Abstract
Purpose of review
This study aims to describe the pathophysiology of pregnancy in pulmonary hypertension (PH) and review recent literature on maternal and fetal outcomes.
Recent findings
There is an increasing number of pregnant women with PH. Maternal mortality in pulmonary arterial hypertension (PAH) ranges from 9 to 25%, most commonly from heart failure and arrythmias. The highest risk of death is peri-partum and post-partum. Fetal/neonatal morbidity and mortality are also substantial. There are high rates of prematurity, intrauterine growth retardation, and preeclampsia. Women should be referred to expert centers for management. Combination PAH therapy with parenteral prostacyclin and a phosphodiesterase type V inhibitor is recommended. Induced vaginal delivery is preferred, except in cases of severe heart failure or obstetric indications for cesarean section.
Summary
Despite advances in management, pregnancy in PAH remains a high-risk condition and should be prevented.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Pulmonary hypertension (PH) in pregnancy is among the most serious challenges in medicine. The potential consequences to both mother and fetus can be devastating. Despite advances in medical therapy and care of high-risk pregnancy, PH during gestation remains a dangerous clinical scenario requiring a comprehensive multi-disciplinary management strategy to optimize outcomes. In this review, we summarize the current state of knowledge of this problem, highlighting areas of uncertainty.
Overview of PH During Pregnancy
PH is defined as a mean pulmonary artery pressure (mPAP) by right heart catheterization > 20 mmHg and is classified into 5 groups (Table 1) [1]. Pulmonary arterial hypertension (PAH) and other types of pre-capillary PH also require a left heart filling or pulmonary artery wedge pressure (PAWP) ≤ 15 mmHg and an elevated pulmonary vascular resistance (PVR) of ≥ 3 Wood units. The most common group in pregnancy is that due to left heart disease (group 2), while pulmonary arterial hypertension (PAH; group 1) is the most life-threatening. Prognosis and appropriate management are critically dependent upon establishing the correct diagnosis and assessing the severity of disease.
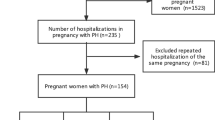
In an international registry, 151 out of 2966 (5.1%) pregnancies in women with cardiac disease had PH based upon Doppler echocardiography (DE) with an estimated right ventricular systolic pressure (RVSP) > 30 mmHg [2]. PH was considered due to left heart disease in 74%, overwhelmingly related to valvular rheumatic heart disease (92%), particularly in developing countries, with cardiomyopathy and myocarditis accounting for the remainder. PAH accounted for 26%. In nearly one quarter, PH was a new diagnosis during pregnancy. Other etiologies of pre-capillary PH such as chronic thromboembolic, chronic lung, and sickle cell disease are less common during pregnancy. Within group 1 PH, idiopathic PAH (IPAH) predominates in developed countries [3•, 4], whereas PAH associated with congenital systemic to pulmonary shunts (PAH-CHD) is more prevalent in resource-limited nations [5]. PAH associated with connective tissue disorders and other conditions may also be encountered in pregnancy [6, 7].
Various factors, including improved care and better survival for women with heart disease, have contributed to the increasing number of pregnant women with PH [8, 9]. The modified World Health Organization (mWHO) classification categorizes pregnant women with cardiovascular disease into four risk categories (Table 2) [10]. PAH specifically (not simply PH), due to any cause, is considered mWHO class IV with an extremely high risk of morbidity and mortality, thereby making pregnancy contraindicated [11].
Prevalence and Temporal Trends
Insight into the prevalence and temporal trends of PH in pregnancy in the USA can be gleaned from a recent analysis of the National Inpatient Sample [4, 9]. Of nearly 7 million delivery-related hospitalizations extracted from 2003 to 2012, a diagnosis of PH was present in 0.02% [4]. Sixty percent were classified as “isolated PH,” 20% due to valvular left heart disease, 13% associated with congenital heart disease, and 7% with cardiomyopathy. During this time frame, the yearly rate for PH, CHD, and cardiomyopathy increased significantly [9]. An analysis of the New York state inpatient database from 2003 to 2014 found a PH prevalence of 25 per 100,000 delivery-related hospitalizations [8]. Primary pulmonary hypertension (IPAH) accounted for 9%, while a secondary PH diagnosis was present in 91%. The prevalence of the latter group increased from 17 to 30 per 100,000 over the study period, reflecting an increase in pregnant women with valvular heart disease, obesity, and systemic hypertension. IPAH diagnosis decreased by 81% during the same period. A case rate of 17.8 per 100,000 deliveries was estimated from a retrospective review at four tertiary North American sites [6].
Physiology of Pregnancy And Delivery
During pregnancy, major cardiovascular changes occur to ensure adequate uteroplacental circulation to support fetal growth and development (Fig. 1). These changes are driven mostly by the hormones estrogen, progesterone, relaxin, vasopressin, and the renin-angiotensin-aldosterone system (RAAS). Other potential mediators include prostaglandins, prolactin, and nitric oxide [12].
Pathophysiology of pulmonary hypertension during pregnancy and delivery. The major physiologic cardiovascular changes during pregnancy are an increase in blood volume and cardiac output (left panel). In the setting of PAH, pulmonary vascular disease limits the rise in cardiac output, potentially compromising placental and fetal development. The additional hemodynamic stress of labor and delivery can precipitate right heart failure
Blood volume begins to increase within the first few weeks and increases throughout the entire pregnancy, peaking in the third trimester [13]. The increase can be as high as 100% of pre-pregnancy blood volume but generally is around 45–50% [13, 14]. Total extracellular water typically increases 6–8 L [15]. The increase in plasma volume is accompanied by a 20–30% increase in red blood cell mass due to erythropoietin stimulation, which results in the physiologic anemia of pregnancy [13].
Systemic vasodilation with reduction in systemic vascular resistance occurs as early as 5 weeks, reaching a nadir of 35–40% of pre-pregnancy values at 20 weeks, followed by a small increase from 32 weeks to term [16]. Cardiac output (CO) starts to increase by 5 weeks, peaking to up to 50% above baseline at mid-gestation. This increase is brought upon predominantly by an increase in stroke volume of 30% and a smaller rise in heart rate averaging 88 bpm in the third trimester [12, 17]. The augmented CO is required to support uterine blood flow which increases from 40 ml/min in the non-gravid state to up to > 1L/min at term and increases in oxygen consumption by 35% [15]. Systemic blood pressure falls slightly reaching a nadir in mid-pregnancy, followed by a rise to pre-pregnancy levels by term. Diastolic blood pressure decreases more than systolic (about 10 mmHg fall) resulting in widening of the pulse pressure [13]. The normally compliant pulmonary vascular bed is able to accommodate the increased cardiac output without an increase in pressure. Hence, pulmonary vascular resistance (PVR) falls as well [18] as a consequence of vasodilation combined with recruitment of the pulmonary microvasculature.
In PAH, the pulmonary vascular bed is noncompliant due to vascular obliteration and an imbalance between vasoconstrictor and vasodilator substances. It is therefore unable to accommodate the higher pulmonary blood flow; hence pulmonary artery pressure rises, and cardiac output becomes limited. The right ventricle (RV) dilates to augment end-diastolic volume and ultimately develops systolic and diastolic dysfunction. Furthermore, reduced CO can decrease systemic blood pressure, leading to compromised right coronary perfusion pressure in the setting of a dilated RV with high pressure. This in turn will promote RV ischemia with exacerbation of RV dysfunction, further reducing CO and initiating a vicious circle of cardiovascular decompensation, refractory right heart failure, and death.
Pregnancy is associated with a fivefold increased risk of venous thromboembolism (VTE) related to the pro-coagulant effects of estrogen on the liver, and pulmonary embolism can be poorly tolerated [19]. Iron deficiency, which is prevalent in up to 1 in 5 pregnancies, can further exacerbate anemia of pregnancy [20] and may have an adverse impact on pulmonary vascular tone and cardiac function [21].
During labor and delivery, CO increases above pre-labor levels by as much as 50% with pushing efforts. Autotransfusion of up to 0.5 L of blood occurs with uterine contraction further augmenting blood volume and circulatory stress. Immediately following delivery, there is a 60–80% increase in CO that is attributed to release of caval obstruction, autotransfusion of uteroplacental blood, and rapid mobilization of extravascular fluid [12]. Cardiac output falls rapidly after delivery and is back to pre-pregnancy levels by two weeks post-partum. These dramatic volume shifts account for the high incidence of cardiovascular morbidity and mortality during the peri-partum period [22].
An additional, but unproven factor in decompensation post-partum could be the sudden drop in cardioprotective hormones after delivery of the placenta, the primary source. Estrogen levels steadily increase throughout pregnancy and contribute to vasodilation in many organs. The effects of estrogen in PH are complex and contradictory. The “estrogen paradox” is used to describe the observation that while the incidence of PH is higher in women, men have greater mortality [23,24,25]. Estrogens have favorable effects on the pulmonary vasculature and RV function in animal models of PH [26,27,28,29,30]. However, the overall effects of estrogen in PH are unclear, and some studies suggest a pathogenic role. Anastrozole, an aromatase inhibitor which blocks conversion of androgens to estrogen, has been trialed therapeutically in PAH [31].
Minute ventilation rises 36% by week 8, reaching 50% above baseline at term. This is brought about mainly by a progesterone mediated increased in tidal volume rather than respiratory rate. The increase in minute volume is somewhat greater than ventilatory demand resulting in hypocapnia, approximately 30 mmHg. Appropriate renal compensation occurs resulting in mild respiratory alkalosis or normal pH. Arterial oxygen tension ranges from 92 to 107 mmHg [22]. Residual volume and functional residual capacity fall by 20% as the gravid uterus enlarges. In susceptible individuals, this could lead to closure of dependent airways and hypoxemia.
Placental Physiology
Oxygen has a high fractional extraction across the placenta; thus its delivery is blood flow-limited. Under normal circumstances, oxygen delivery is more than adequate to sustain fetal oxygenation. Below a certain threshold, however, fetal oxygen uptake falls (Fig. 2) [32]. In animal models, PO2 in the umbilical vein, the most oxygen-rich portion of the fetal circulation, equilibrates with, but remains lower than uterine vein PO2, typically 28 mmHg. With the leftward shift in the oxy-hemoglobin dissociation curve of fetal hemoglobin, this corresponds to an oxygen saturation of near 80% [33]. However, this occurs at the upper inflection point of the curve. Any fall in PO2 will result in steep declines in saturation (Fig. 3). A decrease in uterine vein PO2 and consequently umbilical vein PO2 would result from decreased uterine blood flow, maternal hypoxemia, or anemia. Thus, the impact of any arterial hypoxemia is magnified in the setting of reduced cardiac output or hemoglobin, which results in greater tissue oxygen extraction and lower venous oxygen tension.
Outcomes
Despite advancements in medical therapy, high-risk obstetrical care, and critical care support, PH continues to be associated with high morbidity and mortality for both mother and fetus. Reported outcomes are variable depending on the population studied, inclusion criteria, and duration of follow-up.
Historically, maternal mortality rates have been as high as 30–56% in PAH [34]. More contemporary series report mortality in the range of 9–25% [2, 3•, 6, 7, 35, 36••]. Causes of death are primarily right heart failure, life-threatening arrhythmias, sudden death, and VTE. The overwhelming majority occurs during the peri-partum and early post-partum periods.
In the prospective international Registry Of Pregnancy And Cardiac (ROPAC) disease, 4418 pregnant women with cardiac disorders were analyzed between 2013 and 2018. PAH made up only 1% of cases but had the poorest outcomes (Fig. 4) [36••]. The maternal mortality of 9% in this registry likely underestimates the true risk as right heart catheterization was not required for diagnosis, over half of subjects were NYHA functional class I prior to pregnancy, and outcomes were only tracked up to 1-week post-partum. Other outcomes highlight the risks faced in these pregnancies. Heart failure and arrythmia were higher than any other cardiac disease group (Fig. 4), as were thrombotic events (13%) and pre-eclampsia (11%). Caesarean section was also highest, performed in 71% with 16% on an emergency basis. Fetal outcomes were also the poorest with pre-maturity (defined as < 37 weeks) in 49% and a combined fetal and neonatal mortality of 8% [36••]. Similar findings were noted in the US National Inpatient Sample [4]. Major adverse cardiac events (MACE: mortality, heart failure, arrythmia, thromboembolism, cerebrovascular events, others) were noted in 25%, respiratory failure in 8%, and pre-eclampsia in 8%.
The occurrence of maternal cardiovascular events for different diagnosis groups in the ROPAC registry. CONHD: congenital heart disease; VHD: valvular heart disease; CMP: cardiomyopathy; IHD: ischemic heart disease; AOP: aortic pathology; PAH: pulmonary arterial hypertension. (From: Roos-Hesselink J et al. Eur Heart J 2019;40(47);3848). Used with permission from Oxford Academic
The high frequency of pre-eclampsia (general incidence of 2 to 8% [37]) is notable and maybe under-recognized given the tendency toward hypotension in PAH. An increased risk of pre-eclampsia has been observed in CHD [38]. While the pathogenesis of pre-eclampsia remains poorly understood, impaired uterine blood flow early during pregnancy may interfere with normal placental vascular development, resulting in generation of anti-angiogenic factors from the placenta which induces the subsequent vascular manifestations in the mother (Fig. 1). The potential impact of pre-eclampsia on maternal and fetal outcomes in PAH is not well characterized.
A separate analysis of PH in ROPAC reported maternal death in 3 of 7 IPAH patients (43%) compared to 1 death among 28 women with PAH-CHD [2]. Maternal mortality in PH due to left heart disease was 3%. Only 4% underwent therapeutic abortion. The severity of PH in this cohort was relatively modest with RVSP estimate of 30–50 mmHg in 60%. Importantly, 25% of women with an RVSP > 70 mmHg died within 6-month post-partum. Severe PH was also associated with a high occurrence of low birth weight (< 2500 gm) in 48%. Low birth weight is common, in part related to planned pre-term delivery. However, intrauterine growth restriction (or small for gestational age) has been described in up to 39% of PAH pregnancies [39, 40]. This is likely the result of utero-placental ischemia/hypoxia as discussed earlier (Fig. 1).
A relatively low maternal mortality rate of 4.8% was also reported in uncorrected CHD with PH in another ROPAC analysis [5]. Nevertheless, this rate was markedly higher than the 0.2% mortality observed among uncorrected CHD without PH. Major adverse cardiac events were also dramatically higher among those with PH (35% vs. 8%). Outcomes were worst among those with Eisenmenger syndrome (ES: central cyanosis with reversal of shunt to right to left) who had a maternal mortality of 10% and MACE rate of 66%. Fetal outcomes were not presented separately for the PAH subjects in this report. Previous data in cyanotic congenital heart disease, excluding ES, indicate that when maternal oxygen saturation is < 85%, a live birth occurred in only 12% of cases, whereas live birth occurred in 92% with a saturation > 90% [41].
In a retrospective single-center study of 318 pregnant women with CHD in China, 12 of the 13 maternal deaths were in ES patients in whom the mortality rate was 46% [42]. Significant predictors of major adverse maternal events were ES, severe PH, advanced functional class, lower oxygen saturation, tachycardia and lower left ventricular ejection fraction. Risk factors for adverse fetal outcomes were ES, reduced oxygen saturation, and pre-eclampsia.
In non-pregnant persons, PAH-CHD is generally associated with better survival compared with IPAH, yet survival in PAH-CHD is poorest among those who have undergone defect closure [43]. This is felt to reflect the ability of the shunt lesion to allow “pop-off” of right heart afterload, allaying right heart failure, albeit at the cost of increased right to left shunt and hypoxemia.
An important contemporary experience comes from a multi-national prospective registry of 26 well-characterized pregnant PAH patients [3•]. Sixty-four percent had IPAH and 38% were NYHA functional class III–IV at time of pregnancy discovery. Six women underwent elective termination at a mean of 10 weeks gestation. All survived without complications. Two died after spontaneous abortions during the first trimester. One died and another required extra-corporeal life support followed by urgent heart-lung transplantation, each after delivering a healthy baby, for an overall death/transplant rate of 20% among those who proceeded with pregnancy. Compared with those who survived without transplant, the 4 who died or were transplanted had severe derangements in pulmonary hemodynamics (mPAP, 71 vs. 36 mmHg; cardiac index, 2.0 vs. 3.2 L/min/m2; right atrial pressure, 11 vs. 4 mmHg). Half of the former group were long-term responders to calcium-channel blockers, an uncommon IPAH phenotype.
Similar observations were reported in a retrospective multi-center US experience in PAH where 1/3rd underwent elective termination and maternal mortality was 17% in the remainder [7]. Another recent North American series reported 7 maternal deaths among 30 PAH patients (23%), all post-partum, including 2 after elective termination, whereas all 11 women with PH due to left heart disease survived, 2 of whom underwent therapeutic abortion [6]. There was one fetal death and no neonatal mortality. In contrast, late fetal mortality was observed in 31% of PAH patients in a series from China [44].
Pregnancy Counseling
Professional societies recommend pregnancy avoidance in PAH, along with other serious cardiac disorders classified as mWHO pregnancy risk class IV [10, 22]. Yet, studies suggest that this topic is often not discussed [22, 45]. Over half of women with cardiac disease in the ROPAC registry reported not receiving pre-conceptual counseling, including those with risk class IV conditions [36••]. Interestingly, those who did receive counseling had half the rate of maternal mortality or heart failure during pregnancy as those who did not. Genetic counseling should also be offered to women with heritable or idiopathic PAH and genetic testing considered [22].
Long-acting reversible contraceptives, including intra-uterine devices and progestin-only subcutaneous etonogestrel implants, are safe and effective in women with cardiac disease with a very low incidence of thromboembolism [46]. Tubal ligation is a permanent method, but procedural risks are a potential concern. Male sterilization is the ideal option. Estrogen containing oral contraceptives carry an increased risk of thromboembolism. Progestin-only oral contraceptives are safe but requires strict adherence for sufficient efficacy [22]. For those patients who insist on becoming pregnant, emphasis should be placed on maximizing medical therapy while using contraception to optimize RV function prior to family planning [3•].
Diagnosis and Assessment of Severity
For newly diagnosed PH patients, a comprehensive evaluation is required to establish the diagnosis and type of PH [47]. A nuclear perfusion lung scan can safely be obtained during pregnancy to exclude chronic thromboembolic disease. The absence of segmental perfusion defects obviates the need for a computed tomography (CT) pulmonary angiogram [48]. When required, modern CT imaging techniques to reduce fetal radiation exposure should be applied [49]. Careful interpretation of echocardiography should be performed, with special attention paid to RV size and function and evidence of left heart and congenital heart disease. False elevation in RV systolic pressure can be seen in up to 30% of pregnant patients [50]. A right heart catheterization (RHC) is required to establish the diagnosis and assess current severity for those previously diagnosed. Acute vasodilator challenge during RHC should be performed only in IPAH patients without severe RV dysfunction to identify vasoreactivity and potential therapeutic response to calcium channel blockers [47]. Risk stratification [51] is important to guide medical management, termination considerations, and assess prognosis. Prognostic markers in PAH include advanced functional class, reduced 6-min walk distance and right atrial size, RV dysfunction, and pericardial effusion on echocardiography. Hemodynamic markers are right atrial pressure, cardiac output, and PVR. B-type natriuretic peptide (BNP) levels in healthy women typically increase two-fold during pregnancy; however, the value is expected to remain in the normal range [52,53,54,55,56]. Hence BNP’s retain their utility as useful biomarkers of disease severity in heart disease [57], including PAH [58] during pregnancy.
Termination of Pregnancy
Once a comprehensive evaluation is completed, a multi-disciplinary consensus recommendation should be provided to the patient. Termination is generally the safest option and should be offered to all pregnant women with PAH [10, 22]. While a successful outcome is clearly possible and, in many cases, probable, those with profound derangements in hemodynamics and severe RV dysfunction are at extremely high risk. Since most deaths occur post-partum, these patients and family members need to be clearly advised regarding the distinct possibility of new baby without a mother.
Termination can be performed up until fetal viability, generally 24 weeks. Therapeutic abortion is generally well-tolerated, although does pose risks for women with advanced disease [59] and should be undertaken as early as possible prior to major cardiovascular changes associated with pregnancy. Seriously ill women are at increased risk for spontaneous miscarriage which can be fatal [3•], particularly in an unmonitored setting where uncontrolled hemorrhage can occur.
Management of Pregnancy
Level of Care
Patients who continue their pregnancy should be referred to an experienced PH center with a multi-disciplinary team of PH specialists and high-risk obstetricians. These women should be cared for at a maternal care level IV facility (regional perinatal health care center) as defined by the American College of Obstetrics and Gynecology [60] where a full complement of subspecialty care is available onsite 24/7, including critical care, cardiac surgery, obstetric anesthesia, transplant, and advanced mechanical circulatory support capabilities (Table 3).
The Multi-disciplinary Team
A dedicated interdisciplinary team is critical to the successful management of these complex, high-risk pregnancies [10]. The members of this team should include all the disciplines listed in Table 4. At our center, this group meets monthly for presentation of new patients and status updates on previous cases. All aspects of the treatment plan are reviewed. A clear strategy for timing and mode of delivery are agreed upon. Input is sought from all disciplines, and any differences of opinion are resolved by consensus. Ad hoc meetings are arranged prior to planned delivery to review and finalize details and ensure availability of all necessary personnel and equipment. A written summary is entered into a conspicuous location in the medical record and distributed to all members. Consistent and frequent communication among the team is mandatory. It is also imperative to have regular contact between the outpatient and inpatient teams, particularly for patients who require hospitalization during pregnancy for acute decompensation (the “warm hand-off”). The nurse navigator serves as a constant team member to facilitate communication between the care teams. Informing and educating patients is essential in helping them understand their clinical state and treatment options that best fit their management during pregnancy and post-partum.
Supportive Care
Supplemental oxygen should be provided to maintain saturation ≥ 94% if possible and may have utility in those with right to left intra-cardiac shunting who respond [61]. Volume status requires careful assessment and judicious use of diuretics. Arrythmias, such as atrial flutter or fibrillation, are poorly tolerated and should be aggressively managed with a preference for rhythm control [62]. Iron deficiency should be corrected. Low dose aspirin is advisable starting in the first trimester to reduce the risk of pre-eclampsia [63]. Among women at high risk, aspirin decreases the incidence of pre-eclampsia by 15–20% without major adverse consequences [64]. Avoidance of hypotension, hypoxia, and acidosis is paramount, as these can precipitate refractory heart failure [10].
Therapeutic anticoagulation may be of benefit in IPAH outside of pregnancy [47] and should be initiated in patients not already on it, given the additional thromboembolic risk associated with pregnancy. Anticoagulation should also be considered in PAH-CHD without a history of significant hemoptysis or other risk factors for bleeding and on an individual basis in those with PAH associated with connective tissue disease [10]. Vitamin K antagonists are contraindicated in the first trimester and pose the risk of under and over anticoagulation. Novel oral agents have not been adequately studied in pregnancy; thus low-molecular weight heparins are the drug of choice. Prophylactic dosing may provide adequate protection while reducing bleeding risk.
Targeted PAH Medical Therapy
Considerable advances have been made in medical therapy of PAH. Available drugs target one of three pathways: prostacyclin, endothelin, and nitric-oxide/cGMP. Endothelin-receptor antagonists and the soluble guanylate cyclase stimulator, riociguat, are teratogenic and should be avoided in pregnancy. In high-risk non-pregnant PAH patients, combination therapy including intravenous prostacyclin is recommended [51]. Given the high risk associated with pregnancy, intravenous (IV) epoprostenol is preferred in all but the mildest cases with near normal RV function as it is the only therapy shown to reduce mortality in a randomized controlled trial in IPAH [65]. Inhaled iloprost [66] and intravenous treprostinil [67] have also been successfully used in pregnancy. Experience with subcutaneous treprostinil is extremely limited, and no reports of oral prostacyclin analogs during pregnancy are available. A PDE5 inhibitor, either sildenafil or tadalafil, is often combined with a prostacyclin for additive effect [68]. Some authors have reserved the use of IV therapy until late pregnancy prior to planned delivery [22, 67]. While this approach minimizes the adverse effects and inconvenience of continuous IV infusion, it risks possible progression of disease. Continued need for IV therapy can be reassessed after delivery and if favorable, a trial of de-escalation to an oral regimen undertaken with close monitoring for deterioration. In a small minority of IPAH patients who are deemed vasoreactive based on a positive acute vasodilator challenge and without severe RV dysfunction, calcium channel blockers are appropriate and safe to use in pregnancy [3•]. Importantly, PAH-targeted agents have not been shown to be of benefit and can be detrimental in PH due to left heart disease [69]. Therapy in this group should be directed toward optimization of left heart function.
Monitoring
Careful serial assessment for signs of RV decompensation is critical. Monthly visits during the first trimester with visits every 1–2 weeks thereafter with high-risk obstetricians and pulmonary hypertension specialists are recommended [22]. Limited echocardiography with focus on RV size and function should be obtained every 1–2 months until the third trimester and then monthly or more frequently as clinically indicted. Serial laboratory evaluation can include brain natriuretic peptide (BNP). If there is suspicion for worsening PH, follow-up RHC can be considered to guide subsequent therapy. Monthly fetal ultrasound is essential to detect growth restriction. Fetal echocardiography at 20–24 weeks is recommended to detect congenital heart disease. During the third trimester, regular ante-natal testing allows detection of fetal distress as indicated by decreased heart rate variability, reduced movement and breathing, hypotonia, and oligohydramnios [10]. Such findings may dictate immediate delivery.
Delivery
A detailed plan for the timing and mode of elective delivery should be in place early in third trimester [19]. The European Society of Cardiology recommends induced vaginal delivery for most women with cardiac disease, although planned cesarean section is advised for PAH by others [22]. The main hazards of vaginal delivery are the repeated Valsalva maneuvers during pushing efforts. The profound rise in intra-thoracic pressure will reduce venous return, while high intra-alveolar pressure can compress pulmonary vessels and increase RV afterload. Cesarean section, on the other hand, risks complications from anesthesia and surgical recovery and is associated with more bleeding and infection compared with vaginal delivery. In a ROPAC registry analysis of women with primarily congenital and valvular heart disease, planned vaginal delivery was associated with lower maternal mortality and post-partum heart failure compared with planned cesarean section [70]. We generally prefer induced vaginal delivery with adequate analgesia and vacuum-assisted second stage of labor to attenuate pushing efforts in women with stable cardiopulmonary status. Cesarean section is reserved for those with advanced heart failure or obstetric indications. Timing is preferably at 34–36 weeks to minimize the duration of hemodynamic load on the mother while avoiding severe fetal immaturity. Also, the smaller fetus facilitates vaginal delivery. A 24-h course of steroids is given prior to induction to enhance lung maturity.
Induction is achieved by ripening the cervix with local application of misoprostol (a synthetic PGE-1) or dinoprostone (a PGE-2). Systemic absorption does occur and can rarely cause systemic hypotension, coronary vasospasm, and arrythmia [10]. Mechanical dilation of the cervix is an alternative and adjunctive method. Once the cervix is dilated, if labor has not commenced, judicious use of low-dose oxytocin infusion is begun to stimulate uterine contractions. Oxytocin can induce systemic vasodilatation and pulmonary vasoconstriction and is discouraged by some authors [71].
If post-partum hemorrhage occurs, uterotonic agents such as ergot alkaloids and the synthetic PGF2 alpha, carboprost, should be avoided as they can induce systemic and pulmonary vasoconstriction [19]. Oxytocin infusion and misoprostol should be used with caution, given the risks outlined above. Alternative options to control hemorrhage include uterine massage, tranexamic acid, intrauterine tamponade balloon placement, or surgical management.
Full critical care and extra-corporeal membrane oxygenation (ECMO) resources should be on stand-by in case of cardiopulmonary deterioration during delivery and the early post-partum period. Arterial and central venous lines allow continuous monitoring of right atrial pressure and systemic blood pressure with frequent assessment of arterial blood gases and central venous saturation. Pulmonary artery catheterization may be useful in selected cases. It is crucial that hypotension, hypoxia, hypercapnia, and acidosis be avoided as these can lead to further compromise of RV function. Pre-load should be optimized with volume administration or diuretics as needed. Pulmonary vasoactive medications can be augmented, as tolerated, to maximize their effect on PVR. Vasopressor and/or inotropic support maybe required to maintain adequate organ perfusion. Since most deaths occur in the immediate post-partum period, continued ICU monitoring is recommended for at least 48 h.
Anesthesia Considerations
Regardless of mode of delivery, the plan for anesthesia should be determined early in pregnancy by collaboration between the obstetrician and a combined obstetric and cardiac anesthesiology team. The goal should be to provide adequate pain control while minimizing negative effects on cardiac output, systemic blood pressure, and gas exchange [72]. For vaginal delivery, early neuraxial analgesia (epidural, combined spinal-epidural, or dural puncture epidural) is encouraged to mitigate catecholamine-induced cardiovascular stress from labor pain. Patient-controlled epidural analgesia or programmed intermittent epidural bolus technique with a low-dose local anesthetic plus opioid solution is recommended. The goal for labor is excellent pain control without significant motor block. Importantly, a functioning epidural catheter can also be dosed with more concentrated local anesthetic if necessary. A dense perineal block can facilitate comfortable instrumental assistance in the second stage of labor. Dosing can be augmented for surgical anesthesia if unscheduled cesarean delivery becomes necessary.
Neuraxial anesthesia is also preferred for most scheduled cesarean deliveries to avoid the cardiopulmonary complications of general anesthesia. A systematic review found a fourfold increased mortality rate with general versus regional anesthesia [35]. Although spinal anesthesia with a single injection provides the most dense, reliable block, it is more likely to induce a rapid sympathectomy with systemic hypotension, compared with epidural where the dose of anesthetic can be slowly titrated to desired effect. Volume loading, along with a vasopressor infusion, can attenuate the vasodilatory effects of spinal and/or epidural anesthesia. Many anesthesiologists choose a combined spinal-epidural approach to balance the risks and benefits of the two techniques. Long-acting opioids such as morphine can be added to the spinal dose or via the epidural catheter to ensure good pain control post-operatively.
Careful coordination with the primary care team regarding timing of anticoagulation relative to neuraxial anesthesia is essential to reduce the risk of spinal-epidural hematoma. Pregnancy and pulmonary hypertension are both hypercoagulable states. The risks of altering thromboprophylaxis around the time of delivery are often conflicting with the anesthesiologist's goal of providing neuraxial pain control. Although there is a paucity of data on the incidence of catastrophic spinal-epidural hematoma in pregnant women, a recently published review does provide some guidance on the decision-making process around anticoagulation and neuraxial anesthesia considering the unique physiology of pregnancy [73]. Pregnant women in fact have a very low risk of spinal-epidural hematoma (estimated at 1:250,000) compared to other populations. Conversely, they have an increased risk of difficult airway and aspiration. These considerations, along with the delicate cardiopulmonary balance of the pulmonary hypertension patient, illustrate why neuraxial is preferred over general anesthesia when feasible.
Rescue Strategies
There is limited data on ECMO use during pregnancy or the post-partum period. Successful use of veno-venous ECMO for respiratory failure has been described [74], but there are scant reports of veno-arterial use. If required prior to delivery, urgent delivery should be undertaken to avoid potentially negative effects on the fetus and relieve the hemodynamic stress on the mother. In one series, all 6 women requiring ECMO support for PH during pregnancy died [6], but successful application as a bridge to recovery has been reported [75, 76]. Complications include bleeding, systemic emboli, and infection. Given the high mortality rate with severe PAH in pregnancy and lack of clear predictors of outcome, lung transplantation should be considered an option. However, it is difficult and challenging to evaluate transplant candidacy during critical illness. It is prudent to introduce this possibility early during pregnancy and begin a formal evaluation so that a decision to list the patient can be made expeditiously if it appears that recovery from ECMO will be unlikely [77].
Post-Partum Care
Close monitoring after discharge is mandatory as these patients are at risk for clinical worsening and mortality in the months and years after delivery [35, 77]. It is unknown if pregnancy has a deleterious effect on the natural history of PAH. Breastfeeding is not advised as PAH drugs can be secreted in breast milk [78]. Effective contraception should be offered immediately.
Summary
While improvements have been made in the current era, pulmonary hypertension in pregnancy remains a high-risk condition. Discussion and education on the potential outcomes, contraception options, and pregnancy termination should be a shared decision-making process between the physician and patient. An early multi-disciplinary approach is crucial for those patients who decide to continue their pregnancy.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Simonneau G, Montani D, Celermajer DS, Denton CP, Gatzoulis MA, Krowka M, et al. Haemodynamic definitions and updated clinical classification of pulmonary hypertension. Eur Respir J. 2019;53:1801913.
Sliwa K, van Hagen IM, Budts W, Swan L, Sinagra G, Caruana M, et al. Pulmonary hypertension and pregnancy outcomes: data from the Registry Of Pregnancy and Cardiac Disease (ROPAC) of the European Society of Cardiology. Eur J Heart Fail. 2016;18:1119–28.
Jais X, Olsson KM, Barbera JA, et al. Pregnancy outcomes in pulmonary arterial hypertension in the modern management era. Eur Respir J. 2012;40:881–5 Contemporary multi-center series with prospective identification of PAH in pregnancy. Provides detailed assessment and outcomes.
Thomas E, Yang J, Xu J, Lima FV, Stergiopoulos K. Pulmonary hypertension and pregnancy outcomes: insights from the national inpatient sample. J Am Heart Assoc. 2017;6.
Sliwa K, Baris L, Sinning C, Zengin-Sahm E, Gumbiene L, Yaseen IF, et al. Pregnant women with uncorrected congenital heart disease: heart failure and mortality. JACC Heart Fail. 2020;8:100–10.
Meng ML, Landau R, Viktorsdottir O, et al. Pulmonary hypertension in pregnancy: a report of 49 cases at four tertiary North American sites. Obstet Gynecol. 2017;129:511–20.
Duarte AG, Thomas S, Safdar Z, Torres F, Pacheco LD, Feldman J, et al. Management of pulmonary arterial hypertension during pregnancy: a retrospective, multicenter experience. Chest. 2013;143:1330–6.
Guglielminotti J, Landau R, Friedman AM, Li G. Pulmonary hypertension during pregnancy in New York state, 2003-2014. Matern Child Health J. 2019;23:277–84.
Lima FV, Yang J, Xu J, Stergiopoulos K. National trends and in-hospital outcomes in pregnant women with heart disease in the United States. Am J Cardiol. 2017;119:1694–700.
European Society of G, Association for European Paediatric C, German Society for Gender M, et al. ESC Guidelines on the management of cardiovascular diseases during pregnancy: the task force on the management of cardiovascular diseases during pregnancy of the European society of cardiology (ESC). Eur Heart J. 2011;32:3147–97.
ACOG. Practice Bulletin No. 212: Pregnancy and heart disease. Obstet Gynecol. 2019;133:e320–e56.
Ouzounian JG, Elkayam U. Physiologic changes during normal pregnancy and delivery. Cardiol Clin. 2012;30:317–29.
Sanghavi M, Rutherford J. Cardiovascular physiology of pregnancy. Circulation. 2014;130:1003–8.
Pritchard J. Changes in the blood volume during pregnancy and delivery. Anesthesiology. 1965;26:393–9.
Resnik R, Brace R. A. Physiology of Pregnancy. In: West JB, editor. Best and Taylor's Physiologic Basis of Medical Practice. 12th ed. Baltimore: Williams and Wilkins; 1990. p. 892–910.
Soma-Pillay P, Nelson-Piercy C, Tolppanen H, Mebazaa A. Physiological changes in pregnancy. Cardiovasc J Afr. 2016;27:89–94.
Hunter S, Robson S. Adaptation of the maternal heart during pregnancy. Br Heart J. 1992;68:540–3.
Robson SC, Hunter S, Boys RJ, Dunlop W. Serial changes in pulmonary haemodynamics during human pregnancy: a non-invasive study using Doppler echocardiography. Clin Sci (Lond). 1991;80:113–7.
Banerjee D, Ventetuolo CE. Pulmonary hypertension in pregnancy. Semin Respir Crit Care Med. 2017;38:148–59.
McMahon L. Iron deficiency in pregnancy. Obstet Med. 2010;3:17–24.
Rhodes CJ, Wharton J, Howard L, Gibbs JS, Vonk-Noordegraaf A, Wilkins MR. Iron deficiency in pulmonary arterial hypertension: a potential therapeutic target. Eur Respir J. 2011;38:1453–60.
Hemnes AR, Kiely DG, Cockrill BA, Safdar Z, Wilson VJ, Hazmi MA, et al. Statement on pregnancy in pulmonary hypertension from the Pulmonary Vascular Research Institute. Pulm Circ. 2015;5:435–65.
Umar S, Rabinovitch M, Eghbali M. Estrogen paradox in pulmonary hypertension: current controversies and future perspectives. Am J Respir Crit Care Med. 2012;186:125–31.
Benza RL, Miller DP, Gomberg-Maitland M, et al. Predicting survival in pulmonary arterial hypertension: insights from the registry to evaluate early and long-term pulmonary arterial hypertension disease management (REVEAL). Circulation. 2010;122:164–72.
Humbert M, Sitbon O, Chaouat A, Bertocchi M̀, Habib G, Gressin V, et al. Survival in patients with idiopathic, familial, and anorexigen-associated pulmonary arterial hypertension in the modern management era. Circulation. 2010;122:156–63.
Earley S, Resta TC. Estradiol attenuates hypoxia-induced pulmonary endothelin-1 gene expression. Am J Physiol Lung Cell Mol Physiol. 2002;283:L86–93.
Lahm T, Albrecht M, Fisher AJ, et al. 17β-Estradiol attenuates hypoxic pulmonary hypertension via estrogen receptor-mediated effects. Am J Respir Crit Care Med. 2012;185:965–80.
Lahm T, Crisostomo PR, Markel TA, Wang M, Wang Y, Tan J, et al. Selective estrogen receptor-alpha and estrogen receptor-beta agonists rapidly decrease pulmonary artery vasoconstriction by a nitric oxide-dependent mechanism. Am J Physiol Regul Integr Comp Physiol. 2008;295:R1486–93.
Lahm T, Patel KM, Crisostomo PR, et al. Endogenous estrogen attenuates pulmonary artery vasoreactivity and acute hypoxic pulmonary vasoconstriction: the effects of sex and menstrual cycle. Am J Physiol Endocrinol Metab. 2007;293:E865–71.
Umar S, Iorga A, Matori H, Nadadur RD, Li J, Maltese F, et al. Estrogen rescues preexisting severe pulmonary hypertension in rats. Am J Respir Crit Care Med. 2011;184:715–23.
Kawut SM, Archer-Chicko CL, DeMichele A, Fritz JS, Klinger JR, Ky B, et al. Anastrozole in pulmonary arterial Hypertension. A randomized, double-blind, placebo-controlled Trial. Am J Respir Crit Care Med. 2017;195:360–8.
Wilkening RB, Meschia G. Fetal oxygen uptake, oxygenation, and acid-base balance as a function of uterine blood flow. Am J Phys. 1983;244:H749–55.
Meschia G. Fetal oxygenation and maternal ventilation. Clin Chest Med. 2011;32:15–9.
Weiss BM, Zemp L, Seifert B, Hess OM. Outcome of pulmonary vascular disease in pregnancy: a systematic overview from 1978 through 1996. J Am Coll Cardiol. 1998;31:1650–7.
Bedard E, Dimopoulos K, Gatzoulis MA. Has there been any progress made on pregnancy outcomes among women with pulmonary arterial hypertension? Eur Heart J. 2009;30:256–65.
Roos-Hesselink J, Baris L, Johnson M, et al. Pregnancy outcomes in women with cardiovascular disease: evolving trends over 10 years in the ESC Registry Of Pregnancy And Cardiac disease (ROPAC). Eur Heart J. 2019;40:3848–55 Recent international prospective registry of pregnancy in cardiac disease, including pulmonary arterial hypertension, demonstrating worst outcome in latter.
Steegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R. Pre-eclampsia. Lancet. 2010;376:631–44.
Schlichting LE, Insaf TZ, Zaidi AN, Lui GK, Van Zutphen AR. Maternal comorbidities and complications of delivery in pregnant women with congenital heart disease. J Am Coll Cardiol. 2019;73:2181–91.
Keepanasseril A, Pillai AA, Yavanasuriya J, Raj A, Satheesh S, Kundra P. Outcome of pregnancies in women with pulmonary hypertension: a single-centre experience from South India. BJOG. 2019;126(Suppl 4):43–9.
Ladouceur M, Benoit L, Radojevic J, Basquin A, Dauphin C, Hascoet S, et al. Pregnancy outcomes in patients with pulmonary arterial hypertension associated with congenital heart disease. Heart. 2017;103:287–92.
Presbitero P, Somerville J, Stone S, Aruta E, Spiegelhalter D, Rabajoli F. Pregnancy in cyanotic congenital heart disease. Outcome of mother and fetus. Circulation. 1994;89:2673–6.
Chu R, Chen W, Song G, et al. Predicting the risk of adverse events in pregnant women with congenital heart disease. J Am Heart Assoc. 2020;9:e016371.
Manes A, Palazzini M, Leci E, Bacchi Reggiani ML, Branzi A, Galie N. Current era survival of patients with pulmonary arterial hypertension associated with congenital heart disease: a comparison between clinical subgroups. Eur Heart J. 2014;35:716–24.
Sun X, Feng J, Shi J. Pregnany and pulmonary hypertension: an exploratory analysis of risk factors and outcomes. Medicine. 2018;97:e13035.
Kovacs AH, Harrison JL, Colman JM, Sermer M, Siu SC, Silversides CK. Pregnancy and contraception in congenital heart disease: what women are not told. J Am Coll Cardiol. 2008;52:577–8.
Apter D, Briggs P, Tuppurainen M, Grunert J, Lukkari-Lax E, Rybowski S, et al. A 12-month multicenter, randomized study comparing the levonorgestrel intrauterine system with the etonogestrel subdermal implant. Fertil Steril. 2016;106:151–7 e5.
Galie N, Humbert M, Vachiery JL, et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: the joint task force for the diagnosis and treatment of pulmonary hypertension of the European society of cardiology (ESC) and the European respiratory society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International society for heart and lung transplantation (ISHLT). Eur Heart J. 2016;37:67–119.
Brent R. The pulmonologist's role in caring for pregnant women with regard to the reproductive risks of diagnostic radiological studies or radiation therapy. Clin Chest Med. 2011;32:33–42.
Konstantinides SV, Meyer G, Becattini C, Bueno H, Geersing GJ, Harjola VP, et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European respiratory society (ERS). Eur Heart J. 2020;41:543–603.
Wylie BJ, Epps KC, Gaddipati S, Waksmonski CA. Correlation of transthoracic echocardiography and right heart catheterization in pregnancy. J Perinat Med. 2007;35:497–502.
Galie N, Channick RN, Frantz RP, et al. Risk stratification and medical therapy of pulmonary arterial hypertension. Eur Respir J. 2019;53:1801889.
Balaceanu A. B-type natriuretic peptides in pregnant women with normal heart or cardiac disorders. Med Hypotheses. 2018;121:149–51.
Burlingame JM, Yamasato K, Ahn HJ, Seto T, Tang WHW. B-type natriuretic peptide and echocardiography reflect volume changes during pregnancy. J Perinat Med. 2017;45:577–83.
Tanous D, Siu SC, Mason J, Greutmann M, Wald RM, Parker JD, et al. B-type natriuretic peptide in pregnant women with heart disease. J Am Coll Cardiol. 2010;56:1247–53.
Hameed AB, Chan K, Ghamsary M, Elkayam U. Longitudinal changes in the B-type natriuretic peptide levels in normal pregnancy and postpartum. Clin Cardiol. 2009;32:E60–2.
Mayama M, Yoshihara M, Uno K, Tano S, Takeda T, Ukai M, et al. Factors influencing brain natriuretic peptide levels in healthy pregnant women. Int J Cardiol. 2017;228:749–53.
Singh K, Sikka P, Suri V, Prasad R, Khullar M, Vijayvergiya R. Brain natriuretic peptide in pregnant women with heart disease. Obstet Med. 2020;13:25–9.
Prasad CS, Kumar S, Sumathy S, Kunjukutty R, Puthenveettil N, Sen AC, et al. Pregnancy and pulmonary arterial hypertension-improving surveillance and outcomes with multidisciplinary care and N terminal pro-brain natriuretic peptide trends. J Matern Fetal Neonatal Med. 2020:1–7.
Martin SR, Edwards A. Pulmonary hypertension and pregnancy. Obstet Gynecol. 2019;134:974–87.
American Association of Birth C, Association of Women's Health O, Neonatal N, et al. Obstetric care consensus #9: levels of maternal care: (replaces obstetric care consensus number 2, February 2015). Am J Obstet Gynecol. 2019;221:B19–30.
Baumgartner H, De Backer J, Babu-Narayan SV, et al. ESC Guidelines for the management of adult congenital heart disease. Eur Heart J. 2020;2020.
Georgiopoulos G, Tsiachris D, Kordalis A, Kontogiannis C, Spartalis M, Pietri P, et al. Pharmacotherapeutic strategies for atrial fibrillation in pregnancy. Expert Opin Pharmacother. 2019;20:1625–36.
Mol BWJ, Roberts CT, Thangaratinam S, Magee LA, de Groot CJM, Hofmeyr GJ. Pre-eclampsia. Lancet. 2016;387:999–1011.
ACOG. Committee Opinion No. 743 Summary: low-dose aspirin use during pregnancy. Obstet Gynecol. 2018;132:254–6.
Barst RJ, Rubin LJ, Long WA, McGoon MD, Rich S, Badesch DB, et al. A comparison of continuous intravenous epoprostenol (prostacyclin) with conventional therapy for primary pulmonary hypertension. N Engl J Med. 1996;334:296–301.
Kiely DG, Condliffe R, Webster V, Mills GH, Wrench I, Gandhi SV, et al. Improved survival in pregnancy and pulmonary hypertension using a multiprofessional approach. Bjog. 2010;117:565–74.
Smith JS, Mueller J, Daniels CJ. Pulmonary arterial hypertension in the setting of pregnancy: a case series and standard treatment approach. Lung. 2012;190:155–60.
Simonneau G, Rubin LJ, Galie N, et al. Addition of sildenafil to long-term intravenous epoprostenol therapy in patients with pulmonary arterial hypertension: a randomized trial. Ann Intern Med. 2008;149:521–30.
Guay CA, Morin-Thibault LV, Bonnet S, Lacasse Y, Lambert C, Lega JC, et al. Pulmonary hypertension-targeted therapies in heart failure: a systematic review and meta-analysis. PLoS One. 2018;13:e0204610.
Ruys TP, Roos-Hesselink JW, Pijuan-Domenech A, et al. Is a planned caesarean section in women with cardiac disease beneficial? Heart. 2015;101:530–6.
Zhang J, Lu J, Zhou X, Xu X, Ye Q, Ou Q, et al. Perioperative management of pregnant women with idiopathic pulmonary arterial hypertension: an observational case series study from China. J Cardiothorac Vasc Anesth. 2018;32:2547–59.
Arendt KW, Lindley KJ. Obstetric anesthesia management of the patient with cardiac disease. Int J Obstet Anesth. 2019;37:73–85.
Leffert L, Butwick A, Carvalho B, Arendt K, Bates SM, Friedman A, et al. The society for obstetric anesthesia and perinatology consensus statement on the anesthetic management of pregnant and postpartum women receiving thromboprophylaxis or higher dose anticoagulants. Anesth Analg. 2018;126:928–44.
Pacheco LD, Saade GR, Hankins GDV. Extracorporeal membrane oxygenation (ECMO) during pregnancy and postpartum. Semin Perinatol. 2018;42:21–5.
Rosenzweig EB, Abrams D, Biscotti M, Kerstein D, Drassinower D, Brodie D, et al. Eisenmenger syndrome and pregnancy: novel ECMO configuration as a bridge to delivery and recovery utilizing a multidisciplinary Team. ASAIO J. 2018;64:e8–e10.
Phoophiboon V, Jaimchariyatam N, Srimahachota S, Sirinawin C. Successful multimodality management of severe pulmonary arterial hypertension during pregnancy with VA-ECMO and atrial septostomy using stent. BMJ Case Rep. 2019;12.
Kamp JC, von Kaisenberg C, Greve S, Winter L, Park DH, Fuge J, et al. Pregnancy in pulmonary arterial hypertension: midterm outcomes of mothers and offspring. J Heart Lung Transplant. 2021;40:229–33.
Olsson KM, Channick R. Pregnancy in pulmonary arterial hypertension. Eur Respir Rev. 2016;25:431–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
All authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Women's Health and Lung Disease
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Krishnan, S., Fricke, E.M., Cordoba, M. et al. Pulmonary Hypertension Complicating Pregnancy. Curr Pulmonol Rep 10, 71–83 (2021). https://doi.org/10.1007/s13665-021-00275-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13665-021-00275-1