Calorie restriction with or without time-restricted eating in weight loss. N Engl J Med. 2022;386:1495–504. This study evaluated an e-TRE (eating window: 0800h until 1600h) with caloric restriction compared with traditional caloric restriction for 6 months in patients with overweight and obesity. After 12 months, the two groups had no significant differences in weight loss, waist circumference, and body composition.
Thomas EA, Zaman A, Sloggett KJ, Steinke S, Grau L, Catenacci VA, et al. Early time-restricted eating compared with daily caloric restriction: a randomized trial in adults with obesity. Obesity. 2022;30:1027–38.
Carlson O, Martin B, Stote KS, Golden E, Maudsley S, Najjar SS, et al. Impact of reduced meal frequency without caloric restriction on glucose regulation in healthy, normal-weight middle-aged men and women. Metabolism. 2007;56:1729–34.
Stote KS, Baer DJ, Spears K, Paul DR, Harris GK, Rumpler WV, et al. A controlled trial of reduced meal frequency without caloric restriction in healthy, normal-weight, middle-aged adults. Am J Clin Nutr. 2007;85:981–8.
Arnason TG, Bowen MW, Mansell KD. Effects of intermittent fasting on health markers in those with type 2 diabetes: a pilot study. World J Diabetes. 2017;8:154–64.
Cienfuegos S, Gabel K, Kalam F, Ezpeleta M, Wiseman E, Pavlou V, et al. Effects of 4- and 6-h time-restricted feeding on weight and cardiometabolic health: a randomized controlled trial in adults with obesity. Cell Metab. 2020;32:366-378.e3.
Lowe DA, Wu N, Rohdin-Bibby L, Moore AH, Kelly N, Liu YE, et al. Effects of time-restricted eating on weight loss and other metabolic parameters in women and men with overweight and obesity: the TREAT randomized clinical trial. JAMA Intern Med. 2020;180:1491–9.
Moro T, Tinsley G, Bianco A, Marcolin G, Pacelli QF, Battaglia G, et al. Effects of eight weeks of time-restricted feeding (16/8) on basal metabolism, maximal strength, body composition, inflammation, and cardiovascular risk factors in resistance-trained males. J Transl Med. 2016;14:290.
Tinsley GM, Moore ML, Graybeal AJ, Paoli A, Kim Y, Gonzales JU, et al. Time-restricted feeding plus resistance training in active females: a randomized trial. Am J Clin Nutr. 2019;110:628–40.
Stratton MT, Tinsley GM, Alesi MG, Hester GM, Olmos AA, Serafini PR, et al. Four weeks of time-restricted feeding combined with resistance training does not differentially influence measures of body composition, muscle performance, resting energy expenditure, and blood biomarkers. Nutrients. 2020;12:1126.
Kotarsky CJ, Johnson NR, Mahoney SJ, Mitchell SL, Schimek RL, Stastny SN, et al. Time-restricted eating and concurrent exercise training reduces fat mass and increases lean mass in overweight and obese adults. Physiol Rep. 2021;9:e14868.
Domaszewski P, Konieczny M, Pakosz P, Bączkowicz D, Sadowska-Krępa E. Effect of a six-week intermittent fasting intervention program on the composition of the human body in women over 60 years of age. Int J Environ Res Public Health. 2020;17(11):4138.
Domaszewski P, Konieczny M, Pakosz P, Łukaniszyn-Domaszewska K, Mikuláková W, Sadowska-Krępa E, et al. Effect of a six-week times restricted eating intervention on the body composition in early elderly men with overweight. Sci Rep. 2022;12:9816.
Schroder JD, Falqueto H, Mânica A, Zanini D, de Oliveira T, de Sá CA, et al. Effects of time-restricted feeding in weight loss, metabolic syndrome and cardiovascular risk in obese women. J Transl Med. 2021;19:3.
Gasmi M, Sellami M, Denham J, Padulo J, Kuvacic G, Selmi W, et al. Time-restricted feeding influences immune responses without compromising muscle performance in older men. Nutrition. 2018;51–52:29–37.
Zeb F, Wu X, Chen L, Fatima S, Haq I, Chen A, et al. Effect of time restricted feeding on metabolic risk and circadian rhythm associated with gut microbiome in healthy males. Br J Nutr. 2020;123:1–25.
Hutchison AT, Regmi P, Manoogian ENC, Fleischer JG, Wittert GA, Panda S, et al. Time-restricted feeding improves glucose tolerance in men at risk for type 2 diabetes: a randomized crossover trial. Obesity. 2019;27:724–32.
•• Allison KC, Hopkins CM, Ruggieri M, Spaeth AM, Ahima RS, Zhang Z, et al. Prolonged, controlled daytime versus delayed eating impacts weight and metabolism. Curr Biol. 2021;31:650–657.e3. This randomized crossover under free-living conditions study compared the effects of an 8-week e-TRE and l-TRE on body weight and metabolic changes in normal-weight adults. An e-TRE led to decreased body weight, fasting glucose, insulin levels, HOMA-IR, and reduced trunk-to-leg fat ratio and respiratory quotient compared to l-TRE.
•• Xie Z, Sun Y, Ye Y, Hu D, Zhang H, He Z, et al. Randomized controlled trial for time-restricted eating in healthy volunteers without obesity. Nat Commun. 2022;13:1003. In this 5-week RCT, healthy young adults without obesity were randomized to: 8-hour e-TRE (eating window: 0600h to 1500h), 8-hour l-TRE (eating window: 1100h to 2000h), and an 8-hour control group. In addition to improved inflammation and gut microbiota diversity, the e-TRE group showed reduced fasting glucose, improved insulin resistance, and reduced body weight and fat mass.
do Nascimento Queiroz J, Macedo RCO, dos Santos GC GC, Munhoz SV, Machado CLF, RL de Menezes de, et al. Cardiometabolic effects of early v. delayed time-restricted eating plus energetic restriction in adults with overweight and obesity: an exploratory randomised clinical trial. Br J Nutr. 2023;129(4):637–49.
•• Zhang L, Liu Z, Wang J, Li R, Ren J, Gao X, et al. Randomized controlled trial for time-restricted eating in overweight and obese young adults. iScience. 2022;25:104870. In this 8-week RCT, young adults with overweight and obesity were randomized to: e-TRE (6-h eating window: 0700h to 1300h); l-TRE (6-h eating window: 1200 h to 1800 h); control group. e-TRE was more effective in reducing mean glucose, fasting insulin, c-peptide, HOMA-IR, and systolic blood pressure than the control group.
Wijayatunga N, Preechavanichwong B, Georgestone K, Dhurandhar E. An effectiveness study of early or late time-restricted feeding on body composition – pilot study. Curr Dev Nutr. 2020;4:1701.
Dote-Montero M, Sevilla-Lorente R, Merchan-Ramirez E, Nuñez-Lopez JC, Mochón-Benguigui S, Jurado-Fasoli L, et al. Feasibility of three different 8h time-restricted eating schedules over 4 weeks in Spanish adults with overweight/obesity: a pilot randomized controlled trial. Curr Dev Nutr. 2021;5:466.
Peters B, Koppold-Liebscher DA, Schuppelius B, Steckhan N, Pfeiffer AFH, Kramer A, et al. Effects of early vs. late time-restricted eating on cardiometabolic health, inflammation, and sleep in overweight and obese women: a study protocol for the ChronoFast trial. Front Nutr. 2021;8:765543.
Tapsell L, Batterham M, Huang XF, Tan S-Y, Teuss G, Charlton K, et al. Short term effects of energy restriction and dietary fat sub-type on weight loss and disease risk factors. Nutr Metab Cardiovasc Dis. 2010;20:317–25.
Gordon-Larsen P. Food availability/convenience and obesity Adv Nutr. 2014;5:809–17.
Wadden TA, Butryn ML, Byrne KJ. Efficacy of lifestyle modification for long-term weight control. Obes Res. 2004;12:151S-162S.
Lee SA, Sypniewski C, Bensadon BA, McLaren C, Donahoo WT, Sibille KT, et al. Determinants of adherence in time-restricted feeding in older adults: lessons from a pilot study. Nutrients. 2020;12:874.
Crittenden AN, Schnorr SL. Current views on hunter-gatherer nutrition and the evolution of the human diet. Am J Phys Anthropol. 2017;162:e23148.
Anton SD, Moehl K, Donahoo WT, Marosi K, Lee SA, Mainous AG III, et al. Flipping the metabolic switch: understanding and applying the health benefits of fasting. Obesity. 2018;26:254–68.
Grimm V. From feasting to fasting: the evolution of a sin. 1st ed. London: Routledge; 1996.
Gharbi M, Akrout M, Zouari B. Food intake during and outside Ramadan. East Mediterr Health J. 2003;9(1–2):131–40.
Tippairote T, Janssen S, Chunhabundit R. Restoration of metabolic tempo through time-restricted eating (TRE) as the preventive measure for metabolic diseases. Crit Rev Food Sci Nutr. 2021;61(4):2444–53.
Fanti M, Mishra A, Longo VD, Brandhorst S. Time-restricted eating, intermittent fasting, and fasting-mimicking diets in weight loss. Curr Obes Rep. 2021;10:70–80.
Varady KA, Hellerstein MK. Do calorie restriction or alternate-day fasting regimens modulate adipose tissue physiology in a way that reduces chronic disease risk? Nutr Rev. 2008;66:333–42.
Rajpal A, Ismail-Beigi F. Intermittent fasting and ‘metabolic switch’: effects on metabolic syndrome, prediabetes and type 2 diabetes. Diabetes Obes Metab. 2020;22:1496–510.
• O’Connor SG, Boyd P, Bailey CP, Shams-White MM, Agurs-Collins T, Hall K, et al. Perspective: time-restricted eating compared with caloric restriction: potential facilitators and barriers of long-term weight loss maintenance. Adv Nutr. 2021;12:325–33. This review article gives an overall view, at the biological, behavioral, psychosocial, and environmental levels, on potential barriers and facilitators of TRE (compared with daily caloric restriction) for long-term weight loss maintenance.
Gabel K, Hoddy KK, Haggerty N, Song J, Kroeger CM, Trepanowski JF, et al. Effects of 8-hour time restricted feeding on body weight and metabolic disease risk factors in obese adults: a pilot study. Nutr Healthy Aging. 2018;4:345–53.
Kesztyüs D, Cermak P, Gulich M, Kesztyüs T. Adherence to time-restricted feeding and impact on abdominal obesity in primary care patients: results of a pilot study in a pre–post design. Nutrients. 2019;11:2854.
Martens CR, Rossman MJ, Mazzo MR, Jankowski LR, Nagy EE, Denman BA, et al. Short-term time-restricted feeding is safe and feasible in non-obese healthy midlife and older adults. GeroScience. 2020;42:667–86.
Crose A, Alvear A, Singroy S, Wang Q, Manoogian E, Panda S, et al. Time-restricted eating improves quality of life measures in overweight humans. Nutrients. 2021;13(5):1430.
Antoni R, Robertson TM, Robertson MD, Johnston JD. A pilot feasibility study exploring the effects of a moderate time-restricted feeding intervention on energy intake, adiposity and metabolic physiology in free-living human subjects. J Nutr Sci. 2018;7:e22.
Cuccolo K, Kramer R, Petros T, Thoennes M. Intermittent fasting implementation and association with eating disorder symptomatology. Eat Disord. 2022;30:471–91.
Spreckley M, Seidell J, Halberstadt J. Perspectives into the experience of successful, substantial long-term weight-loss maintenance: a systematic review. Int J Qual Stud Health Well-Being. 2021;16:1862481.
Liu K, Choi TST, Zhao L, Teong XT, Hutchison AT, Heilbronn LK. A qualitative exploration of behaviour change and maintenance experience in people with overweight or obesity in a dietary intervention. Nutr Diet. 2023. https://doi.org/10.1111/1747-0080.12855.
Gill S, Panda S. A smartphone app reveals erratic diurnal eating patterns in humans that can be modulated for health benefits. Cell Metab. 2015;22:789–98.
Chow LS, Manoogian ENC, Alvear A, Fleischer JG, Thor H, Dietsche K, et al. Time-restricted eating effects on body composition and metabolic measures in humans who are overweight: a feasibility study. Obesity. 2020;28:860–9.
Przulj D, Ladmore D, Smith KM, Phillips-Waller A, Hajek P. Time restricted eating as a weight loss intervention in adults with obesity. PLoS ONE. 2021;16:e0246186.
McAllister MJ, Pigg BL, Renteria LI, Waldman HS. Time-restricted feeding improves markers of cardiometabolic health in physically active college-age men: a 4-week randomized pre-post pilot study. Nutr Res. 2020;75:32–43.
Van Cauter E, Blackman J, Roland D, Spire J, Refetoff S, Polonsky K. Modulation of glucose regulation and insulin secretion by circadian rhythmicity and sleep. J Clin Invest. 1991;88:934–42.
Van Cauter E, Polonsky KS, Scheen AJ. Roles of circadian rhythmicity and sleep in human glucose regulation. Endocr Rev. 1997;18(5):716–38.
Johnstone AM. Fasting – the ultimate diet? Obes Rev. 2007;8:211–22.
Leung GKW, Huggins CE, Bonham MP. Effect of meal timing on postprandial glucose responses to a low glycemic index meal: a crossover trial in healthy volunteers. Clin Nutr. 2019;38:465–71.
Chamorro R, Kannenberg S, Wilms B, Kleinerüschkamp C, Meyhöfer S, Park SQ, et al. Meal timing and macronutrient composition modulate human metabolism and reward-related drive to eat. Nutrients. 2022;14(3):562.
Jakubowicz D, Froy O, Wainstein J, Boaz M. Meal timing and composition influence ghrelin levels, appetite scores and weight loss maintenance in overweight and obese adults. Steroids. 2012;77:323–31.
Jakubowicz D, Barnea M, Wainstein J, Froy O. Effects of caloric intake timing on insulin resistance and hyperandrogenism in lean women with polycystic ovary syndrome. Clin Sci. 2013;125:423–32.
Kramer A, Lange T, Spies C, Finger A-M, Berg D, Oster H. Foundations of circadian medicine PLOS Biol. 2022;20:e3001567.
Heilbronn LK, Regmi P. Will delaying breakfast mitigate the metabolic health benefits of time-restricted eating? Obesity. 2020;28:S6-7.
de Castro JM. Circadian rhythms of the spontaneous meal pattern, macronutrient intake, and mood of humans. Physiol Behav. 1987;40:437–46.
Scheer F, Morris CJ, Shea SA. The internal circadian clock increases hunger and appetite in the evening independent of food intake and other behaviors. Obes Silver Spring. 2013;21:421–3.
Bjerre N, Holm L, Quist JS, Færch K, Hempler NF. Watching, keeping and squeezing time to lose weight: implications of time-restricted eating in daily life. Appetite. 2021;161:105138.
Lin S, Cienfuegos S, Ezpeleta M, Gabel K, Pavlou V, Mulas A, et al. Time-restricted eating without calorie counting for weight loss in a racially diverse population. Ann Intern Med. 2023;176:885–95.
Waldman HS, Renteria LI, McAllister MJ. Time-restricted feeding for the prevention of cardiometabolic diseases in high-stress occupations: a mechanistic review. Nutr Rev. 2020;78:459–64.
Ruddick-Collins LC, Morgan PJ, Fyfe CL, Filipe JAN, Horgan GW, Westerterp KR, et al. Timing of daily calorie loading affects appetite and hunger responses without changes in energy metabolism in healthy subjects with obesity. Cell Metab. 2022;34:1472-1485.e6.
Świątkiewicz I, Mila-Kierzenkowska C, Woźniak A, Szewczyk-Golec K, Nuszkiewicz J, Wróblewska J, et al. Pilot clinical trial of time-restricted eating in patients with metabolic syndrome. Nutrients. 2021;13(2):346.
Manoogian ENC, Zadourian A, Lo HC, Gutierrez NR, Shoghi A, Rosander A, et al. Feasibility of time-restricted eating and impacts on cardiometabolic health in 24-h shift workers: the Healthy Heroes randomized control trial. Cell Metab. 2022;34:1442-1456.e7.
Funding
This work was supported by the National Fund for Scientific and Technological Research, FONDECYT Initiation, grant #11230075 (to RC).
Author information
Authors and Affiliations
Contributions
RC and BS designed the study; BS, AM, AS, and RC participated in the acquisition and interpretation of data; BS, RB, and RC wrote the manuscript. All authors have read and approved the final paper.
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no relevant financial or non-financial interests to disclose.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sepúlveda, B., Marín, A., Burrows, R. et al. It’s About Timing: Contrasting the Metabolic Effects of Early vs. Late Time-Restricted Eating in Humans. Curr Nutr Rep (2024). https://doi.org/10.1007/s13668-024-00532-0
Accepted:
Published:
DOI: https://doi.org/10.1007/s13668-024-00532-0