Abstract
In our clinic, more patients wish to treat pathological phimosis with a preputioplasty to preserve their foreskin. This study aims to analyze the long-term effects of preputioplasty. Additionally, we have produced an instructional video for those who want to master this surgical technique. A retrospective cohort study was performed in boys aged ≤ 18 years old suffering from pathological phimosis. All patients underwent preputioplasty between January 2011–2020. The outcome of the preputioplasty is considered positive when the foreskin was retractable months post-operative.
In total, 176 patients were included. The mean age operating was 8.9 years. A positive result after preputioplasty was observed in 163/176 patients (93%). Patients with a negative outcome most often chose a re-operation: circumcision in seven cases and a redo-preputioplasty in three. Four patients showed complications (minor infection (1), wound dehiscence (2), and excess amount of skin (1)). Thus, a preputioplasty is shown to be a feasible operative treatment option.
Samenvatting
Een preputiumplastiek is een behandeloptie voor pathologische fimose waarbij de voorhuid behouden blijft. In de dagelijkse praktijk kiezen steeds meer patiënten voor deze optie. Deze studie beoogt de langetermijneffecten van deze chirurgische interventie te analyseren. Bovendien hebben we een instructievideo van de preputiumplastiek vervaardigd voor degenen die deze chirurgische techniek onder de knie willen krijgen. Een retrospectieve cohortstudie werd uitgevoerd onder jongens van ≤ 18 jaar met pathologische fimose, die tussen januari 2011 en januari 2020 een preputiumplastiek ondergingen in het Wilhelmina Kinderziekenhuis (WKZ). Het resultaat van de preputiumplastiek was geslaagd wanneer de voorhuid maanden postoperatief te retraheren was. In totaal werden 176 patiënten geïncludeerd. De gemiddelde operatieleeftijd was 8,9 jaar. Een positief resultaat na preputiumplastiek werd waargenomen bij 163/176 patiënten (93 %). Vier patiënten vertoonden complicaties (kleine infectie (n = 1), wonddehiscentie (n = 2) en huidoverschot (n = 1)). Dertien patiënten hadden een negatieve uitkomst (7 %). De conclusie is dat een preputiumplastiek een geschikte operatieve behandeloptie is.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Phimosis is a condition where the foreskin cannot be retracted by gentle manipulation over the glans [1]. At birth this condition is physiological, but phimosis can be pathological as well. About 96% of male babies born have a non-retractable foreskin. In most cases, this is physiological since the phimosis is a result of neonatal adhesions between the prepuce and the glans. This commonly causes no complaints or pain. As these children get older, the adhesions will dissipate, and the phimosis will disappear [2]. In some cases, children develop symptoms such as (recurrent) episodes of balanitis. This can cause scarring of the foreskin and persisting phimosis. In that case, we speak of pathologic phimosis. By the age of 16, pathological phimosis occurs in 0.6% of the male population [3].
The initial treatment of pathological phimosis consists of non-invasive, topical administration of corticosteroid ointment. The guideline database of the Netherlands from the Federation Medical Specialists initiated by the Dutch urology professional association the NVU describes a success rate from 45 to 95% [4]. The European Association of Urology (EAU) states that administering corticoid ointment or cream twice a day over a period of 4–8 weeks has a success rate > 80% [5]. When the treatment with corticosteroids is unsuccessful, (recurrence rate of up to 17% [5]) pathological phimosis will often require surgical intervention. Predominantly, circumcision is the technique of choice in those cases [3, 6]. However, to treat the phimosis and preserve the foreskin in the process, preputioplasty is a viable surgical option. In our clinic, the Wilhelmina Children’s Hospital (WKZ), an increasing number of patients or their parents request to preserve the foreskin.
Current literature does not clarify which operative approach is preferable. No significant differences in critical outcome measures or side effects/complications are shown [7]. Based on the guideline it can also be concluded that preputioplasty is a good alternative compared to circumcision. To enlarge the current literature on preputioplasty, this study aims to look at the long-term effects of preputioplasty. To provide tailored treatment per individual the caretaker should provide all treatment options. Surgeons treating pathological phimosis should therefore master the surgical technique of a preputioplasty. For educational purposes, we have produced an instructional video on how to perform a preputioplasty. This video can be viewed by scanning the QR-code attached to this article.
Methods
A retrospective cohort study was performed on boys under the age of 18 who underwent preputioplasty because of pathological phimosis at Wilhelmina Children’s Hospital (WKZ) between the 1st of January 2011 and the 1st of January 2020. Children diagnosed with hypospadias or a buried penis, as well as patients with a previous foreskin operation were excluded. Furthermore, we excluded patients who had objected to using their data for research. A flowchart of this study is shown in Fig. 1.
Various determinants have been collected. At baseline, determinants consisted of initial preoperative complaints and symptoms, including ballooning, spraying of urine, paraphimosis, (recurrent) balanitis and erection pain. In addition, data was collected on the optical presence of balanitis xerotica obliterans (BXO)/lichen sclerosus/scarring. Also, we specified in how many cases this diagnosis was confirmed histopathologically. Finally, post-operative outcomes including complications were documented.
A retractable foreskin (by gentle manipulation) months after the operation was considered a positive outcome. Some patients had to practice retraction postoperatively or had to use topical corticosteroids. In these cases, the foreskin eventually became retractable. The following postoperative outcomes were considered negative: re-operation: redo preputioplasty, re-operation: circumcision, recurrence of phimosis: no intervention.
Surgical technique
Preputioplasty techniques performed included a multiple Z‑plasty, a (multiple) Y‑V plasty, or a (multiple) dorsal slit. The operations were performed by different surgeons.
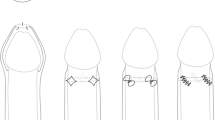
In the multiple Z‑plasty procedures, four perpendicular incisions are made on the constricted ring of the foreskin and are extended into the inner foreskin. The tissue bridges between the incisions are cleaved creating a ‘zigzag’ wound. Equal flaps created are swapped causing an increase in length [8]. The stenotic ring of the foreskin widens, and the foreskin becomes retractable. For an illustration of this technique see Fig. 2 from https://plasticsurgerykey.com/ [9]. Fig. 3a shows a preoperative picture of a patient with pathological phimosis and Fig. 3b a postoperative picture of the same patient after multiple Z‑preputioplasty.
Illustration of the mechanism of a multiple Z‑plasty [9]. a shows drawing of the positions where incision is needed (preoperatively). b shows the situation after operation. Note the elongation of the skinline
Picture of a patient with pathological phimosis. a Preoperative. b The multiple Z‑plasty, postoperative result [9]
The Y‑V plasty, either multiple or single, also creates a widening of the stenotic ring. A previous article by our department entitled ‘Y‑V plasty of the foreskin as an alternative to circumcision for surgical treatment of phimosis during childhood’ contains a clear illustration with an explanation of this procedure [1]. The procedure starts with an inverted V‑shaped incision in the outer foreskin at the dorsal side of the penis. A longitudinal incision is then made in the inner foreskin, extending the V‑shaped incision into a Y-shape. The longitudinal incision of the inner foreskin opens in a diamond shape. Subsequently, the V‑shaped incision of the outer foreskin fits when closing the wound edges. The Y‑incision now becomes V‑shaped. Figs. 4 and 5 are self-made illustrations of the Y‑V plasty originating from the instructional video.
The technique of a longitudinal (multiple) dorsal slit is a relatively simple way to widen the stenotic ring of the foreskin. Hotonu et al. illustrates this technique in a figure [3]. The longitudinal incision(s) on the constricting preputial ring is transversely closed with interrupted sutures.
The instructional video focuses on both the multiple Z‑plasty and the Y‑V plasty.
Results
A total of 176 patients were included in our study. The mean age at the time of surgery was 8.9 years (range 1 month to 18 years). 140 patients were treated with topical corticosteroid cream before surgery as an initial non-invasive treatment option.
Initial preoperative complaints and symptoms are summarized in Tab. 1. Note that some patients had multiple symptoms preoperatively. 21 of the patients were clinically diagnosed with balanitis xerotica obliterans (BXO) of which in thirteen this was proven histopathologically. The type of preputioplasties is also summarized in Tab. 1.
The outcome of the preputioplasty was positive in 163 patients (93%). 87 patients showed a well-retractable foreskin without complaints and further necessary intervention. 29 of patients were advised to apply corticosteroids postoperatively and five patients needed extra encouragement to initiate practicing retraction of the foreskin. Two patients with a retractable foreskin did undergo an extra operation for adhesiolysis. Unfortunately, follow-up data regarding 40 patients was not provided.
Out of the 13 patients (7%) with a negative outcome, circumcision was conducted in seven cases and a redo preputioplasty in four. Two boys with recurrence of phimosis decided not to undergo further intervention. 3/13 patients with a negative outcome were diagnosed with BXO.
A total of four patients showed complications (2%). One patient developed an infection, two patients developed wound dehiscence. The fourth patient was left with an excess amount of skin.
Discussion
In our clinic, many patients with phimosis desire to preserve the foreskin. Our findings show that in a group of 176 boys with pathological phimosis 163 (93%) had a retractable foreskin after preputioplasty. Four patients showed complications (2%). Consistent with other literature a preputioplasty shows to be a feasible operative treatment option for pathological phimosis in our population [1, 3, 6, 10, 11].
The population included in this study consists of 176 pediatric patients. A large study population in the field of pediatric urology. Follow-up time is reasonable namely 76 months. The instructional video attached to this article has not yet been published. It definitely adds value to this article. We hope it enables colleagues to provide preputioplasty as one of the treatment options for phimosis.
Several limitations of this study should nevertheless be considered. Firstly, the study relies on retrospective data research. Especially on the outcome, this resulted in 40 boys without postoperative follow-up information. Based on the assumption that ‘no news is good news’ they were placed in the positive outcome group. In several patient reports, it is stated that revision was only necessary for the presence of post-operative complaints or recurrence of phimosis. Though, for some boys, it may be an obstacle to come forward with genital complaints. If boys did seek medical help in the past, one might expect that they would also present in case of post-operative complaints or recurrence. When we would exclude these 40 patients, our positive result would still be 90%.
Both in literature as guidelines, pathological phimosis with balanitis xerotica obliterans (BXO) practically excludes preputioplasty as a treatment option [5, 7, 10, 12]. The question that arises is whether there is sufficient research on the outcome of a preputioplasty in patients with BXO to exclude this treatment option. Some studies have even excluded patients with (clinical suspicion) BXO from their study population when examining the outcomes of the preputioplasty [13]. In contrast Benson et al. examined the results of a Z-plasty in boys with preputial scarring. They found all 28 boys had a fully retractable foreskin without complication at follow-up [14]. Wilkinson et al. compared the results of a preputioplasty and circumcision in boys with BXO. Their results show a good outcome for most boys undergoing foreskin preputioplasty and intralesional triamcinolone (PIT) [15]. A recent study from 2021 states that it is feasible to perform a multicentered randomized controlled trial (RCT) comparing circumcision to preputioplasty and intralesional triamcinolone (PIT) to treat BXO [16]. In this study three of 13 patients with a negative outcome were diagnosed with BXO (23%), versus 18 patients with a positive outcome (11%). In relative terms, BXO occurs twice as often in the negative outcome group compared to the positive outcome group.
A long-term complication that may occur after a circumcision is the meatal stenosis. By incising at the frenulum, the vascularization of the meatus sometimes gets damaged. Another theory states that this can occur when urine irritates the ventral urethral meatus, causing chemical dermatitis with subsequent scarring. Meatus stenosis rarely, if ever, occurs after a preputioplasty [17, 18]. Circumcision has one big advantage over the preputioplasty as it enholds no evident risk of recurrence. This often requires a re-operation [7]. In this study this was the case in eleven of our patients.
Conclusion
This study examined the results of the foreskin sparing treatment preputioplasty for phimosis. In a group of 176 boys with phimosis 163 had a retractable foreskin after preputioplasty. Complication rates were low. To offer the entire range of treatment options to their patients, surgeons treating phimosis should master the surgical technique of a preputioplasty. In our clinic, we have produced an instructional video on preputioplasty intended to help colleagues to learn this technique. The instructional video can be watched by scanning the QR-code.

References
Nieuwenhuijs JL, Dik P, Klijn AJ, de Jong TPVM. Y‑V plasty of the foreskin as an alternative to circumcision for surgical treatment of phimosis during childhood. J Pediatr Urol. 2007;3(1):45–7.
Shahid SK. Phimosis in children. ISRN Urol. 2012;2012:707329.
Hotonu S, Mohamed A, Rajimwale A, Gopal M. Save the foreskin: Outcomes of preputioplasty in the treatment of childhood phimosis. Surgeon. 2020;18(3):150–3.
Richtlijnendatabase. Federatie Medisch Specialisten. Behandeling voorhuidpathologie. Operatie versus medicatie. https://richtlijnendatabase.nl/richtlijn/behandeling_voorhuidpathologie/voorhuidpathologie_phimosis/phimosis_operatie_versus_medicatie.html. Accessed 19 Jan 2022.
European Association of Urology (EAU) guidelines. Paediatric urology. https://uroweb.org/guideline/paediatric-urology/. Accessed 2 Mar 2022.
te Dorsthorst MJ, Roelofs AWTM, Vrooman OPJ, et al. Verwijden of verwijderen? De preputiumplastiek is een goed alternatief voor therapeutische circumcisie. Tijdschr Urol. 2019;9:74–7.
Richtlijnendatabase. Federatie Medisch Specialisten. Behandeling voorhuidpathologie. Voorhuidsparende behandeling versus circumcisie. https://richtlijnendatabase.nl/richtlijn/behandeling_voorhuidpathologie/voorhuidpathologie_phimosis/phimosis_voorhuidsparende_behandeling_versus_circumcisie.html. Accessed 19 Jan 2022.
Salam GA, Amin JP. The basic Z‑plasty. Am Fam Physician. 2003;67(11):2329–32.
Plastic surgery key. Z‑plasty. https://plasticsurgerykey.com/z-plasty/. Accessed 31 May 2022.
Berber NJ, Chapell B, Carter PG, Britton JP. Is preputioplasty effective and acceptable? J R Soc Med. 2003;96(9):452–3.
Impellizzeri P, Turiaco N, Antonuccio P, et al. Preputioplasty in the treatment of phimosis in pediatric age. Indications and results. Minerva Pediatr. 2006;58(1):15–9.
Nguyen ATM, Holland AJA. Balanitis xerotica obliterans: an update for clinicians. Eur J Pediatr. 2020;179(1):9–16.
Pedersini P, Parolini F, Bulotta AL, Alberti D. “Trident” preputial plasty for phimosis in childhood. J Pediatr Urol. 2017;13(3):278.e1–278.e4.
Benson M, Hanna MK. Prepuce sparing: Use of Z‑plasty for treatment of phimosis and scarred foreskin. J Pediatr Urol. 2018;14(6):545.e1–545.e4.
Wilkinson DJ, Lansdale N, Everitt LH, et al. Foreskin preputioplasty and intralesional triamcinolone: a valid alternative to circumcision for balanitis xerotica obliterans. J Pediatr Surg. 2012;47(4):756–9.
Lansdale N, Arthur F, Corbett HJ. Circumcision versus preputioplasty for balanitis xerotica obliterans: a randomised controlled feasibility trial. BJU Int. 2021;128(6):759–65.
UpToDate. Neonatal circumcision: Risks and benefits. Available from https://www-uptodate-com.proxy.library.uu.nl/contents/neonatal-circumcision-risks-and-benefits?search=circumcision&source=search_result&selectedTitle=1~102&usage_type=default&display_rank=1. Accessed 18 Mar 2022.
UpToDate. Complications of circumcision. Available from https://www-uptodate-com.proxy.library.uu.nl/contents/complications-of-circumcision?search=circumcision&source=search_result&selectedTitle=4~102&usage_type=default&display_rank=4. Accessed 18 Mar 2022.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Bosveld, J., Hornung, P., Klijn, A.J. et al. Retrospective analyses on preputioplasties in boys with pathological phimosis performed over the last nine years. Tijdschr Urol 12, 155–160 (2022). https://doi.org/10.1007/s13629-022-00370-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13629-022-00370-1