Abstract
Introduction
Several clinical trials have established the efficacy and safety of dupilumab for treating atopic dermatitis (AD). However, literature remains scarce in reporting the long-term effectiveness, safety, and drug survival of dupilumab in real-world settings. This study aimed to describe the latter outcomes of dupilumab in patients with AD.
Methods
This Portuguese, multicentric, observational, retrospective study included consecutive adult patients with AD who initiated dupilumab between January 2019 and September 2023, with a follow-up period up to 30 months. Drug discontinuation and adverse effects data were used to estimate drug survival. Clinical assessments included the Eczema Area and Severity Index (EASI), pruritus numerical rating scale (NRS), and Dermatology Life Quality Index (DLQI).
Results
A total of 312 patients were included in the study, with 56.4% being male (median age of 30 years, range 18–83). The 30-month drug survival rate was 82.0%. During the study period, 12.5% of the sample (n = 39 patients) discontinued treatment: 7.3% due to treatment failure, 2.9% due to safety concerns, 1.3% due to complete disease control, 0.6% due to pregnancy, and 0.3% due to lack of compliance. Adverse events not leading to drug discontinuation were noted in 25.6% of the sample (n = 80). Conjunctivitis was the most frequently reported adverse event (17%), followed by facial erythema (9%). At 30 months, the mean EASI decreased significantly from 27.30 ± 11.89 at baseline to 2.92 ± 3.96 (p < 0.001), reflecting an overall improvement of 89.3%. Similarly, pruritus NRS decreased from 7.36 ± 1.90 at baseline to 1.74 ± 2.16 at month 30 (p < 0.001), improving by 76.4%, and mean DLQI changed from 18.0 ± 7.09 at baseline to 2.67 ± 3.95 at month 30 (p < 0.001), decreasing by 85.2%.
Conclusions
This study increases our current understanding of dupilumab in real-world settings, demonstrating its long-term effectiveness and safety in treating AD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The efficacy and safety of dupilumab for treating atopic dermatitis has been assessed in clinical trials, but literature remains scarce in reporting its long-term performance in real-world scenarios. |
We conducted a multicentric study aiming to evaluate the long-term drug survival, effectiveness, and safety of dupilumab in patients with atopic dermatitis in a real-life setting. |
In our study, mean Eczema Area and Severity Index (EASI) showed sustained improvement over the 30-month follow-up period, decreasing by 89%. EASI-75 and EASI-90 were achieved in 88 and 69%, respectively, whereas pruritus Numerical Rating Scale (NRS) and Dermatology Life Quality Index (DLQI) improved by 76% and 85%, respectively. |
Overall, the 30-month drug survival rate was 82%, with 12.5% of patients discontinuing treatment due to failure and 2.9% due to safety concerns. |
Dupilumab demonstrated to be an effective and safe option for treating atopic dermatitis in a real-world clinical setting. |
Introduction
Atopic dermatitis (AD) is a chronic, inflammatory skin disease that significantly affects the quality of life of patients and caregivers [1]. While the complete mechanisms leading to AD are not completely understood, its pathogenesis includes interactions between genetic predisposition and environmental triggers, resulting in immune dysregulation and skin barrier dysfunction [2]. Immunologically, AD is characterized by a predominance of T-helper 2 (Th2) cell-driven inflammation, with interleukin (IL)-4 and IL-13, among others, playing a key role in driving the inflammatory cascade [2]. Clinically, AD is characterized by persistent itching and recurrent eczematous lesions of varying severity [3]. Associated pruritus is often severe enough to disrupt patients’ sleep and self-esteem, chronically impacting daily activities and leading to anxiety and depression [3]. Although AD can manifest at any point in life, its incidence peaks in early infancy, making it a frequent life-long disease requiring targeted approaches.
The management of AD has evolved significantly in recent decades. While traditional immunosuppressive drugs may be effective in controlling the disease in some patients, concerns about their safety have limited their use [3]. The advent of new targeted biological therapies for AD has heralded a new era in the field. Dupilumab, the first biological agent approved for AD, is a monoclonal antibody that targets the IL-4 receptor subunit α (IL-4Rα), blocking the signaling of IL-4 and IL-13 and, consequently, the Th2 pathway [4, 5]. Clinical trials have clearly demonstrated the efficacy and safety of dupilumab for treating AD [6]. However, these trials were performed under ideal conditions, which may not be representative of those encountered in daily clinical practice, where reasons for drug discontinuation and adverse events may vary significantly. Thus, real-world studies demonstrating the effectiveness and safety of dupilumab in diverse, heterogeneous populations commonly encountered in clinical practice are of utmost importance.
In a previous study, we demonstrated the effectiveness of dupilumab in a real-world setting at 48 weeks of continuous treatment [7]. In this study, we present extended data on effectiveness and evaluate the drug survival of dupilumab in a nationwide collaborative setting.
Methods
This is a multicentric, observational, retrospective cohort study involving patients with AD from 11 Portuguese centers. The present study was conducted in accordance with the Declaration of Helsinki initially published in 1964 on Ethical Principles for Medical Research Involving Human Subjects and after approval by the local ethical committees. Patients’ consent was exempted due to the retrospective nature of the study: the study protocol did not deviate from standard clinical practice, and data collection and handling complied with applicable laws, regulations, and guidance regarding patient protection, including patient privacy.
Sampling and Study Design
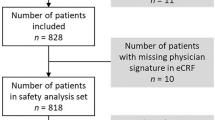
Consecutive adult (≥ 18 years old) patients diagnosed with AD who initiated treatment with dupilumab between January 2019 and September 2023, with a follow-up period of at least 3 months up to 30 months after treatment initiation, were included. Both naïve patients and those who experienced failure/adverse events with previous systemic therapies leading to discontinuation were considered. Dupilumab treatment adhered to current clinical care practice recommendations, with dosing adjustments considered in cases of well-controlled disease or severe adverse events. Patients lacking follow-up information regarding drug maintenance, discontinuation, or adverse events were excluded. No other strict exclusion criteria were applied to ensure the sample was representative of a real, heterogeneous clinical setting.
Data Collection
At baseline (the visit where dupilumab was initiated), we collected data on demographics, body mass index (BMI, weight in kilograms divided by height in square meters), family history, comorbidities (present or past history), time of onset of AD, history of previous systemic treatments, and disease activity. We assessed the further follow-up visits for data on safety, discontinuation rate, and causes, recording all safety events that occurred during the study period, as well as the need for concomitant therapy or dosing adjustments. Whenever available, data on disease severity and treatment response were assessed using the absolute Eczema Area and Severity Index (EASI), Physician Global Assessment (PGA), pruritus numerical rating scale (NRS), and Dermatology Life Quality Index (DLQI). Results were analyzed at baseline, month 3, month 6, month 12, month 18, month 24, and month 30 of follow-up. Effectiveness was also assessed by evaluating the proportion of patients achieving EASI < 7 and a 75% improvement (EASI-75 response), 90% improvement (EASI-90 response), or complete clearance (EASI-100 response) in their EASI score compared with baseline.
Statistical Analysis
Descriptive analysis is presented for all variables. Continuous variables are presented as mean ± standard deviation or median (interquartile range and/or range), while categorical variables are expressed as proportions.
Drug survival was analyzed using the Kaplan–Meier method. Any discontinuation of dupilumab was considered an event. Patients were censored if they were still using dupilumab at the end of follow-up or if follow-up was lost. Based on previous literature and clinical plausibility, the following variables were considered as potential predictors of drug survival: sex, age, BMI, personal history of atopic disease (allergic rhinitis, asthma, food allergy, allergic conjunctivitis, or eosinophilic esophagitis), previous treatment with a JAK inhibitor, AD duration, baseline EASI, and baseline pruritus NRS. To assess the association between these variables and drug survival, a univariate Cox regression analysis was performed for each variable separately. Effectiveness was assessed by comparing baseline and follow-up EASI, pruritus NRS, and DLQI, whenever available. Independent t-test and Mann–Whitney test were used to compare variables with normal and skewed distributions, respectively.
Statistical analysis was performed using the IBM Statistical Package for the Social Sciences software, version 24 (IBM Corporation), with a p value of < 0.05 considered to be statistically significant.
Results
A total of 312 patients were included in the study, comprising 56.4% males (n = 176) that were followed for a mean period of 18.2 ± 9.8 months after starting treatment with dupilumab. Table 1 displays the baseline characteristics of the sample.
Drug Survival
During the study period, 12.5% of the patients (n = 39 patients) discontinued dupilumab. Seven percent (n = 23) discontinued due to treatment failure. Safety issues led to drug discontinuation in 2.9% (n = 9) of patients, including active tuberculosis (n = 1), arthritis/arthralgia (n = 2), conjunctivitis (n = 3), and facial erythema (n = 1). In 1.3% (n = 4) of patients, dupilumab was discontinued due to complete disease control, and in 0.6% (n = 2) the drug was interrupted due to pregnancy. Lack of compliance led to drug discontinuation in one patient (0.3%). The drug survival curve is depicted in Fig. 1, showing that the cumulative proportion of patients remaining under treatment at 30 months was 82.0%. Potential predictors of dupilumab drug survival were studied using univariate Cox regression. Among the included potential predictors (sex, age, BMI, history of atopy, previous treatment with JAK inhibitors, disease duration, baseline EASI, baseline pruritus NRS), no associations were found (Table S1).
Effectiveness
At 30 months, the mean EASI decreased significantly from 27.30 ± 11.89 at baseline to 2.92 ± 3.96 (p < 0.001), reflecting an overall improvement of 89.3% (Fig. 2).
At a 30-month follow-up, EASI-75 was achieved in 88.4%, EASI-90 in 68.6%, and EASI-100 in 29.1% (Fig. 3). In addition, 88.4% of patients reached a EASI < 7 (Fig. 3).
Mean pruritus NRS decreased from 7.36 ± 1.90 at baseline to 1.74 ± 2.16 at month 30 (p < 0.001), decreasing by 76.4%. At 30 months, 65% of patients achieved a pruritus NRS score of 0/1, and 86% achieved an improvement of 4 or greater in their pruritus NRS score. Figure 4 illustrates the decrease in pruritus NRS throughout the follow-up visits.
Mean DLQI decreased from 18.0 ± 7.09 at baseline to 2.67 ± 3.95 at month 30 (p < 0.001), decreasing by 85.2%. At 30 months, 52% of patients achieved DLQI 0/1 and 96% achieved an improvement of 4 or greater in their score. Figure 5 illustrates the decrease in pruritus NRS throughout the follow-up visits.
Considering the subsample of treatment failures (n = 23), the mean EASI varied from 23.87 ± 6.44 at baseline to 16.58 ± 8.55 at the last follow-up evaluation (an improvement of 31%), the mean pruritus NRS varied from 8.73 ± 1.10 to 7.18 ± 2.60 (an improvement of 18%), and the mean DLQI varied from 18.17 ± 7.06 to 12.8 ± 7.64 (an improvement of 30%).
When analyzing the subsample of patients previously treated with a JAK inhibitor (n = 25), we verified that dupilumab subsequently failed in three cases. In the remaining ones (n = 22), the mean EASI varied from 27.28 ± 8.86 at baseline to 5.14 ± 5.61 at the last follow-up evaluation (an improvement of 81%), the mean pruritus NRS varied from 7.17 ± 1.82 to 2.56 ± 1.95 (an improvement of 64%), and the mean DLQI varied from 19.00 ± 8.90 to 5.81 ± 4.81 (an improvement of 69%).
Dupilumab dosing intervals were shortened in 3.8% of patients (n = 12) and prolonged in 13.1% (n = 41). Adjuvant treatment was needed in 15.4% of patients (n = 48), including cyclosporine A (9.3%, n = 29), systemic steroids (3.2%, n = 10), methotrexate (2.2%, n = 7), and phototherapy (0.6%, n = 2).
Safety
Adverse events not leading to drug discontinuation were noted in 25.6% (n = 80) of the cohort, but none of them required hospitalization. Conjunctivitis was the most frequently reported adverse event (16.7%, n = 52), followed by facial erythema (9.3%, n = 29), eosinophilia (2.6%, n = 8), herpes infection (1.6%, n = 5), nonherpetic infections (1.6%, n = 5), and injection site reactions (1.0%, n = 3). Herpetic eczema (0.6%, n = 2), alopecia areata (0.6%, n = 2), arthritis (0.6%, n = 2), and psoriasis-like eruptions (0.6%, n = 2) were among the least noted side effects. One patient completed the full pregnancy under dupilumab with no reported complications.
Discussion
This observational, real-world study demonstrates the sustained effectiveness and safety of dupilumab in treating AD within a Portuguese population up to 30 months of follow-up.
In our study, mean EASI showed sustained improvement over the 30-month follow-up period, decreasing by 89%. EASI-75 and EASI-90 were achieved in 88% and 69%, respectively, and these results corroborate the findings of two previous long-term studies: Miniotti et al. [8] report results at 36 months (EASI-75 and EASI-90 of 92% and 77%, respectively) and Beck et al. [9] report 4-year results, with EASI decreasing by 91% from baseline and pruritus NRS decreasing by 69%. Importantly, subjective measurements also demonstrated significant improvement in our study. Mean pruritus NRS decreased by 76%, results that also align with those reported by Miniotti et al. [8] and Beck et al. [9]. Martínez-Doménech et al. [10], however, reported slightly different results. In their study, EASI-75 was achieved by 100% at month 36 and EASI-90 by 92%. However, only 13 patients reached the 36-month time point, and the small sample potentially explains the differences. Importantly, we verified that 88% of patients achieved EASI < 7. A recent international consensus recommends assessing patients using a treat-to-target strategy that sets optimal objectives (including the aforementioned) to ensure minimal residual disease or relapses and helps decide whether to continue or modify strategies [11, 12]. Future studies implementing these targets are needed to uniformize the practice among patients with AD.
Real-world data on long-term dupilumab drug survival up to 30 months or more are still scarce in the literature. Kang et al. [13] analyzed 102 patients and described a probability of survival at 4 years of 80.4%. Reasons for dupilumab withdrawal included primary loss of efficacy (40%), adverse events (20%), high cost (16%), discomfort with short interval between treatments (12%), pregnancy (8%), and clinical remission (4%). Pezzolo et al. [14] reported data from 363 patients and found a drug survival of 78.8% at 3 years and 76.4% at 4 years. In their analysis, the most common causes of discontinuation were ineffectiveness (25%), adverse events (45%), disease remission (18%), and pregnancy (11%). Spekhorst et al. [15] reported a drug survival of 78.6% at year 3 of follow-up in a registry with 715 patients, with 20% withdrawing treatment due to ineffectiveness and 33% due to adverse events. In our study, drug survival at 30 months was 82% and the main reasons for discontinuation were treatment failure, adverse events/safety concerns, disease remission, and pregnancy, results consistent with those found by Kang et al. [13] The fact that we found a superior rate of ineffectiveness compared with Speckhorst et al. [15] (23/39, 59%) may be related to the severity of disease (mean baseline EASI of 27.3 ± 11.9 versus median 15.6, IQR 10.1–24.9, respectively).
Regarding adverse events, we found conjunctivitis to be the most reported (17%). Indeed, dupilumab has been associated with a wide range of side effects on the ocular surface. Rates vary greatly, with a pooled proportion of 26% in a review of real-world studies, higher than initially estimated in clinical trials. Importantly, most cases were treatable and did not lead to drug discontinuation, similarly to what we found [16]. The mechanisms involved in dupilumab-induced conjunctivitis are not clearly understood, and whether conjunctivitis is related to an intrinsic predisposition in patients with AD and worsening of preexisting ocular surface disease or is a true side effect associated with dupilumab remains under discussion [4, 17]. Prospective studies, including complete ophthalmological assessments before starting dupilumab, are needed to establish a causal relationship [18].
In contrast with clinical trials, real-world data are increasingly showing the occurrence of paradoxical erythema of the head and neck during treatment with dupilumab [19, 20]. Waldman et al. [21] performed a characterization of dupilumab facial redness reporting a prevalence of 9.9%, which is clearly in line with our results. In our sample, facial erythema was the second most common adverse event, noted in 9% of the sample. Although the exact mechanism remains under discussion, various etiologies have been proposed, including the dupilumab-associated suppression of the TH2 axis that leads to sensitization toward TH1-biased haptens and subsequent contact hypersensitivity. The differential diagnosis is broad and includes rosacea, allergic contact dermatitis, periorificial dermatitis, and Demodex, among others [19, 20, 22].
We found other side effects of dupilumab to be rare. Herpes simplex infection occurred in 1.6% of patients, and a pooled analysis from the Food and Drug Administration Adverse Event Reporting database estimated an occurrence rate of < 2%, showing no difference between dupilumab, placebo, topical tacrolimus, and topical pimecrolimus, suggesting that this side effect is not related to the drug per se [23]. Alopecia areata occurred in 0.6% of patients, and none of the cases required drug discontinuation. Napolitano et al. [24] recently reported the adverse events related to dupilumab therapy in a cohort of 916 patients, describing the occurrence of alopecia areata in 1.2%, and, similarly, no case required drug discontinuation. While the exact mechanism is still under debate, it has been suggested that dupilumab may induce a Th1/Th17 polarization that interferes with the hair follicle, and the same mechanism has been suggested to be involved in dupilumab-related arthritis [19]. We noted 0.3% of patients reporting arthralgia in our sample, and in half of them, this was a cause for dupilumab withdrawal. The first report of dupilumab-associated arthritis was described in 2019, and it was estimated to occur in up to 5% of patients [25]. Although pregnancy was a reason for discontinuation in our study, recent studies have highlighted that dupilumab may be a safe option in such scenarios [26,27,28]. AD is the most frequent skin disease during gestation and accounts for up to 50% of all pregnancy dermatoses [29]. While there is no specific concern regarding the potential risk of dupilumab in pregnancy, current recommendations suggest the use of other systemic drugs due to scarce evidence of safety [30]. In our study, one patient completed the full pregnancy with no intercurrences, and recent isolated reports describe similar results [28, 31].
Limitations of our study include its retrospective nature and consequent missing information. Predictive analysis was estimated with a limited number of discontinuations, and potential associations may be hidden. Severity disease indexes were not available in medical charts for all patients in all time points; however, the available sample with reported indexes clearly demonstrates the effectiveness of dupilumab in controlling disease activity even in heterogeneous, clinically challenging scenarios, and our results are consistent with the few available long-term reports. The fact that we applied very few exclusion criteria ensures the data are representative of current clinical practice, which may assist clinicians in making their decisions.
Conclusion
Our study contributes valuable evidence confirming the sustained effectiveness and safety of dupilumab, thereby endorsing its long-term use in effectively managing AD among adults and improving quality of life. This finding holds significance particularly in real-world settings, where the challenges of diverse patient profiles are addressed. The demonstrated efficacy of dupilumab in our study underscores its pivotal role in disease control.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Schuler CF, Billi AC, Maverakis E, Tsoi LC, Gudjonsson JE. Novel insights into atopic dermatitis. J Allergy Clin Immunol [Internet]. 2023;151(5):1145–54. Available from: https://doi.org/10.1016/j.jaci.2022.10.023
Sroka-Tomaszewska J, Trzeciak M. Molecular mechanisms of atopic dermatitis pathogenesis. Int J Mol Sci. 2021;22(8).
Torres T, Ferreira EO, Gonçalo M, Mendes-bastos P. Update on Atopic Dermatitis A Dermatite Atópica em Revisão. Orden Dos Médicos [Internet]. 2019;32(9):606–13. Available from: https://doi.org/10.20344/amp.11963
Neagu N, Dianzani C, Avallone G, Dell’Aquila C, Morariu SH, Zalaudek I, et al. Dupilumab ocular side effects in patients with atopic dermatitis: a systematic review. J Eur Acad Dermatology Venereol. 2022;36(6):820–35.
Gooderham MJ, Hong HC ho, Eshtiaghi P, Papp KA. Dupilumab A review of its use in the treatment of atopic dermatitis. J Am Acad Dermatol. 2018;78(3):S28–36. https://doi.org/10.1016/j.jaad.2017.12.022
Koskeridis F, Evangelou E, Ntzani EE, Kostikas K, Tsabouri S. Treatment with dupilumab in patients with atopic dermatitis: systematic review and meta-analysis. J Cutan Med Surg. 2022;26(6):613–21.
Torres T, Paiva-Lopes MJ, Gonçalo M, Claro C, Oliveira M, Gomes J, et al. Dupilumab for atopic dermatitis: a real-world Portuguese multicenter retrospective study. J Dermatolog Treat. 2022;33(5):2554–9. https://doi.org/10.1080/09546634.2022.2035309.
Miniotti M, Ribero S, Mastorino L, Ortoncelli M, Gelato F, Bailon M, et al. Long-term psychological outcome of patients with moderate-to-severe atopic dermatitis continuously treated with dupilumab: data up to 3 years. Exp Dermatol. 2023;32(6):852–8.
Beck LA, Deleuran M, Bissonnette R, de Bruin-Weller M, Galus R, Nakahara T, et al. Dupilumab provides acceptable safety and sustained efficacy for up to 4 years in an open-label study of adults with moderate-to-severe atopic dermatitis. Am J Clin Dermatol. 2022;23(3):393–408. https://doi.org/10.1007/s40257-022-00685-0.
Martínez-Doménech A, Zaragoza-Ninet V, Esteve-Martínez A, García-Rabasco A, Sánchez-Carazo JL, Pérez-Ferriols A. Efficacy and safety of dupilumab for the treatment of severe atopic dermatitis in clinical practice: a single center experience. Actas Dermosifiliogr. 2024;115(2):T150–8.
De Bruin-Weller M, Biedermann T, Bissonnette R, Deleuran M, Foley P, Girolomoni G, et al. Treat-to-target in atopic dermatitis: an international consensus on a set of core decision points for systemic therapies. Acta Derm Venereol. 2021;101(2):1–7.
Yeung J, Gooderham MJ, Hong HCH, Lynde C, Prajapati VH, Lansang P, et al. Treat-to-target in the management of moderate-to-severe atopic dermatitis in adults: a Canadian perspective. J Am Acad Dermatol. 2023;89(2):372–5. https://doi.org/10.1016/j.jaad.2023.01.053.
Kang DH, Kwon SH, Lew BL. Four-year long-term drug survival of dupilumab analyzed by treatment period in patients with moderate to severe atopic dermatitis: a real-world retrospective study. J Dermatol. 2024;51(3):e63–5.
Pezzolo E, Rossi MT, Caroppo F, Bianchelli T, Belloni Fortina A, Giacchetti A, et al. Long-term drug survival of dupilumab and associated predictors in moderate-to-severe atopic dermatitis: a real-world prospective cohort study. J Eur Acad Dermatol Venereol. 2023;37(6):e757–9.
Spekhorst LS, De Graaf M, Zuithoff NPA, Van Den Reek JMPA, Kamsteeg M, Boesjes CM, et al. Dupilumab drug survival and associated predictors in patients with moderate to severe atopic dermatitis: long-term results from the daily practice bioday registry. JAMA Dermatol. 2022;158(9):1048–56.
Halling AS, Loft N, Silverberg JI, Guttman-Yassky E, Thyssen JP. Real-world evidence of dupilumab efficacy and risk of adverse events: a systematic review and meta-analysis. J Am Acad Dermatol. 2021;84(1):139–47. https://doi.org/10.1016/j.jaad.2020.08.051.
Olesen CM, Halling AS. Conjunctivitis in atopic dermatitis patients treated with dupilumab—worsening of pre-existing disease or de novo development? J Eur Acad Dermatol Venereol. 2023;37(7):1258–9.
Achten R, Thijs J, van der Wal M, van Luijk C, Bakker D, Knol E, et al. Ocular surface disease in moderate-to-severe atopic dermatitis patients and the effect of biological therapy. Clin Exp Allergy. 2024;54:241–52.
Camela E, Giampetruzzi AR, De Pità O, Pallotta S, Russo F. Dupilumab in real-life settings: a review of adverse events and their pathogenesis. Expert Opin Drug Saf. 2024;23(4):1–9. https://doi.org/10.1080/14740338.2024.2326480.
Jaros J, Hendricks AJ, Shi VY, Lio PA. A practical approach to recalcitrant face and neck dermatitis in atopic dermatitis. Dermatitis. 2020;31(3):169–77.
Waldman RA, DeWane ME, Sloan B, Grant-Kels JM. Characterizing dupilumab facial redness: a multi-institution retrospective medical record review. J Am Acad Dermatol. 2020;82(1):230–2.
Jo CE, Finstad A, Georgakopoulos JR, Piguet V, Yeung J, Drucker AM. Facial and neck erythema associated with dupilumab treatment: a systematic review. J Am Acad Dermatol. 2021;84(5):1339–47. https://doi.org/10.1016/j.jaad.2021.01.012.
Wang Y, Jorizzo JL. Retrospective analysis of adverse events with dupilumab reported to the United States food and drug administration. J Am Acad Dermatol. 2021;84(4):1010–4. https://doi.org/10.1016/j.jaad.2020.11.042.
Napolitano M, Fabbrocini G, Patruno C. Dupilumab-associated cutaneous adverse events among adult patients with atopic dermatitis: a retrospective study. J Dermatol. 2023;50(7):880–7.
Willsmore ZN, Woolf RT, Hughes C, Menon B, Kirkham B, Smith CH, et al. Development of inflammatory arthritis and enthesitis in patients on dupilumab: a case series. Br J Dermatol. 2019;181(5):1068–70.
Alvarenga JM, Maria Lé A, Torres T. Dupilumab for atopic dermatitis during pregnancy and breastfeeding: a case report. Actas Dermosifiliogr. 2023;S0001–7310(23):00817–27.
Metko D, Alkofide M, Abu-Hilal M. A real-world study of dupilumab in patients with atopic dermatitis including patients with malignancy and other medical comorbidities. JAAD Int. 2024;15:5–11. https://doi.org/10.1016/j.jdin.2024.01.002.
Hong N, Park SY, Kook HD, Lee DH, Jung HJ, Park MY, et al. Atopic dermatitis treated safely with dupilumab during pregnancy and lactation: a case series of four patients. Australas J Dermatol. 2023;2024:1–4.
Balakirski G, Novak N. Atopic dermatitis and pregnancy. J Allergy Clin Immunol. 2022;149(4):1185–94. https://doi.org/10.1016/j.jaci.2022.01.010.
Adam DN, Gooderham MJ, Beecker JR, Hong CH, Jack CS, Jain V, et al. Expert consensus on the systemic treatment of atopic dermatitis in special populations. J Eur Acad Dermatol Venereol. 2023;37(6):1135–48.
Avallone G, Cavallo F, Tancredi A, Maronese CA, Bertello M, Fraghì A, et al. Association between maternal dupilumab exposure and pregnancy outcomes in patients with moderate-to-severe atopic dermatitis: a nationwide retrospective cohort study. J Eur Acad Dermatol Venereol. 2024. https://doi.org/10.1111/jdv.19794.
Acknowledgements
We thank the participants of the study.
Funding
No funding or sponsorship was received for this study.
Author information
Authors and Affiliations
Contributions
Concept and design: Tiago Torres, Maria João Paiva Lopes. Acquisition, analysis, or interpretation of data: Tiago Torres, Maria João Paiva Lopes, Margarida Gonçalo, Paulo Filipe, Bruno Duarte, João Alves, José Miguel Alvarenga, Gilberto Rosa, Duarte Flor, José Ramos, Diogo Sousa, Aureliu Rosca, César Magalhães, Cristina Claro, Joana Rocha, Catarina Vilarinho, Fernando Mota, Alberto Mota. Drafting of the manuscript and critical review: Tiago Torres, Maria João Paiva Lopes, Margarida Gonçalo, Paulo Filipe, Bruno Duarte, João Alves, José Miguel Alvarenga, Gilberto Rosa, Duarte Flor, José Ramos, Diogo Sousa, Aureliu Rosca, César Magalhães, Cristina Claro, Joana Rocha, Catarina Vilarinho, Fernando Mota, Alberto Mota. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Corresponding author
Ethics declarations
Conflict of Interest
Tiago Torres has received consultancy and/or speaker's honoraria from and/or participated in clinical trials sponsored by AbbVie, Almirall, Amgen, Arena Pharmaceuticals, Biocad, Biogen, Boehringer Ingelheim, Bristol Myers Squibb, Celgene, Fresenius Kabi, Janssen, LEO Pharma, Eli Lilly, MSD, Mylan, Novartis, Pfizer, Samsung-Bioepis, Sanofi-Genzyme, Sandoz and UCB. Maria João Cruz has received consultancy and/or speaker's honoraria from AbbVie, Almirall, Beiersdorf, Eli Lilly, Galderma, La Roche-Posay, LEO Pharma, Novartis, Pfizer, Pierre Fabre, Regeneron Pharmaceuticals Inc.and Sanofi. Margarida Gonçalo was a speaker or advisor for Abbvie, Astrazeneca, Eli Lilly, Leo Pharma, Novartis, Pfizer, Sanofi and Takeda. Bruno Duarte has received speaker and/or consultant fees from Sanofi, Eli-Lilly, Abbvie, Pfizer, Leo, Galderma and Janseen. João Alves has received consultancy and/or speaker’s honoraria from AbbVie and Galderma. Alberto Mota has received consultancy and/or speaker's honoraria from AbbVie, Eli Lilly and Co., LEO Pharma, and Sanofi-Genzyme. Paulo Filipe, José Miguel Alvarenga, Gilberto Rosa, Duarte Flor, José Ramos, Diogo Sousa, Aureliu Rosca, César Magalhães, Cristina Claro, Joana Rocha, Catarina Vilarinho, Fernando Mota, and Maria João Paiva Lopes declare no conflicts of interest.
Ethical Approval
The present study was conducted in accordance with the Declaration of Helsinki initially published in 1964 on Ethical Principles for Medical Research Involving Human Subjects and after approval by the local ethical committees. Patients consent was exempted due to the retrospective nature of the study: the study protocol did not deviate from standard clinical practice, and data collection and handling complied with applicable laws, regulations, and guidance regarding patient protection, including patient privacy.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Torres, T., Cruz, M.J., Gonçalo, M. et al. Dupilumab in Patients with Atopic Dermatitis: A Multicentric, Long-Term, Real-World Portuguese Study. Dermatol Ther (Heidelb) (2024). https://doi.org/10.1007/s13555-024-01235-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13555-024-01235-8