Abstract
Purpose of Review
Pleural mesothelioma (PM) is a rare but fatal cancer of the pleural surface. Most patients have a poor prognosis, despite treatment advances which have improved outcomes. Recent research has focused on improving diagnosis, prognostication and monitoring through radiological, histological and molecular techniques. This review will cover its clinical implications and highlight areas where practice is changing.
Recent Findings
Changes in tumour classification and histological reporting have formalised the differentiation between benign, pre-malignant and malignant pleural disease. CT and thoracic ultrasound (TUS) have good diagnostic yields for pleural biopsy, but PET-CT does not increase diagnostic yield for repeat sampling. immunohistochemistry (IHC) staining for BAP1 and MTAP/CDKN2A pathological samples can increase diagnosis rates, while serum mesothelin shows promise for disease monitoring. Phase 3 RCT results mean dual immunotherapy is the new standard of care, whereas there is no role for extended pleurectomy decortication surgery for PM.
Summary
Best practice for PM diagnosis and management is changing at pace. Key areas for future research involve improving PM diagnostics, therapeutics and targeted therapies. An awareness of active research and clinical trials is essential for clinicians to seek for the best outcomes for their patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pleural Mesothelioma (PM) is a primary malignancy of the pleural surface, associated with prior occupational or environmental asbestos exposure. Latency period is 20–50 years between exposure and disease presentation. In 2020, 30,870 PM cases were reported globally, with the highest age-standardised rates in Northern Europe, New Zealand and Australia. Overall rates worldwide are decreasing, likely as a result of asbestos regulation in many countries, although incidence in women and in countries including Korea, Bulgaria and Brazil are increasing [1••].
Median survival is poor, with 3 year survival persistently around 10% [2]. Chemotherapy in the form of pemetrexed and a platinum agent has been the mainstay of treatment for many years, despite marginal survival benefit and overall response rates of less than 50% [3].
An increased focus on mesothelioma research has led to significant advancements in disease understanding and management in the past 5 years. Novel therapeutic agents, including immunotherapy, have resulted in longer survival for some patients, but response rates remain low and, as the PM population ages, treatment is not suitable for everyone. Improving diagnosis rates, prognostication and identification of those most likely to benefit from treatment are increasingly important.
This article will review novel diagnostic approaches and biomarkers, discuss new understanding of disease phenotypes and survival, as well as recent advances in mesothelioma treatment.
Updates from the WHO 2021 Classification
Disease Phenotypes
In recognition of the pre-invasive tumours outlined in the 2021 WHO classification, ‘malignant mesothelioma’ has been renamed ‘diffuse mesothelioma’, with pleural disease now referred to as ‘pleural mesothelioma’ (PM) rather than malignant pleural mesothelioma (MPM) as it was known in previous literature [4]. Localised pleural mesothelioma is distinguished from diffuse mesothelioma as a completely resected single tumour with histologic features of diffuse mesothelioma without invasion beyond the borders of the tumour.
The 2015 WHO classification of tumours of the pleura outlined 3 histological subtypes of PM: sarcomatoid, biphasic and epithelioid, recognising the different prognostic implications of each. The 2021 classification recognised the heterogeneity within the epithelioid subtype, introducing two-tier nuclear grade, discussed in “Nuclear Grading System and Predicting Prognosis” section. There is no grading system for sarcomatoid and biphasic tumours, although the epithelioid component of biphasic tumours may be graded.
Additional histopathological features of epithelioid tumours were summarised in the 2019 EURACAN/IASLC proposal before being updated in the 2021 classification [5]. Nicholson et al. asserted that reporting architectural features reduced misdiagnosis and some architectural patterns have prognostic implications. Tubulopapillary, trabecular, or adenomatoid are patterns associated with more favourable outcomes, whilst micropapillary or solid growth patterns are a poorer prognostic feature [6, 7].
Pre-invasive mesothelial tumours are categorised separately, with well differentiated papillary mesothelioma (WDPM) renamed as well differentiated papillary mesothelial tumour (WDPMT). The replacement of ‘mesothelioma’ with ‘mesothelial tumour’ in WDPMT reflects the indolent behaviour of this rare pleural tumour. WDPMT consists of papillary stroma covered by bland mesothelium, without stromal invasion. BAP1 expression is usually retained. Caution is needed when making a diagnosis of WDPMT, as superficial biopsies of low-grade epithelioid mesothelioma can appear morphologically similar, necessitating histologic examination of the complete lesion [8••].
A new addition in the 2021 classification is mesothelioma in situ (MIS). MIS was originally postulated in 1992 and is considered to be a precursor to diffuse mesothelioma [9]. It is defined as a mesothelial proliferation limited to the serosal surface with no macroscopically visible tumour on direct inspection or radiological imaging, with either BAP1 loss and/or CDKN2A/p16 homozygous deletion detected. Invasive mesothelioma must be absent for a MIS diagnosis, with cytological analysis alone insufficient to rule out invasive disease. MIS must be diagnosed by a multidisciplinary team (MDT). Most MIS patients present with recurrent pleural effusion. Progression to PM is considered the natural disease course, although the expected time to progression in unknown. Data on MIS is scant with a small series of 10 patients, (9 PM and 1 peritoneal mesothelioma), forming much of the knowledge base. In that series, median time to progression was 60 months (range 12–92). Two patients had not developed PM when the study was published (at 12 and 57 months) and were ultimately diagnosed with benign asbestos pleural effusion (BAPE) [10].
Development of PM
BAPE is one of several benign asbestos-related inflammatory pleural diseases that have been reported to progress to PM. The conversion rate for asbestos associated pleural inflammation has been reported to be as high as 16% [11, 12]. A meta-analysis of 11 similar studies found a conversion rate of 6% but reported significant inter study heterogeneity [13].
For people who have been exposed to asbestos, the fear of developing PM is ever present [14•]. However, little is currently known about the development of PM, including who is most at risk. The Meso-Origins study aims to determine risk factors for progression from BAPE to PM through identification of genomic signatures that can be used as pre-cursors for malignant transformation [12]. Meso-ORIGINS aims to recruit 620 participants by 2025, and the results should improve our understanding of PM evolution and aid development of surveillance strategies in benign pleural disease [15].
Nuclear Grading System and Predicting Prognosis
The introduction of a histopathologic grading system for epithelioid PM in the 2021 WHO classification is a significant development in PM pathology reporting, with nuclear grade linked to overall survival [8••] (See Fig. 1). First proposed in 2012, the three tier grading system was developed using a predominantly surgical population [16]. The system assigns a score of 1–3 for both nuclear atypia and mitotic count at histological analysis. Scores are combined to produce the three-tier grade, which was an independent predictor of survival. During validation in another predominantly surgical cohort, the presence or absence of necrosis added further prognostic value [4]. Necrosis was combined with three-tier grade to form the two-tier nuclear grade.
Both scores were externally validated in non-surgical biopsy samples [17]. Median survival was 8.9 months in high nuclear grade and 19.3 months in low grade. The prognostic relationship disappeared with smaller biopsies, highlighting the importance of biopsy size and number when assessing nuclear grade [17]. This is likely to reflect the histological heterogeneity of PM tumours, requiring multiple large samples from different tumour sites to increase the chance of representative sampling.
Reporting of nuclear grade is now recommended for all epithelioid PM tumours at diagnosis [4]. The prognostic information it provides can help patients and clinicians share decision making when planning treatment.
Other scoring systems have been created. In 2018 Pelosi et al. proposed and validated a pathologic grading system for all histological subtypes of PM. Biopsy samples are scored based on histological subtype, presence of necrosis, mitotic count and Ki67 labelling index [18]. Ki67 is a marker of proliferation, and is used to stratify peritoneal mesothelioma and inform treatment decisions [19]. Exploratory work has shown Ki67 to have some prognostic value in PM, but further validation is required [20].
Outside histopathological techniques, clinical prognostication can be performed at diagnosis using the scoring system developed by Brims et al. [21]. It combines baseline performance status (PS), presence of weight loss, histology subtype, haemoglobin and serum albumin to separate patients into 4 prognostic groups. Median survival ranges from 34 months in group 1 to 7.4 months in group 4.
New Diagnostic Approaches and Biomarkers
Interventional Diagnostics
Biopsy remains the gold standard for PM diagnosis, although an MDT clinico-radiological consensus diagnosis is an acceptable alternative if biopsy is not possible [22].
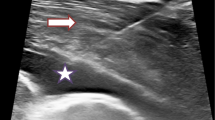
Recent studies have investigated methods of increasing the diagnostic sensitivity of radiologically guided biopsies. A 2021 meta-analysis reviewed 30 studies reporting the diagnostic yield of image-guided pleural biopsies [23]. Although there was significant heterogeneity between studies, the diagnostic yield of CT-guided biopsy was consistently high at 93%. Although thoracic ultrasound (TUS)-guided biopsies had a slightly lower yield of 84%, it has improved with time, unlike that of CT-guided biopsies. Improved operator skill can explain this, as TUS has become more widely used by clinicians in recent years. Complication rates were low for all image-guided biopsies, at 7% for CT-guided biopsy and only 3% for TUS-biopsy.
False negative results remain a challenge, as it is well recognised that mesothelioma deposits can be distributed heterogeneously across the pleural surface. These have been reported in up to 25% of patients with suspected PM [23].
PET-CT is used routinely for staging and to select biopsy sites in other cancers. However, in PM, PET-CT is recommended only where the presence of distant metastases will change management. A 2015 meta-analysis demonstrated PET-CT had variable utility in differentiating between benign and malignant pleural disease, with sensitivity of 81% and specificity of 74% The use of PET-CT to identify biopsy targets is less well understood in PM [24].
The multi-centre randomised controlled trial (RCT) TARGET study investigated the use of PET-CT to increase the diagnostic sensitivity of image guided biopsy in patients with suspected pleural malignancy and an initial non-diagnostic biopsy [25]. The majority of patients were ultimately diagnosed with mesothelioma, but the diagnostic yield was similar in both CT-guided and PET-CT guided biopsy groups. TARGET findings therefore do not recommend PET-CT for targeting biopsy sites in second biopsies [26].
Instrumenting PM for biopsy samples, regardless of technique, can lead to procedure tract metastasis via tumour cell seeding. Incidence rates vary in the literature, ranging anywhere from 2 to 50% of instrumented PM cases [27,28,29,30]. Development of tract metastases are a poor prognostic factor [31]. They can be treated with radiotherapy, especially if painful, but prophylactic irradiation after pleural procedures is no longer indicated [22, 31], based on evidence from the SMART and PIT trials [28, 30].
SMART randomised 203 patients to receive immediate radiotherapy at the site of large bore pleural intervention or deferred radiotherapy at the site once procedure tract metastases developed [30]. It found no difference in tract metastases in either group. No between arms difference was found in pain, quality of life or breathlessness, although it was not powered for these secondary outcomes. PIT randomised 375 patients to receive either radiotherapy following pleural intervention or standard care, without tract site radiotherapy. Its findings supported those of SMART, demonstrating no difference in the 6 month incidence of chest wall metastases [28]. Localised radiotherapy remains recommended only as a palliative treatment measure for localised mesothelioma where the disease matches pain distribution.
Ancillary Diagnostic Tests
Recent advances in laboratory testing have broadened the panel of tests available for suspected PM, reducing diagnostic uncertainty. Homozygous deletion of the 9p21 locus is one of the most common genetic alterations in PM, affecting a cluster of tumour suppression genes that show diagnostic promise. These are BRCA-associated protein 1 (BAP1), CDKN2A/p16 and methylthioadenosine phosphorylase (MTAP) [25, 32].
BAP1 is a tumour suppressor gene. Germline BAP1 loss was initially identified amongst families with high incidence of mesothelioma in 2011 [33]. Somatic mutation causes loss of BAP1 nuclear expression in some PM tumours and this can be tested for using immunohistochemistry (IHC). BAP1 is lost in 70% of epithelioid and 50% of sarcomatoid PM [34]. Although BAP1 testing is not recommended in current mesothelioma guidelines [22, 31], its utility in differentiating between benign and malignant mesothelial lesions, particularly when tissue invasion is not clearly identifiable, has prompted its routine use in many laboratories and its incorporation into the 2021 WHO Classification of tumours of the pleura [4, 32]. A 2017 meta-analysis showed BAP1 loss had moderate diagnostic sensitivity (area under the curve of 0.72) with 100% specificity, making it an excellent ‘rule-in’ test for PM [35]. Furthermore, BAP1 IHC has been shown to increase diagnostic accuracy in atypical pleural fluid cytology [36•], highlighting a potential use in patients unable to tolerate more invasive investigation.
BAP1 is retained in 30–40% of PM, necessitating the use of other markers to improve diagnostic accuracy. CDKN2A/P16 homozygous deletion occurs in around 70–80% of epithelioid PM and close to 100% of sarcomatoid PM [37]. It is demonstrated using the fluorescence in situ hybridisation (FISH) technique. Diagnostic sensitivity of P16 FISH is 0.53 in isolation, but 0.76 if combined with BAP1 testing [38].
FISH is not performed in all laboratories but immunohistochemical (IHC) staining is universally available and faster and cheaper to run [39]. Loss of expression of the protein product of the MTAP gene on IHC has been shown to be an accurate and reproducible surrogate marker for p16 FISH, as they are located in close proximity on the 9p21 region of chromosome 9 [8••]. When used in combination with BAP1, MTAP IHC has 100% specificity and 76.5% sensitivity for differentiating malignant from benign mesothelial disease [35]. MTAP IHC staining is widely accepted as good practice in suspected PM, although is not yet universally available [8••, 40].
Serum Mesothelin as a Biomarker
While routine work up of many cancers now utilises blood-based biomarkers for risk identification, diagnosis and monitoring, there is no biomarker yet that fulfils this role in PM. One of the most studied is serum mesothelin. Mesothelin is a glycoprotein involved in cell to cell adhesion that is expressed on the surface of normal mesothelial cells. Mesothelin is overexpressed in some cancers, including PM, and, when released from the cell surface, can be detected in the blood as soluble mesothelin-related peptides (SMRPs) [41]. Higher mesothelin levels are seen with increasing tumour bulk, and in epithelioid histology [42].
Serum mesothelin has been investigated as a potential diagnostic or screening biomarker for PM [41,42,43,44,45]. However, it has no role in the diagnostic pathway due to low sensitivity and poor negative predictive value. In sarcomatoid disease particularly, mesothelin levels can be low despite a significant burden of disease [22, 31].
Baseline mesothelin has shown promise as a prognostic tool, with studies finding an inverse relationship between baseline levels and survival. However, cut-off values and significance thresholds vary in the literature, making clinical interpretation challenging [42].
Serum mesothelin may aid disease monitoring, as it appears to correlate well with radiological disease status. In 2011, Creaney et al. monitored serum mesothelin in 55 patients with PM undergoing oncological treatment and found an association between radiological disease response and falling serum mesothelin [43]. A 2018 study of 41 patients receiving either chemotherapy (n = 23) or best supportive care (n = 18) showed changes in serum mesothelin reflected disease status on clinically-reported CT scans more accurately than mRECIST. A 10% rise in serum mesothelin from baseline predicted disease progression with 96% sensitivity in epithelioid disease and 80% in sarcomatoid disease [42].
A 2023 study of 209 patients confirmed the value of serial serum mesothelin as a marker of disease status and survival [46]. Rising serum mesothelin values predicted disease progression, whether receiving systemic anticancer treatment (SACT) or best supportive care (OR 1.51, 95% confidence interval [CI] 1.01- 1.95). In people receiving SACT, falling levels predicted disease response (OR 1.4, 95% CI 1.03–1.92). The prognostic utility of serial serum mesothelin was maintained regardless of patient’s baseline mesothelin result. An initial mesothelin level of ≥ 2 nmol/L was associated with higher mortality (HR 1.98, 95% CI 1.13–3.47). Further work is underway to determine the thresholds of mesothelin change that may inform use in clinical settings.
Future Directions in Diagnosis
Breath Testing in Mesothelioma
Effective breath testing techniques could enable earlier, non-invasive diagnosis of PM, and facilitate differentiation between benign and malignant asbestos-related pleural disease. Volatile organic compounds ([47]) reflect underlying pathological metabolic processes, including lung cancer and previous asbestos exposure, and can be measured in exhaled breath [47].
A 2020 literature review of breath testing in PM identified 6 studies, with sample sizes of 39–330 patients. VOC analysis distinguished PM from healthy controls with sensitivity and specificity ranging from 0.62–0.96 and 0.22–1.0 respectively. Identifying PM from asbestos-exposed individuals had sensitivity of 0.62–0.96 and specificity of 0.52–0.71, with the wide range in reported results due to variation in techniques [47]. Lack of external validation is one barrier preventing use of VOC models in clinical practice. However, a 2017 model performed poorly during external validation, with the authors citing high interobserver variability during VOC analysis. This may prove another barrier to clinical translation [48].
Breath testing has also been used to predict response to immune checkpoint inhibitors (ICIs). A 2021 study used ENose technology, which detects VOC combinations, to identify differentiate between immune checkpoint inhibitor (ICI) responders and non-responders in a sample of 31 patients [49]. Further work with larger samples is required.
Artificial Intelligence
Artificial intelligence (AI) holds great potential in medicine, with many possible applications in mesothelioma. Semi-automated methods using computer assisted PM tumour measurement were first published in 2005 [50]. More recently, Kidd et al. created and validated a deep learning AI system to perform volumetric analysis of PM tumours on CT scans [51•]. This showed good agreement between radiologists and AI in assessment of tumour volume, with any AI errors occurring with fissural tumour, contralateral pleural thickening and adjacent lung atelectasis. However, AI was less accurate in determining post-treatment disease status, with kappa of 0.284 compared to mRECIST, whilst radiologist assessment concordance with mRECISt was higher (kappa 0.439).
AI can be used to differentiate between benign and malignant pleural disease on radiological imaging. Kitajima et al. developed several such models using a 525-patient training set, with the best performing combining clinical features and radiology. It distinguished between benign and malignant disease with sensitivity and specificity of 89% and 74% respectively.
AI has also been employed in histological image analysis to improve diagnosis, prognostication and help distinguish benign from malignant mesothelial proliferations [50, 52,53,54]. Naso el at showed AI could distinguish between sarcomatoid PM and benign spindle cell mesothelial proliferations, with potential utility in challenging diagnostic cases [53]. In 2019 Courtiol et al. created a predictive model using survival data and histological images to identify patterns linked with poor prognosis [53].
Although AI models are not in routine use for these indications, the landscape is rapidly changing and incorporation of AI into routine radiological and histological assessment of suspected PM is likely in the future.
Advances in Treatment
Surgery in Mesothelioma
Although less invasive approaches are preferable, video-assisted thoracoscopic surgery VATS biopsy may be required for diagnosis in those where percutaneous biopsy or medical thoracoscopy is not possible or is non-diagnostic.
The role of thoracic surgery as treatment for PM is controversial, and it is not recommended in UK guidelines [22]. The MARS feasibility trial showed no benefit for extrapleural pneumonectomy (EPP) and suggested that EPP was, in fact, associated with higher morbidity and mortality [55]. The multicentre randomised MARS2 trial evaluated the role of extended pleurectomy decortication (EPD) in patients treated with chemotherapy and randomised 335 patients to either EPD plus chemotherapy or chemotherapy alone [56, 57••]. It showed poorer outcomes in the surgical arm with increased mortality (HR 1.28, 95% CI 1.02 -1.60), a higher complication rate (Incidence rate ratio 3.6, 95% CI 2.3–5.5), poorer quality of life and increased costs. These results show definitive surgery is not a good option for these patients.
Surgical management of malignant pleural effusions remains unproven. The MesoVATS trial, published in 2014, found no improvement in OS with video-assisted thoracoscopic partial pleurectomy (VAT-PP) compared to talc pleurodesis, with increased complications and hospital stay in the surgical arm [58]. The randomised MesoTRAP feasibility study aimed to compare the use of indwelling pleural catheters (IPC) with a surgical approach in the management of non-expansile lung, with patient reported outcomes rather than OS as the primary outcome. It closed to recruitment in 2020 and an additional longitudinal element was added due to recruitment challenges, with results awaited [59].
Treatment Advances in Non-resectable Mesothelioma
Immunotherapy
Combination chemotherapy with pemetrexed and a platinum agent was the mainstay of treatment for PM until the recent developments in systemic anti-cancer therapies. Both VEG-F antagonists and checkpoint inhibition have shown modest but important survival benefits and have changed the PM treatment landscape as a result.
Bevacizumab is an anti-VEGF monoclonal antibody which showed initial promise in early small studies [60,61,62]. This led to the 2016 MAPS phase 3 RCT randomising 448 participants to either standard chemotherapy or chemotherapy plus bevacizumab. In the bevacizumab arm median OS increased from 16.07–18.82 months (HR 0.67; 96% CI 0.61–0.94), as did progression-free survival (PFS) [63]. Subgroup analysis between epithelioid and non-epithelioid disease showed no difference. While this treatment was included in some guidelines at the time, licensing restrictions prevented its universal adoption as first line treatment [64].
Following dramatic impact in the melanoma and non-small cell lung cancer sphere, immunotherapy was widely touted as a potential treatment for mesothelioma. Initial results of single agent therapies were disappointing, however [65, 66]. Following publication of the phase 3, randomised Checkmate 743 study in 2021, dual immunotherapy has become the standard first-line management of patients with PS of 0–1 and non-resectable disease [67]. In Checkmate 743, 605 eligible participants were randomised to either nivolumab (a human anti-programmed cell death 1 (PD-1) antibody) with ipilimumab (a human anti-cytotoxic T-lymphocyte 4 (CTLA-4) antibody) or standard chemotherapy (platinum plus pemetrexed). Median OS increased from 14.1 months with chemotherapy to 18.1 months in the immunotherapy arm (HR 0.74; 96.6% CI 0.6–0.91). While OS on dual immunotherapy was higher regardless of histological subtype, the improvement in OS was more marked in non-epithelioid histology, where OS increased from 8·8 months (95% CI 7·4–10·2) with chemotherapy to 18·1 months (95% CI 12·2–22·8) with dual immunotherapy. In epithelioid histology median OS on chemotherapy was 16·5 months (14·9–20·5) and 18·7 months (16·9–22·0) on dual immunotherapy. This reflects the limited efficacy of chemotherapy in non-epithelioid disease, and offers a valid and effective alternative for people with these poor prognosis subtypes.
Rates of drug toxicity were comparable between treatment groups, and the toxicities reported for dual immunotherapy were comparable to those reported previously [68•]. Twice as many patients on dual immunotherapy had treatment-related adverse events that led to discontinuation (15%), than with chemotherapy (7%). However, survival benefit at 1 and 2 years remained higher in the dual immunotherapy group, with ongoing benefit found at 3 years even after treatment discontinuation [69]. Furthermore patient reported outcome measure (PROMs) favoured the dual immunotherapy arm [70] suggesting quality of life and symptom benefits compared with chemotherapy.
Dual immunotherapy has been approved by international regulatory bodies and is recommended in international guidelines as the standard of care as first line treatment for non-operable PM in good performance patients. Phase 3 studies to assess the efficacy of combination chemo-immunotherapy as first line treatment are underway, including DREAM3R [71•], BEAT-meso (NCT03762018) and CCTG IND227/IFCT-1901 [72] which could further advance management once reported.
In non-epithelioid disease, survival improvements have also been shown with the addition of pegylated arginine deiminase to standard chemotherapy. In the phase 2/3 ATOMIC meso trial, 249 patients with non-epithelioid PM were randomised to standard chemotherapy (pemetrexed and cisplatin) plus placebo or chemotherapy plus pegargiminase [73, 74]. Median OS was 9.3 months (95% CI 7.9–11.8) in the intervention group compared to 7.7 months (95% CI 6.1–9.5) in the control group. While survival gains are more modest when compared with the Checkmate 743trial, it is another sign of progress in a subtype with such few treatment successes in recent years.
Identifying Treatment Responders
Treatment response rates for both arms in Checkmate 743 were below 50%. Identifying people with PM who will respond to treatment remains a challenge for clinicians, with therapeutic molecular targets lacking. Although targeted therapy is a rapidly expanding field in lung cancer [75], developments in PM treatments have not kept pace largely due to the lack of driver mutations. While PD-L1 expression has shown some correlation with response to immunotherapy in PM, there is insufficient evidence at present to warrant its, or any other molecular markers use, in treatment selection [76]. Other studies investigating targeted therapies and small molecules have failed to demonstrate effectiveness, and until genetic and molecular targets are identified, personalised therapy seems some way off in PM.
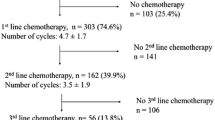
Second-line PM treatment following relapse is an area lacking in evidence, as increasingly patients are receiving first line immunotherapy. The trials to date are conducted on patients following first line chemotherapy [66, 77, 78].
The phase 2 MAPS2 trial randomised 125 PM patients with PS 0–1 who had relapsed after first or second line platinum-based chemotherapy to either single (nivolumab) or dual (nivolumab plus ipilimumab) immunotherapy [77]. 12 week disease control rates were 44% and 50% in the single and dual immunotherapy groups respectively. The phase 3 CONFIRM trial randomised a similar population of 332 PM patients to either single agent immunotherapy (nivolumab) or placebo, showing nivolumab improved survival (adjusted HR 0·69 [95% CI 0·52–0·91]) [78]. OS on nivolumab was 10.2 months (95% CI 8.5–12.1) vs 6.9 months (95% CI 5.0–8.0) with placebo, with improved progression free survival (3 months [95% CI 2·8–4·1] vs 1.8 months [95% CI 1·4–2·6].
These trials show the benefits of immunotherapy in the second line setting, without unexpected toxicities. Therefore in those who have received chemotherapy as first line, dual immunotherapy is a valid second line treatment option while awaiting more evidence.
Intra-pleural Drug-delivery
Intra pleural therapies are an appealing option for PM as it is often confined to the pleura, which can be readily accessed via an IPC. However, research is still early stage with a number of small feasibility/early phase trials.
Danson et al. studied HSV1716, a herpes simplex virus with anti-tumour effects, in 13 patients. It was well tolerated but efficacy could not be determined [79]. Bibby et al. performed a feasibility trial of intra‑pleural bacterial immunotherapy (TILT), randomising patients to intra-pleural OK432, BCG or usual care. With 7 patients it did not meet recruitment targets. However no difference was seen in radiological outcome between groups, and the trial within a cohort methodology was deemed unfeasible in this population [80].
Research is underway to determine safety, tolerability and efficacy of another intra-pleural therapy. MITOPE is a non-randomised phase 1/2 study evaluating intra-pleural RSO-021 (a mitochondrial peroxide scavenging enzyme peroxiredoxin 3 inhibitor) [81]. Aiming to recruit 42 patients, it closes in 2025. This is a developing area, and it remains to be seen if it will lead to survival benefit in this population.
Conclusions
Despite modest improvements in PM survival, recent therapeutic advances have provided patients with much-needed hope, and a sense of incremental gains against this previously treatment refractory disease.
Similar advances in diagnostics could streamline the PM pathway and reduce the period of anxious uncertainty that many experience as they await results or undergo monitoring for suspicious pleural disease. Improvements in prognostication have the potential to contribute positively to decision making and treatment discussions between the clinician and patient.
As diagnostic pathways evolve and treatment options widen, it is vital that routine clinical practice keeps pace with advances in best practice standards. The importance of the MDT, including dedicated specialist nurses, in advocating for the most up to date and evidence-based treatment for their patients remains paramount.
Data Availability
No datasets were generated or analysed during the current study.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Huang J, et al. Global Incidence, Risk Factors, and Temporal Trends of Mesothelioma: A Population-Based Study. J Thorac Oncol. 2023;18(6):792–802. Study of global disease burden illustrating changing trends in mesothelioma incidence and disease burden by country and sex.
Royal College of Physicians. National Mesothelioma Audit report 2020 (for the audit period 2016–18). London: RCP; 2020.
Vogelzang NJ, et al. Phase III study of pemetrexed in combination with cisplatin versus cisplatin alone in patients with malignant pleural mesothelioma. J Clin Oncol. 2003;21(14):2636–44.
WHO Classification of Tumours Editorial Board. WHO Classification of Tumours: Thoracic Tumours. 5th ed. Lyon, France: International Agency for Research on Cancer; 2021.
Nicholson AG, et al. EURACAN/IASLC Proposals for Updating the Histologic Classification of Pleural Mesothelioma: Towards a More Multidisciplinary Approach. J Thorac Oncol. 2020;15(1):29–49.
Mastromarino MG, Lenzini A, Aprile V, Alì G, Bacchin D, Korasidis S, Ambrogi MC, Lucchi M. New Insights in Pleural Mesothelioma Classification Update: Diagnostic Traps and Prognostic Implications. Diagnostics (Basel). 2022;12(12):2905.
Forest F, et al. Histopathological typing in diffuse malignant epithelioid mesothelioma: implication for prognosis and molecular basis. Pathology. 2021;53(6):728–34.
•• Sauter JL, et al. The 2021 WHO Classification of Tumors of the Pleura: Advances Since the 2015 Classification. J Thorac Oncol. 2022;17(5):608–22. Concise summary of major changes in 2021 WHO classification of thoracic tumours compared with 2015, outlining changes in pathological classification of pleural tumours and introduction of prognostic histological features for epithelioid mesothelioma.
Whitaker D, Henderson DW, Shilkin KB. The concept of mesothelioma in situ: implications for diagnosis and histogenesis. Semin Diagn Pathol. 1992;9(2):151–61.
Churg A, et al. Malignant mesothelioma in situ: morphologic features and clinical outcome. Mod Pathol. 2020;33(2):297–302.
Davies HE, et al. Outcome of patients with nonspecific pleuritis/fibrosis on thoracoscopic pleural biopsies. Eur J Cardiothorac Surg. 2010;38(4):472–7.
Ferguson K, et al. Results of the Meso-ORIGINS feasibility study regarding collection of matched benign-mesothelioma tissue pairs by longitudinal surveillance. BMJ Open. 2023;13(8):e067780.
Ferguson K, B.K., Neilson M,. S15 Evolution of mesothelioma following initial biopsies showing benign pleural inflammation, a meta-analysis. Thorax. 2021;76:A14.
• Bibby AC, et al. The priorities of people with mesothelioma and their carers: A qualitative interview study of trial participation and treatment decisions. Eur J Oncol Nurs. 2022;57:102111. Qualitative study providing important insight into the experiences of patients with mesothelioma and their carers, highlighting their key concerns as well as exploring their attitudes to being involved in clinical trials.
Neilly M, et al. An update regarding the Meso-ORIGINS study: part of the PREDICT-Meso International Accelerator. Eur Respir J. 2023;62(suppl 67):PA3434.
Kadota K, et al. A nuclear grading system is a strong predictor of survival in epitheloid diffuse malignant pleural mesothelioma. Mod Pathol. 2012;25(2):260–71.
Zhang YZ, et al. Utility of Nuclear Grading System in Epithelioid Malignant Pleural Mesothelioma in Biopsy-heavy Setting: An External Validation Study of 563 Cases. Am J Surg Pathol. 2020;44(3):347–56.
Pelosi G, et al. Pathologic Grading of Malignant Pleural Mesothelioma: An Evidence-Based Proposal. J Thorac Oncol. 2018;13(11):1750–61.
Boussios S, et al. Malignant peritoneal mesothelioma: clinical aspects, and therapeutic perspectives. Ann Gastroenterol. 2018;31(6):659–69.
Lynch GA, Morley ZY, Brown A, Tucker E, Stadon L, White P, Bhatt N, Nicholson AG, Bibby AC, Maskell NA. Exploring the clinical and pathological features associated with long survival in pleural mesothelioma (PM) patients. in International Mesothelioma Interest Group. 2023. Lille. https://imig2023.org/wp-content/uploads/2023/06/WEB_PROG_IMIG.pdf
Brims FJ, et al. A Novel Clinical Prediction Model for Prognosis in Malignant Pleural Mesothelioma Using Decision Tree Analysis. J Thorac Oncol. 2016;11(4):573–82.
Woolhouse I, et al. BTS guideline for the investigation and management of malignant pleural mesothelioma. BMJ Open Respir Res. 2018;5(1):e000266.
Mei F, et al. Diagnostic Yield and Safety of Image-Guided Pleural Biopsy: A Systematic Review and Meta-Analysis. Respiration. 2021;100(1):77–87.
Porcel JM, et al. Accuracy of fluorodeoxyglucose-PET imaging for differentiating benign from malignant pleural effusions: a meta-analysis. Chest. 2015;147(2):502–12.
de Fonseka D, et al. Randomised controlled trial to compare the diagnostic yield of positron emission tomography CT (PET-CT) TARGETed pleural biopsy versus CT-guided pleural biopsy in suspected pleural malignancy (TARGET trial). BMJ Open Respir Res. 2018;5(1):e000270.
De Fonseka D, et al. PET-CT-guided versus CT-guided biopsy in suspected malignant pleural thickening: a randomised trial. Eur Respir J. 2024;63(2):2301295.
Agarwal PP, et al. Pleural mesothelioma: sensitivity and incidence of needle track seeding after image-guided biopsy versus surgical biopsy. Radiology. 2006;241(2):589–94.
Bayman N, et al. Prophylactic Irradiation of Tracts in Patients With Malignant Pleural Mesothelioma: An Open-Label, Multicenter, Phase III Randomized Trial. J Clin Oncol. 2019;37(14):1200–8.
Boutin C, Rey F, Viallat JR. Prevention of malignant seeding after invasive diagnostic procedures in patients with pleural mesothelioma. A randomized trial of local radiotherapy. Chest. 1995;108(3):754–8.
Clive AO, et al. Prophylactic radiotherapy for the prevention of procedure-tract metastases after surgical and large-bore pleural procedures in malignant pleural mesothelioma (SMART): a multicentre, open-label, phase 3, randomised controlled trial. Lancet Oncol. 2016;17(8):1094–104.
Scherpereel A, Opitz I, Berghmans T, Psallidas I, Glatzer M, Rigau D, Astoul P, Bölükbas S, Boyd J, Coolen J, De Bondt C, De Ruysscher D, Durieux V, Faivre-Finn C, Fennell D, Galateau-Salle F, Greillier L, Hoda MA, Klepetko W, Lacourt A, McElnay P, Maskell NA, Mutti L, Pairon JC, Van Schil P, van Meerbeeck JP, Waller D, Weder W, Cardillo G, Putora PM. ERS/ESTS/EACTS/ESTRO guidelines for the management of malignant pleural mesothelioma. Eur Respir J. 2020;55(6).
Dipper A, Maskell N, Bibby A. Ancillary Diagnostic Investigations in Malignant Pleural Mesothelioma. Cancers (Basel). 2021;13(13):3291.
Testa JR, et al. Germline BAP1 mutations predispose to malignant mesothelioma. Nat Genet. 2011;43(10):1022–5.
Carbone M, et al. Mesothelioma: Scientific clues for prevention, diagnosis, and therapy. CA Cancer J Clin. 2019;69(5):402–29.
Hida T, et al. Immunohistochemical detection of MTAP and BAP1 protein loss for mesothelioma diagnosis: Comparison with 9p21 FISH and BAP1 immunohistochemistry. Lung Cancer. 2017;104:98–105.
• Louw A, et al. Diagnostic utility of BAP1 for malignant pleural mesothelioma in pleural fluid specimens with atypical morphology. Cytopathology. 2022;33(1):84–92. Study of 50 patients with atypical cytology pleural effusion showing the increase in diagnostic accuracy in this group by the additional of BAP1 staining to the initial testing panel.
Chevrier M, et al. Testing for BAP1 loss and CDKN2A/p16 homozygous deletion improves the accurate diagnosis of mesothelial proliferations in effusion cytology. Cancer Cytopathol. 2020;128(12):939–47.
Ali G, et al. A gene-expression-based test can outperform bap1 and p16 analyses in the differential diagnosis of pleural mesothelial proliferations. Oncol Lett. 2020;19(1):1060–5.
Chapel DB, et al. MTAP immunohistochemistry is an accurate and reproducible surrogate for CDKN2A fluorescence in situ hybridization in diagnosis of malignant pleural mesothelioma. Mod Pathol. 2020;33(2):245–54.
Churg A, et al. Highlights of the 14th international mesothelioma interest group meeting: Pathologic separation of benign from malignant mesothelial proliferations and histologic/molecular analysis of malignant mesothelioma subtypes. Lung Cancer. 2018;124:95–101.
Scherpereel A, et al. Soluble mesothelin-related peptides in the diagnosis of malignant pleural mesothelioma. Am J Respir Crit Care Med. 2006;173(10):1155–60.
Arnold DT, et al. Prognostication and monitoring of mesothelioma using biomarkers: a systematic review. Br J Cancer. 2017;116(6):731–41.
Creaney J, et al. Serum soluble mesothelin concentrations in malignant pleural mesothelioma: relationship to tumor volume, clinical stage and changes in tumor burden. Clin Cancer Res. 2011;17(5):1181–9.
de Fonseka D, et al. A prospective study to investigate the role of serial serum mesothelin in monitoring mesothelioma. BMC Cancer. 2018;18(1):199.
Robinson BW, et al. Soluble mesothelin-related protein–a blood test for mesothelioma. Lung Cancer. 2005;49(Suppl 1):S109–11.
Lynch G, et al. Serum mesothelin is a biomarker for disease progression and mortality in mesothelioma. Eur Respir J. 2023;62(suppl 67):OA1556.
Töreyin ZN, Ghosh M, Göksel Ö, Göksel T, Godderis L. Exhaled Breath Analysis in Diagnosis of Malignant Pleural Mesothelioma: Systematic Review. Int J Environ Res Public Health. 2020;17(3):1110. https://doi.org/10.3390/ijerph17031110.
Lamote K, Vynck M, Thas O, Van Cleemput J, Nackaerts K, van Meerbeeck JP. Exhaled breath to screen for malignant pleural mesothelioma: a validation study. Eur Respir J. 2017;50(6):1700919.
Disselhorst MJ, et al. Nose in malignant mesothelioma-Prediction of response to immune checkpoint inhibitor treatment. Eur J Cancer. 2021;152:60–7.
Kitajima K, et al. Deep learning with deep convolutional neural network using FDG-PET/CT for malignant pleural mesothelioma diagnosis. Oncotarget. 2021;12(12):1187–96.
• Kidd AC, et al. Fully automated volumetric measurement of malignant pleural mesothelioma by deep learning AI: validation and comparison with modified RECIST response criteria. Thorax. 2022;77(12):1251–9. Study evaluating the potential utility of artificial intelligence in radiological evaluation of mesothelioma, showing promise but highlighting areas for future work.
Choudhury A. Predicting cancer using supervised machine learning: Mesothelioma. Technol Health Care. 2021;29(1):45–58.
Courtiol P, et al. Deep learning-based classification of mesothelioma improves prediction of patient outcome. Nat Med. 2019;25(10):1519–25.
Naso JR, et al. Deep-learning based classification distinguishes sarcomatoid malignant mesotheliomas from benign spindle cell mesothelial proliferations. Mod Pathol. 2021;34(11):2028–35.
Treasure T, et al. Extra-pleural pneumonectomy versus no extra-pleural pneumonectomy for patients with malignant pleural mesothelioma: clinical outcomes of the Mesothelioma and Radical Surgery (MARS) randomised feasibility study. Lancet Oncol. 2011;12(8):763–72.
Lim E, et al. Mesothelioma and Radical Surgery 2 (MARS 2): protocol for a multicentre randomised trial comparing (extended) pleurectomy decortication versus no (extended) pleurectomy decortication for patients with malignant pleural mesothelioma. BMJ Open. 2020;10(9):e038892.
•• Lim E, Waller D, Lau K, Steele J, Pope A, Ali C, Bilancia R, Keni M, Popat S, O'Brien M, Tokaca N, Maskell N, Stadon L, Fennell D, Nelson L, Edwards J, Tenconi S, Socci L, Rintoul RC, Wood K, Stone A, Muthukumar D, Ingle C, Taylor P, Cove-Smith L, Califano R, Summers Y, Tasigiannopoulos Z, Bille A, Shah R, Fuller E, Macnair A, Shamash J, Mansy T, Milton R, Koh P, Ionescu AA, Treece S, Roy A, Middleton G, Kirk A, Harris RA, Ashton K, Warnes B, Bridgeman E, Joyce K, Mills N, Elliott D, Farrar N, Stokes E, Hughes V, Nicholson AG, Rogers CA; MARS 2 Investigators. Extended pleurectomy decortication and chemotherapy versus chemotherapy alone for pleural mesothelioma (MARS 2): a phase 3 randomised controlled trial. Lancet Respir Med. 2024 May 10:S2213-2600(24)00119-X. The first randomised randomised controlled trial comparing extended pleurectomy decortication for pleural mesothelioma with chemotherapy alone, showing that this surgery for mesothelioma resulted in poorer outcomes.
Rintoul RC, et al. Efficacy and cost of video-assisted thoracoscopic partial pleurectomy versus talc pleurodesis in patients with malignant pleural mesothelioma (MesoVATS): an open-label, randomised, controlled trial. Lancet. 2014;384(9948):1118–27.
Matthews C, et al. MesoTRAP: a feasibility study that includes a pilot clinical trial comparing video-assisted thoracoscopic partial pleurectomy decortication with indwelling pleural catheter in patients with trapped lung due to malignant pleural mesothelioma designed to address recruitment and randomisation uncertainties and sample size requirements for a phase III trial. BMJ Open Respir Res. 2019;6(1):e000368.
Ceresoli GL, et al. Phase II study of pemetrexed and carboplatin plus bevacizumab as first-line therapy in malignant pleural mesothelioma. Br J Cancer. 2013;109(3):552–8.
Dowell JE, et al. A multicenter phase II study of cisplatin, pemetrexed, and bevacizumab in patients with advanced malignant mesothelioma. Lung Cancer. 2012;77(3):567–71.
Kindler HL, et al. Multicenter, double-blind, placebo-controlled, randomized phase II trial of gemcitabine/cisplatin plus bevacizumab or placebo in patients with malignant mesothelioma. J Clin Oncol. 2012;30(20):2509–15.
Zalcman G, et al. Bevacizumab for newly diagnosed pleural mesothelioma in the Mesothelioma Avastin Cisplatin Pemetrexed Study (MAPS): a randomised, controlled, open-label, phase 3 trial. Lancet. 2016;387(10026):1405–14.
Scherpereel A, et al. Novel therapies for malignant pleural mesothelioma. Lancet Oncol. 2018;19(3):e161–72.
Maio M, et al. Tremelimumab as second-line or third-line treatment in relapsed malignant mesothelioma (DETERMINE): a multicentre, international, randomised, double-blind, placebo-controlled phase 2b trial. Lancet Oncol. 2017;18(9):1261–73.
Popat S, et al. A multicentre randomised phase III trial comparing pembrolizumab versus single-agent chemotherapy for advanced pre-treated malignant pleural mesothelioma: the European Thoracic Oncology Platform (ETOP 9–15) PROMISE-meso trial. Ann Oncol. 2020;31(12):1734–45.
Baas P, et al. First-line nivolumab plus ipilimumab in unresectable malignant pleural mesothelioma (CheckMate 743): a multicentre, randomised, open-label, phase 3 trial. Lancet. 2021;397(10272):375–86.
• Nowak AK, Jackson A, Sidhu C. Management of Advanced Pleural Mesothelioma-At the Crossroads. JCO Oncol Pract. 2022;18(2):116–24. Summary of the changing landscape of mesothelioma treatment.
Peters S, et al. LBA65 First-line nivolumab (NIVO) plus ipilimumab (IPI) vs chemotherapy (chemo) in patients (pts) with unresectable malignant pleural mesothelioma (MPM): 3-year update from CheckMate 743. Ann Oncol. 2021;32:S1341–2.
Scherpereel A, Antonia S, Bautista Y, Grossi F, Kowalski D, Zalcman G, Nowak A, Fujimoto N, Peters S, Tsao A, Mansfield A, Popat S, Sun X, Padilla B, Aanur P, Daumont M, Bennett B, McKenna MP. Baas, LBA1 First-line nivolumab (NIVO) plus ipilimumab (IPI) versus chemotherapy (chemo) for the treatment of unresectable malignant pleural mesothelioma (MPM): Patient-reported outcomes (PROs) from CheckMate 743. Ann Oncol. 2020;31.
• Kok PS, et al. Protocol of DREAM3R: DuRvalumab with chEmotherapy as first-line treAtment in advanced pleural Mesothelioma-a phase 3 randomised trial. BMJ Open. 2022;12(1):e057663. Trial protocol for upcoming randomised controlled trial of mesothelioma treatment comparing chemotherapy with combination treatment with an anti-PD-L1 agent and chemotherapy.
Chu QS, et al. IND227 phase III (P3) study of cisplatin/pemetrexed (CP) with or without pembrolizumab (pembro) in patients (pts) with malignant pleural mesothelioma (PM): A CCTG, NCIN, and IFCT trial. J Clin Oncol. 2023;41(17_suppl):LBA8505–LBA8505.
Szlosarek PW, et al. ATOMIC-Meso: A randomized phase 2/3 trial of ADI-PEG20 or placebo with pemetrexed and cisplatin in patients with argininosuccinate synthetase 1-deficient non-epithelioid mesothelioma. J Clin Oncol. 2017;35(15_suppl):TPS8582–TPS8582.
Szlosarek PW, et al. Abstract CT007: Phase 2–3 trial of pegargiminase plus chemotherapy versus placebo plus chemotherapy in patients with non-epithelioid pleural mesothelioma. Cancer Res. 2023;83(8_Supplement):CT007–CT007.
Yuan M, et al. The emerging treatment landscape of targeted therapy in non-small-cell lung cancer. Signal Transduct Target Ther. 2019;4:61.
Popat S, et al. Malignant pleural mesothelioma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2022;33(2):129–42.
Scherpereel A, et al. Nivolumab or nivolumab plus ipilimumab in patients with relapsed malignant pleural mesothelioma (IFCT-1501 MAPS2): a multicentre, open-label, randomised, non-comparative, phase 2 trial. Lancet Oncol. 2019;20(2):239–53.
Fennell DA, et al. Nivolumab versus placebo in patients with relapsed malignant mesothelioma (CONFIRM): a multicentre, double-blind, randomised, phase 3 trial. Lancet Oncol. 2021;22(11):1530–40.
Danson SJ, et al. Oncolytic herpesvirus therapy for mesothelioma - A phase I/IIa trial of intrapleural administration of HSV1716. Lung Cancer. 2020;150:145–51.
Bibby AC, et al. A trial of intra-pleural bacterial immunotherapy in malignant pleural mesothelioma (TILT) - a randomised feasibility study using the trial within a cohort (TwiC) methodology. Pilot Feasibility Stud. 2022;8(1):196.
Dulloo S, Fennell DA, Szlosarek PW, Thistlethwaite F, Lord S, Rahman NM, Greystoke A, Cunniff B, Dzialo J, Poile C, Panchal R, Duncan J, Graham P, Bexon AS, Naumov G, Spicer J. 1643TiP - First-in-human dose-escalation and expansion study (MITOPE) to evaluate mitochondrial PRX3 inhibition by RSO-021 in patients with mesothelioma and other advanced solid tumors. Ann Oncol. 2022;33:S743–9. https://doi.org/10.1016/j.annonc.2022.07.1722.
Author information
Authors and Affiliations
Contributions
All authors conceptualized the manuscript. G.A.L. wrote the main manuscript text. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
G.A.L. declares that she has no conflict of interest. N.A.M. has received grants and consulting fees from BD and Rocket Medical and consulting fees from Cook Medical. A.B. has received grants from Fujirebio.
Human and Animal Rights and Informed Consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of South West – Exeter research ethics committee (REF 15/SW/0156 & Ref 08/H0102/11) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lynch, G.A., Maskell, N.A. & Bibby, A. Recent Advances in Mesothelioma. Curr Pulmonol Rep (2024). https://doi.org/10.1007/s13665-024-00357-w
Accepted:
Published:
DOI: https://doi.org/10.1007/s13665-024-00357-w