Abstract
Psoriasis is a chronic, immune-mediated, inflammatory skin disease, associated with multiple comorbidities and psychological and psychiatric disorders. The quality of life of patients with this disease is severely compromised, especially in moderate-to-severe plaque psoriasis. Secukinumab, a fully humanized monoclonal antibody, was the first anti-interleukin (IL)-17 biologic approved for treating psoriasis. Secukinumab demonstrated long-lasting efficacy and a good safety profile in individuals with plaque psoriasis, and it is associated with an improvement in health-related quality of life. While there is evidence that early treatment with systemic therapy can affect disease progression and improve long-term outcomes in other autoimmune diseases, evidence is limited in psoriasis, especially in real-world settings. This review provides an overview of studies describing the effectiveness of secukinumab in the treatment of psoriasis summarizing the literature and focusing on real-world evidence and early intervention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Secukinumab has long-term clinical efficacy and safety in the treatment of psoriasis, but more focus is needed on early intervention. |
Early treatment of psoriasis with secukinumab improves the quality of life of people with the disease and supports the prevention of long-term disabilities and comorbidities, such as psoriasis arthritis. |
Secukinumab is safe to use and shows benefits also in hard-to-treat populations and difficult-to-treat body areas. |
Secukinumab should be considered as a treatment option for psoriasis, not only for individuals at early disease stages but also for those with a long history of the disease. |
Introduction
Psoriasis (PsO) is a common chronic, systemic, immune-mediated inflammatory disease that affects the skin. PsO affects 125 million people worldwide, and its prevalence and incidence vary according to geographic region, gender, and age [1, 2]. PsO is associated with several comorbidities, including psoriatic arthritis (PsA), Crohn’s disease (CD), and psychological/psychiatric disorders (e.g., depression, and anxiety). In recent years, also metabolic syndrome, inflammatory bowel disease, diabetes, cardiovascular diseases, malignancies (e.g., lymphoma), and infections have been associated with PsO [3]. In addition, individuals with PsO are at a higher risk of reduced life expectancy [4]. Manifestations of the disease may involve itching, stinging, and burning of the skin, which together with extracutaneous clinical manifestations, significantly affects the health-related quality of life (HRQoL) of these patients [5]. Disease progression is often unpredictable, with different degrees of severity and progression. PsO management can minimize physiological and physical harm by treating patients early in the disease to modify its course, preventing associated comorbidities, reducing risks of negative outcomes, and aiming at remission [6]. The pathogenesis of psoriasis is influenced by the interleukin (IL)-23/IL-17 pathway, which is involved in the inflammatory processes underlying this chronic skin condition. IL-23 is a cytokine that fosters the production of IL-17; in the pathogenesis of PsO, the T helper 17 pathway and cytokine interleukin 17 (IL-17) play a fundamental role. The mechanism of action of several antipsoriatic treatments currently in use and under development is aimed at blocking IL-17 and its mediated downstream immunological cascade. IL-17 effectors include IL-17A, IL-17C, IL-17E, and IL-17F, which are responsible for the pro-inflammatory feed-forward cycle in plaque psoriasis [7]. The interplay between IL-17 and IL-23 maintains the chronic inflammatory state characteristic of psoriasis. Monoclonal antibodies targeting interleukin IL-23, like guselkumab and resankizumab, and IL-17, like secukinumab and ixekinumab, showed efficacy in the treatment of moderate-to-severe psoriasis. IL-17 and IL-23 inhibitors are both effective treatments for psoriasis, although they differ in their mechanisms of action and clinical outcomes (Table 1). IL-17 inhibitors target the IL-17 cytokine, thus leading to rapid relief of the symptoms due to the direct action on inflammation. IL-23 inhibitors target the IL-23 cytokine, which is key for the production of IL-17, thus providing sustained control [8, 9]. Drug survival, defined as the duration of a specific treatment, seems accordingly to be more favorable for IL-23 inhibitors in terms of long-time effectiveness [10,11,12,13,14].
Secukinumab is a fully humanized anti-IL-17A monoclonal antibody that was approved in 2015 by the US Food and Drug Administration and the European Commission as the first biologic for the treatment of moderate-to-severe plaque psoriasis, active psoriatic arthritis (PsA), and axial spondyloarthritis (axSpA) [15]. Secukinumab is indicated and well received for the treatment of moderate-to-severe plaque psoriasis in children > 6 years old, adolescents, and adults who are eligible for systemic therapy. In pediatric plaque psoriasis (adolescents and children from the age of 6 years to 18 years old), the recommended dose of secukinumab is based on body weight, while in adult plaque psoriasis it is 300 mg. Secukinumab is administered by subcutaneous injection with initial dosing at weeks 0, 1, 2, 3, and 4, followed by monthly maintenance dosing [16]. In adults, a maintenance dose of 300 mg every 2 weeks can provide additional benefits after initial assessment of clinical response. A multicenter, randomized clinical trial evaluated two different dosing regimens (i.e., secukinumab 300 mg every 2 weeks vs secukinumab 300 mg every 4 weeks) in patients with bodyweight > 90 kg [17]. After 16 weeks, the 2-week dosing demonstrated higher efficacy compared to the 4-week regimen psoriasis area and severity index (PASI) 90, 73.2% vs 55.5%, p = 0.0003. In multiple phase II and III clinical trials, secukinumab was shown to be superior to placebo and to other biologics, such as etanercept and ustekinumab, in the treatment of moderate-to-severe plaque psoriasis, and its clinical efficacy correlated with large improvements in patients’ quality of life [18]. Secukinumab also showed a long-term safety profile in multiple phase II and III clinical trials for the treatment of moderate-to-severe plaque PsO. A pooled safety analysis of ten Phase II and III studies showed that secukinumab has a favorable safety profile that is similar between the 300 and the 150 mg doses [19]. The safety profile of secukinumab was comparable to that of etanercept over 52 weeks in patients with moderate-to-severe plaque psoriasis. Secukinumab also showed a safety profile comparable to ustekinumab in long-term follow-up studies [20]. A pooled analysis including 21 randomized controlled clinical trials examined the long-term (5 years) safety and tolerability profile of secukinumab for the treatment of moderate-to-severe psoriasis, psoriatic arthritis, and ankylosing spondylitis (AS) [21]. The study results suggest that secukinumab has a favorable safety profile over a long treatment period in patients with these chronic conditions. In alignment with previous research, the study supports the long-term use of secukinumab in the treatment of PsO, PsA, and AS, as these disorders share IL-17A overexpression [15, 22]. However, as reported for other biologics, patients with autoimmune diseases taking IL-17 inhibitors are at increased risk of infections, and the most commonly described adverse events associated with secukinumab are upper respiratory tract infections, neutropenia, candidiasis, and rare cases of new or worsening inflammatory bowel disease [19, 23,24,25]. Of note, secukinumab might have a beneficial effect on the cardiometabolic risks associated with psoriasis as a reduction in systemic inflammation could also contribute to indirectly mitigating the risk of adverse cardiovascular conditions [26, 27].
There is evidence that in immune-mediated inflammatory diseases, such as rheumatoid arthritis, early intervention, defined as a time window for the onset of therapy (systemic or biologic) of 6–12–24 months after disease manifestation, with targeted systemic therapy can improve long-term patient outcomes [28]. Similarly, it has been hypothesized that early intervention with systemic agents in plaque psoriasis may alter the course of the disease, improve cutaneous symptoms, and reduce long-term adverse outcomes [28, 29]. Given the high prevalence of this condition in the population and its detrimental impact on patients’ quality of life, evaluating the long-term effectiveness, safety, and comorbidity control of secukinumab in the treatment of psoriasis in a real-world setting is of paramount importance. This review aims to provide a comprehensive overview of the effectiveness of secukinumab in the treatment of psoriasis, also summarizing findings on early interventions (considered as occurring within two years of disease onset) through an analysis of the latest evidence available in the field (Table 2).
Methods
In July 2022, all the authors met to discuss the available evidence on the use of secukinumab in the early treatment of psoriasis, aiming at having a broader view of its use in clinical practice and at supporting the unmet medical needs of individuals affected or at higher risk of the disease. The authors reviewed the literature available, focusing in particular on real-world evidence.
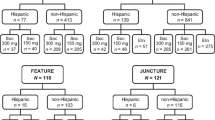
A systematic search of the literature using the Embase database was conducted between inception and June 2022. Without applying restrictions, the terms searched used were the following: “real life setting,” “real world,” “RW,” “real world evidence,” “RWE,” “real life,” “evidence,” “case report,” “case series,” “observational studies,” “observational study,” “prospective observational studies,” “retrospective observational studies,” “retrospective study,” “prospective study,” “secukinumab,” “Cosentyx,” “SEC,” “Italy,” “italian,” “psoriasis,” “PSO,” “early treatment,” “naïve,” “Nail,” “Scalp,” “Palmoplantar Psoriasis,” “problematic area,” “psoriatic arthritis,” “arthritis,” “PSA,” “early PSA,” “naïve,” “quality of life,” “QoL,” “adherence,” “adherence to treatment,” “treatment adherence,” “compliance to therapy,” “therapy compliance,” “adherence to therapy,” “compliance to treatment,” “treatment compliance,” “therapy adherence,” “discontinued,” “discontinue,” “rates of adherence,” “non-adherence,” “Survey,” “questionnaire,” “suspension,” “retention rate,” “Long term use,” “long term,” “naïve,” “biologic-naivety,” “Biologic Disease-Modifying Antirheumatic Drugs,” “bDMARDs,” “DMARDs,” “de novo,” “systemic treatment naïve,” “treatment failure,” “anti-TNFα failure,” and “tnf-inhibitor failure.” The literature search was updated in June 2024 to select additional articles relevant to the topic.
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Early Treatment with Secukinumab in PsO
Psoriasis is often not diagnosed or treated in atimely manner, leading to worse clinical outcomes for the patients. Early systemic treatment of immune-mediated inflammatory diseases, such as rheumatoid arthritis and Crohn’s disease, has been shown to improve long-term patient outcomes [28]. However, to date, there is no universally accepted definition of what constitutes an “early” intervention in PsO treatment as clinicians still need to agree on the criteria to screen patients [28, 29]. Girolomoni and colleagues [28] defined an early intervention as the “time window for the onset of therapy between 6 and 24 months after disease manifestation,” based on observations from other chronic diseases. However, the authors highlighted how immediate treatment at disease onset might favorably impact the long-term course of the disease and halt mental health issues [28].
There are different clinical trials in the literature exploring the effects of secukinumab early treatment in patients with PsO. A randomized, double-blind, placebo-controlled phase II trial showed that early suppression of the IL-23/IL17 axis in individuals with psoriasis by secukinumab treatment improved plaque histopathology and promoted plaque resolution at week 12 [30]. In this study, clinical efficacy was associated with histopathological features, immunohistochemistry (IHC) cell counts, and mRNA transcription profile of lesional plaques and non-lesional skin biopsy specimens collected at baseline, weeks 1, 4, 12, and 52. In these patients, the levels of the upstream genes IL-23 and the related IL-17F were reduced, suggesting that secukinumab disrupts the IL-17A-dependent feedback mechanisms that drive plaque chronicity [30]. A phase II regimen-finding study reported that early and monthly induction therapy with secukinumab 150 mg resulted in significantly higher response rates of Psoriasis Area Severity Index (PASI) 75 than placebo therapy (54.5% and 42.0% vs. 1.5%; p < 0.001 for both regimens) at week 12; similarly, PASI 90 response rates were significantly higher with early and monthly treatment than with placebo (31.8% and 17.4% vs. 1.5%, respectively; p < 0.001 for both regimens) [31]. In a sub-analysis of this study, an improvement in health-related quality of life was observed in patients treated with different secukinumab doses compared to placebo [32]. The early secukinumab regimen was also associated with improvement in difficult-to-treat areas [33]. Interestingly, secukinumab showed early response rates in patients who switched from cyclosporine A (CyA) therapy after inadequate response to treatment. A total of 37 patients were treated subcutaneously with 300 mg secukinumab and 41.2% of patients reached PASI 50 by week 2; 82.4% of patients met the primary endpoint PASI 75 at week 16. PASI 90/100 and IGA 0/1 were met by 64.7%, 29.4%, and 70.6%, respectively. Of note, higher response rates were observed in biologic-naive patients than in patients with prior biologic exposure [34].
The STEPin study was the first trial designed to determine whether early intervention with either standard narrowband UVB (nb-UVB) or secukinumab treatment in patients with new-onset (< 12 months) plaque psoriasis could alter the natural history of the disease [35]. Results at 52 weeks showed that 91.1% (70/77) of patients in the secukinumab arm achieved a PASI 90 response compared to 42.3% (32/76) in the nb-UVB arm (p < 0.0001). This supports the notion that early treatment with secukinumab is more effective than standard treatment with nb-UVB in patients with new-onset moderate-to-severe plaque psoriasis [36]. Of note, recent and ongoing clinical trials on guselkumab and rizamkizumab are exploring PsO early interventions for newly diagnosed patients [37, 38], and additional real-world studies would be key to gaining supportive evidence.
Early administration of secukinumab in biologic-naive patients was shown to improve clinical outcomes compared with biologic-experienced patients also in real-life studies, suggesting that it may be considered as a first-line treatment for psoriatic patients [39,40,41,42,43]. A retrospective analysis of real-world data from 151 patients with moderate-to-severe plaque psoriasis, including patients with palmoplantar psoriasis (PP), found a significant association between positive response to secukinumab and no prior use of biologic therapies [40]. Similarly, a recent real-world study found that biologic-naive patients who did not have concurrent PsA derived the greatest benefit from treatment with secukinumab [41]. The study involved 83 patients diagnosed with psoriasis, 25.3% with palmoplantar psoriasis, and the effectiveness of secukinumab and its good retention time were described [41]. Differences in clinical outcomes were also observed in PsA patients who did not receive biologics versus multi-failure patients when treated with secukinumab [42]. Patients receiving secukinumab as first-line therapy with a biologic showed improvements in multiple outcomes, such as ASDAS, PASI, and MDA, compared to patients with multiple therapeutic failures.
Data from the PURE registry, a prospective cohort study in 2362 adult patients with moderate-to-severe plaque psoriasis treated with secukinumab or standard therapy, confirmed the early and sustained resolution of erythema and scaling of the skin [44], also for non-responders [45].
In conclusion, early treatment with secukinumab can be considered a valuable option not only for the treatment of the early stages of the disease but also in patients with a long history of disease as the early introduction of secukinumab as a primary treatment approach led to better clinical outcomes.
Early Treatment of Difficult-to-Treat Body Areas Can Result in Enhanced Secukinumab Efficacy and Effectiveness
Psoriasis affecting hands, feet, nails, scalp, face, and genitals can be underdiagnosed and difficult to treat. The most common difficult-to-treat areas are the scalp, face, nails, soles, genitals, and palms [46]. Although the areas commonly affected by PsO in these sites may be limited, the impact on patients’ quality of life is significant, mainly because of the psychosocial consequences. The Palmoplantar Psoriasis Area and Severity index (ppPASI), Nail Psoriasis and Severity Index (NAPSI), and Scalp-modified PASI (S-mPASI) are rating scales specifically designed to measure the impact of the disease in these areas. For patients suffering from PsO in hard-to-treat areas of the body, traditional therapeutic options have limitations, and topical agents may not be effective or well tolerated [47]. However, to date, several therapeutic options are available for this subclass of patients, depending on the severity and extent of the disease. Recent evidence supported the effectiveness of anti-IL-17 and anti-IL-23 agents for the treatment of difficult-to-treat areas in patients with PsO [48, 49], with anti IL-17 agents achieving a better control of scalp psoriasis. In this regard, biologics such as secukinumab are playing an important role [50]. The randomized controlled trial GESTURE investigated the efficacy and safety of secukinumab 300 mg and 150 mg versus placebo in 205 individuals with PP. At week 16, the percentage of patients achieving clear or nearly clear palms and soles with secukinumab 300 mg and 150 mg was higher compared with placebo (33.3%, 22.1%, and 1.5%, respectively, p < 0.001). The ppPASI score was significantly reduced with secukinumab 300 mg (54.5%) and 150 mg (35.3%) compared with placebo (4.0%, p < 0.001) [34]. Interestingly, a sub-analysis of a randomized double-blind, placebo-controlled treatment finding study showed that secukinumab improves PsO on the hands, feet, and nails when administered as early therapy [33].
A prospective clinical study was conducted specifically in patients with moderate-to-severe psoriasis of the scalp [35]. This study was a 24-week, double-blind, phase IIIb trial in which patients with extensive moderate-to-severe scalp psoriasis were randomized in a 1:1 ratio to secukinumab 300 mg or placebo. Results showed that secukinumab was effective and well tolerated in these patients, with the safety profile of secukinumab being consistent with previous studies. At week 12, the Psoriasis Scalp Severity Index (PSSI) 90 was significantly higher with secukinumab 300 mg than with placebo (secukinumab 300 mg 52.9% versus placebo 2.0%, p < 0.001). In addition, significantly more patients achieved complete remission of scalp psoriasis at week 12 on secukinumab 300 mg than on placebo.
There are few real-world long-term data on the effectiveness and safety of secukinumab in patients with psoriasis in difficult-to-treat areas. A retrospective analysis conducted in 151 patients with chronic plaque psoriasis showed improvement in plaques after 136 weeks of treatment with secukinumab 300 mg. After 8 weeks of treatment with secukinumab, plaques on the scalp, head, nails, suprapubic area, and penis had almost disappeared [40]. Similarly, a 2-year multicenter, observational study investigated the effectiveness of secukinumab in palmoplantar psoriasis [34] and showed that secukinumab was effective in the treatment of palmoplantar psoriasis also in the real-world setting, with a significant improvement in the mean PASI, reduced to 78.2% at week 16. The mean palmoplantar PASI (ppPASI) score also improved significantly, but more gradually, with a decrease of 55.0% and 79.3% after 16 and 104 weeks, respectively. About half of the patients completely healed after 40 weeks. Secukinumab was well tolerated, and no relevant treatment-related adverse events were reported [51]. A single-center, 104-week study evaluated the efficacy of secukinumab in moderate-to-severe chronic plaque psoriasis, including scalp and palmoplantar involvement [41]. The Physician Global Assessment (PGA), PASI75/90/100, and scalp and palmoplantar PGA were assessed. At week 16, the PASI75/PASI90/PASI100 was observed in 83.8/70.0/46.3% of patients, respectively. Scalp and palmoplantar PGA improved rapidly, with 98.7% and 95.5% achieving clear/almost clear skin at week 16, respectively. In this real-world study, secukinumab was shown to be effective in difficult-to-treat areas with a similar safety profile to clinical trials [41]. These results were confirmed in a study on 99 patients with psoriasis where receiving 300 mg of secukinumab was found to be save and efficacious, also in patients with difficult to treat manifestations, such as the scalp, over 4 years [52]. Secukinumab was shown to be safe and effective in real-world clinical practice in patients with PP and palmoplantar pustular psoriasis (PPPP) who did not respond to previous systemic or biologic treatments over a 24-month follow-up period [53]. Interestingly, statistically significant differences in ppIGA scores were observed at 12 months between therapy-naive patients and patients who had previously received biologics therapy. Secukinumab was found to be more effective in therapy-naive patients than in patients who had previously received biologic therapy [53]. In addition, the first real-world monocentric study comparing secukinumab and ixekizumab in the treatment of PP and erythrodermic psoriasis (EP) showed that patients treated with ixekizumab reached PASI 90, PASI < 3, and PASI 100 faster than those treated with secukinumab, with no statistically significant difference at 12-week follow-up. At 48 weeks, a statistically significant difference was observed between the two groups (100%, 100%, and 75% of patients treated with ixekizumab achieved PASI 90, PASI < 3, and PASI 100, respectively, versus 31%, 46%, and 23% of patients treated with secukinumab, p = 0.01). Secukinumab proved effective in the EP group at week-48 follow-up, as PASI 90 and PASI 100 were achieved in 82% and 54% of patients, respectively [54]. Moreover, a 48-week real-world retrospective study performed on 18 pediatric patients with generalized pustular psoriasis (GPP) receiving secukinumab as first-line treatment showed a significant decrease in the GPPPASI score as well as improvements in Children’s Dermatology Life Quality Index score [55].
Preventing the Development of Psoriasis Arthritis by Early Treatment of Psoriasis
Psoriatic arthritis (PsA), a chronic inflammatory disease, develops in around 14.0–22.7% of the individuals affected by PsO. Patients with psoriasis are at higher risk of developing PsA than healthy individuals or individuals with other diseases [56]. The progression from PsO to PsA occurs in a series of phases [57], with clinically evident disease emerging only at late stages. The transitional phase preceding PsA onset, known as prodromal PsA, is characterized by the spread of the disease from the skin to the joints. The prodromal phase of PsA is difficult to diagnose as characterized by non-specific symptoms, such as inflammatory joint lesions, joint pain, or fatigue [58]. As a result, PsA is often not diagnosed in a timely manner, resulting in treatment delays and missed prevention opportunities [59]. The transition phase from PsO to PsA offers the opportunity to identify individuals at increased risk of developing PsA and to implement early treatment and prevention strategies. The current literature suggests that the development of PsA might have its roots in the complex interplay between environmental factors, an individual's phenotype, and genotype. For example, severe psoriasis affecting the nails, scalp, and genitals is associated with the development of PsA in people with systemic conditions [60]. Patients with PsA have a higher incidence and prevalence of cardiovascular risk factors, such as hypertension, diabetes, hyperlipidemia, and obesity [61]. These known risk factors could be considered in current clinical practice to implement prevention strategies [45]; however, research on clinical indicators to identify individuals with psoriasis at higher risk of developing PsA remains limited. A systematic review and meta-analysis [45] attempted to profile PsO patients at higher risk of developing PsA and identified some potential predictors of PsA development. Skin and nail phenotypes of PsA development included PsO severity and nail pitting. Furthermore, other predictors were having arthralgia and higher categories of body mass index (BMI). This research, while limited by the heterogeneity of the included studies, suggests that these risk factors could support the identification of individuals at higher risk of developing PsA who could receive timely treatment, preventing the disease or worse disease outcome [62]. Of note, treatment of PsA with biologics before the onset of structural damage prevents impairment of physical function and permanent disability [63, 64]. Supporting this evidence, preliminary results on a limited number of individuals suggested that early treatment with biologics in patients with PsO carrying a short-term risk of developing PsA may revert the preclinical manifestations of PsA, such as arthralgia or musculoskeletal pain [65]. Notably, in recent years the number of studies investigating the real-world effectiveness of secukinumab in PsA has significantly increased. For example, one study reported that secukinumab was effective in reducing disease activity and was safe in both biologic-naive and non-naive PsA patients [66]. A prospective, multicenter study assessing real-life long-term secukinumab effectiveness and safety showed that after 24 months, biologic-naive patients had a lower PASI (p = 0.04), erythrocyte sedimentation rate and C-reactive protein (p = 0.03; p = 0.05), and joint count (p = 0.03) compared to biologic-multi-failure patients [42]. When comparing the effectiveness and safety of secukinumab in biologic-naive patients with those in which TNF inhibitors had failed, DAPSA and ASDAS showed that secukinumab was effective in PsA patients over a 24-month follow-up period [67]. Another study conducted in patients with axial spondyloarthritis showed that biologic-naive patients had better physical functioning and lower disease activity compared to the TNF inhibitor failure group [BASDAI 2.2 (1.0–3.8) vs 3.9 (2.7–5.0), ASDAS 1.3(1.0–2.2) vs 2.1(1.6–2.9)] at 24 months, with high retention rate [68]. An analysis of the Italian Lombardy Rheumatology Network (LOHREN) registry found a high 3-year retention rate with secukinumab for both PsA and axSpA [69]. A recent study in the US on patients with PsA described rapid improvements in disease management and quality of life upon secukinumab treatment [70]. Secukinumab also confirmed effectiveness and safety in PsA patients in a recent real-life Italian study conducted over 52 weeks [71]. This evidence was confirmed in other studies conducted in Italian settings [42, 72, 73].
The real-world evidence presented in these studies highlights the effectiveness and safety of secukinumab in the management of PsA and axSpA, with a good patient retention rate. The reduction in disease severity scores and good retention rate observed upon treatment with secukinumab emphasize its potential to provide substantial relief to these patients. These findings encourage a shift towards proactive and early intervention strategies, addressed not only to improving the quality of life of the patients but also aiming at preventing long-term disabilities and comorbidities, and potentially disease onset.
Benefits of Early Treatment with Secukinumab on the QoL of Individuals with PSO
The impact of psoriasis on patients’ health-related quality of life is considerable, as the disease negatively affects physical, emotional, psychological, and economic aspects of life. A survey of psoriasis patients conducted in the US found that the larger the body surface area, the greater the impact on quality of life [74]. Psoriasis patients report that PsO interferes with daily life activities, such as sleeping, washing, or dressing, and with work-related activities [75,76,77,78]. Patients frequently experience a pronounced sense of diminished self-esteem regarding their physical appearance, and they frequently contend with societal stigmatization [79]. This psychological condition triggers coping strategies, such as covering up their lesions or avoiding contact with others, which worsen patients' quality of life [74]. Finally, patients with psoriasis have a higher financial burden of direct and indirect costs, including the cost of treatments and loss of work productivity [5].
In a multicenter, retrospective real-world study of Italian psoriasis patients that lasted 84 weeks, secukinumab appeared to rapidly improve patients' quality of life as assessed by the Dermatology Life Quality Index score (DLQI). Specifically, a significant improvement in DLQI was observed after 4 weeks of treatment with secukinumab (p < 0.001 compared to baseline), which improved significantly at each follow-up visit. Interestingly, the data were comparable between patients who had never been treated with biologics and those who had been previously treated with biologics [80]. As further evidence, in a multicenter real-world study, secukinumab showed remarkable effects on patients' quality of life, even when used in combination therapy after the failure of secukinumab monotherapy [81].
Interestingly, a randomized, double-blind, placebo-controlled phase 2 study has shown that patients with moderate-to-severe plaque psoriasis treated early with secukinumab have a better quality of life compared with patients receiving placebo [82]. DLQI response was significantly higher with all secukinumab regimens compared with placebo at both 4 and 12 weeks, but the greatest changes were observed with the monthly and early regimens [82].
Benefits of Early Treatment with Secukinumab in Hard-to-Treat Patient Populations
Secukinumab is safe and effective in the real-life setting, also for patients in whom previous systemic treatments have failed or who have multiple comorbidities, such as older people. A study following patients > 65 years old with moderate-to-severe PsO treated with secukinumab over a 2-year period reported a mean PASI reduction of 85.1% at week 96, with a significant reduction from week 24 (from 11.4 ± 6.3 at baseline to 2.1 ± 1.7 at week 24, p < 0.001) [83]. In addition to older patients, biologics are proving to be a favorable therapeutic choice for pediatric patients as they have an excellent efficacy and safety profile compared to conventional systemic medications [84]. As previously mentioned [55], in a 48-week real-world retrospective study involving 18 pediatric patients diagnosed with GPP who received secukinumab as their initial treatment, a substantial reduction in the GPPPASI score and a concurrent enhancement in the Children's Dermatology Life Quality Index score were evidenced. Notably, at the end of the 48-week period, 88.9% of the patients attained a GPPASI score of 100, while every patient achieved a Children's Dermatology Life Quality Index score of 0 or 1 [55]. Moreover, real-world evidence has shown that secukinumab has more favorable outcomes in pediatric patients with GPP compared to acitretin [85]. These data highlight the effectiveness of secukinumab in all life stages of patients with PsO.
Findings from secukinumab clinical trials were confirmed in a more complicated patient population (e.g., polypharmacy, comorbidities, failure of conventional systemic treatment) in a 2-year, real-world, multicenter retrospective study. Results showed that PASI, BSA, and DLQI scores improved significantly from baseline to each follow-up visit and that no significant differences were observed between naive and biologic-naive or non-naive patients. Treatment was discontinued in 31 of 324 patients (9.5%), 1.8% of these because of adverse events [86]. A heterogeneous patient population with varying disease severity and comorbidities was enrolled in another real-world, multicenter, retrospective study that lasted 52 weeks. Secukinumab was effective and safe but also showed rapid clinical improvement, particularly in young patients, and in certain subgroups of patients, such as those with obesity and multidrug-resistant patients [87]. A multicenter, real-world observational study involving 15 Italian referral centers assessed the efficacy and safety of secukinumab in patients with PsO and a history of cancer, usually excluded from clinical trials of biologic treatments. After 48 weeks, 64.7% of patients scored PASI 90 and 38.2% scored PASI 100. Significant improvement was also observed in DLQI, itch, and pain visual analog scale (VAS) scores. Furthermore, the study suggests that secukinumab is safe in psoriatic patients with a history of cancer [88]. A European, multicenter, retrospective real-world study contributed to the characterization of secukinumab best responders. The study confirmed that secukinumab treatment was more effective in biologic-naive patients than in patients previously treated with biologics. The better response in biologic-naive patients was observed at weeks 24 and 52 [89].
Conclusions
Biologics therapy is a valuable option for the treatment of moderate-to-severe plaque psoriasis. Secukinumab has long-term clinical efficacy and safety in the treatment of patients with PsO, PsA, and axSpA. While the efficacy of early intervention has been explored and demonstrated in other chronic inflammatory diseases, studies on clinical outcomes of early treatment with secukinumab in individuals with psoriasis are limited. Real-world studies are a valuable resource of information to evaluate the effectiveness of this clinical approach in different groups of patients, with several degrees of disease severity and comorbidities. Real-world data have the advantage of including a broad patient population, often excluded from clinical trials and representative of real-world clinical practice. The analysis of real-world data showed the effectiveness of secukinumab, particularly in biologic-naive patients with a history of diseases. In these patients, early intervention with secukinumab proved to be a valuable treatment option. In addition, secukinumab has a good safety profile, which has been consistently observed in diverse patient cohorts characterized by different comorbidities, such as cancer, liver, and cardiovascular disease, as well as in pediatric and older patients. The cost-benefit ratio of secukinumab could also be better than that of other biologics, considering the sustained clinical response. In addition, secukinumab showed low immunogenicity (< 1%) in psoriasis patients for up to 5 years and patients with PsA exposed for up to 52 weeks [90]. A systematic review conducted to explore the immunogenicity of several biological agents across inflammatory diseases confirmed an overall rate for secukinumab of 0–1%, lower than the one reported for other biologics, such as infliximab and adalimumab, an IL-17 and tumor necrosis factor inhibitor, respectively [91]. Although limited, the data in the literature support effectiveness, safety, and utility as a treatment option for psoriasis of secukinumab also in biologic-naive patients, with improvements in clinical outcomes comparable to those reported for biologic-experience patients [22, 31]. Furthermore, secukinumab could also be an effective alternative when IL-23 inhibitors do not achieve the desired therapeutic outcomes (92).
Early intervention with secukinumab in the treatment of PsO can potentially improve the overall prognosis by reducing disease severity or altering the natural history of the disease towards more severe and complicated stages, leading to remission and improving the quality of life of these patients. The early intervention may also lead to a reduction of costs in treating this disease. For all these reasons, additional real-world studies exploring intervention and early intervention with secukinumab in PsO is of utmost importance.
Data Availability
Data sharing is not applicable to this article, as no datasets were generated or analyzed during the current study.
References
Bu J, Ding R, Zhou L, Chen X, Shen E. Epidemiology of psoriasis and comorbid diseases: a narrative review. Front Immunol. 2022;10:13.
Parisi R, Symmons DPM, Griffiths CEM, Ashcroft DM. Global epidemiology of psoriasis: a systematic review of incidence and prevalence. J Investig Dermatol. 2013;133(2):377–85.
de Oliveira MFSP, Rocha BO, Duarte GV. Psoriasis: classical and emerging comorbidities. An Bras Dermatol. 2015;90(1):9–20.
Noe MH, Shin DB, Wan MT, Gelfand JM. Objective measures of psoriasis severity predict mortality: a prospective population-based cohort study. J Investig Dermatol. 2018;138(1):228–30.
Bhosle MJ, Kulkarni A, Feldman SR, Balkrishnan R. Quality of life in patients with psoriasis. Health Qual Life Outcomes. 2006;4(1):35.
Griffiths CEM, Armstrong AW, Gudjonsson JE, Barker JNWN. Psoriasis. The Lancet. 2021;397(10281):1301–15.
Mosca M, Hong J, Hadeler E, Hakimi M, Liao W, Bhutani T. The role of IL-17 cytokines in psoriasis. Immunotargets Ther. 2021;10:409–18.
Xu S, Gao X, Deng J, Yang J, Pan F. Comparative efficacy and safety of biologics in moderate to severe plaque psoriasis: a multiple-treatments meta-analysis. J Deutschen Derma Gesell. 2021;19(1):47–56.
Menter A, Krueger GG, Paek SY, Kivelevitch D, Adamopoulos IE, Langley RG. Interleukin-17 and Interleukin-23: a narrative review of mechanisms of action in psoriasis and associated comorbidities. Dermatol Ther (Heidelb). 2021;11(2):385–400.
Gargiulo L, Ibba L, Malagoli P, Balato A, Bardazzi F, Burlando M, et al. Drug survival of IL-12/23, IL-17 and IL-23 inhibitors for moderate-to-severe plaque psoriasis: a retrospective multicenter real-world experience on 5932 treatment courses – IL PSO (Italian landscape psoriasis). Front Immunol. 2024;11:14.
Mastorino L, Dapavo P, Susca S, Cariti C, Siliquini N, Verrone A, et al. Drug survival and clinical effectiveness of secukinumab, ixekizumab, brodalumab, guselkumab, risankizumab, tildrakizumab for psoriasis treatment. J der Deutschen Dermatologischen Gesellschaft. 2024;22(1):34–42.
Thomas SE, Barenbrug L, Hannink G, Seyger MMB, de Jong EMGJ, van den Reek JMPA. Drug survival of IL-17 and IL-23 inhibitors for psoriasis: a systematic review and meta-analysis. Drugs. 2024;84(5):565–78.
Russo F, Galluzzo M, Stingeni L, Persechino S, Zichichi L, Conti A, et al. Long-term drug survival and effectiveness of secukinumab in patients with moderate to severe chronic plaque psoriasis: 42-month results from the SUPREME 2.0 study. Clin Cosmet Investig Dermatol. 2023;16:3561–74.
Dastoli S, Passante M, Loconsole F, Mortato E, Balato A, Piccolo V, et al. Long-term efficacy and safety of secukinumab in real life: a 240 weeks multicenter study from Southern Italy. J Dermatol Treat. 2023. https://doi.org/10.1080/09546634.2023.2200868.
Kolbinger F, Di Padova F, Deodhar A, Hawkes JE, Huppertz C, Kuiper T, et al. Secukinumab for the treatment of psoriasis, psoriatic arthritis, and axial spondyloarthritis: physical and pharmacological properties underlie the observed clinical efficacy and safety. Pharmacol Ther. 2022;229: 107925.
European Medicines Agency. Cosentyx, INN-secukinumab - European Medicines Agency - Product information [Internet]. [cited 2024 Feb 11]. Available from: https://www.ema.europa.eu/en/documents/product-information/cosentyx-epar-product-information_en.pdf
Augustin M, Reich K, Yamauchi P, Pinter A, Bagel J, Dahale S, et al. Secukinumab dosing every 2 weeks demonstrated superior efficacy compared with dosing every 4 weeks in patients with psoriasis weighing 90 kg or more: results of a randomized controlled trial*. Br J Dermatol. 2022;186(6):942–54.
Frieder J, Kivelevitch D, Menter A. Secukinumab: a review of the anti-IL-17A biologic for the treatment of psoriasis. Ther Adv Chronic Dis. 2018;9(1):5–21.
van de Kerkhof PCM, Griffiths CEM, Reich K, Leonardi CL, Blauvelt A, Tsai TF, et al. Secukinumab long-term safety experience: a pooled analysis of 10 phase II and III clinical studies in patients with moderate to severe plaque psoriasis. J Am Acad Dermatol. 2016;75(1):83-98.e4.
Papp KA, Griffiths CEM, Gordon K, Lebwohl M, Szapary PO, Wasfi Y, et al. Long-term safety of ustekinumab in patients with moderate-to-severe psoriasis: final results from 5 years of follow-up. Br J Dermatol. 2013;168(4):844–54.
Deodhar A, Mease PJ, McInnes IB, Baraliakos X, Reich K, Blauvelt A, et al. Long-term safety of secukinumab in patients with moderate-to-severe plaque psoriasis, psoriatic arthritis, and ankylosing spondylitis: integrated pooled clinical trial and post-marketing surveillance data. Arthritis Res Ther. 2019;21(1):111.
Blauvelt A, Chiricozzi A. The immunologic role of il-17 in psoriasis and psoriatic arthritis pathogenesis. Clin Rev Allergy Immunol. 2018;55(3):379–90.
Liang J, Zhang S, Li Q, Yu Y, Chen X, Zhang X. Review of secukinumab-induced adverse events of special interest and its potential pathogenesis. Dermatol Ther. 2022. https://doi.org/10.1111/dth.15599.
Eshwar V, Kamath A. Assessment of safety profile of secukinumab in real-world scenario using United States food and drug administration adverse event reporting system database. Sci Rep. 2024;14(1):1222.
Sun R, Bustamante M, Gurusamy VK, Lebwohl M, Gottlieb AB, Mease PJ, et al. Safety of secukinumab from 1 million patient-years of exposure: experience from post-marketing setting and clinical trials. Dermatol Ther (Heidelb). 2024;14(3):729–43.
Merola JF, McInnes IB, Deodhar AA, Dey AK, Adamstein NH, Quebe-Fehling E, et al. Effect of secukinumab on traditional cardiovascular risk factors and inflammatory biomarkers: post hoc analyses of pooled data across three indications. Rheumatol Ther. 2022;9(3):935–55.
von Stebut E, Reich K, Thaçi D, Koenig W, Pinter A, Körber A, et al. Impact of secukinumab on endothelial dysfunction and other cardiovascular disease parameters in psoriasis patients over 52 weeks. J Investig Dermatol. 2019;139(5):1054–62.
Girolomoni G, Griffiths CEM, Krueger J, Nestle FO, Nicolas JF, Prinz JC, et al. Early intervention in psoriasis and immune-mediated inflammatory diseases: a hypothesis paper. J Dermatol Treat. 2015;26(2):103–12.
Felix PAO, Sampaio AL, Silva BL, Viana ALP. Early intervention in psoriasis: Where do we go from here? Front Med (Lausanne). 2022;1:9.
Krueger JG, Wharton KA, Schlitt T, Suprun M, Torene RI, Jiang X, et al. IL-17A inhibition by secukinumab induces early clinical, histopathologic, and molecular resolution of psoriasis. J Allergy Clin Immunol. 2019;144(3):750–63.
Rich P, Sigurgeirsson B, Thaci D, Ortonne JP, Paul C, Schopf RE, et al. Secukinumab induction and maintenance therapy in moderate-to-severe plaque psoriasis: a randomized, double-blind, placebo-controlled, phase II regimen-finding study. Br J Dermatol. 2013;168(2):402–11.
Augustin M, Jullien D, Martin A, Peralta C. Real-world evidence of secukinumab in psoriasis treatment—a meta-analysis of 43 studies. J Eur Acad Dermatol Venereol. 2020;34(6):1174–85.
Paul C, Reich K, Gottlieb AB, Mrowietz U, Philipp S, Nakayama J, et al. Secukinumab improves hand, foot and nail lesions in moderate-to-severe plaque psoriasis: subanalysis of a randomized, double-blind, placebo-controlled, regimen-finding phase 2 trial. J Eur Acad Dermatol Venereol. 2014;28(12):1670–5.
Ohtsuki M, Morita A, Igarashi A, Imafuku S, Tada Y, Fujita H, et al. Secukinumab improves psoriasis symptoms in patients with inadequate response to cyclosporine A: a prospective study to evaluate direct switch. J Dermatol. 2017;44(10):1105–11.
Iversen L, Eidsmo L, Austad J, de Rie M, Osmancevic A, Skov L, et al. Secukinumab treatment in new-onset psoriasis: aiming to understand the potential for disease modification – rationale and design of the randomized, multicenter STEPI n study. J Eur Acad Dermatol Venereol. 2018;32(11):1930–9.
Iversen L, Conrad C, Eidsmo L, Costanzo A, Narbutt J, Pinter A, et al. Secukinumab demonstrates superiority over narrow-band ultraviolet B phototherapy in new-onset moderate to severe plaque psoriasis patients: Week 52 results from the STEPIn study. J Eur Acad Dermatol Venereol. 2023;37(5):1004–16.
Schäkel K, Reich K, Asadullah K, Pinter A, Jullien D, Weisenseel P, et al. Early disease intervention with guselkumab in psoriasis leads to a higher rate of stable complete skin clearance (‘clinical super response’): Week 28 results from the ongoing phase IIIb randomized, double-blind, parallel-group, GUIDE study. J Eur Acad Dermatol Venereol. 2023;37(10):2016–27.
Blauvelt A, Leonardi CL, Gooderham M, Papp KA, Philipp S, Wu JJ, et al. Efficacy and safety of continuous risankizumab therapy vs treatment withdrawal in patients with moderate to severe plaque psoriasis. JAMA Dermatol. 2020;156(6):649.
Strober B, Patil D, McLean RR, Moore-Clingenpeel M, Guo N, Levi E, et al. Utilization trends and impact of secukinumab treatment on clinical outcomes in biologic-naive patients with psoriasis in a US real-world setting. Dermatol Ther (Heidelb). 2022;12(6):1351–65.
Galluzzo M, D’Adamio S, Silvaggio D, Lombardo P, Bianchi L, Talamonti M. In which patients the best efficacy of secukinumab? Update of a real-life analysis after 136 weeks of treatment with secukinumab in moderate-to-severe plaque psoriasis. Expert Opin Biol Ther. 2020;20(2):173–82.
Rompoti N, Katsimbri P, Kokkalis G, Boumpas D, Ikonomidis I, Theodoropoulos K, et al. Real world data from the use of secukinumab in the treatment of moderate-to-severe psoriasis, including scalp and palmoplantar psoriasis: a 104-week clinical study. Dermatol Ther. 2019. https://doi.org/10.1111/dth.13006.
Ramonda R, Lorenzin M, Carriero A, Chimenti MS, Scarpa R, Marchesoni A, et al. Effectiveness and safety of secukinumab in 608 patients with psoriatic arthritis in real life: a 24-month prospective, multicentre study. RMD Open. 2021;7(1): e001519.
Melgosa Ramos FJ, Mateu Puchades A, Guillén Climent S, Galarreta Pascual M, Saéz Belló M, Martínez Ferrer MA, et al. Long-term secukinumab efficacy and safety in bio-naïve patients with moderate-to-severe cutaneous psoriasis: a real-world retrospective noninterventional multicentric experience (128 patients). JEADV Clin Pract. 2023;2(3):576–82.
Gooderham M, Papp KA, Lynde C, Delorme I, Beecker J, Albrecht L, et al. Sustained effectiveness of secukinumab across different body regions in patients with moderate-to-severe plaque psoriasis from the PURE registry. Dermatol Ther (Heidelb). 2023;13(2):535–53.
Papp KA, Gooderham M, Lynde C, Brassard D, Al-Mohammedi F, Prajapati VH, et al. Effectiveness and safety of secukinumab updosing in patients with moderate to severe plaque psoriasis: data from the PURE registry. Arch Dermatol Res. 2024;316(7):362.
Egeberg A, See K, Garrelts A, Burge R. Epidemiology of psoriasis in hard-to-treat body locations: data from the Danish skin cohort. BMC Dermatol. 2020;20(1):3.
Raharja A, Mahil SK, Barker JN. Psoriasis: a brief overview. Clin Med. 2021;21(3):170–3.
Mastorino L, Burzi L, Frigatti G, Fazio A, Celoria V, Macagno N, et al. Clinical effectiveness of IL-17 and IL-23 inhibitors on difficult-to-treat psoriasis areas (scalp, genital, and palmoplantar sites): a retrospective, observational, single-center, real-life study. Expert Opin Biol Ther. 2023;23(9):929–36.
Mrowietz U, Leonardi CL, Girolomoni G, Toth D, Morita A, Balki SA, et al. Secukinumab retreatment-as-needed versus fixed-interval maintenance regimen for moderate to severe plaque psoriasis: a randomized, double-blind, noninferiority trial (SCULPTURE). J Am Acad Dermatol. 2015;73(1):27–36 (e1).
Merola JF, Qureshi A, Husni ME. Underdiagnosed and undertreated psoriasis: nuances of treating psoriasis affecting the scalp, face, intertriginous areas, genitals, hands, feet, and nails. Dermatol Ther. 2018. https://doi.org/10.1111/dth.12589.
Galluzzo M, Talamonti M, Atzori L, Bardazzi F, Campanati A, Di Cesare A, et al. Secukinumab for the treatment of palmoplantar psoriasis: a 2-year, multicenter, real-life observational study. Expert Opin Biol Ther. 2022;22(4):547–54.
Kyrmanidou E, Kemanetzi C, Stavros C, Trakatelli MG, Patsatsi A, Madia X, et al. A real-life 208 week single-centred, register-based retrospective study assessing secukinumab survival and long-term efficacy and safety among Greek patients with moderate to severe plaque psoriasis, including difficult-to-treat manifestations such as genitals and scalp. Dermatol Pract Concept. 2024;14(2): e2024119.
Krueger J, Langley R, Nigen S. 35098 Secukinumab versus guselkumab in the treatment of ustekinumab-resistant psoriatic plaques: 16-week randomized, open-label, multicenter ARROW study. J Am Acad Dermatol. 2022;87(3): AB108.
Avallone G, Cariti C, Dapavo P, Ortoncelli M, Conforto L, Mastorino L, et al. Real-life comparison between secukinumab and ixekizumab in the treatment of pustular and erythrodermic psoriasis. J Eur Acad Dermatol Venereol. 2022;36(7):e574–e576.
Ruan SF, Zhang LL, Liu Z, Lin TT, Wang HQ, Xu QY, et al. Real-world data on the clinical use of secukinumab in pediatric generalized pustular psoriasis: a 48-week retrospective study. J Am Acad Dermatol. 2023;88(1):243–6.
Hioki T, Komine M, Ohtsuki M. Diagnosis and intervention in early psoriatic arthritis. J Clin Med. 2022;11(7):2051.
Scher JU, Ogdie A, Merola JF, Ritchlin C. Preventing psoriatic arthritis: focusing on patients with psoriasis at increased risk of transition. Nat Rev Rheumatol. 2019;15(3):153–66.
McArdle A, Pennington S, FitzGerald O. Clinical features of psoriatic arthritis: a comprehensive review of unmet clinical needs. Clin Rev Allergy Immunol. 2018;55(3):271–94.
Haroon M, Gallagher P, FitzGerald O. Diagnostic delay of more than 6 months contributes to poor radiographic and functional outcome in psoriatic arthritis. Ann Rheum Dis. 2015;74(6):1045–50.
Paek SY, Thompson JM, Qureshi AA, Merola JF, Husni ME. Comprehensive assessment of the psoriasis patient (CAPP): a report from the GRAPPA 2015 annual meeting. J Rheumatol. 2016;43(5):961–4.
Radner H, Lesperance T, Accortt NA, Solomon DH. Incidence and prevalence of cardiovascular risk factors among patients with rheumatoid arthritis, psoriasis, or psoriatic arthritis. Arthritis Care Res (Hoboken). 2017;69(10):1510–8.
Zabotti A, De Lucia O, Sakellariou G, Batticciotto A, Cincinelli G, Giovannini I, et al. Predictors, risk factors, and incidence rates of psoriatic arthritis development in psoriasis patients: a systematic literature review and meta-analysis. Rheumatol Ther. 2021;8(4):1519–34.
Coates LC, Moverley AR, McParland L, Brown S, Navarro-Coy N, O’Dwyer JL, et al. Effect of tight control of inflammation in early psoriatic arthritis (TICOPA): a UK multicentre, open-label, randomised controlled trial. The Lancet. 2015;386(10012):2489–98.
Kamata M, Tada Y. Efficacy and safety of biologics for psoriasis and psoriatic arthritis and their impact on comorbidities: a literature review. Int J Mol Sci. 2020;21(5):1690.
Zabotti A, Giovannini I, McGonagle D, De Vita S, Stinco G, Errichetti E. Arthritis interception in patients with psoriasis treated with guselkumab. Dermatol Ther (Heidelb). 2022;12(1):5–8.
Letarouilly JG, Sellam J, Richette P, Dieudé P, Claudepierre P, Richard CM, et al. AB0760 drug survival and efficacy of ustekinumab and secukinumab in psoriatic arthritis: a real-world multicentric cohort of 186 Patients. In: Abstracts accepted for Publication. BMJ Publishing Group Ltd and European League Against Rheumatism; 2019. pp. 1847.2–1848.
Lorenzin M, Carletto A, Foti R, Chimenti MS, Semeraro A, Costa L, et al. FRI0284 Effectiveness and safety of secukinumab in naïve or TNF-inhibitors failure psoriatic arthritis patients in real life: a 24-months prospective multicenter study. Ann Rheum Dis. 2020;79(Suppl 1):730.1-730.
Marzo-Ortega H, Juanola X, Okano T, Schymura Y, Bradley A, Gerwien J, et al. POS0926 Normalisation of high sensitivity CRP versus clinical response to ixekizumab at week 16 in patients with radiographic& non-radiographic axial spondyloaarthritis: results from the coast studies. Ann Rheum Dis. 2021;80(Suppl 1):725–6.
Favalli EG, Marchesoni A, Balduzzi S, Montecucco C, Lomater C, Crepaldi G, et al. FRI0273 Effectiveness and retention rate of secukinumab for psoriatic arthritis and axial spondyloarthritis: real-life data from the Italian Lohren Registry. Ann Rheum Dis. 2020;79(Suppl 1):722.1-723.
Kivitz AJ, Kremer JM, Legerton CW, Pricop L, Singhal A. Efficacy and safety of secukinumab in US patients with psoriatic arthritis: a subgroup analysis of the phase 3 FUTURE studies. Rheumatol Ther. 2024;11(3):675–89.
Molica Colella F, Zizzo G, Parrino V, Filosa MT, Cavaliere R, Fazio F, et al. Effectiveness and safety of secukinumab in ankylosing spondylitis and psoriatic arthritis: a 52-week real-life study in an Italian cohort. Adv Rheumatol. 2023;63(1):15.
Gentileschi S, Rigante D, Sota J, Lopalco G, Giannotta MG, Emmi G, et al. Long-term effectiveness of secukinumab in patients with axial spondyloarthritis. Mediators Inflamm. 2020;31(2020):1–5.
Chimenti MS, Fonti GL, Conigliaro P, Sunzini F, Scrivo R, Navarini L, et al. One-year effectiveness, retention rate, and safety of secukinumab in ankylosing spondylitis and psoriatic arthritis: a real-life multicenter study. Expert Opin Biol Ther. 2020;20(7):813–21.
Gelfand JM, Feldman SR, Stern RS, Thomas J, Rolstad T, Margolis DJ. Determinants of quality of life in patients with psoriasis: a study from the US population. J Am Acad Dermatol. 2004;51(5):704–8.
Finlay AY, Coles EC. The effect of severe psoriasis on the quality of life of 369 patients. Br J Dermatol. 2006;132(2):236–44.
Zagni E, Frassi M, Mariano GP, Fusaro E, Lomater C, Del Medico P, et al. A real-world economic analysis of biologic therapies for psoriatic arthritis in Italy: results of the CHRONOS observational longitudinal study. BMC Health Serv Res. 2022;22(1):1537.
Mantovani L, Medaglia M, Piacentini P, Tricca M, Vena GA, Vozza A, et al. Burden of moderate-to-severe plaque psoriasis and new therapeutic approaches (secukinumab): an Italian perspective. Dermatol Ther (Heidelb). 2016;6(2):151–67.
Colombo D, Bianchi L, Fabbrocini G, Corrao S, Offidani A, Stingeni L, et al. Real-world evidence of biologic treatments in moderate–severe psoriasis in Italy: results of the CANOVA (effectiveness of biologic treatments for plaque psoriasis in Italy: an observational longitudinal study of real-life clinical practice) study. Dermatol Ther. 2022. https://doi.org/10.1111/dth.15166.
Fortune DG, Richards HL, Griffiths CEM. Psychologic factors in psoriasis: consequences, mechanisms, and interventions. Dermatol Clin. 2005;23(4):681–94.
Megna M, Di Costanzo L, Argenziano G, Balato A, Colasanti P, Cusano F, et al. Effectiveness and safety of secukinumab in Italian patients with psoriasis: an 84 week, multicenter, retrospective real-world study. Expert Opin Biol Ther. 2019;19(8):855–61.
Damiani G, Odorici G, Pacifico A, Morrone A, Conic RRZ, Davidson T, et al. Secukinumab loss of efficacy is perfectly counteracted by the introduction of combination therapy (rescue therapy): data from a multicenter real-life study in a cohort of italian psoriatic patients that avoided secukinumab switching. Pharmaceuticals. 2022;15(1):95.
Augustin M, Abeysinghe S, Mallya U, Qureshi A, Roskell N, McBride D, et al. Secukinumab treatment of plaque psoriasis shows early improvement in DLQI response—results of a phase II regimen-finding trial. J Eur Acad Dermatol Venereol. 2016;30(4):645–9.
Megna M, Camela E, Cinelli E, Fabbrocini G. Real-life efficacy and safety of secukinumab in elderly patients with psoriasis over a 2-year period. Clin Exp Dermatol. 2020;45(7):848–52.
Megna M, Camela E, Battista T, Genco L, Martora F, Noto M, et al. Efficacy and safety of biologics and small molecules for psoriasis in pediatric and geriatric populations. Part I: focus on pediatric patients. Expert Opin Drug Saf. 2023;22(1):25–41.
Miao C, Chen Y, Wang Z, Xiang X, Liu Y, Xu Z. Real-world data on the use of secukinumab and acitretin in pediatric generalized pustular psoriasis. J Dermatol. 2023;50(2):258–61.
Di M.M.L. ACG, and CABP. Secukinumab in real life: a 2-year multicenter retrospective study in Campania region. i. Vol. 324. 8–9 p.
Galluzzo M, Talamonti M, De Simone C, D’Adamio S, Moretta G, Tambone S, et al. Secukinumab in moderate-to-severe plaque psoriasis: a multi-center, retrospective, real-life study up to 52 weeks observation. Expert Opin Biol Ther. 2018;18(7):727–35.
Pellegrini C, Esposito M, Rossi E, Gisondi P, Piaserico S, Dapavo P, et al. Secukinumab in patients with psoriasis and a personal history of malignancy: a multicenter real-life observational study. Dermatol Ther (Heidelb). 2022;12(11):2613–26.
Chiricozzi A, Balato A, Conrad C, Conti A, Dapavo P, Ferreira P, et al. Secukinumab demonstrates improvements in absolute and relative psoriasis area severity indices in moderate-to-severe plaque psoriasis: results from a European, multicentric, retrospective, real-world study. J Dermatol Treat. 2020;31(5):476–83.
Deodhar A, Gladman DD, McInnes IB, Spindeldreher S, Martin R, Pricop L, et al. Secukinumab immunogenicity over 52 weeks in patients with psoriatic arthritis and ankylosing spondylitis. J Rheumatol. 2020;47(4):539–47.
Strand V, Balsa A, Al-Saleh J, Barile-Fabris L, Horiuchi T, Takeuchi T, et al. Immunogenicity of biologics in chronic inflammatory diseases: a systematic review. BioDrugs. 2017;31(4):299–316.
Mastorino L, Roccuzzo G, Dapavo P, Siliquini N, Avallone G, Rubatto M, et al. Switching from IL23 inhibitors to IL17 inhibitors: a safe and effective practice? Dermatol Ther. 2022. https://doi.org/10.1111/dth.15697.
Medical Writing Assistance
Medical writing support in the preparation of this article was provided by Edra S.p.A., with an unconditioned contribution by Novartis.
Funding
This project was unconditionally funded by Novartis. The funder was not involved in the collection, analysis, interpretation of data, or the writing of this article.
Author information
Authors and Affiliations
Contributions
Paolo Amerio, Laura Atzori, Anna Balato, Federico Bardazzi, Luca Bianchi, Angelo Cattaneo, Andrea Chiricozzi, Maurizio Congedo, Antonio Costanzo, Paolo Dapavo, Maria Concetta Fargnoli, Claudia Giofrè, Paolo Gisondi, Claudio Guarneri, Serena Lembo, Francesco Loconsole, Piergiorgio Malagoli, Giampiero Mazzocchetti, Santo Raffaele Mercuri, Pietro Morrone, Anna Maria Offidani, Giovanni Palazzo, Aurora Parodi, Giovanni Pellacani, Stefano Piaserico, Concetta Potenza, Francesca Prignano, Marco Romanelli, Paola Savoia, Luca Stingeni, Massimo Travaglini, Emanuele Trovato, Marina Venturini, Leonardo Zichichiparticipated in the study outline and realization, critically revised the content of the manuscript and agreed to submit the manuscript for publication.
Corresponding author
Ethics declarations
Conflict of Interest
Paolo Amerio declares the following conflicts of interest: Novartis, Sanofi, Jannsen, Eli Lilly, Galderma. Laura Atzori has been consultant, PI, speaker for Abbvie, Novartis, Janssen, UCB Pharma, Sanofi Genzyme, Lilly, Pfizer, Almirall, BMS. Anna Balato has served on Scientific Boards and/or has received fees for Scientific Consultations from: Abbvie, Amgen, Boehringer Ingelheim, Janssen, Eli-Lilly, Novartis, UCB. Luca Bianchi has been consultant, PI, speaker for Abbvie, Novartis, Janssen, UCB Pharma, Sanofi Genzyme, Lilly, Pfizer, Almirall, Sun Pharma, BMS. Andrea Chiricozzi has served as advisory board member and consultant and has received fees and speaker's honoraria or has participated in clinical trials for AbbVie, Almirall, Bristol Myers Squibb, Leo Pharma, Lilly, Janssen, Novartis, Pfizer and Sanofi Genzyme. Antonio Costanzo has been principal investigator in clinical trials sponsored by and/or and has received personal fees for participation in advisory board from Abbvie, Almirall, Amgen, Boehringer, BMS, Leo Pharma, Lilly, Novartis, Pfizer, UCB and Sanofi, outside the submitted work. Maria Concetta Fargnoli has served on advisory boards, received honoraria for lectures and/or research grants from AMGEN, Almirall, Abbvie, Boehringer-Ingelheim, BMS, Galderma, Kyowa Kyrin, Leo Pharma, Pierre Fabre, UCB, Lilly, Pfizer, Janssen, MSD, Novartis, Sanofi-Regeneron, Sunpharma. Claudia Giofrè has served as advisory board member or has received fees and speaker or has participated in clinical trials for Amgen, Novartis, Janssen, Leo Pharma, Almirall, Abbvie, UCB, Lilly. Paolo Gisondi declares the following conflicts of interest: Amgen, Almirall Abbvie Eli Lilly Novartis Janssen UCB Pierre Fabre Pfizer. Claudio Guarneri declares the following conflicts of interest: Pfizer, Abbvie, Janssen, Novartis, Merck-Serono, Eli-Lilly, Celgene, Leo Pharma, Leo Pharma Denmark, Almirall, Amgen, Sanofi-Aventis, Boehringer-Ingelheim, Bristol Myers Squibb, UCB Pharma. Serena Lembo declares the following conflicts of interest: Pfizer, Abbvie, Janssen, Novartis, Eli-Lilly, Leo Pharma, Almirall, Sanofi-Aventis, UCB Pharma. Santo Raffaele Mercuri SRM has been principal investigator in clinical trials sponsored by and/or has received personal fees for participation in advisory board from Abbvie, Almirall, Amgen, Leopharma, Lilly, Jansenn, Novartis, Sanofi and Ucb, outside the submitted work. Pietro Morrone has served as advisory board member or has received fees and speaker for AbbVie, Almirall,Novartis, Sanofi Genzyme, Lilly, Leo Pharma. Giovanni Palazzo declares the following conflicts of interest: Novartis, Abbvie, Leopharma, Lilly, Pfizer, Janssen. Aurora Parodi declares the following conflicts of interest: Almirall, Abbvia, Amgen, Novartis, Pfizer, Lilly, LEO pharma, Euroimmun, Argx, Menarini, Boehringer. Giovanni Pellacani received institutional grants and/or honoraria for Advisory boards: Abbvie, Galderma, Leo-pharma, Lilly, Pfizer, Novartis, Sanofi, UCB. Stefano Piaserico has been a consultant and/or speaker for Abbvie, Almirall, Amgen, Janssen, LEO Pharma, Eli Lilly, Merck Sharp & Dohme, Novartis, Pfizer, Sandoz, andUCB. Francesca Prignano served as consultant, presenter and advisory board member for Abbvie, Novartis, Eli-Lilly, Jannsen-Cilag, Bohringer- Ingelheim, Almirall, Leo-Pharma, UCB, Bristol-Meyers-Squibb. Marco Romanelli: Abbvie, Lilly, Novartis, URGO, ConvaTec. Paola Savoia has served as advisory board member or has received fees and speaker's honoraria or has participated in clinical trials for AbbVie, Almirall, Bristol Myers Squibb, Ganassini, Kyowa Kirin, Janssen, Novartis, Sanofi and Sunpharma. Luca Stingeni has been principal investigator in clinical trials sponsored by and/or and has received personal fees for participation in advisory board from Abbvie, Leo Pharma, Lilly, Novartis, Pfizer, and Sanofi, outside the submitted work. Emanuele Trovato: Speaker for Abbvie, Novartis, Janssen, UCB Pharma, Eli-Lilly, Almirall, Leo Pharma. Marina Venturini has served as advisory board member and consultant and has received fees and speaker's honoraria or has participated in clinical trials for AbbVie, Almirall, Bristol Myers Squibb, Boehringer-Ingelheim, Eli Lilly, Galderma, Janssen, Leo Pharma, Novartis, Pierre Fabre, UCB Pharma. Leonardo Zichichi has been consultant, and speaker for Abbvie, Novartis, Janssen, Sanofi Genzyme, Lilly, Almirall, Sun Pharma.
Ethical Approval
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Malagoli, P., Dapavo, P., Amerio, P. et al. Secukinumab in the Treatment of Psoriasis: A Narrative Review on Early Treatment and Real-World Evidence. Dermatol Ther (Heidelb) (2024). https://doi.org/10.1007/s13555-024-01255-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13555-024-01255-4